Abstract
The ability to rapidly recognize Ebola virus infections is critical to quickly limit further spread of the disease. A rapid, sensitive, and specific laboratory diagnostic test is needed to confirm outbreaks of Ebola virus infection and to distinguish it from other diseases that can cause similar clinical symptoms. A one-tube reverse transcription-PCR assay for the identification of Ebola virus subtype Zaire (Ebola Zaire) and Ebola virus subtype Sudan (Ebola Sudan) was developed and evaluated by using the ABI PRISM 7700 sequence detection system. This assay uses one common primer set and two differentially labeled fluorescent probes to simultaneously detect and differentiate these two subtypes of Ebola virus. The sensitivity of the primer set was comparable to that of previously designed primer sets, as determined by limit-of-detection experiments. This assay is unique in its ability to simultaneously detect and differentiate Ebola Zaire and Ebola Sudan. In addition, this assay is compatible with emerging rapid nucleic acid analysis platforms and therefore may prove to be a very useful diagnostic tool for the control and management of future outbreaks.
Ebola virus is a single-stranded, nonsegmented, negative-sense RNA virus that belongs to the family Filoviridae. It is one of two members (Ebola virus and Marburg virus) that are responsible for sporadic epidemics of hemorrhagic fever in human and nonhuman primates.
Infection with Ebola virus results in rapid disease progression and high mortality rates. The main route of transmission of filoviruses is contact with contaminated bodily fluids, such as through improper needle hygiene, direct contact with infected tissue or fluid samples, or close contact with infected patients, which are the primary routes of transmission (1, 2, 5). Consequently, those at greatest risk for contracting the disease are health care providers and families, who, in rural African communities, may be the primary care providers for sick patients. Because of the mode of transmission, high fatality rates, and the need to institute proper barrier nursing precautions and public health measures during outbreaks, it is essential to establish a diagnosis early in the course of the disease. In regions of Africa where numerous diseases can cause similar clinical syndromes (Lassa fever, Shigella dysentery, and malaria), the diagnosis of filoviral infections can present a challenge. During an Ebola virus outbreak, the ability to establish a rapid diagnosis may help save the lives of patients presenting with treatable diseases such as Shigella dysentery and malaria. In these instances, proper triage of patients depends heavily on a rapid and accurate diagnosis.
Assays currently available for the diagnosis of Ebola virus infections include virus culture, transmission electron microscopy (TEM), immunohistochemistry, antigen detection enzyme-linked immunosorbent assays (ELISAs), antibody detection ELISAs, and a conventional reverse transcription-PCR (RT-PCR) (8, 13, 14, 18, 20). Each method has both advantages and disadvantages; however, few assays that can be used in the field and that are capable of providing a sensitive, specific, and rapid diagnosis are available. Virus culture is sensitive but must be performed in a biological safety level 4 laboratory. TEM is a rapid technique (<3 h), but it is usually available only in well-equipped research facilities (8). Both virus culture and TEM are routinely performed by reference laboratories. Antibody detection ELISAs are often unreliable because patients with symptomatic Ebola virus infections often fail to mount a detectable humoral response prior to death (3, 15). Antigen detection ELISAs are adequate for the detection of Ebola virus infections during the acute stages of infection; however, special precautions must be taken when handling infectious samples. Alternatively, samples can be inactivated with β-propiolactone. To date, the most rapid and potentially deployable assay that also has good clinical sensitivity is based on conventional RT-PCR.
Conventional RT-PCR is a more sensitive method than antigen detection ELISAs and has the advantage of rendering samples noninfectious before use. However, current RT-PCR assays are not capable of detecting all known subtypes of Ebola virus, and they are not compatible with emerging rapid nucleic acid analysis systems (20). Several rapid nucleic acid analysis systems use a fluorogenic probe-based assay to monitor the accumulation of PCR product in real time. With these assays, it is possible to detect a positive sample in 1 h or less. Fluorogenic probes are not incorporated into the design of conventional RT-PCR assays; therefore, these assays are not capable of being monitored on real-time nucleic acid analysis systems. Instead, following RT-PCR, which is routinely performed as two separate steps (an RT step and a PCR step), samples must be analyzed by gel electrophoresis. The total assay time for conventional RT-PCR, including data analysis by gel electrophoresis, can be 3 to 4 h.
The purpose of the present study was to demonstrate a highly sensitive, specific, and rapid assay that would be compatible with emerging rapid nucleic acid analysis platforms.
MATERIALS AND METHODS
Viral growth, purification, and titers.
