Abstract
Background
Buprenorphine is an effective medication for opioid use disorder (MOUD) when offered in community-based settings, but evidence is limited for incarcerated populations, particularly in relation to recidivism. In Massachusetts, Franklin County jail (FCSO) was among the first to provide buprenorphine; adjacent Hampshire County jail (HCHC) offered it more recently. These jails present a natural experiment to determine whether outcomes are different between individuals who did and did not have the opportunity to receive buprenorphine in jail.
Methods
We examined outcomes of all incarcerated adults with opioid use disorder (n=469) who did (FCSO n=197) and did not (HCHC n=272) have the opportunity to receive buprenorphine. The primary outcome was post-release recidivism, defined as time from jail exit to a recidivism event (incarceration, probation violation, arraignment). Using Cox proportional hazards models, we investigated site as a predictor, controlling for covariates. We also examined post-release deaths.
Results
Fewer FCSO than HCHC individuals recidivated (48.2% vs. 62.5%; p=0.001); fewer FCSO individuals were re-arraigned (36.0% vs. 47.1%; p=0.046) or re-incarcerated (21.3% vs. 39.0%; p<0.0001). Recidivism risk was lower in the FCSO group (hazard ratio 0.71, 95% confidence interval 0.56, 0.89; p=0.003), net of covariates (adjusted hazard ratio 0.68, 95% confidence interval 0.53, 0.86; p=0.001). At each site, 3% of participants died.
Conclusions
Among incarcerated adults with opioid use disorder, risk of recidivism after jail exit is lower among those who were offered buprenorphine during incarceration. Findings support the growing movement in jails nationwide to offer buprenorphine and other agonist medications for opioid use disorder.
Keywords: Recidivism, mortality, buprenorphine, naltrexone, medications for opioid use disorder (MOUD), criminal justice settings, Massachusetts Justice Community Opioid Innovation Network (MassJCOIN)
1.0. INTRODUCTION
Incarcerated individuals with opioid use disorder (OUD) are at high risk for overdose and other adverse outcomes after community release (Binswanger et al., 2013; Pizzicato et al., 2018). Medications to treat OUD (MOUD, i.e., buprenorphine, methadone, naltrexone) hold great promise to improve these outcomes among incarcerated populations (Mace et al., 2019; Malta et al., 2019; SAMHSA, 2019), but its implementation is not standard-of-care in U.S. jails and prisons (Grella et al., 2020; Macmadu et al., 2020; Simon et al., 2021). Most correctional facilities that do offer MOUD are large urban jails (e.g. New York City, San Francisco, Albuquerque) or part of unified state systems (e.g., Rhode Island, Vermont), and typically only offer naltrexone, with fewer facilities also offering buprenorphine (Wakeman & Rich, 2015). Prior studies on post-release outcomes have mostly examined the effects of methadone and naltrexone (Moore et al., 2019) and reported reduced overdoses, reduced risks for infectious disease, and other beneficial outcomes (Brinkley-Rubinstein et al., 2018; Fanucchi et al., 2019; Farrell-MacDonald et al., 2014; Haas et al., 2021; Murphy et al., 2017; Springer et al., 2019; Wilson et al., 2012). Few studies, however, have examined the impact of buprenorphine in county jails on post-release recidivism (Moore et al., 2019), a crucial outcome to convince lawmakers and public safety officials of its value in correctional settings.
The Franklin County Sheriff’s Office (FCSO) in Greenfield, Massachusetts was among the first rural jails nationwide to offer buprenorphine (begun in February 2016), in addition to naltrexone, to incarcerated residents (Donelan et al., 2021). Hampshire County (located immediately south of Franklin County) has a similar rural jail, but the Hampshire County House of Corrections (HCHC) did not provide buprenorphine until May 2019. The current study uses the differences in buprenorphine provision between these jails in adjacent counties with similar recidivism rates as a natural experiment to examine the post-release recidivism and mortality outcomes of persons who were offered buprenorphine while incarcerated after their return to the community. We hypothesized that outcomes would be better among individuals who exited FCSO (i.e., offered buprenorphine pre-release) than among individuals who exited HCHC (i.e. not offered buprenorphine pre-release).
