Abstract
Background
Virtual reality (VR) produces a virtual manifestation of the real world and has been shown to be useful as a digital education modality. As VR encompasses different modalities, tools, and applications, there is a need to explore how VR has been used in medical education.
Objective
The objective of this scoping review is to map existing research on the use of VR in undergraduate medical education and to identify areas of future research.
Methods
We performed a search of 4 bibliographic databases in December 2020. Data were extracted using a standardized data extraction form. The study was conducted according to the Joanna Briggs Institute methodology for scoping reviews and reported in line with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines.
Results
Of the 114 included studies, 69 (60.5%) reported the use of commercially available surgical VR simulators. Other VR modalities included 3D models (15/114, 13.2%) and virtual worlds (20/114, 17.5%), which were mainly used for anatomy education. Most of the VR modalities included were semi-immersive (68/114, 59.6%) and were of high interactivity (79/114, 69.3%). There is limited evidence on the use of more novel VR modalities, such as mobile VR and virtual dissection tables (8/114, 7%), as well as the use of VR for nonsurgical and nonpsychomotor skills training (20/114, 17.5%) or in a group setting (16/114, 14%). Only 2.6% (3/114) of the studies reported the use of conceptual frameworks or theories in the design of VR.
Conclusions
Despite the extensive research available on VR in medical education, there continue to be important gaps in the evidence. Future studies should explore the use of VR for the development of nonpsychomotor skills and in areas other than surgery and anatomy.
International Registered Report Identifier (IRRID)
RR2-10.1136/bmjopen-2020-046986
Keywords: virtual reality, medical education, medical students, virtual worlds, digital health education
Introduction
Background
Traditionally, medical education comprises both theoretical learning in classrooms and clinical training in hospitals where students are able to gain clinical experience [1]. This is mainly done by means of face-to-face teaching. However, there has been a recent shift to the greater adoption of technology in medical education. This has been accelerated by the COVID-19 pandemic. After it was learned that transmission of COVID-19 is decreased by social distancing, educators were forced to rethink how best to teach students while decreasing face-to-face teaching [2]. To solve this problem, digital education has been proposed as a possible solution to improve medical education. Digital education (also known as electronic education or e-learning) is defined as the act of teaching and learning by means of digital technologies [3]. It is a broad term that encompasses a large number of different modalities, from a simple e-book to complex modalities such as virtual reality (VR), mobile learning, virtual patients (VPs), serious gaming and gamification, and digital skills trainers [4]. Although there is a wide range of digital education tools available, in this scoping review we will be focusing on investigating a single modality—VR.
VR is defined as an educational tool that uses computer technology to create a 3D image or environment that one can interact with in a seemingly real or physical way [5]. VR is a broad concept that has many different tools and applications. VR simulators can be classified into surgical VR simulators, 3D anatomical models, virtual dissection tables, virtual worlds or environments, and mobile VR. Surgical VR simulators consist of an interface connected to mechanical devices or haptic units and can be displayed on any screen but most commonly using a desktop [6]. Surgical VR simulators are most effective at developing users’ technical psychomotor skills, such as for endoscopic surgery, because they can be used repeatedly and require very little time to set up [7]. 3D anatomical models allow users to explore 3D models by manipulating and rotating the model [8]. They are most commonly developed from 2D radiological images using different types of software tools [8]. Virtual dissection tables often overlap with 3D anatomical structures but are distinct in that they allow manipulation to cut digital models to reveal cross-sectional images; examples include the Anatomage Table [9]. Virtual worlds are 3D virtual environments based on multiplayer web-based gaming, freeing users from the constraints of location and time. Virtual worlds representing a clinical setting have been used to train emergency personnel on the management of situations involving mass casualties or major incidents [10-12]. Avatars representing patients can be generated to provide a more realistic simulation for the user [13]. Mobile VR refers to VR modalities designed for use on a touch screen mobile phone or tablet; examples include the Touch Surgery app [14].
VR can have diverse application in medical education. It has so far been most commonly used for the development of technical competencies, such as surgical skills, or for developing the ability to visualize anatomy in 3D. Examples of its applications include surgical technique training, the development of 3D visualization skills, and training for procedures such as cardiopulmonary resuscitation (CPR) [15-18]. However, VR can also be used to teach soft skills such as empathy and communication skills [13,19,20]. This commonly involves the use of avatars in a virtual world mimicking patients that respond in a certain way so that users can communicate with them [19]. Considering the large range of skills that can be taught with VR, coupled with the widespread reach and convenience of digital education, it holds great potential in the future of medical education.
Given the wide array of tools available in the VR toolbox and the diverse areas in which VR can be applied, there is a need to systematically identify the current VR applications used in medical education, as well as to identify any gaps in the current research of VR in medical education as reported in the literature. Although there are reviews aiming to map different applications of VR used in other types of health care education such as nursing and dentistry education, there seem to be none focusing on medical students’ education [21,22]. Existing systematic reviews on VR in medical education mainly focus on assessing the effectiveness of VR within surgical disciplines, more specifically laparoscopic surgery and neurosurgery [23,24]. This scoping review aims to have a much broader focus by mapping out the extent of VR applications, rather than focusing on the effectiveness of VR in a specific subject.
Objective
The objective of this scoping review is to identify the different VR tools and applications in undergraduate or preregistration medical education as reported in the literature. We also aim to identify any gaps in the existing literature and provide suggestions for future research on the use of VR in medical education.
Methods
Overview
The scoping review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews [25], which comprises the following six stages: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarizing, and reporting the results; and (6) stakeholder consultation. The results were reported in line with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) [26]. The protocol was registered on the Open Science Framework [27].
Stage 1: Identifying the Research Question
The objective of this scoping review is to outline the different VR modes available and the applications of VR in undergraduate or preregistration medical education. In line with the objectives of this scoping review, we have developed the following research questions:
How is VR used in undergraduate or preregistration medical education?
What are the main features of the VR applications in undergraduate or preregistration medical education?
What VR tools are available for undergraduate or preregistration medical education?
To which aspects of undergraduate or preregistration medical education has VR been applied?
Stage 2: Identifying Relevant Studies
A comprehensive search of the literature was performed using the following electronic databases: MEDLINE (Ovid), Embase (Elsevier), Cochrane Central Register of Controlled Trials (Wiley), and Education Resources Information Centre (Ovid). As a first step, a limited search using keywords was conducted in MEDLINE. The search strategy was piloted to check the appropriateness of the keywords and databases. In all retrieved papers, an analysis of the words contained within the title and abstracts as well as index terms was performed to develop a full search strategy. Thereafter, a second search using all the identified keywords and index terms was performed across all databases in December 2020. Finally, the third step included screening of the reference lists of all studies selected for this scoping review to look for additional sources. The complete search strategies for all databases can be found in Multimedia Appendix 1. The initial MEDLINE search strategy was developed with the help of a medical librarian experienced in the field. The search period ranged from 2010 to the present. We chose to start from 2010 because most literature pertaining to VR for education was published in recent years, as shown by our previous work in this area [28]. The capabilities of digital technology and VR have also changed substantially over time. We searched for literature in the English language only. All references identified were imported into the reference manager software, EndNote X9 (Clarivate). The references from different electronic databases were combined and any duplicate records removed.
Stage 3: Study Selection
The study selection followed a two-step screening process, which consisted of a title and abstract screening, followed by a full-text review. In both steps, 2 independent reviewers (JHW and SV) screened the articles against the eligibility criteria. Any disagreements were discussed, and if no consensus could be reached, a third reviewer (BMK) was consulted. We considered eligible studies based on the criteria presented in Textbox 1.
Full inclusion and exclusion criteria.
Inclusion criteria
Studies on undergraduate or preregistration medical students in any geographical setting
Studies involving the use of virtual reality together with another modality such as immersive virtual reality, virtual reality–based serious gaming, and virtual reality–based virtual patients
All primary studies, regardless of study design, and relevant systematic reviews
Exclusion criteria
Studies focusing only on virtual patient simulation, augmented reality, mixed reality, or serious gaming, without any involvement of virtual reality
Studies published before 2010
Studies in languages other than English
Opinion pieces, viewpoints and conceptual frameworks, and conference abstracts
The first step involved the screening of the title and abstract of the studies using EndNote X9. To qualify for the full-text scan, the title and abstract had to (1) focus on the use of VR for educational use only and (2) have medical students as the target population. VPs, that is, computer-generated programs that simulate real-life clinical scenarios, can also be delivered in a VR format. In this scoping review, we included VR-based VPs. We also included studies on VR-based serious gaming education. Augmented reality (VR superimposed onto the real-world environment) [22] and mixed reality (mixing of both virtual and digital elements, allowing one to interact with both simultaneously) [29] are distinct entities that make use of VR and are not classified as VR. Studies focusing solely on mixed reality or augmented reality were excluded from this review.
We considered all primary studies, including experimental, observational, and qualitative study designs. Systematic reviews and meta-analyses were also considered. The full texts of the included studies were retrieved and their citation details imported. Studies excluded at this stage are described in Figure 1. This process followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [30], and 2 review authors (JHW and SV) verified the final list of included studies.
Figure 1.
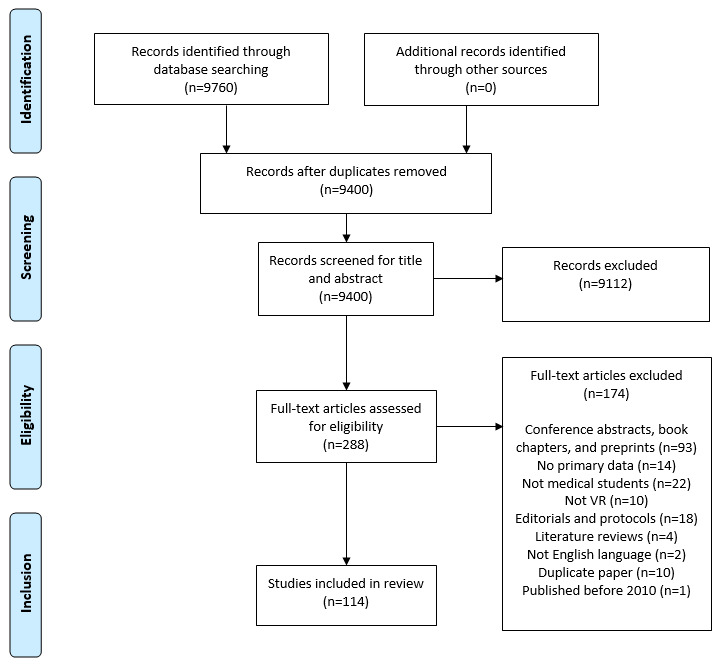
Flow diagram of the literature search and study selection process. VR: virtual reality.
Stage 4: Charting the Data
Relevant data were extracted from all included studies by 2 independent reviewers (JHW and SV). A structured data recording form developed by the reviewers was used and the information recorded using Microsoft Excel 2013. The full data extraction form can be found in Multimedia Appendix 2. The data extraction tool was piloted and revised as necessary during the process of extracting data from each study. Any disagreements that arose between the reviewers were resolved through discussion, and a third review author (BMK) acted as an arbiter when disagreements could not be resolved. We contacted the study authors for any missing or incomplete data.
Stage 5: Collating, Summarizing, and Reporting the Results
To characterize and summarize the results, a map of the data extracted from the included papers was presented in a diagrammatic or tabular form. In alignment with the objectives of this study, we provided an overview of the target participants, content of VR programs, types of studies included, and the context of each included study. The tabulated and charted results were accompanied by a narrative summary, which described how the results met the objectives and aims of this scoping review. We reported the findings in line with the PRISMA-ScR checklist [26]. Using the gap identification process, we detected areas where there was a paucity of data on VR content and its application in undergraduate or preregistration medical education.
We classified VR modalities based on the extent of immersion or interactivity. Immersion can be defined as the sensation of being disconnected with reality [31] or the amount of presence experienced by the user due to the illusion rendered by the VR modality [32]. The level of immersion is largely dependent on the number of senses the user uses to interact with the VR environment: the more the senses used, the more immersive the VR environment is said to be. This reflects the system’s technical capabilities: the greater the number of sensorimotor contingencies the system has, the more immersive it will seem [33]. VR has generally been classified into two levels of immersion: immersive VR and nonimmersive VR. Fully immersive VR is defined as VR combined with devices that allow the user to visualize the recorded image in 3D in their entire field of vision and detect eye motions and leap motions of the hands. Nonimmersive VR involves computer-generated experiences on a desktop with which the user interacts by using a mouse [34]. For this study, we will define a third entity, semi-immersive VR, which does not fall into either of the 2 categories (eg, head-mounted devices that capture eye motions but do not capture hand motions and desktop-based VR, which provides tactile feedback).
Interactivity in VR refers to the extent to which the user can influence the content or form of the VR environment [32]. This can be classified into low, moderate, or high levels of interactivity. A low level of interactivity simply allows the user to choose information, such as using a mouse to select options that display different anatomical models. A moderate level of interactivity allows the user to add or delete objects in the VR environment, such as a virtual dissection tool that allows users to add or delete various anatomical structures individually. A high level of interactivity refers to when the VR environment responds appropriately to the user’s input, such as using a joystick to manipulate the VR environment in a surgical simulator.
Step 6: Stakeholder Consultation
A stakeholder consultation was undertaken on August 12, 2021, with the aim of discussing and improving the presentation of our findings. No ethics approval was required as per Nanyang Technological University ethics board guidance. The stakeholder consultation consisted of a 1-hour-long web-based seminar. The audience comprised 18 researchers in the fields of medical education, digital health professions education, and health service research, as well as educators. The stakeholders were invited to share any comments, questions, or suggestions in relation to our study. In addition, we also specifically asked them to share their views on the most important aspects of our findings for researchers and educators, recommendations for future research, and suggestions on any other research in the field of VR or medical education that we should take note of. We have analyzed and presented our findings in this manuscript in line with the information collated through this stakeholder consultation.
Results
Included Studies
Our searches identified a total of 9400 studies after duplicates were removed, of which 288 (3.06%) were selected for full-text review. Of these 288 studies meeting the criteria for full-text review, 174 (60.4%) did not meet the inclusion criteria, resulting in 114 (39.6%) studies being included in this scoping review (Figure 1).