Ebola, Marburg, and Lassa virus strains were propagated in Vero E6 cells. Crimean-Congo hemorrhagic fever and measles (Edmonston strain) viruses were propagated in Vero cells. Vesicular stomatitis virus was propagated in BHK cells. Upon visualization of 60 to 70% cytopathic effects, the supernatant was harvested and clarified by centrifugation. For Ebola, Marburg, and measles virus purification, the supernatant was clarified by centrifugation at 1,500 × g for 15 min in a Sorvall centrifuge. Polyethylene glycol (PEG; average molecular weight [MW], 8,000) and NaCl were added to the supernatant to final concentrations of 7.5% (wt/vol) and 0.5 M, respectively. Virus was allowed to precipitate for 4 h at 4°C. Precipitated virus was pelleted by centrifugation at 10,000 × g for 30 min and suspended in 5 ml of TNE (10 mM Tris-HCl [pH 8.0], 100 mM NaCl, 1 mM EDTA [pH 8.0]). Suspended virus was then concentrated by ultracentrifugation at 27,000 rpm in a SW28 rotor through a 20 to 60% (wt/wt) sucrose gradient in TNE (10). For Crimean-Congo hemorrhagic fever virus, the supernatant material was precipitated with 8% (wt/vol) PEG containing 2.3% (wt/vol) NaCl for 3 h at 4°C. The precipitate was pelleted, suspended in TNE, and overlaid onto a 15 to 65% (wt/wt) sucrose gradient in TNE. The gradients were centrifuged at 40,000 rpm in a SW41 rotor for 1.5 h at 4°C. Fractions (1 ml) of the gradient were analyzed directly by sodium dodecyl sulfate-polyacrylamide gel electrophoresis as described previously (11). For Lassa virus purification, the supernatant was clarified in a Sorvall centrifuge at 8,000 rpm in a GSA rotor. Seven percent (wt/vol) PEG (average MW, 6,000) and 2.3% (wt/vol) NaCl were added to the supernatant. The virus was then allowed to precipitate for 3 h at 4°C. The precipitate was then purified through a discontinuous 10 to 40% Renografin gradient in an SW41 rotor at 37,000 rpm for 75 min. The visible virus band was harvested, diluted in 3 ml of TNE, and purified through a continuous 10 to 50% Renografin gradient in an SW41 rotor at 30,000 rpm overnight. The virus was harvested, pelleted by centrifugation in an SW41 rotor at 38,000 rpm for 45 min, and suspended in 2 ml of TNE (P. B. Jahrling, unpublished protocol). For vesicular stomatitis virus purification, cell culture supernatants were clarified by centrifugation at 10,000 × g for 30 min. PEG (average MW, 8,000) and NaCl were added to the clarified supernatant to final concentrations of 7 and 2.3%, respectively. Virus was precipitated overnight at 4°C. The precipitated virus was then pelleted by centrifugation at 10,000 × g for 30 min, resuspended in Dulbecco's phosphate-buffered saline (PBS) and then purified by centrifugation through a 20 to 60% (wt/wt) sucrose density gradient for 3.5 h at 100,000 × g. Sucrose solutions were prepared in Hank's balanced salt solution without NaHCO3 containing 0.02 M N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid buffer (pH 7.2) (16).
The titers of the filoviruses were determined by performing plaque assays on Vero E6 cells as described previously (17). Briefly, viral stock was serially diluted in Eagle's minimum essential medium (EMEM) with nonessential amino acids (NEAA), adsorbed onto confluent Vero E6 cells in 12-well dishes, incubated for 1 h at 37°C, and covered with an agarose overlay. A 1:5,000 dilution of neutral red in buffered saline solution was added 7 days later, and plaques were counted the next day.
Primer and probe design.
The characteristics of selected primer and probe sets are listed in Table 1. The sequences of the Zaire and Sudan subtypes of Ebola virus (Ebola Zaire and Ebola Sudan, respectively) were aligned by using the DNA Star MegAlign software. After careful study of the aligned sequences, an 111-bp region of the glycoprotein (GP) was targeted for primer and probe development. In order to achieve efficient amplification of the Ebola Zaire and Ebola Sudan templates, degenerate primers were designed. The EBOGP-1D primer and double-probe set (Table 1) was designed by evaluating the Ebola virus GP gene (GenBank Accession numbers U77384 [Ebola virus subtype Gabon-94], U31033 [Ebola Zaire], U28134 [Ebola Sudan, Boniface strain], U23069 [Ebola Sudan, Maleo strain], U23417 [Ebola virus subtype Reston, Siena strain]) with Primer Express Software (Applied Biosystems, Foster City, Calif.). The primer and double-probe set was designed to meet the guidelines recommended by Applied Biosystems. In brief, the primers were designed with melting temperatures (Tms) between 58 and 60°C. Probes were designed to have a Tm at least 7 to 10°C higher than the Tms of the primers. The presence of a guanine at the 5′ ends of the probes was avoided, and the amplicons were designed to be less than 200 bp in length. Primer and probe dimers, hairpins, stem-loops, and false priming sites were avoided.