2.0. METHODS
2.1. Study sample and data sources
The study sample includes all adults with opioid use disorder (OUD) who exited one of two participating jails between January 1, 2015 and April 30, 2019 (N=469; 197 from FCSO, 272 from HCHC). Research staff extracted data from each jail’s electronic medical records (EMR) system to identify OUD diagnosis, receipt of MOUD while in jail, date of first jail exit (the “index jail episode,” for FCSO only we used first jail exit when MOUD was prescribed), and demographics. We verified OUD diagnosis and MOUD receipt by cross-checking EMR data against other records (prescription monitoring program; criminal justice records), and confirmed that no individuals in HCHC received MOUD while incarcerated (1 received naltrexone at release). In contrast, of individuals included in the FCSO group, 93.4% received MOUD while incarcerated, 1 was eligible for MOUD but did not receive it, and 12 could not be verified. Additionally, 53.1% of the FCSO group was inducted onto MOUD during incarceration, 38.8% continued MOUD at entrance per a prescription on file, and 8.2% had an unknown status. Most Franklin individuals received buprenorphine (86.2%), and fewer received extended-release naltrexone (7.1%), oral naltrexone (<1%), or an undocumented MOUD type (6.1%). Buprenorphine medication dosage ranged from 2–16mg. For naltrexone, 1 person received 50mg orally, and 14 received extended-release 380mg intramuscularly.
To measure post-release outcomes, we obtained administrative data on the entire sample, ensuring that each individual had at least one year of observation after jail exit. Mean±SD days from jail exit to end of observation was 618.8±194.4 for the FCSO group (~20 months) and 745.2 ±269.2 for the HCHC group (~25 months). We determined the one-year follow-up period for each individual based on the index release date.
The Baystate Health Institutional Review Board approved all study procedures and obtained federal certification for prisoner research.
2.2. Measures
2.2.1. Recidivism
Massachusetts Board of Probation (BOP) records contain statewide information on incarcerations, arraignments, and probation violations. Record reviews documented details such as type of event, date of occurrence, and number of events. We defined recidivism as any incarceration, arraignment, or probation violation occurring after release from the index jail episode.
2.2.2. All-Cause Mortality
Death information was searched on the web-based National Death Register, which provides the date of death, and by obtaining death certificates from state or county Vital Statistics offices for the cause of death.
2.3. Data analysis
We determined follow-up duration for our primary outcome using date of exit from the index jail episode to date of first recidivism event, death, or end of record review, whichever occurred first. Record review ended on April 30, 2020 to ensure all participants had at least 1 year of observation. Using a conservative, intent-to-treat approach, analyses treated individuals released from FCSO as having been offered MOUD, and vice-versa if released from HCHC. Cox proportional hazards (PH) models were fit to examine jail site as a predictor of recidivism after the index release, with covariates included based on baseline imbalances of demographic characteristics or criminal justice experiences. Number of prior incarcerations was highly correlated with number of prior arraignments and age of 1st arraignment. Thus, we selected as covariates number of prior incarcerations and index jail status is pre-trial vs. sentences. Chi-square or t-tests compare characteristics at baseline by site. Hypothesis tests use a two-sided, significance level of α=0.05.
We also compared the proportion of participants from each site who had any of the different types of recidivism events and arraignment charges using logistic regression models adjusted for baseline covariates. We limited these analyses to the first year after index jail release in order to 1. Investigate differences which may be most attributable to the MOUD intervention and 2. Eliminate bias due to the fact that HCHC participants, on average, had a longer record review time and thus would have more time to have recidivated.
We performed sensitivity analyses to explore the potential influence of baseline differences between participants from FCSO and HCHC (see Table 1) by fitting a series of separate Cox PH models for time to 1st recidivism using restricted samples. We examined 3 sources of potential bias: 1. Gender, by excluding females; 2. Prior criminal justice system involvement, by excluding participants whose number of prior incarcerations were at or above the 75th percentile and those who were first incarcerated as a juvenile; and 3. Holding status at index jail stay, by excluding participants with sentenced status. In additional sensitivity analyses, we sought to confirm the effectiveness of buprenorphine by excluding FCSO participants who received naltrexone or whose MOUD type was unknown. Hazard ratios and confidence intervals were reported for each analysis.