Study Characteristics
Of the included studies, most studies were either randomized controlled trials (RCTs; 47/114, 41.2%) or other experimental design studies (eg, before-and-after and cross-over studies; 49/114, 42.9%). Of the 114 studies, 14 (12.3%) were cross-sectional studies [35-49], 3 (2.6%) were case series or case studies [42,50,51], and 1 (0.9%) was a meta-analysis that examined the effectiveness of 3D anatomical models in teaching anatomy [52], which found that 3D anatomical models yielded significantly better results for user satisfaction and perceived effectiveness compared with conventional 2D teaching methods. An overview of the study characteristics is provided in Table 1.
Table 1.
Characteristics of included studies (N=114).
| Domain and feature | Values, n (%) | |
| Study design | ||
|
|
Randomized controlled trial | 47 (41.2) |
|
|
Experimental (eg, cross-over and before-and-after studies) | 49 (42.9) |
|
|
Cross-sectional studies | 14 (12.3) |
|
|
Cases studies and case series | 3 (2.6) |
|
|
Meta-analysis | 1 (1.1) |
| Location (by country) | ||
|
|
United States | 30 (26.3) |
|
|
Germany | 11 (9.6) |
|
|
United Kingdom | 11 (9.6) |
|
|
Canada | 9 (7.9) |
|
|
Denmark | 9 (7.9) |
|
|
Others | 44 (38.6) |
| Number of students | ||
|
|
0-50 | 76 (66.7) |
|
|
51-100 | 20 (17.5) |
|
|
>100 | 18 (15.8) |
| Year of study of studentsa | ||
|
|
1 | 31 (27.2) |
|
|
2 | 29 (25.4) |
|
|
3 | 26 (22.8) |
|
|
4 | 23 (20.2) |
|
|
5 | 19 (16.7) |
|
|
6 | 19 (16.7) |
| Study setting | ||
|
|
University | 108 (94.7) |
|
|
Hospital | 6 (5.3) |
| VRb modalities used | ||
|
|
Surgical VR simulator | 69 (60.5) |
|
|
3D anatomical model | 14 (12.2) |
|
|
Virtual dissection table | 4 (3.5) |
|
|
Virtual worlds | 21 (18.4) |
|
|
Mobile VR | 4 (3.5) |
|
|
Others | 2 (1.8) |
| Mode of access | ||
|
|
Commercial product | 84 (73.6) |
|
|
Developed in-house | 30 (26.3) |
|
|
Both commercial and in-house elements | 5 (4.4) |
| Input devices | ||
|
|
Haptic tools | 71 (62.2) |
|
|
Mouse | 21 (18.4) |
|
|
Touch screen | 8 (7.4) |
|
|
Game controllers | 5 (4.4) |
|
|
Joysticks | 2 (1.8) |
|
|
VR gloves | 2 (1.8) |
|
|
Headset | 4 (3.5) |
|
|
Stereoscopic glasses | 1 (0.9) |
| Delivery devices | ||
|
|
Screen | 100 (87.7) |
|
|
Headset | 13 (11.4) |
|
|
3D projector with stereoscopic glasses | 1 (0.9) |
| Extent of immersion | ||
|
|
Fully immersive | 20 (17.5) |
|
|
Semi-immersive | 68 (59.6) |
|
|
Nonimmersive | 26 (22.8) |
| Extent of interactivity | ||
|
|
High | 79 (69.3) |
|
|
Moderate | 19 (16.7) |
|
|
Low | 16 (14) |
| Subject taughta | ||
|
|
Surgical psychomotor skills | 71 (61.4) |
|
|
Anatomy | 21 (18.4) |
|
|
Clinical managementc | 16 (14) |
|
|
Radiology | 4 (3.5) |
|
|
Nonsurgical psychomotor skills | 3 (2.6) |
|
|
Communication | 3 (2.6) |
| Mode of teaching | ||
|
|
Self-directed | 71 (62.3) |
|
|
Guided | 42 (36.8) |
|
|
Not availabled | 1 (0.9) |
| Duration of teaching | ||
|
|
<1 day | 35 (30.7) |
|
|
1 day to 1 month | 28 (24.6) |
|
|
1-6 months | 16 (14) |
|
|
6-12 months | 8 (7) |
|
|
>1 year | 4 (3.5) |
|
|
Not specified | 23 (20.1) |
| Timing of assessment | ||
|
|
Immediate | 96 (84.2) |
|
|
Delayed | 17 (14.9) |
|
|
Not availabled | 1 (0.9) |
| Individual or group deliverya | ||
|
|
Individual | 97 (85.1) |
|
|
Individual and group | 7 (6.1) |
|
|
Group | 9 (7.9) |
|
|
Not availabled | 1 (0.9) |
aPercentages do not add up to 100% because of overlap among the included studies.
bVR: virtual reality.
cExamples include cardiopulmonary resuscitation, pediatric respiratory management, clinical presentation, and trauma management.
dThe systematic review did not investigate any mode of teaching.
Among the 96 RCTs and experimental studies included, 50 (52%) compared VR against a traditional learning method (eg, box trainer and video-based lectures), 27 (28%) evaluated VR modalities by changing another variable (eg, VR vs VR with warm-up and VR with guidance vs no guidance) [9,14,48,49,53-94], 14 (15%) did not have any intervention (eg, before-and-after studies and learning curves) [95-109], and 5 (5%) compared a VR modality against another type of VR modality (eg, LapSim vs ProMIS) [110-113].
Of the 114 studies, 30 (26.3%) were from the United States, 11 (9.6%) each from the United Kingdom and Germany, 9 (7.9%) each from Canada and Denmark, and 13 (11.4%) from Asia. Other countries were uncommon, with notably no studies being published from Africa or any low-income country.
Ethics approval was mentioned in 61.4% (70/114) of the studies, and the source of funding was mentioned in 40.4% (46/114) of the studies. Among the 46 studies that received funding, 19 (41%) received funding from the university, 12 (26%) received charitable funding, 9 (20%) received government-backed funding, and 6 (13%) received private funding.
There was generally an increase in frequency of publication from 2010 to 2020, with 7.9% (9/114) of the studies published in 2010 and 17.5% (20/114) of the studies published in 2020 (Figure 2).
Figure 2.
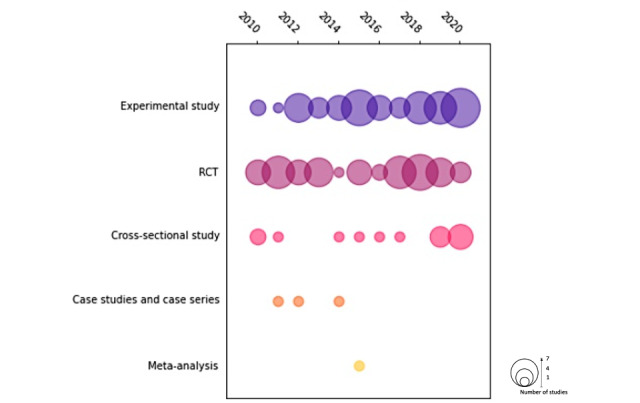
Publication frequency by year of the articles included in this study. RCT: randomized controlled trial.
On the basis of our review of the literature on VR in medical students’ education, we categorized the findings from the included studies as follows: (1) students, (2) VR modalities, (3) development, (4) input and output devices, (5) extent of immersion and interactivity, (6) subjects taught, (7) teaching strategies, and (8) assessment methods. These categories will be explored next.
Students
Of the 114 studies, 76 (66.7%) involved ≤50 students, 20 (17.5%) involved 51-100 students, and 18 (15.8%) involved >100 students. All years of study of medical students were generally well represented, with a slight tendency to include lower-year medical students.
Most of the studies (108/114, 95.7%) took place in a university setting, with the remainder (6/114, 5.3%) taking place in a hospital setting [111,114-118].
VR Modalities
Of the 114 papers, 69 (60.5%) concerned surgical VR simulators [36,37,42,46,47,51,53,55-57,59,66,67,73-75,79,81-84,86,88,90-94,96, 98-100,103,105,107-138], 20 (17.5%) used virtual worlds or virtual environments [39-41,43, 44,48,50,58,69,70,76-78,101, 139-145], 15 (13.2%) used 3D anatomical models, 4 (3.5%) used virtual dissection tables [9,62,97,127,146], 4 (3.5%) used mobile VR [14,63,65,147], 1 (0.9%) examined the use of a virtual palpation simulator, and 1 (0.9%) used a virtual ultrasound simulator (Figure 3).
Figure 3.
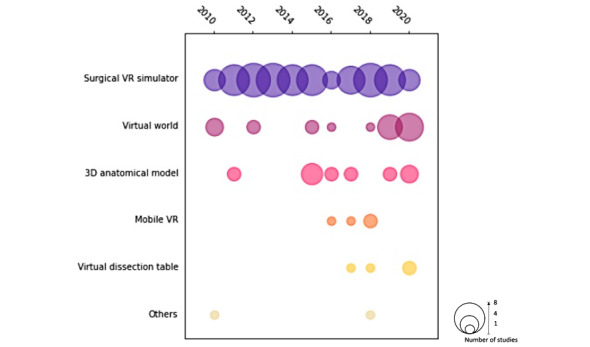
Number of papers of each VR modality published by year. VR: virtual reality.
Most surgical VR simulators were evaluated using either RCTs (34/69, 49%) or experimental studies (29/69, 42%). Similarly, most 3D anatomical models were also evaluated by either RCTs (6/15, 40%) or experimental studies (6/15, 40%). Virtual worlds were mainly evaluated using experimental studies (8/20, 40%) or cross-sectional studies (8/20, 40%). Mobile VR was mainly evaluated through RCTs (3/4, 75%), whereas virtual dissection tables were mainly evaluated through experimental studies (3/4, 75%; Figure 4).
Figure 4.
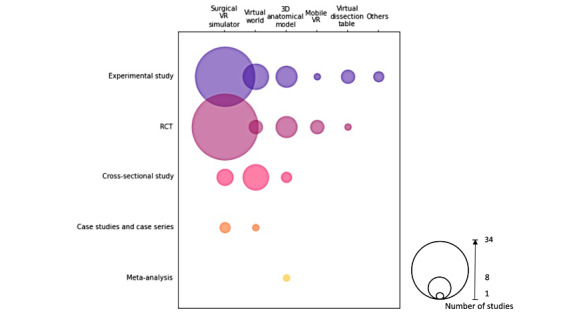
VR modality described against study design. RCT: randomized controlled trial; VR: virtual reality.
Among the studies using surgical simulators, approximately one-third (22/69, 32%) [42,53,59,74,82,86,89,91, 94,105,110,111,113, 119,122,123,128,130, 132,136,148] used some version of LAP Mentor [149]. There were also a notable number of studies using ARTHRO Mentor [150] (7/69, 10%) [36,56,66,110,112,120,121], Eyesi Virtual Simulator (3/69, 4%) [37, 51,133], da Vinci Surgical Simulator (4/69, 6%) [90,96,117,118], dV-Trainer (4/69, 6%) [82,88,103,126], VBLaST suturing simulator (3/69, 4%) [49,84,99], and SimSurgery (3/69, 4%) [106,125,131]. Other surgical VR simulators were uncommon.
Among the studies using 3D anatomical models, most (11/15, 73%) were developed in-house by the authors themselves, with the exception of some studies in which commercial products were used. They include Surgical Theater’s Precision VR visualization platform, which is a commercial product used to visualize cerebrovascular anatomy using a controller [35], and DIVA, which is a 3D VR platform used for craniofacial trauma education [151].
Among the 20 studies involving virtual worlds, 15 (75%) were developed in-house, whereas the remaining 5 (25%) used virtual worlds that are commercial products, including products such as MicroSim [58], Body Interact [141], Otago virtual hospital [50], a beta version of CPR VR learning software [70], and Medical Realities VR [87].
Among the 4 studies involving the use of virtual dissection tables, 2 (50%) used the Anatomage Table [9,146], 1 (25%) used the Sectra Virtual Dissection Table [97], and 1 (25%) used the VH Dissector Pro [62].
Among the 4 studies involving the use of mobile VR, 3 (75%) used the Touch Surgery app, a mobile surgical training platform [14,65,152], and 1 (25%) used the aVOR app, a teaching, training, and testing tool for the vestibulo-ocular reflex system and its disorders [63].
The most common commercial products described in the literature are summarized in Textbox 2.
Common commercial virtual reality (VR) products used in the included studies.
VR modalities and types of tools used
-
Surgical VR simulators
LAP Mentor
ARTHRO Mentor
Eyesi Virtual Simulator
da Vinci Surgical Simulator
dV-Trainer
VBLaST suturing simulator
-
Virtual worlds
MicroSim
Body Interact
Otago virtual hospital
-
Virtual dissection tables
Anatomage Table
Sectra Virtual Dissection Table
VH Dissector Pro
-
Mobile VR
Touch Surgery app
aVOR app
Development
Of the 114 studies, 35 (30.7%) used a VR modality that was developed in-house. The information used in development can be broadly classified into four different categories: development of 3D anatomical models, virtual worlds, VPs (clinical scenarios), and probes and haptic devices.
Of the VR modalities developed in-house, 37% (13/35) were 3D anatomical models. Of these 13 studies, 12 (92%) developed 3D anatomical models that used some form of transverse 2D images in their development, either through magnetic resonance imaging or computed tomography images or transverse cross-sectional images of human cadavers. The information was imported into a software program that could convert the 2D images into 3D models (eg, Mimics, Macromedia Flash, and After Effects) [153]. Any defects or irregularities would then be smoothened out manually by means of the software. The model would then be imported into VR platforms (eg, Unreal Engine VR platform and HTC Vive software development kit) where it could be displayed on various VR modalities. The remaining study used 2D diagrams and anatomical descriptions from textbooks and journals [85].
Of the VR modalities developed in-house, 43% (15/35) were virtual worlds. Virtual worlds followed a somewhat similar development pathway but differed in terms of the software and information used and the outcomes of development. Whereas 3D anatomical models aim to produce a model that can be manipulated by the user on a screen, the structures in 3D worlds do not require as great a degree of manipulation; they mainly involve the users exploring the models and interacting with other users through an avatar, and this influences the software used in development. Structures in virtual worlds were mainly built from standard building shapes such as blocks, spheres, and tubes and are called primitives or prisms [40]. Of the 15 studies focusing on virtual worlds, 5 (33%) used the Second Life platform to develop the virtual world structure, whereas 3 (20%) used Amira. Once the virtual world was completed, users would download the program on a desktop and have to learn the interface before accessing the resources in the world.
