Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic had a striking impact on healthcare services in the world. The present study aimed to investigate the impact of the COVID-19 pandemic on the presentation management and outcomes of acute appendicitis (AA) in different centers in the Middle East.
Methods
This multicenter cohort study compared the presentation and outcomes of patients with AA who presented during the COVID-19 pandemic in comparison to patients who presented before the onset of the pandemic. Demographic data, clinical presentation, management strategy, and outcomes were prospectively collected and compared.
Results
Seven hundred seventy-one patients presented with AA during the COVID pandemic versus 1174 in the pre-COVID period. Delayed and complex presentation of AA was significantly more observed during the pandemic period. Seventy-six percent of patients underwent CT scanning to confirm the diagnosis of AA during the pandemic period, compared to 62.7% in the pre-COVID period. Non-operative management (NOM) was more frequently employed in the pandemic period. Postoperative complications were higher amid the pandemic as compared to before its onset. Reoperation and readmission rates were significantly higher in the COVID period, whereas the negative appendicectomy rate was significantly lower in the pandemic period (p = 0.0001).
Conclusion
During the COVID-19 pandemic, a remarkable decrease in the number of patients with AA was seen along with a higher incidence of complex AA, greater use of CT scanning, and more application of NOM. The rates of postoperative complications, reoperation, and readmission were significantly higher during the COVID period.
Keywords: COVID-19, Pandemic, Appendicitis, Multicenter, Outcome
Introduction
Acute appendicitis (AA) is the most common cause of acute right iliac fossa (RIF) pain in young patients across the world [1]. The lifetime risk of development of AA is estimated to be approximately 8% [1–4]. AA can be divided into uncomplicated and complicated with either perforation, abscess, peritonitis, or mass [4–8].
Many scoring systems were described to aid in the diagnosis of AA. The Alvarado scoring system is the most widely used score [2]; however, it is not the most performing and cannot differentiate between complicated and uncomplicated AA, especially in the elderly [3]. To confirm the diagnosis of AA, imaging modalities such as ultrasound, computed tomography (CT) scan, and magnetic resonance imaging are often used [3, 4].
Although appendectomy is considered to be the gold standard treatment of uncomplicated AA; antibiotic therapy may be a viable alternative to surgery [9–11]. In carefully selected patients with uncomplicated AA, the use of antibiotics first seems to be safe and successful. At 5 years of follow-up after non-operative management (NOM), recurrence of appendicitis may be recorded in up to 39% of patients [4, 11–15].
The coronavirus disease 2019 (COVID-19) pandemic has placed tremendous pressure on the healthcare systems and organizations across the world, with direct and indirect implications for patient care. According to the World Health Organization (WHO), on December 2021, there have been 263,563,622 confirmed cases of COVID-19, including 5,232,562 deaths [16].
Perioperative transmission of COVID-19 has been a great concern during the pandemic; therefore NOM of AA was suggested as a convenient alternative as per expert advice. With the outbreak of the COVID-19, the management of AA was gradually shifted to a more conservative approach [17–25].
While former studies investigated the impact of the pandemic on the management and outcome of AA, most of these studies were based in Western countries [19–25]. The present study aimed to have a Middle East perspective on the impact of the COVID-19 pandemic on the presentation, management, and outcome of AA and to determine whether it had a different pattern to what has been reported in previous studies. Our hypothesis was that COVID-19 may have had a significant impact on the presentation and outcome of acute appendicitis in the Middle East region, similar to that reported in Western countries. We hypothesized that a reduction in the rate of appendicitis admission during COVID era, an increase in the complexity of AA presentation, and shift of the management paradigm would be observed as compared to the pre-COVID period.
Patients and methods
Study design and strategy
This was a multicenter cohort study that was conducted on patients with AA. The study included data of patients managed at four referral hospitals in two Middle-Eastern countries (Egypt and KSA). The hospitals were urban referral hospitals, serving a population size ranging from two to six million people. Health care for AA was provided for patients free of charge, as a part of the emergency service covered by health insurance in the respective countries.
Patients included in the study were subdivided according to the period of inclusion into group 1, pre-COVID period (March 2019–March 2020), and group 2, COVID period (March 2020–March 2021). Using a computerized patient archive, data were reviewed retrospectively before the COVID pandemic and prospectively during the COVID pandemic.
After careful consideration of the nature of AA as well as possible treatment options and their complications, all patients signed informed consent forms to be a part of this report. The protocol was accepted by the research ethics committees of the participating centers. The study was registered in ClinicalTrials.gov under special identifier NCT05104346.
Management strategy
Patients presented to the emergency department were transferred to the emergency surgical service for further assessment and management. Preoperative assessment included physical examination, complete blood count, and imaging by abdominal ultrasound (US) or abdominal CT scanning. Based on the initial clinical presentation and investigations, Alvarado scores were calculated for every patient [2].
Simple or uncomplicated appendicitis is defined as a phlegmonous inflamed appendix without signs of necrosis, perforation, or abscess, whereas complex or complicated appendicitis had focal or transmural necrosis, which eventually led to perforation that can result in peritonitis or localized abscess [26].
AA was managed by either NOM or appendectomy. NOM was first attempted and if failed, appendectomy was performed. There was no official declaration of the preference of the NOM approach in the participating hospitals, but this was approved based upon the recommendation of society guidelines that considered NOM safe and effective, particularly during the COVID-19 pandemic.
NOM was undertaken in the hospital for the first 48 h, according to the presentation of the patients and response to treatment. NOM entailed strict observation of patients and using antibiotics (Amoxicillin/clavulanate1.2–2.2 g 6-hourly and metronidazole 500 mg 6-hourly). The antibiotics were administered intravenously for a minimum of 48 h in the inpatient setting, and then oral antibiotics were given for 7–10 days on an outpatient basis [4]. The insertion of an intra-abdominal drain guided by US or CT scan was referred to as interventional radiology (IR). Surgical treatment included open or laparoscopic appendectomy. The first line of treatment was conservative management with either antibiotic and/or IR drainage. If failed, treatment was then shifted to surgery 2 days after the initial evaluation.
Postoperative pathologic examination of the postoperative specimens classified acute appendicitis into catarrhal, suppurative, and gangrenous and identified appendix with a normal histology.
Follow-up
Follow-up appointments were scheduled at 1 week and 1, 3, and 6 months after surgery. Follow-up assessments included clinical assessment, complete blood count, and abdominal imaging to assess for any complications.
