Abstract
Objectives
Severe cases of COVID-19 have overwhelmed hospital systems across the nation. This study aimed to describe the healthcare resource utilization of patients with COVID-19 from hospital visit to 30 days after discharge for inpatients and hospital-based outpatients in the United States.
Methods
A retrospective cohort study was conducted using Premier Healthcare Database COVID-19 Special Release, a large geographically diverse all-payer hospital administrative database. Adult patients (age ≥ 18 years) were identified by their first, or “index,” visit between April 1, 2020, and February 28, 2021, with a principal or secondary discharge diagnosis of COVID-19.
Results
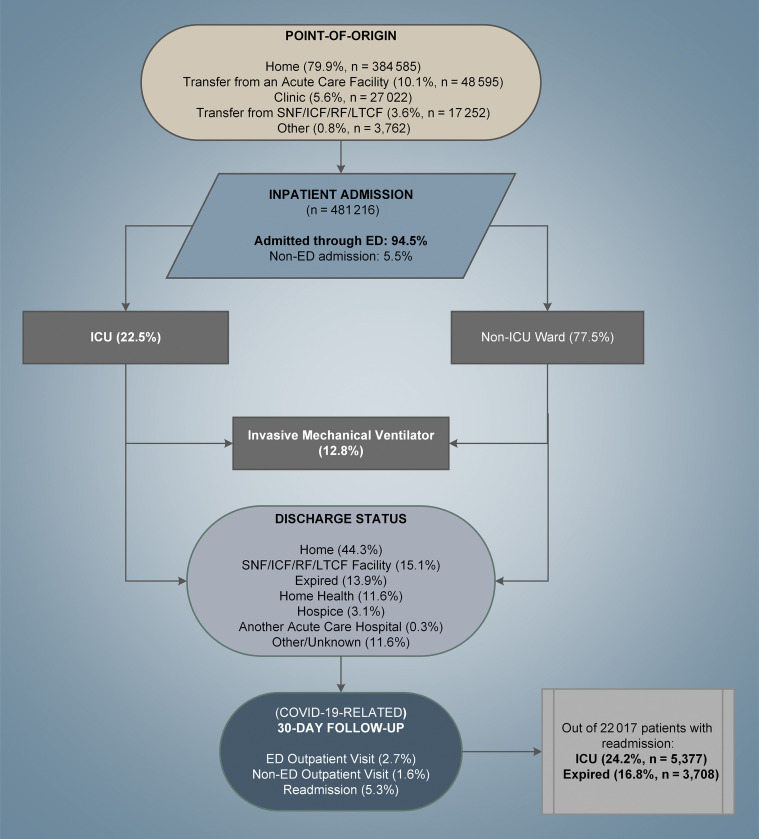
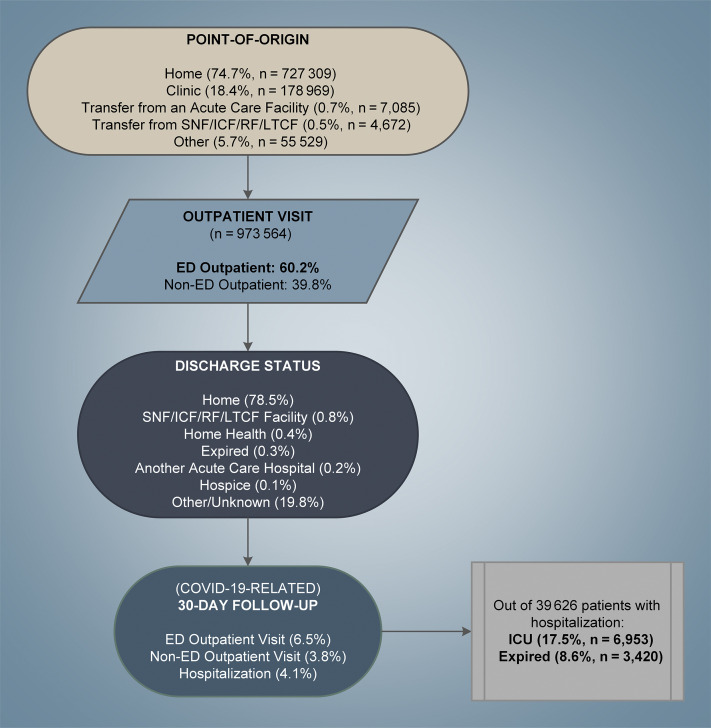
Of 1 454 780 adult patients with COVID-19, 33% (n = 481 216) were inpatients and 67% (n = 973 564) were outpatients. Among inpatients, mean age was 64.4 years and comorbidities were common. Most patients (80%) originated from home, 10% from another acute care facility, and 95% were admitted through the emergency department. Of these patients, 23% (n = 108 120) were admitted to intensive care unit and 14% (n = 66 706) died during index hospitalization; 44% were discharged home, 15% to nursing or rehabilitation facility, and 12% to home health. Among outpatients, mean age was 48.8 years, 44% were male, and 60% were emergency department outpatients (n = 586 537). During index outpatient visit, 79% were sent home but 10% had another outpatient visit and 4% were hospitalized within 30 days.
Conclusions
COVID-19 is associated with high level of healthcare resource utilization and in-hospital mortality. More than one-third of inpatients required post hospital healthcare services. Such information may help healthcare providers better allocate resources for patients with COVID-19 during the pandemic.
Keywords: COVID-19, healthcare resource utilization, hospital setting
Introduction
The level of community infection and hospital volume of COVID-19 are closely associated with patient outcomes.1, 2, 3, 4 When healthcare resources are limited, patients may not get appropriate treatment and those who would be admitted under normal circumstances may be sent home.5 Furthermore, clinicians are compelled to choose inpatients who would benefit more from resource use (ie, intensive care unit [ICU] admission, invasive mechanical ventilator [IMV] use).6 A recent study found that between March 2020 and August 2020, approximately 23% of COVID-19 deaths were associated with hospitals strained with caseload.7
Although public health measures lowered COVID-19 caseload in hospitals after the initial surge in March and April 2020, the number of COVID-19–related hospital visits remained high throughout 2020.1 , 2 , 8, 9, 10, 11 Furthermore, the number of new cases increased substantially in October 2020 through February 2021, possibly overwhelming the hospital systems again.10 , 11
To adequately allocate resources, a comprehensive understanding of healthcare resource utilization (HRU) among patients with COVID-19 is needed, including the source of admission, ICU and IMV use, discharge status, and any other HRU after discharge. Furthermore, the pandemic situation is volatile and much has changed in managing the disease during 2020 and 202112, 13, 14, 15; it would be prudent to examine how the HRU of patients changed across different time periods.
The main objective of this study is to describe the HRU of patients with COVID-19 from the first, or “index,” hospital visit to 30 days after discharge for inpatients and hospital-based outpatients in the United States, overall, and during “early” (April 2020 to June 2020), “middle” (July 2020 to November 2020), and “later” (December 2020 to February 2021) periods using national real-world data.