Table 1.
Participant characteristics and experiences with the criminal justice system (CJS) at baseline
| Franklin County Sheriff’s Office (FCSO) N = 197 | Hampshire County House of Corrections (HCHC) N = 272 | P value* | |
|---|---|---|---|
| Demographics | |||
| Male – N (%) | 179 (91.0) | 272 (100) | <0.0001 |
| Race – N (%) | |||
| White | 189 (96.0) | 260 (96.0) | 0.95 |
| Black/AA | 7 (4.0) | 10 (4.0) | |
| Other/Unknown | 1 (<1) | 2 (<1) | |
| Age – Mean (sd) | 34.5 (9.3) | 35.1 (9.8) | 0.49 |
| Medication for Opioid Use Disorder (MOUD) – N (%) | |||
| Buprenorphine | 170 (86.2) | 0 (0.0) | <0.0001 |
| Naltrexone | 14 (7.1) | 0 (0.0) | |
| Undocumented MOUD type | 12 (6.1) | 0 (0.0) | |
| None | 1 (<1.0) | 272 (100) | |
| CJS experiences before index jail episode | |||
| First arraigned as a juvenile – N (%) | 81 (41.0) | 139 (51.0) | 0.03 |
| Age at first arraignment – Mean (sd) | 19.2 (7.2) | 17.7 (6.2) | 0.02 |
| # of arraignments – Mean (sd) | 11.3 (9.3) | 15.7 (11.6) | <0.0001 |
| # of incarcerations – Mean (sd) | 3.0 (4.5) | 4.9 (6.1) | <0.0001 |
| CJS experiences on index jail episode | |||
| Jail status is sentenced – N (%) | 38 (19.0) | 113 (42.0) | <0.0001 |
| # of days incarcerated – Mean (sd) | 78.1 (126.1) | 85.1 (131.1) | 0.56 |
t-test for continuous and chi square for categorical
3.0. RESULTS
3.1. Baseline characteristics
At baseline, demographics were similar across sites but participants differed in terms of interactions with the criminal justice system (Table 1). Most participants were male, White, and the mean age was 34.5 for FCSO and 35.1 for HCHC. Individuals in FCSO had fewer criminal justice interactions than those in HCHC, and these interactions began at an older age. Compared to individuals in HCHC, fewer individuals in FCSO were first arraigned as a juvenile and the FCSO group also had fewer prior arraignments and incarcerations. On the index jail episode, fewer individuals in FCSO than in HCHC had a sentenced status and more were pre-trial detainees.
3.2. Recidivism
Recidivism was defined as any incarceration, probation violation, or arraignment after index jail release (Table 2). Review and analysis of BOP records indicated that fewer individuals in FCSO than in HCHC recidivated (48.2% vs. 62.5%, respectively). Among people who did recidivate, the most common type of first recidivism event was an arraignment for both the FCSO and HCHC groups (67% vs. 71%), with fewer people recidivating with a re-incarceration (11% vs. 13%) or probation violation (22% vs. 16%) (data not shown).
Table 2.
