Abstract
Background.
Predictors of latent tuberculosis infection (LTBI) among close contacts of persons with infectious tuberculosis (TB) are incompletely understood, particularly the number of exposure hours.
Methods.
We prospectively enrolled adult patients with culture-confirmed pulmonary TB and their close contacts at 9 health departments in the United States and Canada. Patients with TB were interviewed and close contacts were interviewed and screened for TB and LTBI during contact investigations.
Results.
LTBI was diagnosed in 1390 (46%) of 3040 contacts, including 624 (31%) of 2027 US/Canadian-born and 766 (76%) of 1013 non-US/Canadian-born contacts. In multivariable analysis, age ≥5 years, male sex, non-US/Canadian birth, smear-positive index patient, and shared bedroom with an index patient (P < .001 for each), as well as exposure to >1 index patient (P < .05), were associated with LTBI diagnosis. LTBI prevalence increased with increasing exposure duration, with an incremental prevalence increase of 8.2% per 250 exposure hours (P < .0001). For contacts with <250 exposure hours, no difference in prevalence was observed per 50 exposure hours (P = .63).
Conclusions.
Hours of exposure to a patient with infectious TB is an important LTBI predictor, with a possible risk threshold of 250 hours. More exposures, closer exposure proximity, and more extensive index patient disease were additional LTBI predictors.
Keywords: latent tuberculosis infection, close contacts, epidemiology, exposure, exposure hours
Close contacts of patients with infectious tuberculosis (TB) are at high risk of Mycobacterium tuberculosis infection [1] (LTBI) as well as TB disease [2, 3]. Factors that predispose to LTBI are incompletely understood, particularly the relationship between the number of hours of exposure and likelihood of LTBI.
In the United States and Canada, health departments conduct contact investigations for patients with infectious TB to identify recently exposed individuals with active TB and LTBI so that they can be treated, thereby preventing further transmission as well as progression from LTBI to active TB [2, 3]. Index patient smear, contact age, medical risk factors, and household exposure are factors considered in US algorithms to establish contact investigation priority [2, 4]. Exposure duration is infrequently collected and a minimum cutoff for LTBI likelihood has not been established [2]. A better understanding of factors associated with LTBI diagnosis among recently exposed contacts has important implications for determining key data to collect and consider during contact investigations as well as developing improved algorithms to prioritize public health prevention efforts towards persons at highest risk of TB and LTBI diagnosis.
We conducted a prospective study of contact investigations that included index TB patient and contact interviews to collect detailed epidemiologic information on index patient, contact, and exposure environment characteristics, including systematic collection of hours of exposure to the index patient for each contact. In previous reports, we described the rates of TB among close contacts by time interval from index case diagnosis [5] and risk factors for TB [6]. In the current report, we examine factors associated with LTBI diagnosis among close contacts who completed screening for LTBI in the same cohort.
METHODS
Close contacts of adult patients with culture-positive pulmonary TB were prospectively enrolled in a multicenter study at 9 health departments in the Tuberculosis Epidemiologic Studies Consortium [7]. Close contacts were defined, identified, interviewed, and screened for LTBI and TB as previously described [5].
Latent tuberculosis infection was defined as having a positive tuberculin skin test (TST), which was defined as an induration of 5 mm or more; a negative TST was an induration of less than 5 mm [2]. Close contacts were defined as persons in the household, social, workplace, or school settings who had shared indoor airspace with a patient with pulmonary TB for more than 15 hours per week during 1 or more weeks or a total of more than 180 hours during a defined infectious period [5]. Overlapping hours of exposure between index case and contact were determined by systematic standardized interviewing of index patients and close contacts. To facilitate practical application of results and for consistency and comparability with analyses of exposure hours and TB risk [6], we used increments of 250 hours for the main LTBI exposure analyses. Only persons meeting the definition for a close contact were included in the analysis, and all references to contacts refer to close contacts.
Univariate analyses were performed on the potential index patient, individual, contact, and exposure location factors associated with LTBI diagnosis among contacts. We considered variables for multivariable models if their univariate P value was <.20. Using backward elimination, we kept variables if they had a 2-sided statistical significance level less than .05. Statistically significant differences were assessed using chi-square or Fisher’s exact test. All analyses were performed using SAS software version 9.2 (SAS Institute).
This study was reviewed and approved by institutional review boards at the Centers for Disease Control and Prevention and all project sites.
RESULTS
Characteristics of Close Contacts
Of 4490 contacts enrolled [6], 3040 had complete TST results and no evidence of TB disease and constituted the study population for this report. Among these, 1390 (48%) were TST positive, 21% were younger than 15 years, 67% were US/Canadian born, and 62% were household contacts (Table 1).
Table 1.
