Abstract
In this report, we illustrate the different flow-gradient patterns of aortic stenosis associated with discordant grading of stenosis severity at transthoracic echocardiography (TTE). The discordance among TTE parameters (mean gradient and aortic area) can be reconciled and true severity can be confirmed by ruling out potential measurements errors and by using multimodality imaging. (Level of Difficulty: Advanced.)
Key Words: aortic valve, computed tomography, echocardiography
Abbreviations and Acronyms: AS, aortic stenosis; AU, Agatston unit; AV, aortic valve; AVA, aortic valve area; AVAi, indexed aortic valve area; AVAproj, projected aortic valve area; DSE, dobutamine stress echocardiography; LV, left ventricular; LVEF, left ventricular ejection fraction; LVOT, left ventricular outflow tract; LVOTD, left ventricular outflow tract diameter; MG, mean transvalvular gradient; MDCT, multidetector computed tomography; SV, stroke volume; SVi, indexed stroke volume; TTE, transthoracic echocardiography; Vpeak, peak aortic velocity
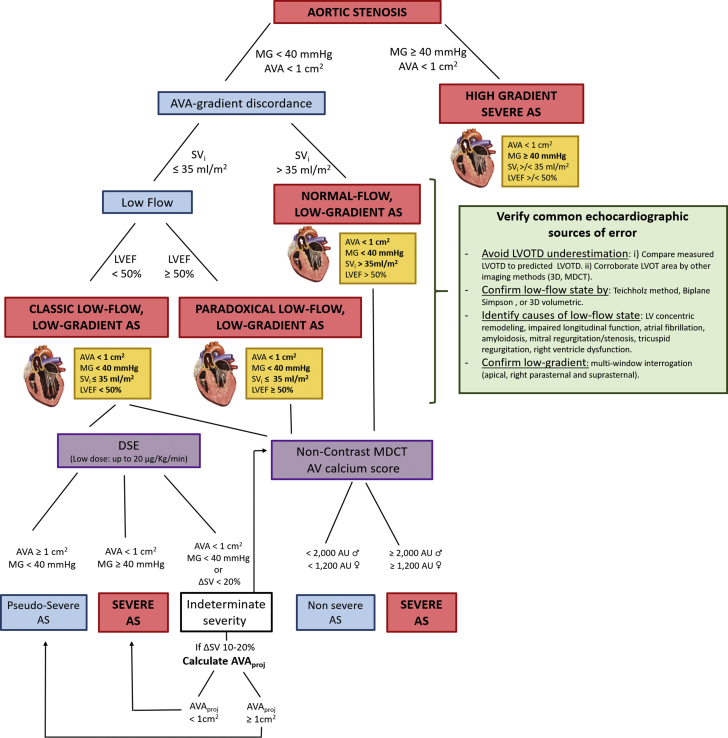
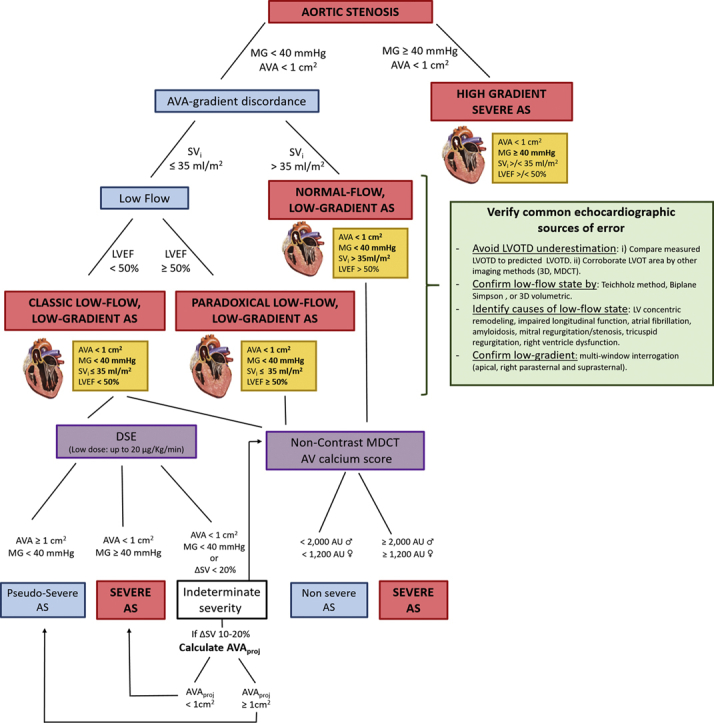
Central Illustration
Introduction
Severe aortic stenosis (AS) has been traditionally defined as a mean transvalvular gradient (MG) ≥40 mm Hg or a peak aortic velocity (Vpeak) ≥4 m/s, typically associated with an aortic valve area (AVA) <1 cm2 (Figure 1).1 However, approximately one-third of patients with AS present with AVA-MG discordance on transthoracic echocardiography (TTE), the most frequent being the coexistence of a small (ie, severe) AVA with low (ie, moderate) MG and Vpeak (Figure 1). This issue raises uncertainty about the true severity of AS and thus the indication for aortic valve (AV) replacement. The objectives of this case series are as follows: 1) to present the possible sources of error leading to discrepancy between AVA and MG; 2) to describe the different flow-gradient patterns of AS; and 3) to present a multimodality and multiparameter integrative approach to AS grading.