Recidivism and mortality during first year post-release
| FCSO (N=197) | HCHC (N=272) | P value* | |
|---|---|---|---|
| Incarcerations | |||
| Any - N (%) | 42 (21.3) | 106 (39.0) | <0.0001 |
| Days to first event, mean (sd) | 185.1 (95.4) | 159.2 (93.9) | 0.13 |
| Probation violations | |||
| Any - N (%) | 34 (17.3) | 44 (16.2) | 0.72 |
| Days to first event, mean (sd) | 229.4 (91.7) | 163.4 (96.3) | 0.003 |
| Arraignments | |||
| Any - N (%) | 71 (36.0) | 128 (47.1) | 0.046 |
| Days to first event, mean (sd) | 117.6 (98.3) | 129.2 (98.3) | 0.43 |
| Charge on arraignment (of first three events) - N (%) | |||
| Property | 19 (9.6) | 63 (23.2) | 0.001 |
| Drug-related | 28 (14.2) | 49 (18.0) | 0.30 |
| Violent | 19 (9.6) | 37 (13.6) | 0.25 |
| Other | 20 (10.2) | 35 (12.9) | 0.44 |
| Recidivism+ | |||
| Any - N (%) | 95 (48.2) | 170 (62.5) | 0.001 |
| Days to first event, mean (sd) | 132.9 (103.8) | 129.4 (100.1) | |
| Mortality | |||
| Died - N (%) | 6 (3.1) | 8 (2.9) | 1.00 |
| Days to death, mean (sd) | 242.3 (106.9) | 160.5 (147.0) | 0.27 |
Logistic models controlled for index jail status and number of prior incarcerations.
recidivism is defined as any incarceration, probation violation, or arraignment that occurred after exit from the index jail episode.
The percentage of participants from FCSO experiencing arraignment or re-incarceration was approximately 11–18% lower than participants from HCHC. Individuals released from FCSO had reduced odds of any type of recidivism during the first year post-release (adjusted odds ratio 0.51 95% CI 0.35, 0.76; p=0.001), and specifically, reduced odds of any post-release arraignment (aOR 0.67 95% CI 0.45, 0.99; p=0.046) and incarceration (aOR 0.37 95% CI 0.24, 0.58; p<0.0001). FCSO participants were less likely to have been arraigned on any property charges compared to HCHC participants (aOR 0.39 95% CI 0.22, 0.69; p=0.001).
The mean±SD days from jail exit to first recidivism event was 132.9±103.8 in FCSO and 129.4±100.1 in HCHC. Cox proportional hazards model results showed a decreased risk of recidivism for FCSO compared to HCHC, with an unadjusted hazard ratio (95% confidence interval) of 0.71 (0.56, 0.89) and an adjusted HR (95% CI) of 0.68 (0.53, 0.86) (Figure 1).