Characteristics of All Close Contacts Screened for Latent Tuberculosis Infection
| Characteristic | n (%) |
|---|---|
| Total | 3040 |
| Age, years | |
| 0–5 | 310 (10) |
| 6–14 | 319 (11) |
| 15–24 | 584 (19) |
| 25–44 | 1017 (33) |
| 45–64 | 652 (21) |
| ≥65 | 153 (5) |
| Unknown | 5 (0) |
| Sex | |
| Male | 1565 (51) |
| Female | 1473 (49) |
| Unknown | 2 (0) |
| Race/ethnicity | |
| White | 374 (12) |
| Black | 1575 (52) |
| Asian | 179 (6) |
| Hispanic | 797 (26) |
| Other/unknown | 115 (4) |
| Birthplace | |
| United States/Canada | 2027 (67) |
| Foreign-born | 1013 (33) |
| Place of contact | |
| Household | 1879 (62) |
| Nonhousehold | 1161 (38) |
| Screening results | |
| TST-positive | 1390 (46) |
| TST-negative | 1650 (54) |
| Hours of contact | |
| Median (interquartile range) | 440 (202–913) |
Abbreviation: TST, tuberculin skin test.
Factors Associated With Latent Tuberculosis Infection Diagnosis
Univariate factors associated with LTBI diagnosis are presented in Table 2 (all close contacts). In univariate LTBI analyses among all close contacts, factors associated with LTBI diagnosis included contact age more than 5 years, male sex, Asian or Hispanic race/ethnicity, and foreign birthplace; index patient positive sputum smear, bilateral disease, and cavitation on chest radiograph; and household exposure, shared bedroom with an index patient within the household, 250 exposure hours or more, and exposure to more than 1 index patient (Table 2). Contacts identified by index patient interview had a higher LTBI prevalence compared with those identified through other sources. Index patient cough, weight loss, fever, and night sweats and contact smoking and passive smoke exposure were not associated with LTBI prevalence. In analysis restricted to the subset of 1879 household close contacts, findings were similar (data not shown).
Table 2.
Univariate Analysis of Factors Associated With Latent Tuberculosis Infection Diagnosis Among All Close Contacts Screened for Latent Tuberculosis Infection
| Characteristic | LTBI, n (%) | No LTBI, n (%) | LTBI Diagnosis Prevalence, % | OR (95% CI) | P |
|---|---|---|---|---|---|
| Total | 1390 | 1650 | 45.7 | … | |
| Contact age, years | |||||
| 0–5 | 60 (4) | 250 (15) | 19.4 | Referent | |
| 6–14 | 104 (7) | 215 (13) | 32.6 | 2.0 (1.4, 2.9) | <.001 |
| 15–24 | 293 (21) | 291 (18) | 49.8 | 4.2 (3.0, 5.8) | <.001 |
| 25–44 | 550 (40) | 467 (28) | 54.1 | 4.9 (3.6, 6.7) | <.001 |
| 45–64 | 310 (22) | 342 (21) | 47.6 | 3.8 (2.7, 5.2) | <.001 |
| ≥65 | 70 (5) | 83 (5) | 45.8 | 3.5 (2.3, 5.4) | <.001 |
| Contact sex | |||||
| Male | 778 (56) | 787 (48) | 49.7 | Referent | |
| Female | 611 (44) | 862 (52) | 58.5 | 0.71 (.6, .8) | <.001 |
| Unknown | 1 (0) | 1 (0) | 50.0 | … | |
| Contact race/ethnicity | |||||
| White | 112 (8) | 262 (16) | 30.0 | Referent | |
| Black | 603 (43) | 972 (59) | 38.3 | 1.5 (1.1, 1.9) | .003 |
| Asian | 112 (8) | 67 (4) | 62.6 | 3.9 (2.7, 5.7) | <.001 |
| AIAN | 28 (2) | 64 (4) | 30.4 | 1.0 (.6, 1.7) | .92 |
| Hispanic | 522 (38) | 275 (17) | 65.5 | 4.4 (3.4, 5.8) | <.001 |
| Other/unknown | 13 (1) | 10 (1) | 56.5 | … | |
| Contact birthplace | |||||
| US/Canada | 624 (45) | 1403 (85) | 30.8 | Referent | |
| Foreign-born | 766 (55) | 247 (15) | 75.6 | 70 (5.9, 8.3) | <.001 |
| Contact HIV status | |||||
| HIV negative | 456 (33) | 355 (22) | 56.2 | Referent | |
| HIV positive | 0 (0) | 6 (100) | 100 | 0.10 (.01, 1.7) | .11 |
| Unknown | 934 (67) | 1289 (78) | 42.0 | … | |
| Index case smear positive | |||||
| No | 139 (10) | 301 (18) | 31.6 | Referent | |