TABLE 1.
Sensitivity of Ebola virus primer-probe sets
| Primer set | Target genea | Assayb | Amplicon length (bp) | LOD for Ebola Zairec
|
LOD for Ebola Sudan
|
Reference or source | ||
|---|---|---|---|---|---|---|---|---|
| PFU | Mass | PFU | Mass | |||||
| ZAI-NP1/NP2 | NP | − | 268 | 8 | 10 fg | NDd | ND | 20 |
| FILOA/FILOB | L | − | 419 | 8 | 10 fg | 74 | 1 pg | 20 |
| EBO-GP1/2 | GP | − | 580 | 680 | 100 pg | 770 | 100 pg | 20 |
| EBOGP1D-DblPrb | GP | + | 111 | 8 | 10 fg | 3 | 100 fg | Newly designed assay |
NP, Ebola virus nucleoprotein; L, Ebola virus polymerase; GP, Ebola virus glycoprotein.
+, TaqMan assay; −, conventional RT-PCR.
PFU LODs are based on a known number of PFU from which viral RNA was extracted. Mass LODs are based on known amounts of purified viral RNA.
ND, not detected.
Two differentially labeled fluorogenic probes that would hybridize to the template between the EBOGP-1D PCR primers were designed. An Ebola Zaire-specific probe which has a covalently linked fluorescent reporter dye, 6-carboxyfluorescein (FAM), attached to the 5′ end and a quencher dye, 6-carboxytetramethylrhodamine (TAMRA), covalently attached to its 3′ end was designed to recognize the Ebola Zaire template. An Ebola Sudan-specific probe which has a covalently linked fluorescent reporter dye, VIC, attached to the 5′ end and a quencher dye, TAMRA, covalently attached to its 3′ end was designed to recognize the Ebola Sudan template. Depending on the template present in the sample, either the FAM-labeled Ebola Zaire-specific probe or the VIC-labeled Ebola Sudan-specific probe would generate a fluorescent signal. These signals could be distinguished from one another on the basis of their emission spectra.
The sequences of the primers and probes are as follows: 5′-TGGGCTGAAAAYTGCTACAATC-3′ for the EBOGP-1D forward primer and 5′-CTTTGTGMACATASCGGCAC-3′ for the EBOGP-1D reverse primer. The probe sequences are 5′-CTACCAGCAGCGCCAGACGG-3′ for EBOGP-1DZPrb and 5′-TTACCCCCACCGCCGGATG-3′ for EBOGP-1DSPrb.
Fluorogenic 5′ nuclease assays.
The RT-PCR assays were performed on an ABI PRISM 7700 sequence detection system with an Applied Biosystems TaqMan EZ RT-PCR kit in accordance with the manufacturer's instructions. Thermocycling conditions for the EBOGP-1D primer and double-probe set were as follows: 55°C for 45 min and 94°C for 1 min followed by 40 cycles at 94°C for 15 s and 60°C for 30 s. The final concentrations used in the 50-μl reaction mixture were as follows: 0.5 μM each primer, 0.2 μM each probe, 5 U of rTth enzyme, 300 μM deoxynucleotide triphosphates, 1× Applied Biosystems TaqMan RT-PCR buffer containing the passive reference dye ROX, and 2.5 mM manganese acetate. The total assay time on the ABI PRISM 7700 sequence detection system was approximately 2 h.
Conventional RT-PCR assays.
Previously published primer sets (Table 1) were tested by using the Applied Biosystems EZ rTth RNA PCR kit in accordance with the manufacturer's instructions. Thermocycling conditions for each set were published previously (20). The final concentrations used in the 50-μl reaction mixture were as follows: 0.5 μM each primer, 5 U of rTth enzyme, 300 μM deoxynucleotide triphosphates, 1× Applied Biosystems EZ buffer, and 2.5 mM manganese acetate. All assays were performed on a PTC 100 thermocycler (MJ Research, Waltham, Mass.).
Direct analysis and detection of RT-PCR-amplified products on agarose gels.
Ten-microliter aliquots of the RT-PCR products were electrophoresed on 4% agarose gels (NuSieve; FMC BioProducts, Rockland, Maine) in Tris-borate-EDTA buffer (TBE) containing 1 μg of ethidium bromide per ml. The DNA bands were visualized with an imaging system (Alpha Inotech Corporation, San Leandro, Calif.).
Sequencing of RT-PCR products.