Figure 1. Time from jail exit to 1st recidivism event survival curves.
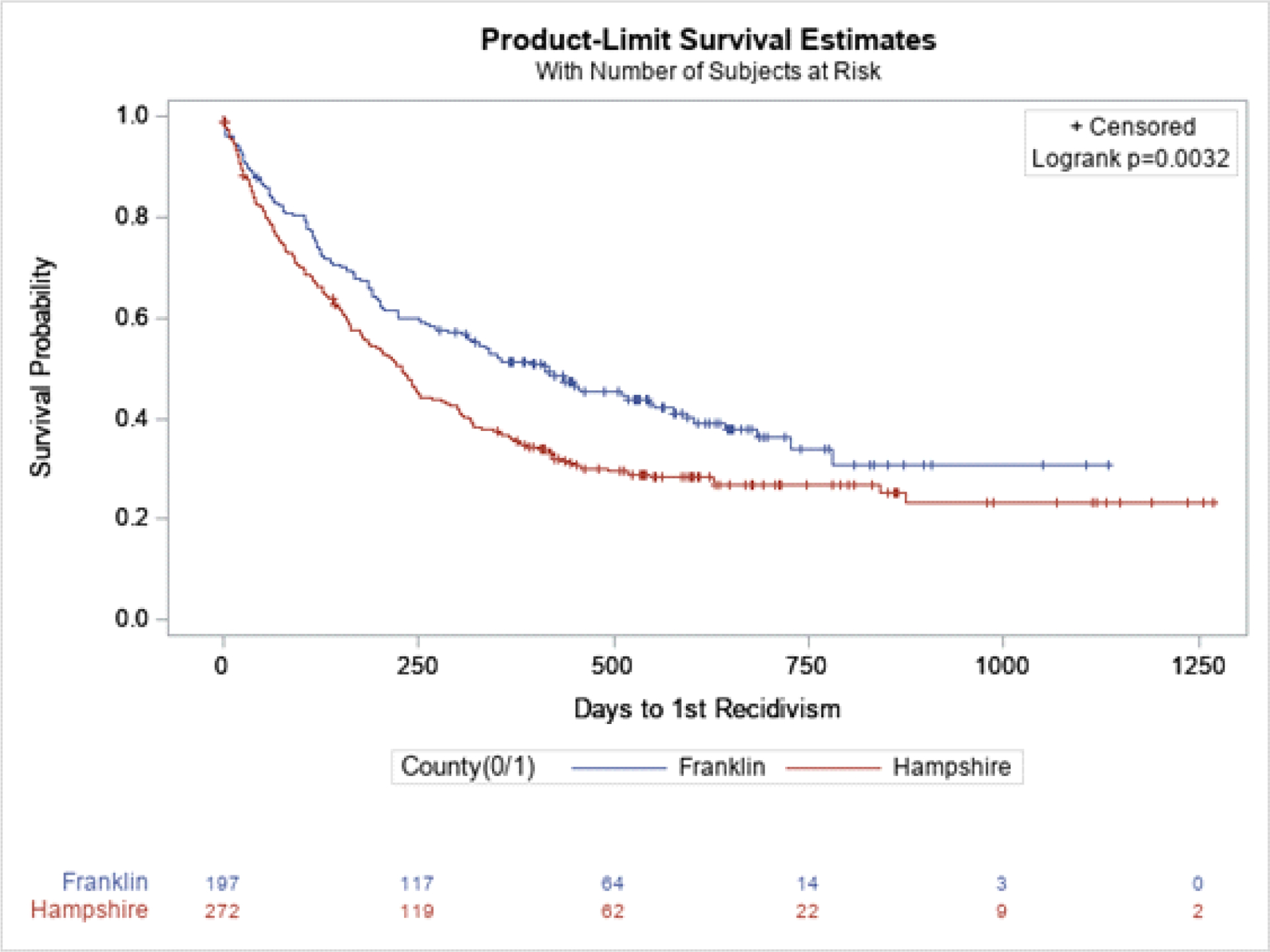
Cox proportional hazards model unadjusted hazard ratio (95% CI) 0.71 (0.56, 0.89), p = 0.003
Adjusted for number of prior incarcerations, index jail status is pre-trial vs. sentence HR 0.68 (0.53, 0.86), p = 0.001
We conducted sensitivity analyses of recidivism hazard ratios (95% confidence interval) for FCSO vs. HCHC using restricted samples. The results were as follows: males only (i.e., females excluded) 0.69 (0.54, 0.87); individuals who are less involved with the criminal justice system (i.e., number of prior arrests >75th percentile excluded) 0.75 (0.57, 0.99); participants first arraigned as an adult (i.e., juveniles excluded) 0.64 (0.46, 0.90); participants on pre-trial status at index jail stay (i.e., sentenced individuals excluded) 0.64 (0.49, 0.84); FCSO participants with documented receipt of buprenorphine only (i.e., naltrexone or unknown discharge MOUD excluded) 0.72 (0.57, 0.93).
3.3. Mortality
During the first year after release, approximately 3% of participants from each site died, 6 participants from FCSO (median time-to-death 287.5 days, IQR [201, 311], and 8 from HCHC (median time-to-death 141.5, IQR [14, 310]). Of the FCSO deaths, 2 were due to overdose (both between 9–12 months after release), 2 were unknown causes, and 2 resulted from injury or disease. Of the HCHC deaths, 5 were attributed to overdose (3 occurred within the first month after release and 2 between 9–12 months after release), 2 had unknown causes, and 1 other causes. After one year post-exit from jail, an additional 6 deaths occurred among HCHC participants (3 from overdose) and no additional deaths among FCSO participants. The larger sample size and longer record review time for HCHC may explain observing at least some of these additional deaths. The mean±sd age at death was 42.2±13.2 for FCSO and 40.9±11.6 for HCHC.