Study outcomes
The primary outcome was the management strategy of AA (either NOM or surgery) with assessment of their outcome.
Secondary outcomes included the clinical presentation, Alvarado score, postoperative complications classified by Dindo et al. classification [27], operation time, reoperation, readmission, hospital stay, mortality, postoperative pathology (catarrhal, suppurative, and gangrenous), and negative appendicectomy rate.
Data collected
The following data were collected: patient demographics, clinical presentation, radiological findings, management strategy, operative records, postoperative morbidities, duration of hospital stay, pathological findings, rate of negative appendicectomy, readmission to the hospital, reoperation, and mortality.
Statistical analysis
Data for categorical variables were expressed as numbers and proportions, while continuous variables were expressed as mean and standard deviation (SD). All statistical analyses were conducted using SPSS 17™ (IBM corp., Chicago, IL, USA). Student t test was used for processing continuous variables and Fisher exact test or Chi-square test was used to process categorical variables. p value < 0.05 was considered significant. Significant variables were analyzed by a binary logistic regression multivariate model to determine the independent predictors of postoperative complications. The independent predictors were expressed as odds ratios (OR) with their 95% confidence intervals (CI).
Results
Demographic data
This multicentric study included 1174 patients with AA in the pre-COVID period and 771 patients in the COVID period. Both groups were comparable with no significant differences in the mean age, gender, BMI, and medical comorbidities (Table 1).
Table 1.
Demographic data
| Variables |
Pre-COVID period 1174 (60.4%) patients |
COVID period 771 (39.6%) patients |
P values |
|---|---|---|---|
| Country | |||
| Egypt | 608 (61.8%) | 376 (38.2%) | 0.19 |
| Kingdom of Saudi Arabia | 566 (58.9%) | 395 (41.1%) | |
| Mean age (years) | 28.83 ± 12.75 (12–75) | 29.71 ± 11.7 (12–72) | 0.13 |
| Sex | |||
| Male | 718 (61.2%) | 482 (62.5%) | 0.57 |
| Female | 456 (38.8%) | 289 (37.5%) | |
| Symptoms | |||
| Abdominal pain | 1174 (100%) | 771 (100%) | 1 |
| Vomiting | 646 (55%) | 403 (52%) | 0.23 |
| Anorexia | 761 (64.8%) | 478 (62%) | 0.21 |
| Tenderness in RIF | 848 (72.2%) | 521 (74.3%) | 0.13 |
| Rebound tenderness RIF | 786 (65.4%) | 501 (65%) | 0.81 |
| Alvarado scoring | 7.29 ± 1.44 (3–10) | 7.52 ± 1.53 (3–10) | 0.001 |
| Low risk ≥ 4 | 95 (8.1%) | 35 (4.5%) | |
| Moderate risk 5–7 | 345 (29.4%) | 211 (27.4%) | 0.003 |
| High risk 8–10 | 734 (62.5%) | 525 (68.1%) | |
| Mean total leucocyte count | 11.84 ± 11.85 (5–27) | 12.11 ± 3.47 (6–28) | 0.09 |
| Radiological imaging | |||
| None | 281 (23.9%) | 110 (14.3%) | |
| Ultrasound | 157 (13.4%) | 75 (9.7%) | 0.0001 |
| Abdominal CT | 736 (62.7%) | 586 (76%) | |
| Type of presentation | |||
| Non-complicated appendicitis | 1061 (90.4%) | 663 (86%) | |
| Complicated appendicitis | 113 (9.6%) | 108 (14%) | 0.02 |
| Management | |||
| Successful non-operative management | 43 (3.7%) | 124 (16.1%) | |
| Antibiotics-only | 10 (0.85%) | 96 (12.5%) | 0.0001 |
| Interventional radiology | 33 (2.8%) | 37 (4.8%) | |
| Surgical treatment | 1131 (96.3%) | 647 (83.9%) |
Radiological imaging
Radiological imaging was used to confirm AA in 893/1174 (76.1%) patients in the pre-COVID period and 661/771 (85.7%) patients in the COVID period (p = 0.0001). Radiological imaging included abdominal CT and US. Abdominal CT scan was the main imaging modality used in both groups (Table 1).
Clinical presentation
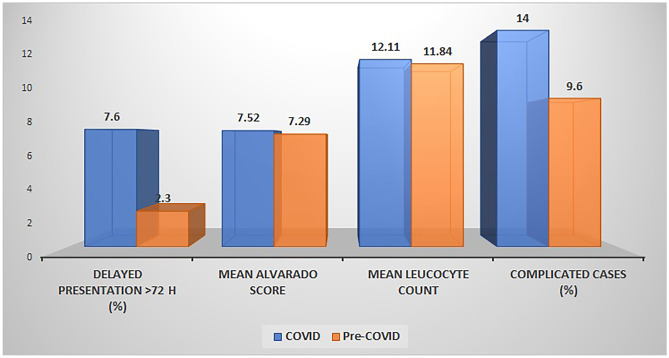
There was no significant difference between the two groups as regards to the clinical symptoms (abdominal pain, anorexia, vomiting), signs, and total leucocytic count. The mean Alvarado score was significantly higher in the COVID period than in the pre-COVID period (Table 1). Complicated AA and delayed presentation after 72 h from the onset of symptoms were more significantly recorded in the COVID period than in the pre-COVID period (Table 2). Of the 1174 patients, 113 (9.6%) were presented with complicated AA in pre-COVID period (33 patients with abscess, 75 with generalized peritonitis, and 5 with mass), while 108/771 (14%) patients were presented with complicated AA in COVID era (37 patients with abscess, 64 with generalized peritonitis, and 7 with mass). Figure 1 illustrates the differences in clinical presentation between the two groups.
Table 2.
Operative data of patients who underwent appendectomy
| Variables | Pre-COVID period 1131 patients | COVID period 647 patients | P value |
|---|---|---|---|
| Country | |||
| Egypt | 636 (70.5%) | 266 (29.5%) | 0.0001 |
| Kingdom of Saudi Arabia | 495 (56.5%) | 381 (43.5%) | |
| Mean Time from presentation to surgery (hours) | 16.97 ± 10.53 | 19.9 ± 13.79 | 0.0001 |
| Surgery within 24 h (early presentation) | 1075 (95%) | 533 (82.4%%) | |
| Surgery 24–72 (borderline presentation) | 30 (2.7%) | 65 (10%) | 0.0001 |
| Surgery after > 72 h (delayed presentation) | 26 (2.3%) | 49 (7.6%) | 0.0001 |
| Presentation | |||
| Non-complicated appendicitis | 1018 (90%) | 539(83.3%) | |
| Complicated appendicitis | 0.02 | ||
| Total | 113 (10%) | 108 (16.7%) | |
| Peritoneal abscess | 33 (2.9%) | 37 (5.7%) | |
| Peritonitis | 75 (6.6%) | 64 (9.9%) | |
| Appendicular inflammatory Mass | 5 (0.44%) | 7 (10.8%) | |
| Operative approach of appendicectomy | |||
| Open | 639 (56.5%) | 380 (58.7%) | |
| Laparoscopic | 492 (43.5%) | 267 (41.3%) | 0.35 |
| Perforated appendix | 95 (8.4%) | 73 (11.3) | 0.046 |
| Site of perforation | |||
| Tip | 68 | 55 | 0.11 |
| Basal | 27 | 18 | 0.11 |
| Appendicular stump closure | |||
| Endoloop | 392 (34.6%) | 190 (29.4%) | 0.0001 |
| Stapled | 76 (6.7%) | 49 (7.6%) | |
| Intracorporeal ligation | 42 (3.7%) | 33 (5.1%) | |
| Open suture ligation | 621 (54.9%) | 375 (58%) | |
| Drain at time of surgery | 136 (12%) | 114 (17.6%) | 0.001 |
| Mean operative time (minutes) | 46.75 ± 8.34 (30–85) | 47.38 ± 9.37 (30–90) | 0.14 |
Fig. 1.
Clinical presentations in COVID period and pre-COVID period
Management of AA
Non-operative management
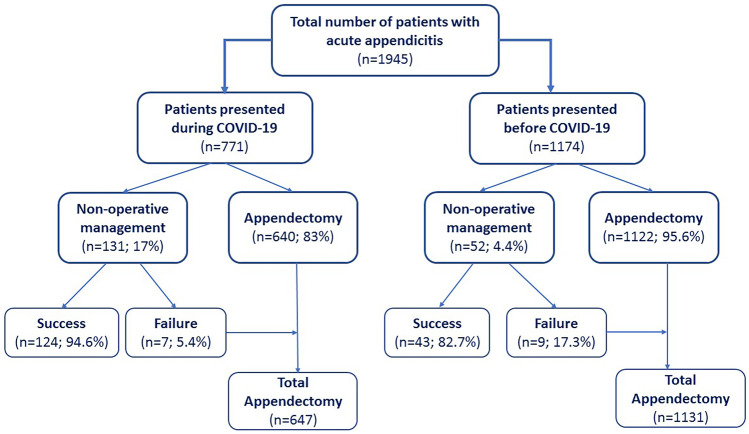
Initial NOM was used in 52 (4.4%) patients in the pre-COVID period versus 131 (17%) in the COVID period (p < 0.0001). Successful NOM was reported in 43/52 patients in the pre-COVID period versus 124/131 patients in the COVID period (p = 0.02) (Fig. 2). Patients who did not respond to NOM underwent appendectomy.
Fig. 2.
Flow chart for management of patients with AA in COVID period and pre-COVID period
Operative management
Of 1131 patients who underwent an appendectomy in the pre-COVID period, the procedure was done laparoscopically in 492 (43.5%) patients and via open approach in 639 (56.5%) patients. Of 647 patients who had an appendectomy in the COVID period, the procedure was done laparoscopically in 267 (41.3%) patients and via an open approach in 380 (58.7%) patients (p = 0.35) (Table 2).
When classified according to the time from symptoms to surgery:
Within 24 h of symptoms onset: 1075 (95%) patients in the pre-COVID period and 533 (82.4%) in the COVID period underwent an appendectomy.
Within 24–72 h of symptoms onset: 30 (2.6%) patients in the pre-COVID period and 65 (10%) patients in the COVID period underwent an appendectomy.
After 72 h from symptoms onset, 26 (2.3%) patients in the pre-COVID period and 49 (7.6%) patients in the COVID period underwent an appendectomy.
Surgical outcomes and complications
The mean hospital stay was significantly longer in the COVID period than in the pre-COVID period (3.57 ± 4.06 vs 2.9 ± 2.18 days; p = 0.0001). The rate of postoperative complications was significantly higher in the COVID period than before COVID (11.3% vs 5.8%, p = 0.0001). A summary of the postoperative complications according to the Clavien-Dindo classification is shown in Table 3. Intra-abdominal collection, ileus, wound infection, pulmonary embolism, and pulmonary complications after appendectomy were significantly more observed in the COVID period.
Table 3.
Outcome of surgical treatment
| Variables | Pre-COVID period | COVID period | P values |
|---|---|---|---|
| Mean hospital stay (days) | 2.9 ± 2.18 (1–25) | 3.57 ± 4.06 (1–28) | 0.0001 |
| Number of patients with complications | 66 (5.8%) | 73 (11.3%) | 0.0001 |
| Complication grade | |||
| I | 26 (2.3%) | 8 (1.2%) | |
| II | 30 (2.7%) | 39 (6%) | 0.0001 |
| III | 10 (0.9%) | 26 (4%) | |
| IV, V | 0 | 0 | |
| Intra-abdominal collection | 26 (2.3%) | 58 (9%) | 0.0001 |
| Mean size of collection | |||
| < 5 cm | 21 | 36 | |
| > 5 cm | 5 | 22 | 0.05 |
| Site of collection | |||
| Pelvic | 15 | 40 | 0..33 |
| Paracolic | 11 | 18 | |
| Management of collection | |||
| Conservative | 22 | 36 | |
| Interventional radiology | 4 | 11 | 0.05 |
| Operative | 0 | 11 | |
| Ileus | 26 (2.3%) | 32 (4.9%) | 0.003 |
| Intestinal obstruction | 6 (0.5%) | 5 (0.8%) | 0.53 |
| Reoperation | 6 (0.5%) | 16 (2.5%) | 0.0001 |
| Indication for reoperation | |||
| Abdominal collection | 0 | 11 | 0.004 |
| Intestinal obstruction | 6 | 5 | |
| Wound infection | 12 (1.1%) | 29 (4.5%) | 0.0001 |
| Pulmonary complications | 14 (1.2%) | 17 (2.6%) | 0.03 |
| DVT | 7 (0.6%) | 5 (0.8%) | 0.7 |
| Pulmonary embolism | 2 (0.2%) | 5 (0.8%) | 0.05 |
| Readmission | 15 (1.3%) | 19 (2.9%) | 0.02 |
| Indications for readmission | |||
| Collection | 6 | 7 | |
| Intestinal obstruction | 3 | 5 | 0.9 |
| Wound infection | 6 | 7 | |
| Postoperative pathology | |||
| Catarrhal appendicitis | 268 (23.7%) | 49 (7.6%) | |
| Suppurative appendicitis | 636 (56.2%) | 404 (62.4%) | 0.0001 |
| Gangrenous appendicitis | 128 (11.3%) | 176 (27.2%) | |
| Normal appendix | 99 (8.8%) | 18 (2.8%) |
Reoperation within 30 days from appendectomy was required for 16 (2.5%) patients in the COVID period (5 had an intestinal obstruction and 11 had abdominal collection) as compared to 6 (0.5%) patients in the pre-COVID period (all 6 had an intestinal obstruction) (p = 00,001). Eleven patients required radiologic-guided drainage of abdominal collection in the COVID period as compared to four patients in the pre-COVID period (Table 3).
