Abstract
Background
Ingestion of the berries of the European yew tree can result in fatal cardiac arrhythmias.
Case summary
A 53-year-old female presented to our emergency department following ingestion of ∼200 European yew tree berries. At presentation, she was in cardiogenic shock due to a mixture of tachy- and bradyarrhythmias including ventricular tachycardia, atrial fibrillation with slow ventricular response and prolonged ventricular conduction, and periods of asystole. She was referred to a specialist cardiac centre and promptly established on mechanical circulatory support with venoarterial extracorporeal membrane oxygenation (V-A ECMO) by a retrieval team. Following resolution of her arrhythmias, she was weaned from V-A ECMO after 4 days of support and was discharged home with full neurological recovery on Day 12.
Discussion
Poisoning can lead to acute reversible but potentially fatal cardiogenic shock. We believe that access to prompt initiation of V-A ECMO was key to this patient’s survival.
Keywords: European yew tree, Taxus baccata, Poisoning, Mechanical circulatory support, Venoarterial extracorporeal membrane oxygenation, Case report
Learning points.
In cases of yew toxicity there must be early anticipation of cardiac instability.
Large metropolitan areas may benefit from a dedicated VA-ECMO retrieval team.
Introduction
The European yew tree (Taxus baccata) produces needles, bark, and berries that contain taxine alkaloids, which are toxic to humans upon consumption. Taxine alkaloids antagonize sodium and calcium channels within the cardiac myocardium, resulting in an increase in cytoplasmic calcium, leading to bizarre and potentially fatal cardiac rhythms.
We report the case of a 53-year-old female, who developed cardiogenic shock in the context of malignant arrhythmias following ingestion of ∼200 yew berries. We believe this patient only survived due to the prompt initiation of venoarterial extracorporeal membrane oxygenation (V-A ECMO).
Following our own literature search, just eight cases were identified where extra-corporeal life support was either used or considered to support life in these instances.
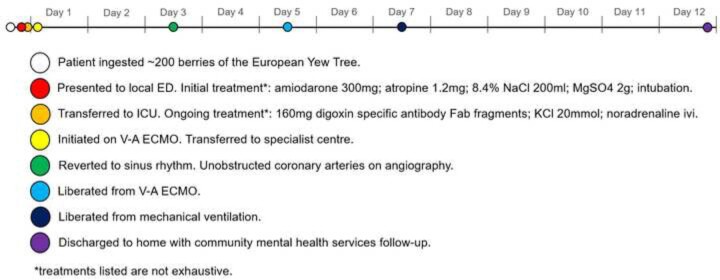
Timeline
A timeline of the patient’s journey from admission to discharge.
Case presentation
A 53-year-old female presented to the emergency department (ED) of a district general hospital having deliberately ingested ∼200 berries from the European yew tree. Her past medical history included depression (treated with olanzapine) and two previous episodes of deliberate drug overdose with suicidal intent. She was brought to the hospital by ambulance having informed her family of the overdose. She denied co-poisoning.
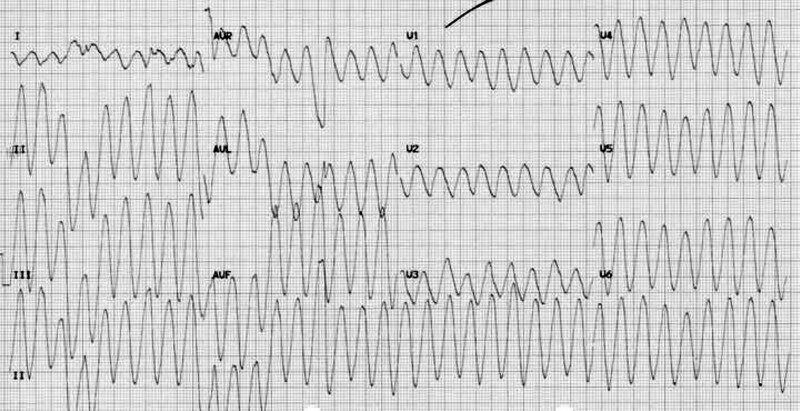
On arrival at the ED, she had a Glasgow Coma Scale score of 12 and was agitated and combative. Her chest was clear on auscultation. Her distal limbs were ice cold on palpation. Electrocardiogram (ECG) monitoring showed rapid cycling between a bizarre irregular rhythm with broad slurred QRS complexes which likely represented atrial fibrillation with abnormal ventricular conduction (Figure 1) and ventricular tachycardia with a pulse (with variable rates from 130 b.p.m. to 210 b.p.m.—Figure 2), interspersed with short episodes of asystole (during one episode, she received 20 s of cardiopulmonary resuscitation (CPR)—terminated due to signs of life). Non-invasive blood pressure was recorded as 50/30 mmHg.
