Abstract
Background
Several studies have reported the use of anterior, posterior and lateral quadratus lumborum block (QLB) for pain control in hip surgeries. However, high-quality evidence is lacking. The current review aimed to summarize data on the efficacy of QLB for pain control in patients undergoing hip surgeries.
Methods
PubMed, Embase, and Google Scholar databases were searched up to August 5, 2021 for randomized controlled trials (RCTs) or non-RCTs assessing the efficacy of QLB for any type of hip surgery.
Results
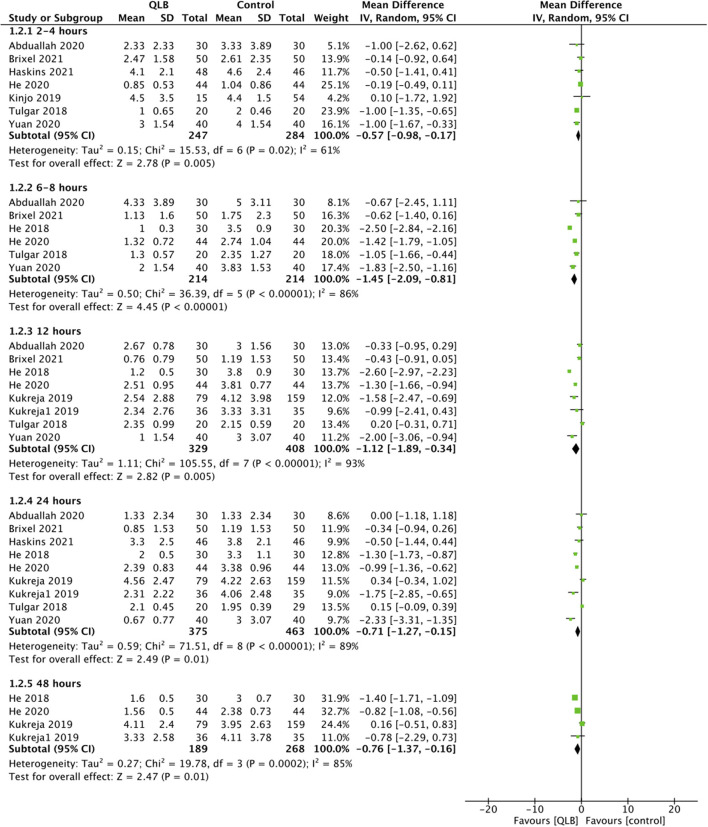
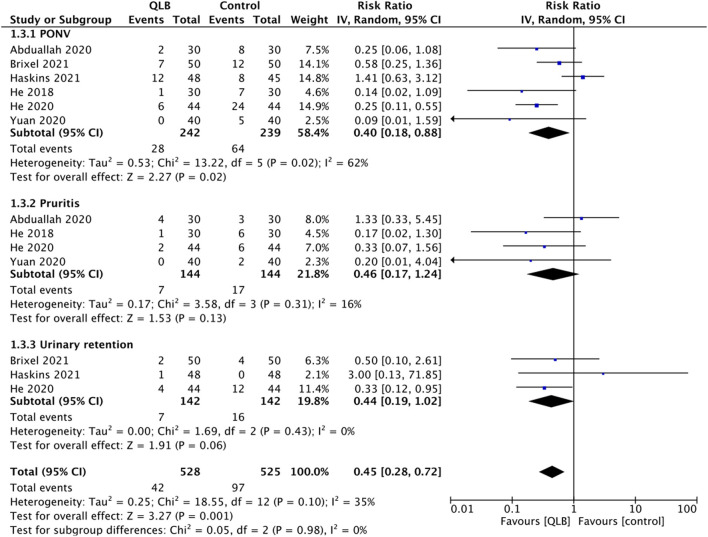
Thirteen studies were included (nine RCTs and four non-RCTs). On pooled analysis, there was a statistically significant reduction of 24-h total opioid consumption in patients receiving QLB as compared to the control group (MD: −9.92, 95% CI: −16.35, −3.48 I2 = 99% p = 0.003). We noted a statistically significant reduction of pain scores in the QLB group as compared to control group at 2–4 h (MD: −0.57, 95% CI: −0.98, −0.17 I2 = 61% p = 0.005), 6–8 h (MD: −1.45, 95% CI: −2.09, −0.81 I2 = 86% p < 0.00001), 12 h (MD: −1.12, 95% CI: −1.89, −0.34 I2 = 93% p = 0.005), 24 h (MD: −0.71, 95% CI: −1.27, −0.15 I2 = 89% p = 0.01) and 48 h (MD: −0.76, 95% CI: −1.37, −0.16 I2 = 85% p = 0.01) after the procedure. There was a statistically significant reduction in the risk of nausea/vomiting (RR: 0.40, 95% CI: 0.18, 0.88 I2 = 62% p = 0.02) in patients receiving QLB but no difference in the risk of pruritis (RR: 0.46, 95% CI: 0.17, 1.24 I2 = 16% p = 0.13) and urinary retention (RR: 0.44, 95% CI: 0.19, 1.02 I2 = 0% p = 0.06).
Conclusion
QLB as a part of a multimodal analgesic regimen reduces opioid consumption and pain scores in patients undergoing hip surgeries. The certainty of evidence based on GRADE was moderate. Despite the statistically significant results, the clinical relevance of the analgesic efficacy of QLB is debatable due to the small effect size.
Systematic Review Registration
https://www.crd.york.ac.uk/prospero/, identifier: CRD42021267861.
Keywords: hip surgery, arthroplasty, arthroscopy, pain, nerve block
Introduction
Surgical intervention of the hip joint is frequently used in adolescents with congenital hip dysplasia, adults and elderly patients requiring arthroscopy or joint replacement surgeries (1). Early physiotherapy and rehabilitation after hip surgery are highly beneficial, and early mobilization is known to improve outcomes (2, 3). However, post-operative pain is an important limiting factor that can slow down the rehabilitation process. Despite extensive research, the most optimal analgesic regime for hip surgeries is still debatable (4, 5). Opioids are the most common drugs used for pain control in the post-operative period, albeit with several side effects like nausea, vomiting, dizziness, and urinary retention (6). As the elderly constitute a significant proportion of patients undergoing hip surgeries, respiratory depression and sedation with opioids can lead to significantly prolonged recovery (7).
In this context, several regional analgesic techniques have been described to manage pain after hip surgeries. Local anesthetic infiltration of the hip joint, either as single-shot injections or continuous infiltration via catheters, has been reported to be ineffective for pain control after arthroplasty surgeries (8, 9). On the other hand, nerve blocks like the femoral nerve block, fascia iliaca block, lumbar plexus block are known to improve pain scores and reduce analgesic consumption after hip surgeries. However, they can also result in muscle weakness which can increase the incidence of falls (4). Furthermore, lumbar plexus block can result in serious adverse events like risk of high neuraxial anesthesia, hypotension, and local anesthetic toxicity (4). Alternatively, epidural anesthesia can provide good pain relief in hip surgery patients but is associated with technical difficulties, side effects like hypotension and headaches, and motor weakness. A modification of the classical technique, the walking epidural anesthesia has shown to improve motor control but could be associated with reduced pain control (4, 5).