| Yes | 1244 (90) | 1322 (80) | 48.5 | 2.0 (1.6, 2.5) | <.001 |
| Not done | 7 (1) | 27 (2) | 20.6 | … | |
| Index case smear quantity | |||||
| Negative | 139 (10) | 301 (18) | 31.6 | Referent | |
| 1+ | 248 (18) | 282 (17) | 46.8 | 1.9 (1.5, 2.5) | <.001 |
| 2–3+ | 344 (25) | 434 (26) | 44.2 | 1.7 (1.3, 2.2) | <.001 |
| 4+ | 529 (38) | 544 (33) | 49.3 | 2.1 (1.7, 2.7) | <.001 |
| Positive, no quantity | 123 (9) | 62 (4) | 66.5 | 4.3 (3.0, 6.2) | <.001 |
| No smear results | 7 (0) | 27 (2) | … | … | |
| Index case cavitary | |||||
| No | 691 (50) | 932 (56) | 42.6 | Referent | |
| Yes | 679 (49) | 677 (41) | 50.1 | 1.4 (1.2, 1.6) | <.001 |
| Unknown | 20 (1) | 41 (2) | 32.8 | … | |
| Index case bilateral | |||||
| No | 969 (70) | 1260 (76) | 43.5 | Referent | |
| Yes | 421 (30) | 390 (24) | 51.9 | 1.4 (1.2, 1.6) | <.001 |
| Index case lobes with disease | |||||
| 0 | 79 (6) | 182 (11) | 30.3 | Referent | |
| 1 | 378 (27) | 452 (27) | 45.5 | 1.9 (1.4, 2.6) | <.001 |
| 2 | 269 (19) | 406 (25) | 39.9 | 1.5 (1.1, 2.1) | .007 |
| 3 | 125 (9) | 96 (6) | 56.6 | 3.0 (2.1, 4.4) | <.001 |
| ≥4 | 63 (5) | 37 (2) | 63.0 | 3.9 (2.4, 6.4) | <.001 |
| Index case cough ≥3 weeks | |||||
| No | 245 (18) | 253 (15) | 49.2 | Referent | |
| Yes | 969 (70) | 1002 (61) | 49.2 | 1.0 (.8, 1.2) | .99 |
| Unknown | 176 (13) | 395 (24) | 30.8 | … | |
| Index case weight loss | |||||
| No | 388 (28) | 471 (29) | 45.2 | Referent | |
| Yes | 984 (71) | 1148 (70) | 46.2 | 1.04 (.9, 1.2) | .62 |
| Unknown | 18 (1) | 31 (2) | … | … | |
| Index case fever | |||||
| No | 627 (45) | 671 (41) | 48.3 | Referent | |
| Yes | 756 (54) | 971 (59) | 43.8 | 0.83 (.7, 1.0) | .013 |
| Unknown | 7 (1) | 8 (0) | … | … | |
| Index case night sweats | |||||
| No | 663 (48) | 738 (45) | 47.7 | Referent | |
| Yes | 721 (52) | 898 (54) | 51.9 | 0.89 (.8, 1.0) | .13 |
| Unknown | 2 (0) | 8 (0) | … | … | |
| Index case smoking | |||||
| No | 924 (66) | 965 (58) | 48.9 | Referent | |
| Yes | 465 (33) | 684 (41) | 40.5 | 0.7 (.6, .8) | <.001 |
| Unknown | 1 (0) | 1 (0) | 50.0 | … | |
| Exposure environment | |||||
| Household | 939 (68) | 940 (57) | 50.0 | Referent | |
| Workplace | 207 (15) | 289 (18) | 41.7 | 0.71 (.59, .88) | .001 |
| Social place | 201 (15) | 376 (23) | 34.8 | 0.53 (.44, .65) | <.001 |
| School | 43 (3) | 45 (3) | 48.9 | 0.96 (.62, 1.46) | .84 |
| Exposure location | |||||
| Nonhousehold | 462 (33) | 722 (44) | 39.0 | Referent | |
| Household, no shared bedroom | 727 (52) | 804 (49) | 47.5 | 1.4 (1.2, 1.6) | <.001 |
| Household, shared bedroom | 176 (13) | 107 (6) | 62.2 | 2.6 (2.0, 3.4) | <.001 |
| Unknown | 25 (2) | 17 (1) | … | … | |
| Number of exposures | |||||
| 1 | 1355 (97) | 1632 (99) | 45.4 | ≥2 vs 1 | |
| 2 | 25 (2) | 15 (1) | 62.5 | 2.0 (1.1, 3.6) | .027 |
| 3 | 3 (0) | 2 (0) | … | … | |
| Exposure hours | |||||
| <250 | 329 (24) | 568 (34) | 36.7 | Referent | |
| 250–499 | 345 (25) | 418 (25) | 45.2 | 1.4 (1.2, 1.7) | <.001 |
| ≥500 | 711 (51) | 662 (40) | 51.8 | 1.9 (1.6, 2.2) | <.001 |
| Identified by | |||||
| Index patient | 722 (52) | 813 (49) | 47.0 | 1.4 (1.2, 1.7) | <.001 |
| Other | 399 (29) | 648 (39) | 38.1 | Referent | |
| Unknown | 269 (19) | 189 (11) | … | … | |
No significant associations were observed for contact diabetes mellitus, smoking, passive smoking, or alcohol use, and these variables are not shown. Number of exposures = number of different index patients with tuberculosis to whom a contact was exposed; bilateral = disease in both the left and right lung fields on chest radiograph; smoking = cigarette smoking in the past 6 months.