Learning Objectives
-
•
To rule out potential sources of error leading to discrepancy between AVA and MG in the assessment of AS severity.
-
•
To describe the different flow-gradient patterns that may result in discordant grading of AS severity at TTE and may require additional tests.
-
•
To apply a multimodality imaging approach (DSE and AV calcium score) to confirm AS severity in the different flow-gradient patterns.
Figure 1.
Algorithm for AS Severity in the Different Flow-Gradient Scenarios
AS = aortic stenosis; AU = Agatston units; AV = aortic valve; AVA = aortic valve area; AVAproj = projected aortic valve area; DSE = dobutamine stress echocardiography; LV = left ventricular; LVEF = left ventricular ejection fraction; LVOT = left ventricular outflow tract; LVOTD = left ventricular outflow tract diameter; MDCT = multidetector computed tomography; MG = mean transvalvular gradient; SV = stroke volume; SVi = indexed stroke volume; ΔSV = change in stroke volume; 3D = 3-dimensional.
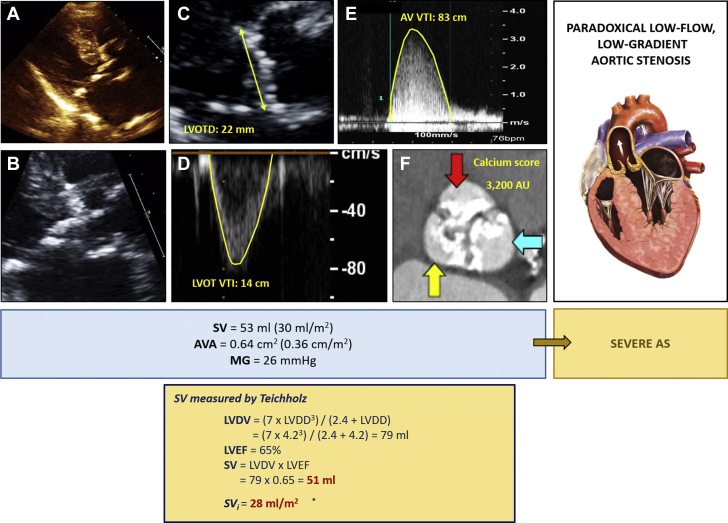
Case 1: Paradoxical Low-flow, Low-gradient Severe AS
An 80-year-old woman with hypertension was referred for heart failure. The TTE revealed a preserved left ventricular (LV) ejection fraction (LVEF) with concentric hypertrophy. The AV leaflets were thickened. MG was 26 mm Hg, and AVA was 0.64 cm2. Stroke volume (SV) and indexed SV (SVi) were 53 mL and 30 mL/m2, respectively (Figures 2A to 2F). A diagnosis of paradoxical low-flow, low-gradient severe AS was suspected (Figure 1). Multidetector computed tomography (MDCT) confirmed severe AS with a calcium score of 3,200 Agatston units (AU) (Figures 2A to 2F). The cutoff values for severe AS are 2,000 and 1,200 AU for men and women, respectively. However, in patients with a small or large aortic annulus, these values should be indexed to the area of the annulus, and thresholds for severity are 500 and 300 AU/cm2 for men and women, respectively.
Figure 2.
Discordant Severity Grading in a Patient With Paradoxical Low-Flow, Low-Gradient AS
(A) Left ventricular concentric hypertrophy. (B) Calcified aortic valve (AV). (C) Left ventricular outflow tract diameter (LVOTD) (arrows). (D) Pulsed-wave Doppler imaging in the left ventricular outflow tract (LVOT) in the apical 5-chamber view and (E) continuous-wave Doppler imaging of transaortic flow in the right sternal border. (F) Aortic valve calcium score. (Bottom) Methods to corroborate stroke volume. LVDD = left ventricular diastolic diameter; LVDV = left ventricular diastolic volume; VTI = velocity-time integral; other abbreviations as in Figure 1.
