Abstract
Background
Restricting the advertisement of products with high fat, salt, and sugar (HFSS) content has been recommended as a policy tool to improve diet and tackle obesity, but the impact on HFSS purchasing is unknown. This study aimed to evaluate the impact of HFSS advertising restrictions, implemented across the London (UK) transport network in February 2019, on HFSS purchases.
Methods and findings
Over 5 million take-home food and drink purchases were recorded by 1,970 households (London [intervention], n = 977; North of England [control], n = 993) randomly selected from the Kantar Fast Moving Consumer Goods panel. The intervention and control samples were similar in household characteristics but had small differences in main food shopper sex, socioeconomic position, and body mass index. Using a controlled interrupted time series design, we estimated average weekly household purchases of energy and nutrients from HFSS products in the post-intervention period (44 weeks) compared to a counterfactual constructed from the control and pre-intervention (36 weeks) series. Energy purchased from HFSS products was 6.7% (1,001.0 kcal, 95% CI 456.0 to 1,546.0) lower among intervention households compared to the counterfactual. Relative reductions in purchases of fat (57.9 g, 95% CI 22.1 to 93.7), saturated fat (26.4 g, 95% CI 12.4 to 40.4), and sugar (80.7 g, 95% CI 41.4 to 120.1) from HFSS products were also observed. Energy from chocolate and confectionery purchases was 19.4% (317.9 kcal, 95% CI 200.0 to 435.8) lower among intervention households than for the counterfactual, with corresponding relative reductions in fat (13.1 g, 95% CI 7.5 to 18.8), saturated fat (8.7 g, 95% CI 5.7 to 11.7), sugar (41.4 g, 95% CI 27.4 to 55.4), and salt (0.2 g, 95% CI 0.1 to 0.2) purchased from chocolate and confectionery. Relative reductions are in the context of secular increases in HFSS purchases in both the intervention and control areas, so the policy was associated with attenuated growth of HFSS purchases rather than absolute reduction in HFSS purchases. Study limitations include the lack of out-of-home purchases in our analyses and not being able to assess the sustainability of observed changes beyond 44 weeks.
Conclusions
This study finds an association between the implementation of restrictions on outdoor HFSS advertising and relative reductions in energy, sugar, and fat purchased from HFSS products. These findings provide support for policies that restrict HFSS advertising as a tool to reduce purchases of HFSS products.
Amy Yau and co-workers study food and drink purchases after the introduction of advertising restrictions in London, UK.
Author summary
Why was this study done?
Many governments and local authorities are considering advertising restrictions to reduce consumption of high fat, salt, and sugar (HFSS) products as part of obesity prevention strategies.
Evidence of the effectiveness of such policies in reducing purchases of HFSS products is limited, especially outside of broadcast media.
The introduction of an outdoor advertising policy across a large transport network provided an opportunity to evaluate a natural experiment assessing whether implementation of such a policy is associated with changes in household food and drink purchases.
What did the researchers do and find?
We compared average weekly household purchases of HFSS products by households in the intervention area (n = 977) to an estimation of what would have happened without the policy—a counterfactual scenario estimated by extrapolating the pre-implementation trend and accounting for the post-implementation changes seen in households in the control area (n = 993).
The average weekly household purchase of energy from HFSS products was 6.7% (1,001.0 kcal) lower in intervention households after the introduction of the policy compared to the counterfactual, and 19.4% (317.9 kcal) lower for energy from chocolate and confectionery.
Average weekly household purchases of nutrients from HFSS products were lower after intervention implementation in intervention households relative to the counterfactual: fat, by 57.9 g; saturated fat, by 26.4 g; and sugar, by 80.7 g.
What do these findings mean?
Our findings provide support for advertising restrictions as a tool to reduce purchases of energy, sugar, and fat from HFSS products.
This study adds to the evidence that can be used by governments and local authorities when developing obesity prevention strategies.
Introduction
The advertisement of foods and drinks with high fat, salt, and sugar (HFSS) content is known to be associated with poor diet and obesity, particularly in children [1–4]. There is a high prevalence of exposure to HFSS food and drink advertising across a variety of media, especially among disadvantaged groups and in more deprived areas [5–9]. In children, exposure to advertising of HFSS foods and drinks has been associated with preferences for HFSS products, requests for purchases, and higher consumption of HFSS products [1,2,4]. Associations in adults are not as well-studied, and findings are inconsistent. However, some studies have found exposure to advertising of HFSS foods and drinks to be positively associated with purchasing and consumption of HFSS products and body mass index (BMI) [10–14]. Evidence suggests that advertisement of HFSS foods and drinks can influence food behaviours by changing dietary norms and shifting population-level food and drink preferences [15].
Policies that restrict the advertising of HFSS products have been promoted as potentially effective tools to reduce the purchase and consumption of HFSS products, with the aim of improving diet, reducing obesity and diet-related diseases, and tackling health inequalities [16,17]. Policies on HFSS advertising have been implemented in many countries, but most policies have been limited in scope, with a focus on broadcast advertising and a reliance on voluntary agreements by the food and advertising industries [18,19]. These voluntary commitments have been limited in effectiveness [19–21]. In 2007, the United Kingdom (UK) implemented statutory regulations to limit children’s exposure to HFSS food and drink advertising through television [22]. Ofcom, the UK’s communications regulator, estimated that children saw 34% fewer HFSS advertisements as a result [23]. However, as the regulations only applied to programmes targeting children, evidence suggests that there was displacement of advertising to television programmes aimed at a mixed audience. Independent research estimated that the policy had no effect on children’s overall exposure to HFSS advertising and that it increased exposure for the population as a whole [24]. Studies of advertising restrictions from other countries and regions provide evidence of statutory regulations reducing the volume of, or exposure to, HFSS advertising [21,25,26] and reducing purchases of HFSS products [19,27]. However, limited evidence exists on the effectiveness of policies that restrict advertising of HFSS products outside of broadcast media [18,20,28]. One study evaluating restrictions on fast food advertising across multiple print and electronic media in Quebec, Canada, found a 13% decrease in likelihood of purchasing following the introduction of the policy [27].
In November 2018, restrictions on the outdoor advertising of HFSS foods and drinks across the Transport for London (TfL) network were announced by the Mayor of London, UK (Box 1) [29,30]. The TfL advertising estate includes the London Underground (rapid transit) network, the TfL Rail network, transport vehicles run by TfL (including some buses, trains, and taxis), and outdoor spaces owned by TfL (e.g., bus stops and land outside train stations) [29]. The restrictions were fully implemented on 25 February 2019. A full description of the policy guidance is available from the TfL website [31]. Though these restrictions formed part of a childhood obesity strategy, they may impact food behaviours (such as purchasing and consumption) across the whole population. We hypothesised that this policy may contribute to improvements in diet by reducing energy and nutrients purchased from HFSS products. In the absence of longitudinal dietary data, we used household purchase data to evaluate the impact of the intervention. This study aimed to estimate the changes in household purchases of energy and nutrients from HFSS products associated with the TfL advertising policy. Research investigating the implementation process [32] and the media representation of opposition to the policy [33] has been published.
Box 1. HFSS advertising restriction policy across the TfL estate
Advertising and TfL
Outdoor, or out-of-home, advertising is advertising seen in public spaces (e.g., billboards, on buses), often on the go and including digital and interactive displays [69].
Outdoor advertising is thought to reach 98% of the UK population at least once a week and is particularly effective at reaching young, urban, affluent consumers [69].
The TfL network is the largest transport network in Western Europe.
TfL has one of the largest outdoor advertising estates in the UK, representing £152.1 million in advertising spending in 2017/2018 [29].
The TfL estate accounts for 40% of London’s outdoor advertising spending and 20% of outdoor advertising spending across the UK [29].
TfL advertising policy
Food and drink products are subject to advertising restrictions if they are classified as HFSS by the Nutrient Profiling Model (NPM) developed by the UK Food Standards Agency [37].
Both direct marketing of HFSS products and incidental images of HFSS products in advertisements are prohibited [31].
Companies can apply to advertise a product through an exceptions process if they can demonstrate that the product is not consumed by children and does not contribute to childhood obesity [31].
Advertisements for some food categories (e.g., chocolate and confectionery) and for brands that do not produce non-HFSS products as part of their range will be completely removed from the TfL network.
Brands with more diverse product ranges (e.g., drinks companies) may have low or zero calorie alternatives that allow continued brand advertising.