To confirm the identities of the PCR products, amplicons from RT-PCR were sequenced with dye-labeled terminators and by cycle sequencing (Taq Prism kit; Applied Biosystems, Foster City, Calif.). The products from the sequencing reactions were analyzed on an Applied Biosystems 377 sequencer. The sequences were then identified with the National Center for Biotechnology Information's Basic Local Alignment Search Tool (BLAST; http://www.ncbi.nlm.nih.gov/BLAST/).
LOD assays.
To determine the limits of detection (LODs) of the numbers of PFU, serial 10-fold dilutions of sucrose-purified Ebola virus seeds (Zaire and Sudan subtypes) were prepared in 1 ml of EMEM with NEAA. Control samples lacking template were prepared with virus-free EMEM with NEAA. One hundred microliters of each dilution was placed in Trizol LS (Gibco BRL, Gaithersburg, Md.), and RNA was isolated in accordance with the manufacturer's instructions. Briefly, chloroform was added to the virus-Trizol LS mixture, the mixture was centrifuged, and the aqueous phase containing the RNA was harvested. The RNA was then precipitated with isopropanol, washed with 75% ethanol, and resuspended in 100 μl of RNase-free water. One microliter of each RNA preparation was used in subsequent TaqMan assays. To determine the number of PFU per dilution, serial 10-fold dilutions were assayed on Vero E6 cells as described above. The LOD was defined as the last dilution in the fluorogenic 5′ nuclease assays in which the threshold cycle (CT value) was less than 40.
To determine LODs by mass, sucrose-purified virus was placed in Trizol LS (Gibco BRL) and the RNA was isolated as described above. The RNA was quantitated by spectrophotometry, and serial 10-fold dilutions containing from 1 ng to 10 fg were prepared. One microliter of each dilution was used in subsequent TaqMan and conventional RT-PCR assays. All assays were performed in triplicate. The LODs of the newly designed Taqman assay were compared to the LODs of previously designed Ebola primers (Table 1).
Spiked clinical samples.
Whole blood, plasma, and serum were collected from nonhuman primates. One hundred microliters each of blood, plasma, serum, and PBS was spiked with known amounts (ranging from 78, 125 to 25 PFU) of sucrose-purified Ebola Zaire. One hundred microliters of EMEM with NEAA was added to each spiked sample, and each sample was placed in the appropriate volume of Trizol LS (Gibco BRL). The RNA was isolated as described above and was resuspended in a volume of 20 μl. Five microliters of each RNA preparation was used in subsequent TaqMan assays.
Cross-reactivity panel.
To evaluate for potential cross-reactivity of the EBOGP-1D primer-probe set, RNA was isolated from genetically related viruses (vesicular stomatitis virus, measles virus, and Marburg virus strains Musoke, Ravn, and Ci67) and other hemorrhagic fever viruses (Lassa virus and Crimean-Congo hemorrhagic fever virus). RNAs were extracted from purified seeds of these viruses with Trizol LS, as described above. One nanogram of each viral template was used for cross-reactivity testing. The cross-reactivity panel was blinded by an independent investigator who assigned random numbers to each sample.
RESULTS
TaqMan primer-probe design.
Two hundred sets of primers and probes specific for a highly conserved region of the Ebola Zaire and Ebola Sudan GP gene were generated by using Primer Express software. The EBOGP-1D primer and double-probe set was chosen on the basis of guidelines recommended by Applied Biosystems, outlined above. The primer and double-probe set chosen, EBOGP-1D, was designed to amplify a 111-bp region of the GP gene. The EBOGP-1D primers are degenerate primers designed to amplify both Ebola Zaire and Ebola Sudan. Because of sequence variability, degenerate primers were required to achieve efficient amplification of both templates. The probes specific for each virus (Ebola Zaire or Ebola Sudan) were designed so that there was 100% homology with the appropriate template. The probes were designed for the same sequence of the Ebola virus GP gene; however, the strains differed by seven nucleotides in this region.
Specificity of a double-probe assay for Ebola Zaire and Ebola Sudan templates.
