Abstract
Background
Normal sexual function is a biopsychosocial process and relies on the coordination of psychological, endocrine, vascular, and neurological factors. Recent data show that psychological factors are involved in a substantial number of cases of erectile dysfunction (ED) alone or in combination with organic causes. However, in contrast to the advances in somatic research of erectile dysfunction, scientific literature shows contradictory reports on the results of psychotherapy for the treatment of ED.
Objectives
To evaluate the effectiveness of psychosocial interventions for the treatment of ED compared to oral drugs, local injection, vacuum devices and other psychosocial interventions, that may include any psycho‐educative methods and psychotherapy, or both, of any kind.
Search methods
The following databases were searched to identify randomised or quasi‐randomised controlled trials: MEDLINE (1966 to 2007), EMBASE (1980 to 2007), psycINFO (1974 to 2007), LILACS (1980 to 2007), DISSERTATION ABSTRACTS (2007) and the Cochrane Central Register of Controlled Trials (CENTRAL) (2007). Besides this electronic search cross checking the references of all identified trials, contact with the first author of all included trials was performed in order to obtain data on other published or unpublished trials. Handsearch of the International Journal of Impotence Research and Journal of Sex and Marital Therapy since its first issue and contact with scientific societies for ED completed the search strategy.
Selection criteria
All relevant randomised and quasi‐randomised controlled trials evaluating psychosocial interventions for ED.
Data collection and analysis
Authors of the review independently selected trials found with the search strategy, extracted data, assessed trial quality, and analysed results. For categorical outcomes the pooled relative risks (RR) were calculated, and for continuous outcomes mean differences between interventions were calculated as well. Statistical heterogeneity was addressed.
Main results
Nine randomised (Banner 2000; Baum 2000; Goldman 1990; Kilmann 1987; Kockott 1975; Melnik 2005; Munjack 1984; Price 1981; Wylie 2003) and two quasi‐randomised trials (Ansari 1976; Van Der Windt 2002), involving 398 men with ED (141 in psychotherapy group, 109 received medication, 68 psychotherapy plus medication, 20 vacuum devices and 59 control group) met the inclusion criteria. In data pooled from five randomised trials (Kockott 1975; Ansari 1976; Price 1981; Munjack 1984; Kilmann 1987), group psychotherapy was more likely than the control group (waiting list ‐ a group of participants who did not receive any active intervention) to reduce the number of men with "persistence of erectile dysfunction" at post‐treatment (RR 0.40, 95% CI 0.17 to 0.98, N = 100; NNT 1.61, 95% CI 0.97 to 4.76). At six months follow up there was continued maintenance of reduction of men with "persistence of ED" in favour of group psychotherapy (RR 0.43, 95% CI 0.26 to 0.72, N = 37; NNT 1.58, 95% CI 1.17 to 2.43).
In data pooled from two randomised trials (Price 1981; Kilmann 1987), sex‐group psychotherapy reduced the number of men with "persistence of erectile dysfunction" in post‐treatment (RR 0.13, 95% CI 0.04 to 0.43, N = 37), with a 95% response rate for sex therapy and 0% for the control group (waiting list ‐ no treatment) (NNT 1.07, 95% CI 0.86 to 1.44).
Treatment response appeared to vary between patient subgroups, although there was no significant difference in improvement in erectile function according to mean group age, type of relationship, and severity of ED. In two trials (Melnik 2005; Banner 2000) that compared group therapy plus sildenafil citrate versus sildenafil, men randomised to receive group therapy plus sildenafil showed significant reduction of "persistence of ED" (RR 0.46, 95% CI 0.24 to 0.88; NNT 3.57, 95% CI 2 to 16.7, N = 71), and were less likely than those receiving only sildenafil to drop out (RR 0.29, 95% CI 0.09 to 0.93).
One small trial (Melnik 2005) directly compared group therapy and sildenafil citrate. It found a significant difference favouring group therapy versus sildenafil in the mean difference of the IIEF (WMD ‐12.40, 95% CI ‐20.81 to ‐3.99, N = 20).
No differences in effectiveness were found between psychosocial interventions versus local injection and vacuum devices.
Authors' conclusions
There was evidence that group psychotherapy may improve erectile function. Treatment response varied between patient subgroups, but focused sex‐group therapy showed greater efficacy than control group (no treatment). In a meta‐analysis that compared group therapy plus sildenafil citrate versus sildenafil, men randomised to receive group therapy plus sildenafil showed significant improvement of successful intercourse, and were less likely than those receiving only sildenafil to drop out. Group psychotherapy also significantly improved ED compared to sildenafil citrate alone. Regarding the effectiveness of psychosocial interventions for the treatment of ED compared to local injection, vacuum devices and other psychosocial techniques, no differences were found.
Plain language summary
Psychosocial interventions for erectile dysfunction
Authors conducted a meta‐analysis to evaluate the effectiveness of psychological interventions for the treatment of erectile dysfunction (ED) compared to oral drugs, local injection, vacuum devices, or other psychological interventions. Distinct sources of randomised clinical trials (RCTs) were searched, such as electronic databases (between 1966 and 2007). We also crosschecked references and contacted scientific societies. Eleven trials involving 398 men met the inclusion criteria. Conclusions: there is evidence that group therapy (GT) improves ED in selected patients. Focused sex GT showed greater efficacy than control group. Men who received GT plus sildenafil showed significant improvement of ED and were less likely than those receiving only sildenafil to drop out. In comparing the effectiveness of psychological interventions for the treatment of ED versus local injection and vacuum devices, no difference was found.
Background
The field of erectile dysfunction treatment has expanded rapidly with the advent of oral drug therapy (Althof 2000; Althof 2002). Normal sexual function is a biopsychosocial process and relies on the coordination of psychological, endocrine, vascular, and neurological factors (Levine 2000). Recent data suggests psychological factors are involved either alone or in combination with organic causes in a substantial number of cases (Ackerman 1995; Althof 2002; Rosen 2001).
Aydin 2001 studied 115 men with ED and found an organic etiology in 43%, psychogenic in 43% and mixed in 19%. Melman 1988 studied 406 with ED and find 117 (28.8%) with organic ED,161 (39.7%) with psychogenic ED,102 (25.1%) mixed ED and 26 (6.4%) dysfunction of unknown the origin.
Psychogenic ED is defined as persistent inability to achieve and maintain an erection satisfactorily for sexual performance owing predominantly or exclusively to psychological or interpersonal factors (Rosen 2001). The main causes of psychogenic ED can be divided into three groups, each one corresponding to a different time phase: 1) immediate factors (performance anxiety); 2) prior recent life events; and 3) developmental vulnerabilities from childhood and adolescence (Althof 1989).
Epidemiologic studies have implicated the role of depressed mood, loss of self‐esteem, anxiety, and other psychosocial stresses in the cause of ED (Rosen 2001; Seidman 2001; Feldman 1994).
The results of psychotherapy in the treatment of ED, in contrast to the advances of pharmacologic interventions, is contradictory in the scientific literature (Rosen 2001; Althof 1989). Few studies have evaluated the benefits of combining drugs and psychotherapy or comparing different psychological approaches (Rosen 2001; Althof 2002; Perelman 2001). Oral drug therapies, intercavernous injections and vacuum devices are the three treatment modalities that have been most extensively evaluated in controlled studies. As noted by the National Institutes of Heath Consensus Conference of Erectile Dysfunction (NIH 1992), "outcome data of psychological and behavioral therapy have not been quantified, and the evaluation of success of these treatments is poorly documented". The aim of this review is to evaluate the effectiveness of psychological approaches for the treatment of ED.
Objectives
Evaluate the efficacy of psychosocial interventions for the treatment of ED compared to oral drugs, local injection, vacuum devices, and other psychological techniques. Evaluate the effectiveness of psychosocial interventions for the treatment of ED compared to oral drugs, local injection, vacuum devices, and other psychosocial intervention, and that may include any psycho‐educative methods or psychotherapy of any kind.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised and quasi‐randomised controlled trials evaluating psychosocial interventions for erectile dysfunction.
Types of participants
Men with diagnosis of ED based on the Diagnostic and Statistical Manual of Mental Disorders (DSM‐III, IV, or R), the International Classification of Diseases (ICD‐10) ‐ or any other described criteria ‐ , older than 18 years, of any ethnic group and nationality, regardless of comorbidities or use of concomitant medications for other diseases, with the exception of prior use of phosphodiesterase‐5 inhibitors.
Types of interventions
Any psychosocial intervention used for treating erectile dysfunction of at least four weeks duration. Psychosocial interventions may include any psycho‐educative methods or psychotherapy of any kind, as long as they are described by the authors.
Types of outcome measures
1. Effectiveness measured by: a) changes in the status of illness, measured by validated questionnaires (e.g. International Index of Erectile Function, Golombok Rust Inventory of Sexual Satisfaction); b) number of patients per treatment group who did not show successful sexual intercourse; c) number of successful sexual intercourse; d) relapse rates characterised by measures of erectile function status.