Methods
Using a controlled interrupted time series (CITS) analysis design, we estimated mean weekly household purchases of energy and nutrients from HFSS products, and packs of HFSS products, in London in the post-intervention period, compared with a counterfactual scenario where the intervention had not occurred. We examined purchases of all products classified as HFSS and within 5 key HFSS categories: (1) chocolate and confectionery, (2) puddings and biscuits, (3) sugary drinks, (4) sugary cereals, and (5) savoury snacks. Assignment to these categories was informed by previous work and is detailed in S1 Table [34]. The protocol was registered (ISRCTN 19928803) (S1 Text), and the study is reported in accordance with STROBE guidelines (for checklist, see S2 Text).
Data
Households
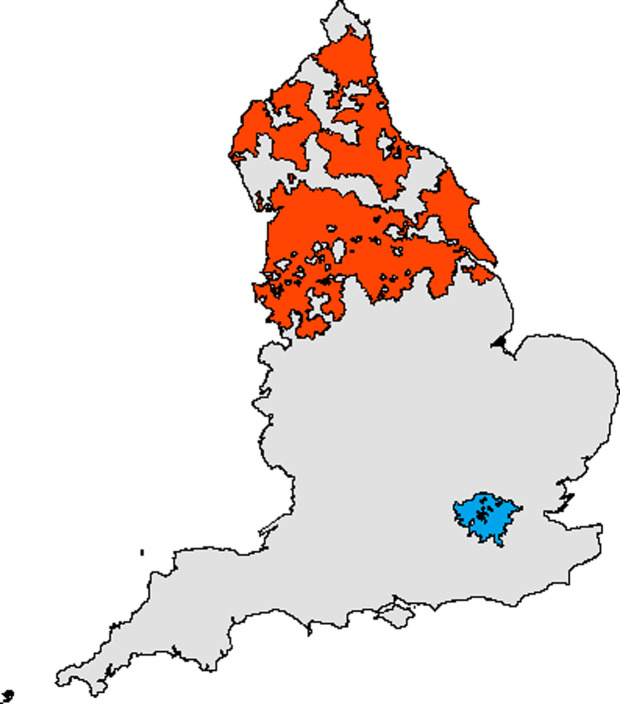
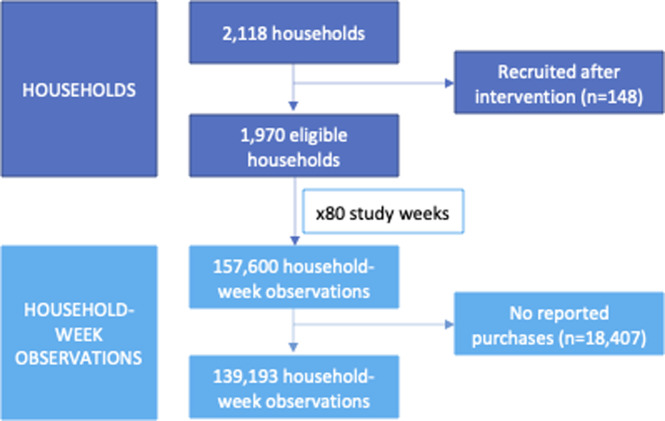
Take-home grocery food and drink purchase data were available from households in the Kantar Fast Moving Consumer Goods (FMCG) panel from 18 June 2018 to 29 December 2019 (80 weeks), with 36 pre-intervention weeks and 44 post-intervention weeks. Kantar (a commercial consumer data company) recruits households to a live panel via email or post using quota sampling, and maintains a nationally representative sample of approximately 32,000 households annually. For this study, households (n = 2,118) were randomly sampled for inclusion from London (intervention group) and the North of England (control group), based on postcode of residence. The North of England sample consisted of households in the North West, North East, and Yorkshire and the Humber regions (Fig 1). The North of England was chosen as a location-based control group due to its distance from London, reducing the likelihood of spillover effects (e.g., contamination of the control group through regular commuting to London from neighbouring counties) [35]. The control group enabled adjustment for the confounding effects that were common to both areas, including seasonal fluctuations and underlying trends in HFSS purchasing. Households recruited to the panel after the intervention was introduced (25 February 2019) were excluded from analyses (n = 148) (Fig 2). Our analytical sample (n = 1,970) included 977 intervention households and 993 control households.
Fig 1. Map of England showing the intervention (London) and control (North of England) areas.
Blue = London; red = North of England. This figure was created using a base map downloaded from https://osdatahub.os.uk/downloads/open/BoundaryLine.
Fig 2. Eligibility and inclusion of households and household-week observations.
Food and drink purchases
Participating households record all grocery (food and drink) items purchased and brought into the home, using a handheld barcode scanner [34]. Non-barcoded products, such as loose fruits and vegetables, are recorded using bespoke barcodes. In this study, 5,089,988 packs of 95,413 unique food and drink products were purchased. A pack is the individual item scanned by the participating household, which could be a single serving or a multipack, and therefore does not reflect volume purchased. For example, 23,564 (9.0%) chocolate and confectionery purchases were boxes of chocolates and 90,694 (34.7%) were multipacks, with a mean energy of 786.5 kcal per pack.
Data were aggregated to weekly purchases per household (n = 157,600). Most households did not report in all 80 study weeks (mean 70.7 [SD 8.7]; median 73 [IQR 66–78]). The reasons for non-reporting are unknown, but could include households habitually purchasing groceries less than weekly, going on holiday, or forgetting to report. The proportion of households with no reported purchases in a given week fluctuated, but with no clear pattern, so we assumed missingness to be random. Household-week observations where households did not report any food and drink purchases were dropped (n = 18,407 [11.7%]), resulting in 139,193 household-week observations for each outcome.
Nutrients
Nutritional data are collected by Kantar either through direct measurement in outlets twice a year or use of product images provided by Brandbank. Regular data collection helps to capture product reformulation. Where nutritional data cannot be collected directly, either nutritional values are copied across from similar products or an average value for the category or product type is calculated. The proportion of imputed values in our dataset is unknown. However, a previous study reported imputed values for between 11.0% (energy) and 19.6% (fibre) of the nutrient data from Kantar [34].
Household and main food shopper characteristics
Sociodemographic data from the panellists are collected annually and include characteristics of the main food shopper: sex (male and female), age (years), socioeconomic position, household size, and weight status. Socioeconomic position is classified according to the National Readership Survey (NRS) occupational social grade classification (A, B, C1, C2, D, E) [36]. We categorised NRS social grade into 3 socioeconomic groups: high (AB), middle (C1C2), and low (DE). Data on household size included number of children <16 years and number of adults. The household main food shopper reports their weight and height (available for n = 1,591 [80.8%]), from which BMI (weight [kg]/height2 [m2]) is calculated. We classified main food shoppers as living with overweight or obesity (BMI ≥ 25 kg/m2) or not (BMI < 25 kg/m2). The main food shoppers from 1,296 (65.8%) households completed an additional survey in February 2019 in which they were asked about typical frequency of public transport use per week [8]. Households were then categorised as typically using public transport at least once a week (yes or no) for use in sensitivity analyses.
Outcomes
We categorised products as HFSS (yes or no) according to the NPM, which was used to determine whether products could be advertised on the TfL estate [31,37]. An NPM score was calculated using points for energy, sugar, sodium, and saturated fat minus points for protein, fibre, and fruit and vegetable content. Information on the energy, sugar, sodium, saturated fat, protein, and fibre content of each purchase was provided by Kantar. Kantar also categorised product markets (e.g., breakfast cereals, chocolate) as high, mixed, or low in fruit, nuts, and vegetables, which we used to score products with 5 (>80%), 1 (>40% and ≤80%) or 0 (≤40%) for fruit and vegetable content. The higher the final score, the less healthy the product. We applied the suggested cut-offs and considered food products that scored ≥4 points and drink products that scored ≥1 point as HFSS [35]. Our primary outcomes were weekly household purchases of energy (kilocalories), fat (grams), saturated fat (grams), sugar (grams), and salt (grams) from HFSS products. We also examined the number of packs of HFSS products purchased. We were unable to assess volume purchased as this information was not available for all products.
Statistical analysis
We used a CITS to estimate changes in the intervention group following the intervention compared to the counterfactual. We constructed the counterfactual by extrapolating the pre-intervention trend of the intervention group (based on 36 weeks) and incorporating the post-intervention changes of the control group (based on 44 weeks).