In an attempt to find a better regional analgesic technique, several studies evaluated the use of quadratus lumborum block (QLB) for pain control in hip surgeries (10, 11). The QLB was first described by Blanco in 2007 and is an interfascial plane block of the posterior abdominal wall (12). The key anatomical landmark involved with the block is the quadratus lumborum muscle and the thoracolumbar fascia (TLF). The TLF is composed of aponeuroses and fascia layers which encloses the back muscles and connects the anterolateral abdominal wall with the lumbar paravertebral region. While the exact mechanism of QLB is unclear, it is postulated that the spread of local anesthetic along the TLF in to the paravertebral space leads to the analgesic action. With time, the approach has evolved into three distinct types with local anesthetic being deposited posterior, anterior, or lateral to the quadratus lumborum muscle (13). In the anterior QLB, local anesthetic is deposited in front of the quadratus lumborum muscle at the level of its attachment to the transverse process of L4 vertebra and the drug spreads between the quadratus lumborum and the psoas major muscle. In the posterior type, the anesthetic is deposited posteriorly between the quadratus lumborum and the medial lamina of TLF while in the lateral block, the medication is injected lateral to the quadratus lumborum muscle in the region of its contact with the transversalis fascia. All three types of QLBs have been used for a variety of indications and to date, the exact mechanism of action of the three types of blocks and their specific indications are still unclear (13–15).
Research indicates that QLB can successfully manage post-operative pain in patients undergoing abdominal surgeries, renal surgeries, and cesarean sections (14), but its efficacy for pain control after hip surgeries is still unclear. Since previous review articles on QLB could include only a limited number of studies on hip surgery (14, 15), there is a need for a comprehensive systematic review assessing the efficacy of QLB in patients undergoing hip surgeries. The main aim of the current study was to systematically search literature and pool evidence on the effectiveness of QLB in reducing analgesic consumption and improving pain scores in patients undergoing hip surgeries.
Materials and Methods
The current study was conducted as per the guidelines of the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses) (16) and the Cochrane Handbook for Systematic Reviews of Intervention (17) (Supplementary Table 1). We registered the study on PROSPERO (CRD42021267861).
Literature Search
We designed a systematic search strategy with the aid of the medical librarian to explore the electronic databases, such as PubMed, Embase, and Google Scholar for relevant articles. The search limits were set from inception to August 5, 2021, with no language restrictions. The keywords used for the literature search included: “Quadratus lumborum block,” “Regional anesthesia,” “Hip surgery,” “Hip fracture,” “Hip arthroplasty,” and “Hip arthroscopy.” Details of the literature search common to all databases are presented in Supplementary Table 2. Two reviewers carried out the electronic search independent of each other. The primary search results were assessed initially by their titles and abstracts to identify citations requiring full-text analysis. The full texts of the articles were reviewed by the two reviewers independently based on the inclusion and exclusion criteria. Any disagreements were resolved by discussion. We also carried out manual scoping of the bibliography in included studies for any additional articles.
Inclusion Criteria
Eligibility criteria for this review were structured using the PICOS (Population, Intervention, Comparison, Outcome, and Study design) framework. Details are as follows:
Population: Patients undergoing any type of hip surgery
Intervention: QLB administered by any approach (anterior/posterior)
Comparison: No block or sham block with normal saline
Outcomes: Post-operative analgesic consumption, and/or pain scores, and/or adverse events.
Study design: Randomized controlled trials (RCTs), Controlled clinical trials (CCTs), and retrospective studies
Exclusion criteria were: (1) Studies comparing QLB with another nerve block. (2) Studies not specifically on hip surgeries. (3) Studies not reporting relevant outcomes. (4) Abstracts, editorials, review articles, and case reports.
Data Extraction and Risk of Bias Assessment
A data extraction sheet was used by two reviewers to extract relevant data from the studies. Details of the first author, publication year, study location, study type, surgery type, sample size, age and gender details, duration of surgery, the protocol of QLB, post-operative analgesic drugs, and study outcomes were extracted. The outcomes of interest for our review were 24-h analgesic consumption in morphine equivalents, pain scores at rest on the Visual Analog Scale (VAS), and adverse events. A descriptive analysis was carried out for studies not reporting data amenable for the meta-analysis.
Two reviewers independently assessed the quality of included RCTs using the Cochrane Collaboration's risk of bias assessment tool-2 (17). Every study was assessed for randomization process, deviation from intended intervention, missing outcome data, measurement of outcomes, and selection of reported results. Based on the risk of bias in individual domains, the overall bias was marked as “high risk,” “some concerns,” or “low risk.” For non-RCTs, the risk of a bias assessment tool for non-randomized studies (RoBANS) was used (18). Studies were assessed for: selection of participants, confounding variables, intervention measurements, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting. Any disagreements related to data extraction or quality assessment were resolved by discussion. The certainty of the evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool using the GRADEpro GDT software [GRADEpro Guideline Development Tool. McMaster University, 2020 (developed by Evidence Prime, Inc.)].
Statistical Analysis
The “Review Manager” software [RevMan, version 5.3; Nordic Cochrane Center (Cochrane Collaboration), Copenhagen, Denmark; 2014] was used for the meta-analysis. Total analgesic consumption in morphine equivalents and pain scores at different time intervals were expressed as the mean difference (MD) with 95% confidence intervals (CI). In case studies that used any other opioid in the post-operative period, data was converted into morphine equivalents for this analysis (19). For graphical data, Engauge Digitizer Version 12.1 was used to extract numerical data. Median, range and interquartile range data was converted into the mean and standard deviation (SD) when required using the method of Wan et al. (20). Data on adverse events were pooled using risk ratios (RR). The random-effects model was used for all the meta-analyses. A sub-group analysis was conducted based on the study type. We also conducted a sensitivity analysis to assess if any study had an undue influence on the overall results of total analgesic consumption and pain outcomes. Each study was sequentially excluded in the meta-analysis software to recalculate the total effect size. To explore the cause of heterogeneity, we conducted a meta-regression analysis for the outcomes of 24 h total analgesic consumption, 12 and 24 h pain scores. Covariates included were age, male gender, sample size, type of QLB block and type of local anesthetic. Meta-regression was not conducted for other outcomes due to limited number of studies. The analysis was conducted using Open MetaAnalyst software. An important limitation of the software is the unavailability of R2-values which, therefore, could not be reported in our analysis.
Heterogeneity was assessed using the I2 statistic. I2-values of 25–50% represented low, values of 50–75% medium, and more than 75% represented substantial heterogeneity. Funnel plot was used to assess publication bias. P < 0.05 was considered statistically significant.