2. Treatment acceptability as measured by: a) treatment compliance; b) number of dropouts during the trial; c) number of subjects who dropped out because of lack of efficacy or for feelings of worsening associated to psychosocial intervention; d) attendance to psychosocial appointments.
3. Other: a) quality of life; b) satisfaction with the treatment; c) improvement in depression or anxiety indices.
Search methods for identification of studies
The following electronic databases were searched: MEDLINE (1966 to 2007), EMBASE (1980 to 2007), PsycLIT (1974 to 2007), LILACS (1980 to 2007), the Cochrane Central Register of Controlled Trials (CENTRAL) (2007), and Dissertation Abstracts (2007). The 'optimal' MEDLINE, EMBASE and LILACS sensitive search strategies for identification of RCTs and systematic reviews were combined with the following phrases: 1. (erectile dysfunction*) OR (impoten* ) OR ( erection failure) OR (male sexual dysfunction) 2. psychotherap* OR (psychosocial intervention) OR (psychoeducation) OR (coping skills) OR (brief motivational counseling) OR ( sexual therapy) OR ( anxiety management training) OR (marital therapy) OR (group therapy) OR (cognitive therapy) OR (behavio* therapy) OR (focal therapy*) OR (general counseling) OR (psychodynamic therapy) OR (supportive therapy) OR (psychoanalyses) OR (interpersonal therapy) OR (cognitive therapy) OR (individual therapy) OR (couples therapy) OR (waiting list) 3. #1 AND #2
In addition we: 1) crosschecked references of all identified trials; 2) contacted with pharmaceutical companies in order to obtain data on unpublished trials; 3) contacted the first authors of all included trials to obtain further information or information regarding unpublished trials; 4) handsearched the International Journal of Impotence Research and Journal of Sex and Marital Therapy since its first issue; and 5) contacted scientific societies for ED.
Data collection and analysis
Two reviewers (TM and BGOS) independently selected trials found with the search strategy, extracted the data, assessed trial quality and analysed the results. In case there were disagreements, the third reviewer (AGN) was consulted, and in the case consensus was not reached, data was not included in this review until the authors of the trial resolved the question.
SELECTION OF TRIALS Reviewers screened the abstracts of all publications obtained by the search strategy. The articles potentially suitable for the review were obtained in full to assess relevance based on inclusion criteria.
QUALITY ASSESSMENT The quality of each trial were based on the criteria of quality established in the Cochrane Handbook, which measures a wider range of factors, including:
1) minimisation of selection bias a) was the randomisation procedure adequate? b) was the allocation concealment adequate?
2) minimisation of attrition bias a) were the withdrawals and dropouts described completely? b) was analysis by intention to treat?
3) minimisation of detection bias a) were outcome assessors blind to the intervention?
Based on this criteria, studies were classified according to criteria described in the Cochrane Handbook. A ‐ Low risk of bias (all the quality criteria met) B ‐ Moderate risk of bias (quality criteria partially met) C ‐ High risk of bias (one or more criteria not met)
DATA EXTRACTION Intervention and outcomes were extracted independently by reviewers using a standard data extraction form.
ANALYSIS Relative risks (RR) with 95% confidence intervals (CI) were estimated for dichotomous data using a fixed‐effects model if no heterogeneity was present and according to an intention‐to‐treat analysis. If possible, the number needed to treat (NNT) and number needed to harm (NNH) were calculated.
Continuous outcomes were analysed if the mean and standard deviation of endpoint measures were presented in original articles. For the meta‐analysis of continuous outcomes, weighted mean differences (WMD) between groups were estimated. Only nonskewed data are presented in this review.
Heterogeneity was assessed by chi‐square test and was assumed to be present when significance was less than 0.1 (P < 0.1). When significant heterogeneity was present, the random‐effects model was applied and attempts were made to explain the differences based on clinical characteristics of the included studies and in the subgroup analysis. Potential publication bias was assessed by a funnel graph (trial effect versus trial size).
SUBGROUP ANALYSIS Subgroups considered for evaluation included: a) patients < 40 years old versus patients ≥ 40; b) subjects with psychogenic erectile dysfunction versus organic ED versus mixed aetiology; c) duration of follow up ‐ 4 weeks versus 8 weeks versus 12 weeks versus 16 weeks versus 20 weeks versus 24 weeks or longer.
Results
Description of studies
SEARCH
The search strategy generated 2184 references: MEDLINE (n = 1019); Cochrane Library (n = 78), EMBASE (n = 454), LILACS (n = 127), psycINFO (n = 501); and Dissertation Abstracts (n = 5). Two papers were identified by crosschecking references. Twenty‐two full papers were evaluated and are listed in this review. INCLUDED STUDIES
For detailed information see 'Table of included studies'.
Nine randomised controlled trials (Banner 2000; Baum 2000; Goldman 1990; Kilmann 1987; Kockott 1975; Melnik 2005; Munjack 1984; Price 1981; Wylie 2003) and two quasi‐randomised trials (Ansari 1976; Van Der Windt 2002) fulfilled the study inclusion criteria. Although no restrictions were made in terms of languages of original reports, all studies included were published in English.
Duration of trials Duration of included trials covered 4 weeks to 12 months.
Participants The 11 trials evaluated 398 men with a mean age 47.4 years old. Half of them were from the USA. Baseline ED severity was estimated in all trials. Diagnosis were stated as primary erectile dysfunction (n = 2) and secondary ED (n = 9). The most common range of age inclusion was 18 years and older, with ED of at least 3 to 6 months duration. Exclusion criteria applied in most trials included genital anatomic deformity, primary nonerectile sexual disorder (e.g., hypoactive sexual disorder), hyperprolactinaemia, hypogonadism, major psychiatric disorders not well controlled with therapy (including schizophrenia and major depression), and alcohol or substance abuse.
Types of interventions Considering the diversity of psychosocial interventions, psychotherapy models were categorised according to their theoretical base, as described below.
a) Rational‐Emotive Therapy (RET). Incorporating core elements of both behavioural and cognitive models, RET challenges negative automatic thoughts and dysfunctional underlying beliefs maintaining erectile dysfunction through collaborative 'hypothesis‐testing', behavioural tasks, and skills training. A number of cognitive‐behavioural therapies guided by manuals have been designed, including problem‐solving therapy and self‐control therapy, and are conducted over 12 to 16 sessions. Key elements of the model are psychoeducational and cognitive intervention, sexual and performance anxiety reduction, script assessment and modification, conflict resolution and relationship enhancement, and relapse‐prevention training (Ellis 1992).
b) Sex Group Therapy (GT). Developed specifically as a time‐limited (8 ‐ 16 sessions) therapy for erectile dysfunction. GT uses the connection between erectile dysfunction and current interpersonal experiences, and includes social skills training and homework assignments that address anxiety in sexual situations, education and information about male sexuality generally, communication training, myths about male sexuality, non‐demand pleasuring, and permission to engage in self‐pleasuring (Rosen 1995).
c) Modified Masters Johnson Therapy. This approach is based on the notions that sexual dysfunction can have many causes, and can be tackled effectively with treatment programs that combine education, homework assignments and counseling (Masters 1970).
d) Educational Intervention. Workshops focused on disseminating information about psychological and physiological changes that occur during sexual response (Goldman 1990).
e) Systematic desensitization. A behaviour therapy technique often used for the treatment of sexual dysfunction in which deep muscle relaxation is used to reduce the anxiety associated with certain situations (Rimm 1987).
Setting All studies included outpatients and were carried out in the United States of America (N = 6), Netherlands (N = 1), England (N = 2), Germany (N = 1), and Brazil (N = 1).
Sample size Studies included between 16 and 70 participants.
EXCLUDED STUDIES
Five studies were excluded because they were not controlled studies (Hartmann 1993; Hawton 1986; Reynolds 1981; Lobitz 1979; Zilbergeld 1975). Most were case reports or case series without a group control. Two studies was excluded because the patients had mixed sexual dysfunction that was not compatible with the review protocol (Golden 1978; Stravynski 1997).
AWAITING ASSESSMENT
Three studies (Phelps 2004; Everaed 1985; Takefman 1984) are awaiting assessment. They all state that they are randomised controlled studies, but their outcomes could not be evaluated properly for the meta‐analysis, mainly due to lack of information (no mention of mean and standard deviation for the main outcomes evaluated). First authors were contacted to seek additional information, but no relevant data were collected.
Risk of bias in included studies
RANDOMISATION
From the nine trials that reported themselves as randomised, just three described a clearly adequate method of allocation concealment, with the use of sealed envelopes (Melnik 2005; Wylie 2003;Banner 2000). Therefore, a Cochrane quality criteria (Schulz 1995) rating of 'A' was given for these studies. Ansari 1976 is a controlled study, using a quasi‐randomisation method. In Van Der Windt 2002, the allocation procedure was done alternatively by a researcher.
BLINDNESS
Blindness is a difficult procedure in psychotherapy studies. There is the possibility of blinding the outcomes' evaluator, and this was described by Melnik 2005. Munjack 1984, Van Der Windt 2002, and Banner 2000.
