Abstract
Background
Sodium intake in China is extremely high and eating in restaurants is increasingly popular. Little research has explored the sodium level of restaurant dishes. The present study aims to assess the content and sources of sodium in Chinese restaurants.
Methods
Cross-sectional data were obtained from the baseline survey of the Restaurant-based Intervention Study (RIS) in 2019. A total of 8131 best-selling restaurant dishes with detailed recipes from 192 restaurants in China were included. Sodium content per 100 g and per serving were calculated according to the Chinese Food Composition Table. The proportion of restaurant dishes exceeding the daily sodium reference intake level in a single serving and the major sources of sodium were determined.
Results
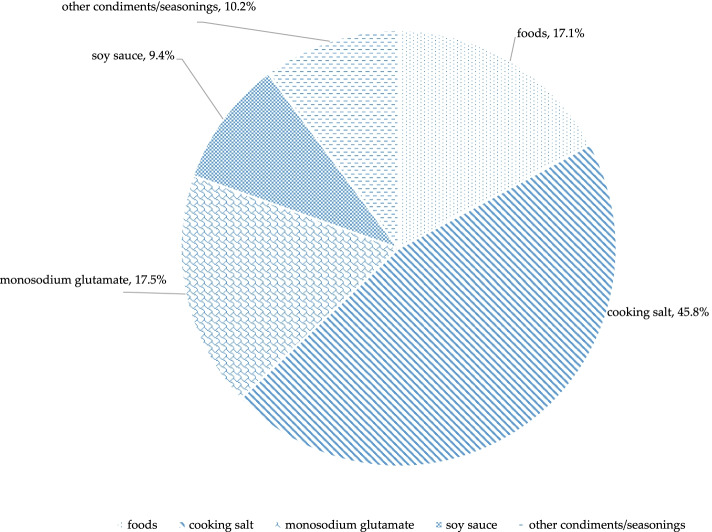
Median sodium content in restaurant dishes were 487.3 mg per 100 g, 3.4 mg per kcal, and 2543.7 mg per serving. For a single serving, 74.9% of the dishes exceeded the Chinese adults’ daily adequate intake for sodium (AI, 1500 mg per day), and 62.6% of dishes exceeded the proposed intake for preventing non-communicable chronic diseases (PI, 2000 mg per day). Cooking salt was the leading source of sodium in Chinese restaurant dishes (45.8%), followed by monosodium glutamate (17.5%), food ingredients (17.1%), soy sauce (9.4%), and other condiments/seasonings (10.2%). More types of salted condiments/seasonings use were related to higher sodium level.
Conclusions
The sodium levels in Chinese restaurant dishes are extremely high and variable. In addition to cooking salt, other salted condiments/seasonings also contribute a large proportion of sodium. Coordinated sodium reduction initiatives targeting the main sources of sodium in restaurant dishes are urgently needed.
Keywords: Sodium, Restaurant, China
Background
High sodium intake is a public health concern worldwide, as it is linked to elevated blood pressure, which leads to cardiovascular disease [1–3]. In 2010, the global mean level of sodium intake was 3950 mg/day, nearly twice the World Health Organization (WHO) recommendation of 2000 mg/day [4, 5]. The Global Burden of Disease Study showed that 3 million deaths were attributable to the high salt intake in 2017 and about half of these deaths occurred in China [1]. East Asia is one of the regions with the highest sodium intake in the world [4]. According to the China National Nutrition and Health Surveillance (CNNHS) 2010–2012, Chinese adults consume 5013 mg/day of sodium on average, much higher than both the WHO and Chinese recommendations [6, 7]. High sodium intake is the leading risk factor for cardiometabolic mortality in China (population attributable fraction (PAF) of 17.3%) [8]. To tackle the adverse effects of high sodium consumption, many countries have implemented salt reduction strategies in recent years [9–12].
A national target of 20% reduction in salt intake by 2030 has been proposed in China’s health development agenda “Healthy China 2030” [13]. Determining local sodium intake levels and the main dietary contributors to sodium intake is critical to develop an effective sodium reduction strategy. In high-income countries, where the majority of the sodium consumed comes from processed foods, efforts focus on reducing the amount of salt added by the food industry, through setting incrementally lower salt targets for specific food categories [14, 15]. In China, salt added when cooking/preparing food is the leading source of sodium (69.2% of sodium intake), followed by soy sauce (8.2%), processed foods (6.0%), and chicken essence (4.5%) [6]. However, the above findings were obtained from the national nutrition and health survey, which did not include salt and condiment use in foods consumed away from home, which may have resulted in an underestimate of the total sodium intake [16]. Restaurant dishes have a higher sodium level than home-made foods [16], thus eating out is reported to be associated with higher intake of sodium [17, 18]. Besides their high sodium content, restaurant foods also are characterized by the use of salt substitutes and flavor enhancers [19], indicating different sources of sodium compared with home-made dishes. With rapid urbanization and economic development, the contribution of restaurant foods to the population’s sodium intake is increasing [20]. To achieve the sodium reduction goals, considerable efforts should thus be taken to reduce the amount of sodium added to restaurant foods [21].