Of the 15 studies that examined virtual worlds, 4 (27%) used VPs [41,43,50,101]. The VPs used in the simulations were designed with a predefined set of responses to questions asked by the user. These responses are usually written onto a script and programmed into the VP. In addition, the modality in the study by Guetterman et al [101] used intelligent VPs that can detect body motion as well as facial expression and speech and then modify their responses appropriately and thus can also train the user in nonverbal behaviors. Another modality incorporated a dynamic analysis process where the program was able to compare the user’s performance with that of peers and expert choices and provide feedback in real time [41]. The study by Kleinert et al [43] also noted the importance of incorporating established game design elements to promote long-time motivation, such as a reward system.
Of the 35 studies that used a VR modality that was developed in-house, 7 (20%) examined the development of probes and haptic devices. Of these 7 studies, 5 (71%) [48,57,112,145,154]. used a surgical VR simulator that was developed in-house and described the processes involved in fine-tuning the VR simulator for students’ use. The probes and haptic devices used in these studies were mainly commercially acquired, but the fine-tuning of these devices was performed in-house. This was mainly done by examining the learning curves of the VR simulators and determining the accuracy and reproducibility of the probes and haptic devices involved. This allowed researchers to determine the optimal sensitivity of the probes and the optimal duration of training. Of the 7 studies, the remaining 2 (29%) described the development of novel VR simulators with unique haptic devices. The study by Karadogan et al [104], which described the use of a virtual palpation simulator, was mainly focused on designing a haptic device needed to quantify the amount of force needed to be applied to the haptic device to instill a change in the VR environment. This was measured using the Weber fraction, which is defined as the ratio of the minimum difference that a person can distinguish to the standard intensity of the stimulus in a sensory modality. The second study involved designing a virtual ophthalmoscope that used a cylindrical plastic canister to view photos of the fundus using the ophthalmoscope [46]. The study also focused on adopting gamification to improve students’ use of the simulator.
In all the studies with VR modalities developed in-house, the main persons in charge of development of the VR modality were the authors themselves. In addition, 60% (21/35) of the studies mentioned the inclusion of additional experts such as ear, nose, and throat (ENT) surgeons; radiologists; or other specialists in the area of interest to help with validation of the study [37,43,44,46,50,58,63-66,71,72,77,78,85,88,120,121,133, 147,155].
There were generally very few frameworks or theories applied in the development of VR simulators in medical education. Among the 35 studies that used a VR modality developed in-house, only 3 (9%) involved any frameworks or theories when developing the VR modality. The study by Lorenzo-Alvarez et al [78], which investigated the design of game-based learning in virtual worlds, used theories on human learning, especially behaviorism, cognitivism, and constructivism. The study by Makransky et al [44], which investigated the feasibility of developing a desktop VR laboratory simulation on the topic of genetics, used feedback based on the cognitive theory of multimedia learning. The study by Hayward et al [41], which designed a novel tool for teaching diagnostic reasoning, used script theory, which states that the clinician draws upon prestored reasoning pathways in the form of illness scripts or profiles when navigating new patient encounters.
Input and Output Devices
Of the 114 studies, 71 (62.2%) used a haptic surgical tool as their input interface [36,37,42,47,49,51,55,56,59,66,67,73-75,79, 81-84,88-91,94,96,99,100,102-113,115-126,128,129,131-138,148,156] (Figure 4). The next most common input device was a mouse (21/114, 18.4%) [8,38-41,43-45,50,54,58,61,62,64,68,71,76-78, 80,92,101,139-142,144,151,157-164], followed by touch screen (8/114, 7%) [9,14,63,65,97,127,146,147,165,166] and handheld game controllers (5/114, 4.4%) [35,57,87,153,155]. Of the 114 studies, 4 (3.5%) [46,143,144,167] used headset devices such as Oculus Rift VR System, Google Cardboard version 1, and RITECH II, whereas 2 (1.8%) used joysticks [69,168] and 3 (2.6%) [70,95,169] used VR gloves. The study by Kockro et al [72] used stereoscopic glasses as the input device (Figure S1 in Multimedia Appendix 3).
The delivery devices used include the use of screens in most of the studies (100/114, 87.7%) [8,9,14,35-47,49-51,53-56, 58,59,61-69,71,73-79,81,83-86,88-91,93-95,97-104, 106-117,119-129,131-138,140-144,146,147,151,156-159, 161-166,168,170,171], headset (13/114, 11.4%) [48,57,70,80, 82,87,92,95,96,105,118,145,153,155,167,172], and 3D projector with stereoscopic glasses (1/114, 0.9%) [72] (Figure S2 in Multimedia Appendix 3).
Extent of Immersion and Interactivity
Most of the studies included modalities that were of high interactivity (79/114, 69.3%) [35-37,42,43,45-51,55-57,59,66, 67,70,73-75,79,81-84,86-91,93,94,96, 98-100,102,103,105-113,115,116,118-129, 131-135,137,143,145-147,156,168,171,173,174], whereas 16.7% (19/114) of the studies [9,38-41,62-64,68, 69,76-78,97,104,140,141,151,153,159,161,162,165,169] included modalities that were of moderate interactivity and 14% (16/114) of the studies included modalities that were of low interactivity [8,14,44,54,58,61,65,71,72,80,85,87,92,101, 142,155,157,158,160,163,164, 167,172,175] (Figure S3 in Multimedia Appendix 3).
In terms of immersion, most of the studies included modalities that were semi-immersive (68/114, 59.6%) [36,37,42-44,47,49,51,53,55,56,59,61,66,67,69,73,75,81,83,84,86, 88,89,91,93,94,96,99-101,103,106,108,109,111-117,120,121,123-129, 131-139,142,146,156,166,168-170,176], followed by nonimmersive (26/114, 22.8%) [8,9,14,38,39,41,45,50,54, 58,62,63,65,68,71,72,76-78,85,97,101,140,141,147,157-159, 161,162,164,165,171] and fully immersive (20/114, 17.5%) [35,46,48,57,70,74,80,82,87,90,92,110,118,119, 145,151,153,155,167,172] (Figure S4 in Multimedia Appendix 3).
Of the 114 studies, 14 (12.3%) were both of high interactivity and fully immersive [35,46,48,57,70,74,82,90,105,110, 118,119,145,154]. Of these 14 studies, 9 (64%) involved the development of surgical psychomotor skills: 6 (67%) for laparoscopy [74,82,105,110,118,119] and 1 (11%) each for neurosurgery [35], orthopedics [57], and robotic surgery [90]. Of the 14 studies, 4 (29%) were relating to clinical management: 3 (75%) for pediatrics [48,145,154] and 1 (25%) for CPR [70]. The study by Wilson et al [46] was relating to ophthalmology anatomy. Keeping to definitions of immersion and interactivity, the VR modalities used in these studies allowed the user to visualize the environment, had motion-tracking capability, and allowed the user to manipulate the VR environment in real time.
Subjects Taught
From the studies, six broad subjects taught were identified: surgical psychomotor skills, anatomy, clinical management of various conditions, radiology, communication, and nonsurgical psychomotor skills.
The most common subject taught was surgical psychomotor skills, with 62.3% (71/114) of the studies including it as a subject taught [14,35-37,47,49,51,53,55-57,59,65-67,73-75, 79,81-84,86-91,93,94,96,99,100,103,105-126,128-138,147,148]. The second most common subject taught was anatomy, with 18.4% (21/114) of the studies including it as a subject taught [9,35,38,40,46,52,54,61,62,64,68,71,72,80,85,92,97,146,153,155,166], followed by 14% (16/114) of the studies including clinical management of various conditions as one of the subjects taught [39,41,43-45,48,50,58,63,69,70,140,141,145,154,167], 3.5% (4/114) of the studies including radiology as a subject taught [64,76-78], 2.6% (3/114) of the studies including nonsurgical psychomotor skills as a subject taught [42,102,104], and 2.6% (3/114) of the studies including communication as one of the subjects taught [44,50,101] (Figure S5 in Multimedia Appendix 3).
Of the 114 studies, 4 (3.5%) taught a combination of subjects. Of these 4 studies, 2 (50%) combined the teaching of clinical management and communication [44,50], 1 (25%) combined anatomy with radiology [64], and 1 (25%) combined anatomy with the development of surgical psychomotor skills [35].
With a focus on surgical psychomotor skills, most of these VR modalities involved the handling of laparoscopic surgeries (39/71, 55%). Of these 39 studies, 23 (59%) explored basic laparoscopic handling skills [49,59,67,74,79,81,83,84,86,96,99, 105,108,111,113, 117,118,123,128,130, 131,148] and 16 (41%) explored advanced laparoscopic surgery procedures [75,82,87,89,91,94,106,110,119,122,125,129, 132,134,136,137] such as cholecystectomy, appendectomy, salpingectomy, and Nissen fundoplication.
Of the 71 studies with a focus on surgical psychomotor skills, 7 (10%) involved arthroscopic VR modalities. Of these 7 studies, 3 (43%) provided training in basic arthroscopic skills [112,120,121], 2 (29%) pertained to knee arthroscopy [56,107], 1 (14%) pertained to hip arthroscopy [36], and 1 (14%) pertained to shoulder arthroscopy [66].
Among the remaining 35% (25/71) of the studies that examined surgical psychomotor skills, specific procedures were involved, such as ENT [114-116,124,138], endoscopy [73,93,100,135], ophthalmology [37,51,55,133], robotic surgery [90,103,126], neurosurgery [35,47], orthopedics [57,147], vascular surgery [53,109], microsurgery [14], urology [88], and emergency procedures (chest tube placement) [65].
Among the studies that explored anatomy, the most prevalent topic was neuroanatomy (6/21, 29%) [35,54,62,64,72,155], followed by regional anatomy (5/21, 24%) [9,52,92,97,146], ENT (3/21, 14%) [68,85,166], vascular anatomy (2/21, 10%) [38,61], and specific anatomical structures (5/21, 24%) [40,46,71,80,153].
Of the 16 studies that included clinical management, 4 (25%) included CPR as a management procedure [39,58,70,140], 3 (19%) were on pediatric respiratory management [48,145,154], and 2 (13%) were on general clinical presentation management [41,141], whereas the remaining 7 (44%) were on specific clinical and situational management procedures, including neurological management for benign paroxysmal positional vertigo [63], trauma [69], surgical [43], palliative [167], prenatal genetic screening [44], patient interaction [50], and clinical ethics management [45].
Of the 4 radiology studies, 3 (75%) pertained to general radiology [76-78] and 1 (25%) explored neuroanatomy together with neuroradiology [64].
Of the 114 studies, 3 (2.6%) involved VR training for nonsurgical psychomotor skills, including intravenous cannulation [42], ultrasound manipulation [102], and palpation [104]. Finally, of the 114 studies, 3 (2.6%) pertained to communication training, which included empathy [101], professionalism in clinical context [50], and prenatal genetic screening [44].
Teaching Strategies
Most of the studies (103/114, 90.4%) were conducted outside of the medical students’ curriculum, whereas 9.6% (10/114) of the studies assessed VR modalities that were incorporated into the curriculum. Among these 10 studies, the most common method of incorporating VR modalities into the curriculum was either by incorporating 3D anatomical models or virtual dissection tables into anatomy education (4/10, 40%) [38,72,97,146] or by incorporating virtual-world scenarios into clinical placements (4/10, 40%) [45,46,48,145], such as training students how to react to different situations that may be difficult to replicate in real life. The remaining 20% (2/20) of the studies incorporated the VR modality in the final year of study to better prepare students before they graduate. The study by De Ponti et al [141] prepared students for the clinical management of cardiovascular, cerebrovascular, trauma, pulmonary, infective, gynecological, gastrointestinal, renal, and metabolic endocrinology clinical cases, and the study by Paschold et al [106] prepared students for handling laparoscopic instruments in retraction of tissue and cystic duct and artery clipping.
More than half of the studies involved students engaging in self-directed learning with the VR modalities they were provided (71/114, 62%) [14,36,37,40,42-47,49,51,53,56,57,65-68,71-76, 78-82,84,85,87-89,91-93,99-105,107,109-112,114-116,118-121, 123,125,126,128,129,131,132,146,148,153,155,166,167]. Of the remaining 43 studies, 42 (98%) [9,35,38,39,41,48,50, 54,55,58,59,61-64,69,70,77,83,86,90,94,96, 97,106,108,113,117,122,124,130,133-138,140,141,145, 147,154] described students engaging in guided teaching sessions with VR use, whereas 1 (2%) did not provide clear description of student guidance [52].
Of the 42 studies with guided VR training sessions, 26 (62%) asked external experts to guide the students in the topic explored through VR [35,38,48,58,59,61-63,86,90,94,97,106,108,117, 122,124,130,133-136,141,145,147,154]. With regard to the external experts, their number and specialty varied greatly. Examples of external experts guiding students in various subjects included experienced surgeons’ demonstration and commentary on laparoscopic surgery [59], an anatomy instructor teaching an anatomy lesson [61], and otorhinolaryngology residents teaching clinical management of benign paroxysmal positional vertigo [63].
Between the self-directed and guided VR trainings, most of the studies incorporated an introductory session where time was allocated for students to become familiar with the VR system they were provided. Among the 71 self-directed studies, 58 (82%) used an introductory session [36,37,42-44,46,47,49,51,53,56,57,65,68,73-76, 78,82,84,85,87-89,91-93,99,100,102,103,105,107,109-112, 114-116,118,120,121,123,125,126,128,129,131,132,146, 153,155,166]. This took on many forms, such as watching demonstration videos [111,112,121], printed instructions [75,112], or live demonstration [65,100]. A few of the studies (9/71, 13%) did not introduce self-directed students to the use of the VR modality [45,66,67,71,72,81,101,104,167]. However, most of the VR modalities used in these studies had guides built into the VR programs.
Of the 71 studies with guided teaching, 36 (51%) incorporated an introduction for the VR modality [35,39,41,48,55,58,59,61-64,69,77,83,86,90,94,96,106,108, 113,117,122,124,130,133-138,140,141,145,147,154], whereas 6 (8%) [9,38,50,54,70,97] did not explicitly state that time was set aside for an introduction to the VR modality. Interestingly, of these 6 studies, 5 (83%) were conducted as part of the medical curriculum. Of these 5 studies, 1 (20%) [9] was conducted over a week. Although the authors did not explicitly set aside time for orientation to the VR modality, there may have been more time available in total for students to get familiar with the VR equipment.