Expert tip
In this scenario, it is important to rule out sources of error in the echocardiographic measurement of SV and AVA. An underestimation of SV may lead to underestimation of AVA. To rule out measurement errors, one should take the following steps: 1) calculate the Doppler velocity index, and if it is >0.25, an underestimation of the left ventricular outflow tract (LVOT) diameter (LVOTD) must be suspected; and 2) corroborate the SV by other methods such as the 2-dimensional biplane Simpson method, the Teichholz method, or 3-dimensional volumes (Figure 2, bottom). The association of low-gradient AS and cardiac amyloidosis is relatively frequent, and a careful assessment of red flags for cardiac amyloidosis should be performed.
In patients with a small-AVA–low-gradient discordance, it is also important to perform careful multiwindow interrogation to avoid underestimation of MG or Vpeak. Indeed, the highest MG or Vpeak values are obtained at the right sternal border in up to 50% of the patients.2
Dobutamine stress echocardiography (DSE) is not recommended in this subset of patients with low-gradient AS. Reduced longitudinal LV function and elevated natriuretic peptides are surrogate markers of subclinical LV dysfunction and decompensation, and they should be taken into account for therapeutic decision making and risk stratification.
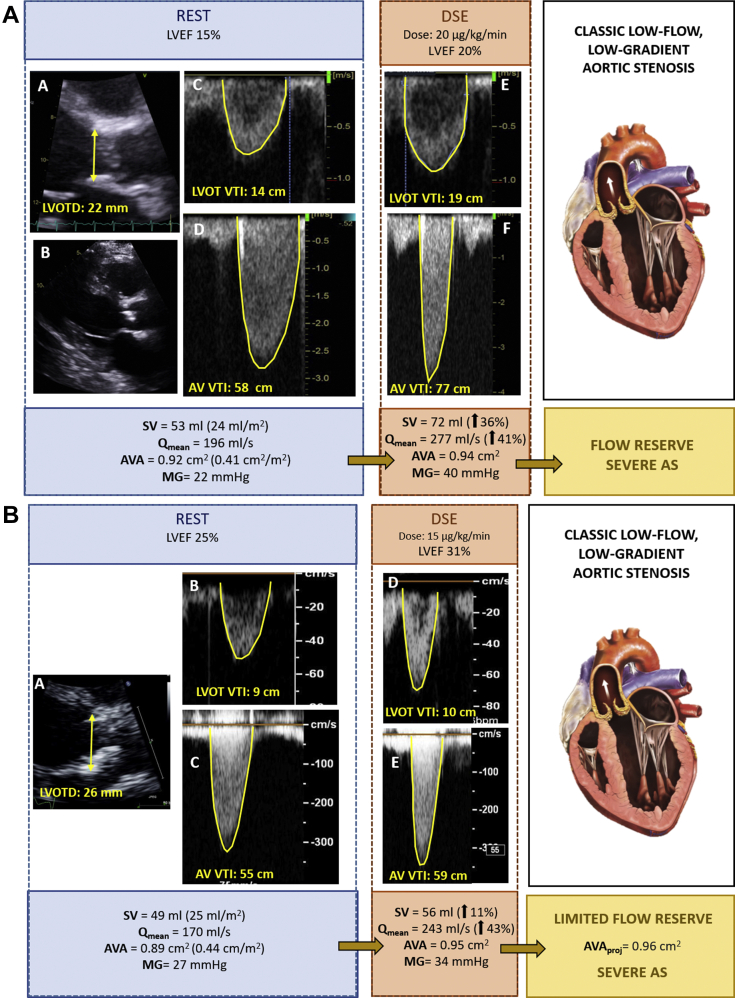
Case 2: Classic Low-Flow, Low-Gradient Severe AS With Flow Reserve
A 55-year-old man with diabetes mellitus was referred for dyspnea. The TTE showed severe LV dysfunction (LVEF, 15%). The AV was moderately calcified, MG was 22 mm Hg, with reduced SVi of 24 mL/m2, and AVA was 0.92 cm2 (Figure 3A). These findings are consistent with classic low-flow, low-gradient AS. Ischemic cardiomyopathy was excluded. DSE was performed to differentiate severe from pseudosevere AS (Figure 1). On DSE, the patient showed significant flow reserve (increase in SV ≥20%), MG increased up to 40 mm Hg, whereas AVA remained at 0.94 cm2 (Figure 3A). This finding confirmed severe AS.