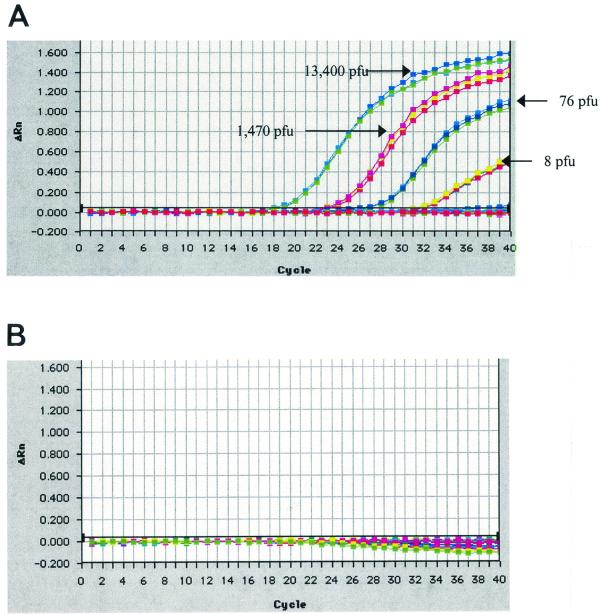
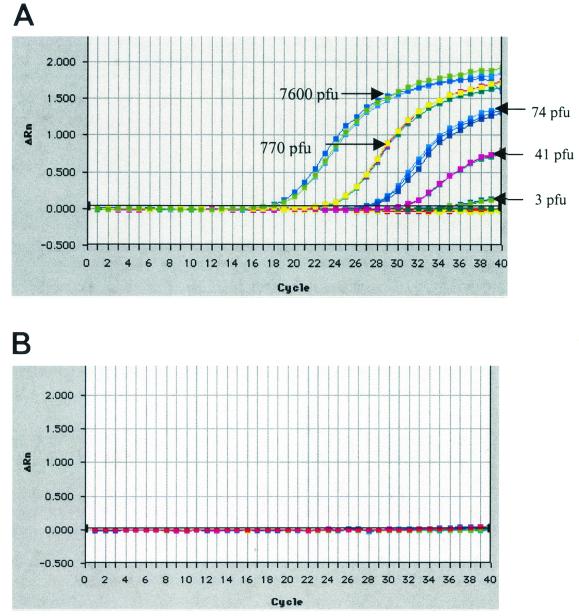
The sequence variability between the two subtypes of Ebola virus (>40%) necessitated the design of a degenerate primer set to efficiently amplify both targets (18, 19). The FAM-labeled Ebola Zaire probe was specific for Ebola Zaire (Fig. 1). Likewise, the VIC-labeled Ebola Sudan probe was specific for Ebola Sudan (Fig. 2). If we observed a CT value less than 40 with the FAM-labeled probe, we positively identified the template as Ebola Zaire. Likewise, if we observed a CT value less than 40 with the VIC-labeled probe, we positively identified the template as Ebola Sudan (Fig. 1 and 2).
FIG. 1.
LOD of EBOGP-1D TaqMan assay for Ebola Zaire with a FAM-labeled Ebola Zaire-specific probe (A) and a VIC-labeled Ebola Sudan-specific probe (B). Total RNA isolated from serial dilutions of sucrose-purified virus was used as the template. Each assay was performed in triplicate. The graphs depict amplification plots for the Ebola Zaire template obtained with both probes. Amplification plots show that the VIC-labeled Ebola Sudan-specific probe does not cross-react with the Ebola Zaire template. ΔRn, change in fluorescence.
FIG. 2.
LOD of EBOGP-1D TaqMan Assay for Ebola Sudan with a VIC-labeled Sudan specific probe (A) and a FAM-labeled Ebola Zaire-specific probe (B). Total RNA isolated from serial dilutions of sucrose-purified virus was used as the template. Each assay was performed in triplicate. The graphs depict amplification plots for the Ebola Sudan template obtained with both probes. Amplification plots show that the FAM-labeled Ebola Zaire-specific probe does not cross-react with the Ebola Sudan template. ΔRn, change in fluorescence.
LOD experiments: assay sensitivity.
The EBOGP-1D primer and double-probe set was as sensitive or more sensitive than previously designed primer sets intended for use in conventional RT-PCR assays (Table 1). The EBOGP-1D primer-probe set was able to detect 10 fg and 8 PFU of purified Ebola Zaire RNA and infectious virus, respectively (Table 1 and Fig. 1A), and 100 fg and 3 PFU of purified Ebola Sudan RNA and infectious virus, respectively (Table 1 and Fig. 2A). Previously designed primer sets (Table 1) for use in conventional RT-PCR assays were able to detect 10 fg and 8 PFU (ZAI-NP1/NP2 and FILOA/FILOB) or 100 pg and 680 PFU (EBOGP1/2) of purified Ebola Zaire RNA and infectious virus, respectively. These same primer sets detected 1 pg and 74 PFU (FILOA/FILOB) or 100 pg and 770 PFU (EBOGP1/2) of Ebola Sudan RNA or infectious virus, respectively. ZAI-NP1/NP2 was not able to detect Ebola Sudan (Table 1). All control samples lacking template were negative.
Assay specificity.