4.0. DISCUSSION
4.1. Key findings
This natural experiment across two similar rural jails in Massachusetts found that, among incarcerated adults with opioid use disorder, offering buprenorphine in jail substantially reduced the risk of recidivism. Results from the unadjusted Cox proportional hazards model found a 29% reduction in risk of recidivism, which reduced further to 32% after adjusting for baseline history of interactions with the criminal justice system and index jail status.
Post-hoc analyses found that recidivism related to property was reduced, in keeping with the logical supposition that MOUD effectively managed the opioid use disorder, and thus reduced associated drug related property crime. Analyses also found no differences in violations of parole or probation, suggesting that differing rates of rearrest for technical violations and variation in community correctional practices did not explain the findings.
The few prior studies detected limited impact of MOUD on recidivism (Perry et al., 2015). Gordon and colleagues (2017) examined outcomes of urban incarcerated individuals randomized to treatment with buprenorphine versus a counseling-only comparison group, reporting no differences in criminal activity one year after jail exit. Magura and colleagues (2009) randomized urban incarcerated individuals to buprenorphine or methadone, and reported no differences in arrests, crime, or incarceration three months after jail exit. These studies both focused on populations returning to large metropolitan areas. The current findings suggest that MOUD may have more substantial impact among persons leaving smaller jails who return to rural communities, although more research is needed.
4.2. Limitations and strengths
Study findings must be considered with its limitations. Findings derive from an observational natural experiment in mostly rural settings in Massachusetts in which one jail provided access to buprenorphine and the other did not. However, participants were not randomized, raising the possibility of selection bias, omitted variable bias, or confounding as explanations for these findings. We did not account for potential variation by site in OUD screening and assessment practices, opioid overdose education practices, linkage to MOUD after jail exit, community re-entry services, availability of MOUD or other services in the community, or other legal and health system practices that may have impacted outcomes. On the other hand, adjustment for baseline characteristics strengthened the findings, suggesting that the magnitude of effect might be conservative, and findings did not change in sensitivity analyses using models with restricted samples. Furthermore, findings from the predominantly white male population in these small rural county jails may not generalize to all incarcerated persons with OUD. Both jails are Massachusetts Justice Community Opioid Innovation Network sites, which offers future opportunities to replicate findings among a larger and more diverse sample (Evans et al., 2021). Also, recidivism outcomes are measured with administrative records. Administrative data enable measurement of outcomes on all participants, a key reason why these data are useful for assessing addiction treatment outcomes (Evans et al., 2010, 2019; Krebs et al., 2017), but they provide information only on those events that resulted in an incarceration, probation violation, or arraignment in Massachusetts. Finally, receipt of psychosocial treatment in these jails was not measured, so its potential effects could not be examined.
4.3. Conclusion and policy implications
This natural experiment found substantial reductions in post-release outcomes among a large sample of individuals with OUD who received buprenorphine in jail compared to those who did not receive MOUD.
After decades in which access to agonist treatments for OUD was limited in corrections, lawsuits and legislation have created momentum for jails and prisons to provide these lifesaving therapies. In Massachusetts, a legislative mandate caused seven jails, including the two examined in the current study, to expand agonist treatment options and related services in 2019. These jails provide all three FDA-approved types of MOUD during incarceration, and programming to connect individuals to MOUD in the community at jail exit. In addition to the demonstrated reduction in overdose mortality, the current study provides legislators and correctional officials with compelling evidence that agonist MOUD in jail will reduce recidivism. Since recidivism and reincarceration are costly, and the implementation costs associated with agonist treatment in jails are substantial, future work should examine the state and societal costs associated with MOUD in jail.
Table 3:
Recidivism during first year post-release, adjusted logistic regression results
| Outcome Odds Ratio (95% Confidence Interval) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Recidivism (any) | Incarceration | Probation violation | Arraign merit (any) | Arraigned: Drug | Arraigned: Property | Arraigned: Violent | Arraigned: Other | |
| County: Franklin (ref = Hampshire) | 0.51 (0.35, 0.76) | 0.37 (0.24, 0.58) | 0.91 (0.55, 1.52) | 0.67 (0.45, 0.99) | 0.76 (0.45, 1.28) | 0.39 (0.22, 0.69) | 0.70 (0.38, 1.28) | 0.79 (0.43, 1.44) |
| # of prior incarcerations | 1.06 (1.02, 1.10) | 1.03 (0.99, 1.07) | 0.99 (0.95, 1.04) | 1.06 (1.02, 1.10) | 1.05 (1.00, 1.09) | 1.05 (1.01, 1.09) | 1.04 (0.99, 1.09) | 1.02 (0.97, 1.07) |
| Jail status: pre-trial (index, ref = sentenced) | 2.05 (1.35, 3.12) | 2.24 (1.41, 3.56) | 2.27 (1.23, 4.21) | 1.26 (0.83, 1.90) | 1.52 (0.87, 2.67) | 0.96 (0.58, 1.62) | 1.27 (0.68, 2.38) | 1.06 (0.57, 1.97) |
Highlights.
We studied outcomes of buprenorphine treatment delivered in jail settings.
Fewer adults offered buprenorphine during incarceration recidivated.
Buprenorphine treatment reduced the risk of recidivism, independent of other factors.
Findings may assist jails to offer buprenorphine and other agonist medications.
ACKNOWLEDGEMENTS
Franklin County Sheriff’s Office:
Sheriff Christopher J. Donelan
Edmond Hayes
Levin Schwartz
Ashley Lipka
Hampshire County Sheriff’s Office:
Sheriff Patrick J. Cahillane
Melinda Cady
Kathryn Peverley
Baystate Health:
Randall Hoskinson, Jr.
Ben Potee
Sam Tarplin
Madison Crawford
Kevin Warwick
University of Massachusetts Amherst:
Elizabeth Delorme
Calla Harrington
Financial support:
The National Institute on Drug Abuse (NIDA) 3UG3DA044830-02S1 and 1UG1DA050067-01
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: No conflict declared.
REFERENCES
- Binswanger IA, Blatchford PJ, Mueller SR, Stern MF 2009. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 159(9), 592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkley-Rubinstein L, McKenzie M, Macmadu A, Larney S, Zaller N, Dauria E, Rich J 2018. A randomized, open label trial of methadone continuation versus forced withdrawal in a combined US prison and jail: Findings at 12 months post-release. Drug Alcohol Depend. 184,57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelan CJ, Hayes E, Potee R, Schwartz L, Evans E 2021. COVID-19 and treating incarcerated populations for opioid use disorder. J Subst Abuse Treat. 124:108216. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Grella C, Murphy D, Hser YI 2010. Using administrative data for longitudinal substance abuse research. J Behav Health Serv Res. 37(2),252–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Stopka TJ, Pivovarova E, Murphy SM, Taxman FS, Ferguson WJ, et al. 2021. Massachusetts Justice Community Opioid Innovation Network (Mass JCOIN). J Subst Abuse Treat. 128. doi: 10.1016/j.jsat.2021.108275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Zhu Y, Yoo C, Huang D, Hser YI 2019. Criminal justice outcomes over 5 years after randomization to buprenorphine-naloxone or methadone treatment for opioid use disorder. Addiction. 114(8),1396–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanucchi L, Springer SA, Korthuis PT 2019. Medications for treatment of opioid use disorder among persons living with HIV. Curr HIV/AIDS Rep. 16(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell-MacDonald S, MacSwain MA, Cheverie M, Tiesmaki M, Fischer B 2014. Impact of methadone maintenance treatment on women offenders’ post-release recidivism. Eur Addict Res. 20(4),192–199. [DOI] [PubMed] [Google Scholar]
