Abstract
Vaccine hesitancy remains a barrier to full population inoculation against highly infectious diseases. Coincident with the rapid developments of COVID-19 vaccines globally, concerns about the safety of such a vaccine could contribute to vaccine hesitancy. We analyzed 1941 anonymous questionnaires completed by healthcare workers and members of the general Israeli population, regarding acceptance of a potential COVID-19 vaccine. Our results indicate that healthcare staff involved in the care of COVID-19 positive patients, and individuals considering themselves at risk of disease, were more likely to self-report acquiescence to COVID-19 vaccination if and when available. In contrast, parents, nurses, and medical workers not caring for SARS-CoV-2 positive patients expressed higher levels of vaccine hesitancy. Interventional educational campaigns targeted towards populations at risk of vaccine hesitancy are therefore urgently needed to combat misinformation and avoid low inoculation rates.
Keywords: COVID-19, SARS-CoV-2 vaccine, Vaccine hesitancy, Healthcare staff, Vaccine safety, Israel
Introduction
The COVID-19 pandemic can be considered a global unifier, with countries worldwide all challenged to contain the spread of SARS-CoV-2. The World Health Organization (WHO) is currently orchestrating a global campaign of prevention, early diagnosis, and medical treatment. Parallel to ongoing efforts to flatten the infection curve, the development of a COVID-19 vaccine represents the holy grail for global health organizations. With numerous clinical vaccine trials in progress, the timeline for public distribution of a safe and effective vaccine is estimated to be between late 2020 and 2022 [1]. However, even vaccine availability does not guarantee sufficient population vaccination as evidenced by vaccine hesitancy [2]. Because previous research indicates that vaccine compliance remains variable and inconsistent, successful inoculation against this disease will require widespread public educational campaigns regarding vaccine safety and efficacy.
To evaluate current vaccination compliance rates among Israeli populations, we distributed a multicenter anonymous questionnaire to medical staff and civilians across the country, inquiring whether they would agree to receive a SARS-CoV-2 vaccine once available. We analyzed the 1941 responses based on occupation, exposure to either suspected or confirmed SARS-CoV-2 patients, and history of vaccinations to influenza strains prior to the COVID-19 epidemic. Responses from 829 healthcare staff were compared with 1112 members of the general population. All questionnaires were completed during the mandatory quarantine period in Israel. We hypothesized that a higher rate of vaccine compliance would be observed among medical personnel at the forefront of the COVID-19 crisis.
Surprisingly, we witnessed a high rate of vaccine skepticism among medical staff. Many responders, noncompliant with recommended vaccinations, expressed concerns regarding the safety of a rapidly-developed vaccine. In contrast, individuals considering themselves to be at a higher risk of disease, demonstrated higher vaccine acquiescence.
Our results imply that vaccination compliance, even among medically informed individuals relies on a personal risk–benefit perception that may be influenced by misinformation regarding vaccine safety. This highlights the necessity of early educational campaigns by global or country-specific health institutions, specifically targeting medical personnel. Because one of the main concerns described by study participants is the speed at which the COVID-19 vaccine is being developed, educational campaigns should focus on alleviating this apprehension in particular.
Methods
Study design
Ethical approval was granted by the Research Ethics Committee of the Galilee Medical Center before study initiation. Informed consent was requested on the introductory web page prior to survey enrollment. The anonymous web-based survey followed the American Association for Public Opinion Research (AAPOR) reporting guideline. Confidentiality of information was assured. Participants were permitted to terminate participation at any time. The survey was conducted by regions and stratified for health care personnel at academic medical centers across Israel, or members of the general population. Questionnaires were distributed electronically via Qualtrics over a 2-week period, 1 week after initiation of social distancing and quarantine regulations in Israel (March 19, 2020).
Data collection
Demographic data including sex (male or female), age (18–25, 26–30, 31–40, 41–50, 51–60 or > 60 years), geographic location, region of residence (urban or rural), marital status, and parenthood status were self-reported by responders. Participants were asked whether they vaccinate themselves or their children (if applicable) against seasonal influenza, and whether they intend to accept future COVID-19 vaccination (for themselves and their children, if applicable). Responders declining the COVID-19 vaccine option were presented with specific questions regarding the reasons for vaccine hesitancy.
Specific questions for healthcare employees included occupation (e.g. physician, nurse, technician, or other healthcare professionals), location of work (e.g. hospital, ambulatory, or community), medical discipline (e.g. internal medicine, general surgery, intensive care unit, imaging, etc.), and whether they directly diagnose, treat, or provide nursing care to patients with either suspected or confirmed SARS-CoV-2. Parallel questions for the general population included occupation status during the COVID-19 crisis (e.g. working as usual, temporary unemployment, job loss), and education level (≤ undergraduate or ≥ postgraduate).
Statistical analysis
To isolate predictors of vaccine compliance, we performed a multivariate logistic regression with age, gender, subjective personal risk, having infected relatives, being a healthcare worker, and parental status as variables. Variables for which we had a high rate of missing data, such as economic status, area of residence, and education were excluded. Dunn, Tukey or Bonferroni were used to adjust P values for multiple comparisons. We used IBM SPSS Statistics (IBM Corporation, Armonk, New York, USA) and GraphPad Prism version 8 (GraphPad Software, La Jolla, CA, USA) for all statistical analyses.
Results
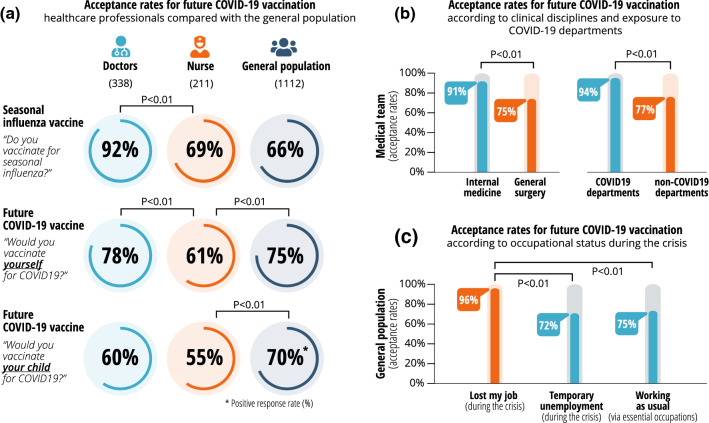
Surprisingly, our findings suggest that employment within the healthcare sector does not significantly influence respondents’ acceptance or rejection of a potential COVID-19 vaccine (Fig. 1). A positive predicting factor to accept the future vaccine is a self-perception of high-risk for severe COVID-19 infection. Interestingly, age was not considered to be a high-risk factor. Healthy septuagenarians with no clinical history apparently disregard age as a contributing factor as to whether or not to be vaccinated. Notably, sex is a positive predicting factor with males more likely to accept the potential COVID-19 vaccine. The prominent trend amongst parents indicated that having a child is a negative predictor for accepting future vaccination (Fig. 1).
Fig. 1.
Forest plot demonstrates the degree to which respondents’ demographics affect future vaccine acceptance. Combined data analysis of 1941 respondents lists the different parameters plotted with overlap. Having children is the strongest negative predictor for acceptance of potential COVID-19 vaccination. Positive predictors include sex (male), and self-perception of disease risk. Other characteristics, such as age and occupation within the healthcare system, do not significantly influence responders’ decisions whether to accept vaccination
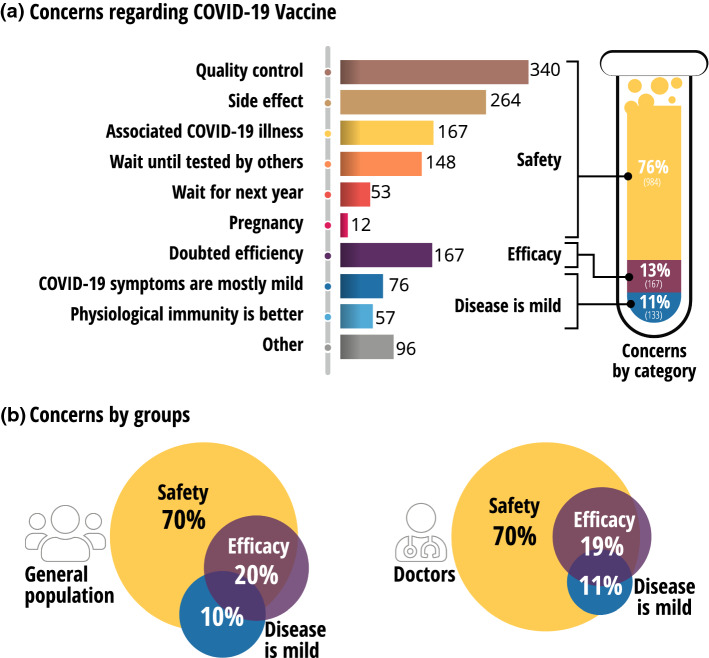