Several genetically related viruses and other hemorrhagic fever viruses were used to determine the cross-reactivity of the EBOGP-1D primer and double-probe set. By using TaqMan chemistry, the EBOGP-1D primer and double-probe set detected Ebola Zaire and Ebola Sudan RNAs; however, it did not detect any of the genetically related or other hemorrhagic fever viruses (Table 2). When examined by gel electrophoresis, the EBOGP-1D primer set also amplified Ebola virus subtype Reston RNA. The amplification efficiency of Ebola virus subtype Reston was not as great as that for Ebola Zaire or Ebola Sudan. EBOGP-1D was able to detect only 1 ng of subtype Reston RNA. Ebola virus subtype Reston was not detected by fluorescence during TaqMan assays. The FILOA/FILOB primer set was able to detect Ebola Zaire, Ebola Sudan, and Ebola virus subtype Ivory Coast (a very weak amplicon was observed with 1 ng of Ebola virus subtype Ivory Coast RNA); however, it also amplified Marburg virus strains Musoke and Ci67. ZAI-NP1/NP2 detected only Ebola Zaire. Therefore, the FILOA/FILOB primer set was not specific for Ebola Zaire or Ebola Sudan and the ZAI-NP1/NP2 primer set was capable of detecting only Ebola Zaire (Table 2). The previously designed EBO-GP1/2 primer set amplified Ebola virus subtypes Zaire, Sudan, and Reston. The amplification efficiency of the EBOGP1/2 primer set was weak with the Ebola virus subtype Reston and Ebola virus subtype Ivory Coast templates. The LOD for EBOGP1/2 with the subtype Reston and Ivory Coast templates was 1 ng (data not shown).
TABLE 2.
Cross-reactivity panel with Ebola virus primer sets
| Primer set | Detection of the followinga:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lassa | Measles | VSV | CCHF | Ebo-Z | Ebo-S | Ebo-IC | Ebo-R | MBG-RAVN | MBG-MSK | MBG-Ci67 | |
| EBOGP-1D | − | − | − | − | + | + | − | + | − | − | − |
| ZAI-NP1/NP2b | ND | ND | ND | ND | + | − | − | − | − | − | − |
| FILOA/FILOBb | ND | ND | ND | ND | + | + | + | − | − | + | + |
| EBOGP1/2b | ND | ND | ND | ND | + | + | − | + | − | − | − |
+, amplicon detected; −, no amplicon detected; ND, no data; Lassa, Lassa virus; Measles, measles virus; VSV, vesicular stomatitis virus; CCHF, Crimean-Congo hemorrhagic fever virus; Ebo-Z, Ebola Zaire; Ebo-S, Ebola Sudan; Ebo-IC, Ebola virus subtype Ivory Coast; Ebo-R, Ebola virus subtype Reston; MBG-RAVN, Marburg virus strain Ravn; MBG-MSK, Marburg virus strain Musoke; MBG-Ci67, Marburg virus strain Ci67.
Previously designed primer sets.
Assay performance in clinical matrices.
The performance of the EBOGP-1D TaqMan assay in clinical matrices was tested by spiking whole blood, serum, and plasma from non-human primates with known amounts of Ebola Zaire (ranging from 78,125 to 25 PFU). PBS was spiked with virus as a control. The sensitivity of the assay in clinical matrices was similar to that observed in PBS, with 5 PFU being the LOD (Table 3).
TABLE 3.
PCR results from clinical matrices spiked with Ebola Zaire
| No. of PFU/5 μl of templatea |
CTb value
|
|||
|---|---|---|---|---|
| PBS | Blood | Serum | Plasma | |
| 15,625 | 22.4 | 19.2 | 22.2 | 19.4 |
| 3,125 | 22.7 | 22.2 | 21.7 | 23.1 |
| 625 | 26.6 | 24.8 | 25.2 | 24.6 |
| 125 | 29.4 | 28.6 | 26.9 | 26.5 |
| 25 | 30.8 | 33.5 | 29.3 | 31.9 |
| 5 | 35.1 | 32.1 | 30.3 | 32.2 |
Number of PFU present in the PCR mixture.
CT is the cycle number at which the fluorescence generated within a reaction crosses the threshold. PBS, blood, serum, and plasma were spiked with known numbers of PFU of Ebola Zaire. The sensitivity of the EBOGP-1D primer-probe set was tested in these matrices.