Figure 1.
An electrocardiogram demonstrating atrial fibrillation with abnormal ventricular contraction.
Figure 2.
An electrocardiogram demonstrating ventricular tachycardia.
An initial venous blood gas revealed metabolic acidaemia (pH 7.31, H+ 48.5 nmol/L, HCO3− 20.5 mmol/L), hyperlactataemia (lactate 4.9 mmol/L), and hypokalaemia (K+ 3.1 mmol/L).
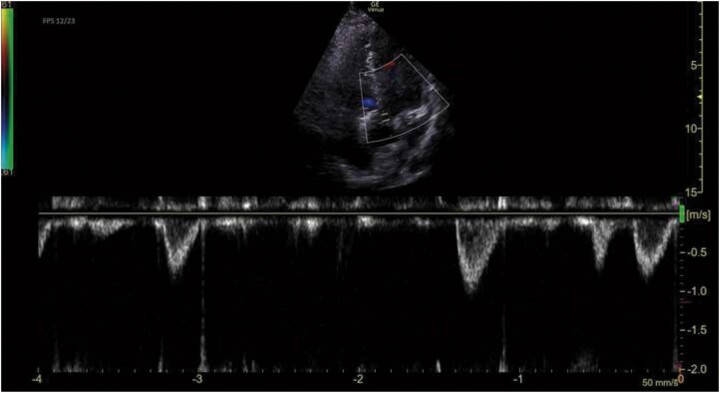
A focused bedside transthoracic echocardiogram (TTE) showed chaotic biventricular activity with occasional ejection (as assessed by pulsed-wave Doppler in the left ventricular outflow tract—Figure 3), a competent aortic valve and mild mitral and tricuspid regurgitation with no pericardial effusion. Following admission to the intensive care unit (ICU) a PiCCO line (Edwards Lifesciences, CA, USA) was inserted, and cardiac output was estimated at 1.5 L/min using a bolus thermodilution method.
Figure 3.
Pulsed-wave Doppler in the left ventricular outflow tract.
The patient was discussed with a consultant toxicologist at the National Poisons Information Service and a consultant electrophysiologist at a local tertiary cardiology centre. Initial management in the ED focused on anti-arrhythmics (summarized in the Timeline); however, this was challenging given the patient cycled between tachy- and bradyarrhythmias, with a resultant heart rate at times as low as 13 b.p.m.
Intravenous adrenaline was administered in 5 mcg boluses to support her blood pressure until a noradrenaline infusion was established via central venous access.
The regional ECMO service for respiratory failure in adults was contacted for consideration for the initiation of mechanical circulatory support (MCS) with V-A ECMO. A retrieval team were promptly dispatched. The patient was initiated on V-A ECMO in the ICU using a 21 Fr multistage drainage cannula sited in the femoral vein and a 15 Fr return cannula sited in the femoral artery. The patient was slim with excellent sub-costal windows for TTE, therefore a sub-costal bi-caval view was used to ensure correct guidewire placement. Venoarterial extracorporeal membrane oxygenation commenced ∼6 h after the patient first presented to our hospital.
Venoarterial extracorporeal membrane oxygenation resulted in an almost immediate improvement in systemic blood pressure, allowing for discontinuation of vasopressor support and a degree of cardiac rhythm stability. She was transferred to the regional ECMO centre for ongoing management.
For the first 48 h following ECMO initiation, arrhythmias continued, including periods of asystole. A TTE at the time showed left ventricular impairment with biplane left ventricular ejection fraction of 49% and regional wall abnormalities including hypokinesia of the anterior septum. Coronary angiography was performed, revealing unobstructed coronaries. After 4 days of V-A ECMO, the TTE was entirely normal, implying recovery of cardiac function and she was weaned from MCS. She was repatriated to her local hospital and weaned from mechanical ventilation on day 7.
She remained stable and following assessment by psychiatric services and initiation of ongoing community mental health follow-up she was discharged home 12 days after presenting to the ED. She made a full recovery with no neurological deficit but required ongoing anti-coagulation due to a linear thrombus within the inferior vena cava, presumed to be related to the ECMO drainage cannula.
Discussion
The yew tree is native to Europe and apart from the red pulp of its berries, all parts are toxic.1 Toxicity is due to the compound Taxane B, which antagonizes calcium and sodium channels in the cardiac myocytes, increasing cytoplasmic calcium.2 Cytotoxic features led to yew being used by the healthcare sector in the chemotherapeutic agents docetaxel and paclitaxel.2 Yew intoxication symptoms are initially non-specific, and include abdominal pain, nausea, vomiting, dizziness, and seizures.3 Subsequently patients can develop ECG rhythm disturbances, including atrioventricular (AV) conduction block, QRS broadening, ventricular fibrillation, and ultimately death.2,4 There are no specific antidotes.5 Transcutaneous and percutaneous pacing are often ineffective.6
A literature search was conducted on Pubmed using the MeSH terms ECMO and yew and intoxication or suicide. This brought up eight studies concerning nine patients.6–13 Patients ranged from 20 years old to 49 years old and six (67%) were female. Common features in their presentations included bradycardia and cardiogenic shock. Seven (78%) of the patients received ECMO and survived with largely good outcomes. One patient had persistent renal failure.11 Two patients did not receive ECMO. One was a 49-year-old male who initially had temporary transvenous pacing and was considered for V-A ECMO but unfortunately deteriorated and suffered cardiorespiratory arrest.6 Another, a 45-year-old female, was supported with a temporary pacemaker and catecholamines and did survive.13
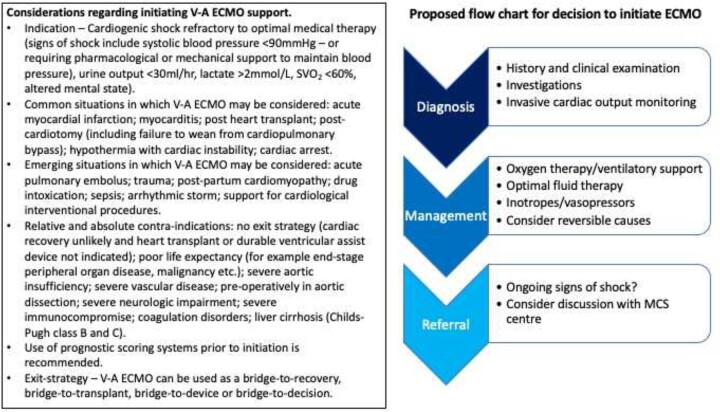
When V-A ECMO is available and can be initiated promptly it provides a bridge to recovery for patients with taxine alkaloid poisoning. Figure 4 details information around the decision-making process of initiating ECMO.14 In the published literature, 100% of those receiving ECMO survived with full neurological recovery. European Society of Cardiology (ESC) guidelines state that mechanical circulatory support can be appropriate in patients with cardiogenic shock secondary to acute heart failure.15 Despite this, ECMO is infrequently used in cases of poisoning. A retrospective review of the Extracorporeal Life Support Organisation (ELSO) registry identified just 22 cases of V-A or ‘hybrid’ ECMO for poisoning between 2011 and 2014 with 59% mortality.16
Figure 4.
Considerations for the decision to initiate extracorporeal membrane oxygenation.
Conclusion
Our case adds to the literature a further case of yew toxicity successfully supported by V-A ECMO. Key to her survival was prompt initiation of V-A ECMO by a specialist team and transfer to a regional referral centre. We propose that this case supports the need for referral pathways for patients presenting with reversible acute cardiogenic shock.
Lead author biography

Dr Catherine Ward attended medical school at GKT School of Medical Education, King’s College London and subsequently completed her foundation years in London. She is now pursuing a master’s degree in extreme and wilderness medicine while working as a locum junior doctor in emergency medicine.
Acknowledgements
With thanks to Dr Richard Fisher at the Department of Critical Care, King’s College Hospital NHS Foundation Trust for his involvement in the care of the patient and his role in the preparation of this case presentation and case report.
Consent : The authors confirm that written consent for submission of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Funding: Open Access fees for this case report have been waived by the European Society of Cardiology, following the presentation of the case at the ESC Acute CardioVascular Care 2021 congress.
Conflict of interest: None declared.
Contributor Information
Catherine Ward, Department of Critical Care, King's College Hospital NHS Foundation Trust, Denmark Hill, London SE5 9RS, UK.
Daveena Meeks, Department of Critical Care, King's College Hospital NHS Foundation Trust, Denmark Hill, London SE5 9RS, UK.
Richard Trimlett, Department of Cardiothoracic Surgery, Royal Brompton & Harefield NHS Foundation Trust, London, UK.
