Abstract
Since December 2019, the coronavirus disease-2019 (COVID-19) has been keeping the world in suspense. Proven risk factors for a severe course of COVID-19 are common diseases like diabetes, hypertension, cardiovascular or respiratory disorders. Until today, little is known about the psychological burden of individuals suffering from these high-risk diseases regard to COVID-19. The aim of the study was to define the impact of the coronavirus pandemic on behavior and mental health in individuals at high risk for developing a severe COVID-19 course. Items assessed generalized anxiety (GAD-7), COVID-19-related fear, adherent/dysfunctional safety behavior, and the subjective risk perception of regarding symptoms, having a severe course and dying because of COVID-19. Data were compared between participants with the high risk diseases and individuals without any of those diseases. 16,983 respondents completed the study. Generalized anxiety, COVID-19-related fear, adherent/dysfunctional safety behavior and subjective risk perception were elevated in participants with high-risk diseases. The increased COVID-19-related fear as a functional concern is a conclusion on the increased risk of a severe course. The functionality of the fear is reflected in people’s increased need for security and includes an increase in both adherent and dysfunctional safety behavior that underlines the need for psychological support strategies.
Keywords: COVID-19, comorbidities, multimorbidity, anxiety, safety behavior, mental health
Introduction
The new respiratory viral infection SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) has developed into a worldwide pandemic since December 2019. The SARS-CoV-2 is formerly also known as 2019-nCoV-2. In scientific and clinical literature, the virus and its subsequent disease is known and termed as COVID-19. In Europe (France) the first cases were reported on the 24th January of 2020. 1
COVID-19 currently has a mortality rate of 1.9% in Germany. Other countries are much more affected with a case-fatality of 5.3% in Italy, 5.2% in China, 4.4% in the United Kingdom and 2.5% in the USA. 2 In mild to moderate COVID-19 cases, the symptoms are loss of smell, headaches, nasal obstruction and fatigue. 3 Severe courses are associated with dyspnoea, hypoxia, or infiltration of more than 50% of lung tissue on imaging. In critical cases, symptoms such as respiratory failure, shock or multiorgan system dysfunction were reported. 4 In the early stages of the pandemic, only few effective treatment options existed. 5
In retrospective analyses of COVID-19 patients, the pattern of comorbidities associated with a worse outcome was disclosed. Overall, 23.7% to 48% of those affected had comorbidities, with diabetes mellitus, hypertension and coronary heart disease being the most frequently described disorders. Less common in general, but also of prognostic importance, were malignancies, chronic kidney disease and conditions of immunodeficiency.6-9 Further studies described a correlation between coronary heart diseases and acute cardiac events or a poor outcome in patients with influenza or other respiratory viral infections.10-14 As further comorbidities that are at risk for a severe course, hypertensive disease, heart failure, sepsis, diabetes, obesity, renal failure, Alzheimer disease and chronic lower respiratory diseases are to be mentioned. 15
Retrospective data analysis of COVID-19 patients showed that patients with at least one of the high-risk conditions (diabetes mellitus, hypertension, chronic respiratory diseases, and cardiovascular diseases) suffered from a more severe course and had increased mortality. Moreover, it was noted that severe pulmonary manifestations of COVID-19 were associated with an increased risk of cardiac complications, 13 especially if cardiovascular diseases were already present. Based on these observations, several diseases were defined as high-risk morbidities for COVID-19.6,15-17 Our focus is on the comorbidities- diabetes, hypertension, chronic respiratory diseases, and cardiovascular diseases. They will be referred to as high-risk diseases in the following.
By restricting travel and social contacts, governments are trying to prevent new SARS-CoV-2 infections. 17 As Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization, reported: “Not only is the COVID-19 pandemic a threat to physical health; it also affects mental health. [. . .] In the current crisis, people can be fearful about becoming ill and dying, losing livelihoods and loved ones, and being socially excluded and separated from families and caregivers.” 18 Studies investigating the mental health of the population in the context of the coronavirus pandemic showed a sharp increase in symptoms of depression and anxiety, a decrease in sleep quality and an escalation of stress.19-22 In Italy 57.1% of respondents reported increased scores in questionnaires for sleep disorders, 32.1% for generalized anxiety and 41.8% reported increased distress experience.19,23 German studies revealed a significantly increased incidence rate of generalized anxiety (44.9%), depression (14.3%), mental distress (65.2%) and COVID-19 related anxiety (59%). These observations are in line with findings from studies conducted in Asia.19,24
On January 23, 2020, the city of Wuhan was under quarantine and closed off. 25 In Germany, individual persons are quarantined if they have symptoms and indication of infection. Previous studies on social isolation during quarantine showed that certain stress factors lead to higher psychological vulnerability. Such factors are in particular: fear of infection, being bored or lack of information.26,27 Examining the mental health of SARS (severe acute respiratory syndrome) survivors, the patients still suffered from psychological stress months after the acute infection. 28 Thus, it is suggested that the coronavirus pandemic may also have long-term effects on the mental health of the population.29,30 Individuals with chronic diseases already have an increased psychological burden due to their medical condition. 31 During the pandemic, they are also “patients at risk.” Hence, the literature suggests that the impact of the chronic disease in addition to the worries about a possible COVID-19 significantly increases the psychological burden in an individual and the general population. 32
To reduce the spread of COVID-19, increased hygiene measures and social distancing are recommended. 33 Even in earlier epidemics, such as swine flu, a change in people’s safety behavior has been shown when they had increased concern about the disease. 34 Recent studies on anxiety and behavior during the COVID-19 pandemic have shown increased levels of non-recommended behavior in people with elevated anxiety. 35 However, it could be suggested that individuals with diagnosed cancer use more often adherent safety behavior. Furthermore, they self-reported an increased COVID-19 related fear. 32
Previous studies focused on the physical effects (immune system, cardiovascular status) of COVID-19 in patients with somatic disease.7,36,37 The aim of the present study therefore is to investigate the generalized anxiety, fear and behavior associated with COVID-19 in people with chronic diseases. The study, focusing on people with high-risk conditions (diabetes, hypertension, chronic respiratory diseases and cardiovascular diseases), 38 aims to objectify the fear and behavior of these risk groups in order to assess how the current pandemic is affecting the mental health of these patients and whether specific help should be offered in the future to those with high-risk diseases. In considering, individuals with high-risk conditions compared to people without these diseases, we expect an increase in generalized anxiety, COVID-19-related fear and a change in their safety behavior. We hypothesized persons with high-risk diseases show an increased adherent safety behavior. In addition, they are more likely to estimate an increased risk of presenting symptoms of COVID-19, having a severe course or dying of the disease.