Results
Details of Included Studies
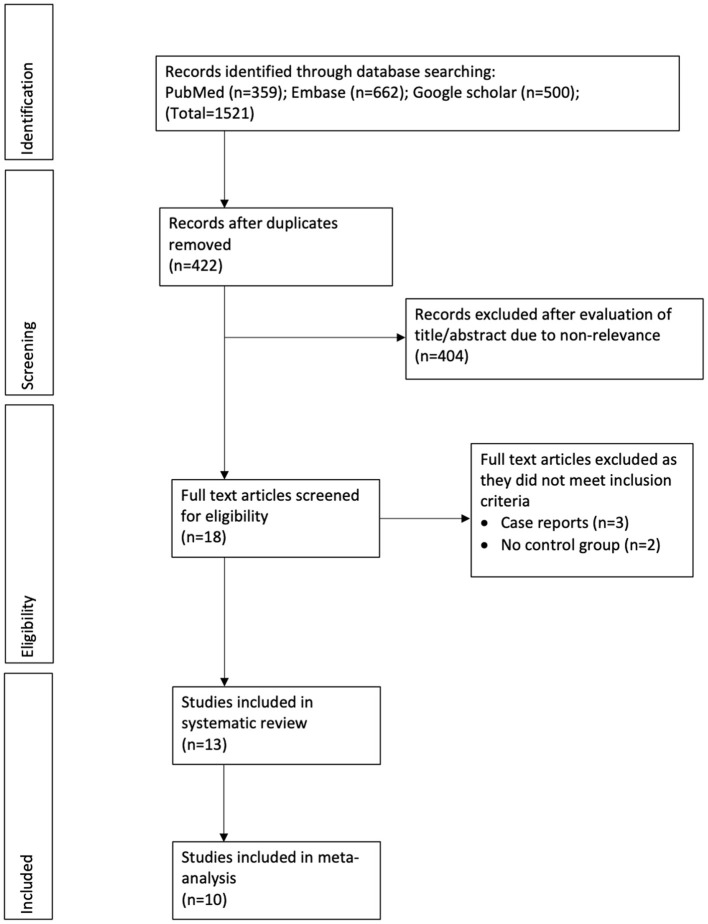
The number of search results at each stage is summarized in Figure 1. Eighteen articles were selected for full-text analysis. Of them, thirteen studies fulfilled the inclusion criteria and were analyzed in this review (21–33).
Figure 1.
Study flow chart.
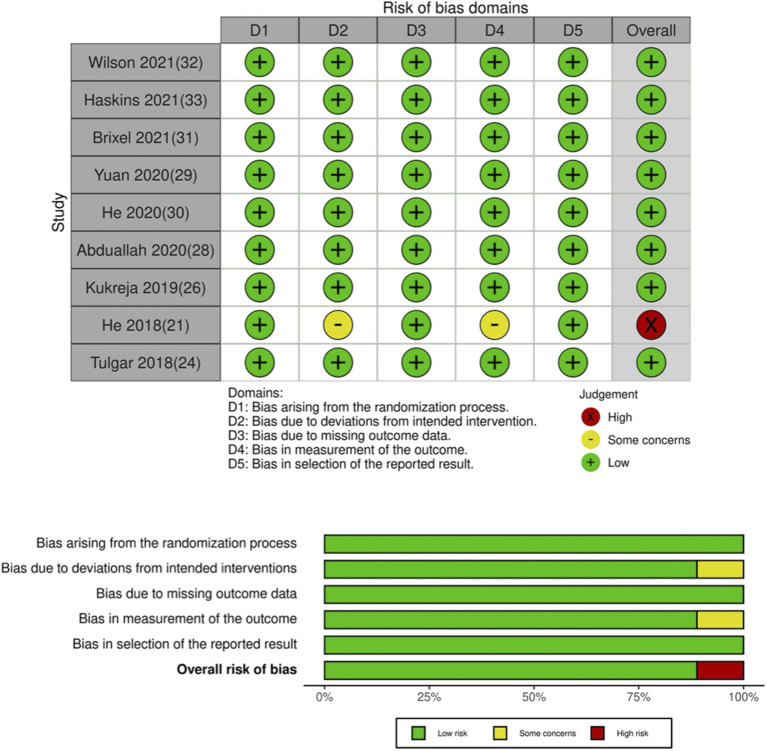
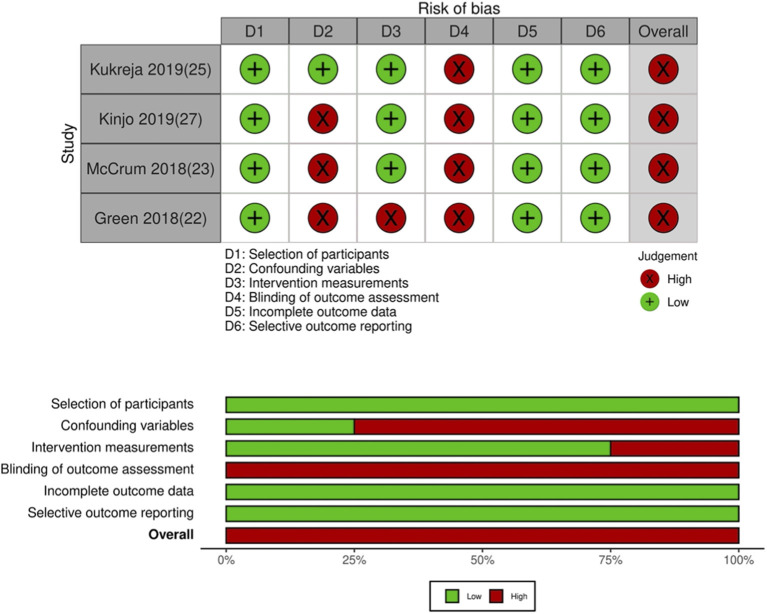
Details of the included studies are presented in Table 1. Nine (21, 24, 26, 28–33) were RCTs while four (22, 23, 25, 27) were retrospective studies. Most studies were carried out in the USA or China. Seven (21, 22, 25, 26, 28, 30, 31) were conducted on patients undergoing hip arthroplasty, while five (23, 27, 29, 32, 33) were on patients undergoing arthroscopic surgeries. The sample size of the QLB group ranged from 10 to 79 patients while that of the control group ranged from 10 to 159 patients. QLB block was administered pre-operatively in all studies except for two RCTs (21, 28) wherein the block was administered after the surgical procedure. Four studies used the anterior approach while one study (32) used the lateral approach for QLB. Ropivacaine was the most common local anesthetic used followed by bupivacaine. The post-operative analgesic protocol differed across the included studies. The authors' judgment of the overall quality of included RCTs is presented in Table 2. Except for the trial of He et al. (21) which has a high risk of bias, all other trials were of high quality with low risk of bias (Figure 2). Quality assessment of non-RCTs is presented in Table 3. The majority of studies had a high risk of bias for confounding factors. Expectedly, all studies had a high risk of bias for blinding of outcome assessment (Figure 3).
Table 1.