“Action on Salt China” (ASC) is a unit for salt reduction, established in June 2017, in collaboration with Queen Mary University of London in the United Kingdom, The George institute for Global Health in China, the Chinese Center for Disease Control and Prevention, and other key national organizations [22]. The ASC program consists of four randomized controlled trials (RCTs), targeting various sources of salt intake in China. As one of the RCTs in ASC, the restaurant-based intervention study (RIS) is designed to test the feasibility and effectiveness of a package of interventions for salt reduction in 192 restaurants from 6 provinces of China. The present article describes the baseline data of RIS to determine the sodium content and sources in popular restaurant dishes in China, which will be helpful in developing effective strategies to reduce salt in restaurant foods.
Methods
Study design
The RIS baseline assessment survey was carried out in 6 provinces of China (Qinghai, Hebei, Heilongjiang, Hunan, Sichuan and Jiangxi) in May 2019. For each province, 2 counties of similar socioeconomic level were selected in the provincial capital city. Then, according to the selection criteria, 16 restaurants mainly offering Chinese cuisine were selected from each county, including 4 large-size, 8 medium-size and 4 small-size restaurants [23]. The detailed recipes of the 50 best-selling dishes from each restaurant were collected by trained investigators. For restaurants offering fewer than 50 dishes in their menu, all the dishes were included.
Characteristics of restaurant dishes
To understand how sodium levels vary according to different characteristics of the restaurant dishes, we conducted our analyses by region, restaurant size and dish type. Region was defined as North (Qinghai, Hebei and Heilongjiang) and South (Hunan, Sichuan and Jiangxi). Restaurant size was classified into large (surface area > 500 m2 and ≤ 3000 m2, or number of seats > 250 and ≤ 1000), medium (surface area > 150 m2 and ≤ 500 m2, or number of seats > 75 and ≤ 250) and small (surface area ≤ 150 m2, or number of seats ≤75). Chinese cuisine substantially varied across geography areas, and was categorized into four types of dishes based on the cooking method: cold dish, fried dish, soup, and staples/snacks.
Assessment of sodium content
A mobile-based electronic data collection system (EDC) developed by the Beijing University of Aeronautics and Astronautics was used for data collection. The recipes were collected by in-depth interviews with chefs who were familiar with the preparation and cooking of the dishes. The detailed recipes included the following information: name of the dish, edible percentage, ingredients and condiments/seasonings used (with amounts), dish type and cooking method. To improve the accuracy of the estimated amount of condiments/seasonings used, the investigators showed the weighed amount using a usual spoon or other measuring instruments during the interview. Sodium content of each dish was calculated according to the Chinese Food Composition Table, combining the sodium content of all ingredients and condiments/seasonings used for the dish. Sodium content is reported as sodium density (mg per 100 g, mg per kcal), as well as sodium (mg) per serving.
Comparison to the Chinese dietary reference intakes (DRIs)
Sodium levels in a single serving of the restaurant dishes were compared to the Chinese DRIs: the daily AI (adequate intake, 1500 mg per day) and PI (proposed intakes for preventing non-communicable chronic diseases, 2000 mg per day) for adults aged 18 to 49 years old. Restaurant dishes were compared to the Chinese DRIs because restaurant sodium reduction targets have not been established in China. The proportions of restaurant dishes exceeding the daily sodium AI and PI in a single serving were calculated.
Assessment of sodium sources
Based on the recipes, we classified the sources of sodium in restaurant dishes (according to the following categories: food ingredients, cooking salt, monosodium glutamate (including chicken powder and chicken essence), soy sauce, and other condiments/seasonings. We then estimated their respective contribution (in percentages) to sodium levels in dishes.
Statistical analysis
We reported the median and interquartile range (IQR) for mg of sodium per 100 g, mg of sodium per kcal, and mg of sodium per serving in restaurant dishes, by region (North, South), restaurant size (large, medium and small), and dish type (cold dish, fried dish, soup and staples/snacks). Descriptive statistics for restaurant dishes, including %AI (sodium per serving divided by 1500 mg), and % of restaurant dishes exceeding the daily sodium AI and PI were conducted. The respective contributions of the main sources of sodium to total sodium content in restaurant dishes were calculated. As sodium values were not normally distributed, the non-parametric Wilcoxon signed-rank test was used to compare the median of sodium content among restaurant dishes stratified by area, restaurant size and dish type. We used SAS 9.4 (SAS Institute, Cary, NC) for data cleaning and analyses, and considered two-sided P < 0.05 as statistically significant.
Results
Sodium density and level in popular restaurant dishes in China
The analysis included a total 8131 dishes from 192 restaurants in 6 provinces of China. The sample encompassed 3829 (47.1%) and 4302 (52.9%) foods from the North and the South, and 2285 (28.1%), 4162 (51.2%) and 1684 (20.7%) foods from large, medium and small restaurants, respectively. The main dish type was fried dish (83.9%), followed by cold dish (11.7%), soup (3.0%) and staples/snacks (1.4%).
