Summary
Background
Pregnant adolescent girls and young women (AGYW, aged 12–24 years) are at high risk for mental health problems, particularly in the Sub-Saharan African (SSA) region.
Methods
We performed a systematic review of mental health studies among pregnant AGYW in SSA published between January 1, 2007 and December 31, 2020 in PubMed, Embase, CINAHL, PsycInfo, and Global Index Medicus following PRISMA guidelines (PROSPERO: CRD42021230980). We used Bronfenbrenner's bioecological model to frame and synthesize results from included studies.
Findings
Our search yielded 945 articles from which 18 studies were included (N = 8 quantitative, N = 9 qualitative, N = 1 case report). The most frequently studied mental health problem was depression (N = 9 studies); the most frequently utilized measurement tool was the Edinburgh Postnatal Depression Scale (N = 3). Studies reported life course factors, individual, microsystem, exosystem, macrosystem, and chronosystem-level factors associated with mental health problems. Gaps in mental health service delivery for pregnant AGYW included lack of confidentiality, judgmental healthcare worker attitudes, and lack of services tailored to their unique needs.
Interpretation
Gaps remain in research and services for mental health among pregnant AGYW in SSA. Integration of mental health services within school, community, and healthcare settings that are tailored to pregnant AGYW could strengthen health systems within SSA.
Funding
Author contributions were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (F31HD101149 to AL) and the Fogarty International Center (K43TW010716 to MK). The funding agencies had no role in the writing of the manuscript or the decision to submit it for publication. The project itself was not funded.
Keywords: Mental health, Pregnant, Adolescents, Young women, Sub-Saharan Africa
Research in context.
Evidence before this study
Pregnant adolescent girls and young women (AGYW) living in low- and middle-income countries (LMICs) are disproportionately impacted by mental health issues due to higher prevalence, lower access to services, and stark systemic barriers of gender discrimination, stigma, and violence. We performed a systematic review according to PRISMA guidelines in five databases (PubMed, Embase, CINAHL, PsycInfo, and Global Index Medicus) focusing on mental health needs including service implementation gaps among pregnant AGYW in Sub-Saharan Africa (SSA) published between January 1, 2007- December 31, 2020. We developed a search strategy with terms adapted for each database including ‘young adult’, ‘adolescent’, ‘pregnancy’, mental health terms such as ‘anxiety’, ‘depression’, and ‘stress and trauma-related disorders’ and terms for methodologies and interventions such as ‘surveys’, ‘focus groups’, and ‘psychotherapy’. Studies were included if they met the following criteria: (1) involved pregnant AGYW aged 12–24 in Sub-Saharan Africa, and (2) focused on mental health problems, (3) were not published before 2007 or in non-English language, and we used Joanna Briggs Institute Quality Assessment Guidelines to appraise the selected studies.
Added value of this study
We found that substantial gaps remain in research and interventions tailored to this unique group. There were very few interventional studies identified, but the overall quality of the studies was reasonable. We were particularly struck by how insightful and detailed qualitative studies were in their description of sociocultural, economic and psychosocial, socioemotional factors. Regional evidence around AGYW's socio-ecological realms of development have been conducted, this has not translated into a sufficient appraisal of all possible mental health conditions or strategies for service improvement, or intervention development to address perinatal mental health among pregnant AGYW in SSA.
Implications of all the available evidence
Scaling up holistic mental health services integrated within school, community, and healthcare settings should be further tailored for this group to ensure privacy, dignity and quality care is offered in a youth friendly manner. Integrating tailored mental health services for pregnant adolescents and young women has the potential to improve maternal and child health as well as strengthen health systems in the sub-continent.
Alt-text: Unlabelled box
Introduction
Over 10% of pregnant women experience a mental disorder during pregnancy,1, 2, 3 and those in low- and middle-income countries (LMICs) are disproportionately impacted due to higher prevalence of mental health problems and lower access to mental health services.3, 4, 5, 6 Changes in reproductive and stress hormones induced by pregnancy, as well as innate genetic factors influence occurrence of maternal mental disorders, yet their specific processes are not fully determined.7
Adolescent girls and young women (AGYW; age 12–24) experience a period of major developmental and hormonal changes8 which add to the physiological and psychosocial alterations experienced in pregnancy.9,10 Frequency of perinatal mental health problems among pregnant and postpartum AGYW11 is up to 30% higher than their adult and non-pregnant counterparts.10,12, 13, 14, 15, 16, 17, 18, 19, 20 Almost all adolescent pregnancies (95%) worldwide occur in LMICs with the highest frequency in the Sub-Saharan African (SSA) region.9 Despite the intersecting burdens of antenatal mental health problems and high frequency of adolescent pregnancy, few data exist on maternal mental health among AGYW in Sub-Saharan Africa.6
Stress and adversities during pregnancy are associated with mental disorders, predominantly depression and anxiety.21, 22, 23, 24, 25 AGYW experience a unique combination of hormonal changes as well as life stressors related to school, relationship dynamics, unplanned pregnancies, societal norms, and transition to adulthood which put them at higher risk of mental disorders in general, and particularly during pregnancy.10 These unique circumstances exacerbate barriers to seeking and accessing mental health care such as lack of financial independence, stigma associated with adolescent pregnancy and mental disorders, and challenging parental and/or partner relationship dynamics.26 Consequently, available adult mental health services may not sufficiently address mental health challenges among pregnant AGYW.4,21
Research and implementation specifically focused on alleviating mental health problems among AGYW is scarce in the African region, despite disproportionate impact in this population. Understanding the mental health problems experienced by pregnant AGYW in SSA, the methodologies used to evaluate mental health in this population, and specific gaps in mental health services for pregnant AGYW is necessary to inform effective interventions tailored to this unique group. To our knowledge, no studies to date have mapped evidence about the key mental health problems and service challenges faced by pregnant AGYW in SSA. We performed a systematic review to synthesize evidence about the mental health problems, methodologies, and service delivery gaps experienced by pregnant adolescent girls and young women in Sub-Saharan Africa.
Methods
Search strategy and selection criteria
We performed a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines (PRISMA).27 In this systematic review, we searched five electronic platforms (PubMed, Embase, CINAHL, PsycInfo, and Global Index Medicus [which incorporates African Index Medicus]) to identify relevant studies regarding mental health among pregnant AGYW in Sub-Saharan Africa published between January 1, 2007- December 31, 2020. We selected 2007 as the starting date since this was the publication year of the Global Mental Health Lancet series, which galvanized international focus on adolescent health and mental health problems and catalyzed new publications with shared focus.28,29 We developed a search strategy with search terms adapted for each database (Supplemental Table 1). Controlled vocabulary and free text included terms for ‘young adult’ or ‘adolescent’ and for ‘pregnancy’, along with terms that combined the concepts such as "Pregnancy in Adolescence"[Mesh]. These were joined with terms for mental health outcomes such as ‘anxiety’, ‘depression’, and ‘stress and trauma related disorders’ and terms for methodologies and interventions such as ‘surveys’, ‘focus groups’, and ‘psychotherapy’. We included all Sub-Saharan African countries as defined by the World Health Organization (Supplemental Table 1) as search terms.30
Studies were included if they met the following criteria: (1) involved pregnant AGYW aged 12–24 in Sub-Saharan Africa, and (2) focused on mental health problems (including but not limited to: addiction disorders, adjustment disorders, affective disorders, anxiety disorders, psychosocial disorders, emotional disorders, mental instability, mood disorders, suicidal behavior, psychosis, psychosomatic disorder, psycho-trauma). All study designs were included (e.g., qualitative, cohort study, cross-sectional study, etc.). Articles that included pregnant women >24 years old were included if stratified results were presented for AGYW versus older women. Articles that included postpartum AGYW were included if stratified results were presented for pregnant AGYW, or if results focused on experiences during pregnancy. Studies were excluded if they were published before 2007, in non-English language, or were not based on pregnant AGYW populations in SSA. We further excluded abstracts, protocols, and theses/dissertations.
All articles were screened for title/abstract by two independent, parallel reviewers using the Rayyan review support application.31 Articles selected for full-text review were uploaded into Rayyan for independent, parallel review by three reviewers of equal qualification to perform the review. Discrepancies were resolved through discussion; at least two authors had to agree for an article to be included.
Data analysis
We assessed the quality of included studies using Joanna Briggs Institute (JBI) Critical Appraisal Tools.32 This suite of tools is comprised of checklists adapted for a range of study designs that includes a 7 item checklist for case reports, an 8 item checklist for cross-sectional studies, an 11 item checklist for cohort studies, and a 10 item checklist for qualitative studies. The checklists pose a series of questions regarding presence of specific information with response options “yes”, “no”, “unclear”, and “not applicable” to guide appraisers toward conclusions about the methodological quality of a study or analysis (Supplemental Table 2).