Details of included studies.
| References | Type | Location | Type of surgery | Protocol for nerve block | Sample size | Mean/median age (years) | Male gender (%) | Surgery duration (min) | Post-operative analgesic drugs | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| QLB | Control | QLB | Control | QLB | Control | QLB | Control | ||||||
| Wilson et al. (32) | RCT | USA | Arthroscopy | Pre-operative USG guided lateral QLB with 40 ml of 0.25% ropivacaine | 22 | 24 | 29.8 | 37.1 | 36.4 | 41.7 | 149.9 ± 53.1 | 163.6 ± 51.1 | Oxycodone, IV hydromorphone |
| Haskins et al. (33) | RCT | USA | Arthroscopy | Pre-operative USG guided anterior QLB with 30 ml of 0.5% bupivacaine and 2 mg of dexamethasone | 48 | 48 | 36 | 36 | 50 | 45.8 | 95 ± 23 | 95 ± 33 | Oxycodone, PCM and naproxen/indomethacin and IV hydromorphone as rescue analgesic |
| Brixel et al. (31) | RCT | France | Arthroplasty | Pre-operative USG guided posterior QLB with 30 ml of 0.33% ropivacaine | 50 | 50 | 68 | 65 | 60 | 40 | 70 (63–77) | 68 (61–81) | IV PCM, IV ketoprofen, and morphine PCA |
| Yuan et al. (29) | RCT | China | Arthroscopy | Pre-operative USG guided posterior QLB with 0.4% ropivacaine | 40 | 40 | 36.7 | 36.5 | 47.4 | 50 | 80.8 ± 8.1 | 82.5 ± 9.3 | Sufentanil PCA, oral PCM and diclofenac |
| He et al. (30) | RCT | China | Arthroplasty | Pre-operative USG guided posterior QLB with 0.33% ropivacaine | 44 | 44 | 66 | 67 | 29.5 | 25 | 98 ± 8 | 100 ± 7 | IV parecoxib, oral PCM, and morphine PCA |
| Abduallah et al. (28) | RCT | Egypt | Arthroplasty | Post-operative USG guided posterior QLB with 30 ml of 0.25% bupivacaine | 30 | 30 | 67.9 | 66.4 | 30 | 36.7 | 122 ± 9.2 | 125 ± 4.6 | IV PCM and morphine rescue analgesic |
| Kukreja et al. (25) | R | USA | Arthroplasty | Pre-operative USG guided posterior QLB with 20 ml of 0.25% bupivacaine | 79 | 159 | NR | NR | NR | NR | NR | NR | NR |
| Kukreja et al. (26) | RCT | USA | Arthroplasty | Pre-operative USG guided anterior QLB with 30 ml of 0.25% bupivacaine | 36 | 35 | 58.6 | 58 | 44.4 | 57.1 | NR | NR | NR |
| Kinjo et al. (27) | R | USA | Arthroscopy | Pre-operative USG guided anterior QLB with 20–30 ml of 0.33–0.5% ropivacaine | 15 | 54 | 35 | 35 | 33 | 55 | 97 ± 22.6 | 89 ± 20.1 | NR |
| Tulgar et al. (24) | RCT | Turkey | Hip and proximal femur surgery | Pre-operative USG guided posterior QLB with 20 ml of 0.5% bupivacaine and 10 ml of 2% lidocaine | 20 | 20 | 68.7 | 68.7 | 25 | 25 | 107 ± 19.9 | 110 ± 21.3 | IV PCM and tramadol PCA, IV fentanyl and IM diclofenac as rescue analgesic |
| McCrum et al. (23) | R | USA | Arthroscopy | Pre-operative USG guided anterior QLB with 20–30 ml of 0.5% ropivacaine, 20–30 mcg of dexmedetomidine and 4 mg dexamethasone | 28 | 28 | 37 | 36 | 39.3 | 28.6 | 74 ± 34 | 69 ± 20 | IV PCM, IV ketorolac, and IV hydromorphone as rescue analgesic |
| He et al. (21) | RCT | China | Arthroplasty | Post-operative USG guided posterior QLB with 30 ml of 0.33% ropivacaine | 30 | 30 | 64 | 65 | 46.7 | 43.3 | 91 ± 21 | 96 ± 19 | Sufentanil PCA |
| Stuart Green et al. (22) | R | USA | Arthroplasty | Pre-operative USG guided QLB with 30 ml of 0.5% ropivacaine | 10 | 10 | NR | NR | NR | NR | NR | NR | NR |
IV, intravenous; IM, intramuscular; R, Retrospective; RCT, randomized controlled trial; PCM, paracetamol; PCA, patient controlled analgesia; NR, not reported; QLB, quadratus lumborum block; USG, ultrasound.
Table 2.
Risk of bias in included RCTs.
| References | Randomization process | Deviation from intended intervention | Missing outcome data | Measurement of outcomes | Selection of reported result | Overall risk of bias |
|---|---|---|---|---|---|---|
| Wilson et al. (32) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Haskins et al. (33) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Brixel et al. (31) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Yuan et al. (29) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| He et al. (30) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Abduallah et al. (28) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kukreja et al. (26) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| He et al. (21) | Low risk | Some concerns | Low risk | Some concerns | Low risk | High risk |
| Tulgar et al. (24) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
Figure 2.
Risk of bias plot for RCTs.
Table 3.
Risk of bias in included non-RCTs.
| References | Selection of participants | Confounding variables | Intervention measurements | Blinding of outcome assessment | Incomplete outcome data | Selective outcome reporting | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| Kukreja et al. (25) | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| Kinjo et al. (27) | Low risk | High risk | Low risk | High risk | Low risk | Low risk | High risk |
| McCrum et al. (23) | Low risk | High risk | Low risk | High risk | Low risk | Low risk | High risk |
| Stuart Green et al. (22) | Low risk | High risk | High risk | High risk | Low risk | Low risk | High risk |
Figure 3.
Risk of bias plot for non-RCTs.
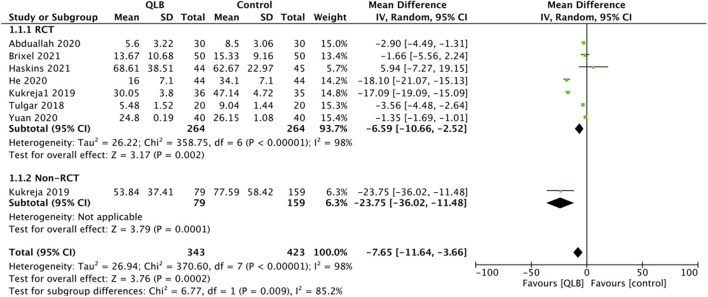
Meta-Analysis
Eight studies reported data on 24-h total analgesic consumption. On pooled analysis, there was a statistically significant reduction of opioid consumption in morphine equivalents in patients receiving QLB as compared to controls (MD: −7.65, 95% CI: −11.64, −3.66 I2 = 98% p = 0.0002) (Figure 4). There was no evidence of publication bias on visual inspection of funnel plot (Supplementary Figure 1). The results did not change on exclusion of any study during a sensitivity analysis. Sub-group analysis of RCTs (MD: −6.59, 95% CI: −10.66, −2.52 I2 = 98% p = 0.002) and the lone non-RCT (MD: −23.75, 95% CI: −36.02, −11.48 p = 0.0001) demonstrated similar results (Figure 4). On excluding two studies on arthroscopy (29, 33), meta-analysis of RCTs reporting only arthroplasty results revealed significantly reduced opioid consumption in the QLB group (MD: −8.67, 95% CI: −14.90, −2.44 I2 = 98% p = 0.006) (Supplementary Figure 2).