Methods
Study Design
A cross-sectional study design was conducted based on an online survey. A period of 66 days (March 10th-May 14th) was reviewed. By 14th of May 2020, 174 478 COVID-19 infections and 7884 deaths have been reported in Germany. 39
A total of 19 870 individuals throughout Germany participated in the study, 16 983 completed the questionnaire (85.4% completion rate). The questionnaire was distributed online via social media channels (Facebook local groups and official groups for example, University Hospital Essen, WhatsApp, and Instagram) and with the support of local and supra-local online and offline media (print, radio and television). The entire survey was compiled and run via Unipark (Questback GmbH).
3735 individuals self-reported a disease comorbidity associated with high risk for SARS-CoV-2 infection (diabetes, hypertension, chronical respiratory and cardiovascular diseases). High-risk diseases are defined as diseases that predict a significantly worse course of COVID-19 compared to those without high risk diseases. 38 No distinction was made between type 1 and type 2 diabetes. If individuals had been diagnosed with more than 1 high-risk disease, they are described in the following as multimorbid. 764 respondents were identified as multimorbid. Respondents without any of those 4 high-risk diseases were defined as the healthy control group. All participants gave written consent to participate in the survey.
Instrument
Basic demographic details, medical status and COVID-19 specific items were assessed, including age, gender, education, marital status. Additionally, the questionnaire contained a validated psychometric instrument to measure the generalized anxiety (GAD-7: Generalized Anxiety Disorder-7, 7 items, four-point-Likert scale, ranging from 0 = never to 3 = nearly every day). 40 Moreover, to measure the COVID-19-related fear, a single item with a seven-point-Likert scale, ranging from 1 to 7, was used (“COVID-19 is disconcerting for me”). Furthermore, the locus of control was measured in terms of its significance for risk perception and safety behavior. 41 Nine Items were used to cover the general recommendations by the Word Health Organization. 42 Concerning the safety behavior, a distinction was made between adherent safety behavior (increased hand washing, avoidance of public places, public transport, and changes of travel plans) and dysfunctional safety behavior. Regarding the dysfunctional safety behavior respondents were asked if they buy large quantities of hand sanitizer, toilet paper or emergency food and if they have become more selfish in their behavior). As well a seven-point Likert scale were used (1 = strongly disagree to 7 = strongly agree). The subjective risk perception (suffering from COVID-19, having a severe course and increased mortality) was recorded in percent (0%-100%). The subjective level of information was assessed by 3 items. Those were seven-point-Likert scaled.
Statistical Analysis
Data analysis was conducted using SPSS Statistics 25 (IMB, Armonk, NY), as well as R 3.6.3. 43 The dependent variables COVID-19-related fear, generalized anxiety, safety behaviors and questions about the subjective risk perception of presenting symptoms of COVID-19, having a severe course or dying of COVID-19 were investigated by univariate ANOVA in the high-risk or multimorbid patients versus the healthy control group. Further regression analyses were performed to assess whether such results are robust to distributional differences in their basic characteristics. Here, the respondents’ gender and age were included as covariates. These analyses will be reported in the Supplemental Online Material.
For the GAD-7 items a sum mean score was calculated
The groups with high-risk diseases were compared with healthy respondents who self-reported do not suffer from any somatic disease defined in the risk group. In addition, multimorbid participants who reported more than 1 risk disease were evaluated and compared with each other.
Post-hoc t-tests were performed to compare the effects. In the following all values of the t-tests are Tukey-corrected. Regarding the indication of significance and effect, in addition to the P-values (significant P < .05), the effect sizes are also indicated as η2 for ANOVAs and as Cohen’s 44 d for t-tests. According to Cohen (1988) the limits for the size of the effect described with ηp2 are 0.01 (small effect), 0.06 (medium effect) and 0.14 (large effect). Significance tests are oversensitive in a large sample as here present. The standard error gets too small. To evaluate and assess the precision of the estimate, the 95% confidence intervals (CIs) are also shown for the t-tests.45,46
Ethical Considerations
The Ethics Committees of the University Hospitals Essen has approved the study (20-9307-BO).
Role of the Funding Source
This study was funded by the Essen University Medicine Foundation (Stiftung Universitätsmedizin Essen). As a funding source the Essen University Medicine Foundation had no influence neither on the study design, collection, analysis, nor interpretation of the data and it had no influence on the writing of the report or on the decision to submit the paper for publication.
Results
A total of N = 16 983 participants completed the survey. 12 885 participants answered the question concerning the presence of a somatic disease with “no.” They form the healthy control group. 3697 participants reported at least one of the 4 defined high-risk diseases. Patients with more than 1 high-risk disease and were defined as multimorbid. They could be separated in groups with 2, 3, or 4 high-risk diseases (Table 1). In total most respondents were between 25-44 years old and 70% were female. Almost half of them have completed a university degree (42,44%), 42,62% are married and more than 50% live a metropolis (55,22%) (Table 2). Considering the demographic data, the sample should be defined as a convenience sample.
Table 1.
Overview of the Number of Participants with the Different High-Risk Diseases and the Analysis of the Frequency of the High-Risk Diseases in Multimorbid Persons.
| Multimorbid | |||||
|---|---|---|---|---|---|
| Healthy (total) | 1 Disease | 2 Diseases | ≥3 Diseases | Total | |
| Diabetes mellitus | 0 | 184 | 226 | 125 | 535 |
| Hypertension | 0 | 1518 | 485 | 155 | 2158 |
| Cardiovascular diseases | 0 | 205 | 222 | 119 | 546 |
| Chronic respiratory diseases | 0 | 1026 | 267 | 122 | 1415 |
| Total | 12 885 | 2933 | 600 | 164 | |
Table 2.