Overall, the restaurant dishes contained on average 487.3 (IQR: 291.1, 781.9) mg sodium per 100 g. Sodium levels varied significantly by area, restaurant size, and dish type (Table 1). The highest sodium densities (in mg per 100 g) were found in dishes from the South (566.3 mg per 100 g), in medium (497.5 mg per 100 g) and small (491.3 mg per 100 g) restaurants, and in soups (687.0 mg per 100 g), cold dishes (528.4 mg per 100 g) and fried dishes (480.9 mg per 100 g). Sodium density in mg per kcal showed similar trends, with an average of 3.4 (1.9, 6.4) mg of sodium per kcal. The dishes with the highest sodium density per kcal were from the South (3.6 mg), from medium (3.5 mg) and large (3.4 mg) restaurants, and in cold dishes (4.8 mg), soups (4.3 mg) and fried dishes (3.3 mg).
Table 1.
Sodium levels in Chinese restaurant dishes
| N | Sodium (mg) per 100 g | Sodium (mg) per kcal | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Median | P25 | P75 | P value | Median | P25 | P75 | P value | ||
| Region | |||||||||
| North | 3829 | 415.7 | 250.7 | 682.8 | < 0.0001 | 3.2 | 1.7 | 6.1 | < 0.0001 |
| South | 4302 | 566.3 | 337.9 | 858.4 | 3.6 | 2.0 | 6.5 | ||
| Restaurant size | |||||||||
| Large | 2285 | 466.1 | 278.1 | 763.3 | 0.0286 | 3.4 | 1.8 | 6.7 | 0.0006 |
| Medium | 4162 | 497.5 | 297.7 | 798.0 | 3.5 | 1.9 | 6.5 | ||
| Small | 1684 | 491.3 | 302.1 | 767.1 | 3.1 | 1.8 | 5.7 | ||
| Dish type | |||||||||
| Cold dish | 950 | 528.4 | 292.1 | 898.4 | < 0.0001 | 4.8 | 2.1 | 10.3 | < 0.0001 |
| Fried dish | 6819 | 480.9 | 291.1 | 762.3 | 3.3 | 1.9 | 6.0 | ||
| Soup | 246 | 687.0 | 409.6 | 1143.3 | 4.3 | 2.3 | 9.3 | ||
| Staples/snacks | 116 | 278.4 | 40.1 | 541.6 | 1.1 | 0.2 | 2.3 | ||
| Total | 8131 | 487.3 | 291.1 | 781.9 | 3.4 | 1.9 | 6.4 | ||
Sodium levels per serving of restaurant dishes and comparison with Chinese dietary reference intakes
Table 2 shows serving size, sodium (mg) per serving, %AI, and proportions of restaurant dishes exceeding the daily sodium AI (1500 mg) and PI (2000 mg) by categories. The average serving size was 575.6 ± 318.0 g, providing 3331.2 ± 4156.9 mg sodium per serving, which represents 222.1% of the AI. Overall, 74.9% of the restaurant dishes exceeded Chinese adults’ daily sodium AI, and 62.6% of the dishes exceeded the adults’ PI. Dishes from the North, from large and medium restaurants, and belonging to the categories of fried dishes and soups had larger serving sizes and higher sodium levels (mg) per serving. In some instances, the higher sodium level per serving was mainly due to higher sodium density, such as in the South, in small restaurants and in cold dishes, while in other instances, it was due to larger serving sizes, such as in the North, in large restaurants, and in staples/snacks, or due to the combination of both serving size and sodium density, such as in medium restaurants, in fried dishes and soups.
Table 2.
Sodium levels per serving of restaurant dishes in China, compared to the dietary reference intakes (DRIs)
| N | Mean serving size (g) | Sodium (mg) levels per serving | % of dishes exceeding the sodium DRIs levels b | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | %AI a | Median | P25 | P75 | AI: 1500 mg | PI: 2000 mg | ||
| Region | |||||||||||
| North | 3829 | 620.0 | 340.2 | 3270.2 | 4849.9 | 218.0 | 2345.5 | 1409.3 | 3734.5 | 72.1 | 58.9 |
| South | 4302 | 536.1 | 291.2 | 3385.5 | 3423.7 | 225.7 | 2759.3 | 1596.3 | 4220.1 | 77.4 | 65.9 |
| Restaurant size | |||||||||||
| Large | 2285 | 611.4 | 377.9 | 3447.0 | 4774.4 | 229.8 | 2604.3 | 1527.5 | 4040.7 | 75.7 | 63.8 |
| Medium | 4162 | 576.4 | 291.3 | 3397.6 | 4219.8 | 226.5 | 2642.6 | 1579.3 | 4081.5 | 76.7 | 64.1 |
| Small | 1684 | 525.0 | 283.6 | 3010.1 | 2894.8 | 200.7 | 2283.6 | 1368.8 | 3901.9 | 69.5 | 57.4 |
