Abstract
Background:
High-resolution manometry (HRM) is generally considered the primary method to evaluate esophageal motility; functional luminal imaging probe (FLIP) Panometry represents a novel method to do so and is completed during sedated endoscopy. This study aimed to compare HRM and FLIP Panometry in predicting esophageal retention on timed barium esophagram (TBE).
Methods:
329 adult patients that completed FLIP, HRM, and TBE for primary esophageal motility evaluation were included. An abnormal TBE was defined by a 1-minute column height >5cm or impaction of a 12.5mm barium tablet. The integrated relaxation pressure (IRP) on HRM was assessed in the supine and upright patient positions. EGJ opening was evaluated with 16-cm FLIP performed during sedated endoscopy via EGJ-distensibility index (DI) and maximum EGJ diameter.
Results:
Receiver operating characteristic curves to identify an abnormal TBE demonstrated AUC (95% confidence interval, CI) of 0.79 (0.75-0.84) for supine IRP, 0.79 (0.76-0.86) for upright IRP, 0.84 (0.79-0.88) for EGJ-DI, and 0.88 (0.85-0.92) for maximum EGJ diameter. Logistic regression to predict abnormal TBE showed odds ratios (95% CI) of 1.8 (0.84-3.7) for consistent IRP elevation and 39.7 (16.4-96.2) for reduced EGJ opening on FLIP Panometry. Of 40 patients with HRM-FLIP Panometry discordance, HRM-IRP was consistent with TBE in 23% while FLIP Panometry was consistent with TBE in 78%.
Conclusions:
FLIP Panometry provided superior detection of esophageal retention over IRP on HRM. However, application of a complementary evaluation involving FLIP Panometry, HRM, and TBE may be necessary to accurately diagnose esophageal motility disorders.
Introduction
Esophageal high-resolution manometry (HRM) is generally considered the primary method to assess for esophageal motility disorders.1-3 With HRM interpretation, an abnormally elevated integrated relaxation pressure (IRP) is considered representative of abnormal lower esophageal sphincter (LES) relaxation and is the principal criterion utilized to classify disorders of esophagogastric junction (EGJ) outflow obstruction, including achalasia.2, 4 Assignment of IRP results represents the initial branch point in the hierarchical classification of esophageal motility disorders described by the Chicago Classification: achalasia is generally diagnosed when the IRP is elevated in conjunction with absent peristalsis, while a classification of EGJ outflow obstruction (EGJOO) is assigned when IRP is elevated and peristalsis is present.2, 4 In the recent update to the Chicago Classification (version 4.0), application of a HRM test protocol that includes two patient positions (supine and upright) was recommended to improve performance of the IRP for detection of EGJ outflow obstruction.4 However, recommendations from the International HRM Working Group also included utilization of supportive testing with timed barium esophagram (TBE) or functional luminal imaging probe (FLIP) when HRM findings are inconclusive.4
The FLIP utilizes impedance planimetry technology to assess lumen dimensions along the length of the esophagus and esophageal distensibility (i.e. the relationship of dimension with distensive pressure) during controlled volumetric distension. By displaying the esophageal diameter changes along a space-time continuum with associated pressure utilizing the FLIP Panometry approach, EGJ opening mechanics and the contractile response to distension, i.e. secondary peristalsis, can be assessed.5, 6 FLIP Panometry is also appealing in that the test is performed on a sedated patient at the time of endoscopy, as opposed to the awake transnasal catheter utilized for HRM. Application of the FLIP Panometry technique previously demonstrated that EGJ opening parameters were consistently abnormal in achalasia, while patients with normal esophageal motility on manometry most commonly had normal EGJ opening on FLIP Panometry.5, 7-10 While agreement was commonly observed in determination of EGJ outflow obstruction with HRM and FLIP Panometry, discordant cases were also observed.5, 9 The clinical implications of FLIP-HRM discordance are relatively unexplored, however, the FLIP Panometry EGJ opening assessment was previously demonstrated to help clarify equivocal achalasia and EGJOO classifications on HRM.11, 12 Overall, previous studies evaluating esophageal motility with FLIP Panometry generally focused on assessing agreement with HRM, as opposed to directly comparing the two modalities using an objective reference standard.
Esophageal clearance can be objectively assessed with TBE and represents a clinically relevant measure of esophageal function.13, 14 Timed barium esophagram is often used to complement the esophageal motility evaluation and is particularly valuable if an initial evaluation is inconclusive.4 Further, TBE provides an objective measure of esophageal clearance that is independent of both HRM and FLIP. Therefore, the aim of this study was to directly compare the accuracy of HRM and FLIP Panometry to determine abnormal esophageal retention as defined by TBE.
Methods
Subjects
Adult patients (age 18-89) presenting to the Esophageal Center of Northwestern for evaluation of esophageal symptoms and esophageal motility testing between November 2012 and December 2019 were prospectively evaluated and data maintained in an esophageal motility registry. Clinical evaluation with TBE was obtained at the discretion of the primary treating gastroenterologist. Consecutive patients that completed FLIP during sedated endoscopy, HRM, and TBE for evaluation for primary esophageal motility disorders were included. Patients with technically limited FLIP or HRM studies were excluded. Patients with previous foregut surgery (including previous pneumatic dilation) or esophageal mechanical obstructions including esophageal stricture, eosinophilic esophagitis, severe reflux esophagitis (Los Angeles-classification C or D), or hiatal hernia > 3cm were excluded as these are causes attributed to secondary esophageal motor abnormalities (Figure S1). No adverse events were reported during performance of HRM or FLIP. No endoscopic or surgical treatment occurred between the times of FLIP, HRM, and TBE.