Abbreviations: AIAN, American Indian, Alaskan Native, or First Nations (Canada); CI, confidence interval; HIV, human immunodeficiency virus; LTBI, latent tuberculosis infection; OR, odds ratio.
Hours of Exposure and Latent Tuberculosis Infection Prevalence
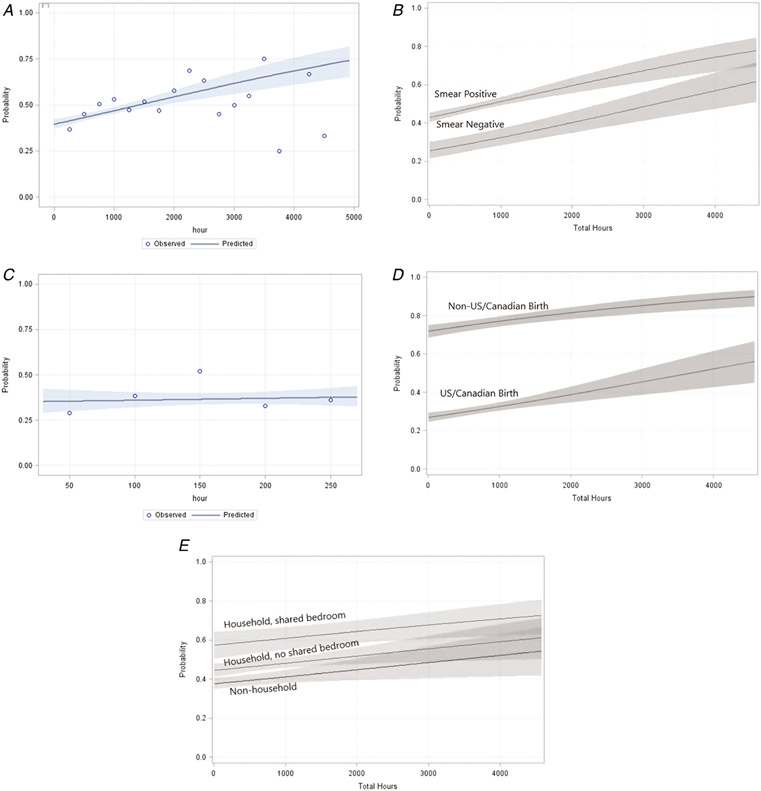
The prevalence of LTBI diagnosis increased with increasing total number of exposure hours, with an incremental increase in prevalence of 8.2% per 250 exposure hours (odds ratio, 1.085; 95% confidence interval, 1.056–1.115; P < .0001) (Figure 1A). The prevalence of LTBI diagnosis was higher for contacts exposed to patients with smear-positive versus smear-negative TB, and LTBI diagnosis prevalence increased with increasing exposure for both groups (Figure 1B). Among contacts with fewer than 250 hours of exposure, the prevalence of LTBI diagnosis was not correlated with exposure hours (odds ratio, 1.024; 95% confidence interval, .930–1.13; P = .63), suggesting that 250 hours of exposure may represent a threshold below which the prevalence of LTBI diagnosis does not vary according to exposure duration (Figure 1C).
Figure 1.
A, Probability of contacts with an LTBI diagnosis by total hours of exposure to an index patient with TB. Observed values are indicated as circles representing the proportion of contacts with LTBI in 250-hour increments (<250 hours, 251–500 hours, 501–750 hours, 751–1000 hours, etc). Denominators for 250-hour increments <2000 hours range from 132 to 899, and denominators for 250-hour increments >2000 hours range from 0 to 64 (denominators for <250, 250–499, 500–749, 750–999, 1000–1249, 1250–1499, 1500–1749, 1750–1999, 2000–2249, 2250–2499, 2500-1749, 2750–2999, 3000–3249, 3250–3499, 3500–3749, 3750–3999, 4000–4249, and 4250–4499 hours are 899, 760, 443, 205, 194, 149, 132, 57, 64, 30, 20, 30, 20, 8, 4, 0, 3, and 6, respectively; exposure hours were missing for 16 contacts). B, Probability of contacts with an LTBI diagnosis by total hours of exposure to an index patient with TB and smear status of the index patient (smear-status positive indicated in red and smear-status negative in blue). C, Probability of contacts with an LTBI diagnosis by total hours of exposure to an index patient with TB for exposure durations <250 hours. Observed values are indicated as circles representing the proportion of contacts with LTBI in 50-hour increments (<50, 51–100, 101–150, 151–200, and 201–250 hours). D, Probability of contacts with LTBI diagnosis by total hours of exposure to an index patient with TB and contact birthplace (US/Canadian birth indicated in blue and non-US/Canadian birth indicated in red). E, Probability of contacts with LTBI diagnosis by total hours of exposure to an index patient with TB and exposure location (nonhousehold in green, shared bedroom in household in red, no shared bedroom in household in blue). Predicted values based on logistic regression modeling of all data points are indicated by the solid lines; the shaded areas represent the 95% confidence intervals. Color figure present online. Abbreviations: BIRTHCONT, contact birthplace; expoEnvir, exposure environment; LTBI, latent tuberculosis infection; TB, tuberculosis.