| Dish type | |||||||||||
| Cold dish | 950 | 426.6 | 237.2 | 2975.5 | 4540.7 | 198.4 | 2018.3 | 1091.0 | 3251.5 | 62.3 | 50.5 |
| Fried dish | 6819 | 598.9 | 317.3 | 3356.1 | 3887.3 | 223.7 | 2614.1 | 1575.8 | 4082.2 | 76.9 | 64.4 |
| Soup | 246 | 574.0 | 357.3 | 4805.4 | 8190.7 | 320.4 | 3373.0 | 2112.2 | 4852.2 | 85.8 | 77.6 |
| Staples/snacks | 116 | 431.3 | 454.6 | 1653.1 | 2011.6 | 110.2 | 934.7 | 107.6 | 2354.3 | 36.2 | 27.6 |
| Total | 8131 | 575.6 | 318.0 | 3331.2 | 4156.9 | 222.1 | 2543.7 | 1496.9 | 4030.9 | 74.9 | 62.6 |
AI Adequate intake, DRI Dietary reference intakes, PI, PI-NCD Proposed intake for preventing non-communicable chronic diseases
aMean sodium levels per serving, expressed as a percentage of the daily AI for adults (1500 mg per day)
bPercentage of dishes in the groups that exceed the daily AI (1500 mg per day) or PI (2000 mg per day) per serving
Sodium sources in restaurant dishes in China
Overall, cooking salt was the leading source of sodium in Chinese restaurant dishes, accounting for 45.8% of the sodium (Fig. 1). Monosodium glutamate was the second contributor (17.5%), followed by food ingredients (17.1%), soy sauce (9.4%), and other condiments/seasonings (10.2%). Beside the sodium already contained in the food ingredients, the majority (82.9%) of the sodium came from the use of salted condiments/seasonings added while cooking. However, cooking salt only contributed to less than half of the sodium contained in restaurant dishes. Monosodium glutamate, soy sauce and other condiments/seasonings (such as other sauces and compound condiments/seasonings) contributed to more than a third of total sodium content in restaurant dishes.
Fig. 1.
Sodium sources of restaurant dishes in China
Condiments/seasonings use and association with sodium level in Chinese restaurant dishes
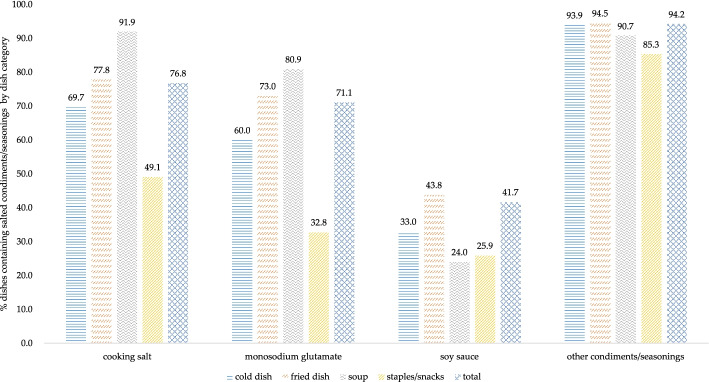
Figure 2 shows the proportion of restaurant dishes containing the main sources of sodium, by dish type. Overall, 76.8% of the dishes contained cooking salt, 71.1% contained monosodium glutamate and 41.7% contained soy sauce. Other condiments/seasonings were found in most (94.2%) restaurant dishes. Cooking salt was a major source of sodium in all type restaurant dishes, especially in soups (91.9%) and fried dishes (77.8%). Monosodium glutamate was more often used in soups (80.9%) and fried dishes (73.0%), followed by cold dishes (60.0%). Soy sauce was found in 43.8% of the fried dishes and 33.0% of the cold dishes. In staples/snack, prevalence of condiments/seasonings was below 50%, except for that of other condiments/seasonings.
Fig. 2.
Percentage of restaurant dishes containing salted condiments/−seasonings by dish category in China
Among all dishes included, nearly half (45.1%) contained 3 types of salted condiments/seasonings, followed by those containing 2 types (24.2%) and those containing 4 types (23.3%) condiments/seasonings (Table 3). Only 7.4% of foods only contained 1 type of salted condiments/seasonings. Dishes from the South, from small restaurants and categorized as fried dishes were more likely to contain all 4 types of salted condiments/seasonings. Generally, foods that contained more types of condiments/seasonings were significantly more likely to have a higher sodium level than those that contained fewer types of salted condiments/seasonings. This trend was seen in all subgroups, and the difference was significant (P < 0.0001). The median sodium level (mg) per 100 g in foods with 4 types of condiments/seasonings (644.4 mg per 100 g) was 4.8 times that of foods with 1 type of condiments/seasonings (134.8 mg per 100 g), 1.7 times of those with 2 types (380.7 mg per 100 g), 1.3 times of those with 3 types (506.4 mg per 100 g).
Table 3.
Sodium level in Chinese restaurant dishes by types of salted condiment/seasonings used(N = 8131)
| P value* | Number of salted condiment/seasonings types useda | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 type used | 2 types used | 3 types used | 4 types used | ||||||||||||||
| % | sodium (mg) per 100 g | % | sodium (mg) per 100 g | % | sodium (mg) per 100 g | % | sodium (mg) per 100 g | ||||||||||
| Median | P25 | P75 | Median | P25 | P75 | Median | P25 | P75 | Median | P25 | P75 | ||||||
| Region | |||||||||||||||||
| North | < 0.0001 | 8.8 | 113.2 | 29.9 | 396.4 | 22.0 | 342.1 | 191.9 | 539.2 | 49.1 | 445.5 | 290.8 | 713.2 | 20.1 | 500.6 | 346.6 | 783.8 |
| South | 6.2 | 146.2 | 43.9 | 488.8 | 26.1 | 408.0 | 259.6 | 705.6 | 41.6 | 578.9 | 370.1 | 911.0 | 26.1 | 704.3 | 533.2 | 998.9 | |
| Restaurant size | |||||||||||||||||
| Large | < 0.0001 | 8.9 | 138.2 | 38.0 | 432.0 | 21.9 | 344.0 | 214.6 | 538.1 | 45.4 | 481.2 | 303.4 | 797.1 | 23.8 | 648.7 | 429.7 | 917.5 |
| Medium | 7.3 | 121.7 | 30.6 | 455.9 | 24.9 | 399.2 | 235.3 | 646.2 | 45.2 | 527.6 | 335.5 | 827.9 | 22.7 | 644.4 | 432.7 | 934.0 | |
| Small | 5.9 | 138.7 | 35.6 | 405.8 | 25.7 | 386.2 | 234.5 | 666.3 | 44.5 | 486.7 | 317.0 | 763.0 | 24.0 | 640.3 | 444.8 | 901.4 | |
| Dish type | |||||||||||||||||
| Cold dish | < 0.0001 | 15.1 | 139.4 | 36.0 | 479.9 | 25.1 | 470.2 | 272.9 | 709.2 | 47.3 | 615.4 | 372.4 | 970.3 | 12.6 | 729.6 | 414.6 | 1191.6 |
| Fried dish | 5.8 | 145.1 | 48.6 | 456.6 | 24.3 | 367.4 | 221.8 | 598.5 | 44.9 | 486.7 | 313.3 | 764.4 | 25.1 | 637.8 | 432.8 | 898.5 | |
| Soup | 5.3 | 73.7 | 21.4 | 309.7 | 22.0 | 667.0 | 401.1 | 1141.9 | 52.4 | 696.4 | 388.2 | 1239.0 | 20.3 | 791.3 | 572.8 | 1118.6 | |
| Staples/snacks | 48.3 | 39.5 | 5.3 | 178.1 | 14.7 | 393.0 | 276.7 | 554.7 | 24.1 | 507.0 | 360.8 | 777.6 | 12.9 | 461.1 | 301.8 | 777.4 | |
| Total | < 0.0001 | 7.4 | 134.8 | 35.9 | 441.6 | 24.2 | 380.7 | 228.3 | 630.7 | 45.1 | 506.4 | 321.6 | 810.0 | 23.3 | 644.4 | 436.6 | 919.7 |
aTypes of salted condiments/seasonings include: cooking salt, monosodium glutamate, soy sauce, and other condiments/seasoning
* Non-parametric Wilcoxon signed-rank tests of the sodium levels between different category amounts groups of salted condiment/seasonings
Discussion
Commercially processed and restaurant foods are the main contributors for sodium intake in most high-income countries, e.g. the UK, USA [14, 24]. Although most sodium consumed in the Chinese population still mainly comes from salt and other salted condiments/seasonings added during cooking [6], there has been a rapid increase in the consumption of foods outside the home in the past decades. As such, reducing sodium in the out-of-home sector plays in increasingly important role for China to achieve the salt reduction targets by 2030.
Main findings
Taking into account both the high sodium level in restaurant dishes and the increasing popularity of eating out, restaurant dishes are becoming increasingly important contributors to sodium intake in China. However, data on the sodium content of restaurant dishes in China is limited. The current study describes the sodium density and sodium content per serving, as well as sources of sodium in 8131 popular restaurant dishes from six provinces in China. Our results show that both the average level of sodium per 100 g and sodium level per serving are extremely high in Chinese restaurant dishes, with significant variations by region, restaurant size and dish type. On average, a single serving of a restaurant dish provided almost 2.2 times the daily recommended AI for sodium for Chinese adults. Sodium levels per serving in 74.9 and 62.6% of restaurant dishes exceeded the Chinese daily recommended AI (1500 mg) and PI (2000 mg), respectively.
Comparison with other studies
Our findings of the very high and wide-ranging sodium levels in restaurant dishes are in agreement with those reported in several other studies [25–28]. Such high sodium levels of restaurant foods are attributed to either large serving sizes or high sodium density, or the combination of both depending on dish type [25]. In our study, the higher sodium level per serving in restaurant dishes, in some instances, was mainly due to higher sodium density, such as in the South, in small restaurants, and in cold dishes, while in other instances, it was mainly due to larger serving sizes, such as in the North, in large restaurants, and in staples/snacks, or due to the combination of both serving size and sodium density, such as in medium restaurants, and in fried dishes and soups. These differences may imply that specific sodium reduction strategies for restaurant dishes are needed in different situations.
Widespread use of salted condiments/seasonings is another explanation for the high sodium content in restaurant dishes. In leading Canadian chain restaurants, more than 60% of the dishes contained a salt substitute/enhancer, such as yeast extracts, calcium chloride, monosodium glutamate and potassium chloride [19]. In our study, salted condiments/seasonings contributed to 82.9% of the sodium found in restaurant dishes (37.1% if excluding cooking salt). This makes sodium sources in Chinese restaurant dishes more complex and diversified. With increasing development of compound condiments/seasonings, restaurant chefs prefer to add several kinds of flavorings rather than cooking salt only. We observed that more than two thirds of the restaurant dishes contained three or four types of salted condiments/seasonings. Sodium density of the dishes increased as more types of condiments/seasonings were used due to most of these condiments being produced by the food industry, effective sodium reduction in restaurants will also require cooperation with food manufacturers [29, 30].
Implications
Many countries have implemented national or regional initiatives for sodium reduction in restaurants [9, 31–35], mainly including: menu labelling, setting sodium targets by food category, reformulation, raising consumer awareness, chef training, and promotional materials delivery. However, there are many potential barriers to reducing sodium content in restaurant dishes. The nutritional monitoring of restaurant dishes has shown that sodium levels continue to be high and the changes in sodium levels vary by food categories, with reductions only seen in a minority of the sampled foods [26, 27]. More effective sodium reduction strategies with multi-stakeholders’ cooperation are needed.
In China, cooking habits and consumers’ preferred taste make sodium reduction difficult in restaurant foods. However, attempts to explore effective sodium reduction strategies for restaurant in China have been made [36]. The RIS program, part of Action on Salt China (ASC), aims to determine the sodium level of restaurant dishes and evaluate the effectiveness of a comprehensive restaurant salt reduction package in China, which consists of menu labelling, chef and waiter/waitress training, reformulation, supportive environment building, and sodium reduction campaign. In addition, monitoring the sodium content of restaurant foods is essential to set specific sodium reduction targets by food categories and help consumers understand the benefits of opting for low-sodium options when eating out.
Strengths and limitations
The strengths of our study include the large sample of restaurant dishes based on both major types of food served in the restaurants and foods frequently ordered by consumers from 6 provinces in China. The notable differences of restaurant food types between China and other countries [37, 38], call for more data based on local studies. Furthermore, we used standard reporting formats (sodium mg per 100 g) to facilitate comparisons across regions, restaurant sizes and dish types. We also reported the sodium content per serving, to help customers compare sodium content between various menu options. Finally, the large sample size in our study could capture the variability in sodium level in restaurant dishes, making the results more robust.
A number of limitations also exist. Sodium content assessing methods usually include laboratory analysis, menu labelling or online nutrition information provided by restaurant companies, and analysis with a nutrient database [39]. There are assessment differences between laboratory and menu items analysis, which may be due to differences in reported versus actual portion size and recall bias by chefs. However, due to the lack of publicly available menu nutrient values and the expensive cost of laboratory analyses, we considered menu items analysis the most cost-effective method to assess the sodium content of restaurant foods in China, especially with such a large sample size. In addition, with the rapid pace of restaurant foods development, this cross-sectional survey could not capture changes of sodium levels. Furthermore, the results in this study could not represent the sodium level for all Chinese restaurant dishes due to wide variations in restaurant foods. Some countries have tracking the sodium content in restaurant foods [40], which will provide dynamic data to guide restaurants in increasing the availability of lower-sodium foods and help consumers decrease their sodium intake.
Conclusions
In conclusion, our study shows that the sodium content of the majority of popular restaurant dishes in China are extremely high and variable. Further, the large number of restaurant dishes that exceeded the daily AI and PI in a single serving, along with the widespread use of salted condiments/seasonings, demonstrate the need for a Chinese sodium reduction strategy that addresses all the major sodium sources. Coordinated government-led efforts should be implemented, with the participation of restaurants, food manufacturers, and consumers to reduce sodium level in restaurant foods, raise sodium-reduction awareness and ultimately lower population sodium intake.
Acknowledgments
The authors would like to acknowledge the support of all the investigators, restaurants and staff involved in the Restaurant-based Intervention Study (RIS) from 6 provinces of China.
Abbreviations
- RIS
Restaurant-based Intervention Study
- AI
Adequate Intake
- PI
Proposed Intake for Preventing Non-Communicable Chronic Diseases
- CNNHS
China National Nutrition and Health Surveillance
- PAF
Population Attributable Fraction
- ASC
Action on Salt China
- RCT
Randomized Controlled Trial
- EDC
Electronic Data Collection System
- DRIs
Dietary Reference Intakes
Authors’ contributions
WWD contributed to the conceptualization of the study, analyzed and interpreted the data, and drafted the manuscript; HJW contributed to the study design and data interpretation; JGZ contributed to data collection and statistical analyses; XFZ and NW contributed to data collection and cleaning; YL and PHZ contributed to study design and data interpretation; MT contributed to language editing and manuscript modification; FJH acquired the funding and contributed to data interpretation. All authors provided comments on the draft manuscript and approved the final version.
Funding
This research was part of the research programme by the NIHR Global Health Research Unit Action on Salt China (ASC), which was commissioned by the National Institute of Health Research using Official Development Assistance (ODA) funding (16/136/77). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to considerations of intellectual property. However, they may be available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Review Board of the National Institute for Nutrition and Health, China CDC (20180314), and Queen Mary Research Ethics Committee (QMERC2018/14).
Consent for publication
Not applicable.
Competing interests
FJH is an unpaid member of Action on Salt and World Action on Salt, Sugar and Health (WASSH). Other authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wenwen Du, Email: duww@ninh.chinacdc.cn.
Huijun Wang, Email: wanghj@ninh.chinacdc.cn.
Jiguo Zhang, Email: zhangjg@ninh.chinacdc.cn.
Xiaofan Zhang, Email: zhangxf@ninh.chinacdc.cn.
Nan Wei, Email: nanw0135@qq.com.
Yuan Li, Email: yli@georgeinstitute.org.cn.
Monique Tan, Email: m.tan@qmul.ac.uk.
Puhong Zhang, Email: zpuhong@georgeinstitute.org.cn.
Feng J. He, Email: f.he@qmul.ac.uk
References
- 1.GBD 2017 Diet Collaborators Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 3.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022. doi: 10.1002/14651858.CD004022.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. doi: 10.1136/bmjopen-2013-003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Guideline: Sodium intake for adults and children. 2012. [PubMed] [Google Scholar]
- 6.Fang K, He Y, Fang Y, Lian Y. Dietary sodium intake and food sources among Chinese adults: data from the CNNHS 2010-2012. Nutrients. 2020;12:453. doi: 10.3390/nu12020453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chinese Nutrition Society . Chinese dietary reference intakes (2013) Beijing: Science Press; 2014. [Google Scholar]
- 8.He Y, Li Y, Yang X, Hemler EC, Fang Y, Zhao L, Zhang J, Yang Z, Wang Z, He L, et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982-2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019;7:540–548. doi: 10.1016/S2213-8587(19)30152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine . Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press; 2010. [Google Scholar]
- 10.Al Jawaldeh A, Rafii B, Nasreddine L. Salt intake reduction strategies in the eastern mediterranean region. East Mediterr Health J. 2019;24:1172–1180. doi: 10.26719/emhj.18.006. [DOI] [PubMed] [Google Scholar]
- 11.He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens. 2014;28:345–352. doi: 10.1038/jhh.2013.105. [DOI] [PubMed] [Google Scholar]
- 12.Webster J, Dunford E, Huxley R, Li N, Nowson CA, Neal B. The development of a national salt reduction strategy for Australia. Asia Pac J Clin Nutr. 2009;18:303–309. [PubMed] [Google Scholar]
- 13.The State Council. ‘Healthy China 2030’ plan outline. http://www.gov.cn/gongbao/2016-11/20/content_5133024.htm. Accessed 20 June 2020.
- 14.Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, Ueshima H, Kesteloot H, Miura K, Curb JD, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the intermap study. J Am Diet Assoc. 2010;110:736–745. doi: 10.1016/j.jada.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15:371–377. doi: 10.1038/s41569-018-0004-1. [DOI] [PubMed] [Google Scholar]
- 16.Jia X, Liu J, Chen B, Jin D, Fu Z, Liu H, Du S, Popkin BM, Mendez MA. Differences in nutrient and energy contents of commonly consumed dishes prepared in restaurants v. at home in Hunan province, China. Public Health Nutr. 2018;21:1307–1318. doi: 10.1017/S1368980017003779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zang J, Luo B, Wang Y, Zhu Z, Wang Z, He X, Wang W, Guo Y, Chen X, Wang C, et al. Eating out-of-home in adult residents in Shanghai and the nutritional differences among dining places. Nutrients. 2018;10:951. doi: 10.3390/nu10070951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen BT, Powell LM. The impact of restaurant consumption among US adults: effects on energy and nutrient intakes. Public Health Nutr. 2014;17:2445–2452. doi: 10.1017/S1368980014001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scourboutakos MJ, Murphy SA, L'Abbe MR. Association between salt substitutes/enhancers and changes in sodium levels in fast-food restaurants: a cross-sectional analysis. CMAJ Open. 2018;6:E118–E125. doi: 10.9778/cmajo.20170137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao F, Zhang P, Zhang L, Niu W, Gao J, Lu L, Liu C, Gao X. Consumption and sources of dietary salt in family members in Beijing. Nutrients. 2015;7:2719–2730. doi: 10.3390/nu7042719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eyles H, Shields E, Webster J, Ni MC. Achieving the WHO sodium target: estimation of reductions required in the sodium content of packaged foods and other sources of dietary sodium. Am J Clin Nutr. 2016;104:470–479. doi: 10.3945/ajcn.115.125146. [DOI] [PubMed] [Google Scholar]