We evaluated information from each article regarding the geographic location (country, study setting), study design (e.g., qualitative/quantitative, study type), study population, sample size and recruitment methods, mental health outcomes assessed, and the outcome measurement tool used (when available). Data were extracted into tables with pre-specified categories. For quantitative studies, we collected estimates of mental health problems and associated factors, and summarized key findings, conclusions, and gaps in mental health services identified by the authors. For qualitative studies, we collected information about emergent themes and author conclusions and recommendations. Data was extracted and synthesized collaboratively by three authors (JM, AL, MK) who read the included manuscripts, identified interpretive themes and concepts, and highlighted consensus findings about mental health outcomes across similar studies, particularly as they substantiated our chosen bio-socioecological model.33
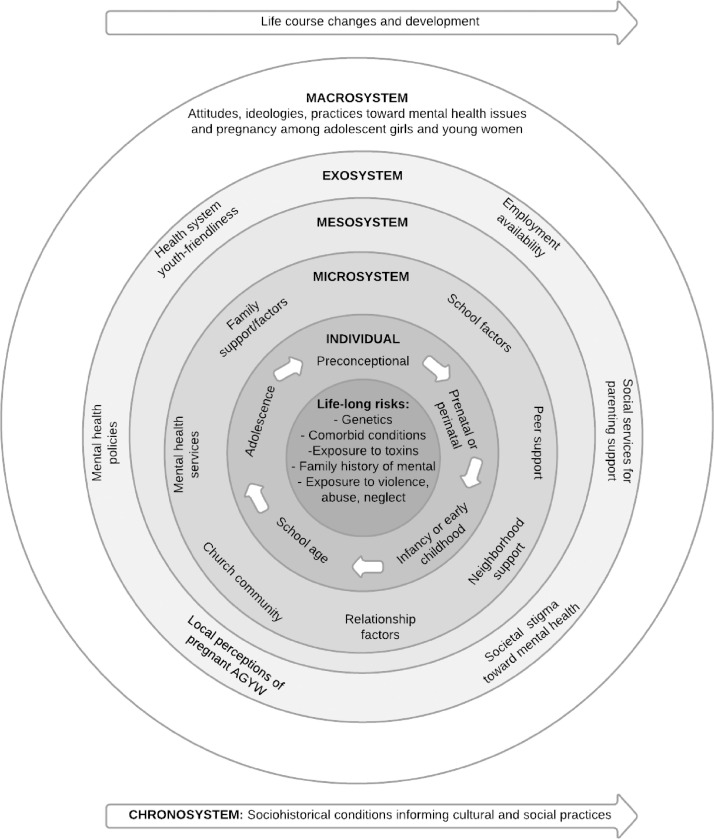
Our overall objective was to identify mental health disorders and problems reported by pregnant AGYW in SSA, map commonly used study designs and methods to identify these problems, as well as the mental health service delivery gaps highlighted within this evidence-base. We utilized Bronfenbrenner's bioecological theory of development to frame and interpret results (Figure 1).34 This model presents proximal and distal factors (individual, microsystem, exosystem, macrosystem) influencing an individual's development over time. We adapted the bioecological framework for pregnant adolescent girls and young women in sub-Saharan Africa. Within the “individual” bioecological level of Bronfenbrenner's model, we incorporated the Lancet lifecycle approach which chronologically describes risk factors for mental disorders among adolescents35 (Figure 1). Both the Lancet lifecycle approach and Bronfenbrenner's bioecological model highlight life and developmental changes that dynamically influence health outcomes over time.
Figure 1.
Adapted bioecological model for mental health among pregnant adolescent girls and young women
Figure legend: Adaptation of Bronfenbrenner's bioecological model of development and Lancet lifecycle approach to risk factors for mental disorders among adolescents [Bronfenbrenner & Morris 2007, Kieling et al. 2011).
Our protocol was registered on Prospero (CRD42021230980) on March 19, 2021. Ethical approval was not required for the study.
Role of the funding source
Funding agencies had no role in the writing of the manuscript or the decision to submit it for publication.
Results
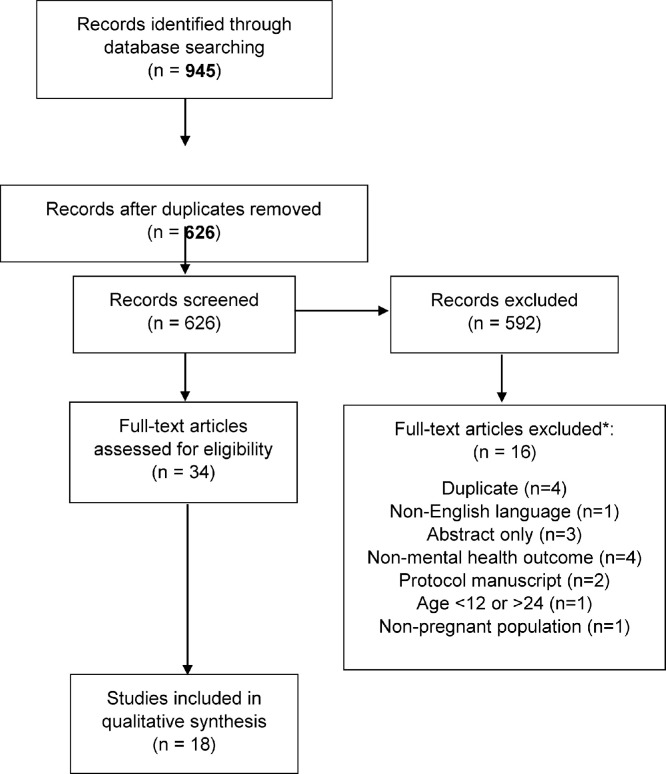
Our systematic database search identified 945 records (PubMed [n = 125], Embase [n = 299], CINAHL [n = 175], PsycInfo [n = 91], and Global Index Medicus [n = 9]), of which 319 were duplicates (Figure 2). We screened titles and abstracts of 626 articles, excluding 592 based on our pre-specified inclusion/exclusion criteria. We evaluated the full text of the remaining 34 articles, excluding 16 for the following reasons: duplicates (n = 4), non-English language (n = 1), abstracts only (n = 3), non-mental health outcome (n = 4), protocol manuscript (n = 2), age <12 or >24 (n = 1), or non-pregnant population (n = 1). Overall, 18 articles were assessed for quality and included in this review.
Figure 2.
PRISMA Flow Diagram
*When articles were excluded for multiple reasons, we eliminated them in order of these categories (top-to-bottom).
Methodological approach and assessment tools utilized in included studies
Among the 18 studies included, 6 were from Nigeria,36, 37, 38, 39, 40, 41 5 were from Kenya,20,42, 43, 44, 45 5 from South Africa,46, 47, 48, 49, 50 1 from Malawi,51 and 1 from Uganda52 (Table 1). Eight studies presented quantitative data,20,37, 38, 39,41,42,49,50 9 were qualitative evaluations,40,43, 44, 45, 46, 47, 48,51,52 and one presented a case study.36 Included studies predominantly focused on depression (n = 9)20,38,39,41,42,44,48, 49, 50 as a mental health outcome; others focused on psychological circumstances such as substance use/abuse, school dropout, loss of self-esteem, and finance-related anxiety.37,43,46,47,52 Among the 9 studies that formally assessed antenatal depression, four used the Edinburgh Postnatal Depression Scale (EPDS) to quantify depressive symptoms,41,42,49,53 two used the Patient Health Questionnaire-9 (PHQ-9),20,45 two used Beck's Depression Inventory II,38,42 and two used survey questions regarding depression experience that were not part of validated mental health screening tools.39,42 All other studies evaluated mental health outcomes using semi-structured qualitative interview guides or researcher-developed survey questionnaires. The studies assessed ranged in sample size from n = 1 (case narrative) to n = 772. Most studies restricted study populations to participants under age 20 (n = 13). The majority of studies recruited participants from health care settings (n = 14), most commonly maternal and child health clinics in primary care or public health services. Only one study enrolled students within a university in South Africa.47
Table 1.
Characteristics of included studies: A systematic review of mental health problems facing pregnant adolescents and young women in sub-Saharan Africa (n = 18 studies).
| Author | Year published | Country | Study setting | Study type/design | Study population | Sample size and recruitment | Mental health outcome(s) | Outcome measurement tool |
|---|---|---|---|---|---|---|---|---|
| Aghukwa et al.1 | 2015 | Nigeria | Health care facility | Case Narration | 24 year old pregnant woman with Schizophrenia |
N = 1 |
Catatonic Schizophrenia in pregnancy | Corroborated clinical interview |
| Ayamolowo et al.2 | 2019 | Nigeria | Health care facilities | Quantitative; Cross-sectional study | pregnant and postpartum adolescent girls and young women (AGYW) aged 13–20 | N = 120 | Perceived social support, depression | Structured questionnaire; Beck Depression Inventory, Multidimensional Scale of Perceived Social Support |
| Babafemi et al.3 | 2012 | Nigeria | Community setting | Quantitative; Cross-sectional study |
13–19 year old pregnant and postpartum AGYW | N = 300 | Depression, anxiety, Psychosocial support | Structured questionnaire |
| Carbone et al.4 | 2019 | Malawi | Health care facilities | Qualitative | 13–19 year postpartum AGYW with HIV | N = 18 | Barriers to, and facilitators of PMTC care. | Focus Group Discussions |
| Govender et al.5 | 2020 | South Africa | Health care facility | Quantitative – Cross-sectional study | 13–19 year old pregnant and postpartum AGYW | N = 326 | Antenatal and postpartum depression | Structured Questionnaire & Edinburg Postnatal Depression Scale (EPDS) |
| Govender et al. (2)6 | 2020 | South Africa | Health care facility | Qualitative – Focus group discussions (FDGs) | 16–19 year old postpartum AGYW | N = 18 | Anxiety, psychological issues (guilt, stress), suicidal ideation | Focus Group Discussions |
| Dare et.al7 | 2016 | Nigeria | Community setting | Quantitative – Cross-sectional study | 13–18 year old pregnant AGYW |
N = 33 pregnant N = 67 never pregnant |
Predictors of adolescent pregnancy and its psychosocial effects (e.g. school dropout, substance use) | A Questionnaire by Guttmacher Institute to evaluate basic psychosocial effects |
| Field et.al.8 | 2020 | South Africa | Health care facility: Maternal and child health (MCH) | Qualitative (Semi-Structured Interviews) | 15–19-year-old AGYW mothers. Part of a Perinatal Mental Health Project (PMHP) during pregnancy and 6–12 weeks after delivery | N = 12 | Barriers and facilitators to mental health among AGYW mothers | Semi-structured qualitative interview guide. |
| Kaye et al.9 | 2008 | Uganda | Health care facility | Qualitative- 22 in-depth interviews (IDIs), 6 FDGs | 14–19 year old AGYW studied from pregnancy to 6 weeks postpartum | N = 52 | Mental health challenges e.g. Anxiety, loss of self-esteem, financial challenges, low support from parents or partners, stigma by health workers, low coping | Qualitative interview guide |
| Kimbui et al.10 | 2018 | Kenya | Health care facility in informal settlements | Quantitative-Cross-sectional study | 14–18 year old pregnant AGYW | N = 212 (N = 106 16–17 years old, N = 106 18 years old) | Depression with comorbid substance use among pregnant AGYW | Structured questionnaire; Edinburgh Postnatal Depression Screen (EPDS), Becks Depression Inventory II, Alcohol Use Disorders Identifcation Test (AUDIT) |
| Kola et al.11 |
2020 | Nigeria | Community and health care facility | Qualitative – (FGDs); | 16–45 year old postpartum AGYW, health care providers | N = 42 (N = 17 mothers who were adolescents during pregnancy, N = 25 health care providers) | Help-seeking behavior for perinatal depressive symptoms | Qualitative focus group discussion interview guide |
| Kumar et al.12 | 2018 | Kenya | Health care facility: MCH | Qualitative: IDIs, FDGs | 15–18-year-old pregnant AGYW, 15–18-year-old AGYW mothers, Caregivers/partners accompanying AGYW, Health care workers (HCWs) from MCH |
N = 8 pregnant AGYW; N = 6 caregivers; N = 22 AGYW mothers; N = 20 HCW, convenience sampling recruited from MCH | Mental health challenges among pregnant adolescents | Qualitative interview guide. |
| Musyimi et al.13 | 2020 | Kenya | Community and health care settings in Makueni County, Kenya | Qualitative: FDGs, Key Informant Interviews (KIIs) | 13–19 year old pregnant and early postpartum AGYW, HCW, traditional birth attendants, community health workers |
N = 27 FGDs, N = 8 KIIs; Purposive and snowball sampling |
Suicidal behavior risk among pregnant/postpartum AGYW | Qualitative interview guide. including individual level factors (chronic psychical illness), interpersonal level (intimate partner violence, family rejection), Community level (social isolation by the community), societal level (poverty) |
| Oladeji et al.14 | 2019 | Nigeria | Health care facility | Quantitative; Cohort study | 16–45 year old pregnant AGYW/women | N = 9352 (N = 772 adolescents ≤19) | Depression, adjustment and attitude to pregnancy and motherhood | Structured questionnaire; Edinburgh Postnatal Depression Scale (EPDS); Maternal Adjustment and Maternal Attitudes scale |
| Osok et al.15 | 2018 (1) | Kenya | Health care facility: MCH in Nairobi County, Kenya | Qualitative: IDIs | 15–19 year old pregnant AGYW screened with score ≥5 on Patient Health Questionnaire-9; Caregivers/partners |
N = 12 pregnant AGYW recruited from MCH visit; N = 4 caregivers/ partners accompanying pregnant AGYW |
Depressive symptoms during pregnancy | Qualitative interview guide. Patient Health Questionnaire-9 |
| Osok et al.16 | 2018 (2) | Kenya | Health care facility: MCH in Nairobi County, Kenya | Quantitative: Cross-sectional study | 15–18 year old pregnant AGYW | N = 176 pregnant AGYW recruited from MCH | Depressive symptoms during pregnancy | Structured Questionnaire & PHQ-9 |
| Thabethe et al.17 | 2020 | South Africa | University of Venda, Limpopo Province, South Africa | Qualitative: IDIs | 19–23 year old pregnant AGYW | N = 12 pregnant AGYW university students; convenience sample from 104 total identified pregnant students at University of Venda | Psychological experiences of pregnant university students | Qualitative interview guide |
| Wong et al.18 | 2017 | South Africa | Health care facility: Gugulethu Midwife Obstetric Unit, Cape Town, South Africa | Quantitative: Cross-sectional study | 18–24 year old postpartum AGYW, ≥25 years postpartum women | N = 625 | Depression, alcohol use, and stigma in younger versus older HIV-infected pregnant women | Edinburgh Postnatal Depression Scale (EPDS), Alcohol Use Disorders Identification Test (AUDIT), Perceived Availability of Social Support, HIV Social Impact scale (stigma) |
Quality assessment
Two independent reviewers (JM and AL) deemed all articles as high quality in this systematic mapping review. One reviewer noted that measurement tools for factors of poverty, substance use, stigma, and depression were not standardized and validated in the Dare et al. article, while the other reviewer noted a small sample size (Supplemental Table 2).37
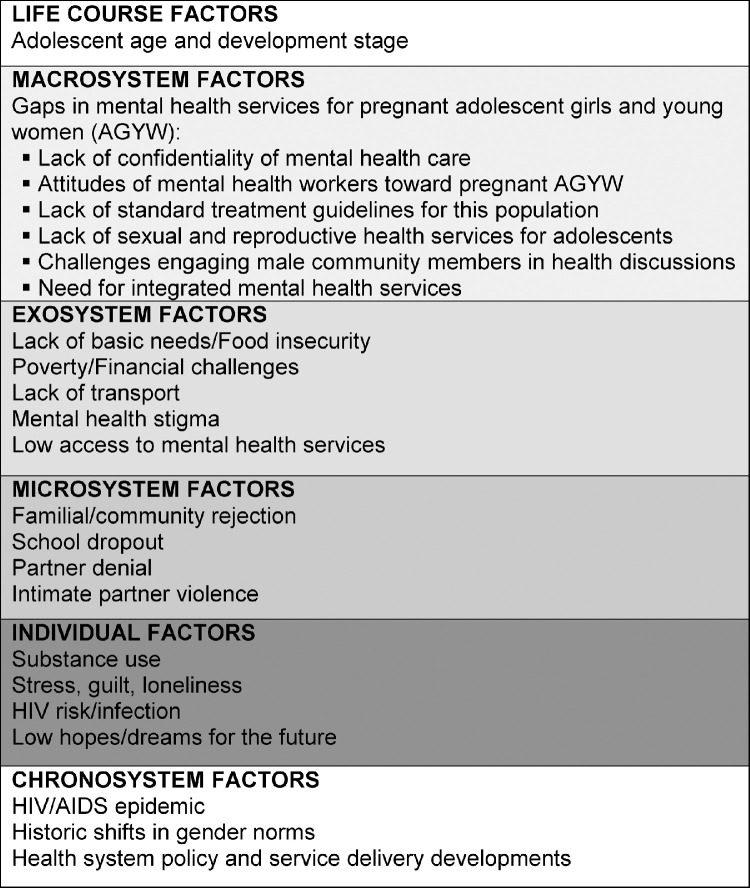
Life course factors: adolescent age and development
One criterion for inclusion within this study was age within 12–24 years, yet the heterogeneity of life and developmental stages within this range should be noted. Two quantitative studies found younger pregnant AGYW had higher frequency of depressive symptoms than older women. In a cohort study of pregnant adolescents and adults (age 16–45), Oladeji and colleagues found that adolescents were significantly more likely to be depressed than adults (15–19 year-olds: 17·7% [EPDS score ≥12], ≥19-year-olds: 6·9%, p< 0·001) and that adolescents had poorer parental skills and attitudes toward their pregnancy (Figure 3).41 Further, Osok et al. also found severe depressive symptoms (PHQ-9 score ≥ 15) were common (15.9%) among 15–18-year-old pregnant women.20 Overall, life course factors of age and developmental stage interact with all other levels within the Bronfenbrenner bioecological model to impact mental health of pregnant AGYW in SSA.34
Figure 3.
