Abstract
Prior studies have shown that self- and manual massage (SMM) increases flexibility in non-adjacent body areas. It is unclear whether this also influences performance in terms of force generation. Therefore, this study investigated the effect of SMM on the plantar surface on performance in the dorsal kinetic chain. Seventeen young participants took part in this within-subject non-randomized controlled study. SMM was applied on the plantar surface of the dominant leg, but not on the non-dominant leg. A functional performance test of the dorsal kinetic chain, the Bunkie Test, was conducted before and after the intervention. We measured the performance in seconds for the so-called posterior power line (PPL) and the posterior stabilizing line (PSL). The performance of the dominant leg in the Bunkie Test decreased significantly by 17.2% from (mean ± SD) 33.1 ± 9.9 s to 27.4 ± 11.1 s for the PPL and by 16.3% from 27.6 ± 9.8 s to 23.1 ± 11.7 s for the PSL. This is in contrast to the non-dominant leg where performance increased significantly by 5.1% from 29.7 ± 9.6 s to 31.1 ± 8.9 s for the PPL and by 3.1% from 25.7 ± 1.5 s to 26.5 ± 1.7 s for the PSL. SMM interventions on the plantar surface might influence the performance in the dorsal kinetic chain.
Key points.
This study investigated the acute effects of self- and therapeutic massage on the plantar fascia on performance in the dorsal kinetic chain.
Our results showed a significantly reduced performance of the treated leg after the intervention.
In contrast, the performance in the contralateral leg (no intervention) improved.
Key words: Fascial chain, myofascial release, foam rolling, plantar fascia, superficial backline, Bunkie Test
Introduction
Fascia used to be seen as a simple connective packaging tissue. However, that has changed over the past few years and it is now considered to be a three dimensional, functional structure which supports the interaction of body systems (Adstrum et al., 2017; Stecco et al., 2018). This highlights fascias’ active role as an expansive tensegrity network with proprioceptive and nociceptive functions (Adstrum et al., 2017). Within this tensegrity network, fascial continuity was observed along functional muscle groups. One of these fascial chains is the superficial backline (SBL), whose existence is widely accepted. It expands from the plantar fascia (PF), over the Achilles tendon, the gastrocnemii muscles, the hamstrings, the sacrotubero-us ligament, the back and, eventually, the head (Myers, 2013; Stecco et al., 2019; Wilke et al., 2016).
Prior reviews have shown that self- and manual massage techniques (SMM) increased acutely either the range of motion of single joints or along myofascial chains (Cheatham et al., 2015; Hughes and Ramer, 2019; Wiewelhove et al., 2019; Wilke et al., 2020a; 2020b). The latter has been already investigated along the SBL. For example, studies showed that a single foam rolling application on the plantar surface led to an acute increase in range of motion of the dorsal thigh and lower back (Grieve et al., 2015; Kwangsun et al., 2018). This implies that fascial chains might be able to modify their properties or functional capacities in non-adjacent areas along their course (Krause et al., 2016). Besides a force transmission along myofascial chains, other potential mechanisms explaining such non-local range of motion augmentations include an altered systemic (i.e. global) pain perception as well as an enhanced stretch tolerance (Behm et al., 2021a).
Yet, the PF shows strong connections to adjoining structures of the Achilles Tendon as well as movement induced stabilizing mechanisms (Wearing et al., 2006; Zwirner et al., 2020). Therefore, its main functional capacity might be rather supporting active force generation in the legs during movement.
Contrary to the studies on the acute effects of SMM on flexibility, the findings concerning the effect of SMM on muscle force or athletic performance on the applied muscle are rather heterogeneous (Cheatham et al., 2015; Hughes and Ramer, 2019; Wiewelhove et al., 2019). Behm et al. (2020a) reported, for example, that after foam rolling slight decreases in strength and jump measures were found. However, the same cannot be claimed for fatigue and sprint performance, as there exists no sufficient evidence for any foam rolling on these parameters. Cadaveric studies provided evidence for a potential transfer of tension between adjacent myofascial structures, as it was shown for flexibility (Krause et al., 2016). Few in-vivo studies speculated that force transmission along the SBL also might be possible (Cruz-Montecinos et al., 2015; Wilke et al., 2020a). Recently, Wilke et al. (2020a) showed that the passive dorsal extension of the ankle influences tissue displacement in the hamstrings region, which the authors interpreted as a surrogate for the measurement of force. However, it is unclear whether direct SMM techniques on the plantar surface, as described in the studies concerning the modification of flexibility along the SBL, also influence force transmission.
Therefore, the aim of the study was to investigate whether a combined self- and therapeutic SMM, namely foam rolling, plantar fascia specific stretching, soft tissue mobilization, gliding massage, direct deep friction and manual pressure on the PF influences myofascial force generation in the SBL. As we designed our study particularly for application of newly gained insights and techniques in everyday practice, we decided to use the Bunkie Test to measure functional force generation in the SBL (De Witt and Venter, 2009).
Methods
Study design
This controlled study was conducted in accordance with the ethical principles of the Declaration of Helsinki, and followed all governmental and hygienic guidelines concerning the COVID 19 pandemic. A vote of approval for the study has also been obtained from the ethics committee of the Technical University of Munich (576/20 S-EB). As fascial connectivity is present within the whole body, the study was conducted in a within subject design, where the intervention was performed on the subjects’ dominant leg while the other leg served as the control. We applied the intervention standardized to the dominant leg instead of randomization due to possible differences in muscular or fascial tissue between the legs. All participants provided written informed consent prior to testing. In order to maintain the reporting quality, the study followed the CONSORT guideline extension for within-person trials (Pandis et al., 2019). In addition, we considered the CONSORT guideline adaptations for non-randomized trials (Reeves and Gaus, 2004).
Objectives
The research question was whether there is a difference between the legs with respect to force generation in the dorsal kinetic chain after an SMM intervention on the plantar surface of the dominant leg. Therefore, we stated the following two-sided hypothesis. H0: There is no difference between the legs with respect to force generation in the dorsal kinetic chain after an SMM intervention on the plantar surface of the dominant leg. The dependent outcome variable was the approximation of force generation in the dorsal kinetic chain. This was measured in seconds through the subjects’ performances in the Bunkie Test for (1) the posterior power line (PPL) and (2) the posterior stabilizing line (PSL), which are both structurally corresponding with the superficial backline.
Participants
In total, 17 healthy, recreationally active participants (nine female, eight male) between 18 and 30 years (mean±SD, age, 25.0 ± 3.2 years; height, 1.72 ± 0.08 m; weight, 66.8 ± 11.4 kg) participated in this study. Subjects were excluded if they suffered from current musculoskeletal pain or other orthopedic diseases in the lower extremity, lower back, shoulders or elbows, as well as other nonspecific musculoskeletal disorders like fibromyalgia. There must not have been any history of surgery or other orthopedic injury in the back or legs in the last twelve months. In addition, participants were excluded if they were pregnant, in the nursing period, diagnosed with any psychiatric, endocrine, neurological and metabolic disorders, or if they took medication that affects perception or proprioception. We screened for red flags and contraindications concerning manual therapeutic techniques and did not allow participation if there were indications for any of the following risk factors: tumor, fracture, rheumatoid arthritis, coagulation disorder, anticoagulation or osteoporosis. Participants were not allowed to take part in the study if they performed regular foam rolling at least once a week or were in current physical therapy or other manual therapeutic treatment. If all eligibility criteria held true, the examiner enrolled subjects in the study.
Study procedure
Before testing, participants were informed about the potential general side effects of manual or massage therapy like feeling discomfort, aching or soreness in the treated area, which commonly resolves within 24 to 36 hours (Carnes et al., 2010). They were not informed of the research question, study design or the expected outcome. Subjects were instructed not to participate in heavy physical exercise and not to drink any alcohol in the 24 hours preceding the examination. They were also asked not to drink caffeine, not to smoke or eat in the two hours before the intervention. The testing procedure consisted of one session and lasted about 60 minutes. First, in order to determine the dominant leg, subjects were asked by the examiner #x2018;with which leg would you kick a ball’, which goes in line with other self-reported and observed assessments and was also applied in prior studies (Cavanaugh et al., 2017; van Melick et al., 2017). Then, the participants’ characteristics were collected with a questionnaire. After that, subjects were instructed on how to perform the Bunkie Test and received additional visual demonstration. The outcome variables (performance in the Bunkie Test of PPL and PSL) were measured before and immediately after the intervention for both legs, where the dominant leg was always tested first and the non-dominant leg second after a thirty-second break.
Intervention
The ten minute intervention was performed on the dominant leg only and consisted of self- and therapeutic SMM techniques. All techniques were supervised or conducted by a physical therapist following protocols described in prior studies (Ajimsha et al., 2014; Alotaibi et al., 2020; Grieve et al., 2015; Kwangsun et al., 2018; Stecco et al., 2016; Thong-On et al., 2019). The non-dominant leg received no intervention.
Self-massage and stretching
In the beginning, subjects performed four minutes of foam rolling at a self-selected speed on the plantar surface, along the course of the PF, using a small foam roller (diameter 5 cm) with a Young modulus of 80 MPa (Blackroll, CH). They were allowed to hold on to a wall and were instructed to adapt the intensity of pressure to their subjective tolerance level. Further, they were encouraged to continue foam rolling for the total of four minutes, but were additionally allowed to take short breaks if needed (Grieve et al., 2015; Kwangsun et al., 2018). This was followed by a plantar fascia specific stretch where subjects crossed the dominant leg over the other in a sitting position and stabilized the heel with their hand. Then, participants performed passive metatarsophalangeal joint dorsiflexion with the other hand for 2x30 seconds with a ten second pause in between (Figure 1) (Alotaibi et al., 2020).
Figure 1.
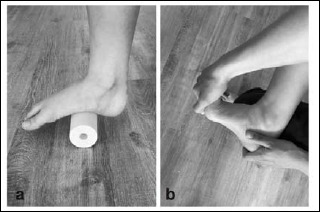
Techniques applied by the participant with (a) foam rolling and (b) a plantar fascia-specific stretch.
Manual massage
Participants were placed in a prone position on a treatment table with the feet placed on a positioning pillow to allow easy dorsiflexion of the ankle. The skin on the dominant foot was cleaned with a wet towel, freed from skincare applications, dried and disinfected. All manual techniques were adapted to subjects’ individual tolerance levels, not exceeding a maximum of seven out of ten, ranked on a numeric rating scale (Cavanaugh et al., 2017).
Soft tissue mobilization
The therapist contacted the PF with the knuckles or the thumb and applied pressure in a gliding movement along the fascia from the heel to the ball of the foot. This was repeated for 2x60 seconds with a ten-second pause in between. The same procedure was then performed adding passive flexion and extension of the toes. The therapist kept the movement speed constant with a rhythm of one second per stroke; thereby applying an average of 60 strokes on the plantar fascia (in a heel to ball direction) within 60 seconds. (Figure 2) (Ajimsha et al., 2014).
Figure 2.
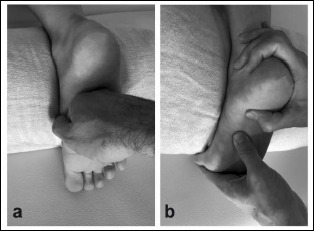
Therapeutic manual techniques with (a) soft tissue mobilisation and (b) gliding massage.
Gliding massage
The therapist applied hyper-dorsiflexion to the toes, mainly to the hallux, in order to stretch the medial band of the PF. Pressure was then applied with a reinforced index finger or the thumb along the PF from proximal to distal for two minutes (Figure 2). Similarly, the therapist attempted to maintain the speed in a one-second rhythm (Thong-On et al., 2019).
Direct deep friction and manual pressure
Direct deep, tangential, oscillation friction or sustained pressure (120 300s), comparable to manual trigger point therapy, was applied to the PF, focusing on areas with increased densification. This technique lasted for four minutes (Ajimsha et al., 2014; Stecco et al., 2016).
Measurement
We designed our study particularly for application of newly gained insights and techniques in everyday practice. Therefore, we decided to use the Bunkie Test to measure functional force generation in the SBL. The test is widely used among clinicians, although validity and reliability have not yet been sufficiently investigated (De Witt and Venter, 2009; Ronai, 2015). According to Van Pletzen and Venter (2012) the results of the Bunkie Test concerning the PPL and PSL are largely comparable to other physical performance tests, namely the 40 m sprint test, the repeated sprint test and the vertical jump test. Hence, the Bunkie Test can be proposed as a tool to identify weaknesses and imbalances in the kinetic chains. We conducted the test as described in the original protocol by De Witt and Venter (2009). Subjects placed their forearms on a mat with the shoulders right over the elbows and their heels on a bench with a height of 30 cm. They were instructed to continue constant breathing during the test. To assess the PPL, subjects had to lift up their pelvis to a neutral position and then raised the non-dominant leg about 20 cm off the bench in order to test the dominant leg. Time of performance was counted in seconds with a stopwatch from the moment the contralateral leg was lifted. The test was stopped when the subject either reported any sensation of pain or cramping, ended the test due to fatigue or reached the cut-off score of 40 seconds, which is seen as the optimum value for athletes. If participants were not able to maintain a neutral body position, they were verbally corrected once. The test was stopped if they were not able to adjust to or hold the neutral position. Then, the non-dominant leg was tested after a thirty-second break. After examining the PPL, subjects were allowed to rest for three minutes. The same testing procedure was then performed for the PSL, with the difference that the knees were flexed in a 90-degree-position and the hips adapted to this (Figure 3).
Figure 3.
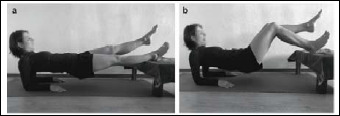
The Bunkie Test for (a) the posterior stabilizing line and (b) the posterior power line.
Statistical analysis
The freely available software environment for statistical computing R (version 3.5.1) (Team, 2018) was used for all statistical analysis. First, we tested for normal distribution with the Shapiro-Wilk test. For the normally distributed descriptive variables (age, height, weight) we calculated mean values and standard deviations (SD). A multilevel linear regression model for repeated measures was used for statistical testing, as this test considers dependency in data and does not require sphericity or normal distribution (Bauer et al., 2013; Woltman et al., 2012). We specified the factors for the time-effect (pre- and post-intervention) and the treatment-effect (dominant/intervention and non-dominant/control leg). First, we fitted four different regression models: (1) intercept-only-model, (2) with time as the predictor variable, (3) with treatment group and time as the predictor variables, and (4) with the main effects of both variables as well as their interaction term as predictors. The factors time and treatment were nested within the variable participant and specified as random. We compared the models using analysis of variance (ANOVA) and calculated confidence intervals (CI) and standard errors (SE) for the outcome variables of the total model (4). The same model was applied to the outcomes of PPL and PSL. A p-value of less than 0.05 was considered as statistically significant. There was no missing data.
Power calculations
The a-priori sample size calculation using G*Power (G*Power version 3.1., Heinrich-Heine-University Düsseldorf, Germany) was based on the effect sizes of the first studies in the field from Wilke et al. (2020a) (d = 2.16) and Cruz-Montecinos et al. (2015) (r = 0.449). According to Sawilowsky (2009) and Cohen (2013), these effect sizes can be seen as a huge (2.0) effect for Cohen’s d and a large (0.5) effect for the correlation coefficient. Therefore, we considered a large effect size using Cohen’s d (d = 0.8) with α = 0.05 and β = 0.8. This resulted in a sample size of 15 people. With an add up of ten percent to meet unforeseen events, our final sample consisted of 17 participants.
Results
All participants reported the right leg as their dominant leg. There were no adverse events or unintended side effects. The performance of the dominant leg in the Bunkie Test (in seconds) respectively decreased by 17.2% (PPL) and 16.3% (PSL) between pre (mean ± SD: PPL: 33.1 ± 9.9; PSL: 27.6 ± 9.8) and post measurement (mean ± sd: PPL: 27.4 ± 11.1; PSL: 23.1 ± 11.7). Contrary, the non-dominant leg showed an increase by 5.1% (PPL) and 3.1% (PSL) from pre (mean ± SD: PPL: 29.7 ± 9.6, PSL: 25.7 ± 1.5) to post intervention (mean ± SD: PPL: 31.1 ± 8.9, PSL: 26.5 ± 1.7).
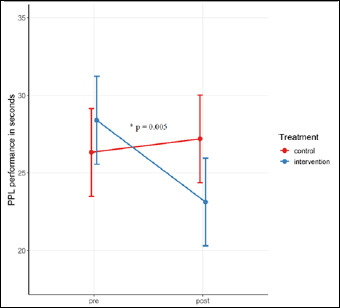
The comparison of the four different linear models with (1) only the intercept, (2) time as predictor variable, (3) treatment group and time as predictor variables, and (4) the main effects of both variables as well as their interaction revealed that the type of treatment alone had no significant overall main effect on the performance in PPL (χ2 = 0.006, p = 0.938) and in PSL (χ2 = 0.468, p = 0.494). There was also no significant overall main effect for the factor time on performance in PPL (χ2 = 2.389, p = 0.122) and PSL (χ2 = 3.238, p = 0.072). Yet, the interaction effect between time and treatment was significant for PPL (χ2 = 8.000, p = 0.005) as well as for PSL (χ2 = 7.751, p = 0.005). The total linear model (4) showed an interaction effect, meaning that the effect of time after the intervention depended on the type of treatment (PPL: p = 0.007; PSL: p = 0.007). The results for the total linear model are listed in Table 1. We observed a crossover interaction between both legs for the performance in PPL (Figure 4) and PSL (Figure 5).
Table 1.
Results of the total linear regression model, including the variables treatment (intervention/control) and time (pre/post).
| b | p | SE b | 95% CI | |
|---|---|---|---|---|
| Posterior Power Line (PPL) | ||||
| Treatment control | -3.412 | 0.095 | 1.919 | -7.359, 0.536 |
| Time post | -5.235 | 0.003* | 1.599 | -8.395, -2.075 |
| Treatment control x Time post | 6.588 | 0.007* | 2.261 | 2.120, 11.057 |
| Posterior Stabilizing Line (PSL) | ||||
| Treatment control | -1.941 | 0.176 | 1.370 | -4.758, 0.876 |
| Time post | -4.471 | 0.002* | 1.309 | -7.058, -1.883 |
| Treatment control x Time post | 5.294 | 0.007* | 1.852 | 1.635, 8.953 |
*Indicates a statistically significant effect.
Figure 4.
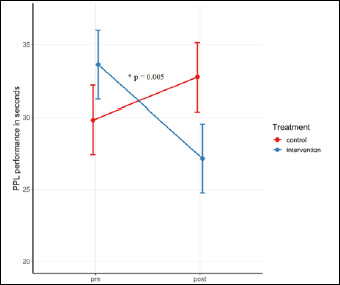
Effect of treatment and time on performance in Bunkie Test for the posterior power line (PPL) (mean ± SE). * indicating a statistically significant effect (p = 0.005).
Figure 5.
Effect of treatment and time on performance in Bunkie Test for the posterior stabilizing line (PSL) (mean ± SE). * indicating a statistically significant effect (p = 0.005).
Discussion
Our results showed a significant reduction of performance in the treated leg after various SMM techniques (foam rolling, plantar fascia specific stretching, soft tissue mobilization, gliding massage, direct deep friction and manual pressure). Interestingly, an improvement of performance was observed in the contralateral leg. Furthermore, the interaction between time and treatment was significant. This means that the impact that one factor, for example time, had on the outcome depended on the level of the other factor, in this case treatment group, and vice versa. Yet, the main effects of these factors were not significant, which can be explained by the observed crossover interaction effect. Therefore, we can reject our null hypothesis.
Strain, tension and force transmission in fascial chains
Our study was one of the first to test the influence of SMM on performance in myofascial chains in a practical setting. In contrast, the change of flexibility along fascial chains after foam rolling has already been investigated via functional measurements. A reason for this might be that several tools and treatment concepts in the fitness and rehabilitation sector are specifically promoted for the practice of ‘loosening tissue’. Yet, the studies showing a change of tensional state along the SBL did not consider the potential side-effect of a decreased performance in terms of force generation (Grieve et al., 2015; Kwangsun et al., 2018). Our results indicate that SMM on the plantar surfaces’ structures could influence strength in non-adjacent areas.
Myofascial force transmission can be present between muscle fibers, between muscles or between muscles and the relating non-muscular tissues. The concept of myofascial force transmission lines received increasing scientific attention as a potential explanation of the fact that tension produced in one area affects body structures non-adjacent to it (Do Carmo Carvalhais et al., 2013). Prior studies have shown, for example, that ankle position and passive torque influence hip mobility and vice versa (Andrade et al., 2016; Marinho et al., 2017; Palmer et al., 2015). Wilke et al. (2020a) applied this concept of changing tensional states in non-adjacent areas of the lower extremity to the SBL. They tested tissue displacement in the hamstrings region after passive ankle dorsiflexion. All these findings suggested force transmission via myofascial pathways in the lower extremity, but more in terms of strain and less in terms of active force generation. Unlike, Do Carmo Carvalhais et al. (2013) showed that passive or active tension of the latissimus dorsi muscle modified the joint kinetic variables of the contralateral hip due to the functional connectivity via the thoracolumbar fascia. Still, there is a need for in-vivo studies regarding myofascial force transmission along the SBL (Wilke et al., 2020a). Besides the evidence that this effect can be seen along a myofascial line, there is evidence that especially stretching exercises are capable of increasing range of motion (Behm et al., 2021a) and decreasing strength parameters (Behm et al., 2021b) in the contra-lateral leg as well as in other non-stretched joints and muscles. The authors of these studies assume that this is due to a non-local (global) changed stretch perception.
A decrease in performance after the SMM intervention
Our study showed that performance in the Bunkie Test decreased after the SMM. Prior literature concerning the effect of SMM, usually foam rolling, on muscle function or athletic performance shows inconsistent results. Yet, most of the studies report no significant effect or a rather positive effect of SMM on isometric muscle force or performance tests, like the vertical jump or the 800-meter run test. There might be no general consensus due to the strong heterogeneity of the study designs, outcome measurements and intervention parameters as well as the difficulties that occur for choosing appropriate measurement techniques (Behara and Jacobson, 2017; Cheatham et al., 2015; Healey et al., 2014; Hughes and Ramer, 2019; Monteiro et al., 2017; Sullivan et al., 2013; Wiewelhove et al., 2019).
Techniques, which aim at decreasing the tensional state of a muscle, like massaging or prolonged stretching (for >60 s and without a preparatory dynamic warm-up), usually go along with a decline in muscle force (Behm et al., 2016; Behm et al., 2020b; Hunter et al., 2006; Konrad et al., 2019; Konrad and Tilp, 2020; Morelli et al., 1999; Sullivan et al., 1991). Some researchers also report this effect for SMM, like Monteiro et al. (2017) who found out that foam rolling on the quadriceps muscle between the sets of force training, led to a decreased maximum repetition performance. Contrarily, MacDonald et al. (2013) reported that a two-minute bout of foam rolling on the quadriceps muscle led to an increase in range of motion of the knee, but did not influence neuromuscular force production in the treated area. In a study by Cavanaugh et al. (2017) it was shown that three repetitions of a 30-second self-massage caused impairments of maximal voluntary isometric contractions, but did not influence other force parameters, like the time to peak twitch torque. These conflicting results suggest that the effect of SMM on force partly depends on the study design, the chosen SMM technique, the outcome measurement and indicate that there might be a dose-response relationship. In this study we applied a combination of different SMM techniques, like foam rolling, stretching and massage techniques. Further, SMM may only have a neutral effect on subsequent muscular force when applied for a shorter duration, like most of the studies describe interventions ranging from 30 seconds to three minutes (Cheatham et al., 2015; Hughes and Ramer, 2019; MacDonald et al., 2013; Sullivan et al., 2013). Contrarily, in our study SMM was applied for an average of ten minutes. These factors might explain our contradicting results to the study from Sullivan et al. (2013) who reported that a three-minute massage of the plantar flexors did not influence jump power, maximal voluntary muscle contraction, force or muscle activation. Further, the Bunkie Test was specifically developed for evaluating the fascial chains. In contrast, most of the measurement techniques in other studies have tested muscle performance of muscle groups or general athletic performance. Additionally, Behm et al. (2021b) reported a moderate non-local muscle fatigue effect in endurance tasks, which might also be caused by muscle groups not directly involved in the fatiguing task. Nevertheless, we would then have expected to see this effect on both sides, as both legs were tested.
To understand the reduction of performance after the MFR in our study, we considered several underlying theories and models, including mechanical, physiological, psychophysiological and neurophysiological parameters (Aboodarda et al., 2015; Chaudhry et al., 2008; MacDonald et al., 2013; Monteiro et al., 2017; Schleip, 2003a; Stecco et al., 2016; Wiewelhove et al., 2019; Yoshimura et al., 2019).
The mechanical model explains the reduction of performance via the softening of fascia, and more likely its connected muscle. Although, reduced muscle stiffness following myofascial release was previously reported in the quadriceps muscle (Baumgart et al., 2019; Reiner et al., 2021), this was not seen in the plantar flexor muscles (Baumgart et al., 2019; Nakamura et al., 2021). Since a decrease in muscle stiffness has a negative impact on force production (Monte and Zignoli, 2021; Trajano et al., 2019) a decreased muscle stiffness might have occurred in the SBL of the participants tested in our study. Furthermore, another effect might be a reduced tissue adhesion or a change in the thixotropic property. This implies that via heat and mechanical stress, which is generated by applying techniques for more than two minutes, fascia’s colloidal substances can change from a solid state to a more gel-like state, which leads to increased soft-tissue compliance and flexibility (Aboodarda et al., 2015; Cheatham et al., 2015; Schleip, 2003a; Sullivan et al., 2013). This might also explain the dose-response relationship of SMM and its effect on muscle force.
From the physiological point of view, performance could be modified via altered hyaluronan and blood flow in or around fascia, which enhances blood lactate removal and oxygen delivery to the muscle. These effects result from a modification of the extracellular matrix of the intrafascial loose connective tissue layers through deep, tangential, oscillating frictions (Cheatham et al., 2015; Wiewelhove et al., 2019). A specific fascia treatment concept is based on the hypothesis that these alterations in fascia, caused by frictions, affect muscle spindle and Golgi tendon organ activity. This treatment concept is also applied with the goal of influencing areas non-adjacent to the treated structure via fascial pathways (Stecco et al., 2016).
A psychophysiological response might include an increase in subjective well-being and relaxation due to an increase of plasma endorphins, a decreased state of arousal or a potential placebo effect, which all could have led to the decrease in performance (Wiewelhove et al., 2019).
Until now there has been no sufficient evidence for these models explaining the effect of SMM. Therefore, neurophysiological mechanisms seem to be the most plausible theory to explain our results (Chaudhry et al., 2008; Schleip, 2003b).
An increase in performance without the SMM intervention
While a decrease in performance was observed for the intervention leg, the control leg showed the opposite. We hypothesize that the increase in performance of the control side was due to a training effect, as the test was performed twice, with a time interval of ten minutes. Prior studies addressed this issue by providing an organized familiarization with the performance test antecedent to the testing session (Wiewelhove et al., 2019). Previous studies reported reactions to SMM, namely an increase in range of motion and pain pressure threshold, not only in the treated area but also on the contralateral body side (Aboodarda et al., 2015; Yoshimura et al., 2019). Yoshimura et al. (2019) also reported that the treatment of the triceps surae led not only to an increased dorsal extension, but surprisingly also to a wider range of motion in plantar flexion. To explain this phenomenon of a generalized effect of SMM the authors mention neurophysiological mechanisms as the most plausible explanation.
According to Schleip (2003a), deep slow or steady manual pressure and tension stimulates interstitial and Ruffini mechanoreceptors within connective tissue. This leads to a general response of the autonomic nervous system, which results in an enhanced parasympathetic state and a lower sympathetic activity. This influences local fluid dynamics, tissue metabolism and viscosity, the general state of arousal and the tonus of motor units that are mechanically linked to the treated tissue (Aboodarda et al., 2015; Schleip, 2003a; Stecco et al., 2016; Wilke et al., 2020b; Yoshimura et al., 2019). The modulation of the central nervous system, specifically the central-pain modulatory system might also explain the increase of the pain pressure thresholds on both body sides reported in the study from Aboodarda et al. (2015).
A stimulation of the sensory receptors might lead to neurological modulation, also called the crossover effect, which can be explained by a suppression of the H-reflex (Sullivan et al., 2013; Yoshimura et al., 2019). A decreased spinal motor neuron excitability after a massage or SMM leads to a reduction in motor unit recruitment, and firing rate, which is linked to a decline in force (Hunter et al., 2006; Morelli et al., 1999; Sullivan et al., 1991; Wilke et al., 2020b). In our study the segmental innervation of muscles in the treated area, for example flexor digitorum brevis, flexor interossei dorsalis, plantaris or quadratus plantae, coincide with the segmental innervation of the muscles mainly activated during the Bunkie Test, namely the hamstrings and the gastrocnemius (Schünke et al., 2005). Therefore, neurophysiological mechanisms also might have had an influence, via the motor unit excitability.
Further, we hypothesize that in our study the described modification of neurophysiological mechanisms, which might have affected both body sides, was offset by the training effect. This in fact strengthens our results, as otherwise the training effect should have been observed on the dominant leg, too.
Strengths and limitations
In general, non-randomized controlled studies are more susceptible to bias and within-subject comparison is less common in orthopedic studies. To ensure quality of reporting we conscientiously stuck to the reporting guidelines, which were extended versions of the CONSORT guideline. However, our rather unusual study design allowed us to observe the interesting crossover interaction effect (Pandis et al., 2019; Reeves and Gaus, 2004). A potential non-local muscle fatigue effect due to the Bunkie Test itself, leading to the observed crossover-effect, is rather unlikely to be influenced by the chosen study design (between versus within-participant) (Behm et al., 2021b).
A limitation of our study is that our intervention depended on individual tolerance levels and personal susceptibilities. We addressed this by only applying techniques, which were already investigated in prior studies according to the reported protocols. These techniques are commonly used, for example in the treatment of plantar fasciitis, and are therefore important for therapists’ daily practice (Fraser et al., 2018). In addition, all treatments were supervised or conducted by the same physical therapist. It should be considered that according to Chaudhry et al. (2008), a plastic deformation of the PF via SMM is not very likely within physiological force ranges in a dead piece of tissue. The authors also suggest, that in alive tissues a long-lasting deformation might be possible due to additional neurophysiological effects, which might influence the response in vivo. We clearly state that we did not intend to influence the mechanical state of the fascia (Behm and Wilke, 2019). Behm and Wilke (2019) also state, that the commonly used term ‘self-myofascial release’ is therefore misleading. The possible underlying theories of the effect of SMM in alive tissues have been discussed above.
We are aware that the validity and reliability of the Bunkie Test have not been sufficiently investigated, yet. However, it is similar to the single leg bridge test, which is reliable and was applied in prior studies (Freckleton et al., 2014; Hallet, 2010). An advantage is that the Bunkie Test is based on the theory of fascial chains (Myers, 2013) and therefore fits our aim of testing the SBL. Furthermore, the PF remains unloaded during the test. It must be considered that crossover effects from either stretching or rolling to the contralateral limb, as reported in prior studies (Aboodarda et al., 2015; Cavanaugh et al., 2017) might have influenced our results and were not detected with this testing procedure. Concerning the test, we want to highlight that, as the test does not aim at testing the maximum strength endurance capacity and hence, likely causes no muscle fatigue, we expect that there was no or even a small crossover effect resulting from the testing procedure. We recommend future studies to include an additional control group, which receives no intervention on the contralateral leg. It should also be considered that a recent study suggested to prefer a resting interval of 1 minute before testing the contralateral leg (O’Neill et al., 2020). Further, the objectivity of the Bunkie Test is rather low as performance is measured in seconds via a stopwatch and partly depends on the participants’ decision. Nevertheless, there were such vast differences between before- and after-values that this can be considered as negligible. In addition, we expected the participants to choose their point of fatigue similar to the first measurement trial, as they were blinded concerning the expected outcome and the aim of the study. In contrast, the experimenter was not blinded in this study.
Recommendations
Our findings suggest that SMM interventions might result in a decreased force transmission and therefore performance in the SBL. This could be of relevance to the field of sports where self-massage is often applied before physical exertion although a large body of evidence already recommended the utilization of foam rolling after the exercise instead of pre-rolling (Cheatham et al., 2015; Wiewelhove et al., 2019). To overcome a possible detrimental effect on performance, especially following stretching exercises, it is suggested to implement post stretching activities, which likely results in a post stretching potentiation effect (Behm et al., 2016; Reid et al., 2018; Reiner et al., 2021; Samson et al., 2012). In addition, therapists should consider this possibly unwanted side-effect when applying SMM. Our findings highlight the importance of applied studies in this field of research in order to develop reliable recommendations for the practical application of self- or therapeutic fascial techniques. Yet, the underlying theories of SMM should be further investigated.
We proposed a within-subject design for a holistic investigation of the fascial system, which could be considered by future studies. In addition, the inconsistent results concerning the effect of SMM on muscle force or athletic performance highlight the importance of uniform, valid and reliable measurement methods. We introduced the Bunkie Test as a quick and easy method to examine the integrity and functionality of the SBL. Still, the validity and reliability of this test should be further assessed.
Conclusion
The combination of self- and therapeutic massage techniques on the plantar surface applied in our study might reduce performance in terms of force generation along the SBL. Our hypothesis is supported by the fact that the PF itself was not loaded during the functional performance test and that the opposite effect was observed on the control side. As we applied a combination of different SMM techniques, it should be considered that some techniques, like foam rolling, might had no effect, while others, like stretching, had a negative effect. We hope that our results contribute to the body of knowledge regarding practical application of fascial techniques.
Acknowledgements
We would like to thank Andrea Gabriel for support with the graphic representation. Our thanks also go to the subjects for participating in our study. The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare. The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author who was an organizer of the study.
Biographies

Anna GABRIEL
Employment
Professorship of Conservative and rehabilitative Orthopedics, Technical University of Munich.
Degree
MSc
Research interests
Physical therapy, orthopedics, myofascial chains, assessment in therapy
E-mail: anna-gabriel@tum.de

Andreas KONRAD
Employment
Institute of Human Movement Science, Sport and Health, University of Graz.
Degree
MSc, PhD, PD
Research interests
Biomechanics, muscle performance, training science, muscle-tendon-unit, soccer science
E-mail: andreas.konrad@uni-graz.at

Anna ROIDL
Employment
Department of Neonatology, University Children’s Hospital Regensburg (KUNO), Hospital St. Hedwig of the Order of St. John, University of Regensburg.
Degree
MSc
Research interests
Physical therapy, myofascial release, behavior change counselling, neurodevelopment, neonatology
E-mail: Anna.Roidl@barmherzige-regensburg.de

Jennifer QUEISSER
Employment
Professorship of Conservative and Rehabilitative Orthopedics, Technical University of Munich.
Degree
M.Ed.
Research interests
Physical therapy, sensorimotor training, diagnostics in therapy
E-mail: jennifer.queisser@tum.de
Robert SCHLEIP
Employment
Professorship for Conservative and Rehabilitative Orthopedics, Technical University of Munich; Diploma University of Applied Sciences, Bad Sooden-Allendorf; Department of Sports Medicine and Health Promotion, Friedrich Schiller University Jena.
Degree
Dr. biol.hum.; Dipl.Psych.
Research interests
Fascia, myofascial force transmission, manual therapy
E-mail: robert.schleip@tum.de

Thomas HORSTMANNA
Employment
Professorship of Conservative and Rehabilitative Orthopedics, Technical University of Munich.
Degree
MD
Research interests
Orthopedic surgery, sports medicine, rehabilitation medicine
E-mail: t.horstmann@tum.de

Torsten POHL
Employment
Professorship of Conservative and Rehabilitative Orthopedics, Technical University of Munich.
Degree
MSc
Research interests
Sensorimotor training, dynamic balance control, sports therapy
E-mail: torsten.pohl@tum.de
References
- Aboodarda S., Spence A., Button D.C. (2015) Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BioMed Central Musculoskeletal Disorders 16, 1-10. https://doi.org/10.1186/s12891-015-0729-5 10.1186/s12891-015-0729-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adstrum S., Hedley G., Schleip R., Stecco C., Yucesoy C.A. (2017) Defining the fascial system. Journal of Bodywork and Movement Therapies 21, 173-177. https://doi.org/10.1016/j.jbmt.2016.11.003 10.1016/j.jbmt.2016.11.003 [DOI] [PubMed] [Google Scholar]
- Ajimsha M., Binsu D., Chithra S. (2014) Effectiveness of myofascial release in the management of plantar heel pain: a randomized controlled trial. The Foot 24, 66-71. https://doi.org/10.1016/j.foot.2014.03.005 10.1016/j.foot.2014.03.005 [DOI] [PubMed] [Google Scholar]
- Alotaibi A., Petrofsky J., Daher N.S., Lohman E., Syed H.M., Lee H. (2020) The Effect of Monophasic Pulsed Current with Stretching Exercise on the Heel Pain and Plantar Fascia Thickness in Plantar Fasciitis: A Randomized Controlled Trial. Healthcare 8, 79. https://doi.org/10.3390/healthcare8020079 10.3390/healthcare8020079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade R.J., Lacourpaille L., Freitas S., McNair P., Nordez A. (2016) Effects of hip and head position on ankle range of motion, ankle passive torque, and passive gastrocnemius tension. Scandinavian Journal of Medicine & Science in Sports 26, 41-47. https://doi.org/10.1111/sms.12406 10.1111/sms.12406 [DOI] [PubMed] [Google Scholar]
- Bauer D.J., Gottfredson N.C., Dean D., Zucker R.A. (2013) Analyzing repeated measures data on individuals nested within groups: accounting for dynamic group effects. Psychological Methods 18, 1. https://doi.org/10.1037/a0030639 10.1037/a0030639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgart C., Freiwald J., Kühnemann M., Hotfiel T., Hüttel M., Hoppe M.W. (2019) Foam rolling of the calf and anterior thigh: biomechanical Loads and acute effects on vertical jump height and muscle stiffness. Sports 7, 27. https://doi.org/10.3390/sports7010027 10.3390/sports7010027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behara B., Jacobson B.H. (2017) Acute effects of deep tissue foam rolling and dynamic stretching on muscular strength, power, and flexibility in division I linemen. The Journal of Strength & Conditioning Research 31, 888-892. https://doi.org/10.1519/JSC.0000000000001051 10.1519/JSC.0000000000001051 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Alizadeh S., Anvar S.H., Drury B., Granacher U., Moran J. (2021a) Non-local acute passive stretching effects on range of motion in healthy adults: a systematic review with meta-analysis. Sports Medicine 51, 945-959. https://doi.org/10.1007/s40279-020-01422-5 10.1007/s40279-020-01422-5 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Alizadeh S., Anvar S.H., Hanlon C., Ramsay E., Mahmoud M.M.I., Whitten J., Fisher J.P., Prieske O., Chaabene H. (2021b) Non-local Muscle Fatigue Effects on Muscle Strength, Power, and Endurance in Healthy Individuals: A Systematic Review with Meta-analysis. Sports Medicine 51(9), 1893-1907. https://doi.org/10.31236/osf.io/w7x3v 10.31236/osf.io/w7x3v [DOI] [PubMed] [Google Scholar]
- Behm D.G., Alizadeh S., Anvar S.H., Mahmoud M.M.I., Ramsay E., Hanlon C., Cheatham S. (2020a) Foam rolling prescription: A clinical commentary. The Journal of Strength & Conditioning Research 34, 3301-3308. https://doi.org/10.1519/JSC.0000000000003765 10.1519/JSC.0000000000003765 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Blazevich A.J., Kay A.D., McHugh M. (2016) Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Applied Physiology, Nutrition, and Metabolism 41, 1-11. https://doi.org/10.1139/apnm-2015-0235 10.1139/apnm-2015-0235 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Kay A.D., Trajano G.S., Blazevich A.J. (2020b) Mechanisms underlying performance impairments following prolonged static stretching without a comprehensive warm-up. European Journal of Applied Physiology 121, 67-94. https://doi.org/10.1007/s00421-020-04538-8 10.1007/s00421-020-04538-8 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Wilke J. (2019) Do self-myofascial release devices release myofascia? Rolling mechanisms: a narrative review. Sports Medicine 49, 1173-1181. https://doi.org/10.1007/s40279-019-01149-y 10.1007/s40279-019-01149-y [DOI] [PubMed] [Google Scholar]
- Carnes D., Mars T.S., Mullinger B., Froud R., Underwood M. (2010) Adverse events and manual therapy: a systematic review. Manual Therapy 15, 355-363. https://doi.org/10.1016/j.math.2009.02.003 10.1016/j.math.2009.02.003 [DOI] [PubMed] [Google Scholar]
- Cavanaugh M.T., Döweling A., Young J.D., Quigley P.J., Hodgson D.D., Whitten J.H., Reid J.C., Aboodarda S.J., Behm D.G. (2017) An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. European Journal of Applied Physiology 117, 109-117. https://doi.org/10.1007/s00421-016-3503-y 10.1007/s00421-016-3503-y [DOI] [PubMed] [Google Scholar]
- Chaudhry H., Schleip R., Ji Z., Bukiet B., Maney M., Findley T. (2008) Three-dimensional mathematical model for deformation of human fasciae in manual therapy. Journal of Osteopathic Medicine 108, 379-390. https://doi.org/10.7556/jaoa.2008.108.8.379 10.7556/jaoa.2008.108.8.379 [DOI] [PubMed] [Google Scholar]
- Cheatham S.W., Kolber M.J., Cain M., Lee M. (2015) The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. International Journal of Sports Physical Therapy 10, 827. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (2013) Statistical power analysis for the behavioral sciences. Academic press. https://doi.org/10.4324/9780203771587 10.4324/9780203771587 [DOI] [Google Scholar]
- Cruz-Montecinos C., González Blanche A., López Sánchez D., Cerda M., Sanzana-Cuche R., Cuesta-Vargas A. (2015) In vivo relationship between pelvis motion and deep fascia displacement of the medial gastrocnemius: anatomical and functional implications. Journal of Anatomy 227, 665-672. https://doi.org/10.1111/joa.12370 10.1111/joa.12370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Witt B., Venter R. (2009) The ‘Bunkie’test: assessing functional strength to restore function through fascia manipulation. Journal of Bodywork and Movement Therapies 13, 81-88. https://doi.org/10.1016/j.jbmt.2008.04.035 10.1016/j.jbmt.2008.04.035 [DOI] [PubMed] [Google Scholar]
- Do Carmo Carvalhais V.O., De Melo Ocarino J., Araújo V.L., Souza T.R., Silva P.L.P., Fonseca S.T. (2013) Myofascial force transmission between the latissimus dorsi and gluteus maximus muscles: an in vivo experiment. Journal of Biomechanics 46, 1003-1007. https://doi.org/10.1016/j.jbiomech.2012.11.044 10.1016/j.jbiomech.2012.11.044 [DOI] [PubMed] [Google Scholar]
- Fraser J.J., Corbett R., Donner C., Hertel J. (2018) Does manual therapy improve pain and function in patients with plantar fasciitis? A systematic review. Journal of Manual & Manipulative Therapy 26, 55-65. https://doi.org/10.1080/10669817.2017.1322736 10.1080/10669817.2017.1322736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freckleton G., Cook J., Pizzari T. (2014) The predictive validity of a single leg bridge test for hamstring injuries in Australian Rules Football Players. British Journal of Sports Medicine 48, 713-717. https://doi.org/10.1136/bjsports-2013-092356 10.1136/bjsports-2013-092356 [DOI] [PubMed] [Google Scholar]
- Grieve R., Goodwin F., Alfaki M., Bourton A.-J., Jeffries C., Scott H. (2015) The immediate effect of bilateral self myofascial release on the plantar surface of the feet on hamstring and lumbar spine flexibility: A pilot randomised controlled trial. Journal of Bodywork and Movement Therapies 19, 544-552. https://doi.org/10.1016/j.jbmt.2014.12.004 10.1016/j.jbmt.2014.12.004 [DOI] [PubMed] [Google Scholar]
- Hallet P. (2010) A reliability study examining the inter-and intra-observer reliability of the muscle capacity tests included in the ECB musculoskeletal screening protocol. University of Nottingham. [Google Scholar]
- Healey K.C., Hatfield D.L., Blanpied P., Dorfman L.R., Riebe D. (2014) The effects of myofascial release with foam rolling on performance. The Journal of Strength & Conditioning Research 28, 61-68. https://doi.org/10.1519/JSC.0b013e3182956569 10.1519/JSC.0b013e3182956569 [DOI] [PubMed] [Google Scholar]
- Hughes G.A., Ramer L.M. (2019) Duration of myofascial rolling for optimal recovery, range of motion, and performance: a systematic review of the literature. International Journal of Sports Physical Therapy 14, 845. https://doi.org/10.26603/ijspt20190845 10.26603/ijspt20190845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter A., Watt J.M., Watt V., Galloway S. (2006) Effect of lower limb massage on electromyography and force production of the knee extensors. British Journal of Sports Medicine 40, 114-118. https://doi.org/10.1136/bjsm.2005.019075 10.1136/bjsm.2005.019075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Reiner M., Thaller S., Tilp M. (2019) The time course of muscle-tendon properties and function responses of a five- minute static stretching exercise. European Journal of Sport Science 19, 1195-1203. https://doi.org/10.1080/17461391.2019.1580319 10.1080/17461391.2019.1580319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Tilp M. (2020) The time course of muscle-tendon unit function and structure following three minutes of static stretching. Journal of Sports Science & Medicine 19, 52-58. https://pubmed.ncbi.nlm.nih.gov/32132827/ [PMC free article] [PubMed] [Google Scholar]
- Krause F., Wilke J., Vogt L., Banzer W. (2016) Intermuscular force transmission along myofascial chains: a systematic review. Journal of Anatomy 228, 910-918. https://doi.org/10.1111/joa.12464 10.1111/joa.12464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwangsun D., Jaeeun K., Jongeun Y. (2018) Acute effect of self-myofascial release using a foam roller on the plantar fascia on hamstring and lumbar spine superficial back line flexibility. Physical Therapy Rehabilitation Science 7, 35-40. https://doi.org/10.14474/ptrs.2018.7.1.35 10.14474/ptrs.2018.7.1.35 [DOI] [Google Scholar]
- MacDonald G.Z., Penney M.D., Mullaley M.E., Cuconato A.L., Drake C.D., Behm D.G., Button D.C. (2013) An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. The Journal of Strength & Conditioning Research 27, 812-821. https://doi.org/10.1519/JSC.0b013e31825c2bc1 10.1519/JSC.0b013e31825c2bc1 [DOI] [PubMed] [Google Scholar]
- Marinho H.V.R., Amaral G.M., Moreira B.S., Santos T.R.T., Magalhães F.A., Souza T.R., Fonseca S.T. (2017) Myofascial force transmission in the lower limb: An in vivo experiment. Journal of Biomechanics 63, 55-60. https://doi.org/10.1016/j.jbiomech.2017.07.026 10.1016/j.jbiomech.2017.07.026 [DOI] [PubMed] [Google Scholar]
- Monte A., Zignoli A. (2021) Muscle and tendon stiffness and belly gearing positively correlate with rate of torque development during explosive fixed end contractions. Journal of Biomechanics 114, 110110. https://doi.org/10.1016/j.jbiomech.2020.110110 10.1016/j.jbiomech.2020.110110 [DOI] [PubMed] [Google Scholar]
- Monteiro E.R., Vigotsky A., Škarabot J., Brown A.F., de Melo Fiuza A.G.F., Gomes T.M., Halperin I., da Silva Novaes J. (2017) Acute effects of different foam rolling volumes in the interset rest period on maximum repetition performance. Hong Kong Physiotherapy Journal 36, 57-62. https://doi.org/10.1016/j.hkpj.2017.03.001 10.1016/j.hkpj.2017.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelli M., Chapman C., Sullivan S. (1999) Do cutaneous receptors contribute to the changes in the amplitude of the H-reflex during massage? Electromyography and Clinical Neurophysiology 39, 441-447. [PubMed] [Google Scholar]
- Myers T.W. (2013) Anatomy trains e-book: myofascial meridians for manual and movement therapists. Elsevier Health Sciences. [Google Scholar]
- Nakamura M., Onuma R., Kiyono R., Yasaka K., Sato S., Yahata K., Fukaya T., Konrad A. (2021) The Acute and Prolonged Effects of Different Durations of Foam Rolling on Range of Motion, Muscle Stiffness, and Muscle Strength. Journal of Sports Science & Medicine 20, 62-68. https://doi.org/10.52082/jssm.2021.62 10.52082/jssm.2021.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill E., Tamjid N., DeRevere J., Kostelis K. (2020) Assessment and application of the Bunkie test in college students. Journal of Bodywork and Movement Therapies 24, 165-169. https://doi.org/10.1016/j.jbmt.2019.10.006 10.1016/j.jbmt.2019.10.006 [DOI] [PubMed] [Google Scholar]
- Palmer T.B., Akehi K., Thiele R.M., Smith D.B., Warren A.J., Thompson B.J. (2015) Dorsiflexion, plantar-flexion, and neutral ankle positions during passive resistance assessments of the posterior hip and thigh muscles. Journal of Athletic Training 50, 467-474. https://doi.org/10.4085/1062-6050-49.6.04 10.4085/1062-6050-49.6.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandis N., Chung B., Scherer R., Elbourne D., Altman D. (2019) Consort 2010 statement: extension checklist for reporting within person randomised trials. British Journal of Dermatology 180, 534-552. https://doi.org/10.1111/bjd.17239 10.1111/bjd.17239 [DOI] [PubMed] [Google Scholar]
- Reeves B., Gaus W. (2004) Guidelines for reporting non-randomised studies. Complementary Medicine Research 11, 46-52. https://doi.org/10.1159/000080576 10.1159/000080576 [DOI] [PubMed] [Google Scholar]
- Reid J.C., Greene R., Young J.D., Hodgson D.D., Blazevich A.J., Behm D.G. (2018) The effects of different durations of static stretching within a comprehensive warm-up on voluntary and evoked contractile properties. European Journal of Applied Physiology 118, 1427-1445. https://doi.org/10.1007/s00421-018-3874-3 10.1007/s00421-018-3874-3 [DOI] [PubMed] [Google Scholar]
- Reiner M.M., Glashüttner C., Bernsteiner D., Tilp M., Guilhem G., Morales-Artacho A., Konrad A. (2021) A comparison of foam rolling and vibration foam rolling on the quadriceps muscle function and mechanical properties. European Journal of Applied Physiology 121, 1461-1471. https://doi.org/10.1007/s00421-021-04619-2 10.1007/s00421-021-04619-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronai P. (2015) The bunkie test. Strength & Conditioning Journal 37 89-92. https://doi.org/10.1519/SSC.0000000000000126 10.1519/SSC.0000000000000126 [DOI] [Google Scholar]
- Samson M., Button D.C., Chaouachi A., Behm D.G. (2012) Effects of dynamic and static stretching within general and activity specific warm-up protocols. Journal of Sports Science & Medicine 11, 279-285. https://pubmed.ncbi.nlm.nih.gov/24149201/ [PMC free article] [PubMed] [Google Scholar]
- Sawilowsky S.S. (2009) New effect size rules of thumb. Journal of Modern Applied Statistical Methods 8, 26. https://doi.org/10.22237/jmasm/1257035100 10.22237/jmasm/1257035100 [DOI] [Google Scholar]
- Schleip R. (2003a) Fascial plasticity–a new neurobiological explanation Part 2. Journal of Bodywork and Movement Therapies 7, 104-116. https://doi.org/10.1016/S1360-8592(02)00076-1 10.1016/S1360-8592(02)00076-1 [DOI] [Google Scholar]
- Schleip R. (2003b) Fascial plasticity–a new neurobiological explanation: Part 1. Journal of Bodywork and Movement Therapies 7, 11-19. https://doi.org/10.1016/S1360-8592(02)00067-0 10.1016/S1360-8592(02)00067-0 [DOI] [Google Scholar]
- Schünke M., Schulte E., Schumacher U., Voll M., Wesker K. (2005) Prometheus: Allgemeine Anatomie und Bewegungssystem. LernAtlas der Anatomie. Stuttgart: Thieme. [Google Scholar]
- Stecco A., Stern R., Fantoni I., De Caro R., Stecco C. (2016) Fascial disorders: implications for treatment. American Academy of Physical Medicine and Rehabilitation 8, 161-168. https://doi.org/10.1016/j.pmrj.2015.06.006 10.1016/j.pmrj.2015.06.006 [DOI] [PubMed] [Google Scholar]
- Stecco C., Adstrum S., Hedley G., Schleip R., Yucesoy C.A. (2018) Update on fascial nomenclature. Journal of Bodywork and Movement Therapies 22, 354. https://doi.org/10.1016/j.jbmt.2017.12.015 10.1016/j.jbmt.2017.12.015 [DOI] [PubMed] [Google Scholar]
- Stecco C., Pirri C., Fede C., Fan C., Giordani F., Stecco L., Foti C., De Caro R. (2019) Dermatome and fasciatome. Clinical Anatomy 32, 896-902. https://doi.org/10.1002/ca.23408 10.1002/ca.23408 [DOI] [PubMed] [Google Scholar]
- Sullivan K.M., Silvey D.B., Button D.C., Behm D.G. (2013) Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. International Journal of Sports Physical Therapy 8, 228. [PMC free article] [PubMed] [Google Scholar]
- Sullivan S.J., Williams L.R., Seaborne D.E., Morelli M. (1991) Effects of massage on alpha motoneuron excitability. Physical Therapy 71, 555-560. https://doi.org/10.1093/ptj/71.8.555 10.1093/ptj/71.8.555 [DOI] [PubMed] [Google Scholar]
- Team R.C. (2018) A language and environment for statistical computing. R Foundation for Statistical Computing. [Google Scholar]
- Thong-On S., Bovonsunthonchai S., Vachalathiti R., Intiravoranont W., Suwannarat S., Smith R. (2019) Effects of strengthening and stretching exercises on the temporospatial gait parameters in patients with plantar fasciitis: A randomized controlled trial. Annals of Rehabilitation Medicine 43, 662. https://doi.org/10.5535/arm.2019.43.6.662 10.5535/arm.2019.43.6.662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trajano G.S., Seitz L.B., Nosaka K., Blazevich A.J. (2019) Passive muscle stretching impairs rapid force production and neuromuscular function in human plantar flexors. European Journal of Applied Physiology 119, 2673-2684. https://doi.org/10.1007/s00421-019-04244-0 10.1007/s00421-019-04244-0 [DOI] [PubMed] [Google Scholar]
- van Melick N., Meddeler B.M., Hoogeboom T.J., Nijhuis-van der Sanden M.W., van Cingel R.E. (2017) How to determine leg dominance: The agreement between self-reported and observed performance in healthy adults. Plos One 12, e0189876. https://doi.org/10.1371/journal.pone.0189876 10.1371/journal.pone.0189876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Pletzen D., Venter R.E. (2012) The relationship between the bunkie-test and physical performance in rugby union players. International Journal of Sports Science & Coaching 7, 543-553. https://doi.org/10.1260/1747-9541.7.3.543 10.1260/1747-9541.7.3.543 [DOI] [Google Scholar]
- Wearing S.C., Smeathers J.E., Urry S.R., Hennig E.M., Hills A.P. (2006) The pathomechanics of plantar fasciitis. Sports Medicine 36, 585-611. https://doi.org/10.2165/00007256-200636070-00004 10.2165/00007256-200636070-00004 [DOI] [PubMed] [Google Scholar]
- Wiewelhove T., Döweling A., Schneider C., Hottenrott L., Meyer T., Kellmann M., Pfeiffer M., Ferrauti A. (2019) A meta-analysis of the effects of foam rolling on performance and recovery. Frontiers in Physiology 10, 376. https://doi.org/10.3389/fphys.2019.00376 10.3389/fphys.2019.00376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke J., Debelle H., Tenberg S., Dilley A., Maganaris C. (2020a) Ankle Motion Is Associated With Soft Tissue Displacement in the Dorsal Thigh: An in vivo Investigation Suggesting Myofascial Force Transmission Across the Knee Joint. Frontiers in Physiology 11, 180. https://doi.org/10.3389/fphys.2020.00180 10.3389/fphys.2020.00180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke J., Krause F., Vogt L., Banzer W. (2016) What is evidence-based about myofascial chains: a systematic review. Archives of Physical Medicine and Rehabilitation 97, 454-461. https://doi.org/10.1016/j.apmr.2015.07.023 10.1016/j.apmr.2015.07.023 [DOI] [PubMed] [Google Scholar]
- Wilke J., Müller A.-L., Giesche F., Power G., Ahmedi H., Behm D.G. (2020b) Acute effects of foam rolling on range of motion in healthy adults: a systematic review with multilevel meta-analysis. Sports Medicine 50, 387-402. https://doi.org/10.1007/s40279-019-01205-7 10.1007/s40279-019-01205-7 [DOI] [PubMed] [Google Scholar]
- Woltman H., Feldstain A., MacKay J.C., Rocchi M. (2012) An introduction to hierarchical linear modeling. Tutorials in Quantitative Methods for Psychology 8, 52-69. https://doi.org/10.20982/tqmp.08.1.p052 10.20982/tqmp.08.1.p052 [DOI] [Google Scholar]
- Yoshimura A., Inami T., Schleip R., Mineta S., Shudo K., Hirose N. (2019) Effects of Self-myofascial Release Using a Foam Roller on Range of Motion and Morphological Changes in Muscle: A Crossover Study. Journal of Strength and Conditioning Research 35(9), 2444-2450. [DOI] [PubMed] [Google Scholar]
- Zwirner J., Zhang M., Ondruschka B., Akita K., Hammer N. (2020) An ossifying bridge–on the structural continuity between the Achilles tendon and the plantar fascia. Scientific Reports 10, 1-10. https://doi.org/10.1038/s41598-020-71316-z 10.1038/s41598-020-71316-z [DOI] [PMC free article] [PubMed] [Google Scholar]