Duration of Teaching
There was a wide variation in VR use periods in the studies. Hence, they were categorized into the following time periods: <1 day, 1 day to 1 month, 1-6 months, 6-12 months, and >1 year. For studies with duration >1 month, the 6-month threshold was chosen to distinguish between an academic semester and an academic year.
The most common lengths of teaching periods were <1 day (35/114, 30.7%) [38,43-45,50,53,54,64,71-73,75-77,79,80,83, 88,89,91,92,106,107,109,116,118,122,129,134,137,147,153, 155,166,167] and 1 day to 1 month (28/114, 24.6%) [9,37,42,48,49,57-59, 69,74,78,84-86,90, 99,100,104,108,110, 123-126,130,131,145,154].
Fewer studies opted for longer teaching periods. Of the 114 studies, 16 (14%) used teaching periods lasting 1-6 months [36,39,56,63,65,66,81,87,97,105,111,135,136,146,148], 8 (7%) used periods lasting 6-12 months [35,40,67,94,114,120,121,141], and 4 (3.5%) were conducted over periods lasting >1 year [41,70,115,140].
Of the 114 studies, 4 (3.5%) investigated attainment of proficiency over time, and thus a predetermined training duration was not applicable [82,113,128,133], whereas 1 (0.9%) was a meta-analysis, and thus training duration was not applicable either [52]. The teaching period was not specified in 15.8% (18/114) of the studies [14,46,47,51,55,61,62,68,93, 96,101-103,112,117, 119,132,138].
Delivery of VR Modalities to Individuals or Groups
The studies had variations in the number of students who were taught using 1 VR device. Hence, the studies were categorized into those that used VR modalities that facilitated teaching an individual and those that facilitated group teaching (>1 person). Some VR modalities were more flexible: they allowed for teaching either an individual or a group.
Most of the study designs involved individual students taught using VR modalities (97/114, 85.1%) [14,36,37,42-49,51,53-59,63,65-67,69-71, 73-76,78-82,84-94,96,99-126,128-138, 141,145-148,153-155,166,167]. A few studies used VR teaching modalities for both individual and group teaching (7/114, 6.1%) [35,40,41,61,62,64,68], whereas some used it solely for group teaching (9/114, 7.9%) [9,38,39,50,72,77,83,97,140]. VR delivery was not applicable for 0.9% (1/114) of the studies [52].
There were distinct group sizes that were characteristic of the modality of VR used. Some studies used small teaching groups of approximately 2-4 students [140]. These VR modalities used virtual world scenario-based teaching methods and involved working in small teams for learning. Other studies used classroom-size teaching methods with 20-30 students [38,72]. These studies mainly focused on anatomy teaching with the use of stereoscopic 3D projectors. Finally, some studies incorporated VR modalities that allowed for trainings to be conducted to hundreds of students at once [77]. These VR modalities were characteristically virtual world massively multiplayer online games such as Second Life.
Discussion
Summary of Findings
In this scoping review, we mapped out the existing VR modalities used in undergraduate medical education, including the characteristics of the VR modalities, target population, tools used in development, educational elements, and the outcomes measured of each VR modality. We found 114 studies that were relevant to our objective, including 47 (41.2%) RCTs, 49 (42.9%) other experimental study designs, 14 (12.3%) cross-over studies, 3 (2.6%) case studies and cases series, and 1 (0.9%) meta-analysis. Most of the papers were published from Europe or the United States. Approximately half of the papers reported the use of surgical VR simulators, with the next most common being 3D anatomical models and virtual worlds. Other VR modalities such as virtual dissection tables and mobile VR were less common. The included studies usually used haptic tools or a mouse as input devices and a screen as a delivery device. Most of the studies were semi-immersive with a high degree of interactivity. The most common subject taught using VR simulators was surgical skills, and the most common mode of training was self-directed. There was a large variation in the duration of teaching. Most studies reported only a single type of outcome measurement, with the most common being skills outcomes. The timing of assessment was most often immediately after the intervention. Most VR modalities were also designed for individual delivery rather than group delivery.
Comparison With Existing Literature and Future Recommendations
Although surgical VR simulators, 3D anatomical models, and virtual worlds are relatively well represented in the literature, there is limited evidence on the use of virtual dissection tables and mobile VR. Indeed, there are a number of systematic reviews evaluating the use of surgical VR simulators in health professions education at both postgraduate and undergraduate level, most of which favor VR, especially for nonsimulation training [177-179]. The relative lack of studies on virtual dissection tables and mobile VR could be due to the fact that these VR modalities are more novel and have been reported in the literature only from 2015 onward, as revealed by our search strategy. Furthermore, some popular VR anatomy applications are not assessed in the included studies, such as Complete Anatomy (3D4Medical) [150] and Anatomy.tv (Primal Pictures) [180]. It seems that although a wide variety of VR tools were mentioned in the results, there are other VR tools that may be commonly used but not mentioned in the literature. Future studies should examine the effectiveness of the use of novel VR modalities in different settings, for example, remote, home-based learning, such as in the case of mobile VR modalities.
Most of the studies included in our review did not report, or refer to, educational or behavior frameworks or theories used in the development of VR applications. This has also been observed in studies on other digital modalities used in health professions education [3]. However, explicit use of frameworks or theories for the design of complex interventions such as the use of VR in education has an important role for improving the quality, transparency, and reproducibility of research. Future research should aim to incorporate and report on the adoption of such frameworks in the design of VR applications where possible.
We also observed several studies exploring the development of particular 3D anatomical models and virtual worlds that had a considerable overlap in terms of the process of development. There is a need for stronger collaboration and easier sharing among educators and researchers in this novel field. This could be achieved through a common platform or database of VR medical education tools and insights similar to Radiopaedia for radiology and GitHub for software engineering.
There is a clear lack of studies from low- and middle-income countries. Adoption of VR tools shown to be effective in high-income countries might not be possible in other settings because of context-specific limitations such as lack of financial resources, knowledge, or technology [181,182]. Given the potential that VR has in improving medical education, there is a need for development and evaluation of VR tools that would be specific to low- and middle-income countries.
We also observed a distinct lack of studies focusing on the use of VR for developing soft skills such as communication skills or empathy. The manner in which health care professionals communicate with patients is argued to be as important as clinical knowledge but often goes underemphasized [50,101]. VPs in particular can be programmed to respond in different manners depending on the response of the user and offer an exciting opportunity to develop students’ communication skills from the comfort of their own homes. There is also scope for more research exploring the use of VR for nonsurgical skills development.
Immersive VR modalities not only offer a realistic experience to the user, but they also have the additional benefit of spatial understanding [155]. The higher the level of immersion, the greater the spatial understanding, which can result in greater effectiveness of scientific visualization. It also helps to reduce the information clutter wrought by the overlapping icons and controls of 2D environments [21]. However, highly immersive systems can be costly and resource intensive [28]. Most of the studies in this review were semi-immersive in nature, possibly to optimize realism while avoiding high costs. Future studies should explore the use of VR modalities with high immersion. Correspondingly, there is scope for more research on VR delivered through headsets and VR using input devices other than haptic surgical tools or a mouse.
Only a few studies reported on the integration of VR training presented in the study into medical school curricula [35,70,141]. Although VR is being increasingly implemented at medical schools worldwide, the literature reporting its implementation and adoption is scarce. This is coupled with a lack of guidance or information on how best to adopt different VR modalities in the curriculum. There is a need for clear guidance and recommendations with the aim of enabling optimal adoption and harnessing of VR within medical curricula.
Strengths and Limitations
We performed a comprehensive search of 4 major bibliographic databases in this review. We covered the search period starting from 2010 to include all available studies on VR-based training for medical students’ education. Our screening and data extraction were also conducted in parallel and independently to ensure reliability and reduce bias in our findings. The topic that we explored was also novel, particularly in the context of undergraduate medical education.
This scoping review was limited to studies published in English. Because of the large number of studies on VR, we only focused our research on the use of VR in medical students’ education and thus the use of VR in other health care professionals’ education and training was not captured in this review. Diverse terminology was used to describe VR; therefore, we may not have captured some studies because of the unfamiliar terminology used. In the categorization of the diverse terminology used in the studies, details specific to singular studies may have been lost. Although this review is as comprehensive as possible, there may still be smaller but important studies that were published only as abstracts that were left out of this review. In accordance with scoping review methodology, there was no quality assessment of the included articles; thus, the included studies may be biased or incomplete in terms of some of the information reported.
Conclusions
The use of VR in medical education is a rapidly expanding and exciting field of study. Current research is mostly centered on surgical VR simulators, virtual worlds, and 3D anatomical models by comparing them with traditional modes of learning. Novel VR modalities such as mobile VR and virtual dissection tables, which are potentially more portable and allow for group learning, respectively, are less well represented in the literature. As an increasing number of medical schools turn toward incorporating VR into their curriculum, there is a need to evaluate these novel VR modalities as well as describe the methods used to incorporate VR into the curriculum. The use of VR to develop communication skills or to allow students to work in a team is also lacking. Most of the VR modalities described are only designed for a single user, which is unlike situations arising in a health care team. The use of modalities such as virtual worlds to create scenarios that require teamwork and communication should be more widely explored.
Acknowledgments
The authors would like to thank Ms Rebecca Lavanie David for her help in the development of the search strategy for MEDLINE. The authors would also like to thank Dr Bhone Myint Kyaw for his assistance with developing the protocol and the participants of the stakeholder consultation seminar for their inputs.
Abbreviations
- CPR
cardiopulmonary resuscitation
- ENT
ear, nose, and throat
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews
- RCT
randomized controlled trial
- VP
virtual patient
- VR
virtual reality
Search strategies.
Data extraction form.
Supplementary figures.
Footnotes
Authors' Contributions: LTC conceived the idea for the review. JHW, SV, and JKW wrote the review. JHW, SV, JKW, and LKK helped in the data extraction and analysis process. LTC provided methodological guidance and critically revised the manuscript. SRM reviewed the work critically and provided feedback. All authors gave their approval for the final version of the work to be published and agreed to be accountable for the integrity of the work published.
Conflicts of Interest: None declared.
References
- 1.Van Way CW. Thoughts on medical education. Mo Med. 2017;114(6):417–8. http://europepmc.org/abstract/MED/30228651 . [PMC free article] [PubMed] [Google Scholar]
- 2.Haroon Z, Azad AA, Sharif M, Aslam A, Arshad K, Rafiq S. COVID-19 era: challenges and solutions in dental education. J Coll Physicians Surg Pak. 2020 Oct;30(10):129–31. doi: 10.29271/jcpsp.2020.supp2.129.040579197 [DOI] [PubMed] [Google Scholar]
- 3.Tudor Car L, Soong A, Kyaw BM, Chua KL, Low-Beer N, Majeed A. Health professions digital education on clinical practice guidelines: a systematic review by Digital Health Education collaboration. BMC Med. 2019 Jul 18;17(1):139. doi: 10.1186/s12916-019-1370-1. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1370-1 .10.1186/s12916-019-1370-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Car J, Carlstedt-Duke J, Tudor Car L, Posadzki P, Whiting P, Zary N, Atun R, Majeed A, Campbell J, Digital Health Education Collaboration Digital education in health professions: the need for overarching evidence synthesis. J Med Internet Res. 2019 Feb 14;21(2):e12913. doi: 10.2196/12913. https://www.jmir.org/2019/2/e12913/ v21i2e12913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim J-H, Park S-T, Lee H, Yuk K-C, Lee H. Virtual reality simulations in physics education. Interact Multimedia Electon J Comput Enhanced Learn. 2001 [Google Scholar]