Figure 4.
Meta-analysis of 24-h total analgesic consumption between QLB and control groups with sub-group analysis based on study type.
On meta-analysis of pain scores at rest, we noted a statistically significant reduction of pain scores in the QLB group at 2–4 h (MD: −0.57, 95% CI: −0.98, −0.17 I2 = 61% p = 0.005), 6–8 h (MD: −1.45, 95% CI: −2.09, −0.81 I2 = 86% p < 0.00001), 12 h (MD: −1.12, 95% CI: −1.89, −0.34 I2 = 93% p = 0.005), 24 h (MD: −0.71, 95% CI: −1.27, −0.15 I2 = 89% p = 0.01) and 48 h (MD: −0.76, 95% CI: −1.37, −0.16 I2 = 85% p = 0.01) as compared to control group (Figure 5). On exclusion of two retrospective studies in the analysis (25, 27), the results did not change significance and there was a statistically significant reduction of pain scores at 2–4 h (MD: −0.60, 95% CI: −1.02, −0.18 I2 = 67% p = 0.005), 6–8 h (MD: −1.45, 95% CI: −2.09, −0.81 I2 = 86% p < 0.0001), 12 h (MD: −1.05, 95% CI: −1.91, −0.20 I2 = 94% p = 0.02), 24 h (MD: −0.85, 95% CI: −1.45, −0.25 I2 = 89% p = 0.006) and 48 h (MD: −1.07, 95% CI: −1.57, −0.57 I2 = 75% p < 0.0001) in patients receiving QLB as compared to controls (Supplementary Figure 3). During the sensitivity analysis, exclusion of the study of Yuan et al. (29) from the 24 h pain score changed the significance of the results, but still indicated a tendency of lower pain scores with QLB (MD: −0.53, 95% CI: −1.08, 0.01 I2 = 88% p = 0.05) (Supplementary Figure 4). Similarly, results of the 48 h pain scores turned non-significant on sequential exclusion of the study by He et al. (21) (MD: −0.46, 95% CI: −1.21, 0.29 I2 = 72% p = 0.23) (Supplementary Figure 5) and He et al. (30) (MD: −0.69, 95% CI: −1.88, 0.50 I2 = 89% p = 0.26) (Supplementary Figure 6). There was no change in the significance of remaining pain scores on exclusion of any study.
Figure 5.
Meta-analysis of pain scores between QLB and control groups with sub-group at different time points.
Adverse events were reported only by RCTs, and the common adverse events noted were post-operative nausea and vomiting (PONV), pruritis, and urinary retention. On pooled analysis, we noted a statistically significant reduced risk of PONV (RR: 0.40, 95% CI: 0.18, 0.88 I2 = 62% p = 0.02) in patients receiving QLB but no difference in the risk of pruritis (RR: 0.46, 95% CI: 0.17, 1.24 I2 = 16% p = 0.13) and urinary retention (RR: 0.44, 95% CI: 0.19, 1.02 I2 = 0% p = 0.06) (Figure 6).
Figure 6.
Meta-analysis of adverse events between QLB and control groups.
Certainty of Evidence
Assessment of certainty of evidence based on GRADE is presented in Supplementary Table 3. GRADE assessment was carried out only for the outcomes from RCTs and not from retrospective studies. Overall, the certainty of the evidence was “moderate” for total analgesic consumption and pain scores and “low-moderate” for complications.
Meta-Regression Analysis
Results of meta-regression analysis for the outcomes of 24-h total analgesic consumption, 12 and 24 h pain scores are presented in Supplementary Tables 4–6, respectively. Scatter plots of the meta-regression analysis are presented as Supplementary Figures 7–21. None of the included covariates were found to significantly affect 24-h total analgesic consumption or 12 h pain scores. For the outcome of 24 h pain scores, only type of local anesthetic was found to significantly impact pain scores. Use of bupivacaine vs. ropivacaine was found to reduce mean difference indicating better pain control with ropivacaine (p = 0.02).
Descriptive Analysis
Three studies were not included in the meta-analysis. The retrospective study of McCrum et al. (23) compared outcomes of 28 patients with QLB with 28 patients receiving no block. The authors noted a statistically significant reduction of opioid consumption in the entire post-operative period for patients receiving QLB as compared to controls (QLB: 6.53 ± 7.61 vs. No block: 14.02 ± 0.38, p < 0.001). Pain at discharge was also significantly lower in the QLB group (2.57 ± 2.29) as compared to the control group (4.18 ± 2.14) (p = 0.015). In the second study, Stuart Green et al. (22) retrospectively compared outcomes of 10 patients receiving QLB with 10 patients not receiving any block. The authors noted no statistically significant difference in fentanyl utilization in the post-anesthetic care unit (PACU) (QLB: 45 ± 59.8 vs. control: 25 ± 42.4; p = 0.4) or in the 24 h mean VAS scores (QLB: 5.48 ± 2 vs. control: 6.45 ± 2.5; p = 0.38) between the two groups. The RCT of Wilson et al. (32) compared outcomes of 22 patients receiving QLB with 24 controls. The authors noted significantly reduced opioid consumption in the PACU in patients receiving QLB as compared to controls [mean (95% CI); QLB: 8.1 (6, 10.2) vs. control 11.3 (9, 13.6) (p = 0.03)]. Pain scores at PACU discharge were, however, not significantly different between the two groups (57.9 ± 22.2 vs. 59.2 ± 22.6) (p = 0.84).
Discussion
The current systematic review and meta-analysis aimed to summarize evidence on the efficacy of QLB for patients undergoing hip surgeries. Our analysis demonstrates that hip surgery patients receiving QLB have significantly reduced total opioid consumption in the first 24 h and have reduced pain scores up to 48 h after the procedure. Furthermore, the incidence of PONV is reduced in patients receiving QLB.
An essential element of post-operative care of hip surgery patients involves optimal pain control, reduced opioid consumption, and early mobilization. Indeed, the enhanced recovery after surgery protocol, which includes multimodal analgesia and early mobilization, has been shown to reduce the length of hospital stay and incidence of complications after hip surgeries (34). While epidural anesthesia and nerve blocks are popular methods of pain control, they can also delay ambulation which can slow down post-operative recovery (31). Therefore, there is a need for less invasive regional anesthetic techniques like the interfacial plane blocks (35). Unlike peripheral regional blocks which have specific neural endpoints, interfacial nerve blocks like the QLB are injected in tissue planes and target variable nerve endings depending upon the spread of local anesthetic (35). Over the past decade, the QLB has been used for proving analgesia after several surgical procedures, but its efficacy for hip surgeries is still unclear (14, 15).
In our analysis, we noted a statistically significant reduction of opioid consumption in the first 24-h after surgery in patients receiving the QLB. While the results were derived mostly from RCTs, one included retrospective study also demonstrated similar conclusions. Qualitative analysis of studies revealed similar outcomes for two of the three studies. Our results are in agreement with prior meta-analysis studies of Jin et al. (14) and Korgvee et al. (15) who have also reported significantly reduced 24-h opioid consumption with QLB on a pooled analysis of studies mostly on cesarean sections, renal or abdominal surgeries. However, high heterogeneity in the quantitative analysis (98%) downgraded the certainty of evidence in our study to “moderate.” This heterogeneity was persistent even on sub-group analysis based on study type, and after excluding two studies on arthroscopy. Similar high heterogeneity has been noted in the previous meta-analysis of the QLB (15). We believe that it stems from the different multimodal analgesia protocols used in the included studies, leading to significantly variable opioid consumption amongst the included patients. This is further strengthened by the fact that none of the included covariates in the meta-regression analysis were found to impact outcomes.
In the second part of our analysis, we noted that patients receiving QLB had consistently lower pain scores at all time points from 2–4 to 48 h. The results remained statistically significant even on the exclusion of the retrospective studies, thereby demonstrating the stability of our results. Nevertheless, the crucial detail lies in the MD between the two groups at the different time intervals. In the analysis of all included studies, the MD in pain scores between QLB and control ranged from −0.57 to −1.45, while in the analysis of RCTs, it ranged from −0.60 to −1.45. Considering these values with the concept of “minimally important clinical difference” (MCID) for pain scores, the pain reduction may not have been clinically relevant (36). In a recent study, Laigaard et al. (37) have shown that MCID for pain at rest after hip/knee arthroplasty was 1.5 and MCID for 24-h opioid consumption was 10 mg in morphine equivalents. Given the small MD in pain scores and MD of 7.65 for total opioid consumption, detected in our analysis, we believe that the clinical relevance of analgesia offered by QLB in hip surgeries may be questionable, despite the statistically significant results. Due to the high heterogeneity amongst the studies, further trials are required to elucidate if the use of QLB in hip surgeries leads to clinically important pain reduction. Secondly, it is important to note that two different local anesthetics were used by the included studies, namely, bupivacaine and ropivacaine. Meta-regression analysis based on type of drug did not demonstrate significant results for 12 h pain scores but indicated that ropivacaine may offer better pain reduction at 24 h. However, the results should be interpreted with caution due to the limited number of studies in the analysis.
An important limitation of the review is that we could not separate outcomes of different QLB via a subgroup analysis due to limited data. Only a meta-regression of important variables was performed which indicated no effect of type of QLB on analgesic consumption and 12, 24 h pain scores. Research has suggested that the approach of the QLB (anterior, lateral, or posterior) can result in variable anesthetic spread ranging from T6 to L4 (13). However, the systematic review of Jin et al. (14) has reported that the approach of QLB does not seem to impact the analgesic efficacy. While most of the studies included in our review utilized the posterior QLB, a few did report the use of anterior or lateral QLB but with variable results. While Haskins et al. (33) reported the lack of beneficial effect with anterior QLB in hip arthroscopic surgeries, Kukreja et al. (26) found a statistically significant reduction in pain scores and opioid consumption with anterior QLB in patients undergoing hip arthroplasties. Another retrospective study of Kinjo et al. (27) also reported no significant difference in pain scores with anterior QLB. Such variability of results can be partly explained by the lack of clarity on the mechanism of action of interfacial blocks (31). Even cadaveric studies investigating dye spread following QLB have produced inconsistent results, with one study (38) reporting dye spread up to the lumbar nerve roots with anterior QLB while another reporting no such effect (39). It has also been postulated that small changes in the needle position and different approaches of QLB can significantly alter the quality of analgesia offered by the block (27). On the other hand, Brixel et al. (31) have demonstrated that even with rigorous control of needle position in the posterior QLB, the anesthetic solution had an unpredictable spread. The authors have suggested that the spread of the anesthetic solution after QLB depends more on tissue compliance rather than the needle position in the thoracolumbar interfascial plane. Since interfacial nerve blocks are relatively new in the field of regional anesthesia, with limited studies on their exact mechanism, further research is needed to shed light on the variability of analgesia with different approaches of these blocks.
Our meta-analysis demonstrated a significantly reduced risk of PONV with QLB. This provides indirect evidence of reduced opioid usage in the QLB group with subsequent reduction of opioid-related side effects. However, there were no differences in the risk of other opioid-related adverse events like pruritis or urinary continence probably due to the limited number of studies in the meta-analysis. Important block-related adverse events of clinical relevance like muscle weakness were not universally reported by the included studies and hence could not be analyzed.
Our results concur with a recently published meta-analysis of Koo et al. (40) which has also assessed the efficacy of QLB for hip surgeries. The authors in their pooled analysis of nine RCTs have demonstrated reduced post-operative opioid consumption and incidence of PONV with the QLB in patients undergoing hip surgeries. However, unlike their review, our study also included non-RCTs to present comprehensive evidence on the efficacy of QLB for hip surgeries. Furthermore, we also conducted subgroup analysis based on the study type and presented separate data for arthroplasty studies in our review.
The results of our review should be interpreted with the following limitations. Firstly, as mentioned earlier, there was significant heterogeneity in our analysis which can be attributed to the methodological differences in the included studies. Other than differences in the post-operative analgesic regimen, the studies varied in the type of surgery, type and volume of local anesthetics, the use of adjuvants, the timing of QLB, and the approach of the block. We were unable to perform subgroup analysis for these variables due to limited data. Therefore, our meta-analysis was unable to judge which is the best approach for QLB for pain control in hip surgeries. Secondly, only 13 studies were available for inclusion in the review, of which just nine were RCTs. Variability in reporting of data further reduced the number of studies available for the meta-analysis. Thirdly, important outcomes like time to first analgesic request and muscle weakness associated with the block, the ideal volume of anesthetic required for the block, and the level of sensory anesthesia provided by the block could not be analyzed due to the lack of reporting from the included studies. Lastly, several different practitioners with variable experience were involved in administering the QLB in the included studies. The impact of practitioner skill on the study outcomes could not be assessed.
Clinical Significance
The treatment strategy for patients undergoing hip surgery should be focused at providing optimal analgesia and improved patient satisfaction in the immediate post-operative period. In this context, we believe that the QLB can be a valuable regional anesthetic technique for patients undergoing hip surgeries. We recommend that anesthetists should routinely use the QLB along with their standard analgesic regimen to provide better pain control in these patients. Use of only systemic analgesics may not be recommended since the addition of QLB seems to be safe without any serious adverse events. Future research focusing on the efficacy of QLB on specific types of hip surgeries like arthroscopy and arthroplasty shall enhance our understanding of the efficacy of this block for pain control. Also, further research is also needed to analyze which is the best QLB approach for patients undergoing hip surgery.
