ABSTRACT
The global pandemic of COVID-19 is caused by the novel coronavirus SARS-CoV-2, which often causes flu-like symptoms and can progress to severe respiratory illness. Thus, as the disease spreads, COVID-19 cases have multiplied across the world, and manifestations involving multiple systems have been described. We report a case of COVID-19-associated meningoencephalitis in a Brazilian male patient who presented with seizures and altered mental status. To the best of our knowledge, this is the first reported case of COVID-19-associated meningoencephalitis in Brazil. COVID-19-associated meningoencephalitis is a rare manifestation of this viral infection and clinicians should be aware of this possible complication.
KEYWORDS: SARS-CoV-2, COVID-19, Meningoencephalitis, Coronavirus
INTRODUCTION
The novel coronavirus disease or COVID-19 is caused by SARS-CoV-2, another RNA virus SARS-CoV that emerged in Wuhan, China, in 2019 1 . Currently, since the World Health Organization officially declared a pandemic state on March 11, 2020, SARS-CoV-2 infection still affects millions of people worldwide 2 . The most common clinical manifestations of COVID-19 are flu-like symptoms, pneumonia and the acute respiratory distress syndrome (ARDS) 3 . However, a wide variety of symptoms related to different organs and systems have been reported. The more affected systems after the respiratory tract are cardiac 4 , central nervous system (CNS) 5 , gastrointestinal and renal 6 . Regarding the neurological involvement, the more commonly reported symptoms are headache, dysgeusia and hyposmia or anosmia. Severe neurological impairment such as encephalitis, meningitis, Guillain-Barré syndrome and vascular events have been described, but they are rare 7 . Several pathological mechanisms have been proposed, such as the direct action of SARS-CoV-2 in the CNS, viral dissemination through neuronal pathways, hematogenic invasion, immune-mediated lesions due to the cytokine storm syndrome and CNS-related hypoxic lesions 7 . Herein, we report a case of COVID-19-associated meningoencephalitis in a male patient hospitalized during the first wave of COVID-19 in Brazil. In addition, we performed a literature review using the PubMed database and the descriptors meningitis and COVID-19, or meningoencephalitis and COVID-19. This case report is part of a cohort study approved by the Research Ethics Committee of Hospital Sao José de Doenças Infecciosas (HSJ) (CAAE N° 35017820.1.0000.5044). An informed consent to publish the patient's clinical data was provided by the patient.
CASE REPORT
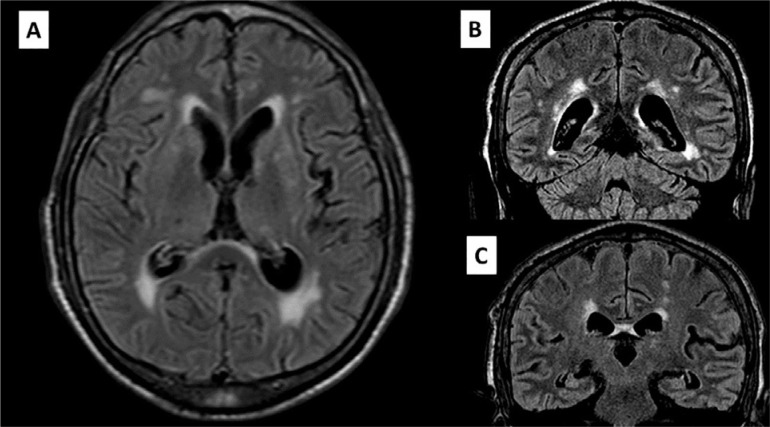
A 68-year-old Brazilian man sought the emergency department (ED) in July 11, 2020, presenting with generalized clonic seizures, nausea, vomiting and altered mental status that started the day before and fever two days before admission. He had no respiratory symptoms. Upon physical examination, the patient was afebrile, disoriented, had a heart rate of 89 bpm and a respiratory rate of 20 rpm, normal vesicular breath sounds in both lungs, accompanied by nuchal rigidity, negative Brudzinski, Kernig and Lasegue signs. The cranial computed tomography (CT) findings were normal. Chest CT findings were unremarkable. Cerebrospinal fluid (CSF) analysis revealed 23 cells/mm3 (89% lymphocytes, 6% monocytes and 5% neutrophils), protein 52 mg/dL, and glucose 58 mg/dL. The CSF gram, fungal stains and bacterial cultures were negative. Intravenous acyclovir was administered. Multiplex PCR (FilmArray Meningitis Encephalitis Panel) of CSF was negative for Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Herpesvirus, Varicella-zoster virus, Cytomegalovirus and Cryptococcus spp. After the results of multiplex PCR, the antiviral administration was discontinued. SARS-CoV-2 was detected by qPCR in