Figure 3.
Discordant Severity Grading in Patients With Classic Low-Flow, Low-Gradient AS
(A) Patient with flow reserve. (A) Left ventricular outflow tract diameter (LVOTD) (arrows).(B) Mild left ventricular dilation. (C) Pulsed-wave Doppler imaging in the left ventricular outflow tract (LVOT) and (D) continuous-wave Doppler imaging of transaortic flow at rest and (E and F) at dobutamine stress echocardiography (DSE). (B) Patient with limited flow reserve. (A) Left ventricular outflow tract diameter (arrows).(B) Pulsed-wave Doppler imaging in the left ventricular outflow tract and (C) continuous-wave Doppler imaging of transaortic flow at rest and (D and E) at dobutamine stress echocardiography. (C) Patient without flow reserve. Doppler echocardiographic images (A-C) at rest and (D-F) at DSE showing (A and D) the left ventricle, (B and E) left ventricular outflow tract pulsed-wave Doppler imaging, and (C and F) transaortic flow continuous-wave Doppler imaging.(D) Pseudosevere AS. Images (A and B) at rest and (C and D) at dobutamine stress echocardiography showing (A and C) left ventricular outflow tract pulsed-wave Doppler imaging and (B and D) transaortic flow continuous-wave Doppler imaging. Qmean = mean transvalvular flow rate; other abbreviations as in Figures 1 and 2.
Case 3: Classic Low-Flow, Low-Gradient Severe AS With Limited Flow Reserve
A 73-year-old man with ischemic cardiomyopathy (LVEF, 25%) presented with a calcified AV. MG and AVA were 27 mm Hg and 0.89 cm2, respectively (Figure 3B). In the setting of low flow (SVi, 25 mL/m2) and LV systolic dysfunction, these findings are consistent with classic low-flow, low-gradient AS (Figure 1). DSE showed limited flow reserve with persistent discordance of AVA and gradients at stress (Figure 3B). In cases of indeterminate AS severity after DSE, projected AVA (AVAproj) or the AV calcium score could be useful to reconcile the discordant grading (Figure 1). The AVAproj for this patient was 0.96 cm2, thus confirming severe AS.
Case 4: Classic Low-Flow, Low-Gradient Severe AS With No Flow Reserve
A 76-year-old woman with previous coronary artery bypass graft and LV dysfunction (LVEF, 25%), had a calcified AV noted on TTE. MG was 27 mm Hg, AVA was 0.82 cm2, and SVi was 26 mL/m2 (Figure 3C). DSE showed no flow reserve and thus no significant change in MG and AVA (Figure 3C). In this case, the discordant grading persisted after DSE, and stenosis severity remained indeterminate (Figure 1). MDCT revealed a high calcium score (3,682 AU), confirming severe AS.
Case 5: Pseudosevere AS
A 70-year-old man with hypertension, diabetes mellitus, and ischemic cardiomyopathy (LVEF, 20%), presented with a MG of 22 mm Hg, an AVA of 0.85 cm2, and a low-flow state (SVi, 20 mL/m2) (Figure 3D). A diagnosis of classic low-flow, low-gradient AS was made (Figure 1). DSE showed flow reserve (SV increased from 36 to 55 mL). MG and AVA increased up to 32 mm Hg and 1.2 cm2, respectively, consistent with pseudosevere (ie, moderate) AS.
Expert tip
In case of depressed LVEF and a low-flow state, DSE is useful to confirm the severity of AS.3 In patients with significant flow reserve and normalization of transvalvular flow (mean flow >210 mL/s), DSE generally allows confirmation of AS severity: truly severe or pseudosevere (Cases 2 and 5). However, if flow reserve is present but not sufficient to normalize flow status, the AVA-MG discordance persists, and AS severity remains undetermined. In such patients, the AVAproj could be an option to confirm AS severity (Case 3). However, a minimum of 10% to 15% increase in flow is required to obtain a reliable estimate of this parameter, and so in patients with no flow reserve, the AVAproj cannot be calculated and the DSE is inconclusive (Case 4). Finally, the AV calcium score may be a parameter of interest to assess in all cases of low-gradient AS (Figure 1).