The study protocol was approved by the Northwestern University Institutional Review Board. There is overlap of the patient cohort with previous publications.5, 7-9, 15
HRM protocol and analysis
After a minimum 6-hour fast, HRM studies were completed using a 4.2-mm outer diameter solid-state assembly with 36 circumferential pressure sensors at 1-cm intervals (Medtronic Inc, Shoreview, MN). The HRM assembly was placed transnasally and positioned to record from the hypopharynx to the stomach with approximately three intragastric pressure sensors. After a 2-minute baseline recording, the HRM protocol was performed with ten, 5-ml liquid swallows in a supine position and with five 5-ml liquid swallows in an upright, seated position.5
Manometry studies were analyzed according to the Chicago Classification v4.0.4 These patients were evaluated prior to or during the consensus development process for Chicago Classification version 4.0. For the purpose of this study, the HRM classifications were based on available HRM data only, and thus all EGJOO were considered inconclusive.4 The IRP was measured using the commercial software (Medtronic Inc) for the 10 supine swallows and 5 upright swallows; median values for each position were applied. Prespecified thresholds were applied with abnormal metrics defined as a median IRP >15 mmHg for supine swallows and median IRP >12 mmHg for upright swallows.4 EGJ outflow obstruction on HRM was classified using the IRP values as “consistent IRP elevation” if both supine and upright IRP were elevated, “isolated IRP elevation” if one (but not the other) IRP was elevated, and “normal” if both IRP values were normal. In cases in which upright swallows were not completed, the supine IRP was independently applied as either isolated IRP elevation (if >15mmHg) or normal (if ≤15mmHg).
FLIP Study Protocol and Analysis
The FLIP study using 16-cm FLIP (EndoFLIP® EF-322N; Medtronic, Inc, Shoreview, MN) was performed during sedated endoscopy as previously described.5, 16 Endoscopy performed in the left-lateral decubitus position was generally performed using conscious sedation with midazolam and fentanyl. Other medications, e.g. propofol, were also used with monitored anesthesia care at the discretion of the performing endoscopist in some cases. Although these medications used for endoscopic sedation can alter esophageal motility, the patterns of motility during the FLIP protocol are reproducible and have been shown to predict motility patterns during HRM performed without these medications.5, 16-18 With the endoscope withdrawn and after calibration to atmospheric pressure, the FLIP was placed transorally and positioned within the esophagus with 1-3 impedance sensors beyond the EGJ with this positioning maintained throughout the FLIP study. Stepwise 10-ml FLIP distensions beginning with 40 ml and increasing to target volume of 60 or 70 ml were then performed; each stepwise distension volume was maintained for 30-60 seconds.
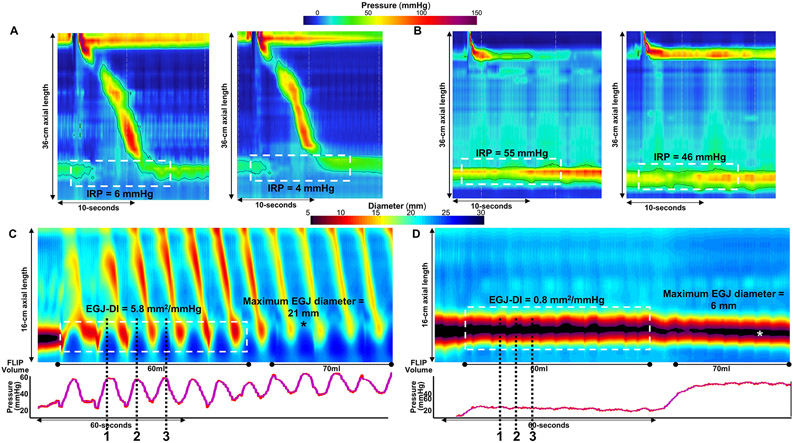
FLIP data were exported using a customized program (available open source at http://www.wklytics.com/nmgi) to generate FLIP Panometry plots for analysis.8, 15 The EGJ analysis specifically focused on the EGJ distensibility index (DI) at the 60ml FLIP fill volume and the maximum EGJ diameter that was achieved during the 60ml or 70ml fill volume (Figure 1) as previous described and was performed blinded to clinical characteristics.9 Areas at the EGJ that were affected by dry catheter artifact (i.e. artifact that impacts diameter measurement when occlusion of the FLIP balloon disrupts the electrical current utilized for the impedance planimetry technology) and the first 5 seconds after achieving the 60ml fill volume (to avoid incorporation of active-filling effects) were omitted from the EGJ analysis. The EGJ-DI was then measured during the 60ml FLIP fill volume dependent on the FLIP contractile response pattern (i.e. presence of antegrade contraction) as illustrated in Figure 1. The EGJ-DI was not calculated if the applied FLIP pressure was <15mmHg; in these cases, the maximum EGJ-diameter was applied independently for analysis.
Figure 1. Esophagogastric junction (EGJ) evaluation on high-resolution manometry (HRM) and FLIP Panometry.
HRM (A-B) and FLIP Panometry (C-D) from two patients are displayed; a patient with normal esophageal motility (A and C) and a patients with type I achalasia (B and D). In A and B, esophageal pressure topography plots of a supine test swallow are displayed in the left panels and of an upright test swallow in the right panels; the integrate relaxation pressure (IRP) was calculated within the region within the white dashed box. In C and D, FLIP Panometry output are displayed as length (16-cm) x time x color-coded diameter FLIP topography (top panels) with corresponding intraballoon pressure (bottom panels). The EGJ-distensibility index (DI) was calculated as the median value of three measures obtained during the 60-ml fill volume (white dashed box); the maximum EGJ diameter is marked by “*” in A and B. When antegrade contractions were present, as in A, the EGJ-DI was measured at the peak EGJ diameters that occurred in response to the pressure ramp associated with the contraction (black dashed lines). When antegrade contractions were absent, as in B, the EGJ-DI measures were obtained during expiration (black dashed lines) and at areas not including EGJ or LES contractions.9 Figure used with permission from the Esophageal Center of Northwestern.
Classification of EGJ opening with FLIP Panometry was developed based on previous evaluation of asymptomatic volunteers and patients with achalasia and normal esophageal motility on HRM and thus pre-specified classifications were applied.7, 9, 16 Reduced EGJ opening (REO) was defined by EGJ-DI <2.0 mm2/mmHg and a maximum EGJ diameter <12mm. Borderline EGJ opening was defined by an EGJ-DI <2.0 mm2/mmHg or a maximum EGJ diameter <16mm (but not REO) and was further differentiated into borderline-reduced EGJ opening (BrEO) if the maximum EGJ diameter was <14mm and borderline-normal EGJ opening (BnEO) if the maximum EGJ diameter was ≥14mm. Normal EGJ opening (NEO) was defined by an EGJ-DI ≥2.0mm2/mmHg and ≥16mm.