a nasopharyngeal and oropharyngeal swab using the Charité, Berlinprotocol for SARS-CoV-2 (E) Bio- Manguinhos kit 8 . Later, SARS-CoV-2 RNA was also amplified in CSF specimens using the CDC protocol 9 . Cranial magnetic resonance imaging (MRI) showed leptomeningeal enhancement and diffuse alteration of the bilateral periventricular white matter suggestive of encephalitis ( Figure 1 ). On day 9 of hospitalization, although the patient presented with neurological improvement, he developed new episodes of fever, cough and purulent sputum. Chest radiography revealed a pulmonary consolidation. Chest CT revealed bilateral pleural effusion and a right lobe consolidation without ground-glass opacities. A 10-day regimen of meropenem and vancomycin was administered. He presented with clinical improvement and was discharged after 20 days of hospitalization.
Figure 1. Brain MRI with areas of hyperintensity in T2w-FLAIR on the bilateral periventricular white matter and leptomeningeal enhancement: (A) Sagittal plane; (B) and (C) Coronal plane. MRI = magnetic resonance imaging; T2w-FLAIR = T2-weighted fluid-attenuated inversion recovery.
DISCUSSION
The neurological findings related to SARS-CoV-2 infection and the pathogenesis of the disease in the CNS are not completely understood. Previous studies in autopsies revealed the presence of the virus in the CSF and brain parenchyma, which may suggest its tropism and ability to penetrate the CNS 10 , 11 .
The two main hypotheses are based on neurotropism by the direct invasion of SARS-CoV-2 in the CNS and indirect mechanisms mediated by the cytokine storm. In a study of post-mortem brain biopsies from patients with COVID-19, activation of microglia and infiltration of cytotoxic T lymphocytes were observed, mainly in the brainstem and cerebellum. Microglia express the CD68 marker intensely, causing an increase in the phagocytic activity 12 . Among the main pathways that the virus can reach the CNS is the hematogenous pathway, which has already been described for other coronaviruses. In addition, viral particles have been found in the capillary endothelium and frontal lobe neurons in autopsies, corroborating this statement. However, in the neuronal pathway, the virus infects nerve endings and migrates across synapses to reach the CNS 7 , 10 , 11 .
The presence of neurological symptoms in COVID-19 usually occurs in more than one-third of patients 7 . The olfactory nerve is the main affected neuronal via due to its proximity to the nasal cavity, the primary site of SARS-CoV-2 infection. The finding of hyposmia or anosmia in the early stages of the disease is frequently observed in many patients 12 , showing that SARS-CoV-2 may have a tendency for neuro-invasion 10 - 12 .
Neurological syndromes have also been associated with SARS-CoV-2 infection. Encephalitis, meningitis, acute disseminated encephalomyelitis, Guillain-Barré syndrome and acute stroke have been reported 6 , 7 , 13 . The first case of COVID-19-associated meningoencephalitis was described in a 24-year-old man that had intense headache and fever 5 . The MRI revealed hiperintensity along the wall of the inferior horn in the right lateral ventricle, as well as hyper intense signal changes in the right mesial temporal lobe and hippocampus 5 .
Since then, other cases have been reported worldwide, but still represent few cases compared to the large pandemic scale 5 , 13 - 20 . Table 1 shows all reported cases of meningitis and meningoencephalites in PubMed database until September 2021. Positive RT-PCR in CSF seems to be a rare finding. Furthermore, the sensitivity and specificity of RT-PCR in CSF are unknown 5 . We only found two cases with positive RT-PCR for SARS-CoV-2 in CSF in the literature review. Herein, we describe the first case of SARS-COV-2 detected in CSF in Brazil.