- 6.Van Herzeele I, Aggarwal R, Neequaye S, Darzi A, Vermassen F, Cheshire NJ. Cognitive training improves clinically relevant outcomes during simulated endovascular procedures. J Vasc Surg. 2008 Nov;48(5):1223–30, 1230.e1. doi: 10.1016/j.jvs.2008.06.034. https://linkinghub.elsevier.com/retrieve/pii/S0741-5214(08)01026-4 .S0741-5214(08)01026-4 [DOI] [PubMed] [Google Scholar]
- 7.Blackburn SC, Griffin SJ. Role of simulation in training the next generation of endoscopists. World J Gastrointest Endosc. 2014 Jun 16;6(6):234–9. doi: 10.4253/wjge.v6.i6.234. https://www.wjgnet.com/1948-5190/full/v6/i6/234.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ammanuel S, Brown I, Uribe J, Rehani B. Creating 3D models from radiologic images for virtual reality medical education modules. J Med Syst. 2019 May 03;43(6):166. doi: 10.1007/s10916-019-1308-3.10.1007/s10916-019-1308-3 [DOI] [PubMed] [Google Scholar]
- 9.Boscolo-Berto R, Tortorella C, Porzionato A, Stecco C, Picardi EE, Macchi V, De Caro R. The additional role of virtual to traditional dissection in teaching anatomy: a randomised controlled trial. Surg Radiol Anat. 2021 Apr;43(4):469–79. doi: 10.1007/s00276-020-02551-2. http://europepmc.org/abstract/MED/32940718 .10.1007/s00276-020-02551-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen D, Sevdalis N, Patel V, Taylor M, Lee H, Vokes M, Heys M, Taylor D, Batrick N, Darzi A. Tactical and operational response to major incidents: feasibility and reliability of skills assessment using novel virtual environments. Resuscitation. 2013 Jul;84(7):992–8. doi: 10.1016/j.resuscitation.2012.12.011.S0300-9572(12)00948-3 [DOI] [PubMed] [Google Scholar]
- 11.Heinrichs WL, Youngblood P, Harter P, Kusumoto L, Dev P. Training healthcare personnel for mass-casualty incidents in a virtual emergency department: VED II. Prehosp Disaster Med. 2010;25(5):424–32. doi: 10.1017/s1049023x00008505. [DOI] [PubMed] [Google Scholar]
- 12.Hudson K, Taylor LA, Kozachik SL, Shaefer SJ, Wilson ML. Second Life simulation as a strategy to enhance decision-making in diabetes care: a case study. J Clin Nurs. 2015 Mar;24(5-6):797–804. doi: 10.1111/jocn.12709. [DOI] [PubMed] [Google Scholar]
- 13.Quail N, Boyle J. Virtual patients in health professions education. Adv Exp Med Biol. 2019;1171:25–35. doi: 10.1007/978-3-030-24281-7_3. [DOI] [PubMed] [Google Scholar]
- 14.Amer KM, Mur T, Amer K, Ilyas AM. A mobile-based surgical simulation application: a comparative analysis of efficacy using a carpal tunnel release module. J Hand Surg Am. 2017 May;42(5):389.e1–.e9. doi: 10.1016/j.jhsa.2017.02.008.S0363-5023(17)30291-5 [DOI] [PubMed] [Google Scholar]
- 15.Khan R, Plahouras J, Johnston BC, Scaffidi MA, Grover SC, Walsh CM. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev. 2018 Aug 17;8:CD008237. doi: 10.1002/14651858.CD008237.pub3. http://europepmc.org/abstract/MED/30117156 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagendran M, Gurusamy KS, Aggarwal R, Loizidou M, Davidson BR. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2013 Aug 27;(8):CD006575. doi: 10.1002/14651858.CD006575.pub3. http://europepmc.org/abstract/MED/23980026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ. 2017 Nov;10(6):549–59. doi: 10.1002/ase.1696. [DOI] [PubMed] [Google Scholar]
- 18.Wong MA, Chue S, Jong M, Benny HW, Zary N. Clinical instructors' perceptions of virtual reality in health professionals' cardiopulmonary resuscitation education. SAGE Open Med. 2018;6:2050312118799602. doi: 10.1177/2050312118799602. https://journals.sagepub.com/doi/10.1177/2050312118799602?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2050312118799602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc. 2018 Oct;106(4):498–500. doi: 10.5195/jmla.2018.518. http://europepmc.org/abstract/MED/30271295 .jmla-106-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bracq M, Michinov E, Jannin P. Virtual reality simulation in nontechnical skills training for healthcare professionals. Sim Healthcare. 2019 Jan 2;14(3):188–94. doi: 10.1097/sih.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 21.Fealy S, Jones D, Hutton A, Graham K, McNeill L, Sweet L, Hazelton M. The integration of immersive virtual reality in tertiary nursing and midwifery education: a scoping review. Nurse Educ Today. 2019 Aug;79:14–9. doi: 10.1016/j.nedt.2019.05.002.S0260-6917(19)30071-1 [DOI] [PubMed] [Google Scholar]
- 22.Huang T, Yang C, Hsieh Y, Wang J, Hung C. Augmented reality (AR) and virtual reality (VR) applied in dentistry. Kaohsiung J Med Sci. 2018 Apr;34(4):243–8. doi: 10.1016/j.kjms.2018.01.009. https://linkinghub.elsevier.com/retrieve/pii/S1607-551X(17)30815-X .S1607-551X(17)30815-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gurusamy KS, Aggarwal R, Palanivelu L, Davidson BR. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD006575. doi: 10.1002/14651858.CD006575.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Bernardo A. Virtual reality and simulation in neurosurgical training. World Neurosurg. 2017 Oct;106:1015–29. doi: 10.1016/j.wneu.2017.06.140.S1878-8750(17)31035-5 [DOI] [PubMed] [Google Scholar]
- 25.JBI Manual for Evidence Synthesis. Adelaide, Australia: Joanna Briggs Institute; 2020. Chapter 11: Scoping Reviews (2020 version) [Google Scholar]
- 26.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp ?, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Sep 04;169(7):467. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 27.Haowen J, Vimalesvaran S, Myint Kyaw B, Tudor Car L. Virtual reality in medical students' education: a scoping review protocol. BMJ Open. 2021 May 26;11(5):e046986. doi: 10.1136/bmjopen-2020-046986. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=34039577 .bmjopen-2020-046986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kyaw BM, Saxena N, Posadzki P, Vseteckova J, Nikolaou CK, George PP, Divakar U, Masiello I, Kononowicz AA, Zary N, Tudor Car L. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res. 2019 Jan 22;21(1):e12959. doi: 10.2196/12959. https://www.jmir.org/2019/1/e12959/ v21i1e12959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tepper OM, Rudy HL, Lefkowitz A, Weimer KA, Marks SM, Stern CS, Garfein ES. Mixed reality with Hololens: where virtual reality meets augmented reality in the operating room. Plast Reconstr Surg. 2017 Nov;140(5):1066–70. doi: 10.1097/PRS.0000000000003802.00006534-201711000-00034 [DOI] [PubMed] [Google Scholar]
- 30.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015 Sep;13(3):141–6. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 31.Ott M, Freina L. A literature review on immersive virtual reality in education: state of the art and perspectives. Proceedings of the eLearning and Software for Education (eLSE); eLearning and Software for Education (eLSE); Apr 23 - 24, 2015; Bucharest (Romania). 2015. [Google Scholar]
- 32.Ippoliti E, Casale A, Calvano M, Guadagnoli F. Analysis, Conservation, and Restoration of Tangible and Intangible Cultural Heritage. Rome, Italy: IGI Global; 2019. Giving form to absence: experiences in representation, communication, and narration for the places and community of Amatrice. [Google Scholar]
- 33.Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, Slater M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med. 2017 Oct;47(14):2393–400. doi: 10.1017/S003329171700040X. http://europepmc.org/abstract/MED/28325167 .S003329171700040X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ayoub A, Pulijala Y. BMC Oral Health. 2019 Nov 08;19(1):238. doi: 10.1186/s12903-019-0937-8. https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-019-0937-8 .10.1186/s12903-019-0937-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Atli K, Selman W, Ray A. A comprehensive multicomponent neurosurgical course with use of virtual reality: modernizing the medical classroom. J Surg Educ. 2021;78(4):1350–6. doi: 10.1016/j.jsurg.2020.11.003.S1931-7204(20)30428-1 [DOI] [PubMed] [Google Scholar]
- 36.Bartlett J, To K. Does virtual reality simulator use influence medical students' attitudes to a career in orthopedic surgery?. Proceedings of the Osteoporosis International; Proceedings of the Osteoporosis International; Jul, 2019; Paris, France. 2019. [DOI] [Google Scholar]
- 37.Bergqvist J, Person A, Vestergaard A, Grauslund J. Establishment of a validated training programme on the Eyesi cataract simulator. A prospective randomized study. Acta Ophthalmol. 2014 Nov;92(7):629–34. doi: 10.1111/aos.12383. doi: 10.1111/aos.12383. [DOI] [PubMed] [Google Scholar]
- 38.Brown P, Hamilton NM, Denison AR. A novel 3D stereoscopic anatomy tutorial. Clin Teach. 2012 Feb;9(1):50–3. doi: 10.1111/j.1743-498X.2011.00488.x. [DOI] [PubMed] [Google Scholar]
- 39.Creutzfeldt J, Hedman L, Medin C, Heinrichs WL, Felländer-Tsai Li. Exploring virtual worlds for scenario-based repeated team training of cardiopulmonary resuscitation in medical students. J Med Internet Res. 2010 Sep 03;12(3):e38. doi: 10.2196/jmir.1426. https://www.jmir.org/2010/3/e38/ v12i3e38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Danforth D. Development of an interactive virtual 3-D model of the human testis using the second life platform. Int J Virtual Personal Learn Environ. 2010;1(2):45–58. doi: 10.4018/jvple.2010040104. [DOI] [Google Scholar]
- 41.Hayward J, Cheung A, Velji A, Altarejos J, Gill P, Scarfe A, Lewis M. Script-theory virtual case: a novel tool for education and research. Medical Teacher. 2016 Apr 21;38(11):1130–8. doi: 10.3109/0142159x.2016.1170776. [DOI] [PubMed] [Google Scholar]
- 42.Isaranuwatchai W, Brydges R, Carnahan H, Backstein D, Dubrowski A. Comparing the cost-effectiveness of simulation modalities: a case study of peripheral intravenous catheterization training. Adv Health Sci Educ Theory Pract. 2014 May;19(2):219–32. doi: 10.1007/s10459-013-9464-6. [DOI] [PubMed] [Google Scholar]
- 43.Kleinert R, Heiermann N, Wahba R, Chang D, Hölscher AH, Stippel DL. Design, realization, and first validation of an immersive web-based virtual patient simulator for training clinical decisions in surgery. J Surg Educ. 2015;72(6):1131–8. doi: 10.1016/j.jsurg.2015.05.009.S1931-7204(15)00140-3 [DOI] [PubMed] [Google Scholar]
- 44.Makransky G, Mayer R, Nøremølle A, Cordoba AL, Wandall J, Bonde M. Investigating the feasibility of using assessment and explanatory feedback in desktop virtual reality simulations. Education Tech Research Dev. 2019 Jul 10;68(1):293–317. doi: 10.1007/s11423-019-09690-3. [DOI] [Google Scholar]
- 45.Torda A. CLASSIE teaching - using virtual reality to incorporate medical ethics into clinical decision making. BMC Med Educ. 2020 Sep 23;20(1):326. doi: 10.1186/s12909-020-02217-y. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02217-y .10.1186/s12909-020-02217-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wilson AS, O'Connor J, Taylor L, Carruthers D. A 3D virtual reality ophthalmoscopy trainer. Clin Teach. 2017 Dec;14(6):427–31. doi: 10.1111/tct.12646. [DOI] [PubMed] [Google Scholar]
- 47.Winkler-Schwartz A, Marwa I, Bajunaid K, Mullah M, Alotaibi FE, Bugdadi A, Sawaya R, Sabbagh AJ, Del Maestro R. A comparison of visual rating scales and simulated virtual reality metrics in neurosurgical training: a generalizability theory study. World Neurosurg. 2019 Jul;127:e230–5. doi: 10.1016/j.wneu.2019.03.059.S1878-8750(19)30699-0 [DOI] [PubMed] [Google Scholar]
- 48.Zackoff MW, Real FJ, Sahay RD, Fei L, Guiot A, Lehmann C, Tegtmeyer K, Klein M. Impact of an immersive virtual reality curriculum on medical students’ clinical assessment of infants with respiratory distress. Pediatric Critical Care Medicine. 2020;21(5):477–85. doi: 10.1097/pcc.0000000000002249. [DOI] [PubMed] [Google Scholar]
- 49.Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM, Epstein SK, De S, Schwaitzberg SD, Jones DB, Cao CG. Characterizing the learning curve of the VBLaST-PT(©) (Virtual Basic Laparoscopic Skill Trainer) Surg Endosc. 2013 Oct;27(10):3603–15. doi: 10.1007/s00464-013-2932-5. http://europepmc.org/abstract/MED/23572217 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Loke S, Blyth P, Swan J. In search of a method to assess dispositional behaviours: the case of Otago Virtual Hospital. Aust J Educ Technol. 2012 Apr 25;28(3):441–58. doi: 10.14742/ajet.844. [DOI] [Google Scholar]
- 51.Selvander M, Åsman P. Stereoacuity and intraocular surgical skill: effect of stereoacuity level on virtual reality intraocular surgical performance. J Cataract Refract Surg. 2011 Dec;37(12):2188–93. doi: 10.1016/j.jcrs.2011.05.048.S0886-3350(11)01479-9 [DOI] [PubMed] [Google Scholar]
- 52.Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ. 2015;8(6):525–38. doi: 10.1002/ase.1510. [DOI] [PubMed] [Google Scholar]
- 53.Aeckersberg G, Gkremoutis A, Schmitz-Rixen T, Kaiser E. The relevance of low-fidelity virtual reality simulators compared with other learning methods in basic endovascular skills training. J Vasc Surg. 2019 Jan;69(1):227–35. doi: 10.1016/j.jvs.2018.10.047. https://linkinghub.elsevier.com/retrieve/pii/S0741-5214(18)32453-4 .S0741-5214(18)32453-4 [DOI] [PubMed] [Google Scholar]
- 54.Allen LK, Eagleson R, de Ribaupierre S. Evaluation of an online three-dimensional interactive resource for undergraduate neuroanatomy education. Anat Sci Educ. 2016 Oct;9(5):431–9. doi: 10.1002/ase.1604. [DOI] [PubMed] [Google Scholar]