Conclusions
Our systematic review and meta-analysis indicated that the QLB as a part of multimodal analgesia protocol reduces opioid consumption and pain scores in patients undergoing hip surgeries. The certainty of evidence based on GRADE was moderate. Despite the statistically significant results, the clinical relevance of the analgesic efficacy offered by the QLB is debatable owing to the small effect size. Further studies assessing the efficacy of QLB against standard analgesic protocols are needed to strengthen the current evidence, and should also compare outcomes with different approaches of QLB to provide evidence on what constitutes the best approach.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
JLi and CW conceptualized and designed the study. JH and YL did literature search and data collection. HL and JLiu analyzed the data. JLi wrote the paper. JLiu and CJ reviewed and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was funded by Science and Technology Research Project of Guangdong Provincial Hospital of Chinese Medicine (No. YN2019ML08), Science and Technology Program of Guangzhou (202102010273), Science and Technology Planning Project of Guangdong Province (No. 2020A1414050050), the Project of Guangdong Provincial Department of Finance [Nos. (2014)157, (2018)8], and National key research and development program (2021YFC1712804).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.771859/full#supplementary-material
Funnel plot for the meta-analysis of 24-h total analgesic consumption between QLB and control groups.
Meta-analysis of 24-h total analgesic consumption between QLB and control groups with exclusion of studies on arthroscopy.
Meta-analysis of pain scores between QLB and control groups with the exclusion of retrospective studies.
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of Yuan et al. (24 h subgroup).
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of He et al. (21) (48 h subgroup).
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of He et al. (30) (48 h subgroup).
Meta-regression plot assessing the impact of mean age on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of male gender on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of sample size on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of QLB type on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of local anesthetic type on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of mean age on 12 h pain scores.
Meta-regression plot assessing the impact of male gender on 12 h pain scores.
Meta-regression plot assessing the impact of sample size on 12 h pain scores.
Meta-regression plot assessing the impact of QLB type on 12 h pain scores.
Meta-regression plot assessing the impact of local anesthetic on 12 h pain scores.
Meta-regression plot assessing the impact of mean age on 24 h pain scores.
Meta-regression plot assessing the impact of male gender on 24 h pain scores.
Meta-regression plot assessing the impact of sample size on 24 h pain scores.
Meta-regression plot assessing the impact of QLB type on 24 h pain scores.
Meta-regression plot assessing the impact of local anesthetic on 24 h pain scores.
PRISMA checklist.
Search strategy.
GRADE assessment of evidence.
Meta-regression analysis for the heterogeneity of post-operative 24 h total analgesic consumption.
Meta-regression analysis for the heterogeneity of 12 h pain scores.
Meta-regression analysis for the heterogeneity of 24 h pain scores.
References
- 1.Hasan K, Shankar S, Sharma A, Carter A, Zaidi R, Cro S, et al. Hip surgery and its evidence base: progress over a decade? J Orthop Traumatol. (2016) 17:291–5. 10.1007/s10195-016-0421-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Min K, Beom J, Kim BR, Lee SY, Lee GJ, Lee JH, et al. Clinical practice guideline for postoperative rehabilitation in older patients with hip fractures. Ann Rehabil Med. (2021) 45:225–59. 10.5535/arm.21110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okamoto T, Ridley RJ, Edmondston SJ, Visser M, Headford J, Yates PJ. Day-of-surgery mobilization reduces the length of stay after elective hip arthroplasty. J Arthroplasty. (2016) 31:2227–30. 10.1016/j.arth.2016.03.066 [DOI] [PubMed] [Google Scholar]
- 4.Bugada D, Bellini V, Lorini LF, Mariano ER. Update on selective regional analgesia for hip surgery patients. Anesthesiol Clin. (2018) 36:403–15. 10.1016/j.anclin.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 5.Indelli PF, Grant SA, Nielsen K, Vail TP. Regional anesthesia in hip surgery. Clin Orthop Relat Res. (2005) 441:250–5. 10.1097/01.blo.0000192355.71966.8e [DOI] [PubMed] [Google Scholar]
- 6.Choi YJ, Kim M-H, Chung EK, Lee JK, Yoon J, Yug JS, et al. Prevalence and seriousness of analgesic-induced adverse events in korea: a 10-year nationwide surveillance. J Patient Saf. (2020) 16:e215–24. 10.1097/PTS.0000000000000742 [DOI] [PubMed] [Google Scholar]
- 7.Hannon CP, Fillingham YA, Nam D, Courtney PM, Curtin BM, Vigdorchik J, et al. The efficacy and safety of opioids in total joint arthroplasty: systematic review and direct meta-analysis. J Arthroplasty. (2020) 35:2759–71.e13. 10.1016/j.arth.2020.05.032 [DOI] [PubMed] [Google Scholar]
- 8.Cuenca-Llavall M, Pérez-Prieto D, Santiveri FJ, Garcia AL, Marqués F. The Influence of Local Infiltration Analgesia After Total Hip Replacement. A Randomized Clinical Trial. undefined (2020). Available online at: https://www.semanticscholar.org/paper/The-influence-of-local-infiltration-analgesia-after-Cuenca-Llavall-Pérez-Prieto/71fa73b54504f5f14ce251f600ede9084a0589ee (accessed August 5, 2021). [PubMed]
- 9.Zoric L, Cuvillon P, Alonso S, Demattei C, Vialles N, Asencio G, et al. Single-shot intraoperative local anaesthetic infiltration does not reduce morphine consumption after total hip arthroplasty: a double-blinded placebo-controlled randomized study. Br J Anaesth. (2014) 112:722–8. 10.1093/bja/aet439 [DOI] [PubMed] [Google Scholar]
- 10.La Colla L, Uskova A, Ben-David B. Single-shot quadratus lumborum block for postoperative analgesia after minimally invasive hip arthroplasty: a new alternative to continuous lumbar plexus block? Reg Anesth Pain Med. (2017) 42:125–6. 10.1097/AAP.0000000000000523 [DOI] [PubMed] [Google Scholar]
- 11.Hockett MM, Hembrador S, Lee A. Continuous quadratus lumborum block for postoperative pain in total hip arthroplasty: a case report. A Case Rep. (2016) 7:129–31. 10.1213/XAA.0000000000000363 [DOI] [PubMed] [Google Scholar]
- 12.Blanco R. Tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. (2007) 32:130–130. 10.1016/j.rapm.2007.06.26817350524 [DOI] [Google Scholar]
- 13.Ueshima H, Otake H, Lin J-A. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed Res Int. (2017) 2017:2752876. 10.1155/2017/2752876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jin Z, Liu J, Li R, Gan TJ, He Y, Lin J. Single injection Quadratus Lumborum block for postoperative analgesia in adult surgical population: a systematic review and meta-analysis. J Clin Anesth. (2020) 62:109715. 10.1016/j.jclinane.2020.109715 [DOI] [PubMed] [Google Scholar]
- 15.Korgvee A, Junttila E, Koskinen H, Huhtala H, Kalliomaki M-L. Ultrasound-guided quadratus lumborum block for postoperative analgesia: a systematic review and meta-analysis. Eur J Anaesthesiol. (2021) 38:115–29. 10.1097/EJA.0000000000001368 [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions. Version 6 Cochrane (2019). Available online at: www.training.cochrane.org/ (accessed June 1, 2021).
- 18.Kim SY, Park JE, Lee YJ, Seo H-J, Sheen S-S, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. (2013) 66:408–14. 10.1016/j.jclinepi.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 19.Washington State Agency Medical Directors' Group . Opioid Dose Calculator. Available online at: http://www.agencymeddirectors.wa.gov/Calculator/DoseCalculator.htm (accessed August 10, 2020).