Melnik 2005 used independent researchers who were unaware of the patient's treatment allocation. Van Der Windt 2002 used a challenge test that was conducted by a researcher who was blinded.
DESCRIPTION OF DROPOUTS
All the studies described those who dropped out before the end of the trial protocol. Dropout rates ranged from 0% (Kockott 1975) to 52% (Baum 2000). The higher dropout rate compared psychotherapy with local injection (Baum 2000).
INTENTION TO TREAT ANALYSIS
Only one study (Wylie 2003) carried out an intention‐to‐treat analysis.
OUTCOME REPORTING
Some outcomes could not be summarised because of poor description of outcomes in the main publications. In some situations there were no numbers; they were presented in graphical form only or with statistical language and P values. For many continuous variables standard deviations were not provided.
Effects of interventions
The 11 studies in this review (Ansari 1976; Banner 2000; Baum 2000; Goldman 1990; Kilmann 1987; Kockott 1975; Melnik 2005; Munjack 1984; Price 1981; Van Der Windt 2002; Wylie 2003) examined eight comparisons. Some results could be pooled or summarised, as they were homogeneous. Intention‐to‐treat analysis was performed if all applicable data were available.
The following scales were used in included studies: International Index of Erectile Function (IIEF); Sexual Interaction Inventory (SII); ASKAS Knowledge Scale (AKLS); ASKAS Attitude Scale (AKAS); Fear of negative evaluation (FNE); and Success/experience patient weekly report form. For most of these scales data were skewed and could not be presented by graphical form or subject to meta‐analysis. Many continuous outcomes were described with means without corresponding standard deviations.
GROUP PSYCHOTHERAPY (GT) VERSUS WAITING LIST (WT)
Group psychotherapy produced a statistically significant improvement in erectile function compared to control group (waiting list ‐ no treatment). A meta‐analysis of five trials comparing group therapy to control group (waiting list ‐ no treatment) to evaluate the 'persistence of erectile dysfunction' found significant differences between group therapy and control group (RR 0.40, 95% CI 0.17 to 0.98, N = 100; NNT 1.61, 95% CI 0.97 to 4.76) (Kilmann 1987; Munjack 1984; Price 1981; Ansari 1976; Kockott 1975).
At six months follow up, there was a continued maintenance of reduction of men with "persistence of ED" in favour of psychotherapy (RR 0.43, 95% CI 0.26 to 0.72, N = 37; NNT 1.58, 95% CI 1.17 to 2.43) (Munjack 1984; Price 1981).
Subgroup analysis Effectiveness by type of psychotherapy
Rational‐emotive therapy (RET) Munjack 1984 conducted a study involving 16 self‐referred men (aged 19 to 63, mean 47.5) presenting with secondary erectile failure. Subjects in this study were required to meet the following inclusion criteria: (a) "a primary complaint of erectile failure with satisfactory erections less than 25% of the time"; (b) persistent complaints of erectile problems for more than 6 months; (c) no organic etiology of erectile problems as judged by a medical evaluation, testosterone and prolactin levels, and the presence of morning erections; and (d) willingness to attend therapy sessions, screening, and assessment. Subjects were excluded from this study if they were taking psychoactive medication, undergoing psychiatric or psychological treatment, or if they had a history of homosexuality, drug abuse, alcoholism, schizophrenia, bipolar disorder, or other major psychiatric disorders.
Subjects in this study were randomly assigned to either a treatment group or a wait‐list control (WLC) group. Treatment consisted of six weeks of biweekly rational‐emotive therapy (RET) sessions designed to correct cognitive distortions that are hypothesized to hinder sexual functioning. Treatment was administered a by graduate student in psychology with specialty training in RET. Measures used in this study included a pretreatment assessment of the severity of the erectile disorder as evaluated using a ratio of successful attempts at intercourse compared to the total number of attempts. Numbers in this ratio were self‐reported retrospectively for the two weeks prior to the assessment. During the treatment phase, subjects were required to compute the success/attempt ratio each week.
Data from the intercourse success/attempts ratio indicated that during the six‐week course of the study in the treatment group all the subjects achieved successful intercourse and only one in the WLC during the study period. Furthermore, the reduction of men with "persistence of ED" favoured psychotherapy (RET) (RR 0.07, 95% CI, 0.00 to 1.00, N = 16, P = 0.05). Follow‐up data for success/attempts ratios were collected for subjects in the RET group at six to nine months post‐treatment and revealed that treatment gains were partially maintaining. Specifically, three subjects of the treatment group had ratio scores of 0%.
Sex‐group therapy Price 1981 conducted a study involving 21 men without partners who presented with erectile difficulties. On the basis of medical consultation, it was determined that none of the subjects' erectile difficulties was attributable to organic aetiologies. Client selection criteria were as follows: (a) a presenting complaint of erectile dysfunction, defined by the male reporting dissatisfaction with his ability to obtain and/ or maintain erections; (b) the male had no steady sexual partner and was not dating at a frequency greater than twice per week; and (c) clients were willing to fulfil study requirements, including attendance at weekly sessions and completion of homework assignments and all questionnaires.
Treatment consisted of weekly, two‐hour group sessions administered by two dual, sex‐therapy teams. Authors reported that each session commenced with the collection of homework assignments from the previous week ‐ including discussion of progress, problems and concerns ‐, presentation of didactic information, seeing films, role playing, and assignment of homework assignments to be completed prior to the next session. Authors provided an outline of the objectives of each session and associated homework assignments. For example, during session three the didactic presentations and discussion topics included presentation of female sexual anatomy and physiology and discussion of the use of fantasy. Homework following session three is described as "tactile exploration: personal erotic fantasy development and tactile exploration". Subjects were also asked to prepare maintenance programs in which they identified the original problems that brought them to treatment, the specific things that they had learned that was beneficial in the resolution of the problem, potential future problems, and potential solutions. It was reported that sessions were supplemented with bibliotherapy, but did not elaborate on the literature provided to subjects.
With regard to clinical outcomes, 14 of the 14 treatment subjects reported improvement with their erectile functioning. All 7 WLC members reported "no change".
Data were collected at six months following treatment. Ten of the 14 subjects in the treatment arm reported improvement in satisfaction with changes in erectile functioning compared with pretreatment functioning.
Kilmann 1987 studied the effects of three group treatment formats on 20 men with secondary erectile dysfunction. After a comprehensive medical and psychological screening, each couple was assigned to one of three treatment groups (Communication Technique Training, Sexual Technique Training, Combination Treatment) or to one of two control groups (Attention‐Placebo, No Treatment). Couples in the three treatment groups and the attention‐placebo group participated in their respective formats in twice weekly sessions for a total of 20 hours. The no‐treatment control group received sex education and treatment after a five‐week, waiting‐list period.
Although these two studies individually failed to show significant differences favouring sex‐group therapy over waiting list for "persistence of erectile dysfunction", the meta‐analysis of these trials favoured the active intervention group (RR 0.13, 95% CI 0.04 to 0.43, N = 37),(Kilmann 1987; Price 1981), with 95% of response for sex therapy and 0% for the waiting‐list group (NNT 1.07, 95% CI 0.86 to 1.44).
The mean percentage per participant of intercourse attempts that were successful appeared greater for sex‐group therapy compared to others types of group interventions (Rational‐Emotive Therapy, Systematic Desensitization, Masters and Johnson Modified Therapy). Three treatment groups (Masters and Johnson Modified Therapy (Ansari 1976), Systematic Desensitization (Kockott 1975), Rational‐Emotive Therapy (Munjack 1984)) demonstrated substantial gains in success/experience intercourse rates but were not statistically significant (respectively P = 0.14, P = 0.27, 1984, P = 0.05).
Effectiveness by the severity of erectile dysfunction
Men categorized at baseline as having primary ED appeared less likely than those with secondary ED to experience improved erections and successful sexual intercourse. However, for men in both categories of ED severity, primary (RR 0.57, 95% CI 0.40 to 0.82, N = 71) (Kockott 1975; Ansari 1976; Munjack 1984) and secondary (RR 0.10, 95% CI 0.02 to 0.40, N = 29) (Price 1981; Kilmann 1987), group therapy produced significantly better results than waiting list for "persistence of erectile dysfunction".
Effectiveness by the mean age of patients
In a subgroup analysis comparing one study with men between 30 and 39 years old (Kockott 1975) to four studies with men aged 45 years and older (Price 1981; Ansari 1976; Kilmann 1987; Munjack 1984), no statistical differences were identified.
Effectiveness according to partnership
In a subgroup analysis dividing studies with men with fixed partnerships (Ansari 1976; Kilmann 1987; Munjack 1984; Kockott 1975) (P = 0.0006) and men without fixed partnerships (Price 1981), only men without fixed partnership had a statistically significant difference (P = 0.02).