Joana Alçada, Department of Intensive Care, Adult Intensive Care Unit, Royal Brompton & Harefield NHS Foundation Trust, London, UK.
References
- 1. Panzeri C, Bacis G, Ferri F, Rinaldi G, Persico A, Uberti F et al. Extracorporeal life support in a severe Taxus baccata poisoning. Clin Toxicol (Phila) 2010;48:463–465. [DOI] [PubMed] [Google Scholar]
- 2. Reijnen G, Bethlehem C, van Remmen JMBL, Smit HJM, van Luin M, Reijnders UJL. Post-mortem findings in 22 fatal Taxus baccata intoxications and a possible solution to its detection. J Forensic Leg Med 2017;52:56–61. [DOI] [PubMed] [Google Scholar]
- 3. Wilson CR, Sauer J, Hooser SB. Taxines: a review of the mechanism and toxicity of yew (Taxus spp.) alkaloids. J Int Soc Toxinol 2001;39:175–185. [DOI] [PubMed] [Google Scholar]
- 4. Willaert W, Claessens P, Vankelecom B, Vanderheyden M. Intoxication with Taxus baccata: cardiac arrhythmias following yew leaves ingestion. Pacing Clin Electrophysiol PACE 2002;25:511–512. [DOI] [PubMed] [Google Scholar]
- 5. Toxbase [Internet]. http://3.%09Toxbase.org/poisons-index-a-z/y-products/yew-berries/ (22 December 2021).
- 6. Natasha G, Chan M, Gue YX, Gorog DA. Fatal heart block from intentional yew tree (Taxus baccata) ingestion: a case report. Eur Hear J Case Rep 2019;4:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ajouri J, Muellenbach RM, Rolfes CB, Weber K, Schuppert F, Peivandi AA et al. Cardiogenic shock following yew needle poisoning: digoxin immune fab, va-ECMO and albumin dialysis for the treatment of a suicidal yew leaf poisoning. Anaesthetist 2021;1–4. doi: 10.1007/s00101-021-01048-w. [DOI] [PubMed] [Google Scholar]
- 8. Baum C, Bohnen S, Sill B, Philipp S, Damerow H, Kluge S et al. Prolonged resuscitation and cardiogenic shock after intoxication with European yew (Taxus baccata): Complete recovery after intermittent mechanical circulatory support. Int J Cardiol 2015;181:176–178. [DOI] [PubMed] [Google Scholar]
- 9. Hermes-Laufer J, Meyer M, Rudiger A, Henze J, Enselmann K, Kupferschmidt H et al. Extracorporeal life support as bridge to recovery in yew poisoning: case reports and literature review. ESC Heart Fail 2021;8:705–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bounes FV, Tardif E, Ruiz S, Gallart J-C, Conil J-M, Delmas C. Suicide attempt with self-made Taxus baccata leaf capsules: survival following the application of extracorporeal membrane oxygenation for ventricular arrhythmia and refractory cardiogenic shock. Clin Toxicol (Phila) 2017;55:925–928. [DOI] [PubMed] [Google Scholar]
- 11. Farag M, Badowski D, Koschny R, Skopp G, Brcic A, Szabo GB. Extracorporeal life support and digoxin-specific Fab fragments for successful management of Taxus baccata intoxication with low output and ventricular arrhythmia. Am J Emerg Med 2017;35:1987.e3–1987.e7. [DOI] [PubMed] [Google Scholar]
- 12. Thooft A, Goubella A, Fagnoul D, Taccone FS, Brimioulle S, Vincent J-L et al. Combination of veno-arterial extracorporeal membrane oxygenation and hypothermia for out-of-hospital cardiac arrest due to Taxus intoxication. Can J Emerg Med 2014;16:504–507. [DOI] [PubMed] [Google Scholar]
- 13. Haring B, Weismann D. Taxus poisoning: an unusual cause of acute heart failure. Dtsch Medizinische Wochenschrift 2021;146:331–334. [DOI] [PubMed] [Google Scholar]
- 14. Lorusso R, Shekar K, MacLaren G, Schmidt M, Pellegrino V, Meyns B et al. ELSO interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. ASAIO J 2021;67:827–844. [DOI] [PubMed] [Google Scholar]
- 15. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS et al. ; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 16. Ramanathan K, Tan CS, Rycus P, MacLaren G. Extracorporeal membrane oxygenation for poisoning in adult patients: outcomes and predictors of mortality. Intensive Care Med 2017;43:1538–1539. [DOI] [PubMed] [Google Scholar]