Sociodemographic.
| n (overall = 16 582) | Proportion in % | |
|---|---|---|
| Age | ||
| 18-24 years | 2177 | 13.13 |
| 25-34 years | 3893 | 23.48 |
| 35-44 years | 3586 | 21.63 |
| 45-54 years | 2980 | 17.97 |
| 55-64 years | 2232 | 13.46 |
| 65-74 years | 700 | 4.22 |
| 75+ | 128 | 0.77 |
| Missing* | 886 | 5.34 |
| Gender | ||
| Female | 11 614 | 70.04 |
| Male | 4917 | 29.65 |
| Other | 51 | 0.31 |
| Community Size | ||
| Metropolis (>100 000 inhabitants) | 9157 | 55.22 |
| Medium-sized city (>20 000 inhabitants) | 3795 | 22.89 |
| Small town (>5000 inhabitants) | 1842 | 11.11 |
| Rural community (<5000 inhabitants) | 1788 | 10.78 |
| Marital Status | ||
| Single | 4722 | 28.48 |
| Married | 7067 | 42.62 |
| Living in relationship | 3439 | 20.74 |
| Divorced | 1017 | 6.13 |
| Widowed | 228 | 1.37 |
| Other | 109 | 0.66 |
| Education | ||
| University degree | 7037 | 42.44 |
| High school degree | 5422 | 32.70 |
| Secondary school degree (Realschule) | 3051 | 18.40 |
| Secondary school degree (Hauptschule) | 740 | 4.46 |
| No school degree | 52 | 0.31 |
| Other | 280 | 1.69 |
Due to technical difficulties during the launch of the survey, age data from 886 participants went missing.
Generalized Anxiety and COVID-19-Related Fear
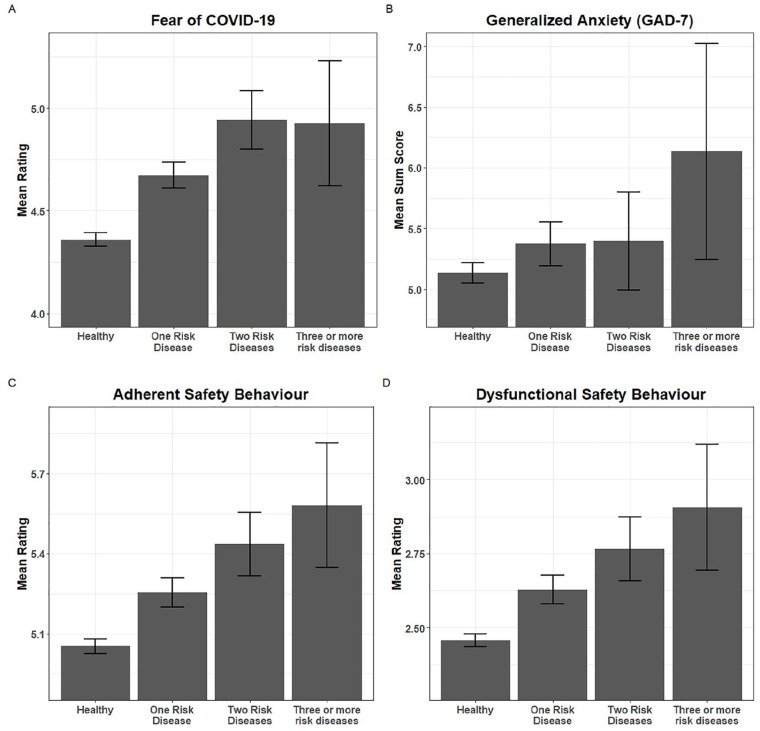
In terms of generalized anxiety (GAD-7), a detailed analysis of people with 1, 2, or more high-risk diseases showed differences. The analysis of the GAD-7 scores showed difference between the investigated groups (F(3,16578) = 4.399, P = .004, η2 < 0.001). Individuals with 2 diseases had significantly more COVID-19-related fear than persons with only 1 high-risk disease (F(3,16578) = 43.92, P < .001, ηp2 = 0.008). Furthermore there were significant differences between the healthy group compared to any group with diseases regardless of the number of diseases (1 disease: mean difference: 4.67: 95%-CI [−0.41, 0.22], P < .001, 2 diseases: mean difference 4.94; 95%-CI [−0.78, −0.38], P < .001; 3 or more diseases: mean difference: 4.93; 95%-CI [−0.94, −0.19], P < .001) (Figure 1A).
Figure 1.
Detailed analysis of multimorbid individuals. Comparison were made between healthy and individuals with 1, 2, 3, or more diseases. Multimorbid means more than 1 (up to 4) high-risk diseases. (A) Note: Sum score (y-axis) for the COVID-19-related fear. Means: eg, 3 or more disease: MCOVID = 4.93; healthy: MCOVID = 4.36. Comparison individuals with 2 high-risk diseases with 1 high-risk disease 95%-CI [−0.48, −0.05], P < .05. Comparison healthy with any individuals with high-risk diseases regardless of the number of diseases: 1 disease: 95%-CI [−0.41, −0.22], P < .01, 2 diseases 95%-CI [−0.78, −0.38], P < .01; 3 or more diseases 95%-CI [−0.94, −0.19], P < .01. (B) Note: Mean sum score for the generalized anxiety—GAD (y-axis). No significant difference between the investigated groups F(3,16578) = 4.399, P = .004, η2 < 0.001. Means: eg, 3 or more diseases: MGAD = 6.13; healthy: MGAD = 5.13. (C) and (D) Note. Mean sum scores (y-axis) describe the safety behavior in respondents—distinguished between adherent and dysfunctional safety behavior. Adherent safety behavior: Means: eg, healthy: Madherent = 5.05; 3 or more disease: Madherent = 5.58; F(3,16578) = 27.172, P < .001, η2 = 0.005; dysfunctional safety behavior: Means: healthy: Mdysfunctional = 2.46; 3 or more disease: Mdysfunctional = 2.9; F(3,16578) = 29.069, P < .001, η2 = 0.005.
Please note that these are the means and 95%-CIs computed based on the data as such, not the marginal means and adjusted 95%-CIs of the ANOVAs and the subsequent post-hoc tests.
Comparison of Adherent and Dysfunctional Safety Behavior in Multimorbid Individuals
Analyses showed significant differences for adherent and dysfunctional safety behavior between the healthy respondents and those with somatic diseases, irrespective of how many high-risk diseases were reported (adherent: F(3,16578) = 27.172, P < .001, η2 = 0.005; dysfunctional: F(3,16578) = 29.069, P < .001, η2 = 0.005). Regarding both adherent and dysfunctional safety behavior, healthy participants had the lowest scores and those with 3 or more high-risk diseases the highest (adherent_healthy: M = 5.05; adherent_3 or more disease: M = 5.58; dysfunctional_healthy: M = 2.46; dysfunctional_3 or more disease: M = 2.9) (Figure 1B).
