Abstract
Iron plays an important role in a wide range of metabolic pathways that are important for neuronal health. Excessive levels of iron, however, can promote toxicity and cell death. An example of an iron overload disorder is hemochromatosis (HH) which is a genetic disorder of iron metabolism in which the body’s ability to regulate iron absorption is altered, resulting in iron build-up and injury in several organs. The retina was traditionally assumed to be protected from high levels of systemic iron overload by the blood-retina barrier. However, recent data shows that expression of genes that are associated with HH can disrupt retinal iron metabolism. Thus, the effects of iron overload on the retina have become an area of research interest, as excessively high levels of iron are implicated in several retinal disorders, most notably age–related macular degeneration. This review is an effort to highlight risk factors for excessive levels of systemic iron build-up in the retina and its potential impact on the eye health. Information is integrated across clinical and preclinical animal studies to provide insights into the effects of systemic iron loading on the retina.
Keywords: retina, iron, hemochromatosis, iron overload, retinal disorder
Introduction
Iron is essential for neuronal development and function (Lozoff et al., 2003). Iron plays key roles in neuronal metabolism, oxygen transport, oxidative phosphorylation, myelin production, and the synthesis of neurotransmitters, as reviewed in detail elsewhere (Crichton et al., 2011; Ward et al., 2014). However, abnormally high levels of intracellular iron, termed iron loading, can be neurotoxic and may lead to cellular injury. The exact mechanism of iron-induced neuronal degeneration is not yet fully understood; however, several mechanisms have been postulated. Perhaps, most well studied mechanism is the role of iron in mediating the formation of reactive oxygen species (ROS), a natural byproduct of Fenton reactions, which can contribute to tissue injury (Lloyd et al., 1997). In addition, high intracellular iron levels can affect the expression of several classes of genes including iron-dependent oxidative metabolism and the attendant oxidative stress genes (Casey et al., 1988; Ingrassia et al., 2019). Another suggested pathway through which errors in iron metabolism can be deleterious is ferroptosis, a recently identified form of cell death, which has been implicated in a number of central nervous system (CNS) diseases (Dixon et al., 2012; Guiney et al., 2017; Lane et al., 2018; Moreau et al., 2018; Masaldan et al., 2019).
To avoid the potential of iron toxicity, living organisms have developed homeostatic mechanisms, that regulate various proteins involved in iron import, storage, and export to maintain iron within a favorable physiological range. Most iron is tightly complexed with proteins or other ligands, which restrict its redox potential. However, excess iron can build-up in the body in several ways including early life exposure to iron feeding (Hare et al., 2015); normal aging (Zecca et al., 2004), eating meat (heme-iron intake) (Haider et al., 2018), and acute toxicity from blood transfusions (Harmatz et al., 2000; Cunningham et al., 2004). In contrast low iron vegan and vegetarian diets have lower accumulation of iron and increased risk of iron deficiency with associated fatigue and impaired learning and concentration symptoms (Desmond et al., 2021). The retinal photoreceptors are the most highly energetically demanding tissue per weight in the whole body (Wong-Riley, 2010; Country, 2017), and photoreceptors are mitochondria-rich cells. The primary function of mitochondria is to generate energy in the form of adenosine triphosphate (ATP). Due to a lack of protective histones and proximity to the inner mitochondrial membrane, where oxidants are formed, mitochondrial DNA is vulnerable to oxidative damage (Gao et al., 2009; Lin et al., 2011). Iron-mediated damage to mitochondria is believed to be through various pathways including altered mitochondrial uptake of other metal ions (Jouihan et al., 2008), ferroptosis (Battaglia et al., 2020; Li et al., 2020) and oxidative damage leading to decreased synthesis of respiratory chain subunits encoded by the mitochondrial genome and further declines in cellular respiration. Mitochondrial iron homeostasis is crucial for normal physiology of the retina and any dysregulation in balance of the redox system in mitochondria has been associated with age-related retinal pathophysiology (Jarrett et al., 2008; Barot et al., 2011).
However, unlike the brain where iron-related pathology has received significant attention (Wessling-Resnick, 2017; Daglas and Adlard, 2018; D’Mello and Kindy, 2020), less is known about retinal susceptibility to iron loading. An improved understanding of iron’s role in retinal health and disease conditions will guide the development of therapies for patients with hemochromatosis and possibly other iron overload conditions. We mainly focus on retinal structural and functional changes in clinical cases and preclinical models. This is particularly important because currently there is no routine clinical visual check–up for high-risk demographic such as patients with hemochromatosis or even people with high levels of dietary iron intake which may have been at risk of retinal iron accumulation and disease-related sequelae. Improving prognosis in people at risk, as some changes may be more easily attenuated or reversed than others are critical and subsequently treatments could be commenced before irreversible damage to the tissue occurs.
Hemochromatosis
Iron build-up in the human body can arise as a result of genetic anomalies, one such example is hemochromatosis (HH) (Feder et al., 1996; Pietrangelo, 2003). HH is an autosomal recessive disorder characterized by increased iron absorption (Andrews, 1999), leading to excessive tissue iron deposition. A number of gene mutations have been found to underlie this phenotype as summarized in Table 1.
TABLE 1.
Summary of hemochromatosis phenotypes with their corresponding genes and clinical manifestationsa.
| Types | Main clinical manifestations | Inheritance | |
| Type 1 | HFE * | Late onset, >30 years old, mild to severe hepatomegaly, elevated aminotransferase levels, arthralgia, arthritis | Recessive |
| Type 2 | Hemojuvelin (HJV)/ Hepcidin (HAMP) | Early onset, <30 years old, severe cardiomyopathy, arrhythmia, diabetes, hypogonadism | Recessive |
| Type 3 | TFR2 | Late onset, >30 years old, mild to severe hepatomegaly, elevated aminotransferase levels | Recessive |
| Type 4 | Ferroportin (SLC40A1) | Late onset, >40 years old, mild hepatomegaly, elevated aminotransferase levels, arthralgia, arthritis | Dominant |
aPietrangelo, 2004; Brissot and de Bels, 2006; Andrews, 2008; Fix and Kowdley, 2008; Powell et al., 2016.
*Variation in this gene including C282Y, H63D, and S65C are associated with increasing risk of neurodegenerative disorders particularly Parkinson’s disease.
There are four main types of HH which have been identified based on their underlying genetic mutations. Type 1 forms the majority of HH cases and is attributed to homozygosity for a single nucleotide polymorphism (SNP) in the HFE gene located on chromosome 6p. This genetic variation causes the substitution of a cysteine with a tyrosine residue at amino acid 282 (C282Y) (Feder et al., 1996). The C282Y SNP has a carrier frequency of 10–20%, with 0.3–0.7% homozygosity in populations of northern European ancestry (Beutler et al., 2002; Allen, 2008). In non-Caucasian populations, however, this SNP is reported to have a low allele frequency (Merryweather-Clarke et al., 1997; Cullen et al., 1998).
Another allelic variant of the HFE gene involving the substitution of an aspartic acid with a histidine (H63D), has an even higher allele frequency that C282Y (Gochee et al., 2002; Adams, 2005). However, it generally does not appear to have considerable effects on iron status, even in the homozygous state. Inheritance of a dual polymorphism (H63D and C282Y) as a compound heterozygous genotype, however, can cause clinical hemochromatosis (Beutler et al., 1996; Jouanolle et al., 1997). HFE – associated hemochromatosis can also be due to a serine – to – cysteine substitution at amino acid position 65 (S65C) (Mura et al., 1999). This variation in the HFE gene is associated with the mild form of hemochromatosis and accounts for 7.8% of HH cases that were neither C282Y nor H63D substitutions (Mura et al., 1999).
Type 2 HH is due to mutations in the hemojuvelin gene (HJV) or the gene encoding hepcidin (HAMP); accounts for a very severe form of iron loading where iron accumulates rapidly in early postnatal life (Papanikolaou et al., 2004).
Mutations in the TFR2 gene causes Type 3 HH in which homozygosity for the Y250X nonsense mutation in the TFR2 gene is reported to be the most common cause (Camaschella et al., 2000). This mutation induces excessive iron loading with a similar phenotype to Type 1 HH, although patients exhibit greater variation in the severity of symptoms (Olynyk et al., 2008). Patients with mutations in both TFR2 and HFE are reported to have a severe iron loading phenotype (Pietrangelo et al., 2005; Rueda Adel et al., 2011; Del-Castillo-Rueda et al., 2012). The common feature of HH Types 1 to 3 is reduction of hepcidin expression which provides a possible mechanistic insight into build-up of iron in tissues (Brissot et al., 2019; Piperno et al., 2020).
Considering the importance of the hepcidin regulatory pathway in influencing body iron homeostasis, any mutation in the SLC40A1 gene which encodes ferroportin; the molecular target for hepcidin results in Type 4 HH (Camaschella et al., 2000; Montosi et al., 2001; Callebaut et al., 2014). In this type of HH, mutation in SLC40A1 gene either restricts the binding of hepcidin to ferroportin (Nemeth et al., 2004) or affects the ability of ferroportin to transport iron (Détivaud et al., 2013).
Most forms of hemochromatosis cause injury in peripheral tissues (heart and liver), however, it should be noted that the principal variants of the HFE gene can affect brain iron homeostasis and is considered as a risk factor for neurodegenerative disorders, particularly Parkinson’s disease (Dekker et al., 2003; Guerreiro et al., 2006). In addition, hematochromatosis associated genes are expressed in the retina in a cell type specific manner (Gnana-Prakasam et al., 2008), which means retinal iron homeostasis may be disrupted in specific retinal cells by systemic iron loading conditions.
The Mammalian Retina
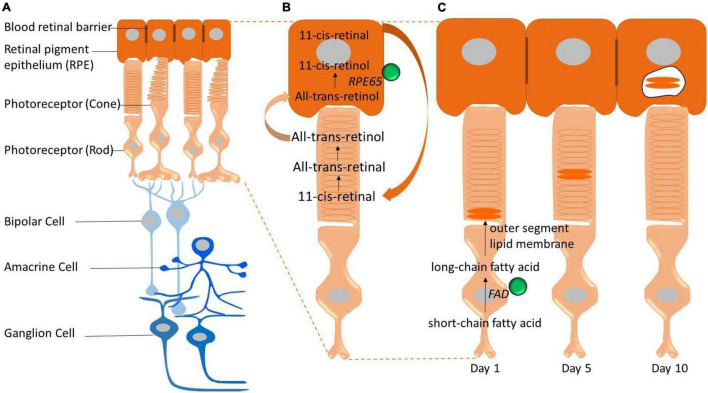
The mammalian retina is an integral part of the CNS; capturing light energy (photons) and transforming it into a chemical signal to be passed onto the brain via electrical impulses. The retina has a multi–layered structure (see Figures 1A,B) composed of five main neuronal classes and supporting glia. Traditionally, it has been assumed that the retina is protected from systemic iron loading by the blood–retinal barrier, however, increasing evidence suggests that the blood–retinal barrier is unable to shield the retina against morbid levels of serum iron (Zhao et al., 2014). This is potentially problematic for the retina, given it is highly energetically demanding (Wong-Riley, 2010; Country, 2017), making it more likely vulnerable to metabolic and oxidative stress related to iron-loading. The potential for injury from excessive iron loading in the retina has become an area of research interest, particularly in conditions where the integrity of the blood–retina barrier is compromised. Indeed, studies have highlighted interactions between aging and iron homeostasis as potential pathological mediators for a number of retinal disorders including age-related macular degeneration (Dunaief, 2006; Biesemeier et al., 2015; Song et al., 2016; Čolak et al., 2018).