Our dataset contained a percentage of zero values for all outcomes because households did not purchase HFSS products every week. This percentage ranged from 2.8% for total HFSS products to 86.1% for sugary cereals. To account for this zero-inflation, we used a 2-part model for mixed discrete–continuous outcomes [38]. This type of model has been used previously to analyse positively skewed behavioural outcomes with a large proportion of zeros [39]. The 2-part model estimated the probability of purchasing a product (part 1—logit model) and, if a product was purchased, how much was purchased (part 2—generalised linear model). A gamma distribution was used for the analysis of energy and nutrients, whilst a negative binomial distribution was used for the analysis of packs. We used cluster-robust standard errors to account for clustering of outcomes by household in all models.
For each outcome, we used a single CITS model containing intervention and control data, with an indicator variable (‘London’, where intervention group = 1 and control group = 0). Our CITS models also included the following variables: time (time elapsed since the start of the study, expressed as week 1–80), a dummy variable (‘intervention’) indicating the pre-intervention period (coded 0) and the post-intervention period (coded 1), and interaction terms that accounted for the trend in the intervention group (time × London), the post-intervention period in the intervention group (intervention × London), the post-intervention trend in the control group (time × intervention), and the post-intervention trend in intervention group (time × intervention × London). All analyses were adjusted for household characteristics (number of adults and number of children) and sociodemographic characteristics of the main food shopper (sex, age, and socioeconomic position). We also included controls for season and festivals associated with HFSS purchasing (an indicator variable for weeks including Valentine’s Day, Easter, Halloween, and Christmas).
From these 2-part models, we estimated mean weekly household energy purchased from HFSS products and used pairwise comparisons to test the difference in marginal means in the intervention group compared to the counterfactual in the post-intervention period. This outcome combined the change in both level and slope over the post-intervention period. The same comparison was used to examine differences in fat, saturated fat, sugar, and salt purchased through HFSS products, and packs of HFSS products purchased. Linear comparisons of parameters were used to estimate the percentage change in average marginal effects compared to the counterfactual. We also compared the changes in the first (25 February 2019 to 3 March 2019) and last (23 December 2019 to 29 December 2019) post-intervention weeks using linear comparisons of parameters, as an indication of the sustainability of any detected changes.
We used interaction terms to explore whether changes in energy purchased differed according to (1) socioeconomic position, (2) whether there were children in the household, and (3) whether the main food shopper was living with overweight or obesity (n = 1,591). However, these analyses were limited by sample size, missing values in the case of BMI, and the uneven distribution of households within categories. Results from sub-group analyses are therefore descriptive and hypothesis generating.
Our results are reported relative to the counterfactual. We present marginalised results in the main paper. Coefficients from the underlying models are available in S2–S7 Tables. All analyses were conducted in Stata SE 16.
Sensitivity analyses
Analysis of a sub-sample of ‘regular reporters’ (n = 1,126)
To test the influence of non-reporting on the results, we undertook analyses using regular reporters only. We defined regular reporters as households that reported purchases of any food or drink in more than 72 (90.0%) of the study weeks.
Methodological triangulation
Whilst the 2-part model enabled us to deal with zero-inflation, it does not fully account for the longitudinal panel nature of the data. To test the consistency of our findings across statistical models, we also fitted a mixed-effects negative binomial model. This model is appropriate for analysing skewed panel data but does not account for zero-inflation.
Temporal falsification
To test whether the observed changes were specific to the time the intervention occurred, we moved the ‘intervention’ week. If the changes were robust to the date of the intervention, we would expect to observe no changes at other times. We moved the ‘intervention’ from the week commencing 25 February 2019 to the week commencing 24 September 2018. This false intervention week was chosen because it was outside of any festival period (Valentine’s Day, Easter, Christmas, and Halloween) and prior to the intervention.
Changes in purchases by transport use
We undertook an analysis of the sub-group of the main analytic sample (n = 1,296) that reported their typical public transport use. This allowed us to examine whether regular TfL users (i.e., those typically using public transport at least once a week in London)—who likely had higher exposure to advertising on the TfL network—had greater changes in their HFSS purchases, thus increasing the likelihood that any observed changes were the result of the intervention.
Restricting the time series
We removed the last 2 weeks of data (16 to 29 December 2019), which represented a peak in HFSS purchases associated with Christmas, to see if this affected our overall findings.
Changes in non-HFSS purchases
We examined changes in mean weekly household purchases of non-HFSS products to see if there were any spillover effects on products not affected by the TfL policy.
Ethics
Ethical approval for this study was granted by the London School of Hygiene & Tropical Medicine Ethics Committee (ref no: 16297/RR/11721). Written informed consent was obtained from all panel participants.
Changes to protocol
Our original protocol specified a follow-up period of 12 months post-intervention. Follow-up was conservatively reduced to 10 months to avoid contamination of outcomes as a result of the early stages of the COVID-19 pandemic (reductions in the use of public transport and the early stages of panic buying). We conducted sensitivity analyses (described above) that were not pre-specified in our protocol, to assess the robustness of our results [40].
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting, or dissemination plans of our research.
Results
Study population
Overall, 1,970 households were included in the analysis, with 977 households in London (intervention) and 993 households in the North of England (control) (Table 1). The intervention and control samples were similar in household characteristics but had small differences in main food shopper characteristics: sex (71.6% versus 74.3% female), socioeconomic position (27.5% versus 19.6% high socioeconomic position), and BMI (44.9% versus 53.1% overweight/obese). Intervention and control households also differed in transport use (67.8% versus 38.3% typically used public transport, of those who responded to the survey question). These differences are in line with differences seen between these regions [41–43]. We previously found that 45.5% of London participants and 28.8% of North of England participants reported seeing HFSS advertising on a transport network in the last 7 days, in a survey conducted in February 2019, prior to the introduction of the TfL advertising restrictions [8].
Table 1. Descriptive characteristics of the overall, intervention, and control samples.
| Characteristic | Sub-category | Total (N = 1,970) |
Intervention (N = 977) |
Control (N = 993) |
|---|---|---|---|---|
| Household characteristics | ||||
| Number of adults in the household, mean (SD) | 2.1 (0.9) | 2.1 (1.0) | 2.1 (0.8) | |
| Number of children in the household, mean (SD) | 0.5 (0.9) | 0.5 (0.9) | 0.5 (0.9) | |
| Children in the household, n (%) | Yes | 575 (29.2) | 279 (28.6) | 296 (29.8) |
| No | 1,395 (70.8) | 698 (71.4) | 697 (70.2) | |
| Main food shopper characteristics | ||||
| Sex, n (%) | Male | 533 (27.1) | 278 (28.5) | 255 (25.7) |
| Female | 1,437 (72.9) | 699 (71.6) | 738 (74.3) | |
| Age (years), mean (SD) | 52.0 (13.8) | 52.1 (13.0) | 52.0 (14.6) | |
| Socioeconomic position, n (%) | High | 464 (23.6) | 269 (27.5) | 195 (19.6) |
| Middle | 1,164 (59.1) | 560 (57.3) | 604 (60.8) | |
| Low | 342 (17.4) | 148 (15.2) | 194 (19.5) | |
| Body mass index, n (%) | Not overweight | 625 (31.7) | 337 (34.5) | 288 (29.0) |
| Overweight/obese | 966 (49.0) | 439 (44.9) | 527 (53.1) | |
| Missing | 379 (19.2) | 201 (20.6) | 178 (17.9) | |
| Public transport use, n (%) | No | 633 (32.1) | 182 (18.6) | 451 (45.4) |
| Yes | 663 (33.7) | 383 (39.2) | 280 (28.2) | |
| Missing | 674 (34.2) | 412 (42.2) | 262 (26.4) | |
Food and drink purchases
In total, 1,952,083 (38.4%) packs of food and drink purchased over the study period were classified as HFSS. Mean weekly household energy purchased from HFSS products was higher among control households (15,776.6 kcal pre-intervention and 15,697.3 kcal post-intervention) than among intervention households (14,199.7 kcal pre-intervention and 13,990.8 kcal post-intervention) overall, and for each HFSS category (Table 2). The CITS design assumes that the difference between the intervention group and control group is constant over time in the absence of the intervention [44]. We tested this assumption using the significance of the London × time interaction term in our models. The pre-intervention trend in purchasing followed a similar pattern in both regions for all HFSS categories, except chocolate and confectionery (S1 Fig; S8 Table). For chocolate and confectionery, there was a parallel trend in the later part of the pre-intervention period (from 19 November 2018), but some deviation in the earlier weeks (S9 Table).