Analysis of Multimorbid Individuals Concerning Their Subjective Risk Perception of Presenting Symptoms of COVID-19, Having a Severe Course or Dying of COVID-19
Concerning the subjective risk perception of contracting COVID-19, of experiencing a severe course or dying of the disease, the analyses of the individual items showed the same pattern: The more high-risk diseases were diagnosed, the subjective risk perception turned out to be larger. Healthy people reported the lowest percentages in any of these questions (healthy: symptoms: M = 47.82, course: M = 20.88, death: M = 8.49; 3 or more disease: symptoms: M = 65.87, course: M = 58.21, death: M = 41.03) (Figure 2). Significant difference were found for each question between all investigated groups, except between the group with 2 diseases and those with 3 or more in the question regarding the risk perception of developing symptoms (symptoms: F(3,16578) = 177.94, P < .001, η2 = 0.031; course: F(3,16578) = 739.48, P < .001, η2 = 0.118; death: F(3,16576) = 548.74, P < .001, η2 = 0.09) (Figure 2).
Figure 2.
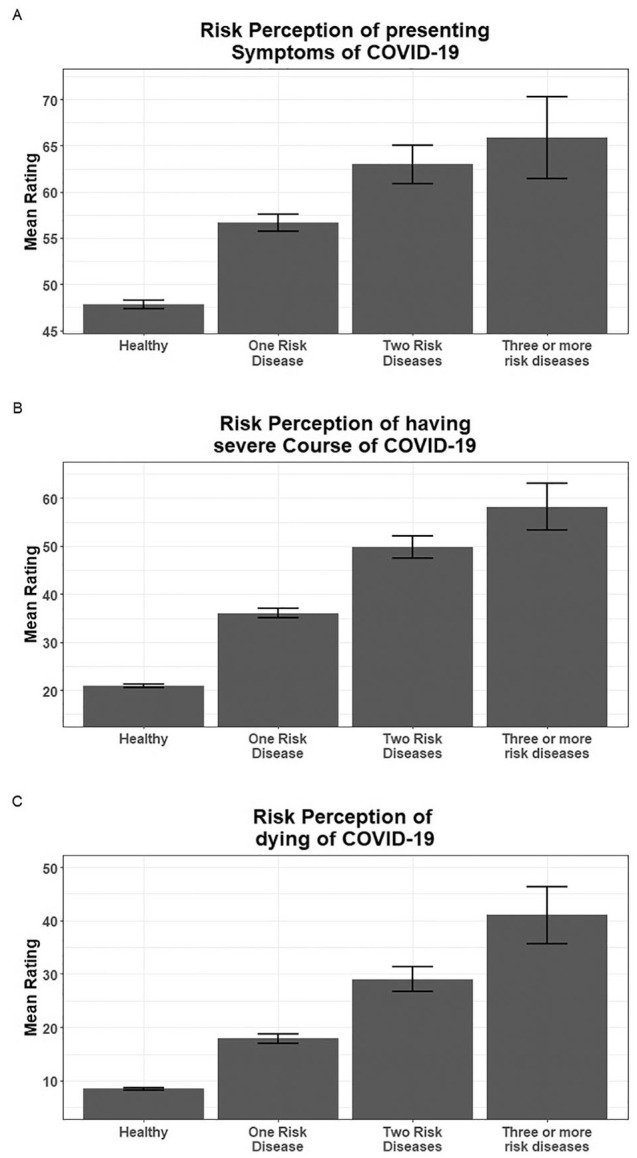
Mean sum score (y-axis) for subjective risk perception of acquire symptoms of COVID-19 (A), have a severe course of COVID-19 (B) and dying on COVID-19 (C) in individuals with 1, 2, 3, or more diseases or healthy respondents. The subjective risk perception was recorded in percent (0-100%). Means: eg, healthy: Msymptoms = 47.82, Mcourse = 20.88, Mdeath = 8.49; 3 or more disease: Msymtpomas = 65.87, Mcourse = 58.21, Mdeath = 41.03. Symptoms: F(3,16578) = 177.94, P < .001, η2 = 0.031; course: F(3,16578) = 739.48, P < .001, η2 = 0.118; death: F(1,5) = 548.74, P < .001, η2 = 0.09.
Please note that these are the means and 95%-CIs computed based on the data as such, not the marginal means and adjusted 95%-CIs of the ANOVAs and the subsequent post-hoc tests.
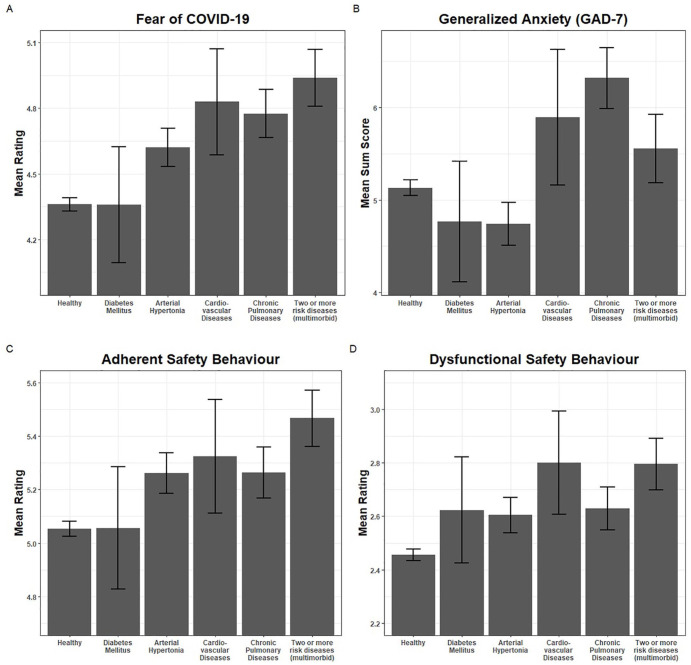
Comparison of the Individuals with High-Risk Diseases
Patients with chronic respiratory diseases had the highest GAD-7 sum score and appeared the most anxious (chronic respiratory diseases: M = 6.32, healthy: M = 5.13). Compared to healthy individuals the difference was significant: Thus, compared to healthy individuals, the GAD-7 score was lowest in participants with diabetes and hypertension (hypertension: M = 4.74, diabetes: M = 4.77). The difference was significant (F(5,16576) = 15.899, P < .001, η2 = 0.005) (Figure 3A).