Timed barium esophagram and outcome assignment
Timed barium esophagram (TBE) was performed in the upright position and involved consumption of 200-mL of low density barium sulfate with images obtained at 1 and 5 minutes.19 The height of the barium column was measured vertically from the EGJ. Patients also ingested a 12.5-mm barium tablet with passage of the tablet assessed in real-time by the performing radiologist; the tablet was not utilized in some patients if there was abnormal liquid retention on TBE. The primary outcome for an “abnormal TBE” was assigned if there was a column height >5cm at 1 minute or impaction of the 12.5mm barium tablet (i.e. tablet was unable to pass from the esophagus).13 As a secondary outcome, the TBE data was applied using an abnormal threshold of 5-minute column height >5cm.
Statistical Analysis
Results were reported as mean (standard deviation; SD), or median (interquartile range; IQR) depending on data distribution. Groups were compared using Chi-square test for categorical variables and ANOVA/t-tests or Kruskal-Wallis/Mann-Whitney U for continuous variables, depending on data distribution. Pre-specified thresholds were applied for categorization of EGJ opening on FLIP Panometry and EGJ outflow obstruction with HRM were applied for comparisons. Additionally, a prespecified sub-group analysis was performed to include patients without HRM classifications of achalasia (subtypes I, II, and III) or absent contractility due to the potential contribution of esophageal dysmotility to esophageal retention independent of EGJ obstruction. Receiver operating characteristic (ROC) curves were applied to predict abnormal TBE versus not abnormal TBE. Binary logistic regression was used to evaluate relationships between HRM-IRP classification, FLIP Panometry EGJ classification, the presence of hiatal hernia (defined by EGJ morphology on HRM), and abnormal TBE; these models controlled for age and gender. Statistical significance was considered at a two-tailed p-value < 0.05. Post-hoc comparison testing, as appropriate, was completed using a Bonferroni correction.
Results
Subjects
329 patients, mean (SD) age 54 (16) years, 57% female (Table 1) were included. The majority (93%) of patients were evaluated for dysphagia. Of the 329 patients, 215 (65%) had an abnormal TBE with a 1 minute column height >5cm or impaction of a barium tablet. Among the abnormal TBEs, there were 7 patients with tablet impaction and 1 minute column height <5cm. 135/329 (41%) patients had a 5 minute column height >5cm. Among the 114 patients with a ‘normal’ esophagram, there were 25 patients that had a 1 minute column height >0cm (but <5cm) or delayed passage of a barium tablet.
Table 1. Patient characteristics.
Abnormal timed barium esophagram (TBE) was defined by a 1 minute column height >5cm or impaction of the 12.5mm tablet.
| All patients | Abnormal TBE | Normal TBE | |
|---|---|---|---|
| N, n | 329 | 215 | 114 |
| Age, mean (SD), years | 54 (16) | 54 (16) | 55 (17) |
| n (%) | n (%) | n (%) | |
| Gender, female * | 186 (57) | 107 (50) | 79 (69) |
| Indication * | |||
| Dysphagia a | 306 (93) | 209 (97) | 97 (85) |
| Reflux symptoms | 14 (4) | 2 (1) | 12 (11) |
| Chest pain | 5 (2) | 2 (1) | 3 (3) |
| Other | 4 (1) | 2 (1) | 2 (2) |
| Endoscopy findings * | |||
| Erosive esophagitis; | |||
| LA-A / LA-B | 12 (4) / 6 (2) | 3 (1) / 2 (1) | 9 (8) / 4 (4) |
| Non-obstructing ring | 7 (2) | 1 (1) | 6 (5) |
| Diverticulum | 7 (2) | 6 (3) | 1 (1) |
| HRM-Chicago Classification v4.0 b * | |||
| Type I achalasia | 38 (12) | 38 (18) | 0 |
| Type II achalasia | 73 (22) | 73 (34) | 0 |
| Type III achalasia | 20 (6) | 18 (8) | 2 (2) |
| EGJ outflow obstruction | 68 (21) | 43 (20) | 26 (23) |
| Hypercontractile esophagus | 4 (1) | 2 (1) | 2 (2) |
| Distal esophageal spasm | 6 (2) | 5 (2) | 1 (1) |
| Absent contractility | 13 (4) | 9 (4) | 4 (4) |
| Ineffective esophageal motility | 30 (9) | 12 (6) | 4 (4) |
| Normal motility | 77 (23) | 15 (7) | 62 (54) |
| HRM-EGJ-morphology * | |||
| Type I (no hiatal hernia) | 269 (82) | 192 (89) | 77 (68) |
| Type II-III (hiatal hernia) | 60 (18) | 23 (11) | 37 (33) |
| IRP-supine, mmHg, median (IQR) * | 20 (12-31) | 25 (17-73) | 13 (8-18) |
| IRP-upright, mmHg, median (IQR) * | 18 (10-29)1 | 24 (13-34)1 | 11 (7-17)1 |
| EGJ-DI, mm2/mmHg, median (IQR) * | 1.5 (0.8-3.5)2 | 1.1 (0.7-1.7)2 | 3.6 (2.1-5.5)2 |
| Maximum EGJ diameter, mm, median (IQR) * | 11.5 (8.5-16.9) | 9.2 (7.7-12.2) | 17.5 (14.5-19.8) |
P<0.001 on comparison between TBE classifications.
Dysphagia +/− reflux symptoms or chest pain.
Reflects manometric classifications, and thus all EGJ outflow obstruction were considered inconclusive; additionally, there was one patient with inconclusive hypercontractile esophagus and one patient with inconclusive distal esophageal spasm , both had normal TBE.
n=312; 201 with abnormal TBE, 111 with normal TBE.
n=324; 211 with abnormal TBE; 113 with normal TBE. LA – Los Angeles grade.
High-resolution manometry and association with TBE results
The most common HRM classifications were achalasia (subtypes I, II, and III) in 131 (40%) patients, EGJ outflow obstruction in 68 (21%), and normal motility in 77 (23%); Table 1. Abnormal TBE occurred in 98% of patients with achalasia on HRM, 63% of patients with EGJOO, and 19% of patients with normal motility.
There were 212 (64%) patients with supine IRP >15mmHg and 212 (68% of 312 patients; 17 patients did not complete upright swallows) with upright IRP >12 mmHg. There were 187 (57%) patients with consistent IRP elevation, 50 (15%) patients with isolated IRP elevation (25 patients with isolated supine IRP elevation, 11 of whom did not complete upright swallows; 25 patients had isolated upright IRP elevation), and 92 (28%) patients with normal IRP.