Table 2. Unadjusted weekly household mean (SD) energy (kilocalories) purchased from high fat, salt, and sugar (HFSS) products and non-HFSS products pre- and post-intervention in the intervention group and control group.
| Category | Pre-intervention weekly household mean | Post-intervention weekly household mean | ||||
|---|---|---|---|---|---|---|
| Total (N = 1,970) | Intervention (N = 977) | Control (N = 993) | Total (N = 1,970) | Intervention (N = 977) | Control (N = 993) | |
| Total food & drink | 27,999.3 (20,661.4) | 26,818.5 (21,500.1) | 29,133.3 (19.756.6) | 27,763.5 (20,215.0) | 26,507.7 (20,872.2) | 28,989.7 (19.474.4) |
| Total HFSS products | 15,004.1 (13,234.2) | 14,199.7 (13,694.7) | 15,776.6 (12,728.8) | 14,854.3 (12,959.5) | 13,990.8 (13,228.2) | 15,697.3 (12,635.1) |
| Chocolate & confectionery | 1,445.4 (2,549.5) | 1,266.9 (2,439.6) | 1,616.8 (2,639.4) | 1,504.5 (2,542.7) | 1,308.9 (2,406.3) | 1,695.5 (2,655.4) |
| Puddings & biscuits | 3,071.1 (3,892.7) | 2,827.2 (3,754.0) | 3,305.3 (4,007.6) | 3,071.5 (3,814.6) | 2,795.9 (3,693.4) | 3,340.6 (3,910.7) |
| Sugary drinks | 248.2 (682.1) | 232.0 (668.0) | 263.9 (695.1) | 221.7 (637.3) | 211.2 (625.3) | 232.0 (648.7) |
| Sugary cereals | 467.8 (1,426.5) | 461.7 (1,496.0) | 473.7 (1,356.4) | 418.8 (1,323.1) | 405.6 (1,346.9) | 431.7 (1,299.4) |
| Savoury snacks | 1,075.0 (1,693.0) | 1,046.7 (1,698.8) | 1,102.1 (1,686.9) | 1,085.3 (1,702.0) | 1,073.8 (1,732.2) | 1,096.4 (1,672.0) |
| Non-HFSS products | 12,995.2 (9,860.4) | 12,618.9 (10,442.5) | 13,356.6 (9,252.8) | 12,909.3 (9,672.6) | 12,516.9 (10,195.1) | 13,292.4 (9,117.6) |
Changes in total HFSS purchases
The implementation of HFSS advertising restrictions was associated with a relative reduction in average weekly household energy purchased from HFSS products of 1,001.0 kcal (95% CI 456.0 to 1,546.0), or 6.7% (95% CI 3.2% to 10.1%), in the intervention group compared to the counterfactual (Fig 3; Table 3). Relative decreases in weekly household purchases of fat (57.9 g; 95% CI 22.1 to 93.7), saturated fat (26.4 g; 95% CI 12.4 to 40.4), and sugar (80.7 g; 95% CI 41.4 to 120.1) from HFSS products, and packs of HFSS products purchased (0.7 packs; 95% CI 0.2 to 1.2), were also observed. The observed relative change in weekly household purchases of salt was not significant (−2.2 g, 95% CI −9.8 to 5.4). The relative reduction in energy purchased detected in the final post-intervention week was larger than that detected in the first week post-intervention (see S10 Table).
Fig 3. Adjusted weekly household mean energy purchased from high fat, salt, and sugar (HFSS) products in London (intervention), the North of England (control), and the counterfactual.
Vertical line = date of intervention implementation. The counterfactual was estimated by extrapolating the pre-intervention trend in London and incorporating the post-intervention changes in the North of England. Weekly household mean energy purchased from HFSS products was estimated from a controlled interrupted time series 2-part model: part 1 (logit) and part 2 (generalised linear model) with gamma distribution. Models were adjusted for festivals, season, number of adults in household, number of children in household, and sex, age, and socioeconomic position of main food shopper. Cluster-robust standard errors were used. Household-week observations where households did not report any food and drink purchases that week were dropped. Data period = 18 June 2018 to 29 December 2019. Spikes represent festival weeks included in the models.
Table 3. Changes and percentage changes in weekly household mean (95% CI) energy and nutrients purchased from high fat, salt, and sugar (HFSS) products and packs of HFSS products purchased, in London (intervention group) compared to the counterfactual, 18 June 2018 to 29 December 2019 (n = 1,970).
| Outcome | Measure | Total HFSS products | Chocolate & confectionery | Puddings & biscuits | Sugary drinks | Sugary cereals | Savoury snacks |
|---|---|---|---|---|---|---|---|
| Energy | Kilocalories | −1,001.0 (−1,546.0 to −456.0) | −317.9 (−435.8 to −200.0) | −198.3 (−389.7 to −6.9) | 19.6 (−14.0 to 53.3) | 4.1 (−88.7 to 96.8) | 61.1 (−20.3 to 142.5) |
| Percent | −6.7 (−10.1 to −3.2) | −19.4 (−25.4 to −13.4) | −6.6 (−12.6 to −0.6) | 10.1 (−8.8 to 29.1) | 1.0 (−22.5 to 24.5) | 6.0 (−2.4 to 14.5) | |
| Fat | Grams | −57.9 (−93.7 to −22.1) | −13.1 (−18.8 to −7.5) | −8.1 (−16.5 to 0.4) | −0.2 (−1.0 to 0.7) | −0.5 (−3.3 to 2.3) | 3.9 (−0.9 to 8.7) |
| Percent | −6.5 (−10.4 to −2.7) | −18.2 (−24.9 to −11.6) | −6.2 (−12.4 to −0.1) | −6.4 (−36.4 to 23.6) | 5.8 (−35.5 to 23.9) | 6.8 (−2.2 to 15.7) | |
| Saturated fat | Grams | −26.4 (−40.4 to −12.4) | −8.7 (−11.7 to −5.7) | −2.9 (−7.4 to 1.6) | −0.1 (−0.8 to 0.6) | −0.3 (−1.1 to 0.5) | 0.8 (−0.1 to 1.7) |
| Percent | −7.3 (−11.0 to −3.7) | −22.8 (−29.2 to −16.4) | −4.5 (−11.2 to 2.2) | −5.4 (−38.4 to 27.6) | −10.9 (−38.5 to 16.8) | 9.2 (−2.0 to 20.4) | |
| Sugar | Grams | −80.7 (−120.1 to −41.4) | −41.4 (−55.4 to −27.4) | −7.8 (−23.7 to 8.2) | 4.9 (−0.9 to 10.7) | 0.7 (−5.0 to 6.5) | 0.8 (−0.4 to 1.9) |
| Percent | −10.5 (−15.2 to −5.9) | −21.8 (−27.8 to −15.7) | −3.3 (−10.0 to 3.3) | 13.9 (−4.6 to 32.4) | 3.0 (−21.7 to 27.7) | 8.4 (5.0 to 21.8) | |
| Salt | Grams | −2.2 (−9.8 to 5.4) | −0.2 (−0.2 to −0.1) | −0.4 (−0.8 to −0.1) | −0.0 (−0.1 to 0.1) | 0.0 (−0.1 to 0.2) | 0.4 (0.1 to 0.7) |
| Percent | −3.6 (−15.5 to 8.3) | −17.4 (−25.5 to −9.2) | −12.0 (−19.6 to −4.4) | −11.6 (−41.5 to 18.4) | 9.0 (−17.1 to 35.2) | 12.5 (2.4 to 22.6) | |
| Packs | Number | −0.7 (−1.2 to −0.2) | −0.4 (−0.6 to −0.3) | −0.1 (−0.3 to 0.1) | 0.0 (−0.1 to 0.1) | −0.0 (−0.1 to 0.0) | 0.1 (0.0 to 0.2) |
| Percent | −4.9 (−8.4 to −1.4) | −21.4 (−28.0 to −14.8) | −1.9 (−8.7 to 4.8) | 4.4 (−11.2 to 20.1) | −7.4 (−27.9 to 13.2) | 9.0 (−0.0 to 17.9) |
Bold indicates significant at the 95% confidence level. Weekly household mean purchases were estimated from a controlled interrupted time series 2-part model: part 1 (logit) and part 2 (generalised linear model), with gamma distribution for energy and nutrients and negative binomial distribution for packs. Models were adjusted for festivals, season, number of adults in household, number of children in household, and sex, age, and socioeconomic position of main food shopper. Cluster-robust standard errors were used. Household-week observations where households did not report any food and drink purchases that week were dropped. Data period = 18 June 2018 to 29 December 2019.