According to our survey, the most significant positive predictor for acceptance of a potential COVID-19 vaccine is current influenza vaccination. People currently vaccinated against seasonal influenza have a strong tendency to accept a future COVID-19 vaccine. Interestingly, the rate of acceptance for a COVID-19 vaccine among physicians and nurses overall is lower than their acceptance rates of seasonal influenza vaccination (Fig. 2a). Further analysis (Fig. 2a) revealed that vaccine acceptance among doctors (78%) is significantly higher than nurses (61%; P < 0.01), which compares to 75% in the entire population. When comparing subspecialties (Fig. 2b), healthcare workers in internal medicine departments display a significantly higher vaccine acceptance rate (91%) than those in general surgery departments (75%; P < 0.01). As expected, medical teams in COVID-19 departments show higher acceptance rates (94%) compared to those in non-COVID-19 departments (77%; P < 0.01).
Fig. 2.
Acceptance rate of future COVID-19 vaccine among doctors, nurses, and the general population. a Compliance for seasonal influenza vaccination and for potential COVID-19 vaccination demonstrate high acceptance rates among doctors but a low acceptance rate among nurses. b Rate of vaccine acceptance is significantly higher among health workers within internal medicine and COVID-19 dedicated departments. c A significantly higher compliance for potential future vaccination among responders who lost jobs during the crisis
Our survey demonstrates a significantly higher intended COVID-19 vaccine compliance (96%) among responders who lost their job during the crisis, compared to those with essential occupations who continued working (72%; P < 0.01), or who stayed home but are confident about returning to work when possible (75%; P < 0.01, Fig. 2c).
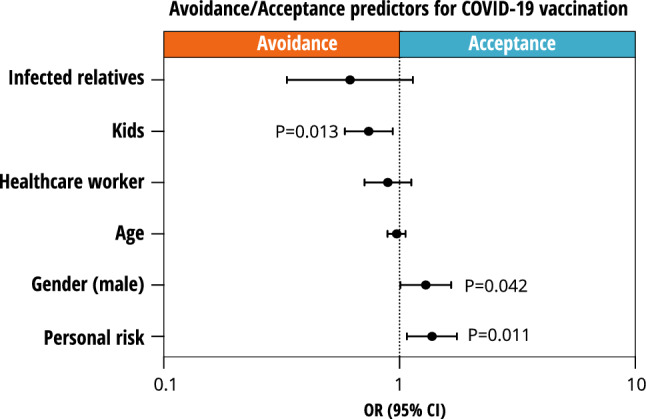
Of greatest concern to both physicians and the general population alike are fears of the vaccine’s safety, given its rapid development (Fig. 3). The most frequently noted safety considerations include quality control, potential side effects, and associated COVID-19 illness.
Fig. 3.
Concerns among responders regarding potential COVID-19 vaccines. a A list of concerns regarding potential COVID-19 vaccines. b Venn diagrams combining the concerns into three main categories of safety, efficacy, and mild symptoms of the disease
Discussion
Global, government efforts to combat the COVID-19 pandemic have included a variety of strict measurements including intermittent lockdowns of regions and countries. The healthcare sector has become one of the most important leaders in efforts against COVID-19, despite shortages of critical protective equipment and resources that impact the survival rates of patients flooding COVID-19 departments. We hypothesized that the current COVID-19 pandemic would promote compliance with potential vaccines, especially among healthcare workers. The data demonstrate several positive predictors for vaccination: status as a physician, employment in healthcare settings caring specifically for SARS-CoV-2 positive patients, unemployment during the quarantine period, and male sex; negative predictors include occupation as a nurse and parenthood.