- 55.Alwadani F, Morsi M. PixEye virtual reality training has the potential of enhancing proficiency of laser trabeculoplasty performed by medical students: a pilot study. Middle East Afr J Ophthalmol. 2012 Jan;19(1):120–2. doi: 10.4103/0974-9233.92127. http://www.meajo.org/article.asp?issn=0974-9233;year=2012;volume=19;issue=1;spage=120;epage=122;aulast=Alwadani .MEAJO-19-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Banaszek D, You D, Chang J, Pickell M, Hesse D, Hopman WM, Borschneck D, Bardana D. Virtual reality compared with bench-top simulation in the acquisition of arthroscopic skill. J Bone Joint Surgery. 2017;99(7):e34. doi: 10.2106/jbjs.16.00324. [DOI] [PubMed] [Google Scholar]
- 57.Blumstein G, Zukotynski B, Cevallos N, Ishmael C, Zoller S, Burke Z, Clarkson S, Park H, Bernthal N, SooHoo NF. Randomized trial of a virtual reality tool to teach surgical technique for tibial shaft fracture intramedullary nailing. J Surg Educ. 2020;77(4):969–77. doi: 10.1016/j.jsurg.2020.01.002. http://europepmc.org/abstract/MED/32035854 .S1931-7204(20)30002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bonnetain E, Boucheix J, Hamet M, Freysz M. Benefits of computer screen-based simulation in learning cardiac arrest procedures. Med Educ. 2010 Jul;44(7):716–22. doi: 10.1111/j.1365-2923.2010.03708.x.MED3708 [DOI] [PubMed] [Google Scholar]
- 59.Brinkmann C, Fritz M, Pankratius U, Bahde R, Neumann P, Schlueter S, Senninger N, Rijcken E. Box- or virtual-reality trainer: which tool results in better transfer of laparoscopic basic skills?-A prospective randomized trial. J Surg Educ. 2017;74(4):724–35. doi: 10.1016/j.jsurg.2016.12.009.S1931-7204(16)30386-5 [DOI] [PubMed] [Google Scholar]
- 60.Chen Y, Huang Q, Sheng C, Zhang W, Shao S, Wang D, Cheng Y, Wang Y, Guo Q, Zhang D, Li Y, Lowres N, Freedman B, Wang J. Detection rate and treatment gap for atrial fibrillation identified through screening in community health centers in China (AF-CATCH): a prospective multicenter study. PLoS Med. 2020 Jul;17(7):e1003146. doi: 10.1371/journal.pmed.1003146. https://dx.plos.org/10.1371/journal.pmed.1003146 .PMEDICINE-D-19-04467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cui D, Wilson TD, Rockhold RW, Lehman MN, Lynch JC. Evaluation of the effectiveness of 3D vascular stereoscopic models in anatomy instruction for first year medical students. Anat Sci Educ. 2017 Jan;10(1):34–45. doi: 10.1002/ase.1626. [DOI] [PubMed] [Google Scholar]
- 62.Deng X, Zhou G, Xiao B, Zhao Z, He Y, Chen C. Effectiveness evaluation of digital virtual simulation application in teaching of gross anatomy. Ann Anat. 2018 Jul;218:276–82. doi: 10.1016/j.aanat.2018.02.014.S0940-9602(18)30047-5 [DOI] [PubMed] [Google Scholar]
- 63.Dlugaiczyk J, Thiemer M, Neubert C, Schorn B, Schick B. The aVOR app increases medical students' competence in treating benign paroxysmal positional vertigo (BPPV) Otol Neurotol. 2018 Jun;39(5):e401–6. doi: 10.1097/MAO.0000000000001778. [DOI] [PubMed] [Google Scholar]
- 64.Drapkin ZA, Lindgren KA, Lopez MJ, Stabio ME. Development and assessment of a new 3D neuroanatomy teaching tool for MRI training. Anat Sci Educ. 2015;8(6):502–9. doi: 10.1002/ase.1509. [DOI] [PubMed] [Google Scholar]
- 65.Haubruck P, Nickel F, Ober J, Walker T, Bergdolt C, Friedrich M, Müller-Stich BP, Forchheim F, Fischer C, Schmidmaier G, Tanner MC. Evaluation of app-based serious gaming as a training method in teaching chest tube insertion to medical students: randomized controlled trial. J Med Internet Res. 2018 May 21;20(5):e195. doi: 10.2196/jmir.9956. https://www.jmir.org/2018/5/e195/ v20i5e195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Henn RF, Shah N, Warner JJ, Gomoll A. Shoulder arthroscopy simulator training improves shoulder arthroscopy performance in a cadaver model (SS-60) Arthroscopy J Arthroscopic Related Surgery. 2013 Jun;29(6):e29. doi: 10.1016/j.arthro.2013.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hiemstra E, Terveer EM, Chmarra MK, Dankelman J, Jansen FW. Virtual reality in laparoscopic skills training: is haptic feedback replaceable? Minim Invasive Ther Allied Technol. 2011 May;20(3):179–84. doi: 10.3109/13645706.2010.532502. [DOI] [PubMed] [Google Scholar]
- 68.Hu A, Shewokis PA, Ting K, Fung K. Motivation in computer-assisted instruction. Laryngoscope. 2016 Aug;126 Suppl 6:S5–13. doi: 10.1002/lary.26040. [DOI] [PubMed] [Google Scholar]
- 69.Luigi Ingrassia P, Ragazzoni L, Carenzo L, Colombo D, Ripoll Gallardo A, Della Corte F. Virtual reality and live simulation: a comparison between two simulation tools for assessing mass casualty triage skills. Eur J Emerg Med. 2015 Apr;22(2):121–7. doi: 10.1097/MEJ.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 70.Jaskiewicz F, Kowalewski D, Starosta K, Cierniak M, Timler D. Chest compressions quality during sudden cardiac arrest scenario performed in virtual reality: a crossover study in a training environment. Medicine (Baltimore) 2020 Nov 25;99(48):e23374. doi: 10.1097/MD.0000000000023374. doi: 10.1097/MD.0000000000023374.00005792-202011250-00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Keedy AW, Durack JC, Sandhu P, Chen EM, O'Sullivan PS, Breiman RS. Comparison of traditional methods with 3D computer models in the instruction of hepatobiliary anatomy. Anat Sci Educ. 2011;4(2):84–91. doi: 10.1002/ase.212. [DOI] [PubMed] [Google Scholar]
- 72.Kockro RA, Amaxopoulou C, Killeen T, Wagner W, Reisch R, Schwandt E, Gutenberg A, Giese A, Stofft E, Stadie AT. Stereoscopic neuroanatomy lectures using a three-dimensional virtual reality environment. Ann Anat. 2015 Sep;201:91–8. doi: 10.1016/j.aanat.2015.05.006.S0940-9602(15)00084-9 [DOI] [PubMed] [Google Scholar]
- 73.Krogh CL, Konge L, Bjurström J, Ringsted C. Training on a new, portable, simple simulator transfers to performance of complex bronchoscopy procedures. Clin Respir J. 2013 Jul;7(3):237–44. doi: 10.1111/j.1752-699X.2012.00311.x. [DOI] [PubMed] [Google Scholar]
- 74.Laski D, Stefaniak TJ, Makarewicz W, Proczko M, Gruca Z, Sledziński Z. Structuralized box-trainer laparoscopic training significantly improves performance in complex virtual reality laparoscopic tasks. Wideochir Inne Tech Maloinwazyjne. 2012 Mar;7(1):27–32. doi: 10.5114/wiitm.2011.25666. http://europepmc.org/abstract/MED/23255997 .17683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lesch H, Johnson E, Peters J, Cendán JC. VR simulation leads to enhanced procedural confidence for surgical trainees. J Surg Educ. 2020;77(1):213–8. doi: 10.1016/j.jsurg.2019.08.008. http://europepmc.org/abstract/MED/31466895 .S1931-7204(19)30407-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lorenzo-Alvarez R, Pavia-Molina J, Sendra-Portero F. Exploring the potential of undergraduate radiology education in the virtual world second life with first-cycle and second-cycle medical students. Acad Radiol. 2018 Aug;25(8):1087–96. doi: 10.1016/j.acra.2018.02.026.S1076-6332(18)30113-2 [DOI] [PubMed] [Google Scholar]
- 77.Lorenzo-Alvarez R, Rudolphi-Solero T, Ruiz-Gomez MJ, Sendra-Portero F. Medical student education for abdominal radiographs in a 3D virtual classroom versus traditional classroom: a randomized controlled trial. AJR Am J Roentgenol. 2019 Sep;213(3):644–50. doi: 10.2214/AJR.19.21131. [DOI] [PubMed] [Google Scholar]
- 78.Lorenzo-Alvarez R, Rudolphi-Solero T, Ruiz-Gomez MJ, Sendra-Portero F. Game-based learning in virtual worlds: a multiuser online game for medical undergraduate radiology education within second life. Anat Sci Educ. 2020 Sep;13(5):602–17. doi: 10.1002/ase.1927. [DOI] [PubMed] [Google Scholar]
- 79.Mann T, Gillinder L, Szold A. The use of virtual reality simulation to determine potential for endoscopic surgery skill acquisition. Minim Invasive Ther Allied Technol. 2014 Aug;23(4):190–7. doi: 10.3109/13645706.2014.894529. [DOI] [PubMed] [Google Scholar]
- 80.Maresky HS, Oikonomou A, Ali I, Ditkofsky N, Pakkal M, Ballyk B. Virtual reality and cardiac anatomy: exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin Anat. 2019 Mar;32(2):238–43. doi: 10.1002/ca.23292. [DOI] [PubMed] [Google Scholar]
- 81.Matzke J, Ziegler C, Martin K, Crawford S, Sutton E. Usefulness of virtual reality in assessment of medical student laparoscopic skill. J Surg Res. 2017 May 01;211:191–5. doi: 10.1016/j.jss.2016.11.054.S0022-4804(16)30532-7 [DOI] [PubMed] [Google Scholar]
- 82.Moglia A, Sinceri S, Ferrari V, Ferrari M, Mosca F, Morelli L. Proficiency-based training of medical students using virtual simulators for laparoscopy and robot-assisted surgery: results of a pilot study. Updates Surg. 2018 Sep;70(3):401–5. doi: 10.1007/s13304-018-0559-8.10.1007/s13304-018-0559-8 [DOI] [PubMed] [Google Scholar]
- 83.Mulla M, Sharma D, Moghul M, Kailani O, Dockery J, Ayis S, Grange P. Learning basic laparoscopic skills: a randomized controlled study comparing box trainer, virtual reality simulator, and mental training. J Surg Educ. 2012;69(2):190–5. doi: 10.1016/j.jsurg.2011.07.011.S1931-7204(11)00232-7 [DOI] [PubMed] [Google Scholar]
- 84.Nemani A, Ahn W, Cooper C, Schwaitzberg S, De S. Convergent validation and transfer of learning studies of a virtual reality-based pattern cutting simulator. Surg Endosc. 2018 Mar;32(3):1265–72. doi: 10.1007/s00464-017-5802-8. http://europepmc.org/abstract/MED/28812196 .10.1007/s00464-017-5802-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ng CL, Liu X, Chee SC, Ngo RY. An innovative 3-dimensional model of the epitympanum for teaching of middle ear anatomy. Otolaryngol Head Neck Surg. 2015 Nov;153(5):832–7. doi: 10.1177/0194599815584600.0194599815584600 [DOI] [PubMed] [Google Scholar]
- 86.Sabench Pereferrer F, Hernández González M, Muñoz García A, Cabrera Vilanova A, Del Castillo Déjardin D. [Evaluation of surgical skills in medical students using a virtual simulator] Cir Esp. 2013 Mar;91(3):177–83. doi: 10.1016/j.ciresp.2012.05.019.S0009-739X(12)00231-X [DOI] [PubMed] [Google Scholar]
- 87.Sattar MU, Palaniappan S, Lokman A, Hassan A, Shah N, Riaz Z. Effects of Virtual Reality training on medical students' learning motivation and competency. Pak J Med Sci. 2019;35(3):852–7. doi: 10.12669/pjms.35.3.44. http://europepmc.org/abstract/MED/31258607 .PJMS-35-852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shim J, Kim J, Pyun J, Cho S, Oh M, Kang S, Lee JG, Kim JJ, Cheon J, Kang SG. Comparison of effective teaching methods to achieve skill acquisition using a robotic virtual reality simulator: expert proctoring versus an educational video versus independent training. Medicine (Baltimore) 2018 Dec;97(51):e13569. doi: 10.1097/MD.0000000000013569. doi: 10.1097/MD.0000000000013569.00005792-201812210-00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Van Bruwaene S, Schijven MP, Napolitano D, De Win G, Miserez M. Porcine cadaver organ or virtual-reality simulation training for laparoscopic cholecystectomy: a randomized, controlled trial. J Surg Educ. 2015;72(3):483–90. doi: 10.1016/j.jsurg.2014.11.015.S1931-7204(14)00317-1 [DOI] [PubMed] [Google Scholar]
- 90.Vargas MV, Moawad G, Denny K, Happ L, Misa NY, Margulies S, Opoku-Anane J, Abi Khalil E, Marfori C. Transferability of virtual reality, simulation-based, robotic suturing skills to a live porcine model in novice surgeons: a single-blind randomized controlled trial. J Minim Invasive Gynecol. 2017;24(3):420–5. doi: 10.1016/j.jmig.2016.12.016.S1553-4650(16)31285-7 [DOI] [PubMed] [Google Scholar]
- 91.Vitish-Sharma P, Knowles J, Patel B. Acquisition of fundamental laparoscopic skills: is a box really as good as a virtual reality trainer? Int J Surg. 2011;9(8):659–61. doi: 10.1016/j.ijsu.2011.08.009. https://linkinghub.elsevier.com/retrieve/pii/S1743-9191(11)00554-1 .S1743-9191(11)00554-1 [DOI] [PubMed] [Google Scholar]
- 92.Wainman B, Pukas G, Wolak L, Mohanraj S, Lamb J, Norman GR. The critical role of stereopsis in virtual and mixed reality learning environments. Anat Sci Educ. 2020 May;13(3):401–12. doi: 10.1002/ase.1928. [DOI] [PubMed] [Google Scholar]
- 93.Willis RE, Gomez PP, Ivatury SJ, Mitra HS, Van Sickle KR. Virtual reality simulators: valuable surgical skills trainers or video games? J Surg Educ. 2014;71(3):426–33. doi: 10.1016/j.jsurg.2013.11.003.S1931-7204(13)00286-9 [DOI] [PubMed] [Google Scholar]
- 94.Yang C, Kalinitschenko U, Helmert JR, Weitz J, Reissfelder C, Mees ST. Transferability of laparoscopic skills using the virtual reality simulator. Surg Endosc. 2018 Oct;32(10):4132–7. doi: 10.1007/s00464-018-6156-6.10.1007/s00464-018-6156-6 [DOI] [PubMed] [Google Scholar]
- 95.Abe T, Dar F, Amnattrakul P, Aydin A, Raison N, Shinohara N, Khan MS, Ahmed K, Dasgupta P. MP32-6 Ureteroscopy simulation training under full immersion decreases mental workload in novice operators. J endourology / Endourological Society. 2017 Sep;31(S2):A376. doi: 10.1186/s12909-019-1752-2. [DOI] [Google Scholar]
- 96.Bric J, Connolly M, Kastenmeier A, Goldblatt M, Gould JC. Proficiency training on a virtual reality robotic surgical skills curriculum. Surg Endosc. 2014 Dec;28(12):3343–8. doi: 10.1007/s00464-014-3624-5. [DOI] [PubMed] [Google Scholar]
- 97.Darras KE, Forster BB, Spouge R, de Bruin AB, Arnold A, Nicolaou S, Hu J, Hatala R, van Merriënboer J. Virtual dissection with clinical radiology cases provides educational value to first year medical students. Acad Radiol. 2020 Nov;27(11):1633–40. doi: 10.1016/j.acra.2019.09.031.S1076-6332(19)30497-0 [DOI] [PubMed] [Google Scholar]
- 98.Duarte R, Brito A, Passerotti C, Colombo J, Arap M, Mitre A, Srougi M. 62 Elaborating a learning program on laparoscopy: assessment of the evolution of the novices' performance according to initial training with simulator or animal model. European Urology Supplements. 2012 Feb;11(1):e62,e62a. doi: 10.1016/s1569-9056(12)60061-x. [DOI] [Google Scholar]