The prevalence of LTBI diagnosis was higher for non–US/Canadian-born contacts compared with US/Canadian-born contacts, but the prevalence for both groups increased with increasing exposure hours (Figure 1D). Latent tuberculosis infection diagnosis prevalence was highest for household contacts who shared a bedroom with the patient with TB, intermediate for household contacts who did not share a bedroom, and lowest for non–household contacts, and increased with increasing exposure hours for all 3 groups (Figure 1E).
Multivariable Analyses
In multivariable analysis, factors associated with LTBI diagnosis among all close contacts included contact age more than 5 years, male sex, nonwhite race/ethnicity, and foreign birth; index patient positive sputum smear and bilateral disease; household contact; shared bedroom with the index case; and exposure to more than 1 index case (Table 3). In multivariable analysis restricted to household close contacts, factors associated with LTBI diagnosis were similar, but also included 500 or more exposure hours and increasing smear quantity as independent predictors of LTBI diagnosis (data not shown).
Table 3.
Multivariable Analysis of Factors Associated With Latent Tuberculosis Infection Diagnosis Among Close Contacts Screened for Latent Tuberculosis Infection
| Risk Factor | All Close Contacts |
|
|---|---|---|
| Adjusted OR (95% CI) | P | |
| Contact factors | ||
| Age >5 years | 2.8 (2.0, 3.8) | <.001 |
| Male gender | 1.4 (1.1, 1.6) | <.001 |
| Nonwhite race/ethnicity | 1.4 (1.1, 1.8) | .018 |
| Foreign birth | 6.4 (5.3, 7.7) | <.001 |
| Index case factors | ||
| Smear positive | 3.0 (2.3, 3.9) | <.001 |
| Bilateral disease | 1.4 (1.2, 1.7) | <.001 |
| Exposure factors | ||
| Shared bedroom vs nonhousehold | 2.9 (2.1, 3.9) | .001 |
| Different bedroom vs nonhousehold | 1.5 (1.2, 1.8) | <.001 |
| Exposure numbera ≥2 | 2.1 (1.05, 4.1) | .036 |
All factors with a univariate P value <.2 were included. Abbreviations: CI, confidence interval; OR, odds ratio.
Exposure number = number of different index patients with tuberculosis to whom a contact was exposed.
DISCUSSION
In our study, close contacts to persons with infectious TB had a high LTBI prevalence, and there was an incremental increase in LTBI prevalence with increasing hours of exposure. Non–US/Canadian-born contacts had the highest LTBI prevalence (55%) but prevalence was also high among US/Canadian-born contacts (45%). Household contacts had a higher LTBI prevalence (50%) than non–household contacts (39%). Risk factors for LTBI diagnosis identified in our study included factors associated with increased exposure to infectious TB (sharing a bedroom, exposure to >1 index patient, more exposure hours), exposure to patients with TB with more advanced or extensive disease (positive sputum smear, higher smear quantity, and bilateral disease), contact age more than 5 years, male sex, and non-US/Canadian birth. Notably, incremental increases in exposure duration were not associated with increases in LTBI prevalence for contacts with fewer than 250 exposure hours; this suggests that 250 hours may represent a risk threshold below which there is not a dose–response relationship between exposure and LTBI diagnosis, and where there may be a lower likelihood that LTBI diagnosis represents recent transmission. We demonstrate that there is a large LTBI burden among recently exposed contacts, including those with shorter durations of exposure, and that contact investigations provide an important opportunity for LTBI detection and treatment to prevent TB disease. These findings underscore the continued importance of contact investigations as a public health prevention effort to interrupt transmission and also have important implications for efforts to eliminate TB [2-4, 8].
In our study, we demonstrate a statistically significant association between increasing exposure duration and LTBI prevalence, with an incremental prevalence increase of 8.2% per 250 exposure hours. Although the association between increasing hours of exposure to a patient with infectious TB and increasing LTBI prevalence is plausible, this association is not well established, and to our knowledge has never been quantified. Moreover, hours of exposure are not among the data elements commonly collected during health department contact investigations and are not included in algorithms used to prioritize these and other public health interventions [2, 4].
We examined several established factors associated with LTBI diagnosis [2, 3, 9] as well as new risk associations identified in our study with stratification by exposure hours both to control for this major identified factor influencing the likelihood of transmission and to determine the relationship of exposure duration to LTBI diagnosis in exposed contacts without the other identified factors. We found a close correlation between increasing exposure hours and increased LTBI prevalence overall, by index patient smear status, by contact birthplace, and by exposure location. Further, the relationship between exposure duration and higher LTBI prevalence was clearly demonstrated in all strata for each of these analyses. Thus, even though contacts exposed to smear-negative index patients had a lower LTBI prevalence than those exposed to smear-positive patients, LTBI prevalence in smear-negative as well as smear-positive contacts increased with increasing exposure hours. Similarly, although non–US/Canada-born contacts had a higher LTBI prevalence than US/Canada-born contacts at all exposure durations, our findings demonstrate that there was an increasing LTBI prevalence for each of these groups with increasing exposure hours. The same was true for exposure location, with the LTBI prevalence increasing with increasing exposure hours for household contacts sharing a bedroom, household contacts not sharing a bedroom, and non–household contacts. In multivariable analysis, hours of exposure was an independent predictor of LTBI among household contacts but not among all contacts, which may reflect a weaker association in nonhousehold settings. Our findings identify exposure duration as a strong correlate of LTBI diagnosis even in the absence of other established factors associated with LTBI diagnosis. Based on our findings, exposure time is a key component of the likelihood of LTBI diagnosis and should be factored into algorithms stratifying the likelihood of LTBI diagnosis and decisions on prioritization within contact investigations.
Health departments have sought to define a practical cutoff for determining the minimum duration of contact required for transmission to occur [2]. Our definition for close contact included either high exposure rates (>15 hours) in 1 or more weeks or high total exposure (>180 hours) during the index patient’s infectious period. Although many contacts met both criteria, some had intensive exposures in only 1 or 2 weeks during the infectious period, and thus had fewer than 180 exposure hours. Many contacts with high rates but low total number of exposure hours were household members who were present for some but not all of the infectious period; friends or relatives who visited a household intermittently for a few days and/or a few nights but did not reside there permanently; and some social site, workplace, and school contacts. We recognized the opportunity to look at smaller increments of exposure within the group of contacts with fewer total hours to see if we could define a threshold below which there was no association with LTBI diagnosis. Because of the distribution of the data (with one-quarter of all contacts having <250 exposure hours), the use of 250-hour increments for the main exposure analysis, and to facilitate practical application of results, we opted to use fewer than 250 hours as the cutoff to define the lowest exposure category and examined 50-hour exposure increments within this group. Our findings demonstrate that, in contrast to longer exposure durations, LTBI prevalence was not correlated with exposure durations of fewer than 250 hours. This suggests that 250 exposure hours may represent a threshold below which there is a lower risk of transmission and a higher likelihood that LTBI diagnosis represents baseline prevalence rather than recent transmission.
Although LTBI prevalence was considerably lower among persons with fewer than 250 hours of exposure, it was not zero even among those with the lowest exposure duration (<50 hours). Thus, our data suggest that 250 hours may be a useful threshold below which contacts are at a lower transmission risk but do not identify a cutoff below which there is no risk of LTBI. Based on these findings, it may be useful for health departments to estimate exposure hours for each contact and factor this information into algorithms to establish the likelihood of LTBI diagnosis and priority for investigation. It should be emphasized, however, that the LTBI prevalence of more than one-third, which we observed among contacts with fewer than 250 hours of exposure, suggests that this population would benefit from LTBI screening and treatment regardless of the degree to which it could reflect baseline prevalence versus recent transmission.
Exposure to patients with TB with more advanced or extensive disease was strongly associated in our multivariable analyses with contact LTBI diagnosis. Contacts exposed to patients with TB with positive sputum smears for acid-fast bacilli had a higher LTBI prevalence than those exposed to patients with smear-negative TB. Chest radiograph cavitation, bilateral disease, and more diseased lobes were also strongly correlated with higher LTBI rates. Chest radiograph cavitation and positive sputum smears are well-known risk factors for transmission [2, 3, 9]. Although very plausible, our demonstration that the LTBI prevalence increases with increasing smear quantity is less well established, with conflicting results reported in the literature [9-11]. Our findings correlating the number of diseased lobes with LTBI prevalence identifies another logical but less well-recognized factor correlated with LTBI diagnosis. In a study conducted in West Africa, no correlation between the number of diseased lobes and LTBI prevalence was found in multivariable analysis [9, 10]. Bilateral disease, a multivariate correlate of LTBI prevalence in our study, is simpler and perhaps operationally more practical as a predictor of LTBI diagnosis than the number of diseased lobes. These findings have practical implications for defining settings where there is a high risk of M. tuberculosis transmission based on index patient clinical characteristics.
In contrast to the well-established high risk of TB disease among young children [5, 6, 12, 13], contacts 15 years of age or older had a higher likelihood of LTBI diagnosis than younger contacts, which is consistent with most but not all previous studies [9]. It is possible that children had less exposure to ill patients with TB than adults and were thus at a lower risk of LTBI, or that they had a lower risk of prior exposure to TB. It is also possible that some of the positive TSTs in older patients could represent the booster phenomenon. In our study the likelihood of LTBI diagnosis in all age groups was considerably higher than background rates expected in the community [14]; however, diagnosis did not increase linearly with age across adult age groups, thus suggesting that contacts with LTBI in our study population acquired infection from recent exposure.
Non-US/Canadian birth was associated in our study with an increased likelihood of LTBI diagnosis compared with persons born in the United States or Canada (76% vs 31%). In contrast, the difference between these 2 groups in recent population-based prevalence surveys was 20.5% versus 1.5% [14]. The higher proportion of persons with a positive TST in this study supports the hypothesis that most of the LTBI observed in this study (in both groups of participants) was due to recent M. tuberculosis transmission. The increased prevalence of a positive TST in non–US/Canada-born populations was due, in part, to receipt of Bacillus Calmette Guérin, but not solely for this reason.
In our study, LTBI prevalence varied by exposure location, with higher LTBI prevalence among household than non–household contacts. Notably, household contacts who did not share a bedroom with the index patient still had a higher LTBI prevalence than non–household contacts. These findings suggest the possibility that the environment where exposure occurs plays a role in the likelihood of LTBI diagnosis. A possible explanation is that household contacts may have greater exposure proximity to the index patient than those in other locations even if they do not share a bedroom, or that there could be a greater degree of crowding in household settings. Despite the lower LTBI prevalence in nonhousehold settings demonstrated in our study, investigation of nonhousehold settings remains important since 32% of all LTBI diagnoses in our study (451/1390 contacts with LTBI) and as much as 50–80% of all M. tuberculosis transmission in other reports are estimated to occur outside the household [15-17].
In our study, approximately half of all contacts were identified in an index patient interview. The remaining contacts were identified by other clinical or health department staff or by other contacts. We observed a difference in the LTBI likelihood based on the source of contact identification, with LTBI diagnosis more frequent among contacts identified by the index patient. This difference was most notable in nonhousehold settings. These findings underscore the importance of theinterview with the patient with TB [2, 4] for identifying contacts with the highest likelihood of exposure and LTBI diagnosis.
Incomplete human immunodeficiency virus (HIV) testing data, precluding our ability to evaluate the association between HIV and LTBI prevalence, and self-reported contact variable data were study limitations. The collection of index TB patient clinical and radiographic variables as well as contact screening results from medical records, large number of contacts included, the prospective and protocol-driven nature of data collection, and ability to prospectively collect information on many epidemiologic factors, including exposure hours, were study strengths.
In conclusion, our prospective study provides important new information on rates and factors associated with LTBI diagnosis in contacts of patients with infectious TB. Index patient, contact, and environmental factors were associated with LTBI prevalence, with a close correlation between exposure hours and LTBI prevalence for exposure durations of 250 hours or more. Our findings support the important role of contact investigation as a means of identifying and treating large numbers of persons with LTBI who are at high risk of developing TB disease [2, 3, 5, 6, 18]. We identify several new factors associated with LTBI diagnosis that may be useful to help inform health department decisions on prioritizing settings and high-risk contacts within each setting during contact investigations. Since recently exposed close contacts with a new LTBI diagnosis are at high risk of rapidly progressing to TB disease [5, 19], and LTBI treatment in contacts has been associated with a substantial decrease in TB risk, [5, 6, 19, 20], these findings have important implications for TB prevention and elimination efforts [2, 4, 8].
Acknowledgments.
The authors thank T. Navin and A. Vernon for helpful guidance and input into scientific and administrative aspects of the project.
Financial support.
This work was supported by the Centers for Disease Control and Prevention (contract numbers 200-2001-00087/0002, 200-2001-00078/0002, 200-2001-00076/0002, 200-2001-00086/0002, 200-2001-00093/0002, 200-2001-00094/0002, 200-2001-00083/0002, and 200-2001-00077/0002).
Disclaimer.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Appendix
Task Order 2 Team. The Tuberculosis Epidemiologic Studies Consortium Task Order 2 study sites, investigators, and study coordinators are as follows: Arkansas Department of Health, Little Rock, Arkansas (I. Bakhtawar, C. LeDoux); Respiratory Health Association of Metropolitan Chicago and Rush University (J. McAuley, J. Beison); University of British Columbia (M. Fitzgerald, M. Naus, M. Nakajima); Columbia University (N. Schluger, Y. Hirsch-Moverman, J. Moran); Emory University (H. Blumberg, J. Tapia, L. Singha); University of Manitoba (E. Hershfeld, B. Roche); New Jersey Medical School National Tuberculosis Center (B. Mangura, A. Sevilla); Vanderbilt University and Tennessee Department of Health (T. Sterling, T. Chavez-Lindell, F. Maruri); and Maryland Department of Health, Baltimore, Maryland (S. Dorman, W. Cronin, E. Munk). The Centers for Disease Control and Prevention Task Order 2 data management team is as follows: A. Khan, Y. Yuan, B. Chen, F. Yan, Y. Shen, H. Zhao, H. Zhang, P. Bessler, M. Fagley, and M. Reichler. The Task Order 2 protocol team is as follows: M. Reichler (Chair), T. Sterling (Co-chair), J. Tapia, C. Hirsch, and C. Luo.