PSYCHO‐EDUCATIONAL INTERVENTION VERSUS NO TREATMENT Goldman 1990 studied the effect of a psychoeducational intervention as an adjunct to treatment of erectile dysfunction in older couples. Twenty couples who presented to a multidisciplinary centre for erectile dysfunction were recruited for participation. Inclusion criteria were as follows: (a) between the ages of 55 and 75; (b) heterosexual; (c) in an ongoing relationship of at least six months duration; (d) had experienced secondary erectile dysfunction; and (e) exhibited no major psychiatric disorder or severe marital distress at initial evaluation.
Assessments were conducted at intake and immediately following treatment. A qualitative interview was also conducted with subjects in the treatment condition "at the time of follow‐up". Treatment consisted of an educational workshop of unspecified length. The goals of the workshop were to (a) increase knowledge levels about the sexual response cycle and normal age‐associated changes that occur in the cycle, (b) increase comfort levels with regard to the discussion of sexuality, (c) increase satisfaction with participants' expression of sexuality, and (d) increase participants' acceptance of their sexual difficulties.
Although the workshop group had improvement in the levels of ASKIS Knowledge Scale, data analysis revealed that the workshop participants reported no significant increases (WMD ‐5.65, 95% CI ‐14.74 to ‐3.44, N = 20). Scores on the ASKAS Attitude Scale (WMD 0.70, 95% CI ‐23.28 to 24.68, N = 20) and the Sexual Interaction Inventory: mean pleasure (WMD 0.20, 95% CI ‐0.32 to ‐ 0.72, N = 20) revealed no statistically significant changes in scores from pre‐ to post‐treatment when comparing the workshop group to controls.
GROUP INTERVENTIONS
Systematic desensitization versus conventional medication plus general advice (routine group therapy) versus waiting list
Kockott 1975 conducted a study to assess the therapeutic effectiveness of systematic desensitization of ED. Three groups of eight patients each were formed. They were treated with systematic desensitization or conventional medication plus general advice (routine group therapy), or put on a waiting list. Therapeutic effects were investigated on the behavioral, subjective, and physiological levels.
There were no significant differences among the systematic desensitization group and routine group therapy in "persistence of erectile dysfunction" (RR 1.00, 95% CI 0.47 to 2.14, N = 16, P = 1.00).
Group interventions versus drug therapy Group therapy versus sildenafil citrate One small study (Melnik 2005) directly compared group therapy versus sildenafil citrate in the treatment of ED. This study found a significant difference favouring group therapy versus sildenafil in the mean score of the International Index of Erectile Function (IIEF) (WMD ‐12.40, 95% CI ‐20.81 to ‐3.99, N = 20, P = 0.004). Two of 10 patients (20%) reported "persistence of ED" in the psychotherapy group in post‐treatment versus 6 of 10 (60%) in the sildenafil group. There was also a significant difference at three months follow up (WMD ‐9.67, 95% CI ‐17.03 to ‐2.31, N = 20), and for the numbers of dropouts ‐ higher in sildenafil ‐ between the two groups (WMD 0.38, 95% CI 0.05 to 2.77, N = 20).
Group therapy plus sildenafil citrate versus sildenafil citrate Two studies (Banner 2000; Melnik 2005) compared group therapy plus sildenafil citrate versus sildenafil citrate in the treatment of ED. The meta‐analysis found a significant statistical difference between the two groups for successful attempts at intercourse, and favoured combined therapy (RR 0.46, 95% CI 0.24 to 0.88; NNT 3.57, 95% CI 2 to 16.7, N = 71). There was also a significant difference in the number of dropouts between the two groups, again favouring the combined therapy group (RR 0.29, 95% CI 0.09 to 0.93, N = 77).
Group therapy versus oxazepam
Little information is available regarding the efficacy of oxazepam for ED. Results from one trial (Ansari 1976) did not reveal a statistical difference between group therapy versus oxazepam (RR 0.76, 95% CI 0.30 to 1.92, N = 37).
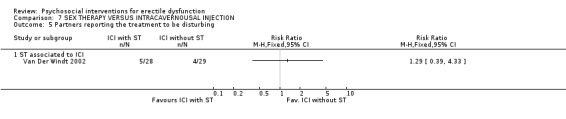
Intracavernosal injection (ICI) plus sex therapy (SC) versus ICI alone Van Der Windt 2002 compared intracavernosal injection (ICI) therapy with and without sexological counseling in men with erectile dysfunction. In a randomised study men were alternately assigned to ICI without sexological counseling or with sexological counseling. In all, 70 patients were included, with 35 in each group. Fifty‐seven (28 without SC, 29 with SC) were interviewed by telephone after a mean follow up of 11.3 months to determine their use of ICI and reasons for discontinuing.
There were no differences between the groups in discontinuation of ICI (overall 30%, P = 0.35), in reasons for discontinuing ICI (24% did so because of the return of spontaneous erections), or in sexual functioning.
In comparing "persistence of erectile dysfunction", no significant results were found (P = 0.24).
Van Der Windt 2002 presented data on "partners reporting the treatment to be disturbing", and found no differences between ICI and counseling (RR 1.29, 95% CI 0.39 to 4.33).
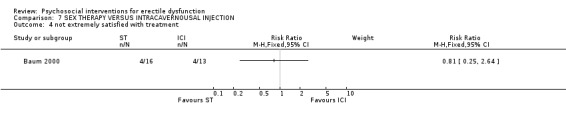
Sex therapy versus intracavernosal injection Baum 2000 compared standard sex therapy versus self‐injected, low‐dose prostaglandin E1 (PGE1). Fifty men with psychogenic ED were divided into two groups: standard sex therapy for twelve weeks; or treatment using low dose (2.5 to 5.0 µg) PGE1.
For "persistence of erectile dysfunction" as well as dropout rates, there were no significant differences between groups (P = 0.25 and P = 0.40, respectively).
Sixty‐nine percent of patients in the PGE1 group were satisfied with their treatment compared to 75% receiving sex therapy. There was no statistical difference (RR=0.81, 95% CI 0.25 to 2.64).
The frequency of intercourse reported in patient diaries for the two groups was similar (20.5 per month for PGE1 versus 20.0 per month for sex therapy). The reported duration of erection by patients receiving PGE1 therapy was longer than that reported by those receiving sex therapy (35 minutes versus 10 minutes).
One relevant aspect described in this study is a comparison of costs of treatment. Sex therapy was approximately 25% more expensive than the PGE1 treatment.
A meta‐analysis of two trials comparing sex therapy to PGE1 (Baum 2000; Van Der Windt 2002) did not find a significantly statistical difference for "persistence of erectile dysfunction" (RR 1.11, 95% CI 0.62 to 1.97, N = 86). However, a trend was observed favouring sex therapy in Baum 2000.
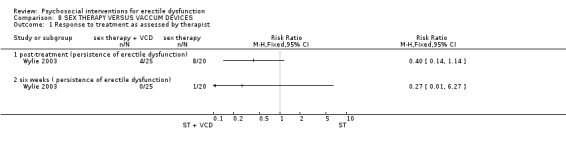
Sex therapy versus vacuum devices Wylie 2003 studied 45 patients diagnosed with predominantly psychogenic erectile dysfunction. They were randomised to a vacuum constriction device (VCD) (N = 25) (also known as a vacuum erectile device) at the second session (group 1). The other group (N = 20) was randomised to psychotherapy without VCD.
Twenty‐one couples (84%) in group 1 reported improvement after the initial psychotherapy and VCD sessions compared with group 2, in which 12 of the 20 couples (60%) reported improvement after couples psychotherapy. We subsequently found that three of the four couples in group 1 reporting no improvement had not used the pump provided.
Results did not reveal any difference between psychotherapy with VCD and psychotherapy without VCD after three weeks of treatment (RR 0.40, 95% CI 0.14 to 1.14, N = 45) and after six weeks of treatment (RR 0.27, 95% CI 0.01 to 6.27, N = 45).
Discussion
As far as we know this review is the first attempt of a meta‐analysis of randomised controlled trials relevant to psychosocial interventions for erectile dysfunction.
This review confirmed that there is, in fact, a dearth of well‐designed research on psychotherapy for erectile dysfunction. Our literature search identified around 2200 references on the topic, but only 11 studies could be re‐analysed and presented by the criteria of random assignment and a controlled condition. Of the 22 studies eligible for inclusion, seven had methodological flaws or contained insufficient information to allow inclusion (Golden 1978; Hartmann 1993; Hawton 1986; Lobitz 1979; Reynolds 1981; Stravynski 1997; Zilbergeld 1975).
General results of this systematic review found that group psychotherapy were effective in treating erectile dysfunction (Ansari 1976; Kilmann 1987; Munjack 1984; Price 1981; Kockott 1975). Related to the type of psychotherapy, two trials (Kilmann 1987; Price 1981) showed the superiority of group therapy focused on sexuality. Sex therapy is a well established form of treatment (Masters 1970). Since then the treatment programme has been modified in various ways and other treatment approaches introduced (Rosen 2001; LoPiccolo 1986).