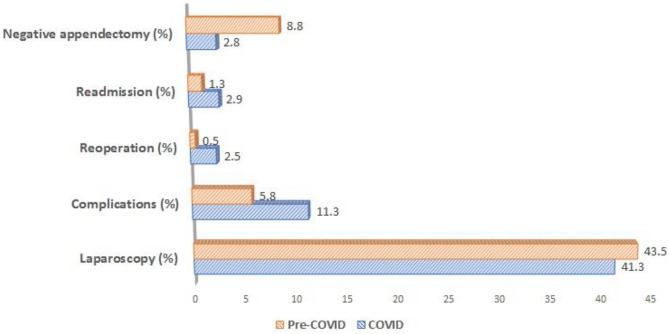
The readmission rate was higher in the COVID period than in the pre-COVID period (2.9% vs 1.3%, p = 0.02). Indications for readmission were intra-abdominal collection, severe wound infection, and intestinal obstruction as summarized in Table 3. Figure 3 illustrates the difference in operative outcomes between the two groups.
Fig. 3.
Surgical outcomes in COVID period and pre-COVID period
Postoperative pathology and negative appendicectomy rate
According to postoperative histopathology, normal appendix histology was confirmed in 99 (8.8%) patients in the pre-COVID period versus 18 (2.8%) patients in the COVID period (p = 0.0001) (Table 3).
The rate of catarrhal appendicitis decreased from 23.7% in the pre-COVID period to 7.6% in the COVID period. Suppurative appendicitis accounted for 60% of cases and gangrenous appendicitis for 25.7% of cases in the COVID period as compared to 56.2% and 11.3% of cases in the pre-COVID period (p = 0.0001).
Factors associated with complications
Univariate analysis revealed seven variables that were significantly associated with the development of postoperative complications. These factors were the time of presentation, complex presentation, perforation of appendix, base status, operation time, postoperative pathology, and period at which patients presented (pre-COVID vs COVID). According to the multivariate logistic regression analysis, presentation during the COVID pandemic, delayed presentation, and perforation of the appendix were the independent predictors of the development of postoperative complications (Table 4).
Table 4.
Univariate and multivariate analyses of complication occurrence
| Variables | Univariate analysis | Multivariate binary logistic regression | |||||
|---|---|---|---|---|---|---|---|
|
No complications 1693 patients |
Complication 139 patients |
P value | Sig. | Exp(B) | 95% C.I. for EXP(B) | ||
| Lower | Upper | ||||||
| Country | |||||||
| Egypt | 831 (92.1%) | 71 (7.9%) | |||||
| Kingdom of Saudi Arabia | 808 (92.2%) | 68 (7.8%) | 0.93 | ||||
| Mean age in years | 29 ± 12.4 | 29.61 ± 13.55 | 0.58 | ||||
| Age group | |||||||
| 12–39 years | 1338 (92.1%) | 114 (7.9%) | |||||
| 40–59 years | 215 (93.7%) | 17 (6.3%) | |||||
| > 60 | 50 (86.2%) | 8 (13.8%) | 0.16 | ||||
| Sex | |||||||
| Male | 1022 (91.9%) | 90 (8.1%) | |||||
| Female | 617 (92.6%) | 49 (7.4%) | 0.58 | ||||
| Period | |||||||
| Pre-COVID | 1065 (94.2%) | 66 (5.8%) | 0.0001 | 0.004 | 1.747 | 1.198 | 2.548 |
| COVID | 574 (88.7%) | 73 (11.3%) | |||||
| Mean Alverado score | 7.41 ± 1.36 | 7.49 ± 1.27 | 0.51 | ||||
| Alvarado scoring | |||||||
| Low risk ≥ 4 | 93 (92.1%) | 8 (7.9%) | |||||
| Moderate risk 5–7 | 439 (93.8%) | 29 (6.2%) | 0.31 | ||||
| High risk 8–10 | 1107 (91.6%) | 102 (8.4%) | |||||
| Time from presentation to surgery (h) | |||||||
| Within 24 h (early presentation) | 1493 (92.8%) | 115 (7.2%) | 0.001 | 0.013 | Ref | ||
| 24–72 (borderline presentation) | 78 (82.1%) | 17 (17.9%) | 0.024 | 3.139 | 1.161 | 8.494 | |
| After > 72 h (late presentation) | 68 (90.7%) | 7 (9.3%) | 0.006 | 2.307 | 1.272 | 4.186 | |
| Presentation | |||||||
| Non-complicated appendicitis | 1494 (92.9%) | 114 (7.1%) | 0.234 | Ref | |||
| Complicated appendicitis | |||||||
| Peritoneal abscess | 18 (90%) | 2 (10%) | 0.004 | 0.104 | 0.533 | 0.250 | 1.139 |
| Peritonitis | 118 (84.9%) | 21 (15.1%) | 0.583 | 0.615 | 0.108 | 3.488 | |
| Appendicular mass | 9 (81.8%) | 2 (18.2%) | 0.341 | 2.150 | 0.445 | 10.839 | |
| Mean leucocyte count | 11.95 ± 3.33 | 12.26 ± 2.92 | 0.3 | ||||
| Approach | |||||||
| Laparoscopic | 693 (91.3%) | 66 (8.7%) | 0.23 | ||||
| Open | 946 (92.8%) | 73 (7.2%) | |||||
| Pathology of appendix | |||||||
| Catarrhal appendicitis | 300 (94.6%) | 17 (12.2%) | 0.307 | 1.684 | 0.620 | 4.575 | |
| Suppurative appendicitis | 961 (92.4%) | 79 (7.6%) | 0.003 | 0.499 | 1.257 | 0.648 | 2.437 |
| Gangrenous appendicitis | 266 (87.5%) | 38 (12.5%) | 0.509 | 1.164 | 0.742 | 1.828 | |
| Normal appendix | 112 (95.7%) | 5 (4.3%) | 0.748 | Ref | |||
| Perforation | |||||||
| Yes | 133 (79.2%) | 35 (20.8%) | 0.0001 | 0.002 | 7.486 | 2.146 | 26.118 |
| No | 1506 (93.5%) | 104 (9.6%) | |||||
| Base status | |||||||
| Healthy | 1491 (93.3%) | 107 (6.7%) | 0.771 | Ref | |||
| Inflamed | 108 (82.4%) | 23 (17.6%) | 0.0001 | 0.515 | 0.634 | 0.161 | 2.500 |
| Necrotic | 40 (81.8%) | 9 (18.4%) | 0.965 | 0.980 | 0.403 | 2.384 | |
| Mean operation time in minutes | 46.75 ± 8.54 | 49.68 ± 10.4 | 0.002 | 0.474 | 0.992 | 0.970 | 1.014 |
Discussion
Clinical practice has changed dramatically amid the COVID-19 pandemic due to concerns about infection transmission, self-isolation/social distancing, shortage of PPE, and overwhelmed healthcare services [15–22]. The present study assessed the impact of the COVID-19 pandemic on the management and outcomes of AA in the Middle East as compared to before the pandemic.
Our first observation was that the number of patients referred with AA during the pandemic was reduced by approximately one third, as compared to a parallel period before COVID-19. This could be explained by either selection bias since some patients with undiagnosed resolving appendicitis during the pandemic remain unreported or because many patients with abdominal pain were reluctant to seek medical care at the hospital as they were afraid of contracting COVID-19. Interestingly, while there was a marked reduction in appendicitis admissions in the Egyptian hospitals, only a slight reduction in admissions was seen in the Saudi hospitals. This difference may be related to different population numbers (6 million versus 2 million), different cultural factors, different healthcare systems with regard to referrals, and different insurance policies between the two countries.
The reduction in the rate of appendicitis admission may also explain the delayed presentation of patients with AA during the pandemic. We postulate that the mandatory confinement and lock-downs have caused delays in consultation, which may have impacted the postoperative outcomes of AA. Delayed presentation of AA has been already observed by other investigators in the COVID period and is often associated with a more severe condition and a higher risk of perforation and intra-abdominal infection [17, 18, 28–33]. Indeed, our study found that delayed presentation after 72 h from the onset of symptoms was significantly higher in the COVID period, and this was associated with more complicated AA than in the pre-COVID period.
Another interesting finding was that radiological investigations were increasingly used to confirm AA amid the pandemic as compared to before its onset. This may explain the lower rate of negative appendicectomy in the COVID period. The use of imaging to confirm the diagnosis of AA before proceeding to surgery, especially in clinically equivocal cases, has been linked to a lower rate of negative appendicectomy in the literature. Although a combination of clinical judgment and US is recommended for the diagnosis of AA, the sensitivity and accuracy of CT scanning are higher than clinical examination and US, and in addition US is mostly operator dependent. Therefore, the use of CT scanning has been favored and expanded considerably since the COVID pandemic [3–7, 17–21, 29, 33–40]. That is why CT scan was the main modality used to confirm the diagnosis of AA in our study.
A paradigm shift in the management of AA was noted during the pandemic. Although appendectomy has been always considered the gold standard for AA care [12], recent research indicates that NOM with antibiotics may be another feasible option. Several systematic reviews and randomized controlled trials evaluated the outcome of NOM for AA over the last decade. As the COVID-19 crisis has evolved, NOM of AA has become more widely adopted [8–13]. Antibiotics are not inferior to appendectomy according to the “CODA” trial [10], yet antibiotic-alone therapy is associated with a longer hospital stay, and nearly 30% of patients treated with antibiotics needed appendectomy within a year [34]. Another important aspect to consider is appendiceal malignancies that account for up to 2.5% of the appendectomy specimens. There is a concern that antibiotic-only treatment may cause a delay in the diagnosis and management of incidental malignancies [35, 36].
Uncomplicated AA should be treated conservatively during the COVID-19 pandemic, when possible, as per the recommendation of a recent meta-analysis. On the other hand, percutaneous drainage should be used to treat an appendicular abscess, whereas perforated appendicitis should be treated with an open approach [19, 20, 37]. Surgical societies have advocated an initial trial of NOM for AA based on the surgeon’s judgment and the patient’s situation due to the increased risks of appendectomy during the pandemic. Since then, many hospitals around the world have accepted NOM as the preferred approach for AA [20, 38–43].
Talan and Di Saverio [43] reported that NOM is associated with a shorter duration of disability than appendectomy, does not usually necessitate hospitalization, and is not related to an increased hazard of perforation. Clinical studies have found similar quality of life after NOM and appendectomy. However, the risk of recurrence of AA after NOM, estimated to be 30–40% in 5 years, should be considered, unlike appendectomy that virtually has zero recurrence rate. Recurrent AA may contribute to an increased rate of subsequent hospitalization after NOM. Patients should be informed of the benefits and drawbacks of each approach and should take part in decision-making.
In the current study, the rate of application and success of NOM was significantly higher in the COVID period than in the pre-COVID period. However, the implementation of NOM during the pandemic might be difficult, as recent studies have shown that AA has a more complicated pathology and a higher risk of perforation during the pandemic, most likely due to the delayed presentation. As a result, many patients with AA do not meet the requirements for NOM. Whether NOM can provide a feasible alternative to appendectomy in patients with AA during the pandemic, this warrants further investigation [38–45].
Laparoscopic appendectomy has many benefits over open surgery, including shorter recovery time and a lower rate of postoperative morbidities [10, 13, 14, 44–51]. In the early stages of the pandemic, open surgery was favored to reduce exposure without impacting operation time. To minimize healthcare worker exposure to virus particles in the peritoneal fluid and aerosolized virus in pneumoperitoneum, it was recommended to perform open rather than laparoscopic surgery [17–23, 47–54]. In the present study, appendectomy was laparoscopically performed in 43.5% of patients in the pre-COVID period versus 41.3% in the COVID period. It is notable that many patients were operated on via an open approach, and this is attributed to the limited resources in some of the participating hospitals that did not allow the use of laparoscopy in the emergency setting. Interestingly, COVID-19 did not have a significant impact on the use of laparoscopy in our region. This goes in line with some studies that could not isolate the virus from the peritoneal fluid in COVID-19-infected patients which renders the use of laparoscopy safe [46–56].
Regardless of the surgical technique, more complicated appendicitis was noted during the COVID period, as compared to the pre-COVID period. This could be explained by patients presenting late to the hospital because of fear during the COVID pandemic or people postponing surgery after failing NOM. Delayed surgery has been related to higher rates of perforation and complex AA [10, 19, 20, 49–55].
Postoperative complications were significantly more recorded in the COVID period. In most of the studies, the complication rate ranged from 10–14% in the COVID period to 5–8% in the pre-COVID period [48–53]. Most complications were minor and included incisional surgical site infections and seromas, with no mortality. Serious complications after appendectomy in the form of intestinal obstruction, intra-abdominal collection, ileus, and pulmonary embolism were significantly more recorded in the COVID period [20–27, 43–56]. This finding is mostly attributed to more complex and delayed presentation in the COVID period. When patients with AA postpone seeking medical care, usually at surgery there would be more peritonitis and free fluid which increase the odds of postoperative collection, infection, ileus, and complications overall [47–58]. Similarly, reoperation and readmission rates were significantly higher in the COVID period. The higher reoperation and readmission can be explained on the same basis as the higher complications; owing to more complex and delayed presentation of patients that results in higher complications that require re-intervention and readmission to manage.
Willms et al. [54] included a total of 1915 appendectomies from 41 hospitals in Germany and found that the rate of complicated appendicitis increased significantly in the COVID period, whereas the rate of negative appendectomies decreased significantly. However; postoperative morbidity and mortality did not change significantly as compared to before the pandemic.
In this study, the negative appendectomy rate was confirmed in 8.8% of patients in the pre-COVID period versus 2.8% in the COVID period (p = 0.0001). The lower negative appendectomy rate in the COVID period may be attributed to strict selection criteria, entailing an increased use of CT scans that were applied before appendectomy during the COVID-19 period. This was to avoid non-indicated surgery and unnecessary use of operation rooms and resources at these difficult times [31, 32, 53, 54, 59].
Finally, although the outcomes of this study were similar to what has been reported in previous studies from Western countries, there were no data on this topic presented from the Middle East before. This manuscript mainly presents a Middle-East perspective on a hot topic that is the management and outcome of AA during the pandemic. It would be useful for the international readers and surgeons to know different perspectives from different data sources around the world in order to determine what is similar and what is different which may help guide their management of AA during the pandemic.
Conclusions
During the COVID-19 pandemic, a significant decrease in the number of patients with AA was seen in the emergency department with a higher incidence of complex AA and delayed presentation. When compared to the pre-COVID period, the Alvarado score during the COVID period was higher. During the COVID period, radiological imaging of AA became increasingly used, and more NOM for AA was applied. No significant decrease in the use of laparoscopy during the pandemic was noted. The negative appendectomy rate was significantly lower in the COVID period. The rates of postoperative complications, reoperation, and readmission were significantly higher in the COVID period. Time of presentation and perforation were the independent predictors of postoperative complications.
Author contribution
Study conception and design: Ayman El Nakeeb, Sameh Hany Emile Mohamed Attia, Mohammed M. Mohammed, Ahmad El Malki. Acquisition of data: Ayman El Nakeeb, Sameh Hany Emile, Mohamed Attia, Ahmed Abd elMawla, Mohamed Alzahrani, Ayman ElGamdi, Abd elwahab Nouh, Abdulaziz Alshahrani, Riyadh AlAreef, Taha Kayed, Hosam Mohamad Hamza, Ahmad AlMalki, Fares Rayzah, Motaz Alsharif, Fares Alsharif, Mohammed M. Mohammed. Analysis and interpretation of data: Ayman El Nakeeb, Sameh Hany Emile, Mohamed Attia, Mohamed Alzahrani, Mohammed M. Mohammed. Critical revision of manuscript: Ayman El Nakeeb, Sameh Hany Emile, Ahmad AlMalki, Mohamed Alzahrani, Mohammed M. Mohammed.
Declarations
Conflict of interest
No any conflict of interest.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ayman El Nakeeb, Email: elnakeebayman@yahoo.com.
Sameh Hany Emile, Email: sameh200@hotmail.com.
Ahmed AbdelMawla, Email: drahmedabdelmawla71@gmail.com.
Mohamed Attia, Email: dr_mohamedattia410@hotmail.com.
Mohamed Alzahrani, Email: mz2am@Hotmail.com.
Ayman ElGamdi, Email: alamodiayman@gmail.com.
Abd elwahab Nouh, Email: awnoah@yahoo.com.
Abdulaziz Alshahrani, Email: jgjc_11@hotmail.com.
Riyadh AlAreef, Email: dr.riyadh55@gmail.com.
Taha Kayed, Email: tahasurg.th@gmail.com.
Hosam Mohamad Hamza, Email: Hossam.hamza@mu.edu.eg.
Ahmad AlMalki, Email: ahmadmosra@gmail.com.
Fares Rayzah, Email: fares_rayzah@yahoo.com.
Motaz Alsharif, Email: motazalshrif@gmail.com.
Fares Alsharif, Email: faresalsharif@gmail.com.