Systematic review findings about mental health problems and associated factors among pregnant adolescent girls and young women in Sub-Saharan Africa.
Individual factors: substance use, stress, anxiety, HIV risk/infection
Quantitative results revealed individual-level contributors to mental health among pregnant AGYW in SSA. Four quantitative studies focused on concurrent depression and substance use among pregnant AGYW (Table 2).20,37,42,49 In their cross-sectional study among over 200 pregnant 16–18 year-olds attending antenatal care in Kenya, Kimbui and colleagues found that 60% had elevated depressive symptoms (≥8) on the Edinburgh Postnatal Depression Scale, and 26·9% reported currently consuming alcohol.42 Among a small sample (n = 33) of 13–18 year-olds who were pregnant or mothers, Dare and colleagues found nearly all participants experienced feelings of depression (n = 31, 94%, measured with Guttmacher Institute survey) and the majority also utilized harmful substances during pregnancy (n = 24, 85%).37 Wong et al. noted higher alcohol-related harm among pregnant AGYW compared to older women (37% vs. 21%, p = 0·02),49 and Osok et al. found that substance use was associated with depressive symptoms among 15–18-year-old pregnant adolescents (prevalence of 14.8% vs. 10.8%, p = 0.019) (data not shown).20
Table 2.
Estimates and correlates identified in quantitative evaluations of mental health among pregnant adolescents and young women in sub-Saharan Africa (N = 8).
| Author, year published, Country | Study design, sample size | Estimates and correlates identified | Key findings | Conclusions about gaps in mental health service Delivery | Bioecological level(s) identified |
|---|---|---|---|---|---|
| Ayamolowo et al. (2019), Nigeria2 | Cross-sectional study; 13–19 year old pregnant and breastfeeding adolescents (N = 120) | Moderate perceived social support: 54·2% Low perceived social support: 1 2·5% Severe depression: 10·0% Correlation between respondents' level of social support and depression at r=- 0·510, P=<0·0001 |
Significant association between perceived social support and development of depression among population. | Need for community health information, education and programs to support and reduce negative mental health outcomes among the population. | Individual |
| Babafemi et al. (2012), Nigeria3 | Cross-sectional study; 13–19 year old pregnant and breastfeeding adolescents; N = 300 (N = 150 pregnant, N = 150 postpartum) | Depression and anxiety: During pregnancy: 27·3% After pregnancy: 59·0% After childbirth and now: 13·7% Poor psychosocial support during pregnancy: 35·7% Poor psychosocial support during breastfeeding: 16·7% Generally, 49·3% who received poor psychosocial support either during pregnancy or breastfeeding also experienced poor health while 17·7% who got good psychosocial support at those times also experienced good health. |
Health and psychosocial problems of adolescent pregnancy include low education, poverty, limited job opportunities, depression, and high blood pressure |
Attention of nurses, health education, conventional education, economic status etc. correlate to increased health status and ability of the pregnant adolescent to cope with pregnancy related stress | Individual |
| Dare et al. (2016), Nigeria7 | Cross-sectional study; 13–18-year-old pregnant adolescent girls and young women (AGYW); N = 100 (N = 33 pregnant; N = 67 never pregnant) |
Depression (n = 31, 93·9%); Substance abuse (n = 28, 84·8%); School dropout (n = 24, 72·7%); Abandonment by friends (n = 24, 72·7%); Rejection by parents/relatives (n = 22, 66·7%); Rejection by church/mosque (n = 17, 51·5%); Stigmatization by the community (n = 22, 66·7%); Suicide attempts (n = 18, 54·5%)” |
Poverty is a major factor causing adolescent pregnancy |
Need for sex education in schools, improved access to health services and staff who understand adolescents and their needs |
Individual Microsystem |
| Govender et al. (2020), South Africa6 | Cross-sectional study 13–19 year old pregnant and postpartum adolescents; N = 326 | Depressive symptoms (EPDS ≥13): 11·7% Among pregnant adolescents: 15·9% Among postpartum adolescents: 8·8% Experiences of physical, sexual, and verbal abuse were associated with risk of depression (p<0·05) |
Prevalence of antenatal depression is higher than postpartum depression. Physical violence, verbal abuse, and absence of partner support associated with antenatal and postpartum depression. | Need to integrate MH needs and MH screening into reproductive health program packages. | Microsystem |
| Kimbui et al. (2018), Kenya10 | Cross-sectional study; 14–18-year-old pregnant AGYW N = 212 (N = 106 16–17 years old, N = 106 18 years old) |
Depressive symptoms (EPDS: ≥8): 60·4%; Severe depression (BDI): 51·9%; Currently consuming alcohol: 26·9%; “Of the 110 pregnant adolescents who were severely depressed, 39 were currently consuming alcohol.” |
Suggested correlation between depression and substance abuse in adolescents | Need to develop culturally relevant systemic interventions for the population. | Individual |
| Oladeji et al. (2019), Nigeria14 | Cohort study; N = 9352 (N = 772 pregnant adolescents ≤19 years old, N = 8580 adult pregnant women) | Depression (EPDS score ≥ 12): 17·7% (15–19 year olds). 6·9% (≥19 year olds, 0·082) Adjustment and attitudes to pregnancy (mean MAMA score): 21·8% (15–19 year olds). 19·8% (≥19 year olds, <0·001) |
Perinatal depression more common and associated with poorer maternal attitudes and parenting skills in pregnant adolescents than in pregnant adults | Need to supplement depression interventions in pregnancy to improve parenting skills. | Microsystem |
| Osok et al. (2018, 2), Kenya16 | Cross-sectional study; N = 176 pregnant adolescents (age 15–18) |
Mild-to-severe depressive symptoms (score ≥5): 78·4%;Severe depressive symptoms (score ≥15): 15·9%;Correlates of depressive symptoms:
|
Risk factors for depression include: having experienced an adverse event or extremely stressful life context, living with HIV/AIDS, absence of support from the partner or family and being a younger adolescent | Need to integrate WHO's Mental Health Treatment Gap Action Program (known as WHO mhGAP) in the healthcare settings for pregnant adolescents | Individual Microsystem Exosystem |
| Wong et al. (2017), South Africa18 | Cross-sectional study; N = 625 (18–24 year old postpartum AGYW, ≥25 year old postpartum women) | Depression: 11% Self-harming thoughts: 6% (18–24 year olds: 11%; >24 year olds: 4%, p-value= 0·002) Risky alcohol use: 16% Alcohol-related harm: 21% (18–24 year olds: 37%; >24 year olds: 20%, p-value= 0·02) |
Young HIV-infected pregnant women more likely to report depressive symptoms and self-harming thoughts compared to older women with the youngest women reported the highest levels of alcohol-related harm | Need for interventions for the population | Individual |
Data from the nine included qualitative studies elucidated emergent themes about mental health problems facing pregnant AGYW in SSA, associated factors, and as well as barriers to achieving mental health care (Table 3). Specific quotations from qualitative emergent themes were highlighted (Supplemental Table 3). The most prominent findings related to the individual- and microsystem-level factors contributing to mental health among pregnant AGYW. Multiple studies found that pregnant AGYW experienced individual-level manifestation of stress, stemming from micro-, exo-, and macrosystem stressors, including stress from new life adjustments, social stigma, and poor health care access.43,44,52 In focus group discussions among AGYW living with HIV, Carbone et al. found resilience and self-efficacy were reported as motivating factors to seek peer support.51 In settings with high-HIV burden, stress regarding an AGYW's personal HIV risk or HIV-infection contributed substantially to the mental health of pregnant, especially younger AGYW (age 13–20).43,44,47 Feelings of guilt, loneliness, anxiety, and stress were key individual-level contributors to poor mental health reported among adolescents, while personal dreams and aspirations toward education offered hope.48
Table 3.