Supine IRP and upright IRP were both higher in patients with abnormal TBE than in normal TBE (Table 1; P-values <0.001). Among the entire cohort, consistent IRP elevation occurred in 71% of patients with an abnormal TBE and 29% of patients with a normal TBE; normal IRP occurred in 17% of patients with abnormal TBE and 49% of patients with a normal TBE; P<0.001; Figure 2A. On subgroup analysis with patients with achalasia or absent contractility on HRM removed, consistent IRP elevation occurred in 54% of patients with an abnormal TBE and 31% of patients with a normal TBE; normal IRP occurred in 35% of patients with an abnormal TBE and 48% of patients with a normal TBE; P=0.005; Figure 2C.
Figure 2. Association of high-resolution manometry (HRM; A and C) and FLIP Panometry (B and D) results with timed barium esophagram (TBE).
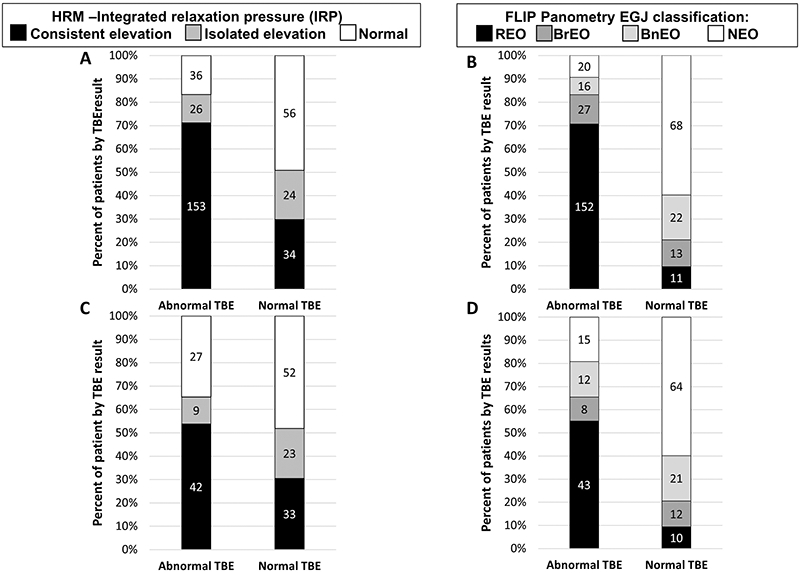
A and B represent the entire study cohort while C and D represent the sub-group analysis that excluded patients with achalasia and absent contractility on HRM. Numbers on the bars reflect the number of patients (n) within each classification. REO - Reduced EGJ opening; BrEO – borderline reduced EGJ opening; BnEO – borderline normal EGJ opening; NEO - normal EGJ opening. Figure used with permission from the Esophageal Center of Northwestern.
FLIP Panometry – EGJ opening parameters and association with TBE results
Among the entire cohort, the classification of EGJ opening was REO in 163 (50%), BrEO in 40 (12%), BnEO in 38 (12%), and NEO in 88 (27%). There were 5 patients with 60-ml pressure was <15mmHg and thus the EGJ-DI was not calculated. The EGJ-DI and maximum EGJ diameter were both lower in patients with abnormal TBE than in normal TBE (Table 1; P-values <0.001). Among the entire cohort, REO occurred in 71% of patients with an abnormal TBE and 10% of patients with a normal TBE; NEO occurred 9% of patients with abnormal TBE and 60% of patients with a normal TBE; P<0.001; Figure 2B. On subgroup analysis with patients with achalasia and absent contractility on HRM removed, REO occurred in 55% of patients with an abnormal TBE and 9% of patients with a normal TBE; NEO occurred in 19% of patients with an abnormal TBE and 60% of patients with a normal TBE; P<0.001; Figure 2D.
Comparative evaluation of FLIP Panometry and HRM-IRP to predict esophageal retention on TBE
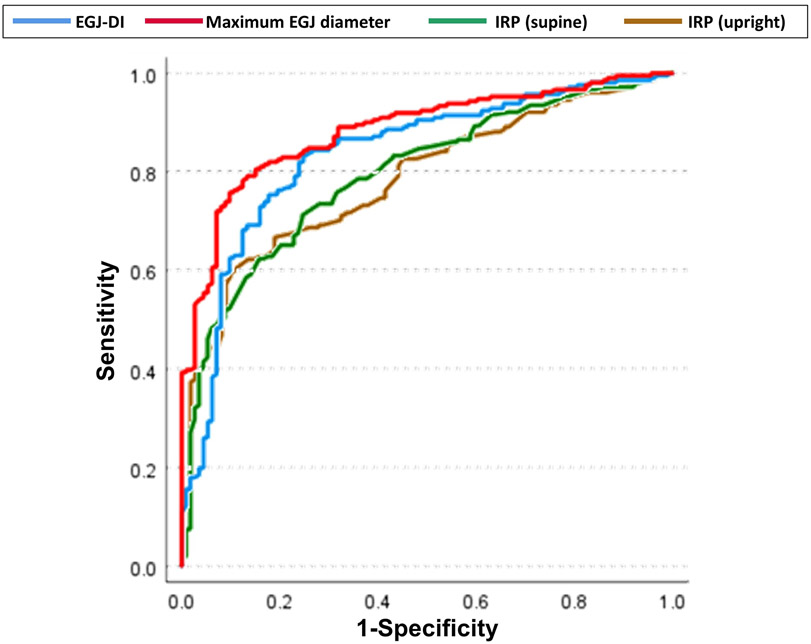
ROC curves to identify an abnormal TBE demonstrated area-under-the ROC curve (AUROC) (95% confidence interval (CI)) of 0.79 (0.75-0.84) for supine IRP, 0.79 (0.76-0.86) for upright IRP, 0.84 (0.79-0.88) for EGJ-DI, 0.88 (0.85-0.92) for maximum EGJ diameter (Figure 3). Sensitivity and specificity for various thresholds among all four metrics are listed in Table 2. For detection of a 5-minute TBE column height >5cm, the AUROCs (95% CIs) were 0.82 (0.77-0.87) for supine IRP, 0.79 (0.74-0.85) for upright IRP, 0.77 (0.72-0.82) for EGJ-DI, 0.86 (0.82-0.90) for maximum EGJ diameter.
Figure 3. Receiver operating characteristic (ROC) curves for identification of abnormal esophagram.