Methods
Data Source
This study used the Premier Healthcare Database (PHD) COVID-19 Special Release (PHD-SR)—a subset of PHD timely released to accommodate urgent COVID-19 research needs.16 The PHD-SR contains data from approximately 800+ hospitals and is currently used by the National Institute of Health and the Centers for Disease Control and Prevention for COVID-19–related studies.17, 18, 19, 20
The PHD is an all-payer hospital administrative database for geographically diverse inpatient and outpatient visits.21 Inpatient discharges in PHD represent approximately 20% to 25% of all inpatient admissions in the United States since 2000. Outpatient discharges included visits to the emergency department (ED), ambulatory surgery center, hospital-based special clinic, and alternate sites of care. PHD patients are tracked within the same hospital or hospital system using a unique identifier. The standard hospital discharge files include demographic characteristics, disease states, and a time-stamped log of billed items (eg, procedures, medications, laboratory services, and diagnostic services) at the patient level and geographic location, rural/urban populations served, teaching status, and bed capacity at the hospital level.
Study Design and Population
A retrospective cohort study was performed for all adult patients (age ≥ 18 years on admission) with COVID-19–related visits in PHD-SR. COVID-19–related inpatient and outpatient visits were identified using the principal or secondary discharge diagnosis of COVID-19 (International Classification of Diseases, 10th revision, Clinical Modification [ICD-10-CM] diagnosis code U07.1) and discharge dates between April 1, 2020, and February 28, 2021.22 For each patient, the first visit within study period was designated as the “index” visit—which was used to categorize patients as inpatient or outpatient. Any subsequent hospital visits within 30 days of index visit discharge were captured in 30-day follow-up.
All data were statistically deidentified and compliant with the Health Insurance Portability and Accountability Act. Based on US Title 45 Code of Federal Regulations, Part 46, the study was exempted from institutional review board approval. We did not pursue an informed consent of study participants because of the nature of deidentified data. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology23 reporting guideline.
Endpoints
Endpoints during index visit included point of origin (ie, nonhealthcare facility, clinic, transfer from an acute care facility, transfer from skilled nursing facility [SNF] or intermediate care facility [ICF] or rehabilitation facility [RF] or long-term care facility [LTCF], other), admission through the ED, discharge status (ie, expired, home, home health, transfer to SNF/ICF/RF/LTCF, transfer to another acute care facility, hospice, other), and in-hospital mortality (patient’s discharge status equal to “expired”) during index visit. For inpatients only, the following endpoints during index hospitalization were also included: ICU admission, IMV use, extracorporeal membrane oxygenation (ECMO) use, total hospital length of stay, and ICU length of stay. Endpoints during 30-day follow-up (among patients who did not die during index visit) included COVID-19–related ED visits, non-ED outpatient visits, hospitalizations (readmissions for inpatients and return hospitalizations for outpatients), hospitalizations with ICU admission, and in-hospital mortality.
ICU admission was identified when the patient incurred any ICU room and board charges (observations after surgery and step-down ICU were excluded). IMV and ECMO use were captured using ICD-10-CM procedure codes (IMV, 5A1935Z, 5A1945Z, 5A1955Z; ECMO, 5A1522%, 5A051%, 5A052%) and Current Procedural Terminology codes (ECMO, 33946-33949, 33951-33959, 33962-33966, 33969, 33984-33989).
Patient, Visit, and Hospital Characteristics
Patient demographic and clinical characteristics assessed at index visit included age, sex, self-reported race and ethnicity, primary insurance payer, and comorbidities. Hospital characteristics included urbanicity of population served (ie, urban or rural), teaching status, US census region (ie, Midwest, Northeast, South, or West), and bed size (ie, 1-299, 300-499, 500+ beds).
Comorbidities known to be associated with COVID-19 severity (ie, hypertension, history of smoking, morbid obesity) and individual comorbidities in the Charlson-Deyo comorbidity index (CCI)24 were identified using ICD-10-CM discharge diagnosis codes during index or any previous visit to the same hospital within 180 days. Weighted CCI score categories (0, 1-4, 5+) were also examined using a previously validated method.25
Statistical Analysis
We used descriptive statistics to present baseline patient, visit, and hospital characteristics of patients with COVID-19 and their HRU, separately for inpatients and outpatients. We also stratified the results based on discharge month, as “early” (April 2020 to June 2020), “middle” (July 2020 to November 2020), and “later” periods (December 2020 to February 2021). June and November were theoretical cutoff points based on changes in in-hospital mortality and hospital COVID-19 caseloads.8 , 12 , 13 For statistical difference, we used one-way analysis of variance (ANOVA) test for continuous variables and chi-square test for categorical variables.
We then fitted multivariable logistic regression models to assess associations between time of discharge and in-hospital mortality/HRU endpoints, using early period as the reference and adjusting for significant patient (sex, age, race, ethnicity, history of hypertension, morbid obesity, diabetes, chronic pulmonary disease, chronic kidney disease [CKD], and Charlson comorbidity index score) and hospital characteristics (bed size, urbanicity of population served, teaching status, and geographic region). Robust standard errors were used to adjust for clustering of patients within hospitals. Multicollinearity was not present in the models based on the variance inflation factor. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
A total of 1 454 780 adult patients with ≥ 1 COVID-19–related discharges from 909 hospitals were identified in PHD-SR from April 2020 to February 2021. Approximately a third (n = 481 216) were inpatients in 871 hospitals and two-thirds (n = 983 564) were outpatients in 895 hospitals at their index visit.
Characteristics of Inpatients With COVID-19
Among COVID-19 adult inpatients, average age was 64.4 years and 51.7% were male; 63.7% were white, 17.7% were black, and 16.9% were Hispanic (Table 1 ). Common comorbidities were hypertension (70.3%), diabetes (42.4%), chronic pulmonary disease (23.6%), morbid obesity (21.3%), CKD (18.5%), and congestive heart failure (18.5%). Most patients (45.8%) were hospitalized in the South (reflective of hospitals included in PHD) and in urban hospitals (87.9%), but patients were evenly distributed across small, medium, and large hospitals, categorized by the number of beds.
Table 1.
Baseline demographics of inpatients and outpatients with COVID-19 at index hospitalization/visit, stratified by the time of discharge from April 1, 2020, to February 28, 2021.
| Characteristics | Inpatients |
Outpatients |
||||||
|---|---|---|---|---|---|---|---|---|
| Total |
Time of discharge |
Total |
Time of discharge |
|||||
| N = 481 216 | Early period: Apr-Jun (n = 95 636) | Middle period: Jul-Nov (n = 173 543) | Later period: Dec-Feb (n = 212 037) | N = 973 564 | Early period: Apr-Jun (n = 126 968) | Middle period: Jul-Nov (n = 408 188) | Later period: Dec-Feb (n = 438 408) | |
| Patient characteristics | ||||||||
| Age category, years, n (%) | ||||||||
| 18-34 | 35 125 (7.3) | 7530 (7.9) | 14 477 (8.3) | 13 118 (6.2) | 261 938 (26.9) | 39 858 (31.4) | 119 871 (29.4) | 102 209 (23.3) |
| 35-49 | 59 364 (12.3) | 13 721 (14.3) | 23 265 (13.4) | 22 378 (10.6) | 244 478 (25.1) | 36 264 (28.6) | 104 372 (25.6) | 103 842 (23.7) |
| 50-64 | 125 769 (26.1) | 26 886 (28.1) | 45 755 (26.4) | 53 128 (25.1) | 253 284 (26.0) | 31 231 (24.6) | 102 695 (25.2) | 119 358 (27.2) |
| 65-79 | 161 331 (33.5) | 28 751 (30.1) | 56 831 (32.7) | 75 749 (35.7) | 159 710 (16.4) | 13 849 (10.9) | 61 250 (15.0) | 84 611 (19.3) |
| 80+ | 99 627 (20.7) | 18 748 (19.6) | 33 215 (19.1) | 47 664 (22.5) | 54 154 (5.6) | 5766 (4.5) | 20 000 (4.9) | 28 388 (6.5) |
| Age, years, continuous | ||||||||
| Mean (SD) | 64.4 (17.5) | 63.1 (17.8) | 63.2 (17.8) | 65.9 (17.0) | 48.8 (18.5) | 45.9 (17.7) | 47.5 (18.4) | 50.9 (18.6) |
| Median (q1, q3) | 66.0 (53.0, 77.0) | 64.0 (51.0, 76.0) | 65.0 (52.0, 77.0) | 68.0 (56.0, 78.0) | 48.0 (33.0, 63.0) | 44.0 (31.0, 58.0) | 47.0 (32.0, 61.0) | 51.0 (36.0, 65.0) |
| Sex, n (%) | ||||||||
| Female | 231 713 (48.2) | 45 429 (47.5) | 84 513 (48.7) | 101 771 (48.0) | 542 105 (55.7) | 69 968 (55.1) | 228 051 (55.9) | 244 086 (55.7) |
| Male | 248 950 (51.7) | 50 001 (52.3) | 88 858 (51.2) | 110 091 (51.9) | 428 969 (44.1) | 56 208 (44.3) | 178 971 (43.8) | 193 790 (44.2) |
| Unknown | 553 (0.1) | 206 (0.2) | 172 (0.1) | 175 (0.1) | 2490 (0.3) | 792 (0.6) | 1166 (0.3) | 532 (0.1) |
| Race, n (%) | ||||||||
| White | 306 564 (63.7) | 43 197 (45.2) | 116 090 (66.9) | 147 277 (69.5) | 619 762 (63.7) | 59 758 (47.1) | 264 416 (64.8) | 295 588 (67.4) |
| Black | 85 126 (17.7) | 23 369 (24.4) | 29 449 (17.0) | 32 308 (15.2) | 160 997 (16.5) | 27 055 (21.3) | 67 704 (16.6) | 66 238 (15.1) |
| Other/unknown | 89 526 (18.6) | 29 070 (30.4) | 28 004 (16.1) | 32 452 (15.3) | 192 805 (19.8) | 40 155 (31.6) | 76 068 (18.6) | 76 582 (17.5) |
| Ethnicity, n (%) | ||||||||
| Hispanic or Latino | 81 418 (16.9) | 18 508 (19.4) | 32 516 (18.7) | 30 394 (14.3) | 192 758 (19.8) | 35 202 (27.7) | 84 763 (20.8) | 72 793 (16.6) |
| Not Hispanic or Latino | 320 574 (66.6) | 55 334 (57.9) | 117 597 (67.8) | 147 643 (69.6) | 621 977 (63.9) | 63 225 (49.8) | 264 018 (64.7) | 294 734 (67.2) |
| Unknown | 79 224 (16.5) | 21 794 (22.8) | 23 430 (13.5) | 34 000 (16.0) | 158 829 (16.3) | 28 541 (22.5) | 59 407 (14.6) | 70 881 (16.2) |
| Payer, n (%) | ||||||||
| Medicaid | 64 605 (13.4) | 17 404 (18.2) | 22 540 (13.0) | 24 661 (11.6) | 152 689 (15.7) | 21 642 (17.0) | 62 591 (15.3) | 68 456 (15.6) |
| Medicare | 267 223 (55.5) | 48 373 (50.6) | 93 070 (53.6) | 125 780 (59.3) | 229 140 (23.5) | 23 893 (18.8) | 87 878 (21.5) | 117 369 (26.8) |
| Private insurance | 112 334 (23.3) | 22 907 (24.0) | 41 923 (24.2) | 47 504 (22.4) | 449 611 (46.2) | 56 028 (44.1) | 196 149 (48.1) | 197 434 (45.0) |
| Other/uninsured | 37 054 (7.7) | 6952 (7.3) | 16 010 (9.2) | 14 092 (6.6) | 142 124 (14.6) | 25 405 (20.0) | 61 570 (15.1) | 55 149 (12.6) |
| Baseline comorbidities, n (%) | ||||||||
| Morbid obesity | 102 407 (21.3) | 17 252 (18.0) | 39 314 (22.7) | 45 841 (21.6) | 37 096 (3.8) | 3796 (3.0) | 15 446 (3.8) | 17 854 (4.1) |
| Hypertension | 338 121 (70.3) | 64 318 (67.3) | 120 309 (69.3) | 153 494 (72.4) | 222 075 (22.8) | 24 752 (19.5) | 88 068 (21.6) | 109 255 (24.9) |
| History of smoking | 40 573 (8.4) | 7027 (7.3) | 14 604 (8.4) | 18 942 (8.9) | 59 871 (6.1) | 7113 (5.6) | 24 394 (6.0) | 28 364 (6.5) |
| Myocardial infarction | 49 973 (10.4) | 8886 (9.3) | 16 889 (9.7) | 24 198 (11.4) | 15 029 (1.5) | 1464 (1.2) | 5899 (1.4) | 7666 (1.7) |
| Congestive heart failure | 88 961 (18.5) | 15 915 (16.6) | 30 967 (17.8) | 42 079 (19.8) | 23 479 (2.4) | 2551 (2.0) | 9263 (2.3) | 11 665 (2.7) |
| Peripheral vascular disease | 22 298 (4.6) | 4202 (4.4) | 7576 (4.4) | 10 520 (5.0) | 7541 (0.8) | 805 (0.6) | 3005 (0.7) | 3731 (0.9) |
| Cerebrovascular disease | 21 970 (4.6) | 3992 (4.2) | 7386 (4.3) | 10 592 (5.0) | 8062 (0.8) | 797 (0.6) | 3054 (0.7) | 4211 (1.0) |
| Dementia | 62 563 (13.0) | 15 626 (16.3) | 21 133 (12.2) | 25 804 (12.2) | 13 381 (1.4) | 2098 (1.7) | 5082 (1.2) | 6201 (1.4) |