FIGURE 1.
Schematic representation of the retina and key pathways that involve iron (iron represented by green spheres). (A) The neural retina is isolated from the bloodstream (choroidal vessels) by the blood–retinal barrier. The outer blood–retinal–barrier is formed by tight junctions located between the retinal pigment epithelium (RPE). Photoreceptors convert light into electrical signals through the visual cycle and these electrical signals are communicated through the retina via the bipolar and ganglion cells. (B) Iron is required for the visual cycle. Regeneration of 11-cis-retinal, the chromophore of visual pigments in photoreceptor cells, is essential for vision and depends on an earlier reaction catalyzed by the iron-containing isomerase, retinal pigment epithelium-specific 65 kDa protein (RPE65). (C) Photoreceptor outer segments (rods and cones) are constantly synthesized and shed. This process is highly dependent on fatty acid desaturase (FAD) enzyme which is iron dependent to synthesize new membrane lipids.
Iron Metabolism and Retinal Iron Homeostasis
Dietary iron is the exclusive source of iron for mammals which consists of heme iron (e.g., meat or offal products) and non-heme iron (e.g., legumes, nuts, and seeds) sources (Bjorn-Rasmussen et al., 1974). Iron cannot be actively excreted through normal pathways such as the intestine or kidney and only small levels of iron can be discarded through sloughing of mucosal cells and desquamation, menstruation and other blood loss (Andrews, 1999; Miret et al., 2003; Kohgo et al., 2008). One of the earliest experiments to show a lack of execratory routs for iron was conducted by Widdowson and McCance (1937). The author orally administrated 1000 mg of ferric ammonium citrate per day to four volunteers over 36–46 days, and found that urinary and fecal output contained only trace amounts of unabsorbed iron (Widdowson and McCance, 1937). This work contributed to the current understanding that iron metabolism is a semi-closed system, with low levels of excretion (Kohgo et al., 2008). This closed system means that non-biodegradable iron can build-up in tissues over time, as reviewed elsewhere (Hahn et al., 2006, 2009; Hare et al., 2015, 2017; Shu and Dunaief, 2018). As iron is rare in our environment the body has adopted to store iron. In an iron replete modern diet, the abundance of iron is potentially contributing to health issues. Therefore, age-related accumulation of iron and its adverse effects may be a contributor to increased risk of neurodegeneration with age.
Dietary iron is chiefly absorbed in the upper part of the intestine through the apical side of the enterocyte brush border (Fuqua et al., 2012). After absorption across the gut, iron forms a complex, most notably with the iron carrier protein transferrin (TF), which chaperones iron in the circulation (Andrews, 1999; Meynard et al., 2014). A transferrin molecule can bind two molecules of ferric (Fe3+) iron and is thought to be the main source of iron delivery to neurons in the CNS (Chua et al., 2007).
The specific locations of iron handling proteins in the retina as summarized in Table 2 may provide clues as to functions that may be impacted by anomalies in iron metabolism and dysregulation. In the retina, transferrin is found in RPE cells, but it is also detectable in the neural retina including photoreceptor inner and outer segments, suggesting that iron is trafficked in the retina itself. Iron uptake from the choroidal circulation into the RPE cells is mediated by transferrin receptors 1 (TFR1), which has been found on basolateral and apical surfaces of RPE cells, suggesting that there is bi-directional iron movement across the RPE cells depending on the iron status of the retina (Yefimova et al., 2000; He et al., 2007). TFR1 has also been colocalized to the ganglion cell layer, inner nuclear layer, outer plexiform layer, and inner segment of photoreceptors (Yefimova et al., 2000; He et al., 2007).
TABLE 2.
Summary of the major iron-related proteins found in the retina.
| Protein | Function | Expression in retina | |
| Iron import | Transferrin receptor 1 (TFR1) | Iron uptake | Ganglion cell layer, inner nuclear layer, outer plexiform layer, photoreceptor inner segment, RPE basolateral membrane, and choroid (Yefimova et al., 2000) |
| Transferrin receptor 2 (TFR2) | Iron uptake | RPE (basolateral membrane) (Martin et al., 2006) | |
| Divalent metal transporter-1 (DMT-1) | Iron uptake | Rod bipolar cell bodies and axon termini, horizontal cell bodies, and photoreceptor inner segments (He et al., 2007) | |
| Iron export | Ferroportin (SLC40A1) | Iron export | RPE, photoreceptor inner segments, inner and outer plexiform layers, and ganglion cell layer (Hahn et al., 2004a) |
| Iron storage | Ferritin (Ft) | Storage; anti-oxidant activity in association with p53 (Lee et al., 2009); regulator of angiogenesis (Coffman et al., 2009); receptor for hepcidin (Nemeth et al., 2004) | Photoreceptor inner segments, RPE, choroid, inner nuclear layer, and ganglion cell layer (He et al., 2007) |
| Iron regulatory | Hepcidin (HAMP) | Internalization of iron in association with ferroportin | Müller cells, photoreceptor cells, and RPE (Gnana-Prakasam et al., 2008; Hadziahmetovic et al., 2011a) |
| Ceruloplasmin (CP) | Catalyzing the oxidization of Fe2+ to Fe3+ (ferroxidase) | Müller glia and RPE(Chen et al., 2003; Hahn et al., 2004b) | |
| Hephaestin (HEPH) | Catalyzing the oxidization of Fe2+ to Fe3+ (ferroxidase) | Müller glia and RPE (Hahn et al., 2004b) | |
| HFE | HFE in association with TFR2 regulates hepcidin (Wallace et al., 2009) | Restricted exclusively to basolateral membrane of RPE (Martin et al., 2006) | |
| Hemojuvelin (HJV) | Induces the expression of hepcidin (Babitt et al., 2006) | RPE (apical membrane facing neural retina), Müller glia, photoreceptors, and ganglion cells (Gnana-Prakasam et al., 2009b) |
Although TFR1 is the predominant protein responsible for cellular iron uptake, another homologous protein called transferrin receptors 2 (TFR2) also has a cooperative role in mediating retinal cellular iron uptake (Kawabata et al., 1999). The expression of TFR2 appears to be primarily in the RPE (Martin et al., 2006). TFR2 also serves as part of a feedback mechanism via its role as a membrane protein for serum iron levels. TFR2 is postulated to activate a downstream signaling pathway that leads to increase the iron-regulatory protein hepcidin. Increased levels of hepcidin, tightly influences intestinal iron absorption and macrophage iron recycling, helping to lower serum iron (Goswami and Andrews, 2006; Schmidt et al., 2008).
In addition, there is a non-transferrin-bound iron protein called divalent metal transporter-1 (DMT-1), which can contribute to transportation of ferrous iron across the plasma membrane or in some cases out of endosomal compartments (Gunshin et al., 1997). DMT-1 has been colocalized to rod bipolar cell bodies and axon termini, horizontal cell bodies and photoreceptor inner segments (He et al., 2007; Song and Dunaief, 2013).
Once iron is taken up into cells, it is primarily stored in ferritin, a large hollow symmetrical protein which is able to sequester around 4500 atoms of iron (Harrison and Arosio, 1996; Koorts and Viljoen, 2007; Arosio et al., 2009). In addition to the choroid and RPE, within the neural retina the regions with highest levels of iron and ferritin are found in the inner segment of photoreceptors, inner nuclear layer and the ganglion layer (Yefimova et al., 2000; He et al., 2007).
Iron efflux is regulated through a transmembrane protein called ferroportin. It is also known as an iron-regulated transporter 1 or solute carrier family 40 member 1 which exports iron from cells in the form of ferrous (Fe2+) iron. Since ferrous iron must be oxidized to its ferric state to be regulated by systemic transferrin, ferroportin functions in conjunction with two extracellular multicopper ferroxidases, ceruloplasmin and hephaestin (Harris et al., 1999; Vulpe et al., 1999; Jeong and David, 2003; Ayton et al., 2013; McCarthy and Kosman, 2013). Ferroportin is found on most cells including retinal neurons and glia (Abboud and Haile, 2000; Donovan et al., 2000, 2005; Jeong and David, 2003; Hahn et al., 2004a). Ferroxidase enzymes including ceruloplasmin and hephaestin are also present in the retina, specifically in Müller glia and retinal pigment epithelial cells (Chen et al., 2003; Hahn et al., 2004b).
Another iron-regulatory protein which plays a crucial role in the maintenance of retinal iron homeostasis is hepcidin (Nicolas et al., 2001; Pigeon et al., 2001). Hepcidin is the main peptide hormone that regulates systemic iron. Hepcidin is primarily expressed by the liver and secreted into the bloodstream, and expression of hepcidin in retinal Müller cells, photoreceptor cells and RPE cells has been reported (Gnana-Prakasam et al., 2008; Hadziahmetovic et al., 2011a). Hepcidin regulates iron homeostasis by binding and antagonizing the only known mammalian iron exporter, ferroportin, leading to reduced cellular iron export thus limiting the amount of iron found in serum or extracellular fluid (Nemeth et al., 2004). Hepcidin also plays an important role in inhibiting the intestinal iron absorption (Ganz, 2005). Finally, hepcidin promotes sequestration of iron by macrophages which further reduce serum iron levels (Abreu et al., 2018).
Role of Iron in Retinal Physiology
Iron is one of the most abundant metals in the retina (Ugarte et al., 2012), critical for retinal function via its role as an integral component of key retinal enzymes (Lohmann, 1964; Yau and Baylor, 1989; Yefimova et al., 2000; Moiseyev et al., 2006; Chen et al., 2009). The characterization of retinal iron content through histochemical approaches showed a heterogeneous distribution, with iron largely found at the choroid, RPE and the photoreceptors layer (Yefimova et al., 2000; Song and Dunaief, 2013). Similarly, iron colocalization at the RPE, choroid and to a lesser degree at the neural retain was confirmed using laser ablation-inductively coupled plasma-mass spectrometry (LA-ICP-MS) which is a sensitive technique that offers a fast and precise spatially resolved measurement of elements in situ at trace and ultra-trace levels (Pamphlett et al., 2020).