Changes by HFSS category
Chocolate and confectionery
Using the whole study period, average weekly household purchases of energy from chocolate and confectionery fell by 317.9 kcal (95% CI 200.0 to 435.8) in the intervention group relative to the counterfactual, equivalent to an observed decrease of 19.4% (95% CI 13.4% to 25.4%). Relative reductions in weekly household purchases of fat (13.1 g; 95% CI 7.5 to 18.8), saturated fat (8.7 g; 95% CI 5.7 to 11.7), sugar (41.4 g; 95% CI 27.4 to 55.4), and salt (0.2 g; 95% CI 0.1 to 0.2) were also detected in the post-intervention period. A relative reduction in the number of packs of HFSS products purchased (0.4; 95% CI 0.3 to 0.6) was also observed. We re-ran this model using a shorter pre-intervention period to satisfy the parallel trends assumption and observed similar changes (S11 Table).
Puddings and biscuits
Relative to the counterfactual, energy purchased from puddings and biscuits was lower in the intervention group in the post-intervention period (198.3 kcal; 95% CI 6.9 to 389.7). A relative reduction in purchased salt was also observed (0.4 g; 95% CI 0.1 to 0.8). However, relative changes in the amount of fat (−8.1 g; 95% CI −16.5 to 0.4), saturated fat (−2.9 g; 95% CI −7.4 to 1.6), and sugar (−7.8; 95% CI −23.7 to 8.2) purchased through puddings and biscuits, and the number of packs of puddings and biscuits purchased (−0.1 packs, 95% CI −0.3 to 0.1), were non-significant.
Sugary drinks and sugary cereals
Small, non-significant relative increases were observed for energy purchased from sugary drinks (19.6 kcal; 95% CI −14.0 to 53.3) and sugary cereals (4.1 kcal; 95% CI −88.7 to 96.8) following the intervention. There were also no significant differences detected for nutrients and packs purchased.
Savoury snacks
There was a non-significant relative increase in energy purchased from savoury snacks (61.1 kcal; 95% CI −20.3 to 142.5) following the intervention. The average weekly number of packs purchased increased marginally (0.1 packs; 95% CI 0.0 to 0.2) relative to the counterfactual. This was accompanied by a small relative increase in salt purchased through savoury snacks (0.4 g; 95% CI 0.1 to 0.7). Relative increases for other nutrients were not significant.
Changes by household and sociodemographic characteristics
There was some indication that observed differences varied by population sub-group, but these did not reach statistical significance. Descriptively, for example, we observed the largest relative reduction in purchased energy in the middle socioeconomic group (S12 Table). The relative reduction was larger in households with children for chocolate and confectionery purchases, but larger in households with no children for total HFSS and puddings and biscuits (S13 Table). Reductions were larger for households with a main food shopper who was living with overweight or obesity for total HFSS, chocolate and confectionery, and puddings and biscuits (S14 Table). However, these results should be interpreted with caution and can be considered hypothesis generating. Studies with greater power are required to explore these associations further.
Sensitivity analyses
Results for regular reporters were comparable to those for the full sample (S15 Table). Similar or larger changes were also observed using mixed-effects negative binomial models compared to the analyses presented above (S16 Table). When the date of intervention implementation was changed, no changes in purchasing were detected, providing strong evidence that the observed changes are robust to the time of implementation (S17 Table). There was some indication that changes were greater among households where the main food shopper reported public transport use, though these results were non-significant (S18 Table). When the last 2 weeks of the study period were removed, the observed changes remained similar (S19 Table). These sensitivity analyses provide additional support for the robustness of our results. No significant changes in non-HFSS purchases were detected in intervention households relative to the counterfactual in the post-intervention period (S20 Table), suggesting no spillover effect on non-HFSS purchases.
Discussion
Compared to the counterfactual, this study found that the introduction of advertising restrictions for HFSS products across the London transport network was associated with a relative decrease in average weekly household purchases of energy from HFSS products of 6.7%, or 1,001.0 kcal. Using the mean household size of 2.6 people in the sample, and assuming an even energy distribution, this equates to a relative reduction in purchased energy of 385.0 kcal per person per week, which is equivalent to approximately 72.1 g of standard milk chocolate. Relative reductions in weekly household purchases of fat (57.9 g), saturated fat (26.4 g), and sugar (80.7 g) from HFSS products were also observed. The magnitude of the observed change in sugar purchased associated with the TfL policy is larger than that reported for the UK Soft Drinks Industry Levy (SDIL), a population-level policy widely regarded as successful, which reduced weekly household purchases of sugar by 29.5 g [45]. We observed the largest relative reduction for chocolate and confectionery (19.4%; 317.9 kcal). However, decreases associated with the intervention are in the context of underlying increases in purchases of HFSS products in both the intervention and control areas over the study period. This means that the intervention was associated with a reduced rate in growth of HFSS purchases in the intervention group rather than an absolute reduction in HFSS purchases.
Strengths and limitations
We used a CITS study design as a robust approach to evaluate a natural experiment where a randomised design was not feasible or pragmatic [35]. Such studies are conducted in real-world settings [35,40], and can provide evidence to inform policy [46]. Use of a control group reduced the risk of national-level, time-varying confounders driving observed results, such as seasonal effects, underlying trends in HFSS purchasing, and the effect of other sugar and calorie reduction strategies such as the SDIL [47–49]. Confounding due to other events occurring at the same time as the intervention in either the intervention or control group cannot be ruled out. The changes detected also do not pass the Bonferroni threshold (i.e., P ~ 0.001, based on P = 0.05/36 tests). However, our sensitivity analyses point to our findings being specific to the time of intervention implementation and only detected for HFSS products, especially for the HFSS category chocolate and confectionery, which has few non-HFSS substitutes. There was also an indication that relative reductions observed were larger among regular public transport users, who likely had a larger change in advertising exposure as a result of the TfL policy. Our sensitivity analyses therefore provide support for the observed changes being associated with the TfL policy rather than other events occurring at the same time, or occurring by chance.
The parallel trends assumption was met for all outcomes except chocolate and confectionery. However, similar magnitudes of change were observed when restricting the chocolate and confectionery sample to a shorter pre-intervention time period that exhibited parallel trends. This suggests that the changes observed for chocolate and confectionery were not affected by the lack of parallel trends at the earlier time points. We also found no changes in weekly household purchases of non-HFSS products associated with the introduction of the policy, suggesting that substitution of non-HFSS product categories was unlikely.
Included households were representative of the regions studied in terms of sex, age, socioeconomic position, and household size. Purchase data have been found to be an accurate estimate of food consumption [50]. Most households did not report purchases every week, and we assumed non-reporting was random. However, missingness may have been associated with purchasing behaviour (e.g., forgetting to report purchases from smaller shopping occasions or choosing not to report purchases from less healthy shopping occasions). This study only considered take-home grocery purchases. Out-of-home purchase data were available for a subset of the Kantar FMCG panel, but we did not include these due to limited nutritional data available for out-of-home purchases and differences in data collection methodology.
Companies may have designed advertisements to be compliant with the TfL regulations and then used these in other locations and media, resulting in contamination in the control area. This would result in underestimation of the effect. As the policy was first subject to a public consultation in May 2018, then announced in November 2018, ahead of implementation in February 2019, companies may have also adapted their advertising before the implementation date, but this is unlikely due to the lead-in time for campaigns and the duration of existing campaigns. Our sensitivity analyses suggest observed decreases are robust to time of implementation.
Comparison with other studies
There are few directly comparable studies on the impact of advertising restrictions on purchasing [20,21,26,28,51]. One international study compared broadcast advertising policies across countries, finding that countries with statutory restrictions had reduced volume of ‘junk food’ sales per capita, whilst countries with no policy or voluntary policies had increased volumes of ‘junk food’ sales per capita [19]. A study conducted in the UK comparing periods of time with no television advertising restrictions (pre-2004), industry self-regulation (2005–2007), and statutory regulation (post-2007) found that statutory regulations were effective in reducing household purchases of HFSS products (by £5.60 for drinks and £14.90 for food per capita per quarter among households with children) [52]. Evaluations of restrictions on unhealthy food advertising to children in Quebec and Singapore found decreases in the likelihood of consuming fast food [27,53]. An evaluation of the Chilean food marketing policy found a decrease in household purchases of sugary drinks [51]. However, there was no evidence to suggest that a reduction in advertising exposure mediated a reduction in HFSS consumption, which may have been caused by other factors related to the policy [26].