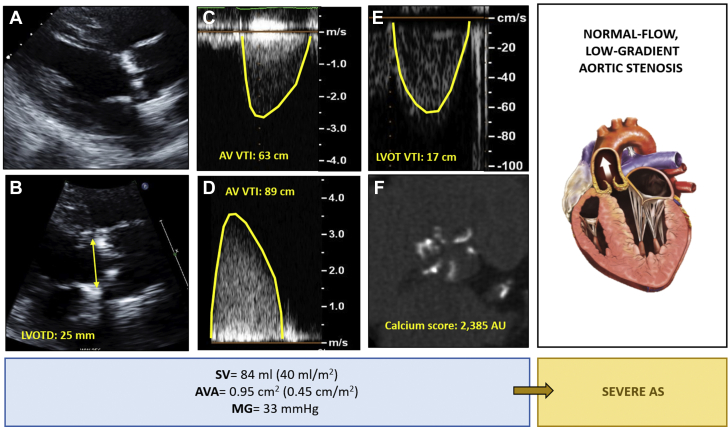
Case 6: Normal-Flow, Low-Gradient Severe AS
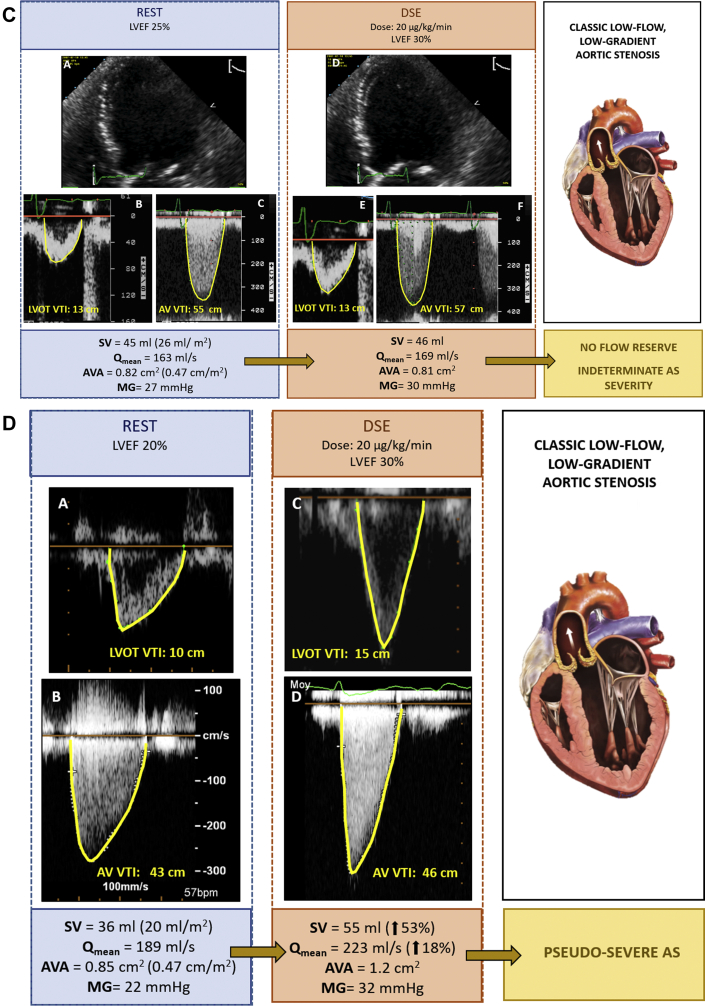
An 84-year-old man with hypertension and diabetes mellitus was referred for dyspnea. The TTE showed normal LVEF, LV hypertrophy, and a severely calcified AV. The highest MG was 33 mm Hg in the right sternal view. SVi was 40 mL/m2, and the AVA was 0.95 cm2 (Figures 4A to 4F). A diagnosis of normal-flow, low-gradient AS was made (Figure 1). In this scenario, an AV calcium score of 2,385 AU was consistent with severe AS (Figures 4A to 4F).
Figure 4.
Discordant Severity Grading in a Patient With Normal-Flow, Low-Gradient AS
(A) Left ventricular hypertrophy. (B) Left ventricular outflow tract diameter (LVOTD) (arrows). Continuous-flow Doppler imaging of transaortic flow in (C) the apical view and (D) the right sternal border and (E) pulsed-wave Doppler imaging in the left ventricular outflow tract (LVOT). (F) Aortic valve (AV) calcium score. Abbreviations as in Figures 1, 2, and 3.
Expert tