To the Editor,
The United Kingdom (UK) government set a target of offering all adults 2 doses of vaccination against the novel pandemic coronavirus (SARS-CoV-2, COVID-19) by 19th July 2021. The success of this national immunisation programme is dependent on both patient engagement and efficacy of the host immune response. Information on these factors remains limited in the setting of primary and secondary immunodeficiency [1, 2]. Here we report on vaccine uptake and responses in adults under care of the Immunodeficiency Centre for Wales (ICW) revealing heterogenous anti-SARS-CoV-2 spike IgG responses across common diagnostic immunodeficiency sub-groups. With continued community circulation of SARS-CoV-2 and rising case rates, serosurveillance of vulnerable patient groups facilitates prompt and rational access to precision therapies such as monoclonal anti-SARS-CoV-2 antibodies.
Vaccine Uptake and Safety
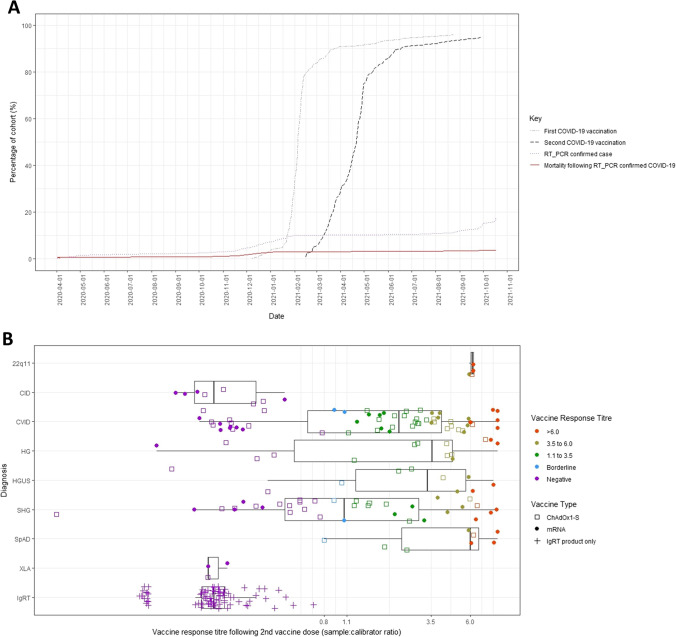
A postal survey and electronic notes review were conducted up to 31st October 2021. Data on vaccine uptake were available for 302/304 (99%) adults under follow-up for immunodeficiency (Supplementary Fig. 1; Supplementary Methods). COVID-19 vaccinations commenced from 8th December 2020, with 287/304 (94.4%) of individuals receiving their first dose by 24th August 2021. Second dose uptake reached 284/304 (93.4%) by 28th September 2021, Fig. 1A. The majority of individuals received the AstraZeneca ChAdOx1-S (176/284, 61.3%), with 39.4% receiving mRNA vaccinations (Pfizer, n = 111; Moderna, n = 1). The median interval between first and second doses was 77 days (inter-quartile range: 50 to 81 days), in line with the UK’s strategy for a 3-month interval. At least fourteen individuals declined or deferred two vaccine doses. The commonest cited reason was the personal belief that they would not respond due to underlying immunodeficiency (n = 6), with 4 patients who had recovered from SARS-CoV-2 infection also declining. Four individuals had deferred courses reflecting recent haematopoietic stem cell transplant, pregnancy, or age under 18 years at the start of the national vaccination scheme. Vaccinations were well tolerated across the cohort with no severe reactions reported.
Fig. 1.
Uptake and serological response following 2 doses of COVID-19 vaccination in adults under care of the Immunodeficiency Centre for Wales. A Uptake of first (grey, dot-dashed) and second (black, dashed) COVID-19 vaccination; cumulative total of patient cohort with molecularly confirmed SARS-CoV-2 infection (purple, dotted) and subsequent mortality (red, solid). Shielding of clinically extremely vulnerable individuals in Wales was implemented between March and August 2020, directing such individuals to stay at home to protect themselves. B Anti-SARS-CoV-2 spike IgG serum responses elicited by 2 doses of COVID-19 vaccination in individuals under care of the Immunodeficiency Centre for Wales (ICW) assayed using the semi-quantitative EUROIMMUN IgG assay. Vaccine response indicated on the x-axis by sample:calibrator ratio. Titre grading shown reflects assay cut-off and reported criteria used for selection of convalescent plasma therapy at that time. Patients are sub-grouped by clinical diagnosis (22q11- DiGeorge 22q11 deletion syndrome; CID- Combined Immunodeficiency (without defined molecular diagnosis, including Good’s syndrome); CVID- common variable immunodeficiency syndrome; HG- hypogammaglobulinaemia (insufficient to meet criteria for CVID); HGUS- hypogammaglobulinaemia of uncertain significance (not requiring immunoglobulin replacement therapy); SHG- secondary hypogammaglobulinaemia; SpAD- specific antibody deficiency; XLA- X-linked agammaglobulinaemia; IgRT- immunoglobulin replacement therapy products, diluted to simulate in vivo infusion at replacement dosing). Vaccine type indicated by open squares (ChAdOx1-S, AstraZeneca) and filled circles (mRNA, Pfizer)
By comparison, at time of submission, at least 49 adults (approximately 16% of the ICW cohort) have had molecularly confirmed SARS-CoV-2 infection between 1st March 2020 and 31st October 2021. COVID-19-related mortality occurred in 11 of these 49 exposed individuals (22.4%). The majority of deaths were in unvaccinated individuals (9/11, 81.8%) prior to vaccine rollout or invitation. Together, this demonstrates vaccination uptake outpaced SARS-CoV-2 infections (Fig. 1A), consistent with national policy for shielding extremely vulnerable individuals between March and August 2020. Notably, two deaths occurred despite two doses of mRNA vaccination, in individuals diagnosed with combined immunodeficiency (CID).
Assessment of Vaccine Efficacy Anti-spike SARS-CoV-2 IgG Responses
Subsequent to these deaths, an increasing range of monoclonal antibody and antiviral therapies have received regulatory approval. In the UK, these have initially been targeted to symptomatic individuals who have failed to initiate a humoral immune response to the virus [3]. We therefore determined anti-spike SARS-CoV-2 IgG responses in patients as part of routine clinical care up to the 2nd September 2021. Primary analysis was undertaken considering samples obtained at least 14 days following completion of two COVID-19 vaccinations (n = 156, 51.3% of the cohort). The median interval from second vaccine to sampling was 49 days (inter-quartile range: 31 to 77 days). As shown in Fig. 1B and Supplementary Table 1, vaccine response varied both between and within common clinical diagnostic groups.
Overall, 51/156 (33%) of patients had an undetectable humoral IgG response to the SARS-CoV-2 spike antigen. Considering diagnostic sub-groups, humoral responses were absent in patients with X-linked agammaglobulinaemia (XLA, n = 3) and CID (n = 8, including both individuals dying from COVID-19 despite vaccination). Failure to seroconvert post-vaccination was common in 16/35 (46%) individuals with secondary hypogammaglobulinaemia (SHG, see online supplementary for full details), and 17/60 (27%) with common variable immunodeficiency (CVID). Conversely, anti-spike IgG responses were consistently observed in individuals with a prior diagnosis of specific antibody deficiency (SpAD, n = 8) and with 22q11 deletion syndrome (n = 4).
A multivariate linear regression model examining the influence of age, time since vaccination, endogenous IgA and IgM levels, CD19 + cell count, vaccine type, immunological diagnosis, and molecularly confirmed SARS-CoV-2 infection preceding the date of vaccine response assessment is presented online (Supplementary Table 2). Increasing time since vaccination was associated with falling titres, consistent with waning (p = 0.041). Combined deficiency of IgA and IgM (p = 0.01) or a CD19 + B-cell count less than 50 × 106/L (p < 0.001) were both independently associated with impairment of the humoral vaccine response. Controlling for other variables, post-vaccination titres were greater in recipients of Pfizer mRNA vaccinations (p = 0.012), equating to a 50% increase, relative to a modelled similar individual receiving the ChAdOx1-S. Conversely, a history of molecularly confirmed SARS-CoV-2 infection prior to vaccination or age was not associated with significant differences in post-vaccine titre.
Anti-spike SARS-CoV-2 IgG Within Immunoglobulin Replacement Therapy Products
The presence of anti-SARS-CoV-2 antibodies within immunoglobulin replacement therapy (IgRT) products has been predicted to interfere with assessment of humoral vaccine immunity [4]. Evaluation of 13 distinct immunoglobulin products (with a total of 87 unique lots) manufactured between December 2018 and March 2021 is shown in Fig. 1B and Supplementary Fig. 2. This confirms increasing levels of IgG with reactivity to the SARS-CoV-2 spike protein in products manufactured since the onset of the pandemic from multiple suppliers. However, at dilutions commonly used to model bioavailability of IgRT therapy, these results fall short of the assay cut-off for a positive immune response. At dilution factors simulating higher replacement or immunomodulatory doses, this threshold was crossed (Supplementary Fig. 3). Together, this suggests the results of vaccine serosurveillance at this timepoint in patients receiving IgRT reflect the endogenous humoral response.
Summary
In conclusion, we observed a high rate of engagement with the COVID-19 vaccination programme in our national cohort of immunodeficient individuals. Whilst of modest size, it compares favourably to existing reports [1, 2]. To our knowledge, we are the first to examine rates and reasons for vaccine hesitancy in this patient group. We show a detectable IgG response to the viral spike protein was absent in approximately 1 in 3 patients, but with marked variation between and within clinical diagnostic groups. Importantly, a diagnosis of CVID, one of the most common primary immunodeficiency disorders, was associated with a detectable vaccine response in two-thirds of individuals. Therefore, our results may also help encourage hesitant individuals, particularly given emerging evidence for T-cell mediated immunity in similar cohorts [1, 2, 4]. Following adjustment for demographic and diagnostic factors, mRNA vaccination was associated with a statistically greater humoral response relative to the AstraZeneca ChAdOx1-S. Whilst consistent with the emerging literature [5], the clinical significance of this remains unclear, given failure of seroconversion following both vaccine types and observed mortality in 2 individuals with CID despite two mRNA vaccinations. Further studies are required to determine the nature and durability of both cellular and humoral immune responses following heterologous booster vaccine regimens. By systematically profiling a range of immunoglobulin products manufactured over the past 2 years, we reveal low but increasing levels of anti-SARS-CoV-2 IgG. Given the severe consequences of vaccine failure in individuals observed in our cohort, our findings support increased access to precision therapies such as monoclonal anti-SARS-CoV-2 antibodies and antiviral therapies [3, 4]. Continued serosurveillance may help identify individuals with waning immunity or partial responses who may benefit from booster vaccinations, whilst prioritising vaccine non-responders to receive pre-exposure prophylaxis and post-exposure interventions.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We gratefully acknowledge the input from all patients and families in supporting this service evaluation.
Additional contributing authors:
The Immunodeficiency Centre for Wales and Cardiff University COVID-19 consortium:
Ms Kathryn Bramhall1, Ms Leanne Grant1, Ms Frances McGuire, Mr Anthony Matthews, Dr Rachel Bradley, Dr Sonali Wijetilleka, Ms Alison Pritchard, Mr Colin R Price1, Dr Daniel Farewell3, Dr Richard Cousins1 and Dr Tariq El-Shanawany1.
1Immunodeficiency Centre for Wales, University Hospital of Wales, Heath Park, Cardiff, UK
2Institute of Infection & Immunity, Henry Wellcome Building, School of Medicine, Cardiff University, Heath Park, Cardiff, UK
3Division of Population Medicine, School of Medicine, Cardiff University, Heath Park, Cardiff, UK
Author Contribution
MJP and SJ conceived the study. KE, FMG, EMC, RB, and MJP conducted the postal survey and electronic notes review. EC and EMC collected IgRT samples and collated dates of manufacture. MJP performed anti-SARS-CoV-2 spike IgG testing on IgRT samples supervised by KB and LG. SW, TES, RC, AP, EC, CRP EMC, and SJ supported patient care and clinical testing for anti-SARS-CoV-2 spike IgG response. KE and MJP collated results. MJP conducted statistical and graphical analyses with supervision from DF. MJP wrote the first manuscript draft. All authors provided critical input and have approved the final version.
Funding
MJP is supported by the Welsh Clinical Academic Training (WCAT) programme and a Career Development Award from the Association of Clinical Pathologists and is a participant in the NIH Graduate Partnership Program.
Declarations
Ethical Approval
This work was performed as a service evaluation. In line with the Health Research Authority (HRA) decision tool, this does not constitute research and requirement for formal ethical application was waived.
Conflict of Interest
SJ has received support for conferences, speaker, advisory boards, trials, data and safety monitoring boards, and projects with CSL Behring, Takeda, Swedish Orphan Biovitrum, Biotest, Binding Site, Grifols, BPL, Octapharma, LFB, Pharming, GSK, Weatherden, Zarodex, Sanofi, and UCB Pharma. TE has received support for education, speaker, advisory boards, and/or research from Allergy Therapeutics, CSL Behring, Mylan, Novartis, Pharming, Takeda, and Thermo Fisher. None of these conflicts relates to the current work. The remaining authors have no potential relevant conflicts of interests to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Stephen Jolles, Email: jollessr@cardiff.ac.uk.
On behalf of the Immunodeficiency Centre for Wales and Division of Population Medicine:
Kathryn Bramhall, Leanne Grant, Frances McGuire, Anthony Matthews, Rachel Bradley, Sonali Wijetilleka, Alison Pritchard, Colin R. Price, Daniel Farewell, Richard Cousins, and Tariq El-Shanawany
References
- 1.Salinas AF, Mortari EP, Terreri S, Quintarelli C, Pulvirenti F, Di Cecca S, et al. SARS-CoV-2 vaccine induced atypical immune responses in antibody defects: everybody does their best. J Clin Immunol. 2021;41(8):1709–1722. 10.1007/s10875-021-01133-0. [DOI] [PMC free article] [PubMed]
- 2.Delmonte OM, Bergerson JRE, Burbelo PD, Durkee-Shock JR, Dobbs K, Bosticardo M, et al. Antibody responses to the SARS-CoV-2 vaccine in individuals with various inborn errors of immunity. J Allergy Clin Immunol. 2021;148(5):1192–1197. doi: 10.1016/j.jaci.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horby P, Lim WS, Emberson J, Mafham M, Bell J, Linsell L, et al. Effect of dexamethasone in hospitalized patients with COVID-19: preliminary report. medRxiv. 2020;2020.06.22.20137273.
- 4.Ponsford MJ, Shillitoe BMJ, Humphreys IR, Gennery AR, Jolles S. COVID-19 and X-linked agammaglobulinemia (XLA) – insights from a monogenic antibody deficiency. Curr Opin Allergy Clin Immunol. 2021;21(6):525–534. doi: 10.1097/ACI.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 5.Shields AM, Faustini S, Hill H. SARS-CoV-2 vaccine responses in individuals with antibody deficiency: findings from the COV-AD study. Pre-print uploaded to Research Square. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.