In the context of visual function, iron serves as a cofactor for the RPE-specific 65 kDa protein (RPE65), an enzyme required for the retinoid metabolic pathway, which is critical for the maintenance of light capturing chromophore levels in photoreceptors and thus phototransduction and visual adaption (Redmond et al., 2005; Moiseyev et al., 2006). The isomerohydrolase activity of RPE65 relies on the presence of metal ions (see Figure 1B). Iron is central to this process, as evidenced by findings that mutations in RPE65 iron coordinating result in a range of retinal dystrophies including Leber congenital amaurosis and some forms of retinitis pigmentosa (Thompson et al., 2000; Simovich et al., 2001; Redmond et al., 2005; Bereta et al., 2008).
In addition, iron is an essential cofactor of fatty acid desaturases enzymes which play an important role in photoreceptor outer segment disc biogenesis (Figure 1C; Shichi, 1969; Song and Dunaief, 2013); whereby old photoreceptor discs containing phototransduction proteins are completely replaced by new ones over the course of about 10 days (Young, 1967; Young and Bok, 1969; Chuang et al., 2007). In addition to the above retina specific role for iron, like the CNS, the retina expresses several iron-dependent enzymes including tyrosine hydroxylase (Ramsey et al., 1996), phenylalanine hydroxylase (Gottschall et al., 1982), and tryptophan hydroxylase (Kuhn et al., 1980) that are involved in the biosynthesis and regulation of neurotransmitters such as dopamine, serotonin, and melatonin (Kaushik et al., 2007). Therefore it is not surprising that the retina expresses a wide array of enzymes that utilize iron as a cofactor, including those involved in energy production; mitochondrial ferredoxins, Redfearn and King (1964) cytochromes (Slater, 1949), and aconitase (Dickman and Cloutier, 1950).
Retinal Changes in Hemochromatosis
One way to consider the importance of iron to the retina and visual function is to examine what happens in those people who have an iron loading disorder. However, assessment of retinal changes in hemochromatosis patients remain limited. One of the earliest reports on the ocular manifestations of high levels of retinal iron loading in hemochromatosis patients was described by Maddox (1933). The author reported that there was normal visual acuity without overt retinal pathology in four cases (Maddox, 1933). Almost 40 years after Maddox, further reports in those with hemochromatosis showed iron accumulation in the peripapillary (around the optic nerve) retinal pigment epithelium, ciliary epithelium (where aqueous humor is produced), corneal epithelium, and sclera (Davies et al., 1972; Roth and Foos, 1972). Drusen-like deposits, which are the prominent clinical feature of age-related macular degeneration, were also detected in these patients (Roth and Foos, 1972). In a more recent study, Menghini et al. (2018) examined 49 patients (∼15 years after diagnosis, average age at examination 60 years) with hemochromatosis and examined the retina in vivo using spectral domain optical coherence tomography, as well as short wavelength autofluorescence and color fundus images. Their results showed no retinal changes such as drusen, RPE alterations, or increased lipofuscin in any of the images.
In contrast, other case studies that examine histopathology and retinal function via electroretinography have indicated the possibility of retinal changes with hemochromatosis. Retinal abnormalities have been reported in a 49-year-old hemochromatosis patient with homozygosity for the C282Y polymorphism in the HFE gene. The patient was characterized by progressive loss of visual function assessed by full – field electroretinography (ERG) and abnormal RPE changes using retinal imaging (Zerbib et al., 2015). Electroretinographic examination at the initial visit revealed a 50% reduction in the rod response and no change in the cone response. Follow-up examinations 6-month later suggested that in addition to a diminished rod response there was a progression of cone dysfunction, with a 50% reduction in the cone response (Zerbib et al., 2015).
Recently, another case of ocular involvement in hereditary hemochromatosis was reported in a 39-year-old patient with a homozygous C282Y mutation in HFE gene, without any other mutations associated with inherited retinal dystrophies. The patient reported bilateral progressive blurry vision and recent onset photopsia and headaches. Electroretinograms demonstrated generalized rod and cone dysfunction with some central preservation of waveforms. There appeared to be no retinopathy progression at 6 month follow-up, after the patient had undergone treatment to normalize his iron levels (Bellsmith et al., 2020).
There remain limited studies exploring the relationship between the systemic iron loading disorders and retinal changes. The heterogeneity in findings between the few case reports and Menghini et al.’s (2018) study could derive from the methodologies employed, for example, electroretinography can be a more sensitive measure of temporary retinal dysfunction than optical coherence tomography, which may only detect more significant structural changes associated with longer term retina injury (Ledolter et al., 2015).
Animal Models of Iron Disorders of the Retina
To gain further insight, preclinical studies have sought to examine in animal models the impact of systemic iron loading on retinal health. Broadly, three types of animal models have been developed including local administration of exogenous iron (e.g., intravitreal injection), oral delivery of iron (dietary iron supplementation), and genetically modified iron loading models.
It should be noted during the earliest stages of neonatal development when mammals nurse on their mother’s milk, the blood–brain barrier is open to iron accumulation (Dwork, 1995; Kaur et al., 2007; Billings et al., 2016). Subsequently the blood–brain barrier becomes fully formed in early life and only then iron is acquired selectively through iron receptors proteins that mediate iron intake.
One of the earliest animal models of local administration of exogenous iron was conducted by Declercq et al. (1977). They examined the consequences of excess iron on retinal function and histopathology in an animal model of siderosis. Ten days after intravitreal injection of a solid iron foreign body into the rabbit eye, they reported reductions in both a- (photoreceptor) and b-wave (ON bipolar cells) amplitudes in conjunction with degeneration of the outer nuclear layer and RPE (Declercq et al., 1977). Subsequently, Doly et al. (1984) showed that intravitreal injection of a solution containing Fe2+ ascorbate into the rat’s eyes selectively attenuated the b-wave in isolated retinal recordings (Doly et al., 1984). A similar study showed intravitreal injection of ferrous sulfate (FeSO4) into mouse’s eyes caused a reduction in the b-wave amplitude (Rogers et al., 2007). These data show that high levels of iron appear to reduce outer and middle retinal function.
The effects of high dietary iron were studied on 2-month-old mice by supplementing mice with 2% iron carbonyl for 3 or 10 months. Compared with a normal diet, dietary iron supplementation changed retinal mRNA levels of iron-responsive genes indicating a modest increase in iron in the RPE. However, even by 18 months of age there was little evidence of increased retinal iron and no retinal degeneration (Bhoiwala et al., 2015). The authors suggested that high levels of dietary iron can only modestly increase the level of iron deposition in the mouse RPE without causing RPE or retinal degeneration, which means the blood–retinal barrier is able to regulate iron levels (Bhoiwala et al., 2015).
The effects of acute systemic iron loading via intravenous injection were investigated by Song et al. (2016). Their study involved two cohorts of C57BL/6J male mice including a group of 2 months old mice administrated a weekly dose of 1.2 mg iron-sucrose for a total of 12 injections. These animals were examined at 12 months of age. The second cohort of mice at 10 weeks of age were subjected to two intravenous injections either with iron-sucrose or sucrose alone and euthanized 24 h after the last injection. Their results showed iron accumulated chiefly at the RPE and choroid in chronic exposure. Additionally, histological features similar to AMD such as Bruch’s membrane thickening, RPE hypertrophy and vacuolization were noted in these mice. The second acute loading group displayed increased levels of ferritin mRNA and reduction of transferrin receptor mRNA within the RPE (Song et al., 2016).
Consistent with susceptibility of the choroid, RPE and outer retina, Song et al. (2016) reported a clinical case of a 43-year-old anemic patient who developed numerous retinal drusen, the hallmark of AMD, within 11 months of intravenous iron therapy. The patient who had no prior ocular history had undergone infusion of 300 mg of iron-sucrose saline over 2 h three times a week. As the treatment progressed the patient noted delayed adaptation to low-light levels and difficulty reading at night. The patient’s DNA was tested and revealed a high genetic risk for AMD. They concluded that iron therapy may have the potential to induce or exacerbate a form of retinal degeneration that shares features with AMD (Song et al., 2016).
It should be noted that the iron regulatory hormone, hepcidin is expressed in the neurosensory retina and may limit iron influx into the inner retina which would be another mechanism to protect the inner retina against high levels of iron (Baumann et al., 2019). Therefore, Shu et al. (2019) designed a study in which retina-specific hepcidin knockout mice were exposed to high systemic iron levels through daily intraperitoneal injection of 10 mg iron dextran for 5 days each week. Their results showed that while they could identify accumulation of high levels of iron in the RPE and retinal vascular endothelial cells of hepcidin knockout mice, there was no change in iron status of neurosensory retina. They reported no alterations in the retina–blood barrier and no signs of retinal degeneration. They concluded that the retinal–blood barrier can protect neurosensory retina from high doses of exogenously administered iron independent of retinal hepcidin production (Shu et al., 2019).
All of the studies analyzing the effects of acute exogenous iron-loading on retina showing similar patterns of iron distribution with RPE and choroid being the main sites of iron accumulation. However, the pathological effects of iron on retina seemed to be varied amongst these studies. Thus further studies of defective retinal iron homeostasis using both functional and histological outcome measures in genetically modified animal models of chronic iron loading could potentially provide a more comprehensive understanding of iron-induced retinal pathology.
Retinal Abnormalities in Genetically – Modified Animal Models of Systemic Iron Loading
Genetically modified animal models of chronic iron loading have been developed to recapitulate human iron loading diseases. One of the earliest mouse models of systemic iron loading was developed by disruption of a single ferroxidase, either Cp or Heph. A study has shown that the Cp knock-out mice at 18 months old showed increased retinal iron levels and degeneration of the retina (Patel et al., 2002) in alignment with aceruloplasminemia patients who have mutations in Cp (Wolkow et al., 2011). In contrast, other animal studies which selectively delete either Cp or Heph did not manifest any retinal iron loading or related pathology even at 2 years of age (Hahn et al., 2004b), suggesting that one ferroxidase can compensate for the functional loss of the other (Jiang et al., 2016). However, simultaneous disruption of Cp and Heph in double knockout mice led to substantial retinal iron build-up (more than 2.5-fold) at 6-month of age compared to wild-type mice (Hahn et al., 2004b; Hadziahmetovic et al., 2008). Double knockout mice showed photoreceptor degeneration, sub-retinal neovascularization and RPE hypertrophy, hyperplasia by 9 months of age (Hahn et al., 2004b). Retinal degeneration in these mice was progressive, becoming more severe by 12–13 months of age (Hadziahmetovic et al., 2008).
Another mouse model of systemic iron loading was developed by Wolkow et al. (2012). Their murine model combined systemic ceruloplasmin deletion with RPE-specific hephaestin knockout resulted in iron accumulation in the RPE by 3 months of age, which was accompanied with a range of pathological features. In contrast, photoreceptor-specific deletion of hephaestin had no substantial effect on iron levels in the neural retina, even with concomitant systemic deletion of ceruloplasmin (Wolkow et al., 2012). Together, these results indicate that hephaestin has a cell-autonomous role in the RPE.
A further mouse model was generated by a single nucleotide (G to A) switch of the transferrin gene to produce hypotransferrinemic Hpx–/– mice (Trenor et al., 2000). Homozygous Hpx–/– mice have no transferrin and injection of human transferrin is required for survival, but even then, only a minority of mice survive up to 2 months of age (Lederman et al., 2012). Despite administration of exogenous human transferrin, the amount of transferrin in the retina of Hpx–/– mouse decreased to 61% of wild-type levels (Dickinson and Connor, 1995). Interestingly, the total iron content in the retina was not different between Hpx–/– and wild-type mice. Although gross retinal structure appeared to be normal in Hpx–/– mouse, assessment of retinal function showed attenuation of scotopic and photopic electroretinogram amplitudes compared to wild-type mice at 1 and 2 months of age (Lederman et al., 2012).
Finally, abnormal systemic iron loading has also been modeled by disruption of the bone morphogenetic protein 6 (Bmp6) gene, a key iron regulator gene that acts through hepcidin. In Bmp6 knockout mice (Bmp6–/–) high levels of iron are found in the neural retina of male Bmp6–/– mice (fourfold compared to wild-type male mice) (Hadziahmetovic et al., 2011c). Male Bmp6–/– mice showed severe retinal pathology by ∼10 months of age, including RPE hypertrophy and hyperplasia, loss of overlying photoreceptors and outer nuclear layer thinning. It is of interest that male Bmp6–/– mice had almost 20-fold more iron in their RPE/choroid compared to female Bmp6–/– mice. Female Bmp6–/– mice showed no evidence of increased retinal iron loading and normal retinal morphology. The sexual dimorphism of iron effects in Bmp6–/– mice was studied by castration and ovariectomy. Higher levels of liver hepcidin was found in castrated Bmp6–/– males relative to non-castrated Bmp6–/– mice, while there was no evidence of abnormal hepcidin expression in ovariectomized females. The authors argued that higher iron accumulation in Bmp6–/– males may have arisen through additional suppressive effects of testosterone on hepcidin synthesis (Latour et al., 2014). These studies highlight that along with age, gender can affect levels of retinal iron loading in the retina (Hahn et al., 2006).
Whilst providing important insight, the genetic mouse models of iron dyshomeostasis introduced thus far are not genetically analogous to human hemochromatosis. Thus, further studies of mouse models with disruption of genes that predispose to heredity hemochromatosis could offer more clinical relevance.
Retinal Abnormalities in Genetically – Modified Animal Models of Hemochromatosis
In addition to the above models, preclinical studies have sought to disrupt genes that predispose to heredity hemochromatosis in humans. The expression of hemochromatosis-related genes in mouse retina (Martin et al., 2006) makes it a useful animal model to address the possibility of iron-induced retinal injury.
Iacovelli et al. (2009) hypothesized that the disruption of ferroportin (Type 4 hemochromatosis) within the retina could lead to aberrant iron accumulation during both development and adulthood in mammals. They generated a polycythemia (high concentration of red blood cells) mouse (Pcm) model, and the results showed that up to 7 weeks of age there was no difference between Pcm and wild-type mice. However, at 12 months of age there were signs of retinal degeneration and morphological changes in aging Pcm mice. Unfortunately, retinal iron levels were not reported for Pcm mice at 1 year of age (Iacovelli et al., 2009).
The hepcidin knockout mouse (Hamp–/–) is another model of hemochromatosis (Type 2) that show age-dependent increases in retinal iron in the RPE/choroid and neural retina (Hadziahmetovic et al., 2011a). Retinal structure was normal at 3 months of age in Hamp–/– mice. Mild focal abnormalities became apparent by 9 months and by 18 months pathology was severe including RPE hyperplasia, accumulation of lipofuscin-like material in the RPE, loss of photoreceptor outer segments and subretinal neovascularization (Hadziahmetovic et al., 2011a). Histochemical analysis of retinal iron levels (Perls’ staining) showed that the RPE and non-pigmented ciliary epithelium are the primary sites of retinal iron accumulation in Hamp–/– mice older than 9-month. Hamp–/– mice also showed changes in retinal iron-related genes and proteins, including reduced Tfr1 mRNA levels, and increased retinal L-ferritin protein levels at 4 months of age (Hadziahmetovic et al., 2011a). It is noticeable that despite progressive retinal iron accumulation in Hamp–/– mice and previously described Cp and Heph double knockout mice, there is a down-regulation in transferrin-bound iron import proteins in the retina of these models. This contradiction was resolved by Sterling et al. (2017) showing upregulation of non-transferrin bound iron import proteins in these two mouse models of retinal iron accumulation.
Another mouse model of hemochromatosis (Type 2) is hemojuvelin knockout (Hjv–/–) mice. This animal model showed early systemic iron loading in particular in the liver, pancreas and heart by two and a half months of age (Niederkofler et al., 2005), with little evidence of retina changes at this age. Hjv–/– mice showed retinal degeneration at 18 months of age as assessed by counting cell bodies in retinal cross sections (Gnana-Prakasam et al., 2012).
Finally, a mouse model of hemochromatosis Type 1, which is one of the most prevalent mutations seen in human is the Hfe knockout mouse (Hfe–/–). This mouse model had normal retinas at 6 months of age. Assessment at 18 months of age revealed severe retinal abnormalities including loss of ganglion cells, uneven distribution of nuclei in the inner and outer nuclear layers, widespread hypertrophy of RPE cells and focal areas of RPE hyperplasia (Gnana-Prakasam et al., 2009a). In addition, Hfe–/– mice showed changes in iron – related proteins including increased levels of both H-ferritin and L-ferritin in photoreceptors, outer and inner plexiform layers and within the RPE, in addition to reduced Tfr1 mRNA levels (Gnana-Prakasam et al., 2009b).
Summary of Animal Studies on Iron and Retina
The pathologic findings in animal models shows that too much iron in the eye leads to dysfunction of photoreceptors and downstream consequences on the inner retina. Under normal conditions it seems that the regulatory system including the blood–retinal barrier protects the retina from systemic dietary iron loading. However, high levels of serum iron can eventually damage the RPE, which then reduces support to photoreceptors. Additionally, disruption to genes associated with iron–regulation leads to iron build-up, particularly the RPE and photoreceptors, resulting in progressive photoreceptor and downstream inner retinal degeneration. There is some evidence that rod photoreceptor dysfunction precedes cone photoreceptor changes with iron accumulation in the RPE. The amount of retinal injury and rate of progression associated with systemic iron loading appears to be varied depending on the specific regulatory protein involved, in addition to the age and sex of the mice (Hahn et al., 2009). While there is an increasing interest in incorporating electroretinography and in vivo imaging, as well as gene expression changes in retinal studies in animal models of iron loading (Liu et al., 2021), the number of such studies are still limited. More comprehensive time course studies, particularly using complementary tools such as electroretinography and in vivo imaging to define the earliest retinal deficits would help to define the role of iron regulation on retinal degeneration. Current animal studies indicate that the major driving factor in retinal degeneration may be iron overload as opposed to the genetic mutation itself having a direct effect, even though many hemochromatosis molecules have been found in the retina (Gnana-Prakasam et al., 2009a). This is because in the genetic modification models retinal changes only manifest at older ages, a stage when iron has had a chance to over-accumulate. Furthermore, treating the Cp-Heph (Hadziahmetovic et al., 2011b) and Hepc (Song et al., 2014) knock out mouse with an iron-chelator decreased retinal iron levels, oxidative stress and ameliorated retinal degeneration. Given different sub-types of hemochromatosis are due to alterations in a variety of genes further interventional studies are still warranted in other animal models.
Conclusion
Iron is known to play a critical role in the metabolic activities of the retina particularly the RPE and photoreceptors, but also the inner retina. Studies of ocular manifestations of systemic iron loading remain confined to case reports (Hudson, 1953; Davies et al., 1972; Roth and Foos, 1972; Zerbib et al., 2015; Bellsmith et al., 2020), with only one study on cohort of hemochromatosis patients (Menghini et al., 2018). Few studies have systematically assessed retinal function aside from visual acuity. Cumulative evidence from animal studies, showed that polymorphisms and mutations in iron-modulating genes are associated with progressive retinal iron accumulation and retinal injury.
The exact pathophysiology of retinal abnormalities in systemic iron loading-disorders is still unclear. Improved understanding of the relationship between retinal iron imbalance and retinal pathology is likely to help in the development of therapeutic strategies that can restore retinal iron homeostasis and mitigate neurotoxicity.
Author Contributions
AS wrote the first draft of the manuscript. CN, BB, and DF contributed to manuscript revision, read, and approved the submitted version. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that this study received funding from an Australian Research Council Linkage grant LP160100126 with funding partners AstraZeneca and Biogen Inc. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Funding
This research was supported by the Australian Research Council Linkage grant LP160100126 (CN and BB).
References
- Abboud S., Haile D. J. (2000). A novel mammalian iron-regulated protein involved in intracellular iron metabolism. J. Biol. Chem. 275 19906–19912. 10.1074/jbc.M000713200 [DOI] [PubMed] [Google Scholar]
- Abreu R., Quinn F., Giri P. K. (2018). Role of the hepcidin-ferroportin axis in pathogen-mediated intracellular iron sequestration in human phagocytic cells. Blood Adv. 2 1089–1100. 10.1182/bloodadvances.2017015255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams P. C. (2005). Screening for haemochromatosisproducing or preventing illness? Lancet 366 269–271. [DOI] [PubMed] [Google Scholar]
- Allen K. J. (2008). Population genetic screening for hereditary haemochromatosis: are we a step closer? Med. J. Aust. 189 300–301. 10.5694/j.1326-5377.2008.tb02043.x [DOI] [PubMed] [Google Scholar]
- Andrews N. C. (1999). Disorders of iron metabolism. N. Engl. J. Med. 341 1986–1995. [DOI] [PubMed] [Google Scholar]
- Andrews N. C. (2008). Forging a field: the golden age of iron biology. Blood 112 219–230. 10.1182/blood-2007-12-077388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arosio P., Ingrassia R., Cavadini P. (2009). Ferritins: a family of molecules for iron storage, antioxidation and more. Biochim. Biophys. Acta 1790 589–599. 10.1016/j.bbagen.2008.09.004 [DOI] [PubMed] [Google Scholar]
- Ayton S., Lei P., Duce J. A., Wong B. X., Sedjahtera A., Adlard P. A., et al. (2013). Ceruloplasmin dysfunction and therapeutic potential for Parkinson disease. Ann. Neurol. 73 554–559. 10.1002/ana.23817 [DOI] [PubMed] [Google Scholar]
- Babitt J. L., Huang F. W., Wrighting D. M., Xia Y., Sidis Y., Samad T. A., et al. (2006). Bone morphogenetic protein signaling by hemojuvelin regulates hepcidin expression. Nat. Genet. 38 531–539. 10.1038/ng1777 [DOI] [PubMed] [Google Scholar]
- Barot M., Gokulgandhi M. R., Mitra A. K. (2011). Mitochondrial dysfunction in retinal diseases. Curr. Eye. Res. 36 1069–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia A. M., Chirillo R., Aversa I., Sacco A., Costanzo F., Biamonte F. (2020). Ferroptosis and cancer: mitochondria meet the “iron maiden” cell death. Cells 9:1505. 10.3390/cells9061505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann B. H., Shu W., Song Y., Sterling J., Kozmik Z., Lakhal-Littleton S., et al. (2019). Liver-specific, but not retina-specific, hepcidin knockout causes retinal iron accumulation and degeneration. Am. J. Pathol. 189 1814–1830. 10.1016/j.ajpath.2019.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellsmith K. N., Dunaief J. L., Yang P., Pennesi M. E., Davis E., Hofkamp H., et al. (2020). Bull’s eye maculopathy associated with hereditary hemochromatosis. Am. J. Ophthalmol. Case Rep. 18:100674. 10.1016/j.ajoc.2020.100674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bereta G., Kiser P. D., Golczak M., Sun W., Heon E., Saperstein D. A., et al. (2008). Impact of retinal disease-associated RPE65 mutations on retinoid isomerization. Biochemistry 47 9856–9865. 10.1021/bi800905v [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutler E., Felitti V. J., Koziol J. A., Ho N. J., Gelbart T. (2002). Penetrance of 845G–> A (C282Y) HFE hereditary haemochromatosis mutation in the USA. Lancet 359 211–218. 10.1016/S0140-6736(02)07447-0 [DOI] [PubMed] [Google Scholar]
- Beutler E., Gelbart T., West C., Lee P., Adams M., Blackstone R., et al. (1996). Mutation analysis in hereditary hemochromatosis. Blood Cells Mol. Dis. 22 187-194; discussion 194a-194b. [DOI] [PubMed] [Google Scholar]
- Bhoiwala D. L., Song Y., Cwanger A., Clark E., Zhao L. L., Wang C., et al. (2015). CD1 mouse retina is shielded from iron overload caused by a high iron diet. Invest. Ophthalmol. Vis. Sci. 56 5344–5352. 10.1167/iovs.15-17026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesemeier A., Yoeruek E., Eibl O., Schraermeyer U. (2015). Iron accumulation in Bruch’s membrane and melanosomes of donor eyes with age-related macular degeneration. Exp. Eye Res. 137 39–49. 10.1016/j.exer.2015.05.019 [DOI] [PubMed] [Google Scholar]
- Billings J. L., Hare D. J., Nurjono M., Volitakis I., Cherny R. A., Bush A. I., et al. (2016). Effects of neonatal iron feeding and chronic clioquinol administration on the parkinsonian human A53T transgenic mouse. ACS Chem. Neurosci. 7 360–366. 10.1021/acschemneuro.5b00305 [DOI] [PubMed] [Google Scholar]
- Bjorn-Rasmussen E., Hallberg L., Isaksson B., Arvidsson B. (1974). Food iron absorption in man. applications of the two-pool extrinsic tag method to measure heme and nonheme iron absorption from the whole diet. J. Clin. Invest. 53 247–255. 10.1172/JCI107545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brissot P., de Bels F. (2006). Current approaches to the management of hemochromatosis. Hematol. Am. Soc. Hematol. Educ. Prog. 2006 36–41. 10.1182/asheducation-2006.1.36 [DOI] [PubMed] [Google Scholar]
- Brissot P., Troadec M. B., Loréal O., Brissot E. (2019). Pathophysiology and classification of iron overload diseases; update 2018. Transfus Clin. Biol. 26 80–88. 10.1016/j.tracli.2018.08.006 [DOI] [PubMed] [Google Scholar]
- Callebaut I., Joubrel R., Pissard S., Kannengiesser C., Gerolami V., Ged C., et al. (2014). Comprehensive functional annotation of 18 missense mutations found in suspected hemochromatosis type 4 patients. Hum. Mol. Genet. 23 4479–4490. 10.1093/hmg/ddu160 [DOI] [PubMed] [Google Scholar]
- Camaschella C., Roetto A., Cali A., De Gobbi M., Garozzo G., Carella M., et al. (2000). The gene TFR2 is mutated in a new type of haemochromatosis mapping to 7q22. Nat. Genet. 25 14–15. 10.1038/75534 [DOI] [PubMed] [Google Scholar]
- Casey J. L., Hentze M. W., Koeller D. M., Caughman S. W., Rouault T. A., Klausner R. D., et al. (1988). Iron-responsive elements: regulatory RNA sequences that control mRNA levels and translation. Science 240 924–928. 10.1126/science.2452485 [DOI] [PubMed] [Google Scholar]
- Chen H., Lukas T. J., Du N., Suyeoka G., Neufeld A. H. (2009). Dysfunction of the retinal pigment epithelium with age: increased iron decreases phagocytosis and lysosomal activity. Invest Ophthalmol. Vis. Sci. 50 1895–1902. 10.1167/iovs.08-2850 [DOI] [PubMed] [Google Scholar]
- Chen L., Dentchev T., Wong R., Hahn P., Wen R., Bennett J., et al. (2003). Increased expression of ceruloplasmin in the retina following photic injury. Mol. Vis. 9 151–158. [PubMed] [Google Scholar]
- Chua A. C., Graham R. M., Trinder D., Olynyk J. K. (2007). The regulation of cellular iron metabolism. Crit. Rev. Clin. Lab Sci. 44 413–459. [DOI] [PubMed] [Google Scholar]
- Chuang J. Z., Zhao Y., Sung C. H. (2007). SARA-regulated vesicular targeting underlies formation of the light-sensing organelle in mammalian rods. Cell 130 535–547. 10.1016/j.cell.2007.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffman L. G., Parsonage D., D’agostino R., Jr., Torti F. M., Torti S. V. (2009). Regulatory effects of ferritin on angiogenesis. Proc. Natl. Acad. Sci. U.S.A. 106 570–575. 10.1073/pnas.0812010106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Čolak E., Žorić L., Radosavljević A., Ignjatović S. (2018). The association of serum iron-binding proteins and the antioxidant parameter levels in age-related macular degeneration. Curr. Eye Res. 43 659–665. 10.1080/02713683.2018.1437452 [DOI] [PubMed] [Google Scholar]
- Country M. W. (2017). Retinal metabolism: a comparative look at energetics in the retina. Brain Res. 1672 50–57. 10.1016/j.brainres.2017.07.025 [DOI] [PubMed] [Google Scholar]
- Crichton R. R., Dexter D. T., Ward R. J. (2011). Brain iron metabolism and its perturbation in neurological diseases. J. Neural. Transm (Vienna) 118 301–314. 10.1007/s00702-010-0470-z [DOI] [PubMed] [Google Scholar]
- Cullen L. M., Gao X., Easteal S., Jazwinska E. C. (1998). The hemochromatosis 845 G–>A and 187 C–>G mutations: prevalence in non-caucasian populations. Am. J. Hum. Genet. 62 1403–1407. 10.1086/301878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham M. J., Macklin E. A., Neufeld E. J., Cohen A. R. (2004). Complications of β-thalassemia major in north America. Blood 104 34–39. 10.1182/blood-2003-09-3167 [DOI] [PubMed] [Google Scholar]
- D’Mello S. R., Kindy M. C. (2020). Overdosing on iron: elevated iron and degenerative brain disorders. Exp. Biol. Med. 245 1444–1473. 10.1177/1535370220953065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daglas M., Adlard P. A. (2018). The involvement of iron in traumatic brain injury and neurodegenerative disease. Front. Neurosci. 12:981. 10.3389/fnins.2018.00981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies G., Dymock I., Harry J., Williams R. (1972). Deposition of melanin and iron in ocular structures in haemochromatosis. Br. J. Ophthalmol. 56 338–342. 10.1136/bjo.56.4.338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Declercq S. S., Meredith P. C., Rosenthal A. R. (1977). Experimental siderosis in the rabbit: correlation between electroretinography and histopathology. Arch. Ophthalmol. 95 1051–1058. 10.1001/archopht.1977.04450060138014 [DOI] [PubMed] [Google Scholar]
- Dekker M. C., Giesbergen P. C., Njajou O. T., Van Swieten J. C., Hofman A., Breteler M. M., et al. (2003). Mutations in the hemochromatosis gene (HFE). Parkinson’s Dis. Parkinsonism. Neurosci. Lett. 348 117–119. 10.1016/s0304-3940(03)00713-4 [DOI] [PubMed] [Google Scholar]
- Del-Castillo-Rueda A., Moreno-Carralero M. I., Cuadrado-Grande N., Alvarez-Sala-Walther L. A., Enriquez-De-Salamanca R., Mendez M., et al. (2012). Mutations in the HFE, TFR2, and SLC40A1 genes in patients with hemochromatosis. Gene 508 15–20. 10.1016/j.gene.2012.07.069 [DOI] [PubMed] [Google Scholar]