Regarding subgroup analysis, no differences were found related to the severity of ED, type of partnership and mean group age. Although the potential roles of these differences in characteristics in the literature are negatively related to 'good prognosis' (Rosen 2001), the variation in efficacy outcomes cannot be evaluated in the included studies. A range of factors makes it difficult to draw conclusions from the subgroup analysis, and include small samples sizes, differences in study design, definitions of outcome variables, and varying amounts of psychotherapy provided.
Only one study, Melnik 2005, found a significant difference favouring group therapy versus sildenafil in mean score of IIEF. The rate of dropout was higher in the sildenafil group (4 versus 2). This result suggests despite the overall efficacy of sildenafil and its worth in treating ED, oral drug therapy is not always effective when used alone (Rosen 2001; Althof 2002). Sometimes the single use can reveal or reinforce other sexual problems, such as lack of sexual desire and premature ejaculation. In some cases, other issues may come to light following unsuccessful or successful use of sildenafil (LoPiccolo 1986). For some couples sexual problems represents a neurotic reaction for deep relational conflicts, lack of communication, or power struggles, and drug therapy may not be a solution to these conflicts (Rosen 2001).
Significant differences also were found in the rate of "persistence of erectile dysfunction" between group therapy plus sildenafil citrate and the sildenafil only for post‐treatment (Banner 2000; Melnik 2005). Strengths of these studies included inclusion of pretreatment assessments (careful clinical history and psychiatric evaluation, focused urological evaluation, and selected laboratory tests) and the use of blind raters.
One study, Ansari 1976, compares benzodiazepines, particularly oxazepam versus psychotherapy, and found no difference between the two treatments.
Overall, no significant differences were found for any of the efficacy measures in comparison of sex therapy and ICI (Baum 2000; Van Der Windt 2002). However, satisfaction with treatment revealed that 69% of patients in the PGE1 group were satisfied with their treatment compared to 75% receiving sex therapy (Baum 2000).
Early combination treatment of psychotherapy plus a physical treatment such as VCD may lead to a beneficial response in men with ED compared to therapy alone. Eighty‐four percent of couples reported some improvement after the initial psychotherapy and VCD sessions compared with 60% who reported some improvement in group 2 (Wylie 2003). However, no significant differences were found for any of the efficacy measures between psychotherapy with VCD and psychotherapy without a VCD after three and six weeks of treatment.
Although we limited our analysis to randomised and quasi‐randomised controlled trials, the majority of the studies had potential methodological flaws. Just three studies described a clearly adequate method of allocation concealment, with the use of sealed envelopes. Other limitations were related to small samples, limited length of follow up, validated outcomes, not reporting of intention‐to‐treat analyses, and variability in study design. Consequently, we were often unable to pool data, limiting our analyses to erectile dysfunction remission and dropout rates. We could not access important issues like improvement in quality of life and impact of the interventions in relationship satisfaction. Meta‐analyses are less robust with small trials and thus the results should be interpreted with caution.
The availability of oral therapy has significantly altered the way in which erectile dysfunction is treated. While this medication is effective in restoring erectile function, it is often necessary to include the psychological and behavioural aspects of patients' diagnosis and management, as well as considering organic causes and risk factors. Integrating sex therapy and other psychological techniques into office practice will improve effectiveness in treating ED.
LACK OF DATA Only eleven trials were identified that could be used in this systematic review. Five studies compared psychotherapy versus control group (waiting list ‐ no treatment) (Price 1981; Ansari 1976Munjack 1984 ; Kilmann 1987; Kockott 1975). One compared different types of psychotherapy (Kockott 1975). Another compared psycho‐educational interventions versus waiting list (Goldman 1990). Three studies compared psychotherapy and drug therapy (Ansari 1976; Melnik 2005; Banner 2000), and two compared psychotherapy and intercavernous injections (Baum 2000; Van Der Windt 2002). Only one compared psychotherapy versus VCD (Wylie 2003).
Authors' conclusions
Implications for practice.
Group psychotherapy improves erectile function in selected individuals. Treatment response seems to vary between patient subgroups, but focused sex group therapy showed greater efficacy than waiting list. In a meta‐analysis that compared sildenafil versus group therapy plus sildenafil citrate, men randomised to receive group therapy showed significant improvement for successful intercourse and were less likely than those receiving only sildenafil to drop out. One study revealed that group psychotherapy had significantly higher scores compared with patients who were exclusively treated with sildenafil citrate. Regarding the effectiveness of psychosocial interventions for the treatment of ED compared to local injection, vacuum devices, and other psychological techniques, no differences were found.
With the evidence currently available, there are data supporting the efficacy of group therapy, in particular focused sex‐group therapy. Further studies are required. We need large randomised trials with longer follow ups in order to examine whether psychosocial interventions alone help patients with erectile dysfunction. These studies would need to take account the study setting, as this may have a confounding effect on the results. The questions that should be raised are whether one psychosocial intervention is more effective than another. Does the effectiveness depend upon personality factors, psychiatric comorbid diagnosis, length of therapy time, severity of erectile dysfunction, or any other factors? The randomised trials should clearly state the method of randomisation, allocation concealment, blinding (where possible), perform intention‐to‐treat analysis, and with power calculations performed prior to the trial. More pragmatic studies can be designed and delivered that provide usable data for better understanding this important component of intervention in the field of ED.
Inherent problems in the of field erectile dysfunction are recruitment difficulties, motivation of patients, study adherence, blinding, follow‐up difficulties, questionable results, high attrition rates, low study completion rates, and comparable, unintended selection of highly motivated patients.
Given the overall benefit of psychosocial interventions, the absence of a clear explanation about how they work means more work is urgently needed to identify which patient is likely to benefit most from what kind of treatment. At the clinical level, patient screening and selective assignment or referral for psychological therapy appears to be more cost efficient than giving all patients the same amount and type of intervention.
Implications for policy Globally, great emphasis is placed on the vital role of psychosocial treatments for the management of erectile dysfunction. However, this is despite a dearth of good evidence on the overall value of psychosocial treatments. Policy makers need to ensure that a better evidence base is developed around psychosocial treatment to assist in the future rationale planning of interventions for erectile dysfunction.
Implications for research.
Well conducted and reported randomised controlled trials are essential to establish the effectiveness of psychosocial interventions for erectile dysfunction.
Large randomised trials with longer follow up to examine whether psychosocial interventions help patients with erectile dysfunction are needed. These studies would need to take account of the study setting as this may have a confounding effect on the results. The questions that should be raised are whether one psychosocial intervention is more effective than another. Does the effectiveness depend upon personality factors, psychiatric co‐morbid diagnosis, length of therapy time, severity of erectile dysfunction use or any other factors?
The randomised trials should clearly state the method of randomisation, allocation concealment, blinding (where possible), perform intention‐to‐treat analysis, and with power calculations performed prior to the trial. More pragmatic studies can be designed and delivered that provide usable data for better understanding this important component of intervention in the field of sexuality.
Inherent problems in the of field of psychosocial interventions for sexual disorders are recruitment difficulties, motivation of patients, study adherence, blinding, follow‐up difficulties, questionable results, high attrition rates, low study completion rates, and comparable, unintended selection of highly motivated patients.
What's new
| Date | Event | Description |
|---|---|---|
| 24 March 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 3, 2004 Review first published: Issue 3, 2007
| Date | Event | Description |
|---|---|---|
| 30 March 2007 | New citation required and conclusions have changed | Substantive amendment |
Data and analyses
Comparison 1. GROUP THERAPY (GT) VERSUS WAITING LIST (WT).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 persistence of erectile dysfunction | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 post‐treatment | 5 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.17, 0.98] |
| 1.2 at 6 months follow up | 2 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.26, 0.72] |
| 2 persistence of erectile dysfunction ‐ according to type of group intervention | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 rational emotive therapy | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.00] |
| 2.2 sex group therapy | 2 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.04, 0.43] |
| 2.3 systematic desensitization | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.39, 1.30] |
| 2.4 Masters and Johnson Modifed technique | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.50, 1.10] |
| 3 persistence of erectile dysfunction ‐ according the severity of ED | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 primary ED | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.40, 0.82] |
| 3.2 secondary ED | 2 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.04, 0.43] |
| 4 persistence of erectile dysfunction ‐ according to the group mean age of the patients | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 from 30 to 39 years old | 1 | 16 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.39, 1.30] |
| 4.2 45 years and older | 4 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.04, 1.21] |
| 5 persistence of erectile dysfunction ‐ according to partnership | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 male with fixed partnership | 4 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.38, 0.77] |
| 5.2 male without fixed partnership | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.04 [0.00, 0.55] |
1.1. Analysis.
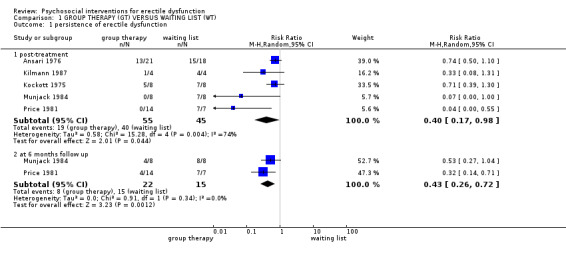
Comparison 1 GROUP THERAPY (GT) VERSUS WAITING LIST (WT), Outcome 1 persistence of erectile dysfunction.
1.2. Analysis.
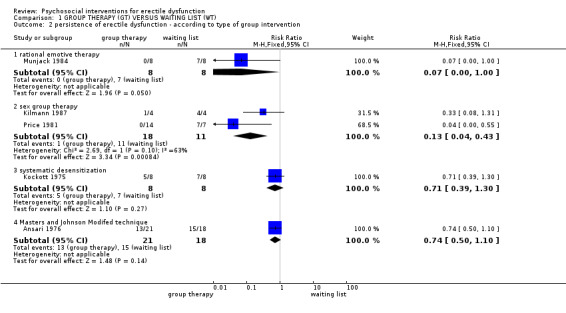
Comparison 1 GROUP THERAPY (GT) VERSUS WAITING LIST (WT), Outcome 2 persistence of erectile dysfunction ‐ according to type of group intervention.
1.3. Analysis.
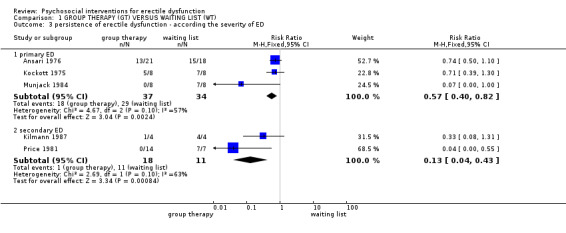
Comparison 1 GROUP THERAPY (GT) VERSUS WAITING LIST (WT), Outcome 3 persistence of erectile dysfunction ‐ according the severity of ED.
1.4. Analysis.
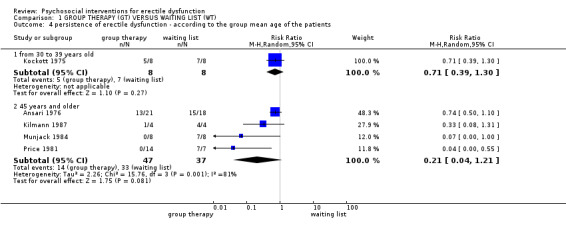
Comparison 1 GROUP THERAPY (GT) VERSUS WAITING LIST (WT), Outcome 4 persistence of erectile dysfunction ‐ according to the group mean age of the patients.
1.5. Analysis.
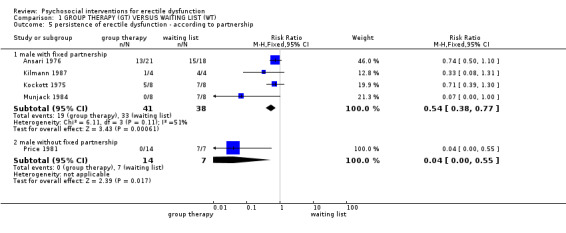
Comparison 1 GROUP THERAPY (GT) VERSUS WAITING LIST (WT), Outcome 5 persistence of erectile dysfunction ‐ according to partnership.
Comparison 2. PSYCHOEDUCATIONAL INTERVENTION VERSUS NO TREATMENT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ASKAS Knowledge Scale (low is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 ASKAS Attitude Scale (low is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Sexual Interaction Inventory: mean pleasure (high is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
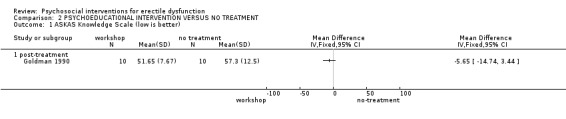
Comparison 2 PSYCHOEDUCATIONAL INTERVENTION VERSUS NO TREATMENT, Outcome 1 ASKAS Knowledge Scale (low is better).
2.2. Analysis.
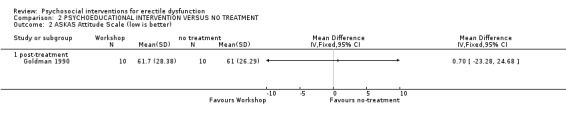
Comparison 2 PSYCHOEDUCATIONAL INTERVENTION VERSUS NO TREATMENT, Outcome 2 ASKAS Attitude Scale (low is better).
2.3. Analysis.
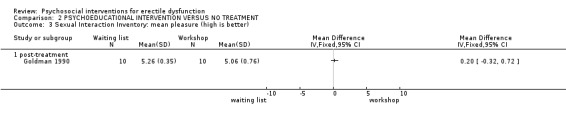
Comparison 2 PSYCHOEDUCATIONAL INTERVENTION VERSUS NO TREATMENT, Outcome 3 Sexual Interaction Inventory: mean pleasure (high is better).
Comparison 3. GROUP INTERVENTIONS: SYSTEMATIC DESENSITIZATION VERSUS ROUTINE GROUP THERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 persistence of erectile dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 post‐treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
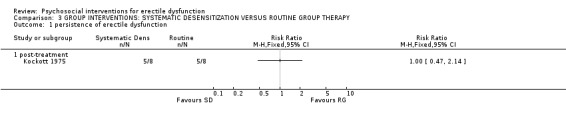
Comparison 3 GROUP INTERVENTIONS: SYSTEMATIC DESENSITIZATION VERSUS ROUTINE GROUP THERAPY, Outcome 1 persistence of erectile dysfunction.
Comparison 4. GROUP THERAPY VERSUS SILDENAFIL CITRATE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 International Index of Erectile Dysfunction (high is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 3 months follow up | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Dropouts | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
4.1. Analysis.

Comparison 4 GROUP THERAPY VERSUS SILDENAFIL CITRATE, Outcome 1 International Index of Erectile Dysfunction (high is better).
4.2. Analysis.
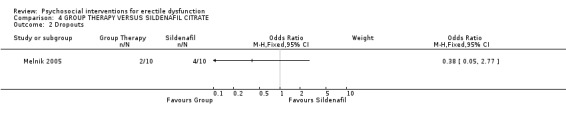
Comparison 4 GROUP THERAPY VERSUS SILDENAFIL CITRATE, Outcome 2 Dropouts.
Comparison 5. GROUP THERAPY PLUS SILDENAFIL VERSUS SILDENAFIL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Persistence of erectile dysfunction | 2 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.24, 0.88] |
| 2 Dropouts | 2 | 77 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.09, 0.93] |
5.1. Analysis.
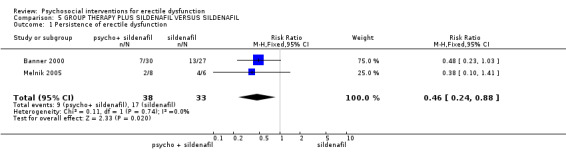
Comparison 5 GROUP THERAPY PLUS SILDENAFIL VERSUS SILDENAFIL, Outcome 1 Persistence of erectile dysfunction.
5.2. Analysis.
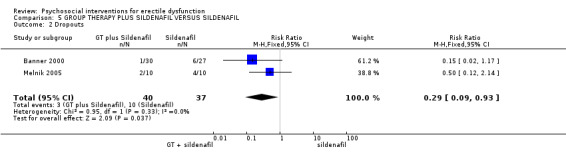
Comparison 5 GROUP THERAPY PLUS SILDENAFIL VERSUS SILDENAFIL, Outcome 2 Dropouts.
Comparison 6. GROUP THERAPY VERSUS OXAZEPAM.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 persistence of erectile dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
6.1. Analysis.
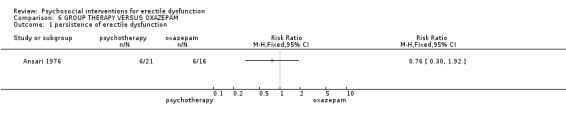
Comparison 6 GROUP THERAPY VERSUS OXAZEPAM, Outcome 1 persistence of erectile dysfunction.
Comparison 7. SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Dropouts | 2 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.83, 2.34] |
| 1.1 ST alone | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.69, 2.59] |
| 1.2 ST associated to ICI | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.66, 3.34] |
| 2 Persistence of erectile dysfunction | 2 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.62, 1.97] |
| 2.1 ST alone | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.14, 1.67] |
| 2.2 ST associated to ICI | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.76, 2.93] |
| 3 Not confident in performance | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 6 months follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 not extremely satisfied with treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Partners reporting the treatment to be disturbing | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 ST associated to ICI | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
7.1. Analysis.
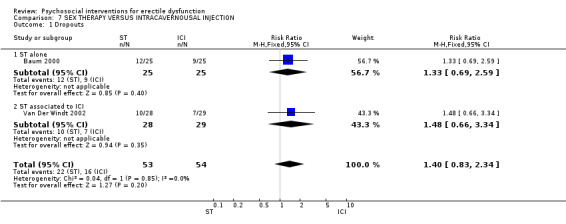
Comparison 7 SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION, Outcome 1 Dropouts.