Emergent themes from qualitative evaluations of mental health among pregnant adolescents and young women in Sub-Saharan Africa (N = 9).
| Author, year published, Country | Study population | Mental health outcome(s) | Emergent themes | Recommendations to address service gaps | Bioecological level(s) identified |
|---|---|---|---|---|---|
| Carbone et al. 2019, Malawi4 | 13–19 year old parenting adolescent girls and young women (AGYW) mothers | Barriers and facilitators to PMTCT. | Barriers: Poverty, stigma, food insecurity, lack of transport, and absence of psychosocial support Facilitators: resilience and self-efficacy Need:- tailored, age-appropriate services, support services delivered by adolescent HIV-infected mentor mothers who have successfully navigated the PMTCT |
Evaluate the intervention and its outcomes for the population. | Individual Microsystem |
| Field et al. (2020), South Africa8 | 15–19 year old adolescents mothers who were part of a Perinatal Mental Health Project (PMHP) during pregnancy and 6–12 weeks after delivery | Barriers and facilitators to mental health among AGYW mothers | Experience of using the mental health service: Mental health literacy, screening, resistance to referral, expectations and experiences of counseling, stigma, confidentiality, access, coordinated appointment times, disclosure of attending counseling and social support | Need to integrate routine mental health screening into existing obstetric services to minimize stigma. |
Macrosystem |
| Govender et al. 2020 (2), South Africa5 | 16–19 year old postpartum AGYW | Anxiety, psychological issues (guilt, stress), suicidal ideation | Different reactions to adolescents’ pregnancies by family such as rejection that resulted in loss of support, anger, disappointment, and other psychosocial issues e.g. suicidal ideation, guilt, loneliness, anxiety, and stress. Experiences of financial constraints, difficulty in returning to school, and stigmatization in society. | Need for a multidisciplinary approach in caring for adolescent mothers. | Individual Microsystem |
| Kaye (2008), Uganda9 | 14–19 year old AGYW followed from pregnancy to 6 weeks postpartum | Mental health challenges: Anxiety, loss of self-esteem, financial challenges, moral/material support from parents or partners, and stigmatization by health workers, coping mechanisms | Coping Mechanisms:
|
Need to assess for various coping mechanisms before developing flexible interventions/goals of care. |
Individual |
| Kola et al. (2020), Nigeria11 | 18+ year old postpartum AGYW (Mean age 22+/- 1•1), health care providers | Help-seeking behavior for perinatal depressive symptoms | Presence of care for perinatal depression despite presence of stigma from health care providers. | Training was helpful for care givers in the management or perinatal depression among population thus need to improve more supportive healthcare settings | Macrosystem |
| Kumar et al. (2018), Kenya12 | 15–18-year-old pregnant adolescents, 15–18-year-old AGYW mothers, Caregivers/partners accompanying AGYW, Health care workers (HCWs) from MCH |
Mental health challenges among pregnant adolescents | Five themes emerged about mental health challenges among pregnant adolescents: Social stigma Lack of emotional support Stress based on new life adjustments Poor health care access Planning for the future Challenges in providing mental health services to pregnant adolescents in MCH contexts: Standard treatment in MCH services is not adequate for pregnant/parenting adolescents Lack of sexual/reproductive health education among adolescents Absence of mental health prevention and treatment programs for pregnant/parenting adolescents Challenges with engaging male community members in discussions/education about adolescent pregnancy/parenting |
Need for follow-up on pregnant adolescents who visit the MCH facility and the provision of support to CHWs Need for risk assessment of the adolescent's family condition and support mechanisms in communities and involvement of child welfare services when need arises. |
Individual Microsystem Exosystem Macrosystem |
| Musyimi et al. (2020), Kenya13 | 13–19 year old pregnant and early postpartum AGYW, HCW, traditional birth attendants, community health workers | Suicidal behavior risk among pregnant/postpartum adolescents | Five main themes about suicidal behavior risks among adolescent mothers: Chronic physical illness (e.g., HIV/AIDS) Intimate partner violence Family rejection Social isolation and stigma from community Poverty |
Explore ways of addressing IPV, economic empowerment and access to youth friendly health care for chronic physical conditions in adolescent mothers. Address Substance use as causing IPV in families through inclusive, integrated approaches | Individual Microsystem Exosystem |
| Osok et al. (2018, 1), Kenya15 | 15–19 year old pregnant adolescents screened with score ≥5 on Patient Health Questionnaire-9; Caregivers/ partners |
Depressive symptoms during pregnancy | Four major themes for adversities and mental health needs of pregnant adolescents: Depression, anxiety, and stress around the pregnancy Denial of the pregnancy Lack of basic needs, provisions, and care Restricted opportunities for personal development post-pregnancy |
“-Presentation of “idioms” of depression -Strengthening sexual and reproductive health education -Training health workers in identifying mental health problems in high-risk adolescents -Implementation of adolescent friendly services at community, school, and health facility” |
Individual Microsystem Exosystem |
| Thabethe et al. (2020), South Africa17 | 19–23 year old pregnant AGYW | Psychological experiences of pregnant university students | Four themes for psychosocial experiences of pregnant university students: Maternal stress and anxiety Inability to cope Poor concentration Low self-esteem |
Higher educational institutions provide psychological support, including counselling to pregnant students and health facilities at the institutions provide antenatal care services. | Individual |
Microsystem factors: rejection, school dropout, partner denial, intimate partner violence
Microsystem factors related to pregnant AGYW's interactions with their families, partners, peers, and communities were identified as influencers of their mental health. Rejection or low support by family, friends, and community members was cited in multiple studies as a contributor to mental distress among pregnant AGYW. Low social support was strongly associated with depressive symptoms in two cross-sectional studies of pregnant 13–19-year-olds in Nigeria,38,39 as well as a cross-sectional study in Kenya.20 Dare et al. found abandonment by friends and rejection by parents, relatives, church and mosques members was high (>65%) among pregnant adolescents (Table 2; Supplemental Table 3).37 The finding was echoed in qualitative results from Govender et al. who similarly found that familial responses ranged from disappointment to fear of abandonement.48
School disruption and dropout were associated with mental distress among pregnant AGYW. Dare and colleagues found Nigerian pregnant adolescents had high prevalence of school dropout (>70%).37 In focus group discussions, South African pregnant adolescents expressed difficulty in returning to school as a stressor associated with their pregnancy, yet used the vision of returning to school as a motivating factor.48
Denial of the pregnancy by their partner, as well as violence by an intimate partner were experiences affecting the mental health of pregnant AGYW in multiple studies. In a cross-sectional study, physical, sexual, and verbal abuse was associated with depressive symptoms among pregnant adolescents in South Africa (p-value= 0·05).50 Experiences of intimate partner violence was also associated with depressive symptoms among Kenyan pregnant AGYW.20 A main theme from Musyimi and colleagues’ qualitative findings was that suicidal behavior among pregnant adolescents was triggered by intimate partner violence44 and Osok et al. identified denial of the pregnancy by an intimate partner as a key adversity influencing mental health among pregnant adolescents.45
Exosystem factors: poverty, unemployment, mental health stigma, poor health care access
Exosystem-level characteristics were more frequently reported in qualitative studies whereas quantitative studies were more likely to identify individual and microsystem- level factors. Specifically, financial concerns, lack of basic needs, and poverty were associated with mental health problems in this population. In a qualitative study among Malawian adolescent mothers (13–19) about their experiences in pregnancy, participants reported poverty, food insecurity, and lack of transport as barriers to engagement in a peer support intervention.51
Financial challenges were also cited as a co-occurring experience with mental distress in another qualitative study among South African adolescent mothers.48 Poverty was identified by Musyimi and colleagues as one of five main contributors to suicidal behavior among pregnant adolescents in Kenya based on qualitative interviews.44 Moreover, lack of basic material provisions was one of four major adversities during pregnancy among Kenyan adolescents with elevated depressive symptoms (PHQ-9 score ≥5).45 Relatedly, one quantitative study identified unemployment as a correlate of moderate-to-severe depressive symptoms among pregnant adolescents in Kenya.20
Pregnant adolescents reported that social stigma associated with mental health problems was a major challenge impacting their wellbeing.43 They reported that mental health information and care within routine maternal and child health care was lacking.43 Overall, results illustrated the complex network of factors at individual, microsystem, and exosystem levels contributing to psychological distress among AGYW during pregnancy.
Macrosystem factors: gaps in health services for mental health among pregnant AGYW
At the macrosystem level, attitudes, ideologies, and practices regarding mental health problems among pregnant AGYW shape the societal response. Mental health problems in sub-Saharan Africa are generally stigmatized and not socially recognized, thus gaps persist in the availability, access, and quality of mental health services for pregnant AGYW. Three qualitative studies included in this review were specifically designed to identify insufficiencies in mental health services for this population. One identified barriers and facilitators to accessing peer support services among pregnant adolescents, one evaluated health-seeking behavior for perinatal depressive symptoms, and one identified challenges in providing mental health services to pregnant adolescents.40,46,51
Pregnant adolescents in South Africa reported specific barriers and facilitators to mental health access.46 Lack of confidentiality was a barrier to care and the absence of designated appointments for this age group was demotivating as stigma related to adolescent pregnancy and mental health made women reticent to attend care publicly.46 Pregnant AGYW preferred to attend mental health services where healthcare workers were sensitive to their situation and withheld judgement.46 Based on these findings, Field et al. concluded that integrating mental health screening into existing maternal and child health services may help de-stigmatize mental health problems.