The supine and upright integrated relaxation pressure (IRP) from high resolution manometry and the EGJ-distensibility index (DI) and maximum EGJ diameter from FLIP Panometry were applied to predict abnormal timed barium esophagram (TBE). Abnormal TBE was defined as a 1 minute column height >5cm or impaction of a 12.5mm barium tablet.13 Figure used with permission from the Esophageal Center of Northwestern.
Table 2. Sensitivity and specificity for detection of abnormal timed barium esophagram (TBE).
Sensitivity (sens) and specificity (spec) values are based on point coordinates of receiver operating characteristic curves in Figure 3. Abnormal TBE was defined by a 1 minute column height >5cm or impaction of the 12.5mm tablet.13
| IRP (supine) | IRP (upright) | EGJ-DI | Maximum EGJ diameter | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cut-point (mm2/mmHg) |
Sens (%) |
Spec (%) |
Cut-point (mmHg) |
Sens (%) |
Spec (%) |
Cut-point (mmHg) |
Sens (%) |
Spec (%) |
Cut-point (mmHg) |
Sens (%) |
Spec (%) |
| 6 | 97 | 15 | 4 | 97 | 11 | 0.5 | 12 | 99 | 8 | 30 | 99 |
| 8 | 94 | 25 | 6 | 94 | 22 | 1.0 | 47 | 93 | 10 | 61 | 93 |
| 10 | 90 | 38 | 8 | 90 | 31 | 1.5 | 69 | 84 | 11 | 70 | 92 |
| 12 | 86 | 45 | 10 | 86 | 45 | 2.0 | 81 | 76 | 12 | 74 | 90 |
| 14 | 83 | 58 | 12 | 82 | 55 | 2.5 | 87 | 67 | 13 | 79 | 85 |
| 15 | 79 | 61 | 14 | 74 | 60 | 2.8 | 87 | 61 | 14 | 83 | 79 |
| 16 | 77 | 65 | 15 | 72 | 64 | 3.0 | 88 | 59 | 15 | 86 | 71 |
| 18 | 72 | 74 | 16 | 70 | 68 | 3.5 | 90 | 52 | 16 | 89 | 65 |
| 20 | 66 | 77 | 18 | 67 | 77 | 4.0 | 92 | 46 | 17 | 92 | 56 |
| 22 | 61 | 85 | 20 | 61 | 87 | 4.5 | 92 | 38 | 18 | 94 | 47 |
| 24 | 54 | 89 | 22 | 53 | 91 | 5.0 | 94 | 33 | 20 | 97 | 21 |
| 26 | 47 | 94 | 24 | 49 | 92 | ||||||
| 28 | 42 | 95 | 26 | 42 | 95 | ||||||
| 30 | 39 | 97 | 28 | 39 | 97 | ||||||
Regression analysis to predict abnormal esophagram demonstrated that presence of hiatal hernia (defined on HRM) and the FLIP Panometry EGJ opening classification were significant predictors of abnormal TBE among both the entire cohort and within the subgroup analysis (Table 3). The HRM-IRP classification was a significant predictor of abnormal TBE among the entire cohort, but not within the subgroup analysis. The FLIP Panometry EGJ classification had the strongest relationship with abnormal TBE among the included covariates: REO was associated with an odds ratio (OR; 95% CI) of 39.7 (16.4-96.2) and 20.8 (7.7-56.1) for an abnormal TBE among the entire cohort and subgroup analysis, respectively (Table 3). Results were similar when utilizing the abnormal TBE threshold of column height of >5cm at 5 minutes (Table S1).
Table 3. Binary logistic regression for prediction of abnormal esophageal retention on timed barium esophagram.
3A reflects the binary logistic regression model that included the entire cohort (n=329). 3B reflects the subgroup analysis that omitted patients with achalasia or absent contractility on high-resolution manometry (n=186).
| 3A – Total Cohort | ||||
|---|---|---|---|---|
| B | SE | OR (95% CI) | P | |
| Age | −0.014 | 0.01 | 0.99 (0.97–1.0) | 0.162 |
| Female Gender | −0.60 | 0.33 | 0.55 (0.29–1.0) | 0.070 |
| Hiatal hernia present a | 1.2 | 0.39 | 3.2 (1.5–6.8) | 0.003 |
| IRP classification (normal IRP) | -- | 0.016 | ||
| Isolated IRP elevation | −0.69 | 0.46 | 0.5 (0.20–1.2) | 0.134 |
| Consistent IRP elevation | 0.57 | 0.38 | 1.8 (0.84–3.7) | 0.133 |
| FLIP-EGJ (Normal EGJ opening) | -- | <0.001 | ||
| Borderline-normal EGJ opening | 1.0 | 0.45 | 2.7 (1.1–6.7) | 0.025 |
| Borderline-reduced EGJ opening | 1.8 | 0.46 | 6.3 (2.6–15.6) | <0.001 |
| Reduced EGJ opening | 3.7 | 0.45 | 39.7 (16.4–96.2) | <0.001 |
| Constant | −1.08 | 0.734 | 0.34 | 0.143 |
| 3B – Subgroup | ||||
|---|---|---|---|---|
| B | SE | OR (95% CI) | P | |
| Age | −0.01 | 0.01 | 0.99 (0.97-1.0) | 0.467 |
| Female Gender | −0.82 | 0.39 | 0.44 (0.20-0.96) | 0.038 |
| Hiatal hernia present a | 0.89 | 0.43 | 2.4 (1.0-5.6) | 0.038 |
| IRP classification (normal IRP) | -- | 0.074 | ||
| Isolated IRP elevation | −1.1 | 0.57 | 0.33 (0.11-0.99) | 0.048 |
| Consistent IRP elevation | 0.15 | 0.42 | 1.2 (0.5-2.6) | 0.713 |
| FLIP-EGJ (Normal EGJ opening) | -- | <0.001 | ||
| Borderline-normal EGJ opening | 0.98 | 0.50 | 2.7 (1.0-7.1) | 0.048 |
| Borderline-reduced EGJ opening | 1.1 | 0.58 | 3.0 (0.96-9.2) | 0.058 |
| Reduced EGJ opening | 3.0 | 0.51 | 20.8 (7.7-56.1) | <0.001 |
| Constant | −1.06 | 0.81 | 0.35 | 0.188 |
Defined by type II or type III EGJ-morphology on high-resolution manometry.4 SE – standard error. OR – odds ratio. IRP – integrated relaxation pressure.
Finally, HRM-IRP and FLIP Panometry EGJ classifications were evaluated for concordance or discordance with associated TBE results (Table 4). Agreement between all three tests (i.e. HRM, FLIP, and TBE) was observed in 49% (160/329) of the cohort: 57% of abnormal TBEs and 33% of normal TBEs. HRM-FLIP concordance (consistent IRP elevation + REO, normal IRP + NEO) was observed in 179/329 (54%) patients. Concordance for abnormal findings, i.e. consistent IRP elevation + REO, was observed in 129/329 (39%) patients, which accounted for 57% of abnormal TBEs and 5% of normal TBE (Table 4). Concordance for normal findings, i.e. normal IRP + NEO, was observed in 50/329 (15%) patients, which accounted for 6% of abnormal TBEs and 33% of normal TBE. Thus, among the 179 FLIP-HRM concordant cases, the TBE results were consistent with the HRM-FLIP results in 89% of cases.
Table 4. Agreement of high-resolution manometry (HRM) and FLIP Panometry assessment of EGJ obstruction and association with barium esophagram.
4A. The frequency agreement of EGJ outflow obstruction on HRM, defined by integrated relaxation pressure (IRP) with the FLIP Panometry classification of EGJ opening are displayed relative to timed barium esophagram (TBE) results. 4B. The HRM classifications among HRM-FLIP Panometry concordant cases and discordant cases are displayed relative to TBE results. Abnormal TBE was defined as a 1 minute column height >5cm or inability of a 12.5mm tablet to pass. Concordance with FLIP EGJ opening and HRM-IRP are shaded blue; discordance is shaded red.
| 4A | ||||
|---|---|---|---|---|
| Abnormal TBE (n, % total abnormal TBE) | ||||
| REO | BEO | NEO | Total | |
| Consistent IRP elevation | 123 (57) | 24 (11) | 6 (3) | 153 (71) |
| Isolated IRP elevation | 18 (8) | 7 (3) | 1 (1) | 26 (12) |
| Normal IRP | 11 (5) | 12 (6) | 13 (6) | 36 (17) |
| Total | 152 (71) | 43 (20) | 20 (9) | 215 (100) |
| /// /// /// /// /// /// /// /// /// /// /// /// | ||||
| Normal TBE (n, % total normal TBE) | ||||
| REO | BEO | NEO | Total | |
| Consistent IRP elevation | 6 (5) | 8 (7) | 20 (18) | 34 (30) |
| Isolated IRP elevation | 2 (2) | 11 (10) | 11 (10) | 24 (21) |
| Normal IRP | 3 (3) | 16 (14) | 37 (33) | 56 (49) |
| Total | 11 (10) | 35 (31) | 68 (60) | 114 (100) |
| 4B | ||||
|---|---|---|---|---|
| Abnormal TBE | ||||
| Concordant results | Discordant results | |||
| Consistent IRP elevation + REO |
Normal IRP + NEO |
Consistent IRP elevation + NEO |
Normal IRP + REO |
|
| n (%) | n (%) | n (%) | n (%) | |
| HRM-Chicago Classification v4.0 | ||||
| Type I achalasia | 20 (16) | 0 | 1 (17)* | 0 |
| Type II achalasia | 58 (47) | 0 | 0 | 0 |
| Type III achalasia | 15 (12) | 0 | 0 | 0 |
| EGJ outflow obstruction | 30 (24) | 0 | 3 (50) | 0 |
| Hypercontractile esophagus | 0 | 1 (8) | 0 | 0 |
| Distal esophageal spasm | 0 | 1 (8) | 0 | 1 (9) |
| Absent contractility | 0 | 4 (31) | 0 | 4 (36) |
| Ineffective esophageal motility | 0 | 2 (15) | 0 | 2 (18) |
| Normal motility | 0 | 5 (39) | 2 (33) | 4 (36) |
| /// /// /// /// /// /// /// /// /// /// /// /// | ||||
| Normal TBE | ||||
| Concordant results | Discordant results | |||
| Consistent IRP elevation + REO |
Normal IRP + NEO |
Consistent IRP elevation + NEO |
Normal IRP + REO |
|
| n (%) | n (%) | n (%) | n (%) | |
| HRM-Chicago Classification v4.0 | ||||
| Type I achalasia | 0 | 0 | 0 | 0 |
| Type II achalasia | 0 | 0 | 0 | 0 |
| Type III achalasia | 1 (17) | 0 | 0 | 0 |
| EGJ outflow obstruction | 3 (50) | 0 | 14 (70) | 0 |
| Hypercontractile esophagus | 0 | 0 | 0 | 0 |
| Distal esophageal spasm | 0 | 0 | 0 | 0 |
| Absent contractility | 0 | 3 (8) | 0 | 0 |
| Ineffective esophageal motility | 0 | 4 (11) | 2 (10) | 1 (33) |
| Normal motility | 2 (33) | 30 (81) | 4 (20) | 2 (2) |
This patient had systemic sclerosis and a patulous appearing EGJ and barium retention on TBE. REO – reduced EGJ opening; BEO – borderline EGJ opening; NEO – normal EGJ opening
HRM-FLIP discordance was observed in 40/329 (12%) patients (Table 4). Discordance as consistent IRP elevation + NEO was observed in 26/329 (8%) patients (24 patients, 92%, had EGJOO classified on HRM) and accounted for 3% of abnormal TBE and 18% of normal TBEs. Discordance as normal IRP + REO occurred in 14/329 (4%) patients and accounted for 5% of abnormal TBEs and 3% of normal TBEs. Thus, among the 40 FLIP-HRM discordant cases, the HRM-IRP classification was consistent (and FLIP inconsistent) with TBE in 23% (n=9) while the FLIP Panometry classification was consistent (and HRM inconsistent) with TBE in 78% (n=31).
Discussion
In this prospective study of consecutive patients that completed HRM, FLIP Panometry, and TBE for evaluation for primary esophageal motility disorders, FLIP Panometry metrics and classification of EGJ opening outperformed HRM-IRP to predict objective esophageal retention on TBE. FLIP Panometry metrics of EGJ opening, the EGJ-DI and maximum EGJ diameter, demonstrated greater AUROCs than IRP on HRM. Additionally, classification of EGJ obstruction on FLIP Panometry was associated with a substantially stronger predictive relationship than classification of EGJ obstruction using HRM-IRP for predicting esophageal retention based on logistic regression. Further, when HRM and FLIP Panometry were discordant, the FLIP Panometry assessment was the better predictor of esophageal retention in 78% (31/40) of cases. Thus, while the complementary evaluation using HRM and FLIP Panometry, as well as TBE, likely remains necessary in cases with equivocal or borderline findings on a single test, the assessment of EGJ opening with FLIP Panometry provided superior performance for predicting an objective outcome of esophageal function over HRM.
Both HRM and FLIP Panometry provide an evaluation of esophageal motility and EGJ function. While there are shared features between the two evaluations, it is worth noting that HRM and FLIP Panometry evaluate different components of esophageal function: the response to swallows with HRM; the response to distension with FLIP Panometry. Similar to previous studies, the present study demonstrated that the majority of patients with abnormal IRP also have reduced EGJ opening, while the majority with normal IRP have normal EGJ opening.5, 7, 9, 20 Discordant results between HRM and FLIP Panometry were observed in previous studies and again in the present study; a scenario with unclear clinical significance. Thus, a novel approach of the present study was to apply TBE as an objective measure of esophageal retention that was independent of both HRM and FLIP to compare the two modalities. Both the IRP on HRM and FLIP Panometry metrics of EGJ opening (EGJ-DI and maximum EGJ diameter) demonstrated capabilities to differentiate between abnormal and normal esophageal retention, which supports confidence in both tool. However, FLIP Panometry parameters did so more accurately and with greater predictive capability as reflected by ROC and regression analysis. Further, when HRM and FLIP Panometry findings were discordant (which most commonly occurred with EGJOO classified on HRM), the FLIP Panometry results were more frequently associated with esophageal retention than was HRM: 78% of the 40 discordant cases. Overall, the superior performance with FLIP may be related to the more mechanical evaluation of EGJ opening relative to distensive pressure that it provides, compared with IRP that assesses EGJ pressure related to LES relaxation and intrabolus pressure that drives open the EGJ during peristalsis (and is also subject to potential pressure artefact).21
Impaired deglutitive LES relaxation is the essential feature of achalasia and is generally detected via an abnormally-elevated IRP on HRM.2, 4, 22 However, reliance on this single threshold of a single value was recognized as a limitation of earlier versions of the Chicago Classification as it was recognized that achalasia can occur with normal IRP, and (more commonly) that IRP can be elevated in patients that do not have achalasia (sometimes related to pressure artefact).12, 21, 23-25 Previous studies have demonstrated that consistent IRP elevation when performing HRM in two patient positions (supine and upright) improved the detection of EGJ outflow obstruction.26, 27 Hence, consistency of IRP elevation was incorporated into Chicago Classification v4.0 for classification of EGJOO, though the EGJOO classification on HRM was still considered inconclusive, requiring additional complementary evaluation with TBE or FLIP.4, 27, 28 The present study’s finding that the most common occurrence of HRM-FLIP discordance involved elevated IRP and NEO with normal TBE (i.e. suspected false positive IRP) supports that recommendation, and also supports the complementary role for FLIP in inconclusive HRM. With the limitations related with relying on a single IRP threshold in mind, the FLIP Panometry classification of EGJ opening was derived with the intent to apply multiple metrics and multiple thresholds to balance potential limitations of each individual metric, as well as balance sensitivities and specificities. Further, it intended to classify EGJ function with increased diagnostic certainty at the extremes (REO and NEO), while also recognizing that borderline EGJ opening classifications are associated with less diagnostic certainty that would prompt pursuit of additional complementary evaluation. Thus, while BrEO or BnEO may be suggestive of reduced or normal EGJ opening, respectively, TBE and/or HRM results could be incorporated to reach a diagnostic impression.
Bolus clearance is the essential function of the esophagus and its impairment is a consequence of esophageal motility disorders characterized by obstruction and/or lack of propulsion, i.e. impaired peristalsis. In the present study that focused on metrics of EGJ obstruction, retention on TBE was applied as an indirect measure of obstruction. Future study remains warranted to further evaluate the impact of primary peristalsis (HRM) and secondary peristalsis (FLIP Panometry), although, the present study addressed this aspect through application of subgroup analysis excluding patients with absent primary peristalsis (including achalasia). When doing so, the superior performance of the FLIP Panometry EGJ assessment over IRP on HRM persisted. Additionally, small hiatal hernia (type II or type III EGJ morphology on HRM) was also an important factor related to esophageal retention that warrants future investigation. While future studies to evaluate longitudinal outcomes related to treatment response ultimately remain essential, esophageal retention on TBE represents an important objective measure of esophageal function independent of both HRM and FLIP Panometry.
While this study carries strengths related to the large sample size of patients that completed comprehensive evaluation with HRM, FLIP, and TBE and may represent the largest study performed to compare different esophageal motility testing modalities for predication of an objective clinical outcome, there are limitations as well. Beyond the potential limitation of application of TBE as the primary outcome and the future need to assess longitudinal outcomes, the composition of the patient cohort reflects a referral bias (quaternary esophageal referral center). The uncertainty associated with the HRM-EGJOO classification and thus need to obtain multiple tests (HRM, FLIP, and TBE) also may have created a selection bias. Thus patients with achalasia and HRM classification of EGJOO are over represented. While this may somewhat limit direct generalizability of these results to other clinical practices, the results of a patient population devoid of achalasia can be inferred from the subgroup analysis from which achalasia patients were omitted. Further, EGJOO on HRM represents an important esophageal motility pattern as this commonly encountered scenario can create clinical challenges; thus a study of the EGJOO cohort is the focus of an ongoing study to expand upon the observations of this study. Additionally, there are other factors available within the tests that can further facilitate reaching a diagnostic impression (e.g. intrabolus pressurization or provocative maneuvers such as rapid drink challenge on HRM, contractile response on FLIP Panometry; morphologic appearance of EGJ on TBE), and thus future studies to incorporate these other components also remains warranted.
In conclusion, this prospective study that compared HRM and FLIP Panometry for detection of esophageal retention demonstrated that while both HRM and FLIP Panometry carried predictive value for detection of abnormal TBE results, FLIP Panometry provided superior performance to HRM. Thus, this study provides additional support for the use of FLIP Panometry to evaluate esophageal motility as it accurately identifies normal and abnormal retention, but also identifies patients that should undergo further complementary diagnostic testing. Future studies incorporating additional test features and global esophageal motility assessments with HRM and FLIP Panometry, as well as longitudinal clinical outcomes, remain needed to continue to advance the evaluation and management of esophageal motor disorders. Overall, complementary evaluation using FLIP Panometry, TBE, and HRM, likely remains necessary in some cases (particularly those with equivocal findings on a single test) to facilitate accurate characterization of esophageal disease processes, and ultimately direct appropriate management decisions.
Supplementary Material
Grant support:
This work was supported by P01 DK117824 (JEP) from the Public Health service and American College of Gastroenterology Junior Faculty Development Award (DAC).
Footnotes
Disclosures:
JEP, PJK, and Northwestern University hold shared intellectual property rights and ownership surrounding FLIP Panometry systems, methods, and apparatus with Medtronic Inc.
DAC: Medtronic (Speaking, Consulting)
WK: Janisys (Consulting)
PJK: Ironwood (Consulting); Reckitt Benckiser (Consulting)
JEP: Crospon, Inc (stock options), Given Imaging (Consulting, Grant, Speaking), Sandhill Scientific (Consulting, Speaking), Takeda (Speaking), Astra Zeneca (Speaking), Medtronic (Speaking. Consulting), Torax (Speaking, Consulting), Ironwood (Consulting), Impleo (Grant).
AJB, AK, JaEP, JMS , END: nothing to disclose.
References
- 1.Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103(1):27–37. [DOI] [PubMed] [Google Scholar]
- 2.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gyawali CP, Carlson DA, Chen JW, Patel A, Wong RJ, Yadlapati RH. ACG Clinical Guidelines: Clinical Use of Esophageal Physiologic Testing. Am J Gastroenterol. 2020;115(9):1412–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33(1):e14058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol. 2016;111(12):1726–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE. Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil. 2015;27(7):981–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rooney KP, Baumann AJ, Donnan E, et al. Esophagogastric Junction Opening Parameters are Consistently Abnormal in Untreated Achalasia. Clin Gastroenterol Hepatol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baumann AJ, Donnan EN, Triggs JR, et al. Normal Functional Luminal Imaging Probe Panometry Findings Associate With Lack of Major Esophageal Motility Disorder on High-Resolution Manometry. Clin Gastroenterol Hepatol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlson DA, Baumann AJ, Donnan E, Krause A, Kou W, Pandolfino J. Evaluating Esophageal Motility Beyond Primary Peristalsis: Assessing esophagogastric junction opening mechanics and secondary peristalsis in patients with normal manometry. Neurogastroenterol Motil. 2021:e14116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandolfino JE, de Ruigh A, Nicodeme F, Xiao Y, Boris L, Kahrilas PJ. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil. 2013;25(6):496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Triggs JR, Carlson DA, Beveridge C, Kou W, Kahrilas PJ, Pandolfino JE. Functional Luminal Imaging Probe Panometry Identifies Achalasia-Type Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2020;18(10):2209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ponds FA, Bredenoord AJ, Kessing BF, Smout AJ. Esophagogastric junction distensibility identifies achalasia subgroup with manometrically normal esophagogastric junction relaxation. Neurogastroenterol Motil. 2016. [DOI] [PubMed] [Google Scholar]
- 13.Blonski W, Kumar A, Feldman J, Richter JE. Timed Barium Swallow: Diagnostic Role and Predictive Value in Untreated Achalasia, Esophagogastric Junction Outflow Obstruction, and Non-Achalasia Dysphagia. Am J Gastroenterol. 2018;113(2):196–203. [DOI] [PubMed] [Google Scholar]
- 14.Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50(6):765–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Triggs JR, Carlson DA, Beveridge C, Kou W, Kahrilas PJ, Pandolfino JE. Functional Luminal Imaging Probe Panometry Identifies Achalasia-Type Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carlson DA, Kou W, Lin Z, et al. Normal Values of Esophageal Distensibility and Distension-Induced Contractility Measured by Functional Luminal Imaging Probe Panometry. Clin Gastroenterol Hepatol. 2019;17(4):674–81 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kraichely RE, Arora AS, Murray JA. Opiate-induced oesophageal dysmotility. Aliment Pharmacol Ther. 2010;31(5):601–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mittal RK, Frank EB, Lange RC, McCallum RW. Effects of morphine and naloxone on esophageal motility and gastric emptying in man. Dig Dis Sci. 1986;31(9):936–42. [DOI] [PubMed] [Google Scholar]
- 19.de Oliveira JM, Birgisson S, Doinoff C, et al. Timed barium swallow: a simple technique for evaluating esophageal emptying in patients with achalasia. AJR Am J Roentgenol. 1997;169(2):473–9. [DOI] [PubMed] [Google Scholar]
- 20.Baumann AJ, Donnan EN, Triggs JR, et al. Normal Functional Luminal Imaging Probe Panometry Findings Associate With Lack of Major Esophageal Motility Disorder on High-Resolution Manometry. Clin Gastroenterol Hepatol. 2021;19(2):259–68 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Babaei A, Lin EC, Szabo A, Massey BT. Determinants of pressure drift in Manoscan() esophageal high-resolution manometry system. Neurogastroenterol Motil. 2015;27(2):277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015;313(18):1841–52. [DOI] [PubMed] [Google Scholar]
- 23.Lin Z, Kahrilas PJ, Roman S, Boris L, Carlson D, Pandolfino JE. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24(8):e356–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Hoeij FB, Smout AJ, Bredenoord AJ. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2015;27(9):1310–6. [DOI] [PubMed] [Google Scholar]
- 25.Schupack D, Katzka DA, Geno DM, Ravi K. The clinical significance of esophagogastric junction outflow obstruction and hypercontractile esophagus in high resolution esophageal manometry. Neurogastroenterol Motil. 2017;29(10):1–9. [DOI] [PubMed] [Google Scholar]
- 26.Triggs JR, Carlson DA, Beveridge C, et al. Upright Integrated Relaxation Pressure Facilitates Characterization of Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2019;17(11):2218–26 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Babaei A, Shad S, Szabo A, Massey BT. Pharmacologic interrogation of patients with esophagogastric junction outflow obstruction using amyl nitrite. Neurogastroenterol Motil. 2019;31(9):e13668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Triggs JR, Carlson DA, Beveridge C, et al. Upright Integrated Relaxation Pressure Facilitates Characterization of Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.