Figure 3.
Detailed analysis of individuals with 1 high-risk disease (diabetes mellitus, hypertension, cardiovascular and chronic respiratory diseases) and multimorbid patients (more than 1 high-risk disease). Comparison were made between healthy and individuals with a high-risk disease. (A) Note. Sum score (y-axis) for the COVID-19-related fear. Means: eg, multimorbid: MCOVID = 4.94; healthy: MCOVID = 4.36. Significant difference between healthy and diabetes mellitus, hypertension, cardiovascular or respiratory diseases. Also significant difference between multimorbid persons, individuals with diabetes, hypertension and healthy F(5,16576) = 28.697, P < .001, η2 = 0.009. (B) Note. Mean sum score for the generalized anxiety—GAD (y-axisMeans: eg, chronic respiratory diseases: MGAD = 6.32, healthy: MGAD = 5.13, hypertension: MGAD = 4.74, diabetes mellitus: MGAD = 4.76. In comparison to the chronical respiratory diseases F(5,16576) = 15.899, P < .001, η2 = 0.005. b. (C) and (D) Note. Mean sum scores (y-axis) describe the safety behavior in respondents with between individuals with high-risk diseases—distinguished between adherent and dysfunctional safety behavior. Means: eg, healthy: Madherent = 5.05; Mdysfunctional = 2.46; multimorbid: Madherent = 5.47: Mdyfunctional = 2.795; cardiovascular diseases: Mdysfunctional = 2.8. Adherent safety behavior: significant between healthy and chronic respiratory diseases, high blood pressure and multiple high-risk diseases F(5,16576) = 16.76, P < .001, η2 = 0.005. Dysfunctional safety behavior: significant differences between healthy and chronic respiratory diseases, high blood pressure and multiple high-risk diseases F(5,16576) = 17.98, P < .001, η2 = 0.005.
Please note that these are the means and 95%-CIs computed based on the data as such, not the marginal means and adjusted 95%-CIs of the ANOVAs and the subsequent post-hoc tests.
Concerning COVID-19-related fear, the mean value of the totals was highest among multimorbid respondents and lowest among healthy participants (multimorbid: M = 4.94; healthy: M = 4.36). A significant difference was found between the healthy and those with diabetes mellitus, hypertension, cardiovascular or respiratory diseases. There was also a significant difference between multimorbid persons, individuals with diabetes, hypertension and the healthy participants (F(5,16576) = 28.697, P < .001, η2 = 0.009) (Figure 3A).
The adherent and dysfunctional safety behavior of people with high-risk diseases differs in comparison to healthy people. Healthy people reported less frequent implementation of both adherent and dysfunctional safety behavior (adherent_healthy: M = 5.05; dysfunctional_healthy: M = 2.46). Multimorbid patients accounted for the highest mean values of the totals regarding questions on adherent safety behavior (adherent_multimorbid: M = 5.47). The highest mean value concerning questions on dysfunctional safety behavior was found in persons with cardiovascular diseases (dysfunctional_cardiovascular diseases: M = 2.8; dysfunctional_multimorbid: M = 2.795) (Figure 3D). Significant differences in adherent safety behavior could be found between healthy respondents and persons with chronic respiratory diseases, high blood pressure and with multiple high-risk diseases (F(5,16576) = 16.76, P < .001, η2 = 0.005) (Figure 3C). Dysfunctional safety behavior showed significant differences for healthy respondents and as well persons with chronic respiratory diseases and with multiple high-risk diseases (F(5,16576) = 17.98, P < .001, η2 = 0.005) (Figure 3D).
Individuals with high-risk diseases estimated their risk of presenting symptoms of COVID-19, of a severe course of COVID-19 and of a COVID-19 related death significantly higher than healthy respondents, with the exception of the comparison between the healthy respondents and persons with diabetes mellitus when asked about the occurrence of symptoms of COVID-19 (eg, healthy: symptoms: M = 47.82, course: M = 20.88, death: M = 8.49; multimorbid: symptoms: M = 63.6, course: M = 51.62, death: M = 31.59). Participants with chronical respiratory, cardiovascular and multiple diseases indicate the highest risk estimates overall. (Symptoms: F(5,16576) = 123.15, P < .001, η2 = 0.036; course: F(5,16576) = 481.67, P < .001, η2 = 0.127; death: F(5,16576) = 342.08, P < .001, ηp2 = 0.094) (Figure 4).
Figure 4.
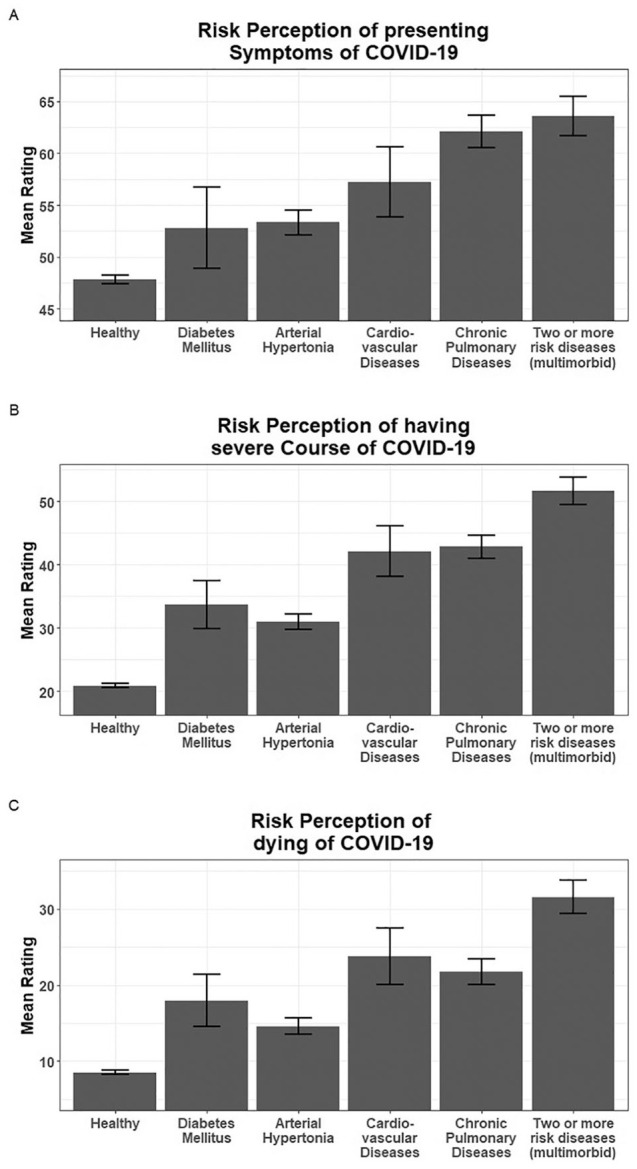
Note. Mean sum score (y-axis) for subjective risk perception of acquire symptoms of COVID-19 (A), have a severe course of COVID-19 (B) and dying on COVID-19 (C) in individuals with a high-risk disease or healthy respondents. The subjective risk perception was recorded in percent (0-100%). Means: eg, healthy: Msymptoms = 47.82, Mcourse = 20.88, Mdeath = 8.49; multimorbid: Msymptoms = 63.6, Mcourse = 51.62, Mdeath = 31.59. Symptoms: F(5,16576) = 123.15, P < .001, η² = 0.036; course: F(5,16576) = 481.67, P < .001, η² = 0.127; death: F(5,16576) = 342.08, P < .001, η² = 0.094.
Please note that these are the means and 95%-CIs computed based on the data as such, not the marginal means and adjusted 95%-CIs of the ANOVAs and the subsequent post-hoc tests.
Comparison of the Results of the ANOVA with Those of Regression Analysis
Further regression analyses were performed to assess if the above reported results might result from group imbalances of the variables age and gender (see Supplemental Online Material). Here, no fundamental differences were found, the overall pattern remains almost identical.
Discussion
Data concerning the psychological burden of individuals at high risk for a severe course of COVID-19 are rare. In this large cross-sectional study it was demonstrated, that individuals with chronic diseases which are defined as high-risk diseases for developing a severe course of COVID-19, (diabetes, hypertension, cardiovascular and chronic respiratory diseases) form a special group that differs significantly in its worries, fears and safety behavior from individuals that were not affected by any of the 4 conditions.
Somatically ill patients are at an elevated risk for a severe course of COVID-19. The risk is increased if they are multimorbid and have more than 1 chronic disease.6-9,13
To minimize the possibility of infection, they must be careful to follow hygiene measures and to develop appropriate behavior. Due to the response rate of 16 983 individuals, this survey was able to investigate different subgroups that are at risk for COVID-19 regarding their psychological burden.
To understand the psychological burden of these individuals is of utmost importance, as they already suffer from an increased psychological burden due to their chronic diseases, even without the threat of COVID-19. Through further stress factors or concerns the risk can multiply, and the mental strain can develop more quickly into a mental illness. Furthermore, it is known that people with mental illness have a worse overall course of their somatic illness. Thus, a chronic somatic disease has a negative impact on the mental health as well as a psychological disorder has an adverse effect on the somatic disease.31-47 In our study the variables examined (COVID-19-related fear and the adherent/dysfunctional safety behavior) were increased in participants with high-risk diseases. Respondents indicate a higher subjective likelihood regarding symptoms, course and COVID-19 related death than the healthy group.
Individuals with High-Risk Diseases Showed an Increased COVID-19-Related Fear Without Increased Generalized Anxiety
There is a high incidence of mental burden in chronic internal diseases. Previous studies showed an elevated number of patients with anxiety and depression combined with cardiovascular disease or diabetes. 13 Due to our study, in multimorbid patients, no significant differences but clear trends could be seen. The more comorbidities the patients had, the higher was the unadjusted generalized anxiety. Patients with a chronic respiratory disease seemed to be more anxious in general than the comparative groups. This observation was supported by previous studies on anxiety in patients with chronic obstructive respiratory diseases.48,49 Surprisingly, and in contrast, diabetes patients reported a significantly lower generalized anxiety than healthy people.
In the context of the coronavirus pandemic, however, the question of COVID-19 specific fear is also of great interest. Thus, the assumption was confirmed that risk groups show a higher level of COVID-19-related fear compared to healthy people. The present study showed that the more high-risk diseases were reported, the higher the COVID-19-related fear.
Subjective Risk Perception Regarding COVID-19 is Consistent with Science-Based Research
Furthermore, individuals with high-risk diseases estimated their own risk of suffering a severe course of COVID-19 higher than healthy ones. According to previous research among the high-risk patients, the respondents who also have increased risk of a severe or lethal course of COVID-19, indicate the highest risk perception. This includes patients with chronic respiratory, cardiovascular diseases and multimorbid individuals. 15 Data of the National Center for Health Statistics of the U.S. show that 94% of the deaths involving COVID-19 are mentioned with comorbidities. On October 24th 210 326 total COVID-19 deaths were reported. 45 574 patients had as a comorbidity hypertension, in 34 627 cases a diabetes was diagnosed and in 14 193 cases a heart failure was reported. 18 421 patients had a lower chronic respiratory disease. 50 In our study, the concern about a severe course of COVID-19 was consistent with the equally increased COVID-19-related fear. However, it should be considered that people with multiple pre-existing diseases show in previous studies a higher level of concern about their own disease as well as less perceived control over their health condition. This leads them to be at risk for developing a poor health related quality of life. 51
Increased COVID-19-Related Fear and Increased Safety Behavior in Individuals with High-Risk Diseases
Increased fear may result in the desire for higher security. Thus, the result of our survey regarding the safety behavior of the participants is not surprising. In case of existing high-risk diseases, individuals payed more attention to hygiene and the implementation of recommendations (eg, avoidance of major events, places). However, they also behaved more often in a dysfunctional way, which leads to a decoupling of the rational recommendation to an anxious state of mind. Interestingly, a trend was found that the more risk diseases are present, the more security measures are implemented. Most likely, COVID-19-related fear may reinforce the dysfunctional behavior. 52
Currently many hypotheses concerning COVID-19 are discussed in social media. One example is the use of dietary supplements to cure and prevent COVID-19. A clear position was taken on this in the Annals of Pharmacotherapy in August 2020. It is a false assumption that COVID-19 can be treated or prevented by dietary supplements. Pharmacists must ensure that consumers receive the correct information. 53 With the flood of new hypotheses every day, people could get misinformation and start to believe in mythbusters about COVID-19, which could lead to incorrect and dysfunctional behavior.
Summarizing, it could be shown that individuals with an increased risk for COVID-19 also had an increased fear of getting the disease and its consequences. However, in comparison to the control group, they did not show increased generalized anxiety. This indicates no additional mental burden in the somatically ill, but a realistic and appropriate fear of COVID-19. Thus, risk patients were realistic in estimating their probability of a severe disease course or even death related to COVID-19. Moreover, our survey shows that the high-risk groups adapted their behavior to their worries and fear. By trying to avoid infections they changed their daily behavior. They reported on the one hand an increased adherent behavior and on the other hand an increased dysfunctional behavior. The discrepancy between appropriate, adherent safety behavior and dysfunctional safety behavior is probably due to the increased fear of a possible infection with a severe course. As the same pattern emerges in regression analyses including age and gender as covariates, the results appear not be a product of an uneven distribution of these variables.
Limitations of the Study
Limitations also need to be considered. It must be critically noted that the differences between the groups are rather small and it should be spoken of a trend. However, the differences are significant. A further critical remark must be made with regard to the distribution of the number of participants. The groups of individuals with the different high-risk diseases have different group sizes. This may also affect the results of the comparisons. A further limitation to be mentioned is, that the survey does not provide a reliable proof of permanent residence in Germany. As a condition for participation, respondents should have a very good knowledge of the German language. The survey also covered only the period of the beginning of the pandemic. Thus, the reliability of the data is limited for the entire period of the corona pandemic. Additionally, the data of the survey were collected via online and analog channels. The possibility of selection bias should therefore be considered. Furthermore, it should be noted that 4 high-risk diseases represent only a selection of comorbidities that have an influence on the course of COVID-19. Further research on anxiety and behavior during the current pandemic in individuals with other high-risk diseases is recommended.
Conclusion
This is one of the first and largest studies on the psychological burden of individuals at high risk for a severe course of COVID-19. Persons with high-risk diseases such as diabetes, hypertension, cardiovascular and chronic respiratory diseases have significantly increased fear of developing symptoms of a COVID-19, having a severe course or dying of COVID-19 related death. Overall, COVID-19 related fear scores increased proportionally to the number of high-risk diseases reported by the respondents.
An important insight of this study is that we not only have to cater to the risk groups from a medical point of view, but also to their psychological needs. The increased COVID-19-related fear as a functional concern can be considered as a conclusion on the increased risk perception of a severe course. The functionality of the fear could reflected in people’s increased need for safety. However, there is an increase in both adaptive, adherent and maladaptive, dysfunctional safety behavior.
These observations let assume that although people realistically assess the situation, their behavior might be partly not target-oriented. To account for that, it is necessary to provide low-threshold advisory and support services. Our data tentatively suggest that it would be desirable to have an online service that is adequately suited to the needs of people with somatic risk diseases which enhances resilience and mindfulness. 19 For a better understanding of the mechanisms further analysis like moderation/mediation models could be performed as the next step.
To prevent the chronification of worries and fears which can lead to mental illnesses in persons with risk diseases, we need to monitor and ensure their psychological wellbeing. Due to the already existing burden of chronic disease, the patient considered in this study already have an increased risk for becoming mentally ill. Thus, this study is an important baseline for the development of preventive treatments for people with chronic diseases during the coronavirus pandemic. Due to the ongoing development of the pandemic it is necessary to research and reevaluate known results to acknowledge and address the psychological burden of individuals with possible other high risk diseases who have not been considered.
Supplemental Material
Supplemental material, sj-pdf-1-jpc-10.1177_2150132721996898 for Increased COVID-19-related fear and subjective risk perception regarding COVID-19 affects behavior in individuals with internal high-risk diseases by Hannah Kohler, Alexander Bäuerle, Adam Schweda, Benjamin Weismüller, Madeleine Fink, Venja Musche, Anita Robitzsch, Corinna Pfeiffer, Anke-Verena Benecke, Nora Dörrie, Dagmar Führer, Christian Taube, Tienush Rassaf, Martin Teufel and Eva-Maria Skoda in Journal of Primary Care & Community Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Essen University Medicine Foundation (Stiftung Universitätsmedizin Essen).
ORCID iDs: Hannah Kohler  https://orcid.org/0000-0002-8855-2699
https://orcid.org/0000-0002-8855-2699
Alexander Bäuerle  https://orcid.org/0000-0003-1488-8592
https://orcid.org/0000-0003-1488-8592
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Origin of SARS-CoV-2. Published March 26, 2020. Accessed January 22, 2021. https://apps.who.int/iris/bitstream/handle/10665/332197/WHO-2019-nCoV-FAQ-Virus_origin-2020.1-eng.pdf
- 2. Johns Hopkins University & Medicine. Mortality analyses. Published November 10, 2020. Accessed November 11, 2020. https://coronavirus.jhu.edu/data/mortality
- 3. Lechien JR, Chiesa-Estomba CM, Place S, et al. Clinical and epidemiological characteristics of 1,420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288:335-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). Published November 3, 2020. Accessed November 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
- 5. WHO Solidarity Trial Consortium, Pan H, Peto R, et al. Repurposed antiviral drugs for COVID-19 –interim WHO SOLIDARITY trial results. medRxiv. 2020:2020.10.15.20209817. doi: 10.1101/2020.10.15.20209817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):e35. [PMC free article] [PubMed] [Google Scholar]
- 8. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020;36:e3319. doi: 10.1002/dmrr.3319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Caramelo F, Ferreira N, Oliveiros B. Estimation of risk factors for COVID-19 mortality—preliminary results. medRxiv. 2020;146:110-118. doi:10.1016/j.jaci.2020.04.006 [Google Scholar]
- 10. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet. 2013;381:496-505. doi: 10.1016/s0140-6736(12)61266-5 [DOI] [PubMed] [Google Scholar]
- 11. Udell JA, Zawi R, Bhatt DL, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA. 2013;310:1711-1720. doi: 10.1001/jama.2013.279206 [DOI] [PubMed] [Google Scholar]
- 12. Blackburn R, Zhao H, Pebody R, Hayward A, Warren-Gash C. Laboratory-confirmed respiratory infections as predictors of hospital admission for myocardial infarction and stroke: time-series analysis of English data for 2004–2015. Clin Infect Dis. 2018;67:8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395: 1054-1062. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Williams RD, Markus AF, Yang C, et al. Seek COVER: Development and validation of a personalized risk calculator for COVID-19 outcomes in an international network. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. doi: 10.1016/s0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harrison SL, Fazio-Eynullayeva E, Lane DA, Underhill P, Lip GYH. Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: a federated electronic medical record analysis. PLoS Med. 2020;17:e1003321. doi: 10.1371/journal.pmed.1003321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bedford J, Enria D, Giesecke J, et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015-1018. doi: 10.1016/s0140-6736(20)30673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ghebreyesus TA. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. 2020;19:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bäuerle A, Teufel M, Musche V, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf). 2020;42:672-678. doi: 10.1093/pubmed/fdaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Forte G, Favieri F, Tambelli R, Casagrande M. The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian population. J Clin Med. 2020;9:1802. doi: 10.3390/jcm9061802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Teufel M, Schweda A, Dörrie N, et al. Not all world leaders use Twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J Public Health (Oxf). 2020;42:644-646. doi: 10.1093/pubmed/fdaa060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. The American Journal of Accountable Care. A timeline of COVID-19 developments in 2020. Published/Updated January 1, 2021. Accessed January 22, 2021. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020
- 26. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. doi: 10.1016/s0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lima CKT, de Medeiros Carvalho PM, Lima de Araújo Araruna Silva Lima I, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020;287:112915. doi: 10.1016/j.psychres.2020.112915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-326. doi: 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63:e32. doi: 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40-48. doi: 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turner J, Kelly B. Emotional dimensions of chronic disease. West J Med. 2000;172:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Musche V, Bäuerle A, Steinbach J, et al. COVID-19-related fear and health-related safety behavior in oncological patients. Front Psychol. 2020;11:1984. doi: 10.3389/fpsyg.2020.01984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Centers for Disease Control and Prevention. How to protect yourself & others. Published November 4, 2020. Accessed November 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- 34. Rubin GJ, Amlôt R, Page L, Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339: b2651. doi: 10.1136/bmj.b2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ben-Ezra M, Cary N, Goodwin R. The association between COVID-19 WHO non-recommended behaviors with psychological distress in the UK population: a preliminary study. J Psychiatr Res. 2020;130:286-288. doi: 10.1016/j.jpsychires.2020.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maddaloni E, Buzzetti R. Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes Metab Res Rev. 2020;36:e33213321. doi: 10.1002/dmrr.3321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. South AM, Diz DI, Chappell MC. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol. 2020;318:H1084-H1090. doi: 10.1152/ajpheart.00217.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94:91-95. doi: 10.1016/j.ijid.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Corona Virus (COVID-19).Published/Updated January 22, 2021 Accessed January 22, 2021. https://news.google.com/covid19/map?hl=de&mid=%2Fm%2F0345h&gl=DE&ceid=DE%3Ade
- 40. Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266-274. doi: 10.1097/mlr.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 41. Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12:e0186458. doi: 10.1371/journal.pone.0186458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. Published March 11, 2020. Accessed November 12, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- 43. Bates D. R: A Language and Environment for Statistical Computing ; 2020. Accessed January 27, 2021. https://www.R-project.org/
- 44. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 45. Lash TL. Heuristic thinking and inference from observational epidemiology. Epidemiology. 2007;18:67-72. doi: 10.1097/01.ede.0000249522.75868.16 [DOI] [PubMed] [Google Scholar]
- 46. Sterne JAC, Smith GD. Sifting the evidence-what’s wrong with significance tests? Phys Ther. 2001;81:1464-1469. doi: 10.1093/ptj/81.8.1464 [DOI] [PubMed] [Google Scholar]
- 47. Schneiderman N, Antoni MH, Saab PG, Ironson G. Health psychology: psychosocial and biobehavioral aspects of chronic disease management. Annu Rev Psychol. 2001;52:555-580. doi: 10.1146/annurev.psych.52.1.555 [DOI] [PubMed] [Google Scholar]
- 48. Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact, and treatment. Psychosom Med. 2003; 65:963-970. doi: 10.1097/01.PSY.0000097339.75789.81 [DOI] [PubMed] [Google Scholar]
- 49. Safa M, Tafti SF, Talischi F, Boroujerdi FG. Severity of anxiety disorders in patients with chronic obstructive pulmonary disease. Iran J Psychiatry. 2015;10:128. [PMC free article] [PubMed] [Google Scholar]
- 50. Centers for Disease Control and Prevention. Weekly updates by select demographic and geographic characteristics: provisional death counts for coronavirus disease 2019 (COVID-19). Published November 4, 2020. Accessed November 11, 2020. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm
- 51. Rijken M, Valderas JM, Heins M, Schellevis F, Korevaar J. Identifying high-need patients with multimorbidity from their illness perceptions and personal resources to manage their health and care: a longitudinal study. BMC Fam Pract. 2020;21:75. doi: 10.1186/s12875-020-01148-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Maner JK, Kenrick DT. When adaptations go awry: functional and dysfunctional aspects of social anxiety. Soc Issues Policy Rev. 2010;4:111-142. doi: 10.1111/j.1751-2409.2010.01019.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Adams KK, Baker WL, Sobieraj DM. Myth busters: dietary supplements and COVID-19. Ann Pharmacother. 2020;54: 820-826. doi: 10.1177/1060028020928052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jpc-10.1177_2150132721996898 for Increased COVID-19-related fear and subjective risk perception regarding COVID-19 affects behavior in individuals with internal high-risk diseases by Hannah Kohler, Alexander Bäuerle, Adam Schweda, Benjamin Weismüller, Madeleine Fink, Venja Musche, Anita Robitzsch, Corinna Pfeiffer, Anke-Verena Benecke, Nora Dörrie, Dagmar Führer, Christian Taube, Tienush Rassaf, Martin Teufel and Eva-Maria Skoda in Journal of Primary Care & Community Health