Abstract
Fear is an indispensable characteristic of any infectious disease, and the alarm will be further amplified when the infection spreads uncontrollable, unpredictable, and global. The novel corona virus (SARS CoV-2) lead Covid-19, has been declared as a global emergency by WHO as it has affected millions of people with a high mortality rate. The non-availability of medicine for Covid-19 and the various control measures such as social distancing, self-isolation, house quarantine, and the new normal implementation by different nations across the world to control the spread of Covid-19 made people vulnerable to fear and anxiety. As a result, considerable number of Covid-19-related suicidal deaths has been reported across the world during this pandemic. There have been several studies which describe the psychosocial aspects of suicidal ideation. However, the research on the biological aspects of suicidal ideation/suicidal risk factors that are related to pandemic are unreported. Hence this review article is intended to provide a comprehensive analysis of suicidal deaths during Covid-19 and also aimed to addresses the possible link between suicidal ideation and different factors, including psycho-social, behavioral, neurobiological factors (proximal, distal, and inflammatory) and immunity. The alterations in glutamatergic and GABAergic neurotransmitters had upregulated the GABARB3, GABARA4, GABARA3, GABARR1, GABARG2, and GAD2 gene expressions in suicidal victims. The changes in the Kynurenine (KYN) pathway, Hypothalamus-Pituitary-Adrenal axis (HPA axis) hyperactivation, and dysregulation of serotonin biosynthesis would significantly alter the brain chemistry in people with suicide ideation.
Keywords: Covid-19, suicidal behavior, psychiatric disorder, neurobiological factors, inflammatory cytokines, suicidal death
Introduction
A tremendous surge of pneumonia-like illness was first reported in Wuhan city of Hubei Province in China, December 2019. 1 The global burden of this disease has quickly spread across the globe, and it caused a life-threatening infectious disease named Coronavirus disease 2019 (Covid-19) named by World Health Organization (WHO) in January 2020. 2 The outbreak of Covid-19 has been declared by WHO as a public health emergency of international concern (PHEIC) on 11th March 2020. 1 Subsequently, the origin and speedy spread of Covid-19 has become largely indefinite. Presently, no approved vaccine or drugs to potentially inhibit Covid-19 are available. 3 Globally, physical distancing and avoiding the public gatherings including sport events, family functions, schools, and other events are recommended by default to prevent the spread of the severe acute respiratory syndrome virus (SARS CoV-2). The non-availability of sophisticated defensive measures is considered as one of the major issues among medical and healthcare personnel. Poor healthcare infrastructures can cause worry in highly populated countries like India and some level of panic also resides in people due to insufficient fundamental health protection measures. 4
The Covid-19 has strongly affected the global population irrespective of gender, age, functional difference (normal or disabled) and created intense economic, mental, and social impacts worldwide.5,6 The impact of Covid-19 affected the routine life of all walks of life.7-11 Fear, uncertainty, and stigmatization are some of the major challenging factors of this pandemic, limiting access to suitable clinical and psychological interventions. Based on the previous global novel viral outbreaks and the collapse of the socio-psychological setting, it is highly crucial to implement mental health assessment, support, treatment, and services for the better health response against Covid-19. 12 Globally, the threat of the virus and pandemic diseases raising the concerns about widespread anxiety, stress, worries, fears, panic attacks in individuals and also an increased the risk of developing brief stress-related psychoses.13-15 The extreme level of psychiatric disorders and psychological disturbances could lead to the different types of suicidal behaviors, including actual suicide, suicide attempts, and suicidal ideation. 16 Suicide is a social, spiritual and cultural issue irrespective of age, sex, gender or race and till now our society has not done sufficient endeavor to assist those people with these kind of psychiatric disorders. 17 Suicide is a complex behavior and neglected global public health issue which includes the order of process from suicidal ideation, planning and finally executing it. 18 Environmental, socio-economic factors (such as social cohesion, economic status) and meteorological factors are reported to be the chief culprits for suicidal thoughts and execution. 19
Multiple constituents of psychological interventions including panic, depressive disorder, social anxiety and alcohol consumption are considered as major underlying causes for acute suicidal affective disturbance. Several psychological distresses such as anxiety, depression and hazardous drinking are believed to be correlated with greater suicidal risk. Among them, depression and social anxiety are said to highly associate with suicidal ideation, suicide attempts, and suicide deaths. 20 The reports of psychological autopsy studies showed that the relationship between physical illness, functional disability and suicide. Individuals with serious physical condition are found to be associated with high and constant suicidal thoughts. Of these increased odds of suicide were found among older adults with multiple physical illnesses. 21 Over 90% of the people who have attempted suicide faced psychiatric distress in their last 6 months of their life. 22 Socio-demographic factors, mainly poor education, unemployment, and low income are often considered to be the major triggers of suicide, including acute stress and demoralization by public humiliation or social rejection or no support from kith and kin. 23 Moreover, either active or passive suicidal thoughts recurrently associated with depressed mood and is part of natural history of major depressive disorder. 23 In addition, other factors like the impaired regulatory function of the immune system and systemic inflammation were also considered as other major contributing factors for the suicidal behavior. 24 The nosology of depressive symptoms significantly change a person’s problem-solving capacity thusly become precipitants of suicidal crises among the victims. 22
As per WHO report 793 000 people were died by suicide across the globe in 2016, and reports from the Centers for Disease Control and Prevention (CDC) indicates that over 47 000 people were died by suicide in the USA in 2017. 25 About 40.1% increase in suicidal deaths was observed in 2016 when compared with suicides in 1990 as per the reports of National Crime Records Bureau (NCRB) of India. 26 Across-national study by Nock et al 27 found that mood disorders are predominantly strong as well as independent predictors of suicide ideation [Odd Ratio (OR)]: 3.4-4.7) and attempts (OR: 4.7-5.9). Even though suicidal ideation is debatably more common than suicide attempts (lifetime prevalence: 9.2% and 2.7%), it was shown that 29% of individuals have an idea of suicide but 59% have made definite plans to execute. 28
Compared to suicide rates of previous years 1996 to 2001, female suicidal attempts were reported to be significantly higher in Hong Kong during the epidemic situation in 2003 due to the spreading of severe acute respiratory syndrome (SARS). Suicide among the elderly women was increased to 1.4162 incident rate ratio (IRR) in 2003, with an IRR of 1.2013 and 1.1769 in 2000 and 2001, respectively. 29 Another study of psychological effects during the SARS outbreak among 129 Canadians indicated the existence of 28.9% of post-traumatic stress disorder (PTSD) and 31.2% of depression within the group. Similar psychosocial patterns were also observed among people during the Ebola outbreak. 30 Public health facility, socio-cultural practices and demographic distribution vary among countries which in turn impacts the suicide rates accordingly and economically poor countries tend to experience the very worst effects. 31 Apart from the “parallel epidemic” of depression, anxiety, and fear in the general community, the Covid-19 and other pre-existing injuries or diseases in aged people further contribute to higher rate of suicidal risks and mental health problems. 32 Likewise, many suicide attempt cases are reported in countries across the globe including India due to Covid-19 pandemic. This work is aimed to illustrate few of the suicidal cases reported in India due to the fear related to Covid-19 and explain the possible involvement of behavior, kynurenine (KYN) pathway and inflammatory responses in the brain.
Methods
The electronic literature search was conducted through databases like Google Scholar, Scopus, and PubMed. The following combination of search terms such as Covid-19, suicide, anxiety, inflammatory cytokines, behavioral health, psychological distress, quarantine, healthcare workers, and neurobiology were prominently used in our search. The papers published in English were used in the study. The suicidal cases among India and international countries during the pandemic between the periods of 19 March to 2 May, 2020 were reported in this review. Based on the collected articles, a narrative review was structured with major topics: (1) suicidal case studies during Covid-19, (2) behavioral health, (3) molecular basis of suicidal brain, and (4) role of inflammation in suicide.
Suicidal Cases
Globally, India is ranked second having least number of psychiatric healthcare professionals. Thus, approaching the individuals with mental distress due to Covid-19 by psychiatric professional becomes difficult. Therefore, psychiatric distress, financial status, healthcare work related stress issues and unemployment due to the lockdown might contribute to some percentage of people to commit suicide in India. 33 Since domestic violence, manifested by alcohol consumption and other social factors because of lockdown, becomes an additional trigger of suicide during the current pandemic. 31 In India, more than 300 deaths were reported due to psychological distress due to imposed nationwide lockdown and in this almost 30% of people (80 out of 300) took their own life due to loneliness and fear of being tested positive for the Covid-19. 34 Moreover, until now the causes of suicides or those due to Covid-19 collectively have not been reported in India. Therefore, we briefly investigated the suicidal deaths that occurred in India during this pandemic with few examples to demonstrate interconnection.
The first suicide in India occurred on 12th February 2020 from the State of Andhra Pradesh due to Covid-19. A 50-year-old man, wrongly correlated the symptoms of some other viral infection with Covid-19 and died by suicide. 35 On 23rd March 2020, 2 younger persons attempted suicide in Uttar Pradesh, India as they confused flu symptoms with Covid-19. 36 Another victim was a 60-year-old man from Arakkattalai, Tamil Nadu, India worked as a daily wager in neighboring state Kerala. After he returned from Kerala he was admitted to Ariyalur government hospital due to fever. The local people said he was suffering from kidney disease and his sample was sent to Mahatma Gandhi Government Medical College Hospital, Tiruchirappalli for the Covid-19 diagnostic test. But unfortunately, he engaged in suicide while being in isolation before the test results came back negative. 37 Yet another 40 year old male was brought to the intensive unit after he attempted suicide, because he was in interaction with a foreign couple and in the fear of acquiring the infection, he self-isolated himself from his family. Later, due to the occurrence of Covid-19 infection like symptoms such as fatigue, abdominal pain, throat dryness, he developed sever anxiety which led him to commit suicide. During treatment, it was identified that he was suffering from adjustment disorder versus severe depressive episode without any psychotic symptoms antidepressant and supportive psychotherapy were prescribed. 38 Moreover, the governments announced series of lockdown and restricted the movement of people, as part of efforts to tackle the spread of Covid-19. This produced a chance of unintended consequences, including crimes. For example, increased time spent at the home might be expected to raise the opportunities for child abuse and domestic violence as the potential victims are spending more time together. 39 The list of nation-wide lock-down deaths in India during Covid-19 pandemic is presented in Table 1.
Table 1.
Lock-down deaths in India during Covid-19 pandemic (19, March to 2, May, 2020).
| S. No | Reason for death | Death toll |
|---|---|---|
| 1 | Loneliness or fear of testing +ve for Covid-19 | 80 |
| 2 | Accidental death of migrant workers on their way to home | 51 |
| 3 | Deaths related to withdrawal symptoms | 45 |
| 4 | Starvation and financial distress | 36 |
| 5 | Physical exhaustion from long-distance walking (no transport) | 24 |
| 6 | Police atrocity/state violence | 11 |
| 7 | Lock-down related crimes | 12 |
| 8 | Denial of medical care | 38 |
| 9 | Un-specified death | 41 |
| Total | 338 |
Source: Suicide leading cause for over 300 lockdown deaths in India: Study. 34
Sleep disturbances, distress, anxiety, depression, and suicides were also reported in other Asian countries, Africa, Australia, Europe, North and South America due to Covid-19. 40 The psychiatric effect of Covid-19 poses increased the risk of suicide and other distress for months and years ahead. In the USA, the 10th leading cause of death occurred by suicide commitment in every 12 minutes, and for each successful suicide, there are 25 suicide attempts. Since March 2020, the inspiration of suicide attempts and completion of suicidal acts appears to happen due to pandemic state and has become a worrisome sign. As the USA comes at top on Covid-19 infected cases, different media sources predict that Covid-19 related suicides will increase 1.6% for each 1% rise in unemployment. 41 There are 90 000 estimated healthcare employees who suffered and 260 nurses who died from Covid-19 infection. Considering the Covid-19 crisis and continuous risk of exposure in medical facilities this could raise stress to an unprecedented levels for nurses or other workers which could eventually trigger the suicide thoughts and execution. 42 WHO reported that a lot of suicides arise during this pandemic crisis and causative factors includes loneliness, financial issues, discrimination, and psychological problems are provoked due to Covid-19 pandemic. This pandemic is said to promote mental illnesses and to raise suicide rates. 43 While clinical treatment of people with Covid-19 exist, the assets to treat the subsequent and related mental effects are insufficient. The physical infection can be seen, however, the mental effects are frequently not seen until it is too late. 44 Though, the suicidal cases due to Covid-19 fear occurs all over the world, here, we report few examples of suicidal related deaths with respect to Bangladesh, UK, Italy, and Germany.
After returning from Dhaka, a 36 years old man attempted suicide due to misdiagnosing symptoms like cold, fever, and weight loss, which made him and his neighbors believe that he was suffering from Covid-19 infection. His autopsy report showed that the suspect was Covid-19 (−ve). 5 A 19-year-old British girl, expired in a hospital located in King’s Lynn on 29th March 2020. Previously, she attempted suicide fearing Covid-19 and she was transferred to the hospital in a critical condition. Later, her relatives decided to remove her from life support and permit the doctors to collect her organs for donation. 45 A 34 year old Italian nurse, who was supporting the treatment of Covid-19 patients in an intensive care unit (ICU) took her own life after she diagnosed Covid-19 positive. 46 One more healthcare person in King’s College Hospital in London, a nurse in her 20s, took her own life, since 8 of her patients have died because of Covid-19. 47 Another 54 year old German finance minister from the State of Hesse, was found dead in the railway station on Saturday, 28th March 2020. It was reported that he did suicide after being profoundly concerned and worried about his State’s financial aid and growing concerns of the Covid-19 pandemic. 48
In conclusion, the above mentioned case studies have implied the increased psychological distress among healthy people and healthcare workers are owing to the increased anxiety of Covid-19. Across the globe, both Covid-19 positive, negative cases and healthy people have also attempted suicide in different ways and also fewer people were engaged in suicide due to inaccessibility to alcohol during this pandemic situation. Therefore, there is an urgent need for psychiatric healthcare advice, support and awareness to help the common public with the assistance of local and international media.
Behavioral Health
The need of studying behavioral health
The implementation of unfamiliar measures especially when imposed on personal freedom leads to emotional distress, which is noticeable during pandemic times. Fear or anxiety, confusion, irritation, frustration, boredom, and self-isolation could make the people emotionally unstable ergo, focus should be on the mental health condition of people as a high priority during pandemic situations. 29 During a pandemic like Covid-19, one of the significant precautions is social distancing in order to prevent further transmission and the implementation of lockdown caused the loss of routine/decreased social contact that could increase frustration among people. The major factors such as fear about getting infected, the length of quarantine period, lack of essential supplies and poor knowledge about quarantine and associated guidelines results in the development of stress among peoples. 49 One of the major characteristic features of pandemic disasters compared with other disasters is that, it insists on isolation and quarantine of the victims that affects the relational functioning in the families. A survey among 398 parents and their children in various containment areas who experienced quarantine or self isolation showed characteristic of PTSD by 25% and 30%, respectively. 50 During and post-pandemic times, there is a need to implement behavioral health strategies to overcome fear, anxiety, and suicidal ideation. As the countries are working to reduce the transmission rate of Covid-19, it is necessary to reduce the individual worries to accomplish a healthy Covid-19 fear free society. 14 Indeed, mentally some people may recover quickly while others may become vulnerable and may not overcome the emotional stress (such as fear and anxiety). Paramount, the primary focus should be on people who are having psychological disorders as they are prone to suicidal ideation easily. There are reports from Iran showing that people are anxious when thinking about corona virus, and many of them were not able to sleep due to this thought. 14 Worries about life, family, financial crisis, loneliness, self-isolation, and fear about social behavior even after the recovery of the disease could increase the mental distress and ultimately form as a base for suicidal ideation. One family affected by MERS conveyed that people started avoiding them when they heard about a MERS infected person in their family, and shopkeepers started to throw things at them and shouted against them to leave. Even after recovering from the disease, people still believed in discrimination and rumors, 51 which certainly would be applicable to other epidemics or pandemics.
Individuals watching the Covid-19 news may feel anxious because the media gives update about the mortality rate, critical situation, non-availability of treatment options for Covid-19, and quarantine. The individual may feel overwhelmed with such kind of information when such a person is tested Covid-19 positive and kept under self-isolation leading to the chances of elevated emotional distress. 52 A study in Wuhan during Covid-19 times reported the impact of social media exposure on mental health in individuals and showed that 82% of the participants were exposed to social media developed higher prevalence of anxiety and depression. 53 One of the significant characteristic features of an infectious disease is fear and transmission rate and fear by itself can amplify the psychological damage. 52 The development of fear could alter the person’s behavior and most of the people who have attempted suicide have compared their symptoms to Covid-19 and died by suicide even without testing. People who are having psychological disorders, especially with stress, anxiety, and depression, are prone to suicide ideation and it was reported that 25% of the SARS survivors showed PTSD, and 15.6% have depression. This insists the need of studying the emotional distress among infected people, along with Covid-19 treatment and as the authors suggest that increase in preparedness of healthcare professionals to find and manage people’s psychological behavior during these kind of infectious outbreaks. 54
Emotional distress in health care workers
The levels of emotional stress in healthcare individuals are seem to be higher than common public and the psychological distress that developed by health care workers (HCWs) during SARS time sustained even after a year and hence remaining as a major concern. 55 Medical practitioners who worked in high-risk locations, and people who contacted SARS patients were susceptible to develop post traumatic symptoms (PTS). The likelihood rate was 2 to 3 times higher than healthy individuals. 56 Koh et al 57 also reported that the anxiety level in >50% of medical practitioners was higher during SARS time and around 18% to 57% of medical professionals experienced emotional distress during SARS period.
The reported levels of anxiety, depression, stress, and PTSD in HCWs across the globe during Covid-19 are mentioned in Table 2. The psychological impact of Covid-19 on healthcare personnel in Singapore showed that the level of psychological distress is more than non-medical healthcare professionals, 58 which shows that HCWs are under huge amount of psychological pressure. The stress level of HCWs in Singapore and India seemed to be on the lower side when compared to other developed countries (such as USA and China), which may be explained by job demand and extended unreasonable working hours. Further, HCWs professionals in India are well experienced with taking care of large number of patients even during non-pandemic times. These kinds of past experiences could have helped to lower the panic associated with a pandemic to certain extent. 59
Table 2.
The comparison of prevalence rate of anxiety, depression, stress, and PTSD among HCWs from various countries.
| Category | Country | Anxiety (%) | Depression (%) | Stress (%) | PTSD (%) | Mode of study | Reference |
|---|---|---|---|---|---|---|---|
| HCWs * | Singapore | 10.8 | 5.2 | 6.4 | 5.7 | Self-administered questionnaire | Tan et al 58 |
| Non-medical HCWs * | Singapore | 20.7 | 10.3 | 6.9 | 1.9 | Self-administered questionnaire | Tan et al 58 |
| HCWs | China (Wuhan) | 24.1 | 13.5 | 29.8 | Questionnaire | Zhu et al 60 | |
| Nurses and physicians | China (Wuhan) | 41.1 | 46.9 | 69.1 | Online survey through social media | Lin et al 55 | |
| Nurses and physicians | China (Wuhan) | 44.6 | 50.4 | 71.5 | Questionnaire | Lai et al 61 | |
| HCWs | China (Wuhan) | 20.1 | 12.7 | 59 | Electronic survey | Du et al 62 | |
| HCWs | USA (New York) | 33 | 48 | 57 | Electronic survey | Shechter et al 63 | |
| HCWs | Singapore | 14.4 | 9 | 6.5 | 7.5 | Self-administered questionnaire | Chew et al 64 |
| HCWs | India | 17.1 | 12.4 | 3.8 | 7.3 | Self-administered questionnaire | Chew et al 64 |
| HCWs | India | 17.7 | 11.4 | 3.7 | Online questionnaire | Wilson et al 59 |
All studies are cross-sectional in nature.
HCWs include physicians, nurses and allied professionals including clinical technicians and others who were actively involved in health care sectors.
Non-medical HCWs include allied health professionals, pharmacists, technicians, administrators, clerical staff, and maintenance workers.
As discussed previously, there have been reports of suicidal deaths associated with Covid-19 fear by HCWs in Italy and Britain. HCWs, in addition to risk of developing anxiety disorders, depressive mood and post-traumatic stress disorders, also have an increased likelihood of experiencing brief psychotic symptoms during the current COVID-19 pandemic. 65 The major reasons behind the development of adjustment disorders in HCWs is due to the asymptomatic nature of Covid-19 transmission, work pressure, fear of the viral spread by them to their families/friends, behavior of patients who do not follow the medical measures or quarantines, non-availability of personal protective equipment (PPEs), sleeplessness and lack of training to face pandemic situations.63,66 The lessons learned from epidemics like SARS and MERS will help us develop a potential strategy to reduce the psychological and emotional distress among the individuals that improve their wellbeing. 67
Measurement of psychological distress
It is necessary to conduct epidemiological studies that evaluate the level of fear, anxiety, depression, and other mental health problems associated with Covid-19. 5 The emotional states can be identified based on the answers to questionnaires by assigning a score from which we can identify mild, moderate, or severe disorders. 68 Nearly half of the patients affected by MERS and SARS displayed psychological distress. 13 For successful Covid-19 psychological distress management it is necessary to include common people as well as patients who are vulnerable during such pandemic times. Emotional states of an individual can be measured by framing various questionnaires to identify the level of distress which can be filled by the patients and or by practitioners/HCWs. The widely used psychological scale is depression anxiety stress scales (DASS-21) by which all psychological symptoms can be obtained from a common scale, which can be further analyzed to get severity of symptoms to classify that state into mild, moderate or severe. Impact of events scale-revised (IES-R) instrument is also used to calculate the emotional distress associated with the outburst of Covid-19. 64 The widely used scales to measure anxiety includes Beck anxiety inventory (BAI), generalized anxiety disorder scale (GAD) while depression can be evaluated based on Beck depression inventory-II (BDI-II).61,62 Questionnaire based on public health are also employed as psychological screening tests and the stress severity is assessed by perceived stress scale (PSS10).62,63 In most of the studies, the data are collected via a link, surveys or via social media through various working institutions or via the web then evaluated via various statistical tools by assigning scores which are analyzed to understand the psychological distress among the individuals.60,61,63 Ahorsu et al 14 developed and validated (among 717 Iranians) a psychometric instrument/scale named Fear of Covid-19 Scale (FCV-19S) to capture individuals’ fear of Covid-19. Further, they reported the severity of fear indicated among the individuals using FCV-19S and that this instrument aided them in reducing social stigma and fear associated with Covid-19.
The Molecular Basis of the Suicidal Brain
Suicide is considered as a universal health concern accounting for a minimum of 800 000 deaths occurs per year. It takes serious toll for people ages from 15 to 44 on worldwide due to several reasons. Over the last decades, the rate of suicide is quite alarming across the globe and especially very high in Europe and United States, which disrupts the socio-economic and country status. Several models have been proposed that differ in their prominence on the role of psychological, psychiatric, neurobiological and social factors in explaining the suicide risk.69,70 The post-mortem reports of the brain, genomic and neuroimaging (in vivo) studies clearly signify a biological basis for diathesis, suggesting relevance of both neurobiological screening and interventions.71,72 The neurobiology of suicide is a vast field, ranging from initial candidate gene studies to recent miRNA expression. Also, the genetic relation among suicide and polymorphisms of the HPA-axis, serotonin system, noradrenergic system and polyamines have been well established. 73 Early-life adversity and epigenetic mechanisms may justify the association among suicide risk, brain circuitry as well as abnormality in neurochemistry. 71 The public normality and restrictions often make it complicated for the people who experience either suicidal ideation or any aspects of suicidal behavior to get help before it is overdue. Thus, a clear understanding on the suicide neurobiology is essential so that the suicidal mortality can be avoided through appropriate treatment. Extensive neuro and cognitive psychological studies helped us to understand the various aspects of suicidal behavior. It further determined how brain anatomy would contribute specific trait-like characteristics that constitute the suicidal behavior vulnerability. Various studies have reported that the dysfunction of brain is also considered as one of the contributing factors causing suicidal behavior. 74 Neurobiological factors that contribute to suicide are broadly classified into distal and proximal risk factors. The distal factors tend to enhance early disposition to suicide, while proximal factors precipitate an act of suicide. Proximal factors show a strong relationship between psychopathology, most conspicuously major depressive disorder (MDD), and suicide risk. 23
Distal factors
Depression and anxiety disorders have genetic predispositions as major risk factor. Suicide/depression often occurs because of the incapability of brain to take correct responses to the external stimuli due to the damage of synaptic and neuronal plasticity. Neurotrophins are interrelated members of the nerve protein nerve growth factor (NGF). The family of neurotrophic factors besides NGF include brain-derived neurotrophic factor (BDNF), Neurotrophin-3 (NT-3), and NT-4/5, that all have a critical function in neuronal survival, differentiation, plasticity throughout development and adulthood. 75 Reports revealed the involvement of BDNF in the physiological functions of mood disorders. 76 The level of BDNF expression is lower in platelets or lymphocytes of both depressed individuals and suicide attempters than healthy normal individuals. 77 The studies on the human model support the function of both BDNF and NT-3 within the pathophysiology of stress and depression. Studies on genetics strengthened the functioning of neurotrophins in mood related disorders since it was previously found that either BDNF or its low-affinity receptor, pan 75 neurotrophin receptor (p75NTR), gene polymorphisms could couple to depressive disorder and suicidal thoughts. 75
One of the significant candidate genes is BDNF and has major function in growth, neuronal survival, differentiation, and synaptic plasticity.78,79 BDNF can mediate stress responses in the brain region, even though its effect is possibly complex, dynamic, and non-linear. 23 BDNF belongs to neurotrophin family and is located on chromosome 11p13. The missense mutation in the precursor BDNF (pro-BDNF) could result in the development of single nucleotide (G196A) polymorphism (SNP) at codon 66 that forms methionine (Met) instead of valine (Val). SNP (SNP ID: rs6265) is believed to reduce the release of BDNF protein in the central nervous system (CNS) that results in lowered BDNF activity which is correlated to neurodegenerative diseases like Parkinson’s disease, Alzheimer’s disease and other psychiatric disorders as well. 80 In healthy individuals, the BDNF Val66Met polymorphism is directly associated with anxiety as well as cognitive activities and both are connected to suicidal thoughts. Pro-BDNF in the mammalian brain undergoes proteolytic cleavage to form a mature BDNF. The BDNF can binds to its higher affinity receptor tropomyosin related kinase B (TrkB) and mediates neuroprotective functions, nerve growth, neural transmission, synaptic plasticity, and other events. 80 The neurotrophic factors including BDNF are produced constitutively or via regulated pathways in non-neural tissues. 81 SNP alters the activity dependent secretion of BDNF which results in reduced BDNF production also it binds with lower affinity to receptor namedp75NTR.82-84 The Met allele or SNP was reported to damage the intercellular trafficking of BDNF with a nearly 30% reduction of activity dependent secretion of BDNF. 84 Lowered expression of neurotrophins, along with low expression and activation of TrK and concomitant enhanced expression of p75NTR represents the abnormalities in suicidal brain. The ratio of expression levels as well as activation of TrK receptors and p75NTR is significant in neurotrophin-assisted process. 85 The binding of neurotrophic factors with Trk activates signaling pathways such as phosphatidylinositol 3-kinase (PI3K), mitogen-activated protein kinase (MAPK), and phospholipase C-γ (PLC-γ) which are required for the proper synaptic functioning including cell survival. While binding of NGF with p75NTR could activate the nuclear factor kappa B (NF-κB) or c-Jun N-terminal kinase which causes apoptosis and excessive activation/binding results in neurodegeneration and stress related issues. The balancing of these signaling pathways by proper receptor binding is highly important in order to maintain the synaptic functioning and to manage stress as well.80,86 Lower BDNF expression is likely to be associated with the pathogenesis of depression and the administration of antidepressants may enhance BDNF production. 74 In general, the alternations in the BDNF signaling pathway could be considered as a significant biological risk factor in both the etiology and development of suicidal acts. 84 The distal risk factors for suicidal commitment are illustrated in Figure 1.
Figure 1.
Role of distal factor in suicidal behavior. Distal risk factor predisposition to suicide. Brain-derived neurotrophic factor (BDNF) is synthesized as a precursor known as proBDNF, which later undergoes proteolytic cleavage to form a mature BDNF. The proBDNF preferentially binds to p75NTR and mature BDNF to TrkB. The binding of BDF with high affinity receptor TrkB activates various signaling pathways such as P13K, MAPK and PLC-γ, which are required for proper synaptic functioning, cell survival and maintaining neural plasticity. A single nucleotide (G196A) polymorphism (SNP) of BDNF gene produce Val to Met substitution in the proBDNF protein at codon 66 (Val66Met). This SNP (SNP ID: rs6265) decreases the activity dependent secretion of BDNF protein in the brain and results in lower trafficking of BDNF. In addition, the BDNF actively binds with lower affinity receptor p75NTR that activates NF-κB and c-Jun N-terminal kinase pathways and it induces apoptosis. The presence of excess levels results in neurodegeneration and mood disorders that can cause suicidal behavior. The abnormality in BDNF signaling pathway function is considered a vital biological risk factor in the pathological process of suicide.
Proximal factors
Serotonergic alterations
The serotonergic system has been extensively studied since 1948 by the discovery of serotonin from beef serum and shortly afterwards serotonin in the mammalian brain was demonstrated by Twarog and Page. Serotonin, a monoamine neurotransmitter is synthesized by hydroxylation of the amino acid, tryptophan (TRP) by the enzymes tryptophan hydroxylase 1 and 2 (TPH1 and TPH2). 87 The dysfunction of the serotonin biosynthesis pathway is an established perception for suicidal behavior, which is mediated by increased aggressiveness in the case of mood disorders. 88 In 1976, Asberg and colleagues, 89 for the first time, demonstrated changes in the serotonergic system in the brain of suicide attempters. Here, 5-hydroxyindoleacetic acid (5-HIAA), the major metabolite of serotonin is detected in lesser amounts in the cerebrospinal fluid (CSF) of patients affected with depression. 90 Reduced level of serotonin and 5-HIAA and change in the kinetics of serotonin as well as its receptor interaction was reported in the brain of suicide attempters compared with healthy individuals. 91 The post-mortem reports of suicide subjects point out a localized decline in serotonin transporter binding in the anterior cingulated and ventro medial prefrontal cortex. Impaired serotonin input into this brain region may result in impaired decision-making, which ultimately leads to the risk of suicidal behavior. Altered level of serotonin uptake into different parts of the brain including the dorsal lateral prefrontal cortex, subgenual prefrontal cortex, and the amygdala is also associated with mood disorders, depression, and suicidal ideation. 92
Glutamatergic and GABAergic alterations
Glutamate and gamma aminobutyric acid (GABA) are the 2 major excitatory and inhibitory, neurotransmitters in the CNS, respectively. Reports suggest that the changes in these neurotransmitter systems are associated with pathophysiology of depression. 93 Glial glutamate transporter (GLT) is involved in the uptake of glutamate and metabolism and the glutamine, which is synthesized from glutamate is released from the astrocytes to the extracellular space and it is further converted back to glutamate or GABA in neurons. In suicide victims with major depression, decrease in glutamine synthetase (GS) was observed in prefrontal and parietal regions of the brain, but suicide victims without mood disorders or depression exhibited normal levels of GS. This suggests that depression is coupled with impaired glutamate recycling, which further results in dysregulated glutamatergic and GABAergic neurotransmission.94,95
Alteration in the GABAergic modulators is speculated to be involved in triggering the suicide and increased expression of genes encoding GABAergic proteins in anterior cingulate cortex (ACC) and differential dorso lateral prefrontal cortex (DLPFC) were observed in suicide victims. Hypermethylation were detected in dysregulated GABA-A receptor subunits and promoter in suicide victims and most of the elevated GABA-A receptor were detected in depressed people following suicidal accomplishment. 96 Abnormalities in GABA A receptor trafficking triggers GABAergic dysfunction in a number of brain pathological conditions that includes most of the neuropsychiatric and neurodegenerative diseases. 97 Some other genes associated with GABAergic neurotransmission (GABARB3, GABARA4, GABARA3, GABARR1, GABARG2, and GAD2) were observed to be involved in the suicide cases, and it showed a prominent association between miRNA-mediated GABAergic deficits and locus coeruleus (LC) based noradrenergic activity. Changes in the production of GABA receptor subtypes such as α3, γ2, β1/3, and ε in the brain samples of depressed individuals were also detected. Moreover, signaling regulator proteins such as protein kinase A (PKA), glucocorticoid, neurotrophins, phospholipase C (PLC), mitogen-activated protein kinase extracellular signal-regulated kinase (ERK/MAPK), glycogen synthase kinase-3 beta (GSK3-ß), monoamine oxidase (MAO), corticotropin-releasing hormone (CRH) were proved to be involved in LC-based neuropathological mechanism of suicide. Taken together, all these signaling components play vital roles in both mood disorders and suicide. 98
Glial cells dysfunction
The clinical findings and cellular evidences have strongly documented the role of gliogenesis and glial pathology is associated with depression. Loss of glial cells within the regions of the ACC, DLPFC, and orbitofrontal cortex which are associated with MDD in postmortem tissue was described. 99 Astrocytes are among the predominant glial cell types and approximately 20% of the cell volume of gray matter is occupied by astrocytes, which are recognized by the expression of glial fibrillary acidic protein (GFAP). 100 Altered synaptic plasticity is a characteristic of depression wherein depression and anxiety disorder are likely to be influenced by tripartite synapses components. In addition, neurotrophic factors such as BDNF and glial cell-derived neurotrophic factor (GDNF) originated from the astrocytes and a reduction of these factors may be a reason for mood disorders associated with astrocyte dysfunction. 101 Astrocytes are also involved in many essential neural circuit and metabolic functions and their functional alterations were observed in patients with schizophrenia and MDD. Also, myelin basic protein which is considered as one of the markers of the oligodendrocytic glial population is lowered completely within the prefrontal cortex of MDD and schizophrenic individuals who attempted suicide. 102 The post-mortem reports showed that changes in expression of the GFAP, GS, and glial-specific excitatory amino-acid transporters (EAATs) in brain tissue from people with MDD, confirmed that the possible impairment in glial cell alters its function. 103 Accumulation of glutamate also activates N-methyl-D-aspartate (NMDA) which inhibits the BDNF pathway. 101 Studies reported a lowered expression of both GFAP mRNA and protein as well as a low density of GFAP-immunoreactive (IR) astrocytes in the LC in MDD. Different astrocyte-associated genes were conjointly dysregulated in MDD in astrocytes which were laser-dissected from LC. 104 The proximal risk factors for suicidal commitment illustrated in Figure 2.
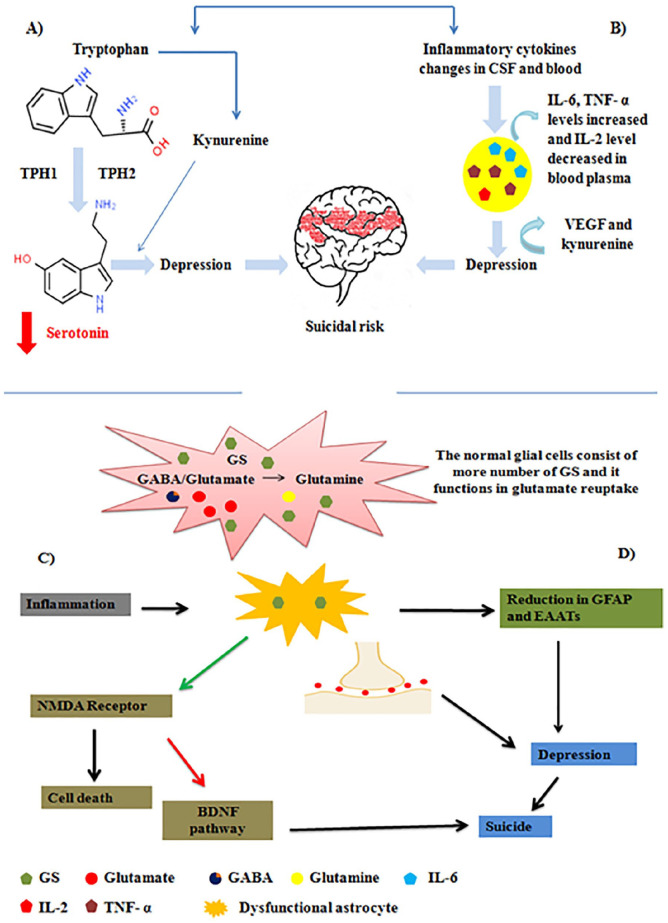
Figure 2.
An overview of the proximal contributors to suicidal behavior: (A) Under normal condition, serotonin (a monoamine neurotransmitter) is synthesized from the hydroxylation of tryptophan (TRP) by the enzymes TPH1 and TPH2. However, increased inflammatory cytokines deviates the tryptophan pathway to produce kynurenine (KYN) hindering the serotonin biosynthesis. Reduced level of serotonin and 5-hydroxyindoleacetic acid (5-HIAA), and changes in the kinetics of serotonin and its receptor interaction leads to impaired decision making which results in suicidal ideation, (B) Suicidal ideation and behavior have pronounced inflammatory changes in both blood and cerebrospinal fluid (CSF). In suicide attempters the levels of plasma IL-6 and TNF- α are increased and IL-2 level is decreased, (C) The impaired glutamate recycling results in dysregulated glutamatergic and/or GABAergic neurotransmission, which leads to mood disorders and suicide. Under normal conditions, the glutamate that is released into the pre synaptic cleft is taken up by the surrounding astrocytes. GS present in the astrocytes plays a major role in glutamate re-uptake from the synaptic cleft. The dysfunction of glial cells results in the down regulation of GS that result in the deposition of glutamate in the presynaptic cleft. This activates the NMDA receptor consequently resulting in cell death. In addition, it inhibits the BDNF pathway leading to suicidal behavior. (Red arrow indicates inhibition, while green indicates activation), and (D) Altered expression of glial fibrillary associated protein (GFAP), glial-specific excitatory amino-acid transporters (EAATs) in tissue, suggests that the glial cell abnormalities include changes in astrocytic cell functions of depressed individuals who engaged in suicidal activities.
Inflammatory factors
There is a growing prima facie case for inflammation being linked with suicide and changes in peripheral cytokine levels accompany suicidal behavior. 105 Shreds of evidence suggest that the patients with suicidal ideation and behavior have pronounced inflammatory reactions in both CSF and blood. 106 A comparative study between suicide attempters and non-suicidal depressed individuals showed higher levels of inflammatory factors like IL-6 and TNF- α and declined IL-2 levels in the former.107,108 The inflammatory mediators contributes a vital function in the pathogenesis of depression and studies implicate that vascular endothelial growth factor (VEGF) and KYN levels could be involved in the pathophysiology of suicide. 109 Inflammatory cytokines will either be generated within the CNS or it may pass through the brain from the periphery via the blood-brain barrier (BBB). Studies reported that the suicidal patients have a higher permeability of BBB, along with higher CSF levels of hyaluronic acid (glycosaminoglycan), which is a ligand for CD44 and is an indication of hyperbolic neuro-inflammation. The activation of toll-like receptors (TLRs) enhances the level of inflammatory cytokines, which said to play a crucial function in regulating innate immune responses. Brundin et al 24 reported that other than psychiatric diagnoses, protein levels of TLR3 and TLR4 and mRNA were systematically dysregulated in both depressed and non-depressed suicide victims. An acute-phase inflammatory protein, C-reactive protein (CRP) of liver kupffer cells induces other cells to disintegrate through complement system which is produced during increase in IL-6 in the serum and thereby CRPs also believed to contribute to suicidal behavior. 108
Most of the viruses that belong to family Coronaviridae show parallel structures as well as infection pathways. Recent research reveals that coronaviruses not only affect respiratory tract but also the CNS that ends up in both neuro-invasion and neurotropism as general characteristics. 110 SARS and MERS also displayed neurological complications (CNS) with a prevalence rate of 0.04% and 0.20%, respectively. Based on these data which is being extrapolated to Covid-19 reports (4.8 million cases globally), nearly 1805 to 9671 patients are having neurological complications. As Covid-19 cases are exponentially increasing, there showed rise in the neurological and psychological complications which will increase the burden of the disease. 111 It can be either direct effects of the alteration of host cell by viral invasion, or cytokine storm due to excessive viral load that in turn induce the excessive production of pro-inflammatory cytokines further damaging various organs and further leads to death. 112 It can also be post infectious meditated by cellular, immune sickness and neurological complications associated with systemic effects of Covid-19. 111 The UK based surveillance study of 125 patients with Covid-19 reported the presence of, neurological or psychiatric diseases over 21 days (31% patients had distorted mental status, in which 13% with encephalopathy (of whom 6% had encephalitis), and 18% with a diagnosis of neuropsychiatric symptoms, including 8% with psychosis, 5% with neurocognitive (dementia-like) syndrome, and 3% with an affective disorder). 113 The immuno-pathological mechanism of brain damage within the SARS patients were observed an increased level of monokine induced by IFN-γ (Mig), a member of CXC chemokine family and it gliocytes could be responsible for Mig production. Moreover, CT scanning indicates the brain damage whereas, pathologic examination revealed gliocytes hyperplasia, neuronal denaturation, and necrosis combined with a striated encephalomalacia, symptomatic of chronic progressive viral cerebritis. 114
Angiotensin-converting enzyme 2 (ACE2) is a cardio-cerebral vascular protection protein present in nervous system and skeletal muscles. It acts as a central target for a variety of influenza and coronaviruses. The viral binding to ACE2 receptors, cause exceptionally high blood pressure and the risk of cerebral hemorrhage could be elevated. Followed by SARS-CoV-2 attack, other pathogenic bacteria may also destroy the BBB and penetrate the CNS by damaging the vascular system. In severe cases of secondary intracranial infections patients experience symptoms such as vision impairment, headache, projectile vomiting, and limb convulsions. 115 The autoimmune disease could be either due to excessive self-response or by antigen-driven immune responses and it is related to infection, genetic susceptibility or stress. SARS-CoV-2 infected individual’s produces autoantibodies against the coronavirus spike protein and were found to attack antigens in human epithelial/endothelial cells, which results in autoimmune encephalitis and cerebral edema. 116 The Covid-19 infected people with cerebrovascular disease showed hypoxia conditions which lead to lowered cerebral oxygenation and infarcts. The risk of ischemic stroke elevates in older patients due to infection, inflammation, and hypercoagulable states. 117 Covid-19 patients with neuropsychiatric symptoms showed “hematic” CSF tap with 960 cell/µL of red and white blood cells and an elevated protein (65 mg/dL) along with evident of NMDA receptor antibodies that can trigger autoantibody production. 118
In most patients, high level of CSF protein, lactate or white blood cells with negative SARS-CoV-2 polymerase chain reaction (PCR) showed inflammatory changes compatible with autoimmune encephalitis. The neurofilament light chain (NfL) level (>5000 pg/mL) was noticeably high in CSF of some Covid-19 infected, thus exceeding established cut-off values (>2500 pg/mL) for rapidly progressing neurodegenerative diseases especially amyotrophic lateral sclerosis (ALS) and multisystem atrophy. Increased NfL levels may direct tissue damage either due to viral replication or inflammatory damage. 119 Till now there are no reports to put forward that SARS-CoV-2 or related coronaviruses are highly neuro-virulent, unlike other viruses such as herpes simplex virus, a number of enteroviruses, and arthropod-borne viruses, which were proven to cause widespread neural damage. 111 The above reports suggests that Covid-19 patients have notable psychiatric disturbances ought to be examine closely for any kind of neurologic manifestations of common symptoms or variations in mental status, signs of meningitis and dyskinesias as well. Severe infection poses high risk for developing neurological squeal which could increase the mortality rate. Besides, novel corona viral infection, there should be a strong consideration given on a differential diagnosis in psychiatric patients with presentation of sudden onset.
Role of Inflammation in Suicide Among Covid-19 Pandemic
According to reports, a higher risk of suicide correlates with the prevalence of high stress during the Covid-19 pandemic. Stress associated with comorbidities makes people even more vulnerable to severe infection of SARS-CoV-2. 120 Psychosocial factors like over thinking about the outbreak of Covid-19 pandemic, health-related anxiety, loneliness, economic stress induces mood disorders like depression among the population. People with pre-existing mental health issues might probably develop worsening symptoms, and others might experience new psychiatric issues during this pandemic. The correlation of suicidal ideation and behavior with inflammatory changes and impaired regulatory function of immune system were also reported.106,24 Recent studies reported the stimulation of enhanced synthesis of TNF-α, IL-6,IL-1 receptor antagonist (IL-1Ra) and IFN-γ due to stress. 121 In addition to the stress linked inflammatory response due to Covid-19, external pathogens like viruses can also believe to induce inflammation within the glial cells that can mediate specific neuro-inflammatory reactions leading to depression and suicidal ideation. 122 Influenza, corona, HIV, and Hepatitis C virus infected patients were shown to have severe mood disorders and suicidal ideation. 24 Replication of coronavirus in the CNS of patients with multiple sclerosis which indicates the possible invasion of the pathogens into the nervous system was also reported. 123 Moreover, in a pathogen-immune-mood disorders connection, it is necessary to conceptualize the pathogen, which induces inflammatory responses as a stress inducer. 124
The inflammatory cytokines induce changes in neuroendocrine function, neurotransmitter metabolism, and triggers the onset of depressive symptoms like any other physical or psychological stressors. 125 Immunological changes are perceived in patients with stress, depression, and other psychiatric disorders, which indicate the interaction of the immune system with CNS. 126 Moreover, studies also reveal that receptors of different hormones exist on the surface of lymphocytes/monocytes. Hence, this endocrine messengers bridges CNS and immune system and elicits inflammatory immune response. 127 Dysregulated inflammatory responses (such as reduced level of anti-inflammatory IL-10, increased concentration of plasma soluble interleukin-2 receptor (S-IL-2R), pro-inflammatory cytokines like IL-1, IL-2, IL-6; decreased natural killer cell activity and T cell function) are reported in the blood and CSF of suicide attempters and or patients with suicide ideation. 126 Several studies described the importance of pro-inflammatory cytokines in comprehending the physiological process of stress and mood related disorders.
The increased levels of mRNA sequences transcripts of anti-inflammatory IL-4 and IL-13 in the orbitofrontal cortex of suicide victims were also observed. 128 Studies reported that an enhanced level of microglia signifying increased inflammatory response among the suicide victims. Besides, a reduced level of neuro-protective IL-8 level was reported in suicide attempters with high anxiety. 129 Reports also indicated that there is a significant reduction in chemokines such as CCL1, CCL8, CCL13, CCL15, CCL17, CCL19, CCL20, and CXCL11 in suicide victims. 130 Thereby, studies showed that there is a high correlation between altered levels of pro-inflammatory cytokines like IL-1β, IL-2, IL-6, TNF-α and anti-inflammatory cytokines like IL 4, IL 10, and IL-13 and depression/suicidal behavior. 131
Interlink between inflammation and suicide behavior
Researchers have identified several possible mechanisms between stress induced inflammation and suicidal behavior. The major mechanisms believed to be involved are KYN metabolism, hyperactivation of HPA axis, and altered monoamine metabolism. Cytokines found in the peripheral immune cells can penetrate the BBB or be synthesized within the CNS by the glial cells and could induce neuroinflammation. 132 The overall scheme representing the mechanisms involved in suicidal behavior due to inflammatory responses are depicted in Figure 3.
Figure 3.
Schematic representation of pathways involved in inflammatory responses causing suicidal behavior. In case of kynurenine (KYN) pathway, tryptophan (TRP) is converted to KYN with the help of the enzyme indoleamine 2,3-dioxygenase (IDO) or tryptophan 2,3-dioxygenase (TDO), which is activated by the inflammatory cytokines. Further, downstream activations lead to the formation of quinolinic acid (QUIN), which increases the extracellular glutamate level resulting in suicidal behavior. Non-availability of TRP for the biosynthesis of serotonin also causes mood related disorders. Increased pro-inflammatory cytokines in the CNS can also desensitize glucocorticoid receptor thereby inhibiting the negative feedback mechanism for activation of HPA axis leading to hyper-activation of HPA axis.
Kynurenine pathway
Increased level of inflammatory cytokines is present in both CNS and peripheral blood of suicidal patients. The pro-inflammatory cytokines are considered as the main triggers to initiate the KYN pathway, which drives to the synthesis of by-products leading to suicidal behavior. 133 In the course of increased inflammation, the inflammatory cytokines induce the TRP to follow the KYN pathway, the catabolic pathway of TRP. The initial step of formation of KYN from TRP is mediated by an enzyme indoleamine 2,3-dioxygenase (IDO) or tryptophan 2,3-dioxygenase (TDO). 24 Pro-inflammatory cytokines like IFN-γ, IL-6, IL-1β, and TNF-α are potential elicitors of IDO/TDO. The subsequent neuroactive metabolites synthesized in the pathway include quinolinic acid (QUIN), kynurenic acid (KYNA), picolinic acid (PIC), and 3-hydroxyanthranilic acid (3-HAA). 134 QUIN increases the extracellular glutamate level, and the uptake of glutamate is reduced. Besides, QUIN also forms ROS when complex with iron leading to lipid peroxidation and the effect of QUIN on glutamate neurotransmission might be the underlying mechanism for suicidal behavior. 135 Serotonin, the happy hormone, exhibits a crucial part in the maintenance of circadian rhythm, cognition, mood, sexual behavior, appetite, and aggression. TRP also acts as a precursor of serotonin biosynthesis. 136 It has been hypothesized that during intensive inflammatory reactions, TRP availability for serotonin biosynthesis is drastically reduced as the amino acid will be catabolized via the KYN pathway. Subsequently, reduced serotonin interferes with the mood and lead to depression. Studies reported that reduced level of 5-HIAA, the primary product of serotonin in CSF of suicide attempters. 134 Studies indicate that 300% higher level of QUIN in CSF were found in patients who attempted suicide than the healthy individuals. Also, the level of QUIN in CSF depends on the IL-6 level, suggesting the initiation of the KYN pathway by inflammatory responses. 137 Recent studies have shown a 40% reduction in the plasma TRP levels and a 40% rise in KYN in case of suicidal cases with mood disorders compared with non-suicidal patients with mood disorders and normal individuals. 134 The possible involvement of TRP and melatonin in Covid-19 was recently reported from our group. 138
Hyperactivation of HPA axis
Altered regulation or hyperactivity of the HPA axis can influence suicide in mood-related illness and psychiatric disorders like depression and PTSD influenced by elevated inflammatory responses.134,139 The modulation of stress response is considered to be one of the major functions of HPA axis and the activity of HPA axis could be stimulated by the secretion of CRH and arginine-vasopressin (AVP) from the hypothalamus. This process initiates the production of adrenocorticotropic hormone (ACTH) from pituitary glands and subsequently induces the efflux of glucocorticoids from the adrenal gland. 140 During a stress response, glucocorticoids act as a potent anti-inflammatory factors and could regulate HPA axis activity in order to control the level of stress by a negative feedback mechanism. 139 The enhanced pro-inflammatory cytokines disrupt the regular function or hyper-activation of the HPA axis at any of its regulatory stages.139,141 HPA axis disturbances said to decrease the sensitivity of glucocorticoids receptor, thus inhibiting the negative feedback regulation and immune system, 142 which further leads to the hyper-activation of the HPA axis. Studies reported an elevated cortisol level and increased concentration of CRH in body fluids of depressive individuals. Also, a higher concentration of circulating cortisol was observed among patients, which could increase the levels of ACTH, 143 resulting in enhanced release of glucocorticoids. Reports have also revealed that patients undergoing interferon-α therapy developed depressive symptoms due to the hyperactivity of the HPA axis. 144
Furthermore, other mechanisms like altered monoamine metabolism, reduced vague nerve activity were reported to be involved in the mood disorders due to inflammatory responses. In addition, they could also induce the dysregulation of prefrontal cortex in the limbic system which further results in suicidal behavior. 132 Dysregulation of the serotonin system is also considered a very essential factor underlying suicidal ideation. 24 With this, inflammatory cytokines act as an essential trigger to incite the development of mood-related disorders and suicidal behavior. 124 Studies have reported that the increased level of IL-β, IL-6, IL 2R, IL 10, IFN)-γ, granulocyte colony-stimulating factor (G-CSF), monocyte chemoattractant protein 1 (MCP1), macrophage inflammatory protein 1 α (MIP1α), TNF-α,C-X-C motif chemokine ligand 10 (CXCL10), and chemokine (C-C motif) ligand 2 (CCL2) in the patients affected with Covid-19, MERS and SARS which further believed to induce the activation of T1 helper cell. However, IL-4 and IL2 levels were also high in case of Covid-19 patients which is responsible for the T2 helper cell activation. 145 The occurrence of cytokine storm among the Covid-19 patients reported by several studies could be due to the positive feedback mechanism induced by inflammatory factors released during the infection. 146 Collective evidence have clearly explained the prominent part of pro-inflammatory cytokines in the undesired condition of suicidal behavior and depression states.
Medications
Since the mood disorders are believed to be the major underlying cause for suicide, treating them clinically would reduce the risk of suicide. Hence, clinical interventions in the biological aspects are highly important factors to be addressed in order to prevent suicidal risks. Though both pharmaco-therapy and psychotherapy are considered to be equally effective, studies have found that combining antipsychotic drugs along with psychotherapy offered better efficacy than individual therapy. 147 The administration of antidepressants could activate monamines including serotonin and also enhance BDNF expression that can improve the neurotransmission, synaptic plasticity and the mental status of wellbeing as well. 148 Cotinine, an alkaloid obtained from leaves of tobacco has anxiolytic, antidepressant, and antipsychotic properties and modulates the serotonergic, dopaminergic, and cholinergic systems. In both neurological and psychiatric conditions the anti-inflammatory effects of cotinine decreases neuroinflammation. 149 Additionally, anti-inflammatory drugs such as TNF, aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), as well as omega-3 fatty acids were widely used. 150 In patients suffering from major depression, Riluzole (FDA approved drug) is used to up-regulate the receptors of GFAP. 151 Ceftriaxone, a clinically available drug shows an antidepressant activity by increasing glutamate transport. 152 Mood disorders caused due to changes in the regulation of inflammation could be treated with anti-inflammatory drugs that could help to bring down the inflammation and further to reduce the depressive symptoms and suicidal thoughts. Acetylsalicylic acid and cyclooxygenase-2 (COX-2) inhibitors can potentially induce anti-inflammatory effects by inhibiting one of the mediators of inflammation like prostaglandin E2. 153 Another drug, Tocilizumab could target IL-6 by preventing the interaction of IL-6 to its respective receptors thus hindering the subsequent inflammatory responses. Lithium, a potential anti-inflammatory agent targets the GSK3 which is involved in the increased production of pro-inflammatory cytokine. 24 Melatonin, a sleep regulatory hormone is also being recommended as an additional treatment for Covid-19 patients as it is considered to reduce the anti-inflammatory cytokines in an efficient manner. 154
During this Covid-19 pandemic, it is essential to keep track of the psychological behaviors of the patients as stress induced elevated inflammation developed during the disease or even the infection itself may lead to mood-related disorders and suicide risks. Patients with previous psychological predisposition factors are to be keenly observed. Targeting the factors involved in the signaling cascade of neuro-inflammation would improve the therapeutic implications for psychological and mood-related disorders.
Possible Prevention Strategies
Mental health problems, prevalence of PTSD more than depressive disorder, may be are long-term sequelae of an epidemic. The WHO recommends to everyone not to monitor the continuous stream of news reports which exacerbates stress and they also suggests that there should be specific time intervals for getting news update and not to trust the rumors. 155 The most important measures to improve psychosocial behavior include regular exercise, balanced nutrition and sleep. It is also necessary that to maintain a strong bonding with families and communities by any medium that could dramatically increase the positive energy and thinking. 13 Telemedicine (online) system offers psychological support from health care professionals to interact and offer constant support to peoples who are showing suicidal behavior (ie, worried, talking about dying, feeling hopeless/worthless). The necessities of life, such as food and medicine, during the lockdown condition should be given to the stressed. 5 Psychiatrists should provide counseling and awareness among people, their families about the stress and fear developed during pandemic times, and train them to overcome it. Quarantine and isolation have a drastic effect on victims and hence, an alternative mechanism to connect people, primarily through the web, might be helpful to reduce the psychological distress and suicidal ideation. 156 Studies reported that psychotherapy via video-conference also believe to improve the adjustment disorders in individuals. The Covid-19 disease acted as a major catalyst for the execution of online therapy and e-health tools for routine medical practices than 2 decades were most of the attempts failed in this regard. 157 In order to reduce the patient visits to hospital as that may enhance the possibility of infection, UK and USA recommended to use video consultation. Most of the countries do not have administrative systems to approve and coordinate telemedicine services under such emergency and or pandemic situations. 158 Helpline will offer more supports to the individuals who are more prone to suicide ideation. Digital training should be provided to volunteers who were not having enough experience on handling such peoples. 31
New York, implemented various health care programs such as programs of assertive community treatment (PACT) that focuses on managing the Covid-19 response protocols including housing facilities, mental health support, creating awareness regarding prevention, social distancing and assessing the epidemiological risk of Covid-19. 159 These kind of monitoring programs are highly necessary from community level in order to capture the true incidence as self-damage is mostly hidden. 160 In Brazil, community HCWs mostly in the age of 18 to 30 years which are less prone to serious consequences are provided with training for 3 to 4 weeks to promote health care activities and awareness among public. Community HCWs are recommended to ensure the hygienic conditions and proper supply of food and medicines among the patients as well as monitoring the psychological health which might help to identify vulnerable groups especially with weaker mental health. 161
While focusing on the health of a country, we should pay special attention to mental behavioral health among public, medical practitioners and HCWs. The general recommendation is to provide constant psychological support, proper information about the outbreak, intensive training, availability of PPE, infection control measures. And also there should be strong consideration need to be given on various factors associated to reduce the level of psychological stress among HCWs. 57 Several PFA models are designed and readily available to reduce the acute stress developed during emergencies which are delivered through telemedicine. 156 A study in which implementation of PFA, among HCWs in UK suggested that the usage of the digital package could improve the emotional status as well as displayed wide usability, practicality, and cost effectiveness. 162 A transparent and constant update regarding the prevalence of epidemic among HCWs and updating the status of attending patient health is also believed to be highly essential. The higher officials should provide constant support to ensure that the HCWs are getting sufficient rest (between shifts), nutritious food and keep in touch with their loved ones/family through any kind of available sources including digital platforms. There should be a regular monitoring of depression, anxiety, post-traumatic stress symptoms, psychotic symptoms and suicidal thoughts among the suspected, diagnosed patients, and health care professionals by mental HCWs. It is necessary to provide psychological assistance as well as value the workers who fall into the category of risk group by exposing themselves for the society.65,155,163
During and after pandemic times, the behavioral health should be considered as an important factor along with providing treatment. To fight against Covid-19 effectively, everyone should be aware of the current situation and implemented measures like quarantine and social distancing for the betterment of the individual and society. The development of psychological distress is common during any biological disaster and mental health assessment, proper support, and treatment are deemed to be necessary to fight against conditions like Covid-19. Special attention must be provided to vulnerable groups such as peoples with psychological disorders.164,165 Considering the psychological impact caused by the current Covid-19, the higher health administration should appoint more psychiatric teams and corresponding health centers to reduce the emotional distress among public due to pandemic. Regular monitoring of the frontline health care workers is also very highly essential as they are more prone to psychological stress due to the asymptomatic nature of the patients, workload, insufficient PPE kits, and lack of support. One of the major concern with Covid-19 is the lack of knowledge on the neuro-invasive nature and neuropsychiatric effects. It will take many more years to get substantial knowledge on the post-infectious neuropsychiatric effects of Covid-19. 166
Some general guidelines are available but a complete strategies or universal protocol to overcome the psychosocial impact to face the pandemic situation is still unknown. There is an urgent need of mental health policies by mental health professionals to be implemented by various organizations in accordance with epidemic and pandemic situations.12,167 The advancement of strategies and complete execution of the policies requires a complete knowledge on the epidemiology and the association of the disease with mental health as well as the risk of suicide which are not understood yet. Performing good quality research to identify suicide prevention research is a challenging one. The collaboration between countries and organization will facilitate a working together mechanism and pool up of various protocols and outcomes of research that may prevent suicidal thoughts and executions. International Association for Suicide Prevention (IASP) collaborates with various organizations such as WHO and provide the data of timely research regarding suicide and prevention protocols globally. 168 Pandemic poses great challenges to the society as well as public health and the effects are prolonged with a major risk factor being suicide. Suicide resulting from the fear of Covid-19 is preventable and research should be encouraged on these areas and we might need more strategies to face any emergency pandemic situations like Covid-19.