Our results indicate that healthcare providers not caring for COVID-19 positive patients appear to trust a COVID-19 vaccine less than the general population, with nurses more vaccine-hesitant than physicians. Although nurses have slightly higher rates of annual influenza vaccination than the general population, they expressed more hesitancy about COVID-19 inoculation than the general population. This low vaccination acceptance rate among nurses could negatively impact the future vaccination compliance of individuals who coincidentally engage with vaccine-hesitant nurses on a professional or personal level.
We assumed that the devastating economic consequences of COVID-19-related restrictions would lead to an increase in compliance rates for potential future vaccines among the general population, due to a desire to prevent catastrophic lay-offs, high underemployment levels, and school closures. Unemployment and job insecurity are indeed positive predictors for acceptance of COVID-19 vaccination, contrasting with parenthood as a negative predictor. A possible explanation for this negative parenthood effect is that parents have heightened concerns for their own safety; potentially deleterious effects of a vaccine could compromise their ability to care for their children. Future research should elucidate the reasons underlying this intriguing association between parenthood and vaccination avoidance.
There is a positive association between male sex and acceptance of COVID-19 vaccination. Several independent reports demonstrate higher risks for COVID-19 complications, infectivity, and death among males [3]. While other sex-based health disparities such as cardiovascular disease, chronic respiratory disease, and cancer have been extensively reviewed [4], the sex-based difference in COVID-19 mortality may bias men to accept a vaccine.
Despite a general “herd immunity” achieved by high vaccination rates [5], even higher compliance is necessary among communities with individuals with higher disease risks. Sustained encouragement of particularly vulnerable people to accept the future COVID-19 vaccine could lead to reduced morbidity and mortality while simultaneously releasing valuable healthcare resources to deliver equally important ambulatory support.
Government-mandated social isolation to avoid viral transmission has led to rising unemployment rates and school suspensions [6], leaving workers in tenuous economic situations and parents struggling to provide a residual educational framework at home [7]. Additional emotional distress in the face of extensive media coverage of the rising numbers of casualties, overburdened health systems, and insufficient government responses to COVID-19 has perhaps fostered communal anxieties and distrust in preventative healthcare. These fears could also be contributing to wariness of the safety of a potential COVID-19 vaccine among the general public.
Concerns among responders regarding a potential COVID-19 vaccine provide important targets for possible interventional educational programs to enhance vaccination rates [8]. Of greatest concern to Israeli healthcare and civilian respondents were issues related to quality control and side effect profiles of a potential COVID-19 vaccine. While current literature covers extensively vaccine efficacy and safety [9, 10], the vast majority of the responders’ concerns, among healthcare and non-healthcare workers alike, are due to the speed of development. These concerns could hamper the achievements of the scientific community and its attempts to disseminate the vaccine. We, as a scientific community, must act to educate, inform, and intervene to increase COVID-19 vaccine compliance rates in the entire population.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580:576–577. doi: 10.1038/d41586-020-01221-y. [DOI] [PubMed] [Google Scholar]
- 2.Omer SB, Salmon DA, Orenstein WA, DeHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. NEJM. 2009;360:1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 3.Galbadage T, Peterson BM, Awada J, Buck AS, Ramirez DA, Wilson J, et al. Systematic review and meta-analysis of sex-specific COVID-19 clinical outcomes. Front Med. 2020 doi: 10.1101/2020.05.11.20098673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 5.Rashid H, Khandaker G, Booy R. Vaccination and herd immunity: what more do we know? Curr Opin Infect Dis. 2012;25:243–249. doi: 10.1097/QCO.0b013e328352f727. [DOI] [PubMed] [Google Scholar]
- 6.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Heal. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020;35:325–330. doi: 10.1007/s10654-020-00634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corey BL, Mascola JR, Fauci AS, Collins FS. A strategic approach to COVID-19 vaccine R&D. Science. 2020;368:948–950. doi: 10.1126/science.abc5312. [DOI] [PubMed] [Google Scholar]
- 10.Dean NE, Gsell P-S, Brookmeyer R, De Gruttola V, Donnelly CA, Halloran ME, et al. Design of vaccine efficacy trials during public health emergencies. Sci Transl Med. 2019;11:eaat0360. doi: 10.1126/scitranslmed.aat0360. [DOI] [PMC free article] [PubMed] [Google Scholar]