Table 1. Thorough description of reported cases of meningitis and meningoencephalitis due to SARS-CoV-2.
| Authors | Title | Neurological Syndrome | Month/Year 1 | Country | Age | Sex | CSF RT-PCR for SARS-CoV-2 | Nasopharyngeal Swab for SARS-CoV-2 | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Moriguchi et al. 5 | A first case of meningitis/encephalitis associated with SARS-CoV-2 | Meningitis | April/2020 | Japan | 24 y | M | Positive | Negative | N/A |
| Packwood et al . 13 | Unusual Case Report of COVID-19 presenting with Meningitis symptoms and shingles | Meningitis | August/2020 | United States | 58 y | M | N/A | Positive | Discharge |
| Dharsandiya et al . 14 | SARS-CoV-2 viral sepsis with meningoencephalitis | Meningoencephalitis | June/2020 | India | 68 y | M | NP | Positive | Death |
| Bernard-Valn et al . 15 | Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection | Meningoencephalitis | September/2020 | Switzerland | 64/67 y | F | Negative | Positive | Discharge * |
| Ferreira et al . 16 | Acute meningoencephalitis as initial presentation of SARS-CoV-2 Infection in pediatrics | Meningoencephalitis | November/2020 | Colombia | 5 m | N/A | Negative | Positive 2 | Discharge |
| Dugue et al . 17 | Neurologic manifestations in an infant with COVID-19 | Meningoencephalitis | June/2020 | United States | 1 m | M | Negative | Positive | Discharge |
| Regev et al. 18 | Pediatric Inflammatory Multisystem Syndrome with Central Nervous System involvement and hypocomplementemia following SARS-CoV-2 infection | Meningoencephalitis | August/2020 | Israel | 16 y | M | Negative | Positive | Discharge |
| Al-Olama et al. 19 | COVID-19-associated meningoencephalitis complicated with intracranial hemorrhage: a case report | Meningoencephalitis | May/2020 | United Arab Emirates | 36 y | M | Positive 2 | Positive 2 | N/A |
| Chaumont et al. 20 | Acute meningoencephalitis in a patient with COVID-19 | Meningoencephalitis | June/2020 | France | 69 y | M | Negative | Positive 3 | Discharge |
Publication date;
Second swab was positive;
Performed as bronchoalveolar lavage; M = Male; F = Female; N/A = Not Available; NP=Not performed;
both patients were female, had negative CSF RT-PCR for SARS-CoV-2 , and discharged; m = months; y = years.
In a recent systematic review of 61 cases, Mondal et al. 12 found that confusion, disorientation and altered mental status were observed in 22.22% of cases. Kernig's and Lasegue's signs were absent, although nuchal rigidity was present in 9.25% 12 . In this case, the main symptoms were seizures and altered mental status. Signals of meningism were not detected.
Viral meningoencephalitis usually causes leptomeningeal inflammation that may be present adjacent to the subpial cortical lesions. Lymphocytic pleocytosis and CSF protein levels are typically observed in viral meningoencephalitis 7 , 12 . Previous studies revealed that MRI without abnormalities occurs in the majority of cases. However, the most common abnormality reported was T2/FLAIR hyperintensity affecting the temporal lobes, which may occur in other viral conditions 7 , 12 . Electroencephalography (EEG) may reveal non-specific findings such as focal epileptiform discharges and generalized slowness of the waves 12 .
In our case, the diagnosis of COVID-19-associated meningoencephalitis was diagnosed based on clinical symptoms, CSF analysis and MRI findings. EEG was unavailable in our service and there was also a high risk of SARS-CoV-2 transmission during the patient's transportation.