7.2. Analysis.
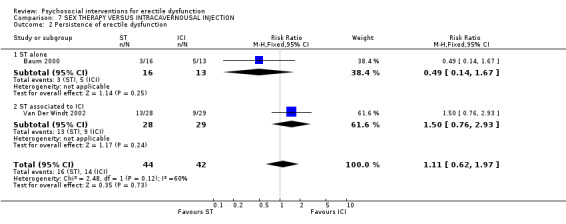
Comparison 7 SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION, Outcome 2 Persistence of erectile dysfunction.
7.3. Analysis.
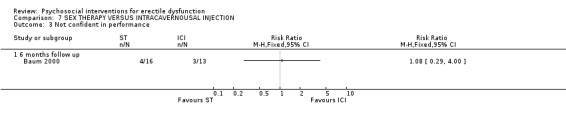
Comparison 7 SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION, Outcome 3 Not confident in performance.
7.4. Analysis.
Comparison 7 SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION, Outcome 4 not extremely satisfied with treatment.
7.5. Analysis.
Comparison 7 SEX THERAPY VERSUS INTRACAVERNOUSAL INJECTION, Outcome 5 Partners reporting the treatment to be disturbing.
Comparison 8. SEX THERAPY VERSUS VACCUM DEVICES.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response to treatment as assessed by therapist | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 post‐treatment (persistence of erectile dysfunction) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 six weeks ( persistence of erectile dysfunction) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
Comparison 8 SEX THERAPY VERSUS VACCUM DEVICES, Outcome 1 Response to treatment as assessed by therapist.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ansari 1976.
| Methods | Allocation: quasi‐randomised Analysis: non ITT | |
| Participants | N= 61 (55) Age= group I ‐mean 29 y , group II‐ mean 46.4, group III‐ 45.0 Diagnosis: psychogenic erectile and mixed factors Centres:England | |
| Interventions | 1. Oxazepam 30‐90 mg/day (N=16 ) 2. Modifed Masters technique (n=21) 3. No treatment (N=18 ) | |
| Outcomes | ‐ Dropout ‐Persistence of erectile dysfunction ‐ Not recovered ‐ Not improved | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Banner 2000.
| Methods | Allocation: randomised Evaluator blind | |
| Participants | N= 57 couples (50) Age=group I‐ 55.3 yr group II ‐57.2 yr Diagnosis: psychogenic erectile dysfunction Centres: USA | |
| Interventions | 1. sildenafil 50 mg (n=27) 2. sildenafil 50mg plus cognitive behavioral sex therapy (n=30) | |
| Outcomes | ‐ Dropout ‐ Persistence of erectile dysfunction ‐ IIFE | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Baum 2000.
| Methods | Allocation: randomised Blindness: none Analysis: non ITT | |
| Participants | N= 50 Age: PGE1 group mean age= 49.6 ST mean age= 50.1 Diagnosis: psychogenic erectile dysfunction Centres: Los Angeles | |
| Interventions | 1. Sex therapy‐weekly sessions during 12 weeks (N=25) 2. PGE1 low dose (2.5‐5.0) (N=25) | |
| Outcomes | ‐ Dropout ‐ Sex situations producing erections ‐ Satisfation with the treatment ‐ confidence in performance after 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Goldman 1990.
| Methods | Allocation: randomised Blindness: none Analysis: none ITT | |
| Participants | N= 20 couples Age= mean 61 years Diagnosis: secondary ED Centres: Philadelphia | |
| Interventions | 1. Workshop (N=10) 2. Control (N=10) | |
| Outcomes | Sexual Interaction Inventory (SII); Frequency of Sexual Behavior Form (SSBF); Aging Sexual Knowledge and Attitude (ASKAS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kilmann 1987.
| Methods | Allocation: randomised Blindness: none Analysis:none ITT | |
| Participants | N= 20 couples age= mean avarage 51y (31‐67) Centres:Columbia | |
| Interventions | 1. Comunication techniques training (CTT) (N=4 couples) 2. Sexual techniques training (STT) (N=4) 3. Combination (CTT + STT) (N=4) 3. Attention‐ placebo (control group) (N=4) 4. No treatment (N=4) Setting: Columbia | |
| Outcomes | ‐ MAT ‐ SII ‐ Coital Success ‐ SAI ‐ SPR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kockott 1975.
| Methods | Allocation: randomised Blindeness: none Analysis: none ITT | |
| Participants | N= 24 men with a partnership age= mean 31 Diagnosis= ED Centres:Germany | |
| Interventions | 1. Behavior therapy group (14 sessions of systematic desensitization) (N=8) 2. Routine therapy seen by psychiatrists 4 times at intervals of 3‐5 weeks (N=8) 3. Waiting list (N=8) | |
| Outcomes | ‐Droup out ‐Persistence of erectile dysfunction ‐semi‐structured interview ‐ Persistence of erectile dysfunction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Melnik 2005.
| Methods | Allocation: randomised ( sealed envelope method) evaluator blind the outcomes Analysis: none ITT | |
| Participants | N=30 mean age= 39.74 Diagnosis= psychogenic ED Centres: Brazil | |
| Interventions | 1. group therapy ( weekly sessions for 6 months) plus 50mg sidenafil citrate orally on demand for 6 months; 2. 50 mg sildenafil citrate orally on demand for 6 months; 3. group therapy (weekly sessions for 6 months) | |
| Outcomes | ‐ Droup out ‐Persistence of erectile dysfunction ‐ IIFE | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Munjack 1984.
| Methods | Allocation:randomised Blindeness: evaluator blind the outcomes Analysis: none ITT | |
| Participants | N= 16 married or living with their sexual partners age= 19‐ 63( mean 47.5 y) Centres :Los Angeles | |
| Interventions | 1.12 bi‐ weekly rational‐ emotive therapy sessions (6 weeks) Vs 2. 6 weeks waiting list | |
| Outcomes | ‐Persitence of erectile dysfunction ‐ Sex attempts | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Price 1981.
| Methods | Allocation: randomised Blindness: none Analysis: none ITT | |
| Participants | N= 21men who had no steady sexual partner age= 25‐61(mean 45.4) Diagnosis: secondary ED Centres: Los Angeles | |
| Interventions | 1. 8 weekly 2‐ hour sessions of group therapy (conducted by dual sex therapists) Vs 2. waiting list Duration = Couples in the 5 groups had twice‐weekly sessions for a total of 20 hours | |
| Outcomes | ‐Persistence of erectile dysfunction attempts of sexual intercourse | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Van Der Windt 2002.
| Methods | Allocation: Allocation: randomised (alternately assigned by a medical secretary) Analysis: non ITT Duration: 6 months follow up Analysis: none ITT | |
| Participants | N= 70 (57 analysed) age=23‐75 (mean 56 years) excluded= major organic cases for ED (all etiologies) Setting= urology clinic Centres: Netherlands duration= april 1998 to August 1999 history= social ‐ relational and psycho‐medical history. A questionnarie, VSS and VSS + estimulation | |
| Interventions | 1. ICI (androskat 0,25 mL) with SC
(n=28) 2. ICI without SC (n=29) |
|
| Outcomes | ‐ Droup out (discontinuation of ICI) ‐ non fully penile erection ‐ partners reporting the treatment to be disturbing | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Wylie 2003.