- 99.Fu Y, Cavuoto L, Qi D, Panneerselvam K, Arikatla VS, Enquobahrie A, De S, Schwaitzberg SD. Characterizing the learning curve of a virtual intracorporeal suturing simulator VBLaST-SS©. Surg Endosc. 2020 Jul;34(7):3135–44. doi: 10.1007/s00464-019-07081-6. http://europepmc.org/abstract/MED/31482354 .10.1007/s00464-019-07081-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gopal M, Skobodzinski AA, Sterbling HM, Rao SR, LaChapelle C, Suzuki K, Litle VR. Bronchoscopy simulation training as a tool in medical school education. Ann Thorac Surg. 2018 Jul;106(1):280–6. doi: 10.1016/j.athoracsur.2018.02.011.S0003-4975(18)30322-9 [DOI] [PubMed] [Google Scholar]
- 101.Guetterman TC, Sakakibara R, Baireddy S, Kron FW, Scerbo MW, Cleary JF, Fetters MD. Medical students' experiences and outcomes using a virtual human simulation to improve communication skills: mixed methods study. J Med Internet Res. 2019 Nov 27;21(11):e15459. doi: 10.2196/15459. https://www.jmir.org/2019/11/e15459/ v21i11e15459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jensen JK, Dyre L, Jørgensen ME, Andreasen LA, Tolsgaard MG. Simulation-based point-of-care ultrasound training: a matter of competency rather than volume. Acta Anaesthesiol Scand. 2018 Jul;62(6):811–9. doi: 10.1111/aas.13083. [DOI] [PubMed] [Google Scholar]
- 103.Kang SG, Yang KS, Ko YH, Kang SH, Park HS, Lee JG, Kim JJ, Cheon J. A study on the learning curve of the robotic virtual reality simulator. J Laparoendosc Adv Surg Tech A. 2012 Jun;22(5):438–42. doi: 10.1089/lap.2011.0452. [DOI] [PubMed] [Google Scholar]
- 104.Karadogan E, Williams 2nd RL, Howell J, Conatser JR. A stiffness discrimination experiment including analysis of palpation forces and velocities. Simul Healthc. 2010 Oct;5(5):279–88. doi: 10.1097/SIH.0b013e3181e9e783.01266021-201010000-00006 [DOI] [PubMed] [Google Scholar]
- 105.Nomura T, Mamada Y, Nakamura Y, Matsutani T, Hagiwara N, Fujita I, Mizuguchi Y, Fujikura T, Miyashita M, Uchida E. Laparoscopic skill improvement after virtual reality simulator training in medical students as assessed by augmented reality simulator. Asian J Endosc Surg. 2015 Nov;8(4):408–12. doi: 10.1111/ases.12209. [DOI] [PubMed] [Google Scholar]
- 106.Paschold M, Schröder M, Kauff DW, Gorbauch T, Herzer M, Lang H, Kneist W. Virtual reality laparoscopy: which potential trainee starts with a higher proficiency level? Int J Comput Assist Radiol Surg. 2011 Sep;6(5):653–62. doi: 10.1007/s11548-010-0542-4. [DOI] [PubMed] [Google Scholar]
- 107.Rahm S, Wieser K, Wicki I, Holenstein L, Fucentese SF, Gerber C. Performance of medical students on a virtual reality simulator for knee arthroscopy: an analysis of learning curves and predictors of performance. BMC Surg. 2016 Mar 25;16:14. doi: 10.1186/s12893-016-0129-2. https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-016-0129-2 .10.1186/s12893-016-0129-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sánchez-Peralta LF, Sánchez-Margallo FM, Moyano-Cuevas JL, Pagador JB, Enciso S, Gómez-Aguilera EJ, Usón-Gargallo J. Learning curves of basic laparoscopic psychomotor skills in SINERGIA VR simulator. Int J Comput Assist Radiol Surg. 2012 Nov;7(6):881–9. doi: 10.1007/s11548-012-0686-5. [DOI] [PubMed] [Google Scholar]
- 109.Van Herzeele I, O'Donoghue KG, Aggarwal R, Vermassen F, Darzi A, Cheshire NJ. Visuospatial and psychomotor aptitude predicts endovascular performance of inexperienced individuals on a virtual reality simulator. J Vasc Surg. 2010 Apr;51(4):1035–42. doi: 10.1016/j.jvs.2009.11.059. https://linkinghub.elsevier.com/retrieve/pii/S0741-5214(09)02385-4 .S0741-5214(09)02385-4 [DOI] [PubMed] [Google Scholar]
- 110.Akhtar K, Sugand K, Wijendra A, Sarvesvaran M, Sperrin M, Standfield N, Cobb J, Gupte C. The transferability of generic minimally invasive surgical skills: is there crossover of core skills between laparoscopy and arthroscopy? J Surg Educ. 2016;73(2):329–38. doi: 10.1016/j.jsurg.2015.10.010.S1931-7204(15)00275-5 [DOI] [PubMed] [Google Scholar]
- 111.Feifer A, Al-Ammari A, Kovac E, Delisle J, Carrier S, Anidjar M. Randomized controlled trial of virtual reality and hybrid simulation for robotic surgical training. BJU Int. 2011 Nov;108(10):1652–6; discussion 1657. doi: 10.1111/j.1464-410X.2010.10060.x. [DOI] [PubMed] [Google Scholar]
- 112.Gandhi MJ, Anderton MJ, Funk L. Arthroscopic skills acquisition tools: an online simulator for arthroscopy training. Arthroscopy. 2015 Sep;31(9):1671–9. doi: 10.1016/j.arthro.2015.03.019.S0749-8063(15)00246-7 [DOI] [PubMed] [Google Scholar]
- 113.Hagelsteen K, Langegård A, Lantz A, Ekelund M, Anderberg M, Bergenfelz A. Faster acquisition of laparoscopic skills in virtual reality with haptic feedback and 3D vision. Minimally Invasive Therapy & Allied Technologies. 2017 Apr 03;26(5):269–277. doi: 10.1080/13645706.2017.1305970. [DOI] [PubMed] [Google Scholar]
- 114.Andersen SA, Guldager M, Mikkelsen PT, Sørensen MS. The effect of structured self-assessment in virtual reality simulation training of mastoidectomy. Eur Arch Otorhinolaryngol. 2019 Dec 20;276(12):3345–52. doi: 10.1007/s00405-019-05648-6.10.1007/s00405-019-05648-6 [DOI] [PubMed] [Google Scholar]
- 115.Andersen SA, Konge L, Cayé-Thomasen P, Sørensen MS. Learning curves of virtual mastoidectomy in distributed and massed practice. JAMA Otolaryngol Head Neck Surg. 2015 Oct;141(10):913–8. doi: 10.1001/jamaoto.2015.1563.2432653 [DOI] [PubMed] [Google Scholar]
- 116.Andersen SA, Konge L, Cayé-Thomasen P, Sørensen MS. Retention of mastoidectomy skills after virtual reality simulation training. JAMA Otolaryngol Head Neck Surg. 2016 Jul 01;142(7):635–40. doi: 10.1001/jamaoto.2016.0454.2516466 [DOI] [PubMed] [Google Scholar]
- 117.Chiu H, Kang Y, Wang W, Chen C, Hsu W, Tseng M, Wei P. The role of active engagement of peer observation in the acquisition of surgical skills in virtual reality tasks for novices. J Surg Educ. 2019;76(6):1655–62. doi: 10.1016/j.jsurg.2019.05.004.S1931-7204(19)30055-8 [DOI] [PubMed] [Google Scholar]
- 118.Moglia A, Ferrari V, Morelli L, Melfi F, Ferrari M, Mosca F, Cuschieri A. Distribution of innate ability for surgery amongst medical students assessed by an advanced virtual reality surgical simulator. Surg Endosc. 2014 Jun;28(6):1830–7. doi: 10.1007/s00464-013-3393-6. [DOI] [PubMed] [Google Scholar]
- 119.Bjerrum F, Maagaard M, Led Sorensen J, Rifbjerg Larsen C, Ringsted C, Winkel P, Ottesen B, Strandbygaard J. Effect of instructor feedback on skills retention after laparoscopic simulator training: follow-up of a randomized trial. J Surg Educ. 2015;72(1):53–60. doi: 10.1016/j.jsurg.2014.06.013.S1931-7204(14)00191-3 [DOI] [PubMed] [Google Scholar]
- 120.Cychosz CC, Tofte JN, Johnson A, Carender C, Gao Y, Phisitkul P. Factors impacting initial arthroscopy performance and skill progression in novice trainees. Iowa Orthop J. 2019;39(1):7–13. http://europepmc.org/abstract/MED/31413668 . [PMC free article] [PubMed] [Google Scholar]
- 121.Cychosz CC, Tofte JN, Johnson A, Gao Y, Phisitkul P. Fundamentals of arthroscopic surgery training program improves knee arthroscopy simulator performance in arthroscopic trainees. Arthroscopy. 2018 May;34(5):1543–9. doi: 10.1016/j.arthro.2017.11.028.S0749-8063(17)31473-1 [DOI] [PubMed] [Google Scholar]
- 122.da Cruz JA, Dos Reis ST, Cunha Frati RM, Duarte RJ, Nguyen H, Srougi M, Passerotti CC. Does warm-up training in a virtual reality simulator improve surgical performance? A prospective randomized analysis. J Surg Educ. 2016;73(6):974–8. doi: 10.1016/j.jsurg.2016.04.020.S1931-7204(16)30033-2 [DOI] [PubMed] [Google Scholar]
- 123.Eldred-Evans D, Grange P, Cheang A, Yamamoto H, Ayis S, Mulla M, Immenroth M, Sharma D, Reedy G. Using the mind as a simulator: a randomized controlled trial of mental training. J Surg Educ. 2013;70(4):544–51. doi: 10.1016/j.jsurg.2013.04.003.S1931-7204(13)00111-6 [DOI] [PubMed] [Google Scholar]
- 124.Hardcastle T, Wood A. The utility of virtual reality surgical simulation in the undergraduate otorhinolaryngology curriculum. J Laryngol Otol. 2018 Dec;132(12):1072–6. doi: 10.1017/S0022215118002025.S0022215118002025 [DOI] [PubMed] [Google Scholar]
- 125.Jungmann F, Gockel I, Hecht H, Kuhr K, Räsänen J, Sihvo E, Lang H. Impact of perceptual ability and mental imagery training on simulated laparoscopic knot-tying in surgical novices using a Nissen fundoplication model. Scand J Surg. 2011;100(2):78–85. doi: 10.1177/145749691110000203. [DOI] [PubMed] [Google Scholar]
- 126.Kang SG, Ryu BJ, Yang KS, Ko YH, Cho S, Kang SH, Patel VR, Cheon J. An effective repetitive training schedule to achieve skill proficiency using a novel robotic virtual reality simulator. J Surg Educ. 2015;72(3):369–76. doi: 10.1016/j.jsurg.2014.06.023.S1931-7204(14)00303-1 [DOI] [PubMed] [Google Scholar]
- 127.Kwon K, Park JS, Shin B. Virtual anatomical and endoscopic exploration method of internal human body for training simulator. J Korean Med Sci. 2020 Mar 30;35(12):e90. doi: 10.3346/jkms.2020.35.e90. https://jkms.org/DOIx.php?id=10.3346/jkms.2020.35.e90 .35.e90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Loukas C, Nikiteas N, Schizas D, Lahanas V, Georgiou E. A head-to-head comparison between virtual reality and physical reality simulation training for basic skills acquisition. Surg Endosc. 2012 Sep;26(9):2550–8. doi: 10.1007/s00464-012-2230-7. [DOI] [PubMed] [Google Scholar]
- 129.Onishi S, Ikee T, Murakami M, Yano K, Harumatsu T, Baba T, Yamada K, Yamada W, Masuya R, Machigashira S, Nakame K, Mukai M, Kaji T, Ieiri S. A comparison of the effectiveness between three different endoscopic surgical skill training programs for medical students using the infant laparoscopic fundoplication simulator: a randomized controlled trial. J Laparoendosc Adv Surg Tech A. 2019 Oct;29(10):1252–8. doi: 10.1089/lap.2019.0212. [DOI] [PubMed] [Google Scholar]
- 130.Paschold M, Huber T, Zeißig SR, Lang H, Kneist W. Tailored instructor feedback leads to more effective virtual-reality laparoscopic training. Surg Endosc. 2014 Mar;28(3):967–73. doi: 10.1007/s00464-013-3258-z. [DOI] [PubMed] [Google Scholar]
- 131.Paschold M, Niebisch S, Kronfeld K, Herzer M, Lang H, Kneist W. Cold-start capability in virtual-reality laparoscopic camera navigation: a base for tailored training in undergraduates. Surg Endosc. 2013 Jun;27(6):2169–77. doi: 10.1007/s00464-012-2735-0. [DOI] [PubMed] [Google Scholar]
- 132.Salkini MW, Doarn CR, Kiehl N, Broderick TJ, Donovan JF, Gaitonde K. The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol. 2010 Jan;24(1):99–102. doi: 10.1089/end.2009.0307. [DOI] [PubMed] [Google Scholar]
- 133.Selvander M, Åsman P. Virtual reality cataract surgery training: learning curves and concurrent validity. Acta Ophthalmol. 2012 Aug;90(5):412–7. doi: 10.1111/j.1755-3768.2010.02028.x. doi: 10.1111/j.1755-3768.2010.02028.x. [DOI] [PubMed] [Google Scholar]
- 134.da Cruz JA, Nguyen H, dos Reis ST, Lobo Filho MM, Cunha Frati RM, de Mattos BV, Crozatti LL, Duarte RJ, Srougi M, Passerotti CC. 878 does warm-up training in a virtual reality simulator improves surgical performance for the novice laparoscopic surgeons? A prospective randomized study. Journal of Urology. 2013 Apr;189(4S):e362. doi: 10.1016/j.juro.2013.02.449. [DOI] [Google Scholar]
- 135.Snyder CW, Vandromme MJ, Tyra SL, Hawn MT. Retention of colonoscopy skills after virtual reality simulator training by independent and proctored methods. Am Surgeon. 2010 Jul 01;76(7):743–6. doi: 10.1177/000313481007600732. [DOI] [PubMed] [Google Scholar]
- 136.Snyder CW, Vandromme MJ, Tyra SL, Porterfield JR, Clements RH, Hawn MT. Effects of virtual reality simulator training method and observational learning on surgical performance. World J Surg. 2011 Feb;35(2):245–52. doi: 10.1007/s00268-010-0861-1. [DOI] [PubMed] [Google Scholar]
- 137.Strandbygaard J, Bjerrum F, Maagaard M, Winkel P, Larsen C, Ringsted C, Gluud C, Grantcharov T, Ottesen B, Sorensen JL. Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: a randomized trial. Ann Surg. 2013 May;257(5):839–44. doi: 10.1097/SLA.0b013e31827eee6e. [DOI] [PubMed] [Google Scholar]
- 138.Wijewickrema S, Zhou Y, Ioannou I, Copson B, Piromchai P, Yu C, Briggs R, Bailey J, Kennedy G, O'Leary S. Presentation of automated procedural guidance in surgical simulation: results of two randomised controlled trials. J Laryngol Otol. 2018 Mar;132(3):257–63. doi: 10.1017/S0022215117002626.S0022215117002626 [DOI] [PubMed] [Google Scholar]
- 139.Chen J, Smith AD, Khan MA, Sinning AR, Conway ML, Cui D. Visualization of stereoscopic anatomic models of the paranasal sinuses and cervical vertebrae from the surgical and procedural perspective. Anat Sci Educ. 2017 Nov;10(6):598–606. doi: 10.1002/ase.1702. [DOI] [PubMed] [Google Scholar]
- 140.Creutzfeldt J, Hedman L, Felländer-Tsai L. Effects of pre-training using serious game technology on CPR performance--an exploratory quasi-experimental transfer study. Scand J Trauma Resusc Emerg Med. 2012 Dec 06;20:79. doi: 10.1186/1757-7241-20-79. https://sjtrem.biomedcentral.com/articles/10.1186/1757-7241-20-79 .1757-7241-20-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.De Ponti R, Marazzato J, Maresca AM, Rovera F, Carcano G, Ferrario MM. Pre-graduation medical training including virtual reality during COVID-19 pandemic: a report on students' perception. BMC Med Educ. 2020 Sep 25;20(1):332. doi: 10.1186/s12909-020-02245-8. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02245-8 .10.1186/s12909-020-02245-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gout L, Hart A, Houze-Cerfon C, Sarin R, Ciottone GR, Bounes V. Creating a novel disaster medicine virtual reality training environment. Prehosp Disaster Med. 2020 Apr;35(2):225–8. doi: 10.1017/S1049023X20000230.S1049023X20000230 [DOI] [PubMed] [Google Scholar]
- 143.Design, development and evaluation of collaborative team training method in virtual worlds for time-critical medical procedures. Dissertation Abstracts International Section A: Humanities and Social Sciences. [2022-01-24]. https://psycnet.apa.org/record/2014-99230-318 .