| Chronic pulmonary disease | 113 571 (23.6) | 20 916 (21.9) | 40 421 (23.3) | 52 234 (24.6) | 83 837 (8.6) | 9979 (7.9) | 33 667 (8.2) | 40 191 (9.2) |
| Rheumatic disease | 11759 (2.4) | 1973 (2.1) | 4254 (2.5) | 5532 (2.6) | 5544 (0.6) | 503 (0.4) | 2132 (0.5) | 2909 (0.7) |
| Peptic ulcer disease | 5628 (1.2) | 1072 (1.1) | 1840 (1.1) | 2716 (1.3) | 1621 (0.2) | 198 (0.2) | 648 (0.2) | 775 (0.2) |
| Diabetes mellitus | 204 263 (42.4) | 39 768 (41.6) | 73 331 (42.3) | 91 164 (43.0) | 118 302 (12.2) | 14 157 (11.2) | 46 633 (11.4) | 57 512 (13.1) |
| Hemiplegia or paraplegia | 6684 (1.4) | 1469 (1.5) | 2152 (1.2) | 3063 (1.4) | 1253 (0.1) | 181 (0.1) | 479 (0.1) | 593 (0.1) |
| Chronic kidney disease | 89 265 (18.5) | 22 540 (23.6) | 32 492 (18.7) | 34 233 (16.1) | 26 121 (2.7) | 3376 (2.7) | 10 725 (2.6) | 12 020 (2.7) |
| Mild liver disease | 5394 (1.1) | 937 (1.0) | 1949 (1.1) | 2508 (1.2) | 2074 (0.2) | 246 (0.2) | 773 (0.2) | 1055 (0.2) |
| Moderate or severe liver disease | 5493 (1.1) | 1021 (1.1) | 1915 (1.1) | 2557 (1.2) | 1263 (0.1) | 160 (0.1) | 488 (0.1) | 615 (0.1) |
| Any malignancy | 24 161 (5.0) | 4252 (4.4) | 8215 (4.7) | 11 694 (5.5) | 13 052 (1.3) | 1391 (1.1) | 5034 (1.2) | 6627 (1.5) |
| Metastatic solid tumor | 6334 (1.3) | 1166 (1.2) | 2176 (1.3) | 2992 (1.4) | 2524 (0.3) | 295 (0.2) | 995 (0.2) | 1234 (0.3) |
| HIV disease | 1389 (0.3) | 431 (0.5) | 412 (0.2) | 546 (0.3) | 1224 (0.1) | 246 (0.2) | 438 (0.1) | 540 (0.1) |
| CCI score category, n (%) | ||||||||
| 0 | 133 349 (27.7) | 27 362 (28.6) | 50 351 (29.0) | 55 636 (26.2) | 748 145 (76.8) | 100 142 (78.9) | 318 787 (78.1) | 329 216 (75.1) |
| 1-4 | 282 003 (58.6) | 53 690 (56.1) | 99 977 (57.6) | 128 336 (60.5) | 210 228 (21.6) | 24 847 (19.6) | 83 335 (20.4) | 102 046 (23.3) |
| 5+ | 65 864 (13.7) | 14 584 (15.2) | 23 215 (13.4) | 28 065 (13.2) | 15 191 (1.6) | 1979 (1.6) | 6066 (1.5) | 7146 (1.6) |
| CCI score, mean (SD) | 2.0 (2.2) | 2.1 (2.3) | 2.0 (2.2) | 2.1 (2.2) | 0.4 (1.1) | 0.4 (1.1) | 0.4 (1.0) | 0.5 (1.1) |
| Hospital characteristics | ||||||||
| Hospital size, n (%) | ||||||||
| 1-299 beds | 183 753 (38.2) | 30 478 (31.9) | 68 313 (39.4) | 84 962 (40.1) | 445 866 (45.8) | 52 112 (41.0) | 187 718 (46.0) | 206 036 (47.0) |
| 300-499 beds | 147 038 (30.6) | 30 912 (32.3) | 52 269 (30.1) | 63 857 (30.1) | 247 158 (25.4) | 32 080 (25.3) | 105 044 (25.7) | 110 034 (25.1) |
| 500+ beds | 149 766 (31.1) | 34 209 (35.8) | 52 780 (30.4) | 62 777 (29.6) | 278 109 (28.6) | 42 534 (33.5) | 114 684 (28.1) | 120 891 (27.6) |
| Other/unknown | 659 (0.1) | 37 (0.0) | 181 (0.1) | 441 (0.2) | 2431 (0.2) | 242 (0.2) | 742 (0.2) | 1447 (0.3) |
| Teaching status, n (%) | ||||||||
| Nonteaching hospital | 252 269 (52.4) | 37 111 (38.8) | 99 534 (57.4) | 115 624 (54.5) | 584 296 (60.0) | 67 075 (52.8) | 248 660 (60.9) | 268 561 (61.3) |
| Teaching hospital | 228 947 (47.6) | 58 525 (61.2) | 74 009 (42.6) | 96 413 (45.5) | 389 268 (40.0) | 59 893 (47.2) | 159 528 (39.1) | 169 847 (38.7) |
| Population served, n (%) | ||||||||
| Rural | 58 236 (12.1) | 6862 (7.2) | 24 189 (13.9) | 27 185 (12.8) | 195 307 (20.1) | 14 313 (11.3) | 87 324 (21.4) | 93 670 (21.4) |
| Urban | 422 980 (87.9) | 88 774 (92.8) | 149 354 (86.1) | 184 852 (87.2) | 778 257 (79.9) | 112 655 (88.7) | 320 864 (78.6) | 344 738 (78.6) |
| Geographic location, n (%) | ||||||||
| Midwest | 99197 (20.6) | 18 368 (19.2) | 40 386 (23.3) | 40 443 (19.1) | 218 352 (22.4) | 23 939 (18.9) | 110 728 (27.1) | 83 685 (19.1) |
| Northeast | 93 432 (19.4) | 41 522 (43.4) | 13 113 (7.6) | 38 797 (18.3) | 124 918 (12.8) | 27 672 (21.8) | 33 053 (8.1) | 64 193 (14.6) |
| South | 220 256 (45.8) | 27 352 (28.6) | 94 435 (54.4) | 98 469 (46.4) | 516 594 (53.1) | 62 917 (49.6) | 216 685 (53.1) | 236 992 (54.1) |
| West | 68 331 (14.2) | 8394 (8.8) | 25 609 (14.8) | 34 328 (16.2) | 113 700 (11.7) | 12 440 (9.8) | 47 722 (11.7) | 53 538 (12.2) |
Apr indicates April; CCI, Charlson-Deyo comorbidity index; Dec, December; Feb, February; HIV, human immunodeficiency virus; Jun, June; Nov, November; q, quartile.
The early period consisted of 95 636 (19.9%), middle period had 173 543 (36.1%), and later period included 212 037 patients (44.1%). Compared with early, patients discharged in later period had a higher mean age (65.9 years vs 63.1 years) and patients in the middle and later periods were more likely to be white (66.9% and 69.5% vs 45.2%, respectively). Patients in middle and later periods were more likely to have hypertension, morbid obesity, congestive heart failure, chronic pulmonary disease, and diabetes, but were less likely to have dementia (12.2% and 12.2% vs 16.3%) and CKD (18.7% and 16.1% vs 23.6%) than patients in early period (all P < .001).