CONCLUSION
In conclusion, although COVID-19-associated meningoencephalitis is a rare condition, in a pandemic context, meningitis or encephalitis must be suspected in acute neurological conditions. Herein, we presented a case of COVID-19-associated meningoencephalitis in Brazil, with a favorable prognosis. This case is unique and provides evidence of neurological complications associated with COVID-19. More studies are necessary to fully understand the clinical implications of this rare neurological complication. Physicians should be aware of this diagnosis.
ACKNOWLEDGMENTS
The authors would like to acknowledge the patient and all the staff from Hospital Sao Jose de Doenças Infecciosas .
Footnotes
FUNDING
None
REFERENCES
- 1.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO Director-General's opening remarks at the media briefing on COVID-19. Mar 11, 2020. [[cited 2022 Jan 18]]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–––11-march-2020 . [Google Scholar]
- 3.Jiang F, Deng L, Zhang L, Cai Y, Cheung CW, Xia Z. Review of the clinical characteristics of Coronavirus disease 2019 (COVID-19) J Gen Intern Med. 2020;35:1545–1549. doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–1667. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai CC, Ko WC, Lee PI, Jean SS, Hsueh PR. Extra-respiratory manifestations of COVID-19. Int J Antimicrob Agents. 2020;56:106024–106024. doi: 10.1016/j.ijantimicag.2020.106024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg. 2020;194:105921–105921. doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045–2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . CDC's diagnostic test for COVID-19 only and supplies. [[cited 2022 Jan 18]]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/lab/virus-requests.html . [Google Scholar]
- 10.Puccioni-Sohler M, Poton AR, Franklin M, Silva SJ, Brindeiro R, Tanuri A. Current evidence of neurological features, diagnosis, and neuropathogenesis associated with COVID-19. Rev Soc Bras Med Trop. 2020;53:e20200477. doi: 10.1590/0037-8682-0477-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11:995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 12.Mondal R, Ganguly U, Deb S, Shome G, Pramanik S, Bandyopadhyay D, et al. Meningoencephalitis associated with COVID-19: a systematic review. J Neurovirol. 2021;27:12–25. doi: 10.1007/s13365-020-00923-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Packwood R, Galletta G, Tennyson J. An unusual case report of COVID-19 presenting with meningitis symptoms and shingles. Clin Pract Cases Emerg Med. 2020;4:316–320. doi: 10.5811/cpcem.2020.4.47557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dharsandiya M, Shah K, Patel K, Patel T, Patel A, Patel A. SARS-CoV-2 viral sepsis with meningoencephalitis. Indian J Med Microbiol. 2020;38:219–221. doi: 10.4103/ijmm.IJMM_20_291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M, et al. Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. Eur J Neurol. 2020;27:e43–e44. doi: 10.1111/ene.14298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferreira C, Correa-Roda M. Acute meningoencephalitis as initial presentation of SARS-CoV-2 infection in pediatrics. Pediatr Infect Dis J. 2020;39:e386–e387. doi: 10.1097/INF.0000000000002885. [DOI] [PubMed] [Google Scholar]
- 17.Dugue R, Cay-Martínez KC, Thakur KT, Garcia JA, Chauhan LV, Williams SH, et al. Neurologic manifestations in an infant with COVID-19. Neurology. 2020;94:1100–1102. doi: 10.1212/WNL.0000000000009653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Regev T, Antebi M, Eytan D, Shachor-Meyouhas Y, Ilivitzki A, Aviel YB, et al. Pediatric inflammatory multisystem syndrome with central nervous system involvement and hypocomplementemia following SARS-COV-2 infection. Pediatr Infect Dis J. 2020;39:e206–e207. doi: 10.1097/INF.0000000000002804. [DOI] [PubMed] [Google Scholar]
- 19.Al-Olama M, Rashid A, Garozzo D. COVID-19-associated meningoencephalitis complicated with intracranial hemorrhage: a case report. Acta Neurochir (Wien) 2020;162:1495–1499. doi: 10.1007/s00701-020-04402-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaumont H, Etienne P, Roze E, Couratier C, Roger PM, Lannuzel A. Acute meningoencephalitis in a patient with COVID-19. Rev Neurol (Paris) 2020;176:519–521. doi: 10.1016/j.neurol.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]