- Desmond M. A., Sobiecki J. G., Jaworski M., Płudowski P., Antoniewicz J., Shirley M. K., et al. (2021). Growth, body composition, and cardiovascular and nutritional risk of 5- to 10-y-old children consuming vegetarian, vegan, or omnivore diets. Am. J. Clin. Nutr. 113 1565–1577. 10.1093/ajcn/nqaa445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Détivaud L., Island M. L., Jouanolle A. M., Ropert M., Bardou-Jacquet E., Le Lan C., et al. (2013). Ferroportin diseases: functional studies, a link between genetic and clinical phenotype. Hum. Mutat. 34 1529–1536. 10.1002/humu.22396 [DOI] [PubMed] [Google Scholar]
- Dickinson T. K., Connor J. R. (1995). Cellular distribution of iron, transferrin, and ferritin in the hypotransferrinemic (Hp) mouse brain. J. Comput. Neurol. 355 67–80. 10.1002/cne.903550109 [DOI] [PubMed] [Google Scholar]
- Dickman S. R., Cloutier A. A. (1950). Activation and stabilization of aconitase by ferrous ions. Arch. Biochem. 25 229–231. [PubMed] [Google Scholar]
- Dixon S. J., Lemberg K. M., Lamprecht M. R., Skouta R., Zaitsev E. M., Gleason C. E., et al. (2012). Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149 1060–1072. 10.1016/j.cell.2012.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doly M., Braquet P., Bonhomme B., Meyniel G. (1984). Effects of lipid peroxidation on the isolated rat retina. Ophthalmic. Res. 16 292–296. 10.1159/000265332 [DOI] [PubMed] [Google Scholar]
- Donovan A., Brownlie A., Zhou Y., Shepard J., Pratt S. J., Moynihan J., et al. (2000). Positional cloning of zebrafish ferroportin1 identifies a conserved vertebrate iron exporter. Nature 403 776–781. 10.1038/35001596 [DOI] [PubMed] [Google Scholar]
- Donovan A., Lima C. A., Pinkus J. L., Pinkus G. S., Zon L. I., Robine S., et al. (2005). The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab 1 191–200. 10.1016/j.cmet.2005.01.003 [DOI] [PubMed] [Google Scholar]
- Dunaief J. L. (2006). Iron induced oxidative damage as a potential factor in age-related macular degeneration: the cogan lecture. Invest. Ophthalmol. Vis. Sci. 47 4660–4664. 10.1167/iovs.06-0568 [DOI] [PubMed] [Google Scholar]
- Dwork A. J. (1995). Effects of diet and development upon the uptake and distribution of cerebral iron. J. Neurol. Sci. 134 45–51. 10.1016/0022-510x(95)00207-i [DOI] [PubMed] [Google Scholar]
- Feder J. N., Gnirke A., Thomas W., Tsuchihashi Z., Ruddy D. A., Basava A., et al. (1996). A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat. Genet. 13 399–408. 10.1038/ng0896-399 [DOI] [PubMed] [Google Scholar]
- Fix O. K., Kowdley K. V. (2008). Hereditary hemochromatosis. Minerva Med. 99 605–617. [PubMed] [Google Scholar]
- Fuqua B. K., Vulpe C. D., Anderson G. J. (2012). Intestinal iron absorption. J. Trace Elem Med. Biol. 26 115–119. [DOI] [PubMed] [Google Scholar]
- Ganz T. (2005). Hepcidina regulator of intestinal iron absorption and iron recycling by macrophages. Best Pract. Res. Clin. Haematol. 18 171–182. 10.1016/j.beha.2004.08.020 [DOI] [PubMed] [Google Scholar]
- Gao X., Campian J. L., Qian M., Sun X. F., Eaton J. W. (2009). Mitochondrial DNA damage in iron overload. J. Biol. Chem. 284 4767–4775. 10.1074/jbc.M806235200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnana-Prakasam J. P., Martin P. M., Mysona B. A., Roon P., Smith S. B., Ganapathy V. (2008). Hepcidin expression in mouse retina and its regulation via lipopolysaccharide/toll-like receptor-4 pathway independent of Hfe. Biochem. J. 411 79–88. 10.1042/BJ20071377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnana-Prakasam J. P., Tawfik A., Romej M., Ananth S., Martin P. M., Smith S. B., et al. (2012). Iron-mediated retinal degeneration in haemojuvelin-knockout mice. Biochem. J. 441 599–608. 10.1042/BJ20111148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnana-Prakasam J. P., Thangaraju M., Liu K., Ha Y., Martin P. M., Smith S. B., et al. (2009a). Absence of iron-regulatory protein Hfe results in hyperproliferation of retinal pigment epithelium: role of cystine/glutamate exchanger. Biochem. J. 424 243–252. 10.1042/BJ20090424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnana-Prakasam J. P., Zhang M., Martin P. M., Atherton S. S., Smith S. B., Ganapathy V. (2009b). Expression of the iron-regulatory protein haemojuvelin in retina and its regulation during cytomegalovirus infection. Biochem. J. 419 533–543. 10.1042/BJ20082240 [DOI] [PubMed] [Google Scholar]
- Gochee P. A., Powell L. W., Cullen D. J., Du Sart D., Rossi E., Olynyk J. K. (2002). A population-based study of the biochemical and clinical expression of the H63D hemochromatosis mutation. Gastroenterology 122 646–651. 10.1016/s0016-5085(02)80116-0 [DOI] [PubMed] [Google Scholar]
- Goswami T., Andrews N. C. (2006). Hereditary hemochromatosis protein, HFE, interaction with transferrin receptor 2 suggests a molecular mechanism for mammalian iron sensing. J. Biol. Chem. 281 28494–28498. 10.1074/jbc.C600197200 [DOI] [PubMed] [Google Scholar]
- Gottschall D. W., Dietrich R. F., Benkovic S. J., Shiman R. (1982). Phenylalanine hydroxylase. correlation of the iron content with activity and the preparation and reconstitution of the apoenzyme. J. Biol. Chem. 257 845–849. [PubMed] [Google Scholar]
- Guerreiro R. J., Bras J. M., Santana I., Januario C., Santiago B., Morgadinho A. S., et al. (2006). Association of HFE common mutations with Parkinson’s disease, Alzheimer’s disease and mild cognitive impairment in a portuguese cohort. BMC Neurol. 6:24. 10.1186/1471-2377-6-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guiney S. J., Adlard P. A., Bush A. I., Finkelstein D. I., Ayton S. (2017). Ferroptosis and cell death mechanisms in Parkinson’s disease. Neurochem. Int. 104 34–48. 10.1016/j.neuint.2017.01.004 [DOI] [PubMed] [Google Scholar]
- Gunshin H., Mackenzie B., Berger U. V., Gunshin Y., Romero M. F., Boron W. F., et al. (1997). Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature 388 482–488. 10.1038/41343 [DOI] [PubMed] [Google Scholar]
- Hadziahmetovic M., Dentchev T., Song Y., Haddad N., He X., Hahn P., et al. (2008). Ceruloplasmin/hephaestin knockout mice model morphologic and molecular features of AMD. Invest. Ophthalmol. Vis. Sci. 49 2728–2736. 10.1167/iovs.07-1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadziahmetovic M., Song Y., Ponnuru P., Iacovelli J., Hunter A., Haddad N., et al. (2011a). Age-dependent retinal iron accumulation and degeneration in hepcidin knockout mice. Invest. Ophthalmol. Vis. Sci. 52 109–118. 10.1167/iovs.10-6113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadziahmetovic M., Song Y., Wolkow N., Iacovelli J., Grieco S., Lee J., et al. (2011b). The oral iron chelator deferiprone protects against iron overload-induced retinal degeneration. Invest. Ophthalmol. Vis. Sci. 52 959–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadziahmetovic M., Song Y., Wolkow N., Iacovelli J., Kautz L., Roth M. P., et al. (2011c). Bmp6 regulates retinal iron homeostasis and has altered expression in age-related macular degeneration. Am. J. Pathol. 179 335–348. 10.1016/j.ajpath.2011.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn P., Dentchev T., Qian Y., Rouault T., Harris Z. L., Dunaief J. L. (2004a). Immunolocalization and regulation of iron handling proteins ferritin and ferroportin in the retina. Mol. Vis. 10 598–607. [PubMed] [Google Scholar]
- Hahn P., Qian Y., Dentchev T., Chen L., Beard J., Harris Z. L., et al. (2004b). Disruption of ceruloplasmin and hephaestin in mice causes retinal iron overload and retinal degeneration with features of age-related macular degeneration. Proc. Natl. Acad. Sci. U.S.A. 101 13850–13855. 10.1073/pnas.0405146101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn P., Song Y., Ying G. S., He X., Beard J., Dunaief J. L. (2009). Age-dependent and gender-specific changes in mouse tissue iron by strain. Experimental gerontology 44 594–600. 10.1016/j.exger.2009.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn P., Ying G. S., Beard J., Dunaief J. L. (2006). Iron levels in human retina: sex difference and increase with age. Neuroreport 17 1803–1806. [DOI] [PubMed] [Google Scholar]
- Haider L. M., Schwingshackl L., Hoffmann G., Ekmekcioglu C. (2018). The effect of vegetarian diets on iron status in adults: a systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 58 1359–1374. 10.1080/10408398.2016.1259210 [DOI] [PubMed] [Google Scholar]
- Hare D. J., Arora M., Jenkins N. L., Finkelstein D. I., Doble P. A., Bush A. I. (2015). Is early-life iron exposure critical in neurodegeneration? Nat. Rev. Neurol. 11 536–544. 10.1038/nrneurol.2015.100 [DOI] [PubMed] [Google Scholar]
- Hare D. J., Cardoso B. R., Raven E. P., Double K. L., Finkelstein D. I., Szymlek-Gay E. A., et al. (2017). Excessive early-life dietary exposure: a potential source of elevated brain iron and a risk factor for Parkinson’s disease. NPJ Parkinson’s Dis. 3:1. 10.1038/s41531-016-0004-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmatz P., Butensky E., Quirolo K., Williams R., Ferrell L., Moyer T., et al. (2000). Severity of iron overload in patients with sickle cell disease receiving chronic red blood cell transfusion therapy. Blood 96 76–79. [PubMed] [Google Scholar]
- Harris Z. L., Durley A. P., Man T. K., Gitlin J. D. (1999). Targeted gene disruption reveals an essential role for ceruloplasmin in cellular iron efflux. Proc. Natl. Acad. Sci. U.S.A. 96 10812–10817. 10.1073/pnas.96.19.10812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison P. M., Arosio P. (1996). The ferritins: molecular properties, iron storage function and cellular regulation. Biochim. Biophys. Acta 1275 161–203. 10.1016/0005-2728(96)00022-9 [DOI] [PubMed] [Google Scholar]
- He X., Hahn P., Iacovelli J., Wong R., King C., Bhisitkul R., et al. (2007). Iron homeostasis and toxicity in retinal degeneration. Prog. Retin Eye Res. 26 649–673. 10.1016/j.preteyeres.2007.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson J. R. (1953). Ocular findings in haemochromatosis. Br. J. Ophthalmol. 37 242–246. 10.1136/bjo.37.4.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacovelli J., Mlodnicka A. E., Veldman P., Ying G. S., Dunaief J. L., Schumacher A. (2009). Brain and retinal ferroportin 1 dysregulation in polycythaemia mice. Brain Res. 1289 85–95. 10.1016/j.brainres.2009.06.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingrassia R., Garavaglia B., Memo M. (2019). DMT1 expression and iron levels at the crossroads between aging and neurodegeneration. Front. Neurosci. 13:575. 10.3389/fnins.2019.00575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett S. G., Lin H., Godley B. F., Boulton M. E. (2008). Mitochondrial DNA damage and its potential role in retinal degeneration. Prog. Retin Eye Res. 27 596–607. 10.1016/j.preteyeres.2008.09.001 [DOI] [PubMed] [Google Scholar]
- Jeong S. Y., David S. (2003). Glycosylphosphatidylinositol-anchored ceruloplasmin is required for iron efflux from cells in the central nervous system. J. Biol. Chem. 278 27144–27148. 10.1074/jbc.M301988200 [DOI] [PubMed] [Google Scholar]
- Jiang B., Liu G., Zheng J., Chen M., Maimaitiming Z., Chen M., et al. (2016). Hephaestin and ceruloplasmin facilitate iron metabolism in the mouse kidney. Sci. Rep. 6:39470. 10.1038/srep39470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jouanolle A. M., Fergelot P., Gandon G., Yaouanq J., Le Gall J. Y., David V. (1997). A candidate gene for hemochromatosis: frequency of the C282Y and H63D mutations. Hum. Genet. 100 544–547. 10.1007/s004390050549 [DOI] [PubMed] [Google Scholar]
- Jouihan H. A., Cobine P. A., Cooksey R. C., Hoagland E. A., Boudina S., Abel E. D., et al. (2008). Iron-mediated inhibition of mitochondrial manganese uptake mediates mitochondrial dysfunction in a mouse model of hemochromatosis. Mol. Med. 14 98–108. 10.2119/2007-00114.Jouihan [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur D., Peng J., Chinta S. J., Rajagopalan S., Di Monte D. A., Cherny R. A., et al. (2007). Increased murine neonatal iron intake results in Parkinson-like neurodegeneration with age. Neurobiol. Aging 28 907–913. 10.1016/j.neurobiolaging.2006.04.003 [DOI] [PubMed] [Google Scholar]
- Kaushik P., Gorin F., Vali S. (2007). Dynamics of tyrosine hydroxylase mediated regulation of dopamine synthesis. J. Comput. Neurosci. 22 147–160. 10.1007/s10827-006-0004-8 [DOI] [PubMed] [Google Scholar]
- Kawabata H., Yang R., Hirama T., Vuong P. T., Kawano S., Gombart A. F., et al. (1999). Molecular cloning of transferrin receptor 2. a new member of the transferrin receptor-like family. J. Biol. Chem. 274 20826–20832. 10.1074/jbc.274.30.20826 [DOI] [PubMed] [Google Scholar]
- Kohgo Y., Ikuta K., Ohtake T., Torimoto Y., Kato J. (2008). Body iron metabolism and pathophysiology of iron overload. Int. J. Hematol. 88 7–15. 10.1007/s12185-008-0120-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koorts A. M., Viljoen M. (2007). Ferritin and ferritin isoforms I: Structure-function relationships, synthesis, degradation and secretion. Arch Physiol. Biochem. 113 30–54. 10.1080/13813450701318583 [DOI] [PubMed] [Google Scholar]
- Kuhn D. M., Ruskin B., Lovenberg W. (1980). Tryptophan hydroxylase. the role of oxygen, iron, and sulfhydryl groups as determinants of stability and catalytic activity. J. Biol. Chem. 255 4137–4143. [PubMed] [Google Scholar]
- Lane D. J. R., Ayton S., Bush A. I. (2018). Iron and Alzheimer’s disease: an update on emerging mechanisms. J. Alzheimer’s Dis. 64 S379–S395. 10.3233/JAD-179944 [DOI] [PubMed] [Google Scholar]
- Latour C., Kautz L., Besson-Fournier C., Island M. L., Canonne-Hergaux F., Loreal O., et al. (2014). Testosterone perturbs systemic iron balance through activation of epidermal growth factor receptor signaling in the liver and repression of hepcidin. Hepatology 59 683–694. 10.1002/hep.26648 [DOI] [PubMed] [Google Scholar]
- Lederman M., Obolensky A., Grunin M., Banin E., Chowers I. (2012). Retinal function and structure in the hypotransferrinemic mouse. Invest. Ophthalmol. Vis. Sci. 53 605–612. 10.1167/iovs.11-7436 [DOI] [PubMed] [Google Scholar]
- Ledolter A. A., Monhart M., Schoetzau A., Todorova M. G., Palmowski-Wolfe A. M. (2015). Structural and functional changes in glaucoma: comparing the two-flash multifocal electroretinogram to optical coherence tomography and visual fields. Doc. Ophthalmol. 130 197–209. 10.1007/s10633-015-9482-1 [DOI] [PubMed] [Google Scholar]
- Lee J. H., Jang H., Cho E. J., Youn H. D. (2009). Ferritin binds and activates p53 under oxidative stress. Biochem. Biophys. Res. Commun. 389 399–404. 10.1016/j.bbrc.2009.08.125 [DOI] [PubMed] [Google Scholar]
- Li N., Wang W., Zhou H., Wu Q., Duan M., Liu C., et al. (2020). Ferritinophagy-mediated ferroptosis is involved in sepsis-induced cardiac injury. Free Radic Biol. Med. 160 303–318. 10.1016/j.freeradbiomed.2020.08.009 [DOI] [PubMed] [Google Scholar]
- Lin H., Xu H., Liang F. Q., Liang H., Gupta P., Havey A. N., et al. (2011). Mitochondrial DNA damage and repair in RPE associated with aging and age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 52 3521–3529. 10.1167/iovs.10-6163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Bell B. A., Song Y., Kim H. J., Sterling J. K., Kim B. J., et al. (2021). Intraocular iron injection induces oxidative stress followed by elements of geographic atrophy and sympathetic ophthalmia. Aging Cell 20:e13490. 10.1111/acel.13490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd R. V., Hanna P. M., Mason R. P. (1997). The origin of the hydroxyl radical oxygen in the fenton reaction. Free Radic Biol. Med. 22 885–888. 10.1016/s0891-5849(96)00432-7 [DOI] [PubMed] [Google Scholar]
- Lohmann W. (1964). The importance of sulfur and iron in the retina as determined by paramagnetic resonance studies. Experientia 20 399–401. 10.1007/BF02147991 [DOI] [PubMed] [Google Scholar]
- Lozoff B., De Andraca I., Castillo M., Smith J. B., Walter T., Pino P. (2003). Behavioral and developmental effects of preventing iron-deficiency anemia in healthy full-term infants. Pediatrics 112 846–854. 10.1542/peds.112.4.846 [DOI] [PubMed] [Google Scholar]
- Maddox K. (1933). The retina in haemochromatosis. Br. J. Ophthalmol. 17 392–394. 10.1136/bjo.17.7.392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin P. M., Gnana-Prakasam J. P., Roon P., Smith R. G., Smith S. B., Ganapathy V. (2006). Expression and polarized localization of the hemochromatosis gene product HFE in retinal pigment epithelium. Invest. Ophthalmol. Vis. Sci. 47 4238–4244. 10.1167/iovs.06-0026 [DOI] [PubMed] [Google Scholar]
- Masaldan S., Bush A. I., Devos D., Rolland A. S., Moreau C. (2019). Striking while the iron is hot: iron metabolism and ferroptosis in neurodegeneration. Free Radic Biol. Med. 133 221–233. 10.1016/j.freeradbiomed.2018.09.033 [DOI] [PubMed] [Google Scholar]
- McCarthy R. C., Kosman D. J. (2013). Ferroportin and exocytoplasmic ferroxidase activity are required for brain microvascular endothelial cell iron efflux. J. Biol. Chem. 288 17932–17940. 10.1074/jbc.M113.455428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menghini M., Prünte C., Krayenbuehl P. A., Nowak A. (2018). Assessment of drusen and other retinal degenerative changes in patients with hereditary hemochromatosis. Retina 38 594–599. 10.1097/IAE.0000000000001577 [DOI] [PubMed] [Google Scholar]
- Merryweather-Clarke A. T., Pointon J. J., Shearman J. D., Robson K. J. (1997). Global prevalence of putative haemochromatosis mutations. J. Med. Genet. 34 275–278. 10.1136/jmg.34.4.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meynard D., Babitt J. L., Lin H. Y. (2014). The liver: conductor of systemic iron balance. Blood 123 168–176. 10.1182/blood-2013-06-427757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miret S., Simpson R. J., Mckie A. T. (2003). Physiology and molecular biology of dietary iron absorption. Annu Rev. Nutr. 23 283–301. 10.1146/annurev.nutr.23.011702.073139 [DOI] [PubMed] [Google Scholar]
- Moiseyev G., Takahashi Y., Chen Y., Gentleman S., Redmond T. M., Crouch R. K., et al. (2006). RPE65 is an iron(II)-dependent isomerohydrolase in the retinoid visual cycle. J. Biol. Chem. 281 2835–2840. 10.1074/jbc.M508903200 [DOI] [PubMed] [Google Scholar]
- Montosi G., Donovan A., Totaro A., Garuti C., Pignatti E., Cassanelli S., et al. (2001). Autosomal-dominant hemochromatosis is associated with a mutation in the ferroportin (SLC11A3) gene. J. Clin. Invest. 108 619–623. 10.1172/JCI13468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau C., Duce J. A., Rascol O., Devedjian J. C., Berg D., Dexter D., et al. (2018). Iron as a therapeutic target for Parkinson’s disease. Mov. Disord 33 568–574. 10.1002/mds.27275 [DOI] [PubMed] [Google Scholar]
- Mura C., Raguenes O., Férec C. (1999). HFE mutations analysis in 711 hemochromatosis probands: evidence for S65C implication in mild form of hemochromatosis. Blood 93 2502–2505. [PubMed] [Google Scholar]
- Nemeth E., Tuttle M. S., Powelson J., Vaughn M. B., Donovan A., Ward D. M., et al. (2004). Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306 2090–2093. 10.1126/science.1104742 [DOI] [PubMed] [Google Scholar]
- Nicolas G., Bennoun M., Devaux I., Beaumont C., Grandchamp B., Kahn A., et al. (2001). Lack of hepcidin gene expression and severe tissue iron overload in upstream stimulatory factor 2 (USF2) knockout mice. Proc. Natl. Acad. Sci. U.S.A. 98 8780–8785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederkofler V., Salie R., Arber S. (2005). Hemojuvelin is essential for dietary iron sensing, and its mutation leads to severe iron overload. J. Clin. Invest. 115 2180–2186. 10.1172/JCI25683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olynyk J. K., Trinder D., Ramm G. A., Britton R. S., Bacon B. R. (2008). Hereditary hemochromatosis in the post-HFE era. Hepatology 48 991–1001. 10.1002/hep.22507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pamphlett R., Cherepanoff S., Too L. K., Kum Jew S., Doble P. A., Bishop D. P. (2020). The distribution of toxic metals in the human retina and optic nerve head: implications for age-related macular degeneration. PLoS One 15:e0241054. 10.1371/journal.pone.0241054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papanikolaou G., Samuels M. E., Ludwig E. H., Macdonald M. L., Franchini P. L., Dube M. P., et al. (2004). Mutations in HFE2 cause iron overload in chromosome 1q-linked juvenile hemochromatosis. Nat. Genet. 36 77–82. 10.1038/ng1274 [DOI] [PubMed] [Google Scholar]