Characteristics of Hospital-Based Outpatients With COVID-19
Among 973 564 COVID-19 adult outpatients, mean age was 48.8 years and 44.1% were male; 63.7% were white, 16.5% were black, and 19.8% were Hispanic (Table 1). Most patients did not have a preexisting condition (76.8% of the patients had no CCI comorbidity); among those who did, hypertension (22.8%) and diabetes (12.2%) were most common. Most patients (53.1%) visited hospitals in the South (reflective of hospitals included in PHD), urban hospitals (79.9%), and small hospitals (1-299 beds, 45.8%).
Early, middle, and later periods consisted of 126 968 (13.0%), 408 188 (41.9%), and 438 408 outpatients (45.0%), respectively. Compared with early, patients in middle and later periods had higher mean ages (47.5 and 50.9 years vs 45.9 years) and were more likely to be white (64.8% and 67.4% vs 47.1%, respectively) and have hypertension (21.6% and 24.9% vs 19.5%, respectively). Middle and later cohorts were also more likely to visit smaller rural hospitals in the South (all P < .001).
HRU of Inpatients With COVID-19
Most inpatients originated from a nonhealthcare facility (79.9%) (Fig. 1 and Table 2 ). Approximately 10% were transferred from another acute care facility, another 3.6% from SNF/ICF/RF/LTCF, and 94.5% of the patients were admitted through the ED. Of these patients, 22.5% required an ICU stay, 12.8% were put on IMV, and 13.9% died during index hospitalization. Less than half of the patients (44.3%) were discharged home; 11.6% were discharged to home health, 15.1% were discharged to SNF/ICF/RF/LTCF, and 12.3% (n = 8911) were transferred from an acute care facility. Among patients discharged to SNF/ICF/RF/LTCF (n = 72 765), only 11.3% (n = 8211) initially came from SNF/ICF/RF/LTCF and the majority (70.5%) had originated from nonhealthcare facility. After discharge, 2.7% returned to ED and 5.3% were readmitted to the same hospital within 30 days. Among readmitted patients (n = 22 017), 24.4% (n = 5377) had ICU admission and 16.8% (n = 3708) died.
Figure 1.
Healthcare resource utilization flow of COVID-19 patients with index inpatient visit during April 1, 2020, and February 28, 2021.
ED indicates emergency department; ICF, intermediate care facility; ICU, intensive care unit; LTCF, long-term care facility; RF, rehabilitation facility; SNF, skilled nursing facility.
Table 2.
Healthcare resource utilization of inpatients with COVID-19 during index hospitalization and 30-day follow-up.
| Healthcare resource utilization | Total |
Time of discharge |
P value | ||
|---|---|---|---|---|---|
| N = 481 216 | Early period: Apr-Jun (n = 95 636) | Middle period: Jul-Nov (n = 173 543) | Later period: Dec-Feb (n = 212 037) | ||
| During index hospitalization | |||||
| Point of origin, n (%) | <.001 | ||||
| Nonhealthcare facility (eg, home) | 384 585 (79.9) | 75 077 (78.5) | 139 491 (80.4) | 170 017 (80.2) | |
| Clinic | 27 022 (5.6) | 5436 (5.7) | 9083 (5.2) | 12 503 (5.9) | |
| Transfer from an acute care facility | 48 595 (10.1) | 8759 (9.2) | 18 637 (10.7) | 21 199 (10.0) | |
| Transfer from SNF/ICF/RF/LTCF | 17 252 (3.6) | 5835 (6.1) | 4910 (2.8) | 6507 (3.1) | |
| Other | 3762 (0.8) | 529 (0.6) | 1422 (0.8) | 1811 (0.9) | |
| Admitted through the ED, n (%) | 454 871 (94.5) | 90 409 (94.5) | 163 561 (94.2) | 200 901 (94.7) | <.001 |
| Discharge status, n (%) | <.001 | ||||
| Expired | 66 706 (13.9) | 16 975 (17.7) | 20 625 (11.9) | 29 106 (13.7) | |
| Home | 213 227 (44.3) | 38 786 (40.6) | 83 134 (47.9) | 91 307 (43.1) | |
| Home health | 55 871 (11.6) | 8686 (9.1) | 18 789 (10.8) | 28 396 (13.4) | |
| Transfer to SNF/ICF/RF/LTCF | 72 765 (15.1) | 16 846 (17.6) | 23 148 (13.3) | 32 771 (15.5) | |
| Transfer to another acute care facility | 1674 (0.3) | 388 (0.4) | 696 (0.4) | 696 (0.4) | |
| Hospice | 15 106 (3.1) | 3040 (3.2) | 5147 (3.0) | 6919 (3.3) | |
| Other | 55 867 (11.6) | 10 915 (11.4) | 22 004 (12.7) | 22 948 (10.8) | |
| In-hospital mortality during index hospitalization, n (%) | 66 706 (13.9) | 16 975 (17.7) | 20 625 (11.9) | 29 106 (13.7) | <.001 |
| ICU admission, n (%) | 108 120 (22.5) | 23 986 (25.1) | 40 469 (23.3) | 43 665 (20.6) | <.001 |
| Invasive mechanical ventilator use, n (%) | 61 432 (12.8) | 17 149 (17.9) | 19 551 (11.3) | 24 732 (11.7) | <.001 |
| Extracorporeal membrane oxygenation use, n (%) | 983 (0.2) | 242 (0.3) | 395 (0.2) | 346 (0.2) | <.001 |
| Total length of hospital stay, days | <.001 | ||||
| Mean (SD) | 8.5 (10.5) | 9.3 (11.1) | 8.1 (11.2) | 8.4 (9.6) | |
| Median (q1, q3) | 5.0 (3.0, 10.0) | 6.0 (3.0, 12.0) | 5.0 (3.0, 10.0) | 5.0 (3.0, 10.0) | |
| Length of ICU stay, days | <.001 | ||||
| Mean (SD) | 8.9 (10.0) | 9.4 (9.7) | 8.7 (10.5) | 8.7 (9.7) | |
| Median (q1, q3) | 5.0 (2.0, 12.0) | 6.0 (3.0, 13.0) | 5.0 (2.0, 11.0) | 5.0 (2.0, 12.0) | |
| During 30 days after index hospitalization∗ | |||||
| COVID-19–related ED outpatient visit within 30 days, n (%) | 11 152 (2.7) | 2100 (2.7) | 4451 (2.9) | 4601 (2.5) | <.001 |
| COVID-19–related non-ED outpatient visit within 30 days, n (%) | 6707 (1.6) | 1193 (1.5) | 2833 (1.9) | 2681 (1.5) | <.001 |
| COVID-19–related readmission within 30 days, n (%) | 22 017 (5.3) | 3782 (4.8) | 9021 (5.9) | 9214 (5.0) | <.001 |
| COVID-19–related readmission with ICU within 30 days, n (%) | 5377 (1.3) | 878 (1.1) | 2424 (1.6) | 2075 (1.1) | <.001 |
| Mortality during COVID-19–related readmission within 30 days (excluding death during index visit), n (%) | 3708 (0.9) | 558 (0.7) | 1479 (1.0) | 1671 (0.9) | <.001 |
| Mortality during any COVID-19–related hospital visit within 30 days (excluding death during index visit), n (%) | 4042 (1.0) | 625 (0.8) | 1593 (1.0) | 1824 (1.0) | <.001 |
Apr indicates April; Dec, December; ED, emergency department; Feb, February; ICF, intermediate care facility; ICU, intensive care unit; Jun, June; LTCF, long-term care facility; Nov, November; q, quartile; RF, rehabilitation facility; SNF, skilled nursing facility.