Footnotes
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Horsburgh CR Jr, Rubin EJ. Clinical practice. Latent tuberculosis infection in the United States. N Engl J Med 2011; 364:1441–8. [DOI] [PubMed] [Google Scholar]
- 2.Guidelines for the investigation of contacts of persons with infectious tuberculosis: recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Morb Mortal Wkly Rep 2005; 54(RR-15):1–37. [PubMed] [Google Scholar]
- 3.Reichler MR, Reves R, Bur S, et al. ; Contact Investigation Study Group. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA 2002; 287:991–5. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Recommendation for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries. Geneva, Switzerland: World Health Organization; 2012. Publication no. WHO/HTM/TB/2012.9. [PubMed] [Google Scholar]
- 5.Reichler MR, Khan A, Sterling TR, et al. ; Tuberculosis Epidemiologic Studies Consortium Task Order 2 Team. Risk and timing of tuberculosis among close contacts of persons with infectious tuberculosis. J Infect Dis 2018; 218:1000–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reichler MR, Khan A, Sterling TR, et al. ; Tuberculosis Epidemiologic Studies Consortium Task Order 2 Team. Risk factors for tuberculosis and effect of preventive therapy among close contacts of persons with infectious tuberculosis. Clin Infect Dis 2020; 70:1562–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katz D, Albalak R, Wing JS, Combs V; Tuberculosis Epidemiologic Studies Consortium. Setting the agenda: a new model for collaborative tuberculosis epidemiologic research. Tuberculosis (Edinb) 2007; 87:1–6. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Ending neglect: the elimination of tuberculosis in the United States. Washington, DC: National Academies Press, 2000. [PubMed] [Google Scholar]
- 9.Melsew YA, Doan TN, Gambhir M, Cheng AC, McBryde E, Trauer JM. Risk factors for infectiousness of patients with tuberculosis: a systematic review and meta-analysis. Epidemiol Infect 2018; 146:345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lienhardt C, Fielding K, Sillah J, et al. Risk factors for tuberculosis infection in sub-Saharan Africa: a contact study in The Gambia. Am J Respir Crit Care Med 2003; 168:448–55. [DOI] [PubMed] [Google Scholar]
- 11.Lienhardt C, Sillah J, Fielding K, et al. Risk factors for tuberculosis infection in children in contact with infectious tuberculosis cases in the Gambia, West Africa. Pediatrics 2003; 111:e608–14. [DOI] [PubMed] [Google Scholar]
- 12.Sloot R, Schim van der Loeff MF, Kouw PM, Borgdorff MW. Risk of tuberculosis after recent exposure: a 10-year follow-up study of contacts in Amsterdam. Am J Respir Crit Care Med 2014; 190:1044–52. [DOI] [PubMed] [Google Scholar]
- 13.Marais BJ, Gie RP, Schaaf HS, et al. The natural history of childhood intrathoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis 2004; 8:392–402. [PubMed] [Google Scholar]
- 14.Miramontes R, Hill AN, Yelk Woodruff RS, et al. Tuberculosis infection in the Untied States: prevalence estimates from the National Health and Nutrition Examination Survey, 2011–2012. PLoS One 10: e0140881. Available at: 10.1371/journal.pone.0140881. Accessed 30 July 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez L, Shen Y, Mupere E, Kizza A, Hill PC, Whalen CC. Transmission of Mycobacterium tuberculosis in households and the community: a systematic review and meta-analysis. Am J Epidemiol 2017; 185:1327–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verver S, Warren RM, Munch Z, et al. Proportion of tuberculosis transmission that takes place in households in a high-incidence area. Lancet 2004; 363:212–4. [DOI] [PubMed] [Google Scholar]
- 17.Martinez L, Lo NC, Cords O, et al. Paediatric tuberculosis transmission outside the household: challenging historical paradigms to inform future public health strategies. Lancet Respir Med 2019; 7:544–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 2008; 8:359–68. [DOI] [PubMed] [Google Scholar]
- 19.Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Adv Tuberc Res 1969; 17:29–106. [PubMed] [Google Scholar]
- 20.Fiske CT, Yan F-X, Hirsch-Moverman Y, Sterling TR, Reichler MR; Tuberculosis Epidemiologic Studies Consortium Task Order 2 Team. Risk factors for treatment default in close contacts with latent tuberculosis infection. Int J Tuberc Dis 18:421–7. [DOI] [PMC free article] [PubMed] [Google Scholar]