- Patel B. N., Dunn R. J., Jeong S. Y., Zhu Q., Julien J. P., David S. (2002). Ceruloplasmin regulates iron levels in the CNS and prevents free radical injury. J. Neurosci. 22 6578–6586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrangelo A. (2003). Haemochromatosis. Gut 52(Suppl. 2) ii23–ii30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrangelo A. (2004). Hereditary hemochromatosis—a new look at an old disease. N. Engl. J. Med. 350 2383–2397. 10.1056/NEJMra031573 [DOI] [PubMed] [Google Scholar]
- Pietrangelo A., Caleffi A., Henrion J., Ferrara F., Corradini E., Kulaksiz H., et al. (2005). Juvenile hemochromatosis associated with pathogenic mutations of adult hemochromatosis genes. Gastroenterology 128 470–479. 10.1053/j.gastro.2004.11.057 [DOI] [PubMed] [Google Scholar]
- Pigeon C., Ilyin G., Courselaud B., Leroyer P., Turlin B., Brissot P., et al. (2001). A new mouse liver-specific gene, encoding a protein homologous to human antimicrobial peptide hepcidin, is overexpressed during iron overload. J. Biol. Chem. 276 7811–7819. 10.1074/jbc.M008923200 [DOI] [PubMed] [Google Scholar]
- Piperno A., Pelucchi S., Mariani R. (2020). Inherited iron overload disorders. Trans. Gastroenterol. Hepatol. 5:25. 10.3324/haematol.2018.189845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell L. W., Seckington R. C., Deugnier Y. (2016). Haemochromatosis. Lancet 388 706–716. [DOI] [PubMed] [Google Scholar]
- Ramsey A. J., Hillas P. J., Fitzpatrick P. F. (1996). Characterization of the active site iron in tyrosine hydroxylase. redox states of the iron. J. Biol. Chem. 271 24395–24400. 10.1074/jbc.271.40.24395 [DOI] [PubMed] [Google Scholar]
- Redfearn E. R., King T. E. (1964). Mitochondrial nadh2 dehydrogenase and nadh2 oxidase from heart muscle: possible existence of a ferredoxin-like component in the respiratory chain. Nature 202 1313–1316. 10.1038/2021313a0 [DOI] [PubMed] [Google Scholar]
- Redmond T. M., Poliakov E., Yu S., Tsai J. Y., Lu Z., Gentleman S. (2005). Mutation of key residues of RPE65 abolishes its enzymatic role as isomerohydrolase in the visual cycle. Proc. Natl. Acad. Sci. U.S.A. 102 13658–13663. 10.1073/pnas.0504167102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers B. S., Symons R. C., Komeima K., Shen J., Xiao W., Swaim M. E., et al. (2007). Differential sensitivity of cones to iron-mediated oxidative damage. Invest. Ophthalmol. Vis. Sci. 48 438–445. 10.1167/iovs.06-0528 [DOI] [PubMed] [Google Scholar]
- Roth A. M., Foos R. Y. (1972). Ocular pathologic changes in primary hemochromatosis. Arch. Ophthalmol. 87 507–514. 10.1001/archopht.1972.01000020509003 [DOI] [PubMed] [Google Scholar]
- Rueda Adel C., Grande N. C., Fernandez E. A., Enriquez De Salamanca R., Sala L. A., Jimenez M. J. (2011). Mutations in HFE and TFR2 genes in a spanish patient with hemochromatosis. Rev. Esp. Enferm Dig. 103 379–382. 10.4321/s1130-01082011000700010 [DOI] [PubMed] [Google Scholar]
- Schmidt P. J., Toran P. T., Giannetti A. M., Bjorkman P. J., Andrews N. C. (2008). The transferrin receptor modulates Hfe-dependent regulation of hepcidin expression. Cell Metab 7 205–214. 10.1016/j.cmet.2007.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shichi H. (1969). Microsomal electron transfer system of bovine retinal pigment epithelium. Exp. Eye Res. 8 60–68. 10.1016/s0014-4835(69)80081-3 [DOI] [PubMed] [Google Scholar]
- Shu W., Baumann B. H., Song Y., Liu Y., Wu X., Dunaief J. L. (2019). Iron accumulates in retinal vascular endothelial cells but has minimal retinal penetration after IP Iron dextran injection in mice. Invest. Ophthalmol. Vis. Sci. 60 4378–4387. 10.1167/iovs.19-28250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu W., Dunaief J. L. (2018). Potential treatment of retinal diseases with iron chelators. Pharmaceuticals (Basel) 11:112. 10.3390/ph11040112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simovich M. J., Miller B., Ezzeldin H., Kirkland B. T., Mcleod G., Fulmer C., et al. (2001). Four novel mutations in the RPE65 gene in patients with leber congenital amaurosis. Hum. Mutat. 18:164. 10.1002/humu.1168 [DOI] [PubMed] [Google Scholar]
- Slater E. C. (1949). The measurement of the cytochrome oxidase activity of enzyme preparations. Biochem. J. 44 305–318. 10.1042/bj0440305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song D., Dunaief J. L. (2013). Retinal iron homeostasis in health and disease. Front. Aging Neurosci. 5:24. 10.3389/fnagi.2013.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song D., Kanu L. N., Li Y., Kelly K. L., Bhuyan R. K., Aleman T., et al. (2016). AMD-like retinopathy associated with intravenous iron. Exp. Eye Res. 151 122–133. 10.1016/j.exer.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song D., Zhao L., Li Y., Hadziahmetovic M., Song Y., Connelly J., et al. (2014). The oral iron chelator deferiprone protects against systemic iron overload-induced retinal degeneration in hepcidin knockout mice. Invest Ophthalmol Vis Sci 55 4525–4532. 10.1167/iovs.14-14568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling J., Guttha S., Song Y., Song D., Hadziahmetovic M., Dunaief J. L. (2017). Iron importers Zip8 and Zip14 are expressed in retina and regulated by retinal iron levels. Exp. Eye Res. 155 15–23. 10.1016/j.exer.2016.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson D. A., Gyurus P., Fleischer L. L., Bingham E. L., Mchenry C. L., Apfelstedt-Sylla E., et al. (2000). Genetics and phenotypes of RPE65 mutations in inherited retinal degeneration. Invest. Ophthalmol. Vis. Sci. 41 4293–4299. [PubMed] [Google Scholar]
- Trenor C. C., Campagna D. R., Sellers V. M., Andrews N. C., Fleming M. D. (2000). The molecular defect in hypotransferrinemic mice. Blood 96 1113–1118. [PubMed] [Google Scholar]
- Ugarte M., Grime G. W., Lord G., Geraki K., Collingwood J. F., Finnegan M. E., et al. (2012). Concentration of various trace elements in the rat retina and their distribution in different structures. Metallomics 4 1245–1254. 10.1039/c2mt20157g [DOI] [PubMed] [Google Scholar]
- Vulpe C. D., Kuo Y. M., Murphy T. L., Cowley L., Askwith C., Libina N., et al. (1999). Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat. Genet. 21 195–199. 10.1038/5979 [DOI] [PubMed] [Google Scholar]
- Wallace D. F., Summerville L., Crampton E. M., Frazer D. M., Anderson G. J., Subramaniam V. N. (2009). Combined deletion of Hfe and transferrin receptor 2 in mice leads to marked dysregulation of hepcidin and iron overload. Hepatology 50 1992–2000. 10.1002/hep.23198 [DOI] [PubMed] [Google Scholar]
- Ward R. J., Zucca F. A., Duyn J. H., Crichton R. R., Zecca L. (2014). The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol. 13 1045–1060. 10.1016/S1474-4422(14)70117-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessling-Resnick M. (2017). Excess iron: considerations related to development and early growth. Am. J. Clin. Nutr. 106 1600s–1605s. 10.3945/ajcn.117.155879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widdowson E. M., McCance R. A. (1937). The absorption and excretion of iron before, during and after a period of very high intake. Biochem. J. 31:2029. 10.1042/bj0312029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolkow N., Song D., Song Y., Chu S., Hadziahmetovic M., Lee J. C., et al. (2012). Ferroxidase hephaestin’s cell-autonomous role in the retinal pigment epithelium. Am. J. Pathol. 180 1614–1624. 10.1016/j.ajpath.2011.12.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolkow N., Song Y., Wu T. D., Qian J., Guerquin-Kern J. L., Dunaief J. L. (2011). Aceruloplasminemia: retinal histopathologic manifestations and iron-mediated melanosome degradation. Arch. Ophthalmol. 129 1466–1474. 10.1001/archophthalmol.2011.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong-Riley M. T. (2010). Energy metabolism of the visual system. Eye Brain 2 99–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yau K. W., Baylor D. A. (1989). Cyclic GMP-activated conductance of retinal photoreceptor cells. Annu Rev. Neurosci. 12 289–327. 10.1146/annurev.ne.12.030189.001445 [DOI] [PubMed] [Google Scholar]
- Yefimova M. G., Jeanny J. C., Guillonneau X., Keller N., Nguyen-Legros J., Sergeant C., et al. (2000). Iron, ferritin, transferrin, and transferrin receptor in the adult rat retina. Invest. Ophthalmol. Vis. Sci. 41 2343–2351. [PubMed] [Google Scholar]
- Young R. W. (1967). The renewal of photoreceptor cell outer segments. J. Cell. Biol. 33 61–72. 10.1083/jcb.33.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R. W., Bok D. (1969). Participation of the retinal pigment epithelium in the rod outer segment renewal process. J. Cell. Biol. 42 392–403. 10.1083/jcb.42.2.392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zecca L., Youdim M. B., Riederer P., Connor J. R., Crichton R. R. (2004). Iron, brain ageing and neurodegenerative disorders. Nat. Rev. Neurosci. 5 863–873. 10.1038/nrn1537 [DOI] [PubMed] [Google Scholar]
- Zerbib J., Pierre-Kahn V., Sikorav A., Oubraham H., Sayag D., Lobstein F., et al. (2015). Unusual retinopathy associated with hemochromatosis. Retin. Cases Brief Rep. 9 190–194. 10.1097/ICB.0000000000000135 [DOI] [PubMed] [Google Scholar]
- Zhao L., Li Y., Song D., Song Y., Theurl M., Wang C., et al. (2014). A high serum iron level causes mouse retinal iron accumulation despite an intact blood-retinal barrier. Am. J. Pathol. 184 2862–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]