Proportions are calculated only among patients who were discharged alive at index hospitalization.
Patients in middle and later periods were slightly more likely to come from a nonhealthcare facility or an acute care facility and less likely to come from SNF/ICF/RF/LTCF (2.8% and 3.1% vs 6.1%, respectively) (Table 2 ) than patients in early period. Compared with early, middle and later cohort patients were significantly less likely to die (11.9% and 13.7% vs 17.7%, respectively), less likely to be admitted to the ICU (23.3% and 20.6% vs 25.1%, respectively), and less likely to be put on IMV (11.3% and 11.7% vs 17.9%, respectively) than early cohort patients during index hospitalization (all P < .001). These observations were consistent after adjusting for patient and hospital characteristics—patients in the middle and later periods were 36% and 30% less likely to die and 23% and 32% less likely to be admitted to the ICU, respectively, than early cohort (adjusted odds ratio [aOR] 0.64 and 0.70 for mortality and 0.77 and 0.68 for ICU admission) (Table 4). After being discharged from index hospitalization, middle period patients were more likely to be readmitted within 30 days (aOR 1.24; 95% confidence interval [CI] 1.18-1.31) than early period patients.
Table 4.
Associations between time of discharge and mortality/healthcare resource utilization during index visit and 30-day follow-up for inpatients and outpatients with COVID-19.
| Endpoints | Middle period (vs early period) |
Later period (vs early period) |
||
|---|---|---|---|---|
| Adjusted OR∗ | 95% CI | Adjusted OR∗ | 95% CI | |
| Inpatients | ||||
| During index hospitalization (n = 481 216) | ||||
| In-hospital mortality | 0.64 | 0.60-0.69 | 0.70 | 0.66-0.75 |
| Intensive care unit admission | 0.77 | 0.73-0.82 | 0.68 | 0.64-0.72 |
| Invasive mechanical ventilator use | 0.56 | 0.53-0.60 | 0.59 | 0.56-0.62 |
| During 30 days after index hospitalization† (n = 414 510) | ||||
| COVID-19–related ED outpatient visit | 1.06 | 0.99-1.12 | 0.92 | 0.85-0.98 |
| COVID-19–related readmission | 1.24 | 1.18-1.31 | 1.00 | 0.95-1.06 |
| In-hospital mortality during follow-up | 1.24 | 1.11-1.39 | 1.12 | 1.00-1.25 |
| Outpatients | ||||
| During index outpatient visit (n = 973 564) | ||||
| In-hospital mortality | 0.63 | 0.55-0.73 | 0.60 | 0.52-0.69 |
| During 30 days after index outpatient visit† (n = 971 122) | ||||
| COVID-19–related ED outpatient visit | 0.95 | 0.89-1.01 | 0.87 | 0.81-0.93 |
| COVID-19–related hospitalization | 0.96 | 0.91-1.03 | 0.75 | 0.70-0.80 |
| In-hospital mortality during follow-up | 1.07 | 0.94-1.21 | 0.77 | 0.68-0.88 |
CI indicates confidence interval; ED, emergency department; OR, odds ratio.
Adjusted for patient characteristics (sex, age, race, ethnicity, history of hypertension, morbid obesity, diabetes, chronic pulmonary disease, chronic kidney disease, and Charlson comorbidity index score category) and hospital characteristics (bed size, urbanicity of population served, teaching status, and geographic region).
Only among patients who were discharged alive at index hospitalization/outpatient visit.
HRU of Hospital-Based Outpatients With COVID-19
Most outpatients originated from a nonhealthcare facility (74.7%) or clinic (18.4%), and 60.2% of the patients were ED outpatients (Fig. 2 and Table 3). Non-ED outpatient visits included diagnostic testing (17.4%), clinic (8.5%), observation (3.8%), and same-day surgery (1.7%). Most patients were discharged home (78.5%) after the index outpatient visit. After discharge, 6.5% returned to ED and 4.1% had a return hospitalization within 30 days for COVID-19. Among patients who were hospitalized for COVID-19 (n = 39 626) within 30 days, 17.5% (n = 6953) required ICU admission and 8.6% (n = 3420) died during hospitalization.
Figure 2.
Healthcare resource utilization flow of COVID-19 patients with index hospital-based outpatient visit during April 1, 2020, and February 28, 2021.
ED indicates emergency department; ICF, intermediate care facility; ICU, intensive care unit; LTCF, long-term care facility; RF, rehabilitation facility; SNF, skilled nursing facility.
Table 3.
Healthcare resource utilization of hospital-based outpatients with COVID-19 during index visit and 30-day follow-up.