Young pregnant girls and women reported resisting referrals to available mental health care due to judgmental attitudes of healthcare workers.40 They suggested that mental health services be offered within primary care settings. Mental health skills training among primary and non-specialist healthcare workers to improve quality of mental health care for pregnant adolescents was also proposed.40 Kumar and colleagues, in interviews with healthcare workers in maternal and child health clinics working with pregnant adolescents, found that the absence of standard treatment guidelines specific to pregnant AGYW was a barrier to care provision.43 The authors proposed mental health services tailored to the unique needs of adolescents and young women to increase uptake.43
Kimbui, Dare, Kumar and their colleagues emphasized the need for sexual and reproductive health services for teenagers as a main strategy for reducing adolescent pregnancy as a source of undue stress and challenge.37,42,43 Osok and colleagues advocate for adoption of task-shifting models to increase access to mental health services for pregnant adolescents experiencing mental health challenges in low-resource settings.20 Additionally, challenges with engaging male community members (young and older) in these discussions limits their impact.43,45 Recommendations highlighted by 8 of the included studies suggest the need for integrated mental health promotion and treatment focused interventions in community as well as at the health care facilities for this population.
Chronosystem: sociohistorical conditions over time
As illustrated by Bronfenbrenner's inclusion of chronosystem within the bioecological model, it is important to contextualize all life course, individual, microsystem, mesosystem, exosystem, and macrosystem factors within their place in history and societal evolution.34 The chronosystem influences the mental health problems prevalent within a population, the multi-level factors contributing to those issues, the methods used to measure them, and the services available (and unavailable) to address them.54 Across articles included in this mapping review, we noted increasing publications focused on mental health within pregnant AGYW in SSA over time. The earliest included article was published in 2008, the next in 2012, one each in the years 2015–2017, then multiple per year from 2018 suggesting increasing scientific and societal focus on this topic at the chronosystem level. Articles highlighted historic and social factors such as the evolving HIV/AIDS pandemic, changing gender norms, and health system policy and service delivery development impacting the mental health of this population.
Overall, the 18 studies included in this review demonstrate that mental health problems are common among pregnant AGYW; influenced by life course, individual, microsystem, exosystem, macrosystem, and chronosystem factors; and that gaps exist in adequately addressing peripartum mental health within sub-Saharan African settings.
Discussion
We mapped evidence from the last 14 years regarding mental health problems and service barriers faced by pregnant adolescent girls and young women in sub-Saharan Africa. Across 18 studies from Eastern, Southern, and Western Africa sub-regions, we found depression was the most frequent mental health problem of focus and that comorbid psychosocial concerns were common among this population. Hormonal changes during adolescence and young adulthood compound psychosocial needs and everyday stresses in lives of young people and the context of unplanned pregnancy may trigger stress and exacerbate physiological and emotional distress. Further, the need for mental health services is even more acutely needed during pregnancy and postpartum period. Peripartum AGYW face barriers to health care access and encounter stigma, discrimination, and prejudiced responses from family members, peers, community, and health care workers. Our review provides a summary of the state of the evidence for mental health among this group and highlights gaps requiring urgent prioritization.
We used Bronfenbrenner's bioecological model of development, adapted for mental health among pregnant AGYW in SSA to contextualize factors influencing mental health at multiple levels of individual and social functioning. Each of the domains of the adapted model is inextricably linked to the others. Services and research gaps need to be understood from the macro- and exo-system levels so that improvements in these areas track down to the micro level. The life course approach and chronosystem are a pertinent reminder that human individuals and populations are ever-evolving such that adolescent risks and health outcomes may compound over time as they mature within the context of sociohistorical changes. Systems and services should be adapted to ensure age- and developmentally relevant health care services. Microsystem level changes may not be sustainable if accompanying exo- and macrosystem changes do not occur in tandem.
Depression and general psychological distress were reported frequently within the literature as impacting pregnant AGYW particularly significantly in SSA. The impact of mental health problems among pregnant AGYW may be more substantial and long-lasting among younger girls and adolescents than older women.55, 56, 57 we found that depression was the only mental health condition assessed with a formal tool (e.g., PHQ-9, EPDS) in the included studies; other conditions were reported via survey questions unrelated to validated depression screening tools or qualitative interview responses. Future studies among pregnant AGYW should evaluate common mental health disorders in general adolescent populations such as substance use, trauma, stress, self-harm, and suicidality using validated psychological scales to contribute valid estimates. There is also a need to augment these efforts by including assessments of common maternal mental health conditions including anxiety, puerperal psychoses, and bipolar disorders. Addressing quality of life, disability, resilience and overall functioning would also provide indicators to broad domains that map psychological well-being in AGYW. We found that the studies did not cover an in-depth exploration of the relationship between cultural and gender norms associated stigma and disenfranchisement of these populations that may trigger mental distress or challenges. The mental health consequences of rigid cultural and gender norms, exploitation and oppression of females, and patriarchal power dynamics in the sub-Saharan African region deserve further exploration in future studies about mental health in this population. We did find a disjunct between sociocultural psychology of gender and mental health literature in the scholarship covered under our review.
Many of the stressors identified as co-occurring with mental health problems among AGYW are similar to those found in adult women later in their reproductive spectrum. Thus, some of these factors may impact maternal mental health more generally. Financial stressors, lack of security in relationships, lack of social support systems, substance use, and chronic health conditions (e.g., HIV) contributed to psychological distress among AGYW, and are well-understood correlates of maternal mental health problems.2, 3, 4,6 Our study identified psychosocial stressors specific to AGYW that may exacerbate mental health problems during pregnancy and set the stage for more lasting health impacts. Dropping out of school and pausing career pursuits led pregnant AGYW to fear loss of aspirations and opportunities.12 Fear of rejection from partners, parents, friends, and religious or community leaders emerged as an important concern among pregnant AGYW. Social rejection and exclusion may be particularly detrimental to mental health among pregnant AGYW since adolescence is a socioemotional stage highly influenced by peer interaction.57 The stark awareness that one's expectations and dreams may no longer be attainable due to early motherhood may cause loss of hope that is especially discouraging among AGYW who have not yet experienced independence.48 The issues of social isolation and rejection, reduced opportunities, stalled career and education, as well as poor health care access point to issues at the macro-, exo-, and meso‑levels. Improved investment is needed to advance adolescent well-being within the development agenda in SSA.58
Three studies included in this review explored challenges in accessing mental health services among pregnant AGYW, yet we did not find any study specifically focused in identifying service delivery gaps.46,51,52 Mental health services and psychosocial support remain a significant gap in SSA indicating need for adolescent responsive health policies and evidence-based approaches to integrate sexual and reproductive health (SRH) and mental health services.
The following service implementation approaches may address some of the individual adolescent level risk factors and contextual problems identified in our review: (a) Combine sensitive adolescent responsive mental health and counseling services alongside obstetric care that addresses adolescent treatment needs and preferences in a life course/chronosystem approach, (b) Train care providers to employ non-judgmental care to AGYW, (c) Integrate preventative and promotive mental health messaging and interventions into antenatal and postnatal services to de-stigmatize mental health problems among AGYW (this will build literacy resilience and help mitigate intersectional stigma that is one of the most potent barriers to mental health care).20,43,46 and (e) a systematic approach to understanding oppressive sociocultural practices that aggravate the gender divide, disenfranchise young girls in being able to make vital decisions and choices about their lives.59
These strategies and integrated steps may take time to evolve and need to be tested across services that AGYW use. One of the recommendations made in almost all of the reviewed qualitative and quantitative studies was the need for enhanced education and training within communities on mental health problems faced by pregnant AGYW.20,37,42,44,52 Some felt the education should focus on adolescents, while others on healthcare providers and community members.20,42, 43, 44, 45, 46, 47,52 Both types of literacy and efforts at building capacity is critical. Sexual and reproductive health education for male and female adolescents was strongly recommended by multiple studies to address pregnancy as a source of psychological distress.20,37,44 Other researchers suggested training for task-shifting models to increase the availability of mental health services for pregnant AGYW.20,43 Task-shifting is one of the most successful of the implementation strategies in closing the ‘mental health treatment gap’ as well as helpful in achieving the Universal Health Coverage that is an important marker for progress around Sustainable Development Goals.60,61 However, the complexity of sustaining gains through task-shifting and evaluating task-shifted interventions merit further exploration.62 Investment and appropriate financing across the domains we have suggested remains a concern. One study recommended embedding psychological support and mental health counseling within academic institutions to support pregnant students better.47 School and higher educational institution based mental health interventions have been long been known to be the missing piece in the scaling up of mental health interventions for AGYW.63 We do not want to undermine the value of building and strengthening capacity through school and community mental health programs and interventions as well as targeting family strengthening approaches64,65 as per the WHO's recommended pyramid of care.66 While provider level capacity building is critical to development of the more enhanced service structure, there is a need for prioritizing grassroot capacity building in disseminating mental health literacy and first aid.
Our review was not without limitations that need further consideration. We included full manuscripts published in English language, thus we may have facilitated publication bias by not including all publication languages and abstracts especially given how diverse SSA is culturally and linguistically. A recent review found literature about mental health from Central sub-Saharan Africa was published in French only.67 Our study did not have resources for language translation services, thus we may have missed French-language publications from the Central African region. We would like to acknowledge that SSA is not a homogenous entity and we may have missed out on important geographies within Central SSA and tapping into other gray literature where these bio-socioecological factors pertaining to pregnant adolescents and young women may have been highlighted. The 18 articles included in our review represent 5 African countries thus our results are not generalizable across the diverse contexts and experiences of pregnant AGYW in SSA. Most articles recruited participants in formal health care settings, thus the current literature on this topic does not include mental health experiences of pregnant AGYW in SSA outside of formal health services. We summarized data from existing literature about the mental health experiences of pregnant AGYW in SSA yet were limited by the scarcity of published work on this important topic.
Pregnant adolescent girls and young women are at high risk for mental health problems yet substantial gaps remain in research and interventions tailored to this unique group. Programs that address financial challenges such as economic empowerment and cash-transfers, enhancement of social support, and alleviation of multidimensional stigma associated with pregnancy or poor mental health or both may be particularly useful to prevent and address psychological distress among pregnant AGYW. Further, services, interventions and programs that enable AGYW bring their dreams and aspirations to fruition despite unplanned pregnancy and motherhood, may reduce psychiatric morbidity and mental ill-health among this group, as current evidence highlights loss of hope for achieving life goals as a source of persistent psychological stress among AGYW. Scaling up holistic mental health services integrated within school, community, and healthcare settings should be further tailored for this group to ensure privacy, dignity and quality care is offered in youth friendly manner. Integrating tailored mental health services for pregnant adolescents and young women in sub-Saharan Africa has the potential to improve maternal and child health as well as strengthen health systems in the sub-continent.
Data sharing statement
Articles included in this systematic review and the study protocol are available upon request to the corresponding author.
Funding
Author contributions were supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (F31HD101149 to AL) and the Fogarty International Center (K43TW010716 to MK). The funding agencies had no role in the writing of the manuscript or the decision to submit it for publication. The project itself was not funded.
Contributors
JM-conceptualized the systematic review, reviewed articles, performed formal analysis, led the project administration, wrote the original draft, conducted edits for the drafts, reviewed and approved final draft. AL-conceptualized the systematic review, reviewed articles, performed formal analysis, led the project administration, wrote the original draft, conducted edits for the drafts, reviewed and approved final draft. MK- conceptualized the systematic review, supervised development of systematic review, oversaw all administration of project, contributed to writing original draft, reviewed all drafts, reviewed and approved final draft. TJ-developed and implemented search strategy for systematic review, reviewed and approved final draft. PC and SSP contributed to writing drafts, commented on methodology, reviewed and approved final draft. FG, OG, JK, DW, JU, JL, GJS, and MM contributed to writing drafts, reviewed and approved final draft. All authors had full access to all the data in the study and accept responsibility to submit for publication.
Declaration of interests
Dr. John-Stewart reports grants from NIH, grants from CDC, grants from Thrasher, grants from IMPAACT, personal fees from UW, personal fees from UpToDate, other from Malaika, outside the submitted work. All other authors declare no competing interests.
Acknowledgments
The project itself was not funded and this paper represents the opinions of the authors and is not meant to represent the position or opinions of organizations, nor the official position of any staff members.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101289.
Appendix. Supplementary materials
References
- 1.Hendrick V., Altshuler L., Cohen L., Stowe Z. Evaluation of mental health and depression during pregnancy: position paper. Psychopharmacol Bull. 1998;34 https://pubmed.ncbi.nlm.nih.gov/9803758/ (Accessed 26 Feb 2021) [PubMed] [Google Scholar]
- 2.Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Fisher J., Cabral de Mello M., Patel V., et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139–149H. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gelaye B., Rondon M., Araya R., Williams M. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3:973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman A., Patel V., Maselko J., Kirkwood B. The neglected ‘m’ in MCH programmes - why mental health of mothers is important for child nutrition. Trop Med Int Health. 2008;13:579–583. doi: 10.1111/j.1365-3156.2008.02036.x. [DOI] [PubMed] [Google Scholar]
- 6.Dadi A.F., Akalu T.Y., Baraki A.G., Wolde H.F. Epidemiology of postnatal depression and its associated factors in Africa: a systematic review and meta-analysis. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0231940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Payne J.L., Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019;52:165–180. doi: 10.1016/j.yfrne.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Adolescent mental health. 2018 https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed 23 March 2019).
- 9.World Health Organisation (WHO). Adolescent pregnancy. 2018. https://www.who.int/en/news-room/fact-sheets/detail/adolescent-pregnancy (Accessed 23 March 2019).
- 10.Reid V., Meadows-Oliver M. Postpartum depression in adolescent mothers: an integrative review of the literature. J Pediatr Health Care. 2007;21:289–298. doi: 10.1016/j.pedhc.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Adolescent health. World Health Organization, 2019 https://www.who.int/maternal_child_adolescent/adolescence/en/ (Accessed 22 March 2019).
- 12.Patton G.C., Sawyer S.M., Santelli J.S., et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodgkinson S.C., Colantuoni E., Roberts D., Berg-Cross L., Belcher H.M.E. Depressive symptoms and birth outcomes among pregnant teenagers. J Pediatr Adolesc Gynecol. 2010;23:16–22. doi: 10.1016/j.jpag.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thapar A., Collishaw S., Pine D.S., Thapar A.K. Depression in adolescence. Lancet. 2012;379:1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merikangas K.R., Nakamura E.F., Kessler R.C. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11:7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Troutman B.R., Cutrona C.E. Nonpsychotic postpartum depression among adolescent mothers. J Abnorm Psychol. 1990;99:69–78. doi: 10.1037//0021-843x.99.1.69. [DOI] [PubMed] [Google Scholar]
- 17.Cynthia Logsdon M., Birkimer J.C., Simpson T., Looney S. Postpartum depression and social support in adolescents. J Obstet Gynecol Neonatal Nurs. 2005;34:46–54. doi: 10.1177/0884217504272802. [DOI] [PubMed] [Google Scholar]
- 18.Hudson D.B., Elek S.M., Campbell-Grossman C. Depression, self-esteem, loneliness, and social support among adolescent mothers participating in the new parents project. Adolescence. 2000;35:445–453. [PubMed] [Google Scholar]
- 19.Schoenbach V.J., Garrison C.Z., Kaplan B.H. Epidemiology of adolescent depression. Public Health Rev. 1984;12:159–189. [PubMed] [Google Scholar]
- 20.Osok J., Kigamwa P., Vander S.A, Huang K.Y., Kumar M. Depression and its psychosocial risk factors in pregnant Kenyan adolescents: a cross-sectional study in a community health Centre of Nairobi. BMC Psychiatry. 2018;18:136. doi: 10.1186/s12888-018-1706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stein A., Pearson R.M., Goodman S.H., et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800–1819. doi: 10.1016/S0140-6736(14)61277-0. [DOI] [PubMed] [Google Scholar]
- 22.Howard L.M., Molyneaux E., Dennis C.L., Rochat T., Stein A., Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384:1775–1788. doi: 10.1016/S0140-6736(14)61276-9. [DOI] [PubMed] [Google Scholar]
- 23.Kramer M., Lydon J., Séguin L., et al. Stress pathways to spontaneous preterm birth: the role of stressors, psychological distress, and stress hormones. Am J Epidemiol. 2009;169 doi: 10.1093/AJE/KWP061. [DOI] [PubMed] [Google Scholar]
- 24.Lancaster C.A., Gold K.J., Flynn H.A., Yoo H., Marcus S.M., Davis M.M. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jörns-Presentati A., Napp A.-.K., Dessauvagie A.S., et al. The prevalence of mental health problems in sub-Saharan adolescents: a systematic review. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0251689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D., Shamseer L., Clarke M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev Esp Nutr Humana Diet. 2016;20:148–160. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horton R. Launching a new movement for mental health. Lancet. 2007;370:806. doi: 10.1016/S0140-6736(07)61243-4. [DOI] [PubMed] [Google Scholar]
- 29.Patel V., Saxena S., Lund C., et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 30.Africa Region WHO Regional Office for Africa. https://www.afro.who.int/countries (Accessed 7 Dec 2021 ).