- 144.Kleinert R, Wahba R, Chang D, Plum P, Hölscher AH, Stippel DL. 3D immersive patient simulators and their impact on learning success: a thematic review. J Med Internet Res. 2015 Apr 08;17(4):e91. doi: 10.2196/jmir.3492. https://www.jmir.org/2015/4/e91/ v17i4e91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zackoff MW, Real FJ, Cruse B, Davis D, Klein M. Medical student perspectives on the use of immersive virtual reality for clinical assessment training. Acad Pediatr. 2019;19(7):849–51. doi: 10.1016/j.acap.2019.06.008.S1876-2859(19)30295-5 [DOI] [PubMed] [Google Scholar]
- 146.Paech D, Giesel FL, Unterhinninghofen R, Schlemmer H, Kuner T, Doll S. Cadaver-specific CT scans visualized at the dissection table combined with virtual dissection tables improve learning performance in general gross anatomy. Eur Radiol. 2017 May;27(5):2153–60. doi: 10.1007/s00330-016-4554-5.10.1007/s00330-016-4554-5 [DOI] [PubMed] [Google Scholar]
- 147.Sugand K, Mawkin M, Gupte C. Training effect of using Touch Surgery for intramedullary femoral nailing. Injury. 2016 Feb;47(2):448–52. doi: 10.1016/j.injury.2015.09.036.S0020-1383(15)00574-4 [DOI] [PubMed] [Google Scholar]
- 148.Duarte R, Cury J, Neves L, Srougi M. 65 Establishing the minimal number of simulator training sessions necessary to develop basic laparoscopic skills competence: Evaluation of the learning curve. European Urology Supplements. 2012 Feb;11(1):e65–e65a. doi: 10.1016/s1569-9056(12)60064-5. [DOI] [PubMed] [Google Scholar]
- 149.Developmental Research: The Definition and Scope. ERIC. 1994. [2022-01-24]. https://eric.ed.gov/?id=ED373753#:~:text=Developmental%20research%2C%20as%20opposed%20to, of%20internal%20consistency%20and%20effectiveness .
- 150.The world's most advanced 3D anatomy platform. Complete Anatomy. [2022-01-24]. https://3d4medical.com/
- 151.Bouaoud J, El Beheiry M, Jablon E, Schouman T, Bertolus C, Picard A, Masson J, Khonsari RH. DIVA, a 3D virtual reality platform, improves undergraduate craniofacial trauma education. J Stomatol Oral Maxillofac Surg. 2021 Sep;122(4):367–71. doi: 10.1016/j.jormas.2020.09.009.S2468-7855(20)30221-4 [DOI] [PubMed] [Google Scholar]
- 152.Sugand K, Mawkin M, Gupte C. Training effect of using Touch Surgery for intramedullary femoral nailing. Injury. 2016 Feb;47(2):448–52. doi: 10.1016/j.injury.2015.09.036.S0020-1383(15)00574-4 [DOI] [PubMed] [Google Scholar]
- 153.Chen S, Zhu J, Cheng C, Pan Z, Liu L, Du J, Shen X, Shen Z, Zhu H, Liu J, Yang H, Ma C, Pan H. Can virtual reality improve traditional anatomy education programmes? A mixed-methods study on the use of a 3D skull model. BMC Med Educ. 2020 Oct 31;20(1):395. doi: 10.1186/s12909-020-02255-6. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02255-6 .10.1186/s12909-020-02255-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zackoff MW, Young D, Sahay RD, Fei L, Real FJ, Guiot A, Lehmann C, Klein M. Establishing objective measures of clinical competence in undergraduate medical education through immersive virtual reality. Acad Pediatr. 2021 Apr;21(3):575–9. doi: 10.1016/j.acap.2020.10.010. http://europepmc.org/abstract/MED/33091608 .S1876-2859(20)30566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Stepan K, Zeiger J, Hanchuk S, Del Signore A, Shrivastava R, Govindaraj S, Iloreta A. Immersive virtual reality as a teaching tool for neuroanatomy. Int Forum Allergy Rhinol. 2017 Oct;7(10):1006–13. doi: 10.1002/alr.21986. [DOI] [PubMed] [Google Scholar]
- 156.Paschold M, Huber T, Lang H, Kneist W. Influence of a short term camera navigation training on laparoscopic performance and team cooperation in a virtual reality setting. J Am College Surgeons. 2014 Oct;219(4):e165. doi: 10.1016/j.jamcollsurg.2014.07.830. [DOI] [Google Scholar]
- 157.Adams CM, Wilson TD. Virtual cerebral ventricular system: an MR-based three-dimensional computer model. Anat Sci Educ. 2011;4(6):340–7. doi: 10.1002/ase.256. [DOI] [PubMed] [Google Scholar]
- 158.Allen LK, Bhattacharyya S, Wilson TD. Development of an interactive anatomical three-dimensional eye model. Anat Sci Educ. 2015;8(3):275–82. doi: 10.1002/ase.1487. [DOI] [PubMed] [Google Scholar]
- 159.Asensio Romero L, Asensio Gómez M, Prats-Galino A, Juanes Méndez JA. 3D models of female pelvis structures reconstructed and represented in combination with anatomical and radiological sections. J Med Syst. 2018 Jan 15;42(3):37. doi: 10.1007/s10916-018-0891-z.10.1007/s10916-018-0891-z [DOI] [PubMed] [Google Scholar]
- 160.Cui D, Lynch JC, Smith AD, Wilson TD, Lehman MN. Stereoscopic vascular models of the head and neck: a computed tomography angiography visualization. Anat Sci Educ. 2016;9(2):179–85. doi: 10.1002/ase.1537. [DOI] [PubMed] [Google Scholar]
- 161.Fang B, Wu Y, Chu C, Li Y, Luo N, Liu K, Tan L, Zhang S. Creation of a virtual anatomy system based on Chinese visible human data sets. Surg Radiol Anat. 2017 Apr;39(4):441–9. doi: 10.1007/s00276-016-1741-7.10.1007/s00276-016-1741-7 [DOI] [PubMed] [Google Scholar]
- 162.Hu N, Shan J, Zheng X, Tan L, Xia Y, Luo H, Hou W, Fang B, Wang G. Development of an e-learning environment for anatomical education of female pelvic region. J Med Imaging Hlth Inform. 2014 Oct 01;4(5):701–4. doi: 10.1166/jmihi.2014.1302. [DOI] [Google Scholar]
- 163.Shu HS, Li XL, Deng Y, Qv TJ, Li YS, Yuan W, Shao H. Establishment and application of human interactive three-dimensional spine software. Applied Mechanics Materials. 2011 Nov;140:132–6. doi: 10.4028/www.scientific.net/amm.140.132. [DOI] [Google Scholar]
- 164.Zilverschoon M, Vincken KL, Bleys RL. The virtual dissecting room: creating highly detailed anatomy models for educational purposes. J Biomed Inform. 2017 Jan;65:58–75. doi: 10.1016/j.jbi.2016.11.005. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(16)30164-2 .S1532-0464(16)30164-2 [DOI] [PubMed] [Google Scholar]
- 165.Lewis TL, Burnett B, Tunstall RG, Abrahams PH. Complementing anatomy education using three-dimensional anatomy mobile software applications on tablet computers. Clin Anat. 2014 Apr;27(3):313–20. doi: 10.1002/ca.22256. [DOI] [PubMed] [Google Scholar]
- 166.O'Rourke JC, Smyth L, Webb AL, Valter K. How can we show you, if you can't see it? Trialing the use of an interactive three-dimensional micro-CT model in medical education. Anat Sci Educ. 2020 Mar;13(2):206–17. doi: 10.1002/ase.1890. [DOI] [PubMed] [Google Scholar]
- 167.Taubert M, Webber L, Hamilton T, Carr M, Harvey M. Virtual reality videos used in undergraduate palliative and oncology medical teaching: results of a pilot study. BMJ Support Palliat Care. 2019 Sep;9(3):281–5. doi: 10.1136/bmjspcare-2018-001720. http://europepmc.org/abstract/MED/30808627 .bmjspcare-2018-001720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.From Vesalius to virtual reality: how embodied cognition facilitates the visualization of anatomy. ERIC. [2022-01-24]. https://eric.ed.gov/?id=ED519321 .
- 169.Djukic T, Mandic V, Filipovic N. Virtual reality aided visualization of fluid flow simulations with application in medical education and diagnostics. Comput Biol Med. 2013 Dec;43(12):2046–52. doi: 10.1016/j.compbiomed.2013.10.004.S0010-4825(13)00282-5 [DOI] [PubMed] [Google Scholar]
- 170.Cui D, Wilson T, Rockhold R, Lehman M, Lynch J. Stereoscopic (3D) visualization improves medical student comprehension of head and neck vascular anatomy. FASEB J. 2016;30:S570. [Google Scholar]
- 171.Teistler M, Brunberg JA, Bott OJ, Breiman RS, Ebert LC, Ross SG, Dresing K. Understanding spatial relationships in US: a computer-based training tool that utilizes inexpensive off-the-shelf game controllers. Radiographics. 2014 Sep;34(5):1334–43. doi: 10.1148/rg.345130039. [DOI] [PubMed] [Google Scholar]
- 172.Ros M, Debien B, Cyteval C, Molinari N, Gatto F, Lonjon N. Applying an immersive tutorial in virtual reality to learning a new technique. Neurochirurgie. 2020 Aug;66(4):212–8. doi: 10.1016/j.neuchi.2020.05.006.S0028-3770(20)30348-9 [DOI] [PubMed] [Google Scholar]
- 173.Anderson RH, Bolender D, Mori S, Tretter JT. Virtual reality perhaps, but is this real cardiac anatomy? Clin Anat. 2019 May;32(4):468. doi: 10.1002/ca.23306. [DOI] [PubMed] [Google Scholar]
- 174.Wijewickrema S, Piromchai P, Zhou Y, Ioannou I, Bailey J, Kennedy G, O'Leary S. Developing effective automated feedback in temporal bone surgery simulation. Otolaryngol Head Neck Surg. 2015 Jun;152(6):1082–8. doi: 10.1177/0194599815570880.0194599815570880 [DOI] [PubMed] [Google Scholar]
- 175.Chang PW, Chen BC, Jones CE, Bunting K, Chakraborti C, Kahn MJ. Virtual reality supplemental teaching at low-cost (VRSTL) as a medical education adjunct for increasing early patient exposure. Med Sci Educ. 2017 Oct 26;28(1):3–4. doi: 10.1007/s40670-017-0483-4. [DOI] [Google Scholar]
- 176.Jensen L, Konradsen F. A review of the use of virtual reality head-mounted displays in education and training. Educ Inf Technol. 2017 Nov 25;23(4):1515–29. doi: 10.1007/s10639-017-9676-0. [DOI] [Google Scholar]
- 177.Alaker M, Wynn GR, Arulampalam T. Int J Surg. 2016 May;29:85–94. doi: 10.1016/j.ijsu.2016.03.034. https://linkinghub.elsevier.com/retrieve/pii/S1743-9191(16)00251-X .S1743-9191(16)00251-X [DOI] [PubMed] [Google Scholar]
- 178.Aïm F, Lonjon G, Hannouche D, Nizard R. Effectiveness of virtual reality training in orthopaedic surgery. Arthroscopy. 2016 Jan;32(1):224–32. doi: 10.1016/j.arthro.2015.07.023.S0749-8063(15)00648-9 [DOI] [PubMed] [Google Scholar]
- 179.Yoo JS, Patel DS, Hrynewycz NM, Brundage TS, Singh K. The utility of virtual reality and augmented reality in spine surgery. Ann Transl Med. 2019 Sep;7(Suppl 5):S171. doi: 10.21037/atm.2019.06.38. doi: 10.21037/atm.2019.06.38.atm-07-S5-S171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Anatomy TV homepage. Anatomy TV. [2022-01-24]. https://www.anatomy.tv/titles .
- 181.Parham G, Bing EG, Cuevas A, Fisher B, Skinner J, Mwanahamuntu M, Sullivan R. Creating a low-cost virtual reality surgical simulation to increase surgical oncology capacity and capability. Ecancermedicalscience. 2019;13:910. doi: 10.3332/ecancer.2019.910. http://europepmc.org/abstract/MED/31123493 .can-13-910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shakarishvili G. Virtual reality technology for experiential learning in global health training curricula: a prototype for testing. The Lancet Global Health. 2019 Mar;7:S27. doi: 10.1016/s2214-109x(19)30112-3. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies.
Data extraction form.
Supplementary figures.