| Healthcare resource utilization | Total |
Time of discharge |
P value | ||
|---|---|---|---|---|---|
| N = 973 564 | Early period: Apr-Jun (n = 126 968) | Middle period: Jul-Nov (n = 408 188) | Later period: Dec-Feb (n = 438 408) | ||
| During index outpatient visit | |||||
| Point of origin, n (%) | <.001 | ||||
| Nonhealthcare facility (eg, home) | 727 309 (74.7) | 95 864 (75.5) | 307 181 (75.3) | 324 264 (74.0) | |
| Clinic | 178 969 (18.4) | 20 352 (16.0) | 76 361 (18.7) | 82 256 (18.8) | |
| Transfer from an acute care facility | 7085 (0.7) | 796 (0.6) | 3109 (0.8) | 3180 (0.7) | |
| Transfer from SNF/ICF/RF/LTCF | 4672 (0.5) | 1113 (0.9) | 1595 (0.4) | 1964 (0.4) | |
| Other | 55 529 (5.7) | 8843 (7.0) | 19 942 (4.9) | 26 744 (6.1) | |
| ED outpatient visit, n (%) | 586 537 (60.2) | 80 000 (63.0) | 243 188 (59.6) | 263 349 (60.1) | <.001 |
| Discharge status, n (%) | <.001 | ||||
| Expired | 2442 (0.3) | 467 (0.4) | 874 (0.2) | 1101 (0.3) | |
| Home | 764 445 (78.5) | 97 410 (76.7) | 319 708 (78.3) | 347 327 (79.2) | |
| Home health | 3851 (0.4) | 765 (0.6) | 1972 (0.5) | 1114 (0.3) | |
| Transfer to SNF/ICF/RF/LTCF | 7514 (0.8) | 1165 (0.9) | 2811 (0.7) | 3538 (0.8) | |
| Transfer to another acute care facility | 1998 (0.2) | 193 (0.2) | 840 (0.2) | 965 (0.2) | |
| Hospice | 510 (0.1) | 74 (0.1) | 215 (0.1) | 221 (0.1) | |
| Other | 192 804 (19.8) | 26 894 (21.2) | 81 768 (20.0) | 84 142 (19.2) | |
| In-hospital mortality during index outpatient visit, n (%) | 2442 (0.3) | 467 (0.4) | 874 (0.2) | 1101 (0.3) | <.001 |
| During 30 days after index outpatient visit∗ | |||||
| COVID-19–related ED outpatient visit within 30 days, n (%) | 63 262 (6.5) | 8860 (7.0) | 27 130 (6.7) | 27 272 (6.2) | <.001 |
| COVID-19–related non-ED outpatient visit within 30 days, n (%) | 36 950 (3.8) | 5417 (4.3) | 14 615 (3.5) | 16 918 (3.9) | <.001 |
| COVID-19–related hospitalization within 30 days, n (%) | 39 626 (4.1) | 5480 (4.3) | 17 595 (4.3) | 16 551 (3.8) | <.001 |
| COVID-19–related ICU admission within 30 days, n (%) | 6953 (0.7) | 1149 (0.9) | 3348 (0.8) | 2456 (0.6) | <.001 |
| Mortality during COVID-19–related hospitalization within 30 days (excluding death during index visit), n (%) | 3420 (0.4) | 402 (0.3) | 1539 (0.4) | 1479 (0.3) | <.001 |
| Mortality during any COVID-19–related hospital visit within 30 days (excluding death during index visit), n (%) | 3651 (0.4) | 431 (0.3) | 1647 (0.4) | 1573 (0.4) | <.001 |
Apr indicates April; Dec, December; ED, emergency department; Feb, February; ICF, intermediate care facility; ICU, intensive care unit; Jun, June; LTCF, long-term care facility; Nov, November; q, quartile; RF, rehabilitation facility; SNF, skilled nursing facility.
Proportions are calculated only among patients who were discharged alive at index outpatient visit.
Compared with early period, patients in the middle and later periods were slightly more likely to come from a clinic (18.7% and 18.9% vs 16.0%, respectively) and be discharged home (78.3% and 79.2% vs 76.7%, respectively) (all P < .001). After discharge, patients in middle period were slightly less likely to visit the ED than early period patients (6.7% vs 7.0%), but the difference attenuated after adjusting for patient and hospital characteristics (aOR 0.95; 95% CI 0.89-1.01) (Table 4 ). Later period patients were 13% less likely to return to ED (aOR 0.87; 95% CI 0.81-0.93) and 25% less likely to be hospitalized (aOR 0.75; 95% CI 0.70-0.80) within 30 days than early period patients.
Discussion
This large real-world study of HRU among patients with COVID-19 in more than 900 US hospitals showed high-level utilizations of ED and ICU services among inpatients and high level of initial and return ED visits among outpatients. Across 3 different time periods between April 2020 and February 2021, ED utilization of inpatients and outpatients changed only slightly; ICU and IMV use among inpatients decreased but remained at a high level. The utilization of healthcare services after discharge was high among inpatients.
We would like to note that 95% of inpatients were admitted through the ED, and this level remained steady from April of 2020 to February of 2021. Although studies have reported decreased ED visits related to COVID-19 from April 2020 to June of 2020 because of the decrease of overall COVID-19 incidence, the demand of ED services remained high among patients with COVID-19.26 , 27 High ED utilization during a pandemic is expected and has been observed before (eg, H1N1 influenza); nevertheless, it tended to be seasonal and not continuously at a high level for more than 10 months.28 , 29 Our study showed that the absolute number of inpatients with COVID-19 almost doubled during the later period possibly overwhelming the ED. Furthermore, although the percentage of ED utilization was lower (∼60%) among hospital-based outpatients than that of inpatients, the absolute number of outpatients using ED exceeded that of inpatients (n = 454 871 vs n = 586 537). Approximately 6% to 7% of outpatients also had follow-up ED visits within 30 days. Our findings highlight the significant burden of COVID-19 on ED services and imply that other patients who need ED services (eg, patients with trauma, acute cardiovascular diseases, injury) might have been severely affected during the pandemic.
This study also showed high utilization of ICU and IMV among inpatients. Overall, 23% of inpatients and 18% of outpatients with return hospitalization (within 30 days) were admitted to the ICU. Therefore, hospitals struggled to secure sufficient ICU and IMV resources for treating inpatients when COVID-19 case counts skyrocketed during the pandemic.30, 31, 32 Possibly because of time and experience in treating COVID-19,1 the proportion of inpatients needing ICU care decreased from 25% to 21%. The use of IMV also decreased from 18% during early to 12% in later period of the pandemic. Nevertheless, the utilization of ICU and IMV remained high among inpatients with COVID-19—especially when the absolute number of COVID-19 hospitalizations increased in later period.
Among inpatients with COVID-19, only 44% were discharged home from index hospitalization when 80% originated from home. A substantial proportion of patients needed continued care (42%) and this level remained high throughout the study period. Although only 4% of inpatients originated from SNF/ICF/RF/LTCF, 15% were discharged to one—indicating a new burden in ICFs and LTCFs. Our finding is congruent with previous reports on patients suffering from lingering symptoms of COVID-19 months after discharge.17 , 33 As Felten-Barentsz et al34 suggested, continuous care during hospitalization and after discharge may be important for inpatients with COVID-19. The high-level postdischarge care used by inpatients with COVID-19 implies that healthcare decision makers may need to allocate more resources to provide continuous care for such patients.
Our study also showed that in-hospital mortality during index hospitalization decreased from 18% in early to 12% in middle period and then bounced back to 14% in later period. Kadri et al7 reported that high hospital COVID-19 caseload was detrimental to survival between March 2020 and August of 2020. Higher mortality in later period could also have been associated with increased caseload in hospitals between December 2020 and February 2021.11 Further study is needed to clarify the association between caseload in ED and ICU and in-hospital mortality.
Limitations
Our study has several limitations. First, this was a secondary data analysis using a hospital administrative database. We relied on hospital-reported diagnosis and procedure codes and chargemaster descriptions in identifying the HRU of patients, and misclassification may exist. Second, we were only able to capture revisits to the same hospital during the study period. This could have underestimated true 30-day outpatient visits, return hospitalizations, and readmissions—patients may have visited a different hospital or moved to a rehabilitation center after being discharged home. Furthermore, a patient with a second COVID-19 visit at a different hospital would have been treated as a different patient with a new index visit. Third, some hospitals did not report ethnicity and this could have resulted in underestimating the actual percentage of Hispanic patients in the study cohort.