- Gordon MS, Kinlock TW, Schwartz RP, O’Grady KE, Fitzgerald TT, Vocci FJ 2017. A randomized clinical trial of buprenorphine for prisoners: Findings at 12-months post-release. Drug Alcohol Depend. 172, 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Ostile E, Scott CK, Dennis M, Carnavale J 2020. A scoping review of barriers and facilitators to implementation of medications for treatment of opioid use disorder within the criminal justice system. Int J Drug Policy. 81, 102768. doi: 10.1016/j.drugpo.2020.102768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas A, Viera A, Doernberg M, Barbour R, Tong G, Grau LE, Heimer R 2021. Post-incarceration outcomes for individuals who continued methadone treatment while in Connecticut jails, 2014–2018. Drug Alcohol Depend. 227:108937. doi: 10.1016/j.drugalcdep.2021.108937. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs E, Urada D, Evans E, Huang D, Hser YI, Nosyk B 2017. The costs of crime during and after publicly funded treatment for opioid use disorders: a population-level study for the state of California. Addiction. 112(5), 838–851. doi: 10.1111/add.13729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mace S, Siegler A, Wu KC, Latimore A, Flynn H 2019. Medication-assisted treatment for opioid use disorder in jails and prisons: A planning & implementation toolkit. The National Council. [Google Scholar]
- Macmadu A, Goedel WC, Adams JW, Brinkley-Rubinstein L, Green TC, Clarke JG, et al. 2020. Estimating the impact of wide scale uptake of screening and medications for opioid use disorder in US prisons and jails. Drug Alcohol Depend. 208:107858. doi: 10.1016/j.drugalcdep.2020.107858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, et al. 2009. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 99(1–3), 222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malta M, Varatharajan T, Russell C, Pang M, Bonato S, Fischer B 2019. Opioid-related treatment, interventions, and outcomes among incarcerated persons: A systematic review. PLoS Med. 16(12), e1003002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KE, Roberts W, Reid HH, Smith KMZ, Oberleitner LMS, McKee SA 2019. Effectiveness of medication assisted treatment for opioid use in prison and jail settings: A meta-analysis and systematic review. J Subst Abuse Treat. 99, 32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SM, Polsky D, Lee JD, Friedmann PD, Kinlock TW, Nunes EV, et al. 2017. Cost-effectiveness of extended release naltrexone to prevent relapse among criminal justice-involved individuals with a history of opioid use disorder. Addiction. 112(8), 1440–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry AE, Neilson M, Martyn-St. James M, Glanville JM, Woodhouse R, Godfrey C, et al. 2015. Pharmacological interventions for drug-using offenders. Cochrane Database Syst Rev. 6, CD010862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzicato LN, Drake R, Domer-Shank R, Johnson CC, Viner KM 2018. Beyond the walls: Risk factors for overdose mortality following release from the Philadelphia Department of Prisons. Drug Alcohol Depend. 189, 108–115. [DOI] [PubMed] [Google Scholar]
- Simon R, Rich JD, Wakeman SE 2021. Treating Opioid Use Disorder in Correctional Settings. In: Wakeman SE, Rich JD (eds) Treating Opioid Use Disorder in General Medical Settings. Springer, Cham. 10.1007/978-3-030-80818-1_6 [DOI] [Google Scholar]
- Springer SA, Di Paola A, Azar MM, Barbour R, Biondi BE, Desabrais M, Lincoln T, Skiest DJ, Altice FL 2018. Extended-release naltrexone improves viral suppression among incarcerated persons living with HIV with opioid use disorders transitioning to the community: Results of a double-blind, placebo-controlled randomized trial. J Acquir Immune Defic Syndr. 1;78(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). 2019. Use of medication-assisted treatment for opioid use disorder in criminal justice settings. Rockville, MD: National Mental Health and Substance Use Policy Laboratory. (HHS publication no. PEP19-MATUSECJS) [Google Scholar]
- Wakeman SE, Rich JD 2015. Addiction treatment within U.S. correctional facilities: Bridging the gap between current practice and evidence-based care. J Addict Dis. 34(2–3), 220–225. [DOI] [PubMed] [Google Scholar]
- Wilson ME, Kinlock TW, Gordon MS, O’Grady KE, Schwartz RP 2012. Postprison release HIV-risk behaviors in a randomized trial of methadone treatment for prisoners. Am J Addict. 21(5), 476–87. [DOI] [PMC free article] [PubMed] [Google Scholar]