DISCUSSION
Here we have reported on the development and evaluation of a fluorogenic double-probe-based, one-step RT-PCR assay on the ABI PRISM 7700 sequence detection system for the identification of Ebola Zaire and Ebola Sudan infections. This assay is based on the 5′ nuclease assay, which exploits the 5′ nuclease activity of rTth polymerase to cleave a nonextendable, dual-labeled fluorogenic probe that is annealed to the target sequence during amplification (4, 7, 12). We chose the GP gene of Ebola virus as an assay target for several reasons. First, the GP protein of Ebola virus is required for entry into cells. Second, the membrane-bound GP of Ebola virus is reported to play a central role in the virus-mediated cytotoxicity of endothelial cells and therefore appears to be an important virulence factor of Ebola virus (21). Finally, sequence analysis of the GP genes of Ebola Zaire and Ebola Sudan revealed that regions within this gene would permit the design of a primer-probe set on the basis of the guidelines set forth by Applied Biosystems. This assay has several advantages over the conventional RT-PCR assays used to detect Ebola virus. First, the use of a fluorogenic probe results in an increased level of specificity compared to that of conventional RT-PCR. The EBOGP-1D primer and double-probe set was specific for Ebola Zaire and Ebola Sudan when it was tested in a blinded cross-reactivity panel (Table 2). In contrast, a previously designed primer-probe set (FILOA/FILOB) amplified two of three Marburg virus strains tested and therefore lacked the specificity of the EBOGP-1D primer and double-probe set (Table 2). ZAI-NP1/NP2 was capable of identifying only Ebola Zaire. Second, this assay provides the capability of simultaneously detecting and differentiating two of the three subtypes of Ebola virus that are pathogenic for humans. This unique feature will provide public health officials with an assay that can not only identify an Ebola virus outbreak but also give them the information they need to predict probable mortality rates and the severities of epidemics. Ebola Zaire infections traditionally result in higher fatality rates during an outbreak compared to the fatality rates that result from Ebola Sudan infections. Third, the one-tube fluorogenic RT-PCR assay is compatible with emerging rapid nucleic acid analysis platforms (6). These new platforms are capable of performing both thermocycling and fluorescence detection in real time. Sources of these instruments include Applied Biosystems, Roche Diagnostics (Indianapolis, Ind.), Idaho Technologies (Salt Lake City, Utah), Cepheid (Sunnyvale, Calif.), and Bio-Rad (Hercules, Calif.). With the more rapid thermocycling instruments, i.e., Lightcycler (Roche Molecular Systems), the Ruggedized Advanced Pathogen Identification Device (R.A.P.I.D.; Idaho Technologies), or the SmartCycler (Cepheid), it is reasonable to assume that once a sample is received and processed, a definitive diagnosis can be made within 20 to 40 min (9). In addition, the use of this technology in field laboratories has become a reality now that instruments such as the R.A.P.I.D. and SmartCycler XC instruments, which have been specifically designed for use by field medical laboratories, have become available (9).
In order to obtain an early diagnosis and contain future outbreaks of Ebola hemorrhagic fever, it will be necessary to implement rapid diagnostic assays in laboratories throughout Africa. These assays must be simple to perform, accurate, and reproducible. Transfer of the newly designed fluorogenic 5′ nuclease assay described in this report to rapid nucleic acid analysis platforms would be a first step toward providing public health authorities in Africa with a tool to help diagnose and contain possible outbreaks.
This assay will allow public health officials to detect two of the three Ebola virus subtypes recognized to be pathogenic for humans. The sequence divergence among Ebola virus subtypes Zaire, Sudan, and Ivory Coast prevented the design of a primer set that could efficiently amplify all three strains. Therefore, future developments should include the design of an assay that identifies Ebola virus subtype Ivory Coast. Successful multiplexing of a newly designed Ebola virus subtype Ivory Coast assay with the EBOGP-1D assay would provide the capability of detecting and differentiating all known Ebola virus subtypes that are pathogenic for humans. In addition, the design of a rapid detection assay that is capable of detecting all known strains of filoviruses would provide a screening tool for differentiation of filoviral hemorrhagic fevers from other more common diseases that occur throughout regions of Africa. Future developments that produce a “dried-down” chemistry for RT-PCR (making the addition of water and sample the only reagents needed for performance of the fluorogenic RT-PCR assay) should make this assay even easier to use in the field and would provide a valuable diagnostic capability that would enhance future outbreak investigations.
ACKNOWLEDGMENTS
We thank Deanna Bridge, Bill Hurtle, Steven Kerby, and Brian Kearney for excellent technical assistance. We also thank David Shoemaker and George Ludwig for helpful suggestions and critical input in the preparation of the manuscript. We are especially indebted to George Ludwig for providing Lassa virus, Crimean-Congo hemorrhagic fever virus, measles virus, and vesicular stomatitis virus seeds for growth and purification.
REFERENCES
- 1.Anonymous. Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team. Bull W H O. 1978;56:247–270. [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymous. Ebola haemorrhagic fever in Zaire, 1976. Bull W H O. 1978;56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 3.Baize S, Leroy E M, Georges-Courbot M C, Capron M, Lansoud-Soukate J, Debre P, Fisher-Hoch S P, McCormick J B, Georges A J. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat Med. 1999;5:423–426. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- 4.Bassler H A, Flood S J, Livak K J, Marmaro J, Knorr R, Batt C A. Use of a fluorogenic probe in a PCR-based assay for the detection of Listeria monocytogenes. Appl Environ Microbiol. 1995;61:3724–3728. doi: 10.1128/aem.61.10.3724-3728.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Update: management of patients with suspected viral hemorrhagic fever—United States. JAMA. 1995;274:374–375. [PubMed] [Google Scholar]
- 6.Espy M J, Uhl J R, Mitchell P S, Thorvilson J N, Svien K A, Wold A D, Smith T F. Diagnosis of herpes simplex virus infections in the clinical laboratory by LightCycler PCR. J Clin Microbiol. 2000;38:795–799. doi: 10.1128/jcm.38.2.795-799.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eun A J, Seoh M, Wong S. Simultaneous quantitation of two orchid viruses by the TaqMan real-time RT-PCR. J Virol Methods. 2000;87:151–160. doi: 10.1016/S0166-0934(00)00161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geisbert T W, Jahrling P B. Differentiation of filoviruses by electron microscopy. Virus Res. 1995;39:129–150. doi: 10.1016/0168-1702(95)00080-1. [DOI] [PubMed] [Google Scholar]
- 9.Henchal E A, Teska J D, Ludwig G V, Shoemaker D R, Ezell J W. Current laboratory methods for biological threat agent identification. Clin Lab Med. 2001;21:7.1–7.13. [PubMed] [Google Scholar]
- 10.Hevey M, Negley D, Geisbert J, Jahrling P, Schmaljohn A. Antigenicity and vaccine potential of Marburg virus glycoprotein expressed by baculovirus recombinants. Virology. 1997;239:206–216. doi: 10.1006/viro.1997.8883. [DOI] [PubMed] [Google Scholar]
- 11.Hodgsen L. The sequence, genomic organization, and expression of the small genomic segment of Crimean Congo hemorrhagic fever virus for the potential use as a diagnostic antigen. Frederick, Md: Hood College; 1992. [Google Scholar]
- 12.Holland P M, Abramson R D, Watson R, Gelfand D H. Detection of specific polymerase chain reaction product by utilizing the 5′-3′ exonuclease activity of Thermus aquaticus DNA polymerase. Proc Natl Acad Sci USA. 1991;88:7276–7280. doi: 10.1073/pnas.88.16.7276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ksiazek T G, Rollin P E, Jahrling P B, Johnson E, Dalgard D W, Peters C J. Enzyme immunosorbent assay for Ebola virus antigens in tissues of infected primates. J Clin Microbiol. 1992;30:947–950. doi: 10.1128/jcm.30.4.947-950.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leroy E M, Baize S, Lu C Y, McCormick J B, Georges A J, Georges-Courbot M C, Lansoud-Soukate J, Fisher-Hoch S P. Diagnosis of Ebola haemorrhagic fever by RT-PCR in an epidemic setting. J Med Virol. 2000;60:463–467. [PubMed] [Google Scholar]
- 15.Leroy E M, Baize S, Volchkov V E, Fisher-Hoch S P, Georges-Courbot M C, Lansoud-Soukate J, Capron M, Debre P, McCormick J B, Georges A J. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355:2210–2215. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- 16.Ludwig G V, Kondig J P, Smith J F. A putative receptor for Venezuelan equine encephalitis virus from mosquito cells. J Virol. 1996;70:5592–5599. doi: 10.1128/jvi.70.8.5592-5599.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moe J B, Lambert R D, Lupton H W. Plaque assay for Ebola virus. J Clin Microbiol. 1981;13:791–793. doi: 10.1128/jcm.13.4.791-793.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. Filoviridae: Marburg and Ebola viruses. In: Fields B N, Knipe D M, Howley P M, et al., editors. Fields Virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Press; 1996. pp. 1161–1176. [Google Scholar]
- 19.Sanchez A, Kiley M P, Holloway B P, Auperin D D. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 1993;29:215–240. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez A, Ksiazek T G, Rollin P E, Miranda M E, Trappier S G, Khan A S, Peters C J, Nichol S T. Detection and molecular characterization of Ebola viruses causing disease in human and nonhuman primates. J Infect Dis. 1999;179(Suppl. 1):S164–S169. doi: 10.1086/514282. [DOI] [PubMed] [Google Scholar]
- 21.Yang Z Y, Duckers H J, Sullivan N J, Sanchez A, Nabel E G, Nabel G J. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]