Conclusions
Our study used a large, multicenter, and geographically diverse national sample to provide a robust overview of HRU during the index hospital visit and 30-day follow-up among patients with COVID-19 for 3 distinctive phases of the pandemic. Our findings showed that ED utilization was high for both inpatients and hospital-based outpatients in the US and it remained steady throughout April 2020 to February 2021. Although ICU use among inpatients decreased, the level remained above 20%. Among inpatients, greater than a third required additional healthcare services after discharge, highlighting the burden of COVID-19 on various sectors of healthcare services. Results from this study are valuable for healthcare service decision makers as they prepare and allocate resources for managing future waves of patients with COVID-19 and mitigate its negative impact on patients without COVID-19.
Article and Author Information
Author Contributions: Concept and design: Moon, Rosenthal
Acquisition of data: Brown
Analysis and interpretation of data: Moon, Brown, Rosenthal
Drafting of the manuscript: Moon
Critical revision of the paper for important intellectual content: Moon, Rosenthal
Statistical analysis: Moon
Provision of study materials or patients: Brown, Rosenthal
Obtainingfunding: Rosenthal
Administrative, technical, or logicalsupport: Rosenthal
Supervision: Rosenthal
Conflict of Interest Disclosures: All authors are employed by and reported stock ownership in Premier Inc during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was funded by Premier Inc.
Role of Funder/Sponsor: The funder has no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Acknowledgment
The abstract of this article was presented as Top 5% Research Presentation Award Finalist at Virtual ISPOR 2021 (May 17-20, 2021). The authors thank Ms Denise Juliano and Ms Myla Maloney for their support of the study and the PHD-SR data team for making the data available for analysis.
References
- 1.Asch D.A., Sheils N.E., Islam M.N., et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181(4):471–478. doi: 10.1001/jamainternmed.2020.8193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doidge J.C., Gould D.W., Ferrando-Vivas P., et al. Trends in intensive care for patients with COVID-19 in England, Wales and Northern Ireland. Am J Respir Crit Care Med. 2021;203(5):565–574. doi: 10.1164/rccm.202008-3212OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madahar P., Wunsch H., Jha P., Slutsky A.S., Brodie D. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9(4):322–324. doi: 10.1016/S2213-2600(21)00080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartsch S.M., Ferguson M.C., McKinnell J.A., et al. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff (Millwood) 2020;39(6):927–935. doi: 10.1377/hlthaff.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilaru A.S., Lee K., Snider C.K., et al. Return hospital admissions among 1419 COVID-19 patients discharged from five U.S. emergency departments. Acad Emerg Med. 2020;27(10):1039–1042. doi: 10.1111/acem.14117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8(4) doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kadri S.S., Sun J., Lawandi A., et al. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med. 2021;174(9):1240–1251. doi: 10.7326/M21-1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horwitz L.I., Jones S.A., Cerfolio R.J., et al. Trends in COVID-19 risk-adjusted mortality rates. J Hosp Med. 2021;16(2):90–92. doi: 10.12788/jhm.3552. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen N.T., Chinn J., Nahmias J., et al. Outcomes and mortality among adults hospitalized with COVID-19 at US medical centers. JAMA Netw Open. 2021;4(3) doi: 10.1001/jamanetworkopen.2021.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVID-19 dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. Johns Hopkins University. https://coronavirus.jhu.edu/map.html
- 11.CDC COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#hospitalizations-severity
- 12.FDA’s approval of Veklury (remdesivir) for the treatment of COVID-19 - the science of safety and effectiveness. Food and Drug Administration. https://www.fda.gov/drugs/drug-safety-and-availability/fdas-approval-veklury-remdesivir-treatment-covid-19-science-safety-and-effectiveness
- 13.FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems. U.S. Food and Drug Administration. https://www.fda.gov/drugs/drug-safety-and-availability/fda-cautions-against-use-hydroxychloroquine-or-chloroquine-covid-19-outside-hospital-setting-or
- 14.RECOVERY Collaborative Group. Horby P., Lim W.S., et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corticosteroids for COVID-19. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Corticosteroids-2020.1
- 16.Premier Healthcare Database (COVID-19): data that informs and performs. Premier. https://offers.premierinc.com/WCFY20PASCOVIDWhitepaper_LandingPage.html
- 17.Chevinsky J.R., Tao G., Lavery A.M., et al. Late conditions diagnosed 1-4 months following an initial coronavirus disease 2019 (COVID-19) encounter: a matched-cohort study using inpatient and outpatient administrative data - United States, 1 March-30 June 2020. Clin Infect Dis. 2021;73(suppl 1):S5–S16. doi: 10.1093/cid/ciab338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kompaniyets L., Goodman A.B., Belay B., et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lavery A.M., Preston L.E., Ko J.Y., et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695–1699. doi: 10.15585/mmwr.mm6945e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Premier Healthcare Database being used by National Institutes of Health to evaluate impact of COVID-19 on patients across the U.S. Premier. https://www.premierinc.com/newsroom/press-releases/premier-healthcare-database-being-used-by-national-institutes-of-health-to-evaluate-impact-of-covid-19-on-patients-across-the-u-s
- 21.Premier Healthcare Database White Paper data that informs and performs. Premier. https://products.premierinc.com/downloads/PremierHealthcareDatabaseWhitepaper.pdf
- 22.ICD-10-CM official coding and reporting guidelines April 1, 2020 through September 30, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/icd/COVID-19-guidelines-final.pdf
- 23.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 24.Deyo R.A., Cherkin D.C., Ciol M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 25.Rosenthal N, Cao Z, Chung J, et al. Updated coding algorithm for assessing Charlson comorbidity index using large hospital administrative data. Paper presented at: ISPOR 22nd Annual International Meeting; May 20-24, 2017; Boston, MA.
- 26.Gormeli Kurt N., Gunes C. How has Covid-19 pandemic affected crowded emergency services? Int J Clin Pract. 2020;74(12) doi: 10.1111/ijcp.13624. [DOI] [PubMed] [Google Scholar]
- 27.Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Self W.H., Grijalva C.G., Zhu Y., et al. Emergency department visits for influenza A(H1N1)pdm09, Davidson County, Tennessee, USA. Emerg Infect Dis. 2012;18(5):863–865. doi: 10.3201/eid1805.111233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gruneir A., Kwong J.C., Campitelli M.A., et al. Influenza and seasonal patterns of hospital use by older adults in long-term care and community settings in Ontario, Canada. Am J Public Health. 2014;104(2):e141–e147. doi: 10.2105/AJPH.2013.301519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 31.Goh K.J., Wong J., Tien J.C., et al. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. 2020;24(1):215. doi: 10.1186/s13054-020-02916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Docherty A.B., Harrison E.M., Green C.A., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Writing Committee for the COMEBAC Study Group. Morin L., Savale L., et al. Four-month clinical status of a cohort of patients after hospitalization for COVID-19 [published correction appears in JAMA. 2021;326(18):1874] JAMA. 2021;325(15):1525–1534. doi: 10.1001/jama.2021.3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Felten-Barentsz K.M., van Oorsouw R., Klooster E., et al. Recommendations for hospital-based physical therapists managing patients with COVID-19. Phys Ther. 2020;100(9):1444–1457. doi: 10.1093/ptj/pzaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]