- 20.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He J, Zheng X, Luo C, Huang Z, He W, Wang H, et al. Effects and safety of quadratus lumborum block in analgesia after hip arthroplasty. Natl Med J China. (2018) 98:565–9. 10.3760/cma.j.issn.0376-2491.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 22.Stuart Green M, Hoffman CR, Iqbal U, Ives OO, Hurd B. Transmuscular quadratus lumborum block reduces length of stay in patients receiving total hip arthroplasty. Anesthesiol Pain Med. (2018) 8:e80233. 10.5812/aapm.80233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCrum CL, Ben-David B, Shin JJ, Wright VJ. Quadratus lumborum block provides improved immediate postoperative analgesia and decreased opioid use compared with a multimodal pain regimen following hip arthroscopy. J hip Preserv Surg. (2018) 5:233–9. 10.1093/jhps/hny024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tulgar S, Kose HC, Selvi O, Senturk O, Thomas DT, Ermis MN, et al. Comparison of ultrasound-guided lumbar erector spinae plane block and transmuscular quadratus lumborum block for postoperative analgesia in hip and proximal femur surgery: a prospective randomized feasibility study. Anesth Essays Res. (2018) 12:825–31. 10.4103/aer.AER_142_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kukreja P, MacBeth L, Potter W, Buddemeyer K, DeBell H, Elsharkawy H, et al. Posterior quadratus lumborum block for primary total hip arthroplasty analgesia: a comparative study. Einstein (São Paulo). (2019) 17:eAO4905. 10.31744/einstein_journal/2019AO4905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kukreja P, MacBeth L, Sturdivant A, Morgan CJ, Ghanem E, Kalagara H, Chan VWS. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled study. Reg Anesth Pain Med. (2019) 44:1075–9. 10.1136/rapm-2019-100804 [DOI] [PubMed] [Google Scholar]
- 27.Kinjo S, Kolodzie K, Dong K, Zhang AL. The effects of transmuscular quadratus lumborum blocks on postoperative pain in arthroscopic hip surgery: a cohort analysis. J Anesth. (2019) 33:516–22. 10.1007/s00540-019-02659-9 [DOI] [PubMed] [Google Scholar]
- 28.Abduallah MA, Ahmed SA, Abdelghany MS. The effect of post-operative ultrasound-guided transmuscular quadratus lumborum block on post-operative analgesia after hip arthroplasty in elderly patients: a randomised controlled double-blind study. Indian J Anaesth. (2020) 64:887–93. 10.4103/ija.IJA_275_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuan L, Zhang Y, Xu C, Wu A. Postoperative analgesia and opioid use following hip arthroscopy with ultrasound-guided quadratus lumborum block: a randomized controlled double-blind trial. J Int Med Res. (2020) 48:300060520920996. 10.1177/0300060520920996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He J, Zhang L, He WY, Li DL, Zheng XQ, Liu QX, et al. Ultrasound-guided transmuscular quadratus lumborum block reduces postoperative pain intensity in patients undergoing total hip arthroplasty: a randomized, double-blind, placebo-controlled. Trial Pain Res Manag. (2020) 2020:1035182. 10.1155/2020/1035182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brixel SM, Biboulet P, Swisser F, Choquet O, Aarab Y, Nguyen H, et al. Posterior quadratus lumborum block in total hip arthroplasty: a randomized controlled trial. Anesthesiology. (2021) 134:722–33. 10.1097/ALN.0000000000003745 [DOI] [PubMed] [Google Scholar]
- 32.Wilson SH, George RM, Matos JR, Wilson DA, Johnson WJ, Woolf SK. Preoperative quadratus lumborum block reduces opioid requirements in the immediate postoperative period following hip arthroscopy: a randomized, blinded clinical trial. Arthroscopy. (2021). 10.1016/j.arthro.2021.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haskins SC, Tseng A, Zhong H, Mamic M, Cheng SI, Nejim JA, et al. Anterior quadratus lumborum block does not provide superior pain control after hip arthroscopy: a double-blinded randomized controlled trial. Anesthesiology. (2021) 135:433–41. 10.1097/ALN.0000000000003853 [DOI] [PubMed] [Google Scholar]
- 34.Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. (2017) 93:736–42. 10.1136/postgradmedj-2017-134991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. (2018) 43:341–6. 10.1097/AAP.0000000000000750 [DOI] [PubMed] [Google Scholar]
- 36.Olsen MF, Bjerre E, Hansen MD, Hilden J, Landler NE, Tendal B, Hróbjartsson A. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. (2017) 15:1–18. 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laigaard J, Pedersen C, Rønsbo TN, Mathiesen O, Karlsen APH. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: a systematic review. Br J Anaesth. (2021) 126:1029–37. 10.1016/j.bja.2021.01.021 [DOI] [PubMed] [Google Scholar]
- 38.Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ, et al. radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. (2017) 72:73–9. 10.1111/anae.13647 [DOI] [PubMed] [Google Scholar]
- 39.Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. (2017) 125:303–12. 10.1213/ANE.0000000000001922 [DOI] [PubMed] [Google Scholar]
- 40.Koo CH, Ahn S, Na HS Ryu JH, Shin HJ. Efficacy of quadratus lumborum block for analgesia in adult participants undergoing hip surgery: a meta-analysis of randomized controlled trials. J Clin Anesth. (2021) 75:110560. 10.1016/j.jclinane.2021.110560 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Funnel plot for the meta-analysis of 24-h total analgesic consumption between QLB and control groups.
Meta-analysis of 24-h total analgesic consumption between QLB and control groups with exclusion of studies on arthroscopy.
Meta-analysis of pain scores between QLB and control groups with the exclusion of retrospective studies.
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of Yuan et al. (24 h subgroup).
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of He et al. (21) (48 h subgroup).
Meta-analysis of pain scores between QLB and control groups with exclusion of the study of He et al. (30) (48 h subgroup).
Meta-regression plot assessing the impact of mean age on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of male gender on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of sample size on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of QLB type on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of local anesthetic type on 24-h total analgesic consumption.
Meta-regression plot assessing the impact of mean age on 12 h pain scores.
Meta-regression plot assessing the impact of male gender on 12 h pain scores.
Meta-regression plot assessing the impact of sample size on 12 h pain scores.
Meta-regression plot assessing the impact of QLB type on 12 h pain scores.
Meta-regression plot assessing the impact of local anesthetic on 12 h pain scores.
Meta-regression plot assessing the impact of mean age on 24 h pain scores.
Meta-regression plot assessing the impact of male gender on 24 h pain scores.
Meta-regression plot assessing the impact of sample size on 24 h pain scores.
Meta-regression plot assessing the impact of QLB type on 24 h pain scores.
Meta-regression plot assessing the impact of local anesthetic on 24 h pain scores.
PRISMA checklist.
Search strategy.
GRADE assessment of evidence.
Meta-regression analysis for the heterogeneity of post-operative 24 h total analgesic consumption.
Meta-regression analysis for the heterogeneity of 12 h pain scores.
Meta-regression analysis for the heterogeneity of 24 h pain scores.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.