Interpretation and policy implications
The observed relative reductions in energy, fat, and sugar purchased from HFSS products associated with the restriction of HFSS product advertising across the TfL network could have a meaningful impact on population health. A recent modelling study in the UK estimated that restricting HFSS advertising on television from 5:30 AM to 9:00 PM has the potential to reduce daily energy intake by 9.1 kcal for UK children and result in 40,000 fewer children with obesity [54]. Another modelling study predicted a 24.6 kcal reduction in daily household energy purchased if the price of sugary snacks increased by 20% [55]. The reductions observed in our study were larger than both of these previous estimates, equating to around 55.0 kcal per person (or 143.0 kcal per household) per day. The reduction of 80.7 g of sugar per household per week estimated in our study is also larger than that reported for the SDIL (29.5 g per household per week) [45]. This suggests that the TfL policy has the potential to be a highly effective intervention.
Advertisements were vetted by TfL and only approved if compliant with the policy. For brands selling products with no policy-compliant alternatives (e.g., chocolate and confectionery), advertising was no longer possible. The intervention ‘dose’ was therefore plausibly strongest for chocolate and confectionery, where we found the largest change in purchases. An exceptions process allowed companies to apply to advertise a HFSS product by providing evidence that the product does not contribute to childhood obesity. This mechanism has not been widely used, which suggests that companies are not directly challenging the policy. However, other tactics to circumvent the policy could have been used. For brands with policy-compliant alternative products (e.g., low or zero calorie drinks), brand advertising continued even though advertisement of specific products was restricted. This may explain the lack of change in sugary drink, sugary cereal, and savoury snack purchases—product categories that often have non-HFSS substitutes. Brands ceasing advertising because they had no policy-compliant products may have also created advertising space for brands that have policy-compliant products, allowing them to increase visibility and penetration of their brands [56]. Brand advertising has been found to elicit a brain response and to increase consumption of unhealthy foods and drinks, even when the advertised product is healthy [57,58]. This indicates the potential importance of restricting brand advertising, in addition to individual product advertising, in order to optimise the effectiveness of the policy. It may also be beneficial to restrict advertising of certain nutrient-poor product categories (e.g., cakes and energy bars) regardless of the individual product’s NPM score [59].
We observed larger relative reductions in the last week of the post-intervention period compared to the first. This could be because of delays in the removal of existing HFSS advertising. Consumer behaviour change may also require a longer time frame to shift because food preferences can be difficult to change and there are strong associations between certain brands and HFSS products [60,61]. Although we were unable to assess the sustainability of the observed relative reductions beyond 44 weeks, the larger changes over time indicate that the changes could plausibly be sustained, and may even increase, over time. However, further studies are needed to confirm this.
Sub-group descriptive analyses provide some indication that relative reductions in purchases were greater in less affluent households and households where the main food shopper was living with overweight or obesity. However, these were not statistically significant. If these findings are confirmed in other studies, the policy would be well-targeted to households that would benefit the most from this intervention, and may help reduce inequalities in diet [5,8,9]. This supports previous work that suggests population-level policies are more effective and equitable [62,63]. However, further confirmatory research is required.
The policy was associated with attenuated growth of HFSS purchases rather than an absolute reduction in HFSS purchases. Single interventions cannot be expected to work on their own and should be seen as one part of a wider strategy to improve population health, with multiple interventions needed at multiple points within the food system to improve diet [64,65]. In the UK, the recently proposed restrictions on HFSS advertising before the television ‘9:00 PM watershed’ and on all online HFSS advertising [66], coupled with restrictions on outdoor HFSS advertising being considered in other locations [67], may be an example of emerging policy coherence in this area. This will likely create an overall healthier advertising environment by limiting the displacement of HFSS advertising across advertising media [18,24].
Future research
Future studies need to explore the possible longer-term effects of HFSS advertising restriction policies. Monitoring the response of brands and advertisers and their adaptiveness to a changed policy environment is important in order to optimise and design future policy. For example, the policy may stimulate further product reformulation or the use of unregulated advertising media, or prompt companies to focus more on brand advertising [56,68]. Future studies should also explore the impact of advertising restrictions on out-of-home purchases of HFSS products, which may reveal even further reductions. Studies to quantify the potential impact of such interventions on obesity and related diseases are needed. Replication of this study elsewhere is also important as apparent effect sizes may be lower in settings outside of London where routine use of public transport is lower and the outdoor advertising estate is smaller [69]. In addition, better powered studies to assess differential effects on population sub-groups and inequalities are required. Studies that explore the mechanisms behind changes in food and drink purchases associated with advertising policies, such as changes in advertising exposure, are also important.
Conclusions
In the 10 months following the introduction of the TfL’s HFSS advertising restrictions, we observed a relative reduction in average weekly household purchases of energy from HFSS products of 6.7%, or 1,001.0 kcal. This included a 19.4% (317.9 kcal) reduction for chocolate and confectionery. These findings provide support for policies that restrict HFSS product advertising as a tool to reduce purchases of HFSS products, as a way of improving population diet and preventing obesity.
Supporting information
Vertical line = date of intervention implementation.
(TIF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank Dr. Samantha Hajna for help with producing Fig 1.
Abbreviations
- BMI
body mass index
- CITS
controlled interrupted time series
- FMCG
Fast Moving Consumer Goods
- HFSS
high fat, salt, and sugar
- NPM
Nutrient Profiling Model
- SDIL
Soft Drinks Industry Levy
- TfL
Transport for London
Data Availability
Purchase data, nutrient data and social and demographic data were provided by Kantar Worldpanel Plus. The terms of our data agreement with Kantar mean that we cannot share these data.
Funding Statement
This study is funded by the National Institute for Health Research (NIHR) School for Public Health Research (grant number PD-SPH-2015). The NIHR School for Public Health Research is a partnership between the Universities of Sheffield; Bristol; Cambridge; Imperial; and University College London; The London School for Hygiene and Tropical Medicine (LSHTM); LiLaC – a collaboration between the Universities of Liverpool and Lancaster; and Fuse - The Centre for Translational Research in Public Health, a collaboration between Newcastle, Durham, Northumbria, Sunderland and Teesside Universities. SC is also funded by Health Data Research UK (HDR-UK). HDR-UK is an initiative funded by the UK Research and Innovation, Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities. JA, TB and MW are supported by the MRC Epidemiology Unit, University of Cambridge [grant number MC/UU/12015/6] and Centre for Diet and Activity Research (CEDAR), a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Funding for CEDAR from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the NIHR [grant numbers ES/G007462/1 and MR/K023187/1], and the Wellcome Trust [grant number 087636/Z/08/Z], under the auspices of the UKCRC, is gratefully acknowledged. CT is funded by the NIHR Applied Research Collaboration East of England. AAL is a member of Fuse, the Centre for Translational Research in Public Health (www.fuse.ac.uk). Fuse is a Public Health Research Centre of Excellence funded by the five North East Universities of Durham, Newcastle, Northumbria, Sunderland and Teesside. FdV is partly funded by the NIHR Applied Research Collaboration West (NIHR ARC West) at University Hospitals Bristol NHS Foundation Trust. LC is funded by a UK Medical Research Council fellowship (grant number MR/P021999/1). RG is funded by a UK Medical Research Council studentship [grant number MR/N013638/1]. The views expressed are those of the authors and do not necessarily represent those of any of the above named funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Boyland EJ, Nolan S, Kelly B, Tudur-Smith C, Jones A, Halford JCG, et al. Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am J Clin Nutr. 2016;103:519–33. doi: 10.3945/ajcn.115.120022 [DOI] [PubMed] [Google Scholar]