Limitations of the Review
Although this review comprehends the factors involved in suicidal behavior, the nature of the review being narrative, the method of selecting reference articles was subjective based on the topic. The characterization of studies specifying inclusion, exclusion criteria, and other selection criteria is also limited. Mostly, psychological measurement studies appear to be cross-sectional and hence we face some limitations that arise due to its observational nature as it does not permit understanding the causality. Most of these studies are conducted via online mode to prevent possible Covid-19 transmission. Hence, there may be a possibility for some bias. Another potential prejudice is the self-administered nature of the surveys and data integrity as there is less scope for verification of the information. 64 Studies comparison to conclude could be difficult due to the sample size variation and varying generalizations among countries to derive assessments of health problems. The current knowledge regarding the neurobiology of suicide continues to be incomplete due to highly complex nature of the nervous system and technical limitations. Moreover, the neurobiology field is overwhelmed by a lack of unifying theory, thus literature emphasized different aspects of similar neural circuits. 169 Suicide attempt methods, their comorbidities, and pre-medical history differs for each and every individual and thereby influencing the inflammatory profile accordingly. 109 Patients under medications of inflammatory drugs or psychotropic drugs tend to show differences in the inflammatory profile. Likewise, the mechanisms of inflammation-inducing pathways are still not very well explored. Therefore, considering these limitations some believe that it may not significantly effective to conclude the exact role of inflammatory biomarkers in suicide. 170 The suicide victims normally suffer from a variety of psychiatric disorders other than biological abnormalities. Therefore, it is important to examine the particular cause of death with a specific diagnosis and post-mortem brain samples from subjects with that particular diagnosis who died of natural causes. Undeniably, post-mortem brain studies tend to give sufficient opportunities and insights into the neurobiology of suicide, and these studies are likely to grow extensively within the near future. 49
Conclusion
Globally, suicide has taken a very heavy toll on our society due to various reasons, yet the pandemic related suicides are very new trend and not well documented at all. The implementation of innovative infection control measures has triggered the development of psychological distress among the common public. The imbalance of different psychobiological factors believed to accelerate the conversion of fear to suicide. Early diagnosis of a psychological crisis may address or avoid unwanted suicidal ideations. Therefore, intricate studies of these biological factors, along with proper treatment plans, might be able to prevent suicidal deaths. This study further recommends that the behavioral and molecular investigation after the post-pandemic period could be helpful to reduce suicidal ideation in high-risk individuals who have experienced enormous stress, fear, and anxiety during the pandemic. Understanding and mapping the major risk factors might also help to address the psychological health issues at earlier stages as this problem is being overlooked. Though the suicidal occurrence during the pandemic is increasing at steep and an alarming rate, lack of definite mental wellbeing guidelines to equip the general public, healthcare staff and patients during a pandemic disease makes the current status even worse. This paper reviewed the factors and the existing preventive suicidal measures, suggesting to handle the psychosocial issues of vulnerable population through interdisciplinary approaches and to frame effective psychological strategic approach specifically for a pandemic situation in order to avoid the surge in suicidal deaths. This review also established that the alternations in kynurenine (KYN) pathway and imbalance in inflammatory cytokines could be the key reasons for the prolonged psychological distress and subsequent suicidal act. Studying brain-neurological factors may also help us to understand the risk of acquiring suicidal pathophysiology.
Acknowledgments
The authors want to thank their respective institutions for their continued support. The author Dr Subramaniam Sadhasivam acknowledges DBT, Government of India for the financial support provided by the Ramalingaswami Re-entry fellowship (Order No.BT/RLF/Re-entry/55/2013). The authors highly acknowledge The Editing Refinery, MD, USA, for providing language and technical editing support.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author Contributions: CD, MP, RB, and SA performed research and collected information, and generated short write-ups. SS, MME, GJG, SBC, BAB, and MWQ conceptual work, framework, draft write-up, critical reading, and editing. All authors read and approved the final manuscript.
ORCID iDs: Musthafa Mohamed Essa  https://orcid.org/0000-0001-7505-9785
https://orcid.org/0000-0001-7505-9785
Gilles J Guillemin  https://orcid.org/0000-0001-8105-4470
https://orcid.org/0000-0001-8105-4470
Availability of Data and Materials: This is a review article. All data generated or analyzed during this study are included in this published article.
References
- 1. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71-76. doi: 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang W, Zhao Y, Zhang F, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the experience of clinical immunologists from China. Clin Immunol. 2020;214:108393. doi: 10.1016/j.clim.2020.108393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shereen MA, Khan S, Kazmi A, et al. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91-98. doi: 10.1016/j.jare.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roy D, Tripathy S, Kar SK, et al. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J Psychiatr. 2020. a;51:102073. doi: 10.1016/j.ajp.2020.102073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Usman N, Mamun MA, Ullah I. COVID-19 infection risk in Pakistani health-care workers: the cost-effective safety measures for developing countries. Social Health Behav. 2020;3:75-77. doi: 10.4103/SHB.SHB_26_20 [DOI] [Google Scholar]
- 7. Muthuraman S, Al Haziazi M. COVID-19 impact on health, social & economy. Int J Nutr Pharmacol Neurol Dis. 2020;10:159-160. doi: 10.4103/ijnpnd.ijnpnd_64_20 [DOI] [Google Scholar]
- 8. Subramanian S, Mohamed S, Khanzadah T. The coronavirus’ impact on education − school students’ perspective. Int J Nutr Pharmacol Neurol Dis. 2020;10:166-167. doi: 10.4103/ijnpnd.ijnpnd_59_20 [DOI] [Google Scholar]
- 9. Fernandes AJ. Impact of COVID-19: university students’ perspective. Int J Nutr Pharmacol Neurol Dis. 2020;10:168-169. [Google Scholar]
- 10. Al-Balushi B, Essa MM. The impact of COVID-19 on children − parent’s perspective. Int J Nutr Pharmacol Neurol Dis. 2020;10:164-165. doi: 10.4103/ijnpnd.ijnpnd_55_20 [DOI] [Google Scholar]
- 11. Prabhakar P, Punnaveetil S. COVID-19 impact − a physician’s perspective. Int J Nutr Pharmacol Neurol Dis. 2020;10:161-163. doi: 10.4103/ijnpnd.ijnpnd_62_20 [DOI] [Google Scholar]
- 12. Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-229. doi: 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim SW, Su KP. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. 2020;87:4-5. doi: 10.1016/j.bbi.2020.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahorsu DK, Lin CY, Imani V, et al. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020:1-9. doi: 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Valdés-Florido MJ, López-Díaz Á, Palermo-Zeballos FJ, et al. Reactive psychoses in the context of the COVID-19 pandemic: clinical perspectives from a case series. Rev Psiquiatr Salud. 2020;13:90-94. doi: 10.1016/j.rpsm.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mamun MA, Griffiths MD. A rare case of Bangladeshi student suicide by gunshot due to unusual multiple causalities. Asian J Psychiatr. 2020. b;49:101951. doi: 10.1016/j.ajp.2020.101951 [DOI] [PubMed] [Google Scholar]
- 17. Ross M. Suicide prevention methods within a modern-day society: focusing on mental health in our school prevention programs. Integr Stud. 2019;186. https://digitalcommons.murraystate.edu/bis437/186. [Google Scholar]
- 18. Wu CY, Lee MB, Liao SC, et al. Psychological distress of suicide attempters predicts one-year suicidal deaths during 2007-2016: a population-based study. J Formos Med Assoc. 2020;119:1306-1313. doi: 10.1016/j.jfma.2020.04.033 [DOI] [PubMed] [Google Scholar]
- 19. Lee H, Jung J, Myung W, et al. Association between dust storm occurrence and risk of suicide: case-crossover analysis of the Korean national death database. Environ Int. 2019;133:105146. doi: 10.1016/j.envint.2019.105146 [DOI] [PubMed] [Google Scholar]
- 20. Buckner JD, Lewis EM, Tucker RP. Mental health problems and suicide risk: the impact of acute suicidal affective disturbance. Arch Suicide Res. 2019;24:303-313. doi: 10.1080/13811118.2019.1574688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fässberg MM, Cheung G, Canetto SS, et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment Health. 2016;20:166-194. doi: 10.1080/13607863.2015.1083945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Turecki G. The molecular bases of the suicidal brain. Nat Rev Neurosci. 2014;15:802-816. doi: 10.1038/nrn3839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Turecki G, Ernst C, Jollant F, et al. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012;35:14-23. doi: 10.1016/j.tins.2011.11.008 [DOI] [PubMed] [Google Scholar]
- 24. Brundin L, Bryleva EY, Rajamani KT. Role of inflammation in suicide: from mechanisms to treatment. Neuropsychopharmacology. 2017;42:271-283. doi: 10.1038/npp.2016.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. LeCloux MA, Weimer M, Culp SL, et al. The feasibility and impact of a suicide risk screening program in rural adult primary care: a pilot test of the ask suicide-screening questions toolkit. Psychosomatics. 2020;61:698-706. doi: 10.1016/j.psym.2020.05.002 [DOI] [PubMed] [Google Scholar]
- 26. Dandona R, Kumar GA, Dhaliwal RS, et al. Gender differentials and state variations in suicide deaths in India: the Global Burden of Disease Study 1990-2016. Lancet Public Health. 2018;3:e478-e489. doi: 10.1016/S2468-2667(18)30138-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2014;192:98-105. doi: 10.1192/bjp.bp.107.040113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pulay AJ, Réthelyi JM. Multimarker analysis suggests the involvement of BDNF signaling and microRNA biosynthesis in suicidal behavior. Am J Med Genet. 2016;171:763-776. doi: 10.1002/ajmg.b.32433 [DOI] [PubMed] [Google Scholar]
- 29. Chan SMS, Chiu FKH, Lam CWL, et al. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry. 2006;21:113-118. doi: 10.1002/gps.1432 [DOI] [PubMed] [Google Scholar]
- 30. Kumar M, Wani AA, Devi S, et al. Coronavirus diseasae (COVID-19) psychological, behavioural and interpersonal impacts of infectious diseases outbreaks: a review. Asian J Med Sci. 2020;2:1-5. https://mbimph.com/index.php/AJOAIMS/article/view/1528. [Google Scholar]
- 31. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468-471. doi: 10.1016/S2215-0366(20)30171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wand APF, Zhong BL, Chiu HFK, et al. Covid-19: the implications for suicide in older adults. Int Psychogeriatr. 2020;32:1225-1230. doi: 10.1017/S1041610220000770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dsouza DD, Quadros S, Hyderabadwala ZJ, et al. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020;290:113145. doi: 10.1016/j.psychres.2020.113145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. The Economic Times. Suicide leading cause for over 300 lockdown deaths in India: study. 2020. Updated May 4, 2020. Accessed July 1, 2020. https://www.newindianexpress.com/nation/2020/may/04/suicide-leading-cause-for-over-300-lockdown-deaths-in-india-study-2138877.html
- 35. Goyal K, Chauhan P, Chhikara K, et al. Fear of COVID 2019: first suicidal case in India! Asian J Psychiatr. 2020;49:101989. doi: 10.1016/j.ajp.2020.101989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. The Times of India. Covid-19: corona fear drives two to suicide in UP. 2020. Updated March 23, 2020. Accessed April 17, 2020. https://timesofindia.indiatimes.com/city/lucknow/corona-fear-drives-two-to-suicide-in-up/articleshowprint/74768582.cms
- 37. The New Indian Express. Elderly man in coronavirus isolation ward commits suicide in Ariyalur General Hospital. 2020. Updated April 10, 2020. Accessed April 17, 2020. https://www.newindianexpress.com/states/tamil-nadu/2020/apr/10/elderly-man-in-coronavirus-isolation-ward-commits-suicide-in-ariyalur-general-hospital-2128486.html