- 22.Zhang P, He FJ, Li Y, Li C, Wu J, Ma J, Zhang B, Wang H, Li Y, Han J, et al. Reducing salt intake in China with “action on salt China” (ASC): protocol for campaigns and randomized controlled trials. JMIR Res Protoc. 2020;9:e15933. doi: 10.2196/15933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Du W, Zhang J, Li Y, He FJ, Zhou X, Xu Z, Gao Y, Yin L, Chang X, Yan W, et al. Restaurant interventions for salt reduction in China: protocol for a randomised controlled trial. BMJ Open. 2020;10:e038744. doi: 10.1136/bmjopen-2020-038744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quader ZS, Zhao L, Gillespie C, Cogswell ME, Terry AL, Moshfegh A, Rhodes D. Sodium intake among persons aged≥2 years - United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66:324–238. doi: 10.15585/mmwr.mm6612a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scourboutakos MJ, L'Abbe MR. Sodium levels in Canadian fast-food and sit-down restaurants. Can J Public Health. 2013;104:e2–e8. doi: 10.1007/BF03405645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahuja JKC, Li Y, Haytowitz DB, Bahadur R, Pehrsson PR, Cogswell ME. Assessing changes in sodium content of selected popular commercially processed and restaurant foods: results from the USDA: CDC sentinel foods surveillance program. Nutrients. 2019;11:1754. doi: 10.3390/nu11081754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scourboutakos MJ, L'Abbe MR. Changes in sodium levels in chain restaurant foods in Canada (2010-2013): a longitudinal study. CMAJ Open. 2014;2:E343–E351. doi: 10.9778/cmajo.20140028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahuja JK, Wasswa-Kintu S, Haytowitz DB, Daniel M, Thomas R, Showell B, Nickle M, Roseland JM, Gunn J, Cogswell M, et al. Sodium content of popular commercially processed and restaurant foods in the United States. Prev Med Rep. 2015;2:962–967. doi: 10.1016/j.pmedr.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones A, Magnusson R, Swinburn B, Webster J, Wood A, Sacks G, Neal B. Designing a healthy food partnership: lessons from the Australian food and health dialogue. BMC Public Health. 2016;16:651. doi: 10.1186/s12889-016-3302-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK food standards agency's salt reduction programme. Public Health Nutr. 2012;15:254–261. doi: 10.1017/S1368980011000966. [DOI] [PubMed] [Google Scholar]
- 31.Park HK, Lee Y, Kang BW, Kwon KI, Kim JW, Kwon OS, Cobb LK, Campbell NRC, Blakeman DE, Kim CI. Progress on sodium reduction in South Korea. BMJ Glob Health. 2020;5:e002028. doi: 10.1136/bmjgh-2019-002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Byrd K, Almanza B, Ghiselli RF, Behnke C, Eicher-Miller HA. Adding sodium information to casual dining restaurant menus: beneficial or detrimental for consumers? Appetite. 2018;125:474–485. doi: 10.1016/j.appet.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 33.Webster J, Trieu K, Dunford E, Nowson C, Jolly KA, Greenland R, Reimers J, Bolam B. Salt reduction in Australia: from advocacy to action. Cardiovasc Diagn Ther. 2015;5:207–218. doi: 10.3978/j.issn.2223-3652.2015.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park S, Lee H, Seo DI, Oh KH, Hwang TG, Choi BY. Educating restaurant owners and cooks to lower their own sodium intake is a potential strategy for reducing the sodium contents of restaurant foods: a small-scale pilot study in South Korea. Nutr Res Pract. 2016;10:635–640. doi: 10.4162/nrp.2016.10.6.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Curtis CJ, Clapp J, Niederman SA, Ng SW, Angell SY. US food industry progress during the national salt reduction initiative: 2009-2014. Am J Public Health. 2016;106:1815–1819. doi: 10.2105/AJPH.2016.303397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu A, Ma J, Guo X, Wang L, Wu J, Zhang J, Bai Y, Xu J, Lu Z, Xu Z, et al. Association of a province-wide intervention with salt intake and hypertension in Shandong province, China, 2011-2016. JAMA Intern Med. 2020;180:877–886. doi: 10.1001/jamainternmed.2020.0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prentice CA, Smith C, McLean RM. Sodium in commonly consumed fast foods in New Zealand: a public health opportunity. Public Health Nutr. 2016;19:958–966. doi: 10.1017/S1368980015001731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Drewnowski A, Rehm CD. Sodium intakes of US children and adults from foods and beverages by location of origin and by specific food source. Nutrients. 2013;5:1840–1855. doi: 10.3390/nu5061840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maalouf J, Cogswell ME, Gunn JP, Curtis CJ, Rhodes D, Hoy K, Pehrsson P, Nickle M, Merritt R. Monitoring the sodium content of restaurant foods: public health challenges and opportunities. Am J Public Health. 2013;103:e21–e30. doi: 10.2105/AJPH.2013.301442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahuja JK, Pehrsson PR, Haytowitz DB, Wasswa-Kintu S, Nickle M, Showell B, Thomas R, Roseland J, Williams J, Khan M, et al. Sodium monitoring in commercially processed and restaurant foods. Am J Clin Nutr. 2015;101:622–631. doi: 10.3945/ajcn.114.084954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to considerations of intellectual property. However, they may be available from the corresponding author on reasonable request.