- 2.Sadeghirad B, Duhaney T, Motaghipisheh S, Campbell NRC, Johnston BC. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes Rev. 2016;17:945–59. doi: 10.1111/obr.12445 [DOI] [PubMed] [Google Scholar]
- 3.Deschasaux M, Huybrechts I, Murphy N, Julia C, Hercberg S, Srour B, et al. Nutritional quality of food as represented by the FSAm-NPS nutrient profiling system underlying the Nutri-Score label and cancer risk in Europe: results from the EPIC prospective cohort study. PLoS Med. 2018;15:e1002651. doi: 10.1371/journal.pmed.1002651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Reducing the impact of marketing of foods and non-alcoholic beverages on children. Geneva: World Health Organization; 2019. [cited 2020 Jul 28]. Available from: https://www.who.int/elena/titles/food_marketing_children/en/. [Google Scholar]
- 5.Adams J, Ganiti E, White M. Socio-economic differences in outdoor food advertising in a city in Northern England. Public Health Nutr. 2011;14:945–50. doi: 10.1017/S1368980010003332 [DOI] [PubMed] [Google Scholar]
- 6.Thomas F, Thomas C, Hooper L, Rosenberg G, Vohra J, Bauld L. Area deprivation, screen time and consumption of food and drink high in fat salt and sugar (HFSS) in young people: results from a cross-sectional study in the UK. BMJ Open. 2019;9:e027333. doi: 10.1136/bmjopen-2018-027333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Backholer K, Gupta A, Zorbas C, Bennett R, Huse O, Chung A, et al. Differential exposure to, and potential impact of, unhealthy advertising to children by socio-economic and ethnic groups: a systematic review of the evidence. Obes Rev. 2021;22:e13144. doi: 10.1111/obr.13144 [DOI] [PubMed] [Google Scholar]
- 8.Yau A, Adams J, Boyland E, Burgoine T, Cornelsen L, de Vocht F, et al. Sociodemographic differences in self-reported exposure to high fat, salt and sugar food and drink advertising: a cross-sectional analysis of 2019 UK panel data. BMJ Open. 2021;11:e048139. doi: 10.1136/bmjopen-2020-048139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palmer G, Green M, Boyland E, Vasconcelos YSR, Savani R, Singleton A. A deep learning approach to identify unhealthy advertisements in street view images. Sci Rep. 2021;11:4884. doi: 10.1038/s41598-021-84572-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris JL, Bargh JA, Brownell KD. Priming effects of television food advertising on eating behavior. Health Psychol. 2009;28:404–13. doi: 10.1037/a0014399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koordeman R, Anschutz DJ, van Baaren RB, Engels RCME. Exposure to soda commercials affects sugar-sweetened soda consumption in young women. An observational experimental study. Appetite. 2010;54:619–22. doi: 10.1016/j.appet.2010.03.008 [DOI] [PubMed] [Google Scholar]
- 12.Zimmerman FJ, Shimoga S V. The effects of food advertising and cognitive load on food choices. BMC Public Health. 2014;14:342. doi: 10.1186/1471-2458-14-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forde H, White M, Levy L, Greaves F, Hammond D, Vanderlee L, et al. The relationship between self-reported exposure to sugar-sweetened beverage promotions and intake: cross-sectional analysis of the 2017 international food policy study. Nutrients. 2019;11:3047. doi: 10.3390/nu11123047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Critchlow N, Bauld L, Thomas C, Hooper L, Vohra J. Awareness of marketing for high fat, salt, or sugar (HFSS) foods, and the association with higher weekly consumption among adolescents: a rejoinder to the UK Government’s consultations on marketing regulation. Public Health Nutr. 2020;23:2637–46. doi: 10.1017/S1368980020000075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cairns G. A critical review of evidence on the sociocultural impacts of food marketing and policy implications. Appetite. 2019;136:193–207. doi: 10.1016/j.appet.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: World Health Organization; 2010. [cited 2022 Jan 25]. Available from: https://www.who.int/publications/i/item/9789241500210. [Google Scholar]
- 17.World Health Organization Regional Office for Europe. Tackling food marketing to children in a digital world: trans-disciplinary perspectives. Copenhagen: World Health Organization Regional Office for Europe; 2016. [cited 2022 Jan 25]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0017/322226/Tackling-food-marketing-children-digital-world-trans-disciplinary-perspectives-en.pdf. [Google Scholar]
- 18.World Health Organization Regional Office for Europe. Evaluating implementation of the WHO set of recommendations on the marketing of foods and non-alcoholic beverages to children: progress, challenges and guidance for next steps in the WHO European Region. Copenhagen: World Health Organization Regional Office for Europe; 2018. [cited 2022 Jan 25]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0003/384015/food-marketing-kids-eng.pdf. [Google Scholar]
- 19.Kovic Y, Noel JK, Ungemack JA, Burleson JA. The impact of junk food marketing regulations on food sales: an ecological study. Obes Rev. 2018;19:761–9. doi: 10.1111/obr.12678 [DOI] [PubMed] [Google Scholar]
- 20.Galbraith-Emami S, Lobstein T. The impact of initiatives to limit the advertising of food and beverage products to children: a systematic review. Obes Rev. 2013;14:960–74. doi: 10.1111/obr.12060 [DOI] [PubMed] [Google Scholar]
- 21.Chambers SA, Freeman R, Anderson AS, MacGillivray S. Reducing the volume, exposure and negative impacts of advertising for foods high in fat, sugar and salt to children: a systematic review of the evidence from statutory and self-regulatory actions and educational measures. Prev Med. 2015;75:32–43. doi: 10.1016/j.ypmed.2015.02.011 [DOI] [PubMed] [Google Scholar]
- 22.Ofcom. Television advertising of food and drink products to children. Final statement. London: Ofcom; 2007. [cited 2022 Jan 25]. Available from: https://www.ofcom.org.uk/__data/assets/pdf_file/0028/47746/Television-Advertising-of-Food-and-Drink-Products-to-Children-Final-statement-.pdf. [Google Scholar]
- 23.Ofcom. HFSS advertising restrictions. Final review. London: Ofcom; 2010. [cited 2022 Jan 25]. Available from: https://www.ofcom.org.uk/__data/assets/pdf_file/0024/31857/hfss-review-final.pdf. [Google Scholar]
- 24.Adams J, Tyrrell R, Adamson A, White M. Effect of restrictions on television food advertising to children on exposure to advertisements for ‘less healthy’ foods: repeat cross-sectional study. PLoS ONE. 2012;7:e31578. doi: 10.1371/journal.pone.0031578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carpentier FRD, Correa T, Reyes M, Taillie LS. Evaluating the impact of Chile’s marketing regulation of unhealthy foods and beverages: pre-school and adolescent children’s changes in exposure to food advertising on television. Public Health Nutr. 2020;23:747–55. doi: 10.1017/S1368980019003355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jensen ML, Dillman Carpentier FR, Adair L, Corvalán C, Popkin BM, Taillie LS. TV advertising and dietary intake in adolescents: a pre- and post- study of Chile’s food marketing policy. Int J Behav Nutr Phys Act. 2021;18:60. doi: 10.1186/s12966-021-01126-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhar T, Baylis K. Fast-food consumption and the ban on advertising targeting children: the Quebec experience. J Mark Res. 2011;48:799–813. doi: 10.1509/jmkr.48.5.799 [DOI] [Google Scholar]
- 28.Taillie LS, Busey E, Stoltze FM, Dillman Carpentier FR. Governmental policies to reduce unhealthy food marketing to children. Nutr Rev. 2019;77:787–816. doi: 10.1093/nutrit/nuz021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Transport for London. Advertising annual report: 2017/18. London: Transport for London; 2018. [cited 2022 Jan 25]. Available from: https://content.tfl.gov.uk/tfl-advertising-report-1718.pdf. [Google Scholar]
- 30.Greater London Authority. Unhealthy weight in London’s children. What we know. London: Greater London Authority; 2019. [cited 2022 Jan 25]. Available from: https://www.london.gov.uk/sites/default/files/unhealthy_weight_in_londons_children.pdf. [Google Scholar]
- 31.Transport for London. TfL ad policy: approval guidance food and non-alcoholic drink advertising. London: Transport for London; 2019. [cited 2022 Jan 25]. Available from: http://content.tfl.gov.uk/policy-guidance-food-and-drink-advertising.pdf. [Google Scholar]
- 32.Meiksin R, Er V, Thompson C, Adams J, Boyland E, Burgoine T, et al. Restricting the advertising of high fat, salt and sugar foods on the Transport for London estate: process and implementation study. Soc Sci Med. 2021;292:114548. doi: 10.1016/j.socscimed.2021.114548 [DOI] [PubMed] [Google Scholar]