- 31.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5 doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joanna Briggs Institute (2017). Checklist for critical appraisal of tools and research synthesis. https://jbi.global/critical-appraisal-tools (Accessed 9 June 2021).
- 33.Evans D., Pearson A. Systematic reviews of qualitative research. Clin Eff Nurs. 2001;5:111–119. [Google Scholar]
- 34.Bronfenbrenner U., Morris P.A. Handbook of Child Psychology. John Wiley & Sons, Inc.; 2007. The Bioecological Model of Human Development. [DOI] [Google Scholar]
- 35.Kieling C., Baker-Henningham H., Belfer M., et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 36.Aghukwa N.C., Takai M.G. Persistent catatonia in a pregnant nigerian woman: a case report. Niger J Med. 2015;24:179–182. [PubMed] [Google Scholar]
- 37.Dare A.A., Omolade D.G., Samuel A.E., Folashade W., Adaku O.G. Psychosocial effects of pregnancy on teenage mothers in Angwan Rukuba community, Jos, Plateau State, Nigeria. Afr J Midwifery Womens Health. 2016;10:72–77. [Google Scholar]
- 38.Ayamolowo S.J., Olajubu A.O., Akintola F.E. Perceived social support and depression among pregnant and child-rearing teenagers in Ile-Ife, Southwest Nigeria. Afr J Midwifery Womens Health. 2019;13:1–9. [Google Scholar]
- 39.Babafemi A.A., Adeleke A.J. Health and social problems of teenage pregnancy and future childbearing in Amassoma community, Bayelsa State, Nigeria. Res J Med Sci. 2012;6:251–260. [Google Scholar]
- 40.Kola L., Bennett I.M., Bhat A., et al. Stigma and utilization of treatment for adolescent perinatal depression in Ibadan Nigeria. BMC Pregnancy Childbirth. 2020;20:1–8. doi: 10.1186/s12884-020-02970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oladeji B.D., Bello T., Kola L., Araya R., Zelkowitz P., Gureje O. Exploring differences between adolescents and adults with perinatal depression-data from the expanding care for perinatal women with depression trial in Nigeria. Front Psychiatry. 2019;10 doi: 10.3389/fpsyt.2019.00761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kimbui E., Kuria M., Yator O., Kumar M. A cross-sectional study of depression with comorbid substance use dependency in pregnant adolescents from an informal settlement of Nairobi: drawing implications for treatment and prevention work. Ann Gen Psychiatry. 2018;17:53. doi: 10.1186/s12991-018-0222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kumar M., Huang K.Y., Othieno C., et al. Adolescent pregnancy and challenges in kenyan context: perspectives from multiple community stakeholders. Glob Soc Welf. 2018;5:11–27. doi: 10.1007/s40609-017-0102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Musyimi C.W., Mutiso V.N., Nyamai D.N., Ebuenyi I., Ndetei D.M. Suicidal behavior risks during adolescent pregnancy in a low-resource setting: a qualitative study. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0236269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Osok J., Kigamwa P., Huang K.Y., Grote N., Kumar M. Adversitiesand mental health needs of pregnant adolescents in Kenya: identifying interpersonal, practical, and cultural barriers to care. BMC Womens Health. 2018;18 doi: 10.1186/s12905-018-0581-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Field S., Abrahams Z., Honikman S. Adolescent mothers: a qualitative study on barriers and facilitators to mental health in a low-resource setting in Cape Town, South Africa. Afr J Prim Heal Care Fam Med. 2020;12:1–9. doi: 10.4102/phcfm.v12i1.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thabethe L.R., Mulondo S.A., Tugli A.K. Psychological experiences of pregnant students at the University of Venda, Limpopo Province, South Africa. Afr J Reprod Health. 2020;24:18–23. doi: 10.29063/ajrh2020/v24i3.2. [DOI] [PubMed] [Google Scholar]
- 48.Govender D., Naidoo S., Taylor M. I have to provide for another life emotionally, physically and financially”: understanding pregnancy, motherhood and the future aspirations of adolescent mothers in KwaZulu-Natal South, Africa. BMC Pregnancy Childbirth. 2020;20:1–21. doi: 10.1186/s12884-020-03319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong M., Myer L., Zerbe A., et al. Depression, alcohol use, and stigma in younger versus older HIV-infected pregnant women initiating antiretroviral therapy in Cape Town, South Africa. Arch Womens Ment Health. 2017;20:149–159. doi: 10.1007/s00737-016-0688-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Govender D., Naidoo S., Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. 2020;2020 doi: 10.1155/2020/5364521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carbone N.B., Njala J., Jackson D.J., et al. ‘I would love if there was a young woman to encourage us, to ease our anxiety which we would have if we were alone’: adapting the Mothers2Mothers Mentor Mother Model for adolescent mothers living with HIV in Malawi. PLoS ONE. 2019;14 doi: 10.1371/journal.pone.0217693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaye D.K. Negotiating the transition from adolescence to motherhood: coping with prenatal and parenting stress in teenage mothers in Mulago hospital, Uganda. BMC Public Health. 2008;8:1–6. doi: 10.1186/1471-2458-8-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Govender D., Naidoo S., Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. 2020;2020:1–12. doi: 10.1155/2020/5364521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xia M., Li X., Tudge J.R.H. Operationalizing urie bronfenbrenner's process-person-context-time model. Hum Dev. 2020;64:10–20. [Google Scholar]
- 55.Nagata J.M., Ferguson B.J., Ross D.A. Research priorities for eight areas of adolescent health in low- and middle-income countries. J Adolesc Health. 2016;59:50–60. doi: 10.1016/j.jadohealth.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duby Z., McClinton Appollis T., Jonas K., et al. As a Young Pregnant Girl… The Challenges You Face”: exploring the intersection between mental health and sexual and reproductive health amongst adolescent girls and young women in South Africa. AIDS Behav. 2021;25:344–353. doi: 10.1007/s10461-020-02974-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brown B.B., Larson J. Handbook of Adolescent Psychology. 2009. Peer relationships in adolescence. published online Oct 30. [DOI] [Google Scholar]
- 58.Chandra-Mouli V., Neal S., Moller A.B. Adolescent sexual and reproductive health for all in sub-Saharan Africa: a spotlight on inequalities. Reprod Health. 2021;18:1–4. doi: 10.1186/s12978-021-01145-4. 2021 181. Wiley New York. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Starrs A.M., Ezeh A.C., Barker G., et al. Accelerate progress-sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. Lancet. 2018;391:2642–2692. doi: 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- 60.Patel V., Saxena S. Achieving universal health coverage for mental disorders. BMJ. 2019;366 doi: 10.1136/BMJ.L4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Agyapong V.I.O., Farren C., McAuliffe E. Improving Ghana's mental healthcare through task-shifting- psychiatrists and health policy directors perceptions about government's commitment and the role of community mental health workers. Glob Health. 2016;12 doi: 10.1186/S12992-016-0199-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Javadi D., Feldhaus I., Mancuso A., Ghaffar A. Applying systems thinking to task shifting for mental health using lay providers: a review of the evidence. Glob Ment Health. 2017;4:1–32. doi: 10.1017/gmh.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kutcher S., Perkins K., Gilberds H., et al. Creating evidence-based youth mental health policy in Sub-Saharan Africa: a description of the integrated approach to addressing the issue of youth depression in Malawi and Tanzania. Front Psychiatry. 2019;10:542. doi: 10.3389/fpsyt.2019.00542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bhana A., Mellins C.A., Small L., et al. Resilience in perinatal HIV+ adolescents in South Africa. AIDS Care. 2016;28:49. doi: 10.1080/09540121.2016.1176676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bhana A., McKay M.M., Mellins C., Petersen I., Bell C. Family-based HIV prevention and intervention services for youth living in poverty-affected contexts: the CHAMP model of collaborative, evidence-informed programme development. J Int AIDS Soc. 2010;13:S8. doi: 10.1186/1758-2652-13-S2-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Patel V., Chisholm D., Dua T., Laxminarayan R., Medina-Mora M.L. Mental, neurological, and substance use disorders: Disease Control Priorities, 3rd ed. (Vol. 4). Dis Control Priorities, Third Ed (Volume 4) Ment Neurol Subst Use Disord 2016; published online March 21. DOI:10.1596/978-1-4648-0426-7. [PubMed]
- 67.Quarshie E.N.B., Waterman M.G., House A.O. Self-harm with suicidal and non-suicidal intent in young people in sub-Saharan Africa: a systematic review. BMC Psychiatry. 2020;20 doi: 10.1186/S12888-020-02587-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.