- 38. Sahoo S, Rani S, Parveen S, et al. Self-harm and COVID-19 pandemic: an emerging concern—a report of 2 cases from India. Asian J Psychiatr. 2020;51:102104. doi: 10.1016/j.ajp.2020.102104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Halford E, Dixon A, Farrell G, et al. Crime and coronavirus: social distancing, lockdown, and the mobility elasticity of crime. Crime Sci. 2020;9:1-12. doi: 10.1186/s40163-020-00121-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nelson PA, Adams SM. Primary cares’ role in suicide prevention during the COVID-19 pandemic. J Nurse Pract. 2020;16;654-659. doi: 10.1016/j.nurpra.2020.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rahman A, Plummer V. COVID-19 related suicide among hospital nurses; case study evidence from worldwide media reports. Psychiatry Res. 2020;291:113272. doi: 10.1016/j.psychres.2020.113272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Singh R, Baral KP, Mahato S. An urgent call for measures to fight against increasing suicides during COVID-19 pandemic in Nepal. Asian J Psychiatr. 2020;54:102259. doi: 10.1016/j.ajp.2020.102259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Griffiths MD, Mamun MA. COVID-19 suicidal behavior among couples and suicide pacts: case study evidence from press reports. Psychiatry Res. 2020;289:113105. doi: 10.1016/j.psychres.2020.113105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. New York Post. British teen dies after suicide attempt due to coronavirus fears. 2020. Updated 2020. Accessed April 17, 2020. https://nypost.com/2020/03/25/british-teen-dies-after-suicide-attempt-due-to-coronavirus-fears/
- 46. New York Post. Italian nurse with coronavirus kills herself over fear of infecting others. 2020. Updated March 25, 2020. Accessed April 17, 2020. https://nypost.com/2020/03/25/italian-nurse-with-coronavirus-kills-herself-amid-fears-of-infecting-others/
- 47. The Sun. Nurse in her 20s ‘kills herself’ at London hospital where eight coronavirus patients have died. 2020. Updated March 25, 2020. Accessed April 17, 2020. https://www.thesun.co.uk/news/11249067/nurse-kills-herself-london-hospital/
- 48. The Local. German minister commits suicide after ‘crisis over coronavirus worries’. 2020. Updated March 29, 2020. Accessed April 17, 2020. https://www.thelocal.de/20200329/german-minister-commits-suicide-due-to-coronavirus-worries
- 49. Pandey GN, Dwivedi Y. What can post-mortem studies tell us about the pathoetiology of suicide? Future Neurol. 2010;5:701-720. doi: 10.2217/fnl.10.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7:105-110. doi: 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- 51. Sim M. Psychological trauma of Middle East Respiratory Syndrome victims and bereaved families. Epidemiol Health. 2016;38:e2016054. doi: 10.4178/epih.e2016054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pappas G, Kiriaze IJ, Giannakis P, et al. Psychosocial consequences of infectious diseases. Clin Microbiol Infect. 2009;15:743-747. doi: 10.1111/j.1469-0691.2009.02947.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. Plos One. 2020;15:e0231924. doi: 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mak IWC, Chu CM, Pan PC, et al. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-326. doi: 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lin K, Yang BX, Luo D, et al. The mental health effects of COVID-19 on health care providers in China. Am J Psychiatry. 2020;177:635-636. doi: 10.1176/appi.ajp.2020.20040374 [DOI] [PubMed] [Google Scholar]
- 56. Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302-311. doi: 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Koh D, Lim MK, Chia SE, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore what can we learn? Med Care. 2005;676-682. http://www.jstor.com/stable/3768367. [DOI] [PubMed]
- 58. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173:317-320. doi: 10.7326/M20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wilson W, Raj JP, Rao S, et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J Psychol Med. 2020;42:353-358. doi: 10.1177/0253717620933992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zhu Z, Xu S, Wang H, et al. COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. Preprint. Posted online March 16, 2020. MedRxiv. doi: 10.1101/2020.02.20.20025338 [DOI] [Google Scholar]
- 61. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Du J, Dong L, Wang T, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. Published online April 3, 2020. S0163-8343(20)30045-1. doi: 10.1016/j.genhosppsych.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp. Psychiatry. 2020;66;1-8. doi: 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Chew NW, Lee GK, Tan BY, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-565. doi: 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. de Burgos-Berdud I, Valdés-Florido MJ, López-Díaz Á. Are healthcare workers during the COVID-19 pandemic at risk of psychosis? Findings from a scoping review. Gen Hosp Psychiatry. 2020;20:300992. doi: 10.1016/j.genhosppsych.2020.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020a;7:e15-e16. doi: 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Shah K, Kamrai D, Mekala H, et al. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12:e7405. doi: 10.7759/cureus.7405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003; 60:184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 69. Girgis RR. The neurobiology of suicide in psychosis: a systematic review. J Psychopharmacol. 2020;34:811-819. doi: 10.1177/0269881120936919 [DOI] [PubMed] [Google Scholar]
- 70. O’Connor DB, Gartland N, O’Connor RC. Stress, cortisol and suicide risk. Int Rev Neurobiol. 2020;152:101-130. doi: 10.1016/bs.irn.2019.11.006 [DOI] [PubMed] [Google Scholar]
- 71. Van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry. 2014;1:63-72. doi: 10.1016/S2215-0366(14)70220-2 [DOI] [PubMed] [Google Scholar]
- 72. Van Heeringen K. The neurobiology of suicide and suicidality. Can J Psychiatry. 2003;48:292-300. doi: 10.1177/070674370304800504 [DOI] [PubMed] [Google Scholar]
- 73. Ludwig B, Roy B, Wang Q, et al. The life span model of suicide and its neurobiological foundation. Front Neurosci. 2017;11:74. doi: 10.3389/fnins.2017.00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Van Heeringen C, Marušic A. Understanding the suicidal brain. Br J Psychiatry. 2003;183:282-284. doi: 10.1192/bjp.183.4.282 [DOI] [PubMed] [Google Scholar]
- 75. Karege F, Vaudan G, Schwald M, et al. Neurotrophin levels in postmortem brains of suicide victims and the effects of antemortem diagnosis and psychotropic drugs. Mol Brain Res. 2005;136:29-37. doi: 10.1016/j.molbrainres.2004.12.020 [DOI] [PubMed] [Google Scholar]
- 76. Hong CJ, Huo SJ, Yen FC, et al. Association study of a brain-derived neurotrophic-factor genetic polymorphism and mood disorders, age of onsetandsuicidal behavior. Neuropsychobiology. 2003;48:186-189. doi: 10.1159/000074636 [DOI] [PubMed] [Google Scholar]
- 77. Pandey GN, Dwivedi Y, Rizavi HS, et al. Brain-derived neurotrophic factor gene and protein expression in pediatric and adult depressed subjects. Prog Neuro Psychoph. 2010;34:645-651. doi: 10.1016/j.pnpbp.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 78. Rasmussen P, Brassard P, Adser H, et al. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp Physiol. 2009;94:1062-1069. doi: 10.1113/expphysiol.2009.048512 [DOI] [PubMed] [Google Scholar]
- 79. Chen ZY, Jing D, Bath KG, et al.Genetic variant BDNF (Val66Met) polymorphism alters anxiety-related Behavior. Science. 2006;314:140-143. doi: 10.1126/science.1129663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Lu B. Pro-region of neurotrophins: role in synaptic modulation. Neuron. 2003;39:735-738. doi: 10.1016/S0896-6273(03)00538-5 [DOI] [PubMed] [Google Scholar]
- 81. Al-Qudah MA, Al-Dwairi A. Mechanisms and regulation of neurotrophin synthesis and secretion. Neurosciences. 2016;21:306. doi: 10.17712/nsj.2016.4.20160080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Zarrilli F, Angiolillo A, Castaldo G, et al. Brain derived neurotrophic factor (BDNF) genetic polymorphism (Val66Met) in suicide: a study of 512 cases. Am J Med Genet B Neuropsychiatr Genet B. 2009;150:599-600. doi: 10.1002/ajmg.b.30849 [DOI] [PubMed] [Google Scholar]
- 83. Hashimoto K. BDNF variant linked to anxiety-related behaviors. BioEssays. 2007;29:116-119. doi: 10.1002/bies.20534 [DOI] [PubMed] [Google Scholar]
- 84. Shen T, You Y, Joseph C, et al. BDNF polymorphism: a review of its diagnostic and clinical relevance in neurodegenerative disorders. Aging Dis. 2018;9:523.doi: 10.14336/AD.2017.0717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Dwivedi Y. Brain-derived neurotrophic factor and suicide pathogenesis. Ann Med. 2010;42:87-96. doi: 10.3109/07853890903485730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. McKernan DP, Dinan TG, Cryan JF. “Killing the Blues”: a role for cellular suicide (apoptosis) in depression and the antidepressant response? Prog Neurobiol. 2009;88:246-263.doi: 10.1016/j.pneurobio.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 87. Sadkowski M, Dennis B, Clayden RC, et al. The role of the serotonergic system in suicidal behavior. Neuropsychiatr Dis Treat. 2013;9:1699-1716. doi: 10.2147/NDT.S50300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Pompili M, Serafini G, Innamorati M, et al. The hypothalamic–pituitary–adrenal axis and serotonin abnormalities: a selective overview for the implications of suicide prevention. Eur Arch Psy Clin Neurosci. 2010;260:583-600.doi: 10.1007/s00406-010-0108-z [DOI] [PubMed] [Google Scholar]
- 89. Asberg M, Thorén P, Träskman L, et al. “Serotonin depression”–a biochemical subgroup within the affective disorders? Science. Feb 6, 1976;191(4226):478-480. doi:10.1126/science.1246632 [DOI] [PubMed] [Google Scholar]
- 90. Purselle DC, Nemeroff CB. Serotonin transporter: a potential substrate in the biology of suicide. Neuropsychopharmacology. 2003;28:613-619.doi: 10.1038/sj.npp.1300092 [DOI] [PubMed] [Google Scholar]
- 91. Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467-477. doi: 10.1016/S0893-133X(00)00228-1 [DOI] [PubMed] [Google Scholar]
- 92. Mann JJ, Currier DM. Stress, genetics and epigenetic effects on the neurobiology of suicidal behavior and depression. Eur Psychiatry.2020;25:268-271. doi: 10.1016/j.eurpsy.2010.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Choudary PV, Molnar M, Evans SJ, et al. Altered cortical glutamatergic and GABAergic signal transmission with glial involvement in depression. PNAS. 2005;102:15653-15658. doi: 10.1073/pnas.0507901102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sequeira A, Mamdani F, Ernst C, et al. Global brain gene expression analysis links glutamatergic and GABAergic alterations to suicide and major depression. PLoS One. 2009;4:e6585. doi: 10.1371/journal.pone.0006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Castegna A, Aksenov M, Aksenova M, et al. Proteomic identification of oxidatively modified proteins in Alzheimer’s disease brain. Part I: creatine kinase BB, glutamine synthase, and ubiquitin carboxy-terminal hydrolase L-1. Free Radic Biol Med. 2002;33:562-571. doi: 10.1016/S0891-5849(02)00914-0 [DOI] [PubMed] [Google Scholar]
- 96. Zhao J, Verwer RWH, Gao SF, et al. Prefrontal alterations in GABAergic and glutamatergic gene expression in relation to depression and suicide. J Psychiatry Res. 2018;102:261-274. doi: 10.1016/j.jpsychires.2018.04.020 [DOI] [PubMed] [Google Scholar]
- 97. Mele M, Costa RO, Duarte CB. Alterations in GABAA-receptor trafficking and synaptic dysfunction in brain disorders. Front Cell Neurosci. 2019;13:77. doi: 10.3389/fncel.2019.00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Roy B, Wang Q, Palkovits M, et al. Altered miRNA expression network in locus coeruleus of depressed suicide subjects. Sci Rep. 2017;7:1-15. doi: 10.1038/s41598-017-04300-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Chandley MJ, Ordway GA. Noradrenergic dysfunction in depression and suicide. In: The neurobiological basis of suicide. CRC Press/Taylor & Francis, 2012. https://www.ncbi.nlm.nih.gov/books/NBK107205/. [PubMed]
- 100. Zhou BY, Liu Y, oh Kim B, et al. Astrocyte activation and dysfunction and neuron death by HIV-1 Tat expression in astrocytes. Mol Cell Neurosci. 2004;27:296-305. doi: 10.1016/j.mcn.2004.07.003 [DOI] [PubMed] [Google Scholar]
- 101. Zhou X, Xiao Q, Xie L, et al. Astrocyte, a promising target for mood disorder interventions. Front Mol Neurosci. 2019;12:136. doi: 10.3389/fnmol.2019.00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Cotter DR, Pariante CM, Everall IP. Glial cell abnormalities in major psychiatric disorders: the evidence and implications. Brain Res Bull. 2001;55:585-595. doi: 10.1016/S0361-9230(01)00527-5 [DOI] [PubMed] [Google Scholar]
- 103. Banasr M, Chowdhury GMI, Terwilliger R, et al. Glial pathology in an animal model of depression: reversal of stress-induced cellular, metabolic and behavioral deficits by the glutamate-modulating drug riluzole. Mol Psychiatry. 2010;15:501-511. doi: 10.1038/mp.2008.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Rajkowska G, Stockmeier CA. Astrocyte pathology in major depressive disorder: insights from human postmortem brain tissue. Curr Drug Targets. 2013;14:1225-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Batty GD, Bell S, Stamatakis E, et al. Association of systemic inflammation with risk of completed suicide in the general population. JAMA Psychiatry. 2016;73:993-995. doi: 10.1001/jamapsychiatry.2016.1805 [DOI] [PubMed] [Google Scholar]