- 33.Thompson C, Clary C, Er V, Adams J, Boyland E, Burgoine T, et al. Media representations of opposition to the ‘junk food advertising ban’ on the Transport for London (TfL) network: a thematic content analysis of UK news and trade press. SSM Popul Health. 2021;15:e100828. doi: 10.1016/j.ssmph.2021.100828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berger N, Cummins S, Smith RD, Cornelsen L. Recent trends in energy and nutrient content of take-home food and beverage purchases in Great Britain: an analysis of 225 million food and beverage purchases over 6 years. BMJ Nutr Prev Health. 2019;2:63–71. doi: 10.1136/bmjnph-2019-000036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–55. doi: 10.1093/ije/dyw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Readership Survey. Social grade. London: PAMCo; 2018. [cited 2020 Sep 22]. Available from: http://www.nrs.co.uk/nrs-print/lifestyle-and-classification-data/social-grade/. [Google Scholar]
- 37.Department of Health and Social Care. The nutrient profiling model. London: Department of Health and Social Care; 2011. [cited 2022 Jan 25]. Available from: https://www.gov.uk/government/publications/the-nutrient-profiling-model. [Google Scholar]
- 38.Belotti F. twopm: two-part models. Stata J. 2015;15:3–20. doi: 10.1177/1536867X1501500102 [DOI] [Google Scholar]
- 39.Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PLoS Med. 2017;14:e1002283. doi: 10.1371/journal.pmed.1002283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Vocht F, Katikireddi SV, Mcquire C, Tilling K, Hickman M, Craig P. Conceptualising natural and quasi experiments in public health. BMC Med Res Methodol. 2021;21:32. doi: 10.1186/s12874-021-01224-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Office for National Statistics. CT0203_2011 census—National Statistics Socio-economic Classification (NS-SeC) of Household Reference Person (HRP)—national to local authority. Newport: Office for National Statistics; 2014. [cited 2021 Jul 1]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/adhocs/002630ct02032011censusnationalstatisticssocioeconomicclassificationnssecofhouseholdreferencepersonhrpnationaltolocalauthority. [Google Scholar]
- 42.Statista. How often do you use passenger transport within the UK in your everyday life (underground, bus, train)? New York: Statista; 2021. [cited 2021 Jul 1]. Available from: https://www.statista.com/statistics/682749/passenger-transport-service-in-the-united-kingdom-uk-by-region/. [Google Scholar]
- 43.NHS Digital. Health survey for England 2019: data tables. Leeds: NHS Digital; 2020. [Google Scholar]
- 44.Marcus M, Sant’Anna PHC. The role of parallel trends in event study settings: an application to environmental economics. J Assoc Environ Resour Econ. 2021;8:235–75. doi: 10.1086/711509 [DOI] [Google Scholar]
- 45.Pell D, Mytton O, Penney TL, Briggs A, Cummins S, Penn-Jones C, et al. Changes in soft drinks purchased by British households associated with the UK soft drinks industry levy: controlled interrupted time series analysis. BMJ. 2021;372:11–6. doi: 10.1136/bmj.n254 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 46.Ogilvie D, Adams J, Bauman A, Gregg EW, Panter J, Siegel KR, et al. Using natural experimental studies to guide public health action: turning the evidence-based medicine paradigm on its head. J Epidemiol Community Health. 2020;74:203–8. doi: 10.1136/jech-2019-213085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tedstone A, Targett V, Allen R. Sugar reduction: the evidence for action. London: Public Health England; 2015. [cited 2022 Jan 25]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/470179/Sugar_reduction_The_evidence_for_action.pdf. [Google Scholar]
- 48.Tedstone A, Targett V, Mackinlay B. Calorie reduction: the scope and ambition for action. London: Public Health England; 2018. [cited 2022 Jan 25]. Available from: https://www.gov.uk/government/publications/calorie-reduction-the-scope-and-ambition-for-action. [Google Scholar]
- 49.Department of Health and Social Care. Childhood obesity: a plan for action. Chapter 2. London: HM Government; 2018. [cited 2022 Jan 25]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/718903/childhood-obesity-a-plan-for-action-chapter-2.pdf. [Google Scholar]
- 50.Appelhans BM, French SA, Tangney CC, Powell LM, Wang Y. To what extent do food purchases reflect shoppers’ diet quality and nutrient intake? Int J Behav Nutr Phys Act. 2017;14:46. doi: 10.1186/s12966-017-0502-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taillie LS, Reyes M, Colchero MA, Popkin B, Corvalán C. An evaluation of Chile’s Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: a before-and-after study. PLoS Med. 2020;17:e1003015. doi: 10.1371/journal.pmed.1003015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Silva A, Higgins LM, Hussein M. An evaluation of the effect of child-directed television food advertising regulation in the United Kingdom. Can J Agric Econ. 2015;63:583–600. doi: 10.1111/cjag.12078 [DOI] [Google Scholar]
- 53.Lwin MO, Yee AZH, Lau J, Ng JS, Lam JY, Cayabyab YM, et al. A macro-level assessment of introducing children food advertising restrictions on children’s unhealthy food cognitions and behaviors. Int J Advert. 2020;39:990–1011. doi: 10.1080/02650487.2020.1717856 [DOI] [Google Scholar]
- 54.Mytton OT, Boyland E, Adams J, Collins B, O’Connell M, Russell SJ, et al. The potential health impact of restricting less-healthy food and beverage advertising on UK television between 05.30 and 21.00 hours: a modelling study. PLoS Med. 2020;17:e1003212. doi: 10.1371/journal.pmed.1003212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scheelbeek PFD, Cornelsen L, Marteau TM, Jebb SA, Smith RD. Potential impact on prevalence of obesity in the UK of a 20% price increase in high sugar snacks: modelling study. BMJ. 2019;366:l4786. doi: 10.1136/bmj.l4786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morrison O. How UK brands are reformulating to avoid the HFSS ad ban. Crawley: William Reed Business Media; 2021. [cited 2021 Jun 22]. Available from: https://www.foodnavigator.com/Article/2021/05/19/How-UK-brands-are-reformulating-to-avoid-the-HFSS-ad-ban. [Google Scholar]
- 57.Boyland EJ, Kavanagh-Safran M, Halford JCG. Exposure to “healthy” fast food meal bundles in television advertisements promotes liking for fast food but not healthier choices in children. Br J Nutr. 2015;113:1012–8. doi: 10.1017/S0007114515000082 [DOI] [PubMed] [Google Scholar]
- 58.Masterson TD, Stein WM, Beidler E, Bermudez M, English LK, Keller KL. Brain response to food brands correlates with increased intake from branded meals in children: an fMRI study. Brain Imaging Behav. 2019;13:1035–48. doi: 10.1007/s11682-018-9919-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.World Health Organization Regional Office for the Western Pacific. WHO nutrient profile model for the Western Pacific region: a tool to protect children from food marketing. Manila: World Health Organization Regional Office for the Western Pacific; 2016. [cited 2022 Jan 25]. Available from: http://iris.wpro.who.int/handle/10665.1/13525. [Google Scholar]
- 60.Nicklaus S, Boggio V, Chabanet C, Issanchou S. A prospective study of food preferences in childhood. Food Qual Prefer. 2004;15:805–18. doi: 10.1016/J.FOODQUAL.2004.02.010 [DOI] [Google Scholar]
- 61.Connell PM, Brucks M, Nielsen JH. How childhood advertising exposure can create biased product evaluations that persist into adulthood. J Consum Res. 2014;41:119–34. doi: 10.1086/675218 [DOI] [Google Scholar]
- 62.McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, O’Flaherty M, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health. 2015;15:457. doi: 10.1186/s12889-015-1781-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Adams J, Mytton O, White M, Monsivais P, Marteau T, Woods J. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 2016;13:e1001990. doi: 10.1371/journal.pmed.1001990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390:2602–4. doi: 10.1016/S0140-6736(17)31267-9 [DOI] [PubMed] [Google Scholar]
- 65.White M, Aguirre E, Finegood DT, Holmes C, Sacks G, Smith R. What role should the commercial food system play in promoting health through better diet? BMJ. 2020;368:m545. doi: 10.1136/bmj.m545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.The Queen’s Speech 2021. London: Prime Minister’s Office; 2021 [cited 2022 Jan 25]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/985029/Queen_s_Speech_2021_-_Background_Briefing_Notes..pdf.
- 67.Sustain. Bristol becomes first city outside London to restrict junk food advertising. London: Sustain; 2021. [cited 2021 Mar 12]. Available from: https://www.sustainweb.org/news/mar21-bristol-launch-healthier-food-advertising-policy/. [Google Scholar]
- 68.Finlay A, Lloyd S, Lake AA, Armstrong T, Fishpool M, Green M, et al. An analysis of food and beverage advertising on bus shelters in a deprived area of Northern England. Public Health Nutr. 2022. Jan 3. doi: 10.1017/S1368980021005048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Outsmart. Who sees OOH? London: Outsmart; 2021. [cited 2021 Feb 26]. Available from: https://www.outsmart.org.uk/who-sees-ooh. [Google Scholar]