| Methods | Allocation: randomised ( sealed envelope method) Blindeness: none Analysis: non ITT | |
| Participants | N= 45 couples age= 40 Diagnosis: psychogenic ED and mixeed aethology setting: England | |
| Interventions | 1. Relationship therapy and Masters Sex therapy (each session lasted 40‐50 min every 2 weeks) 2. Therapy plus VCD at the session |
|
| Outcomes | Response to treatment as assesed by therapist | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
ED ‐ Erectile Dysfunction ICI‐ Intracavernosal injection ITT ‐ Intention to Treat MAT ‐ Marital Adjustment Test PGE ‐ Prostaglandin SAI ‐ Sex Anxiety Inventory SII ‐ Sexual Interaction Inventory SPR ‐ Sexual Pleasure Rating
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Golden 1978 | Allocation: RCT Participants: mixed sexual dysfunctions |
| Hartmann 1993 | Allocation: not randomised, case series |
| Hawton 1986 | Allocation: not randomised, case series |
| Lobitz 1979 | Allocation: not randomised, case series |
| Reynolds 1981 | Allocation: not randomised, case series |
| Stravynski 1997 | Participants: mixed sexual dysfunctions |
| Zilbergeld 1975 | Allocation: not randomised, case series |
Contributions of authors
TM ‐ protocol writing, searching, trial selection, data extraction, completion of report
BGOS ‐ protocol writing, searching, trial selection, data extraction, completion of report
AGN ‐ trial selection, data extraction, expertise advice and completion of report
Sources of support
Internal sources
No sources of support supplied
External sources
Brazilian Cochrane Center, Brazil.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Ansari 1976 {published data only}
- Ansari JMA. Impotence : Prognosis ( a controlled study). British Journal of Psychiatry 1976;128:194‐98. [DOI] [PubMed] [Google Scholar]
Banner 2000 {published data only}
- The effects of collaborative care in the treatment of erectile dysfunction (ED): an integrative treatment protocol (ITP). The Fielding Institute. [UMI 9997519]
Baum 2000 {published data only}
- Baum N, Randrup E, Junot D, Hass S. Prostragandin E1 versus sex therapy in the managment of psychogenic erectile dysfunction. Int J Impot Res 2000;12:191‐4. [DOI] [PubMed] [Google Scholar]
Goldman 1990 {published data only}
- Goldman J, Carroll JL. Educational Intervention as an adjunct treatment of erectile dysfunction in older couples. Journal of Sex and Marital Therapy 1990;16:127‐41. [DOI] [PubMed] [Google Scholar]
Kilmann 1987 {published data only}
- Kilmann R P, Milan J R, Boland P J, Nankin R H, Davidson E, West O M, Sabalis R F, Caid C, Devine M J. Group treatment of secondary erectile dysfunction. Journal of Sex and Marital Therapy 1987;13:168‐82. [DOI] [PubMed] [Google Scholar]
Kockott 1975 {published data only}
- Kockott G, Dittmar F, Nusselt L. Systematic Desensitization of erectile impotence: a controlled study. Archives of Sexual Behavior 1975;4(5):493‐500. [DOI] [PubMed] [Google Scholar]
Melnik 2005 {published data only}
- Melnik T. Psychogenic erectile dysfunction: comparative study of three therapeutic approches. Journal of Sex and Marital Therapy 2005;31(3):243‐55. [DOI] [PubMed] [Google Scholar]
Munjack 1984 {published data only}
- Munjack DJ, Schlaks A, Sanchez VC, Usigli R, Zulueta A, Leonard M. Rationale ‐ emotive therapy in the treatment of erectile failure: an initial study. Journal of Sex and Marital Therapy 1984;10:170‐75. [DOI] [PubMed] [Google Scholar]
Price 1981 {published data only}
- Price CS, Reynolds RS, Cohen BD, Anderson AJ, Schochet BV. Group Treatment of Erectile Dsyfunction for men without partners: a controlled evaluation. Archives of Sexual Behavior 1981;10:253‐268. [DOI] [PubMed] [Google Scholar]
Van Der Windt 2002 {published data only}
- Windt F, Dohle GR, Tak J, Slob AK. Intracavernosal injectons therapy with or without sexological counselling in men with erectile dysfunction. BJU international 2002;89:901‐4. [DOI] [PubMed] [Google Scholar]
Wylie 2003 {published data only}
- Wylie KR, Jones RH, Walters S. The potential benefit of vaccum devices augmenting psychosexual therapy for erectile dysfunction. Journal of Sex and Marital Therapy 2003;29:227‐36. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Golden 1978 {published data only}
- Golden JS, Price S, Heinrich AG, Lobitz WC. Group vs couple treatment of sexual dysfunctions. Archives of Sexual Behavior 1978;7:593‐602. [DOI] [PubMed] [Google Scholar]
Hartmann 1993 {published data only}
- Hartmann U, Langer D. Combination of psychosocial therapy and Intrapenile Injections in the treatment of erectile dysfunctions: rationale and predictors of outcome. Journal of Sex Education and Therapy 1993;19:1‐12. [Google Scholar]
Hawton 1986 {published data only}
- Hawton K, Catalan J, Martin P, Fagg J. Long term outcome of sex therapy. Beh Res Ther 1986;24:665‐75. [DOI] [PubMed] [Google Scholar]
Lobitz 1979 {published data only}
- Lobitz WC, Baker EL Jr. Group Treatment of single males with erectile dysfunction. Archives of Sexual Behavior 1979;8:127‐38. [DOI] [PubMed] [Google Scholar]
Reynolds 1981 {published data only}
- Reynolds BS, Cohen BD, Schochet BV, Price SC, Anderson AJ. Dating skills training in the group treatment of erectile dysfunction men without partners. Journal of Sex and Marital Therapy 1981;7:184‐94. [DOI] [PubMed] [Google Scholar]
Stravynski 1997 {published data only}
- Stravynski A, Gaudette G, Lesage A, Petit N, Pascale C, Fabian J, Lamontagne Y, Langlois R, Lipp O, Sidoun P. The treatment of sexually dsyfunctional men without partners: a controlled study of three behavioural group approaches. The British Journal of Psychiatry 1997;170:338‐44. [DOI] [PubMed] [Google Scholar]
Zilbergeld 1975 {published data only}
- Zilbergeld B. Group Treament of sexual dysfunction in men without partners. Journal of Sex and Marital Therapy 1975;1:204‐14. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Everaed 1985 {published data only}
- Everaed W, Dekker J. Treatment of male sexual dysfunction: sex therapy compared with systematic desensitization and rational emotive therapy. Beh. Res. Ther 1985;23:13‐25. [DOI] [PubMed] [Google Scholar]
Phelps 2004 {published data only}
- Phelps J, Jain A, Monga M. The PsychoedplusMed Approch to erectile dysfunction treatment: the impact of combining a psychoeducacional intervention with sildenafil. Journal of Sex and Marital Therapy 2004;30:305‐14. [DOI] [PubMed] [Google Scholar]
Takefman 1984 {published data only}
- Takefman J, Brender W. An analysis of the effectiveness of two components in the treatment of erectile dysfunction. Archives of Sexual Behavior 1984;13:321‐39. [DOI] [PubMed] [Google Scholar]
Additional references
Ackerman 1995
- Ackerman MD, Carey MP. Psychologys role in the assessment of erectile dysfunction: historical precedents, current knowledge and methods. Consult Clin Psychol 1995;63:862‐76. [DOI] [PubMed] [Google Scholar]
Althof 1989
- Althof S. Psychogenic impotence: treatment of men and couples. Principles and practice of sex therapy: update for the 1990s. New York: Guilford, 1989:237‐65. [Google Scholar]
Althof 2000
- Althof S. The patient with erectile dysfunction: psychological issues. Nurse Pract 2000;Suppl 1:11‐13. [DOI] [PubMed] [Google Scholar]
Althof 2002
- Althof S. When an erection alone is not enough: biopsychosocial obstacles to lovemaking. Int J Impot Res 2002;14 Suppl 1:99‐104. [DOI] [PubMed] [Google Scholar]
Aydin 2001
- Aydin S, Unal D, Erol H, Karaman I, Yilmaz Y, Sengul E, Bayrakli H. Multicentral clinical evaluation of etiology of erectile dysfunction: a survey report. Int Urol Nephrol 2001;32:213‐217. [DOI] [PubMed] [Google Scholar]
Cochrane Handbook
- Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006]. In: The Cochrane Library. Chichester: John Wiley & Sons, Ltd., 2006, issue 4.
Ellis 1992
- Ellis A. Links Group rational‐emotive and cognitive‐behavioral therapy. Int J Group Psychother 1992;42(1):63‐80. [DOI] [PubMed] [Google Scholar]
Feldman 1994
- Feldman HA, Goldstein I, Hatzichristou DG, Kranes RJ, Makinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts male aging study. J Urol 1994;151(1):151‐54. [DOI] [PubMed] [Google Scholar]
Levine 2000
- Levine LA. Diagnosis and treatment of erectile dysfunction. Am J Med 2000;Suppl 9A Discussion:29S‐30S. [DOI] [PubMed] [Google Scholar]
LoPiccolo 1986
- LoPiccolo J, Stock WE. Treatment of sexual dysfunction. Journal of Consulting and Clinical Psychology 1986;54:158‐67. [DOI] [PubMed] [Google Scholar]
Masters 1970
- Masters WH, Johnson VE. Human Sexual Inadequacy. Little, Brown, 1970. [ISBN 055326317X] [Google Scholar]
Melman 1988
- Melman A, Tiefer L, Pederson R. Evaluation of first 406 patients in urology department based center for male sexual dysfunction. Urology 1988;32:6‐10. [DOI] [PubMed] [Google Scholar]
NIH 1992
- Anonymous. Impotence. NIH Consens Statement. National Institutes of Health Consensus Development Conference Statement. 1992; Vol. 10, issue 4:1‐31.
Perelman 2001
- Perelman MA. The impact of new sexual pharmaceuticals on sex therapy. Curr Psychiatry Rep 2001;3:195‐201. [DOI] [PubMed] [Google Scholar]
Rimm 1987
- Rimm DC, Masters JC. Behavior therapy: Techniques and empirical findings. NY: Academic Press, 1987. [Google Scholar]
Rosen 1995
- Rosen RC, Leiblum SR. Treatment of sexual disorders in the 1990s: an integrated approach. J Consult Clin Psychol 1995;63(6):877‐90. [DOI] [PubMed] [Google Scholar]
Rosen 2001
- Rosen RC. Psychogenic erectile dysfunction: classification and management. Urol Clin North Am 2001;28:269‐78. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408‐12. [DOI] [PubMed] [Google Scholar]
Seidman 2001
- Seidman SN, Roose SP. Sexual dsyfunction and depression. Curr Psychiatry Rep 2001;3:202‐8. [DOI] [PubMed] [Google Scholar]