- 106. Keaton SA, Madaj ZB, Heilman P. An inflammatory profile linked to increased suicide risk. J Affect Disord. 2019;247:57-65.doi: 10.1016/j.jad.2018.12.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Brundin L, Erhardt S, Bryleva EY. The role of inflammation in suicidal behaviour. Acta Psychiatr Scand. 2015;132:192-203. doi: 10.1111/acps.12458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Gibbs HM, Davis L, Han X, et al. Association between C-reactive protein and suicidal behavior in an adult inpatient population. J Psychiatr Res. 2016;79:28-33. doi: 10.1016/j.jpsychires.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 109. Serafini G, Pompili M, Seretti ME, et al. The role of inflammatory cytokines in suicidal behavior: a systematic review. Eur Neuropsychopharm. 2013; 23:1672-1686. doi: 10.1016/j.euroneuro.2013.06.002 [DOI] [PubMed] [Google Scholar]
- 110. Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;11:116832. doi: 10.1016/j.jns.2020.116832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ellul M, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurology. 2020.19:767-783. doi: 10.2139/ssrn.3589350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Ragab D, Salah Eldin H, Taeimah M, et al. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Varatharaj A, Thomas N, Ellul MA, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7:875-882. doi: 10.1016/S2215-0366(20)30287-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41:1089-1096. doi: 10.1086/444461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 | other coronaviruses. Brain Behav Immun. 2020(b);87:18-22. doi: 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Li H, Xue Q, Xu X. Involvement of the nervous system in SARS-CoV-2 infection. Neurotox Res. 2020;38:1-7. doi: 10.1007/s12640-020-00219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Bridwell R, Long B, Gottlieb M. Neurologic complications of COVID-19. Am J Emerg Med. 2020;38:1549.e3-1549.e7. doi: 10.1016/j.ajem.2020.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Panariello A, Bassetti R, Radice A, et al. Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: a case report. Brain Behav Immun. 2020;87:179-181. doi: 10.1016/j.bbi.2020.05.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Franke C, Ferse C, Kreye J, et al. High frequency of cerebrospinal fluid autoantibodies in COVID-19 patients with neurological symptoms. Preprint. Posted online July 6, 2020. MedRxiv. doi: 10.1101/2020.07.01.20143214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Anderson G. Psychological stress and Covid-19: interactions with gut microbiome and circadian rhythm in driving symptom severity. 2020. [Google Scholar]
- 121. Maes M, Song C, Lin A, et al. The effects of psychological stress on humans: increased production of pro-inflammatory cytokines and Th1-like response in stress-induced anxiety. Cytokine. 1998;10:313-318. doi: 10.1006/cyto.1997.0290 [DOI] [PubMed] [Google Scholar]
- 122. Singhal G, Baune BT. Inflammatory abnormalities in major depressive disorder. In: McIntyre RS, ed. Major Depressive Disorder. Elsevier; 2020; 75-89. doi: 10.1016/B978-0-323-58131-8.00006-9 [DOI] [Google Scholar]
- 123. Arbour N, Day R, Newcombe J, et al. Neuroinvasion by human respiratory coronaviruses. J Virol. 2000;74:8913-8921. doi: 10.1128/JVI.74.19.8913-8921.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Okusaga O, Yolken RH, Langenberg P, et al. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord. 2011;130:220-225. doi: 10.1016/j.jad.2010.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Cattaneo A, Macchi F, Plazzotta G, et al. Inflammation and neuronal plasticity: a link between childhood trauma and depression pathogenesis. Front Cell Neurosci. 2015;9:40. doi: 10.3389/fncel.2015.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Mendlovic S, Doron A, Eilat E. Short note: can depressive patients exploit the immune system for suicide? Med Hypotheses. 1997;49:445-446. doi: 10.1016/S0306-9877(97)90095-5 [DOI] [PubMed] [Google Scholar]
- 127. Jackson JC, Cross RJ, Walker RF, et al. Influence of serotonin on the immune response. Immunology. 1985;54:505. [PMC free article] [PubMed] [Google Scholar]
- 128. Tonelli LH, Stiller J, Rujescu D, et al. Elevated cytokine expression in the orbitofrontal cortex of victims of suicide. Acta Psychiatr Scand. 2008;117:198-206. doi: 10.1111/j.1600-0447.2007.01128.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Janelidze S, Suchankova P, Ekman A, et al. Low IL-8 is associated with anxiety in suicidal patients: genetic variation and decreased protein levels. Acta Psychiatr Scand. 2015;31:269-278. doi: 10.1111/acps.12339 [DOI] [PubMed] [Google Scholar]
- 130. Shinko Y, Otsuka I, Okazaki S, et al. Chemokine alterations in the postmortem brains of suicide completers. J Psychiatr Res. 2020;120:29-33. doi: 10.1016/j.jpsychires.2019.10.008 [DOI] [PubMed] [Google Scholar]
- 131. Farooq RK, Asghar K, Kanwal S, et al. Role of inflammatory cytokines in depression: focus on interleukin-1β. Biomed Rep. 2017;6:15-20. doi: 10.3892/br.2016.807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Maydych V. The interplay between stress, inflammation, and emotional attention: relevance for depression. Front Neurosci. 2019;13:384. doi: 10.3389/fnins.2019.00384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Jeon SW, Kim YK. Inflammation-induced depression: its pathophysiology and therapeutic implications. J Neuroimmunol. 2017;313:92-98. doi: 10.1016/j.jneuroim.2017.10.016 [DOI] [PubMed] [Google Scholar]
- 134. Bryleva EY, Brundin L. Kynurenine pathway metabolites and suicidality. Neuropharmacology. 2017;112:324-330. doi: 10.1016/j.neuropharm.2016.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Erhardt S, Lim CK, Linderholm KR, et al. Connecting inflammation with glutamate agonism in suicidality. Neuropsychopharmacology. 2013;38:743-752. doi: 10.1038/npp.2012.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Juhl JH. Fibromyalgia and the serotonin pathway. Altern Med Rev. 1998;3:367-375. [PubMed] [Google Scholar]
- 137. Schwieler L, Larsson MK, Skogh E, et al. Increased levels of IL-6 in the cerebrospinal fluid of patients with chronic schizophrenia—significance for activation of the kynurenine pathway. J Psychiatry Neurosci. 2015;40:126. doi: 10.1503/jpn.140126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Essa MM, Hamdan H, Chidambaram SB, et al. Possible role of tryptophan and melatonin in COVID-19. Int J Tryptophan Res. 2020;13:1-2. doi: 10.1177/1178646920951832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Silverman MN, Sternberg EM. Glucocorticoid regulation of inflammation and its behavioral and metabolic correlates: from HPA axis to glucocorticoid receptor dysfunction. Ann NY Acad Sci. 2012;1261:55. doi: 10.1111/j.1749-6632.2012.06633.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Zunszain PA, Anacker C, Cattaneo A, et al. Glucocorticoids, cytokines and brain abnormalities in depression. Prog Neuro Psychopharmacol Biol Psychiatry. 2011;35:722-729. doi: 10.1016/j.pnpbp.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Silverman MN, Pearce BD, Biron CA, et al. Immune modulation of the hypothalamic–pituitary–adrenal (HPA) axis during viral infection. Viral Immunol. 2005;18:41-78. doi: 10.1089/vim.2005.18.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Muneer A. Bipolar disorder: role of inflammation and the development of disease biomarkers. Psychiatry Investig. 2016;13:18. doi: 10.4306/pi.2016.13.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Pariante CM, Miller AH. Glucocorticoid receptors in major depression: relevance to pathophysiology and treatment. Biol Psychiatry. 2001;49:391-404. doi: 10.1016/S0006-3223(00)01088-X [DOI] [PubMed] [Google Scholar]
- 144. Capuron L, Ravaud A, Miller AH, et al. Baseline mood and psychosocial characteristics of patients developing depressive symptoms during interleukin-2 and/or interferon-alpha cancer therapy. Brain Behav Immun. 2004;18:205-213. doi: 10.1016/j.bbi.2003.11.004 [DOI] [PubMed] [Google Scholar]
- 145. Mazza MG, De Lorenzo R, Conte, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020.89:594-600. doi: 10.1016/j.bbi.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Vepa A, Bae JP, Ahmed F, et al. Diabetes & metabolic syndrome: clinical research & reviews COVID-19 and ethnicity: a novel pathophysiological role for inflammation. Diabetes Metab Syndr. 2020;14:1043-1051. doi: 10.1016/j.dsx.2020.06.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Mintz D. Combining drug therapy and psychotherapy for depression. Psychiatr Times. 2006;23:18-18. [Google Scholar]
- 148. Björkholm C, Monteggia LM. BDNF—a key transducer of antidepressant effects. Neuropharmacology. 2016;102:72-79. doi: 10.1016/j.neuropharm.2015.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Echeverria V, Alex Grizzell J, Barreto GE. Neuroinflammation: a therapeutic target of cotinine for the treatment of psychiatric disorders? Curr Pharm Des. 2016;22:1324-1333. doi: 10.2174/138161282210160304112511 [DOI] [PubMed] [Google Scholar]
- 150. Mitchell RH, Goldstein BI. Inflammation in children and adolescents with neuropsychiatric disorders: a systematic review. J Am Acad Child Adoles Psychiatry. 2014;53:274-296. doi: 10.1016/j.jaac.2013.11.013 [DOI] [PubMed] [Google Scholar]
- 151. Ernst C, Nagy C, Kim S, et al. Dysfunction of astrocyte connexins 30 and 43 in dorsal lateral prefrontal cortex of suicide completers. Biol Psychiatry. 2011;70:312-319. doi: 10.1016/j.biopsych.2011.03.038 [DOI] [PubMed] [Google Scholar]
- 152. Liu F, Wu J, Gong Y, et al. Harmine produces antidepressant-like effects via restoration of astrocytic functions. Prog Neuro Psychopath. 2017;79:258-267. doi: 10.1016/j.pnpbp.2017.06.012 [DOI] [PubMed] [Google Scholar]
- 153. Lotrich FE, El-Gabalawy H, Guenther LC, et al. The role of inflammation in the pathophysiology of depression: different treatments and their effects. J Rheumatol. 2011;88:48-54. 10.3899/jrheum.110903 [DOI] [PubMed] [Google Scholar]
- 154. Chen Y, Zhao A, Xia Y, et al. In the big picture of COVID-19 pandemic: what can sleep do. Sleep Med. 2020. b;72:109-110. doi: 10.1016/j.sleep.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. World Health Organization, 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. March 18, 2020. (No. WHO/2019-nCoV/MentalHealth/2020.1). World Health Organization. [Google Scholar]
- 156. Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Wind TR, Rijkeboer M, Andersson G, et al. The COVID-19 pandemic: the ‘black swan’for mental health care and a turning point for e-health. Internet Interv. 2020.20:100317. doi: 10.1016/j.invent.2020.100317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health and Surveillance. 2020;6:e18810. doi: 10.2196/18810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Bojdani E, Rajagopalan A, Chen A, et al. COVID-19 pandemic: impact on psychiatric care in the United States, a review. Psychiatry Res. 2020;289:113069. doi: 10.1016/j.psychres.2020.113069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020.7:547-560. doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Haines A, de Barros EF, Berlin A, et al. National UK programme of community health workers for COVID-19 response. Lancet. 2020;395:1173-1175. doi: 10.1016/S0140-6736(20)30735-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Blake H, Bermingham F, Johnson G, et al. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Env Res Pub He. 2020;17:2997. doi: 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531-542. doi: 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Onyeaka HK, Zahid S, Patel RS. The unaddressed behavioral health aspect during the coronavirus pandemic. Cureus. 2020;12:e7351. doi: 10.7759/cureus.7351.(155) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395: 912-920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Losilla-Rodríguez B, Maldonado N, Moreno-Mellado E, et al. COVID-19 natural herd immunity and risk of neuropsychiatric disorders. Rev Psiquiatr Salud Ment. 2020;11:228-229. doi: 10.1016/j.rpsm.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Ornell F, Schuch JB, Sordi AO, et al. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42:232-235. doi: 10.1590/1516-4446-2020-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Niederkrotenthaler T, Gunnell D, Arensman E, et al. Suicide research, prevention, and COVID-19. Int Assoc Suicide Prevent. 2020;41:321-330. doi: 10.1027/0227-5910/a000731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Luyten P, Fonagy P. The neurobiology of mentalizing. Pers Disord Theory Res Treat. 2015;6:366-379. doi: 10.1037/per0000117 [DOI] [PubMed] [Google Scholar]
- 170. O’Donovan A, Rush G, Hoatam G, et al. Suicidal ideation is associated with elevated inflammation in patients with major depressive disorder. Depress Anxiety. 2013;30:307-314. doi: 10.1002/da.22087 [DOI] [PubMed] [Google Scholar]