Mohammed M. Mohammed, Email: drmohammedmostafa83@gmail.com
References
- 1.Bhangu A, Søreide K, Di Saverio S, et al. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(278–1287):10000. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 2.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 3.Bhangu A, RIFT Study Group on behalf of the West Midlands Research Collaborative Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg. 2020;107:73–86. doi: 10.1002/bjs.11440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27. doi: 10.1186/s13017-020-00306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho SU, Oh SK. Diagnostic accuracy of magnetic resonance imaging for acute appendicitis during pregnancy: a systematic review. Ulus Travma Acil Cerrahi Derg. 2021;27(3):271–277. doi: 10.14744/tjtes.2020.02416. [DOI] [PubMed] [Google Scholar]
- 6.Bom WJ, Bolmers MD, Gans SL, et al. Discriminating complicated from uncomplicated appendicitis by ultrasound imaging, computed tomography or magnetic resonance imaging: systematic review and meta-analysis of diagnostic accuracy. BJS Open. 2021;5(2):zraa030. doi: 10.1093/bjsopen/zraa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ranieri DM, Enzerra MD, Pickhardt PJ. Prevalence of appendicoliths detected at CT in adults with suspected appendicitis. AJR Am J Roentgenol. 2021;216(3):677–682. doi: 10.2214/AJR.20.23149. [DOI] [PubMed] [Google Scholar]
- 8.van Rossem CC, Bolmers MD, Schreinemacher MH, et al. Diagnosing acute appendicitis: surgery or imaging? Colorectal Dis. 2016;18(12):1129–1132. doi: 10.1111/codi.13470. [DOI] [PubMed] [Google Scholar]
- 9.Podda M, Gerardi C, Cillara N, et al. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg. 2019;270(6):1028–1040. doi: 10.1097/SLA.0000000000003225. [DOI] [PubMed] [Google Scholar]
- 10.Collaborative CODA, Flum DR, Davidson GH, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020;383(20):1907–1919. doi: 10.1056/NEJMoa2014320. [DOI] [PubMed] [Google Scholar]
- 11.Köhler F, Hendricks A, Kastner C, et al. Laparoscopic appendectomy versus antibiotic treatment for acute appendicitis-a systematic review. Int J Colorectal Dis. 2021 doi: 10.1007/s00384-021-03927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marin D, Ho LM, Barnhart H, et al. Percutaneous abscess drainage in patients with perforated acute appendicitis: effectiveness, safety, and prediction of outcome. Am J Roentgenol. 2010;194(2):422–429. doi: 10.2214/AJR.09.3098. [DOI] [PubMed] [Google Scholar]
- 13.Ruffolo C, Fiorot A, Pagura G, et al. Acute appendicitis: what is the gold standard of treatment? World J Gastroenterol. 2013;19(47):8799–8807. doi: 10.3748/wjg.v19.i47.8799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Athanasiou C, Lockwood S, Markides GA. Systematic review and meta-analysis of laparoscopic versus open appendicectomy in adults with complicated appendicitis: an update of the literature. World J Surg. 2017;41(12):3083–3099. doi: 10.1007/s00268-017-4123-3. [DOI] [PubMed] [Google Scholar]
- 15.Quah GS, Eslick GD, Cox MR. Laparoscopic appendicectomy is superior to open surgery for complicated appendicitis. Surg Endosc. 2019;33(7):2072–2082. doi: 10.1007/s00464-019-06746-6. [DOI] [PubMed] [Google Scholar]
- 16.WHO (2021) Coronavirus disease 2019 (COVID-19) Situation Report. Weekly epidemiological update on COVID-19 - 30 March 2021. Data as received by WHO from national authorities, as of 10, as received by WHO from national authorities, as of 10, am CEST 28 March 2021 Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---31-march-2021. https://covid19.who.int/
- 17.Nepogodiev D, Bhangu A, Glasbey JC, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finkelstein P, Picado O, Muddasani K, et al. A retrospective analysis of the trends in acute appendicitis during the COVID-19 pandemic. J Laparoendosc Adv Surg Tech A. 2021;31(3):243–246. doi: 10.1089/lap.2020.0749. [DOI] [PubMed] [Google Scholar]
- 19.Cheruiyot I, Sehmi P, Ngure B, et al. Laparoscopic surgery during the COVID-19 pandemic: detection of SARS-COV-2 in abdominal tissues, fluids, and surgical smoke. Langenbecks Arch Surg. 2021 doi: 10.1007/s00423-021-02142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Saverio S, Pata F, Khan M, et al. Convert to open: the new paradigm for surgery during COVID-19? Br J Surg. 2020;107(7):e194. doi: 10.1002/bjs.11662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Saverio S, Khan M, Pata F, et al. Laparoscopy at all costs? Not now during COVID-19 outbreak and not for acute care surgery and emergency colorectal surgery: a practical algorithm from a hub tertiary teaching hospital in Northern Lombardy. Italy. J Trauma Acute Care Surg. 2020;88(6):715–718. doi: 10.1097/TA.0000000000002727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Köhler F, Acar L, van den Berg A, et al. Impact of the COVID-19 pandemic on appendicitis treatment in Germany-a population-based analysis. Langenbecks Arch Surg. 2021;406(2):377–383. doi: 10.1007/s00423-021-02081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antakia R, Xanthis A, Georgiades F, et al. Acute appendicitis management during the COVID-19 pandemic: a prospective cohort study from a large UK centre. Int J Surg. 2021;86:32–37. doi: 10.1016/j.ijsu.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basamh M, Rajendiran A, Chung WY, et al. Management of appendicitis during the COVID pandemic: lessons from the first month of the outbreak. Br J Surg. 2020;107(11):e450–e451. doi: 10.1002/bjs.11910. [DOI] [PubMed] [Google Scholar]
- 25.Ielpo B, Podda M, Pellino G, et al. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Appy Study. Br J Surg. 2021;108(6):717–726. doi: 10.1002/bjs.11999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bom WJ, Scheijmans JCG, Salminen P, Boermeester MA. Diagnosis of uncomplicated and complicated appendicitis in adults. Scand J Surg. 2021;110(2):170–179. doi: 10.1177/14574969211008330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tankel J, Keinan A, Blich O, et al. The decreasing incidence of acute appendicitis during COVID-19: a retrospective multi-centre study. World J Surg. 2020;44(8):2458–2463. doi: 10.1007/s00268-020-05599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao Z, Li M, Zhou H, et al. Complicated appendicitis are common during the epidemic period of 2019 novel coronavirus (2019-nCoV) Asian J Surg. 2020;43(10):1002–1005. doi: 10.1016/j.asjsur.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Javanmard-Emamghissi H, Boyd-Carson H, Hollyman M, et al. The management of adult appendicitis during the COVID-19 pandemic: an interim analysis of a UK cohort study. Tech Coloproctol. 2021;25(4):401–411. doi: 10.1007/s10151-020-02297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ceresoli M, Coccolini F, Magnone S, Appendicitis-COVID study group et al. The decrease of non-complicated acute appendicitis and the negative appendectomy rate during pandemic. Eur J Trauma Emerg Surg. 2021;47(5):1359–1365. doi: 10.1007/s00068-021-01663-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somers K, Abd Elwahab S, Raza MZ, et al. Impact of the COVID-19 pandemic on management and outcomes in acute appendicitis: should these new practices be the norm? Surgeon. 2021;19(5):e310–e317. doi: 10.1016/j.surge.2021.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turanli S, Kiziltan G. Did the COVID-19 pandemic cause a delay in the diagnosis of acute appendicitis? World J Surg. 2020 doi: 10.1007/s00268-020-05825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015:CRD42015016882) Ann Surg. 2017;265(5):889–900. doi: 10.1097/SLA.0000000000002039. [DOI] [PubMed] [Google Scholar]
- 35.Smeenk RM, van VelthuysenMLF VVJ, et al. Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol. 2008;34(2):196–201. doi: 10.1016/j.ejso.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 36.Kangaspunta H, Tahkola K, Wirta EV, et al. Preoperative computed tomography is poor in detecting tumors of the appendix among patients with acute appendicitis: a cohort study of 5,224 appendectomies. J Trauma Acute Care Surg. 2020;88(3):396–401. doi: 10.1097/TA.0000000000002567. [DOI] [PubMed] [Google Scholar]
- 37.Moletta L, Pierobon ES, Capovilla G, et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int J Surg. 2020;2020(79):180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Emile SH, Hamid HKS, Khan SM, et al. Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: systematic review and meta-analysis. J Gastrointest Surg. 2021;25(7):1905–1915. doi: 10.1007/s11605-021-04988-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Emile SH. Finding a place for non-operative management of acute appendicitis: COVID-19 as an example. Am J Surg. 2021 doi: 10.1016/j.amjsurg.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giljaca V, Nadarevic T, Poropat G, et al. (2017), Diagnostic accuracy of abdominal ultrasound for diagnosis of acute appendicitis: systematic review and meta-analysis. World J Surg. 2017;41(3):693–700. doi: 10.1007/s00268-016-3792-7. [DOI] [PubMed] [Google Scholar]
- 41.Podda M, Cillara N, Di Saverio S, et al. Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15(5):303–314. doi: 10.1016/j.surge.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Di Saverio S, Sibilio A, Giorgini E, et al. Treatment of acute uncomplicated appendicitis. Ann Surg. 2014;260(1):109–117. doi: 10.1097/SLA.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 43.Talan DA, Di Saverio S. Treatment of acute uncomplicated appendicitis. N Engl J Med. 2021;385(12):1116–1123. doi: 10.1056/NEJMcp2107675. [DOI] [PubMed] [Google Scholar]
- 44.Emile SH, Hamid HKS (2020) A critical review of the safety of minimally invasive surgery in the era of COVID-19. Minim Invasive Ther Allied Technol 1–7 [DOI] [PubMed]
- 45.Dreifuss NH, Schlottmann F, Sadava EE, et al. Acute appendicitis does not quarantine: surgical outcomes of laparoscopic appendectomy in COVID-19 times. Br J Surg. 2020 doi: 10.1002/bjs.11806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.GlobalSurg Collaborative Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a multicenter, prospective, cohort study. Surg Endosc. 2018;32(8):3450–3466. doi: 10.1007/s00464-018-6064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ngaserin SH, Koh FH, Ong BC, et al. COVID-19 not detected in peritoneal fluid: a case of laparoscopic appendicectomy for acute appendicitis in a COVID-19-infected patient. Langenbecks Arch Surg. 2020;405(3):353–355. doi: 10.1007/s00423-020-01891-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Romero-Velez G, Pereira X, Zenilman A, et al. SARS-Cov-2 was not found in the peritoneal fluid of an asymptomatic patient undergoing laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech. 2020;30(6):e43–e45. doi: 10.1097/SLE.0000000000000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Turanli S, Kiziltan G. Did the COVID-19 pandemic cause a delay in the diagnosis of acute appendicitis? World J Surg. 2021;45(1):18–22. doi: 10.1007/s00268-020-05825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El Boghdady M, Ewalds-Kvist BM. Laparoscopic surgery and the debate on its safety during COVID-19 pandemic: a systematic review of recommendations. Surgeon. 2021;19(2):e29–e39. doi: 10.1016/j.surge.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mintz Y, Arezzo A, Boni L, et al. The risk of COVID-19 transmission by laparoscopic smoke may be lower than for laparotomy: a narrative review. Surg Endosc. 2020;34(8):3298–3305. doi: 10.1007/s00464-020-07652-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Köhler F, Müller S, Hendricks A, et al. Changes in appendicitis treatment during the COVID-19 pandemic - A systematic review and meta-analysis. Int J Surg. 2021;95:106148. doi: 10.1016/j.ijsu.2021.106148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ganesh R, Lucocq J, Ekpete NO, et al. Management of appendicitis during COVID-19 pandemic; short-term outcomes. Scott Med J. 2020;65(4):144–148. doi: 10.1177/0036933020956316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Willms AG, Oldhafer KJ, Conze S, et al. Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch Surg. 2021;406(2):367–375. doi: 10.1007/s00423-021-02090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim CW, Lee SH. Impact of COVID-19 on the care of acute appendicitis: a single-center experience in Korea. Ann Surg Treat Res. 2021;101(4):240–246. doi: 10.4174/astr.2021.101.4.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Patel M, Thomas JJ, Sarwary H. We can reduce negative paediatric appendicectomy rate: A cohort study. Ann Med Surg (Lond). 2021;71:102901. doi: 10.1016/j.amsu.2021.102901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zheng Z, Bi JT, Liu YQ (2021) The impact of COVID-19 pandemic on the treatment of acute appendicitis in China. Int J Color Dis 1–5 [DOI] [PMC free article] [PubMed]
- 58.Rudnicki Y, Soback H, Mekiten O et al (2021) The impact of COVID-19 pandemic lockdown on the incidence and outcome of complicated appendicitis. Surg Endosc 1–7 [DOI] [PMC free article] [PubMed]
- 59.Sartori A, Podda M, Botteri E, et al. Appendectomy during the COVID-19 pandemic in Italy: a multicenter ambispective cohort study by the Italian Society of Endoscopic Surgery and new technologies (the CRAC study) Updates Surg. 2021;73(6):2205–2213. doi: 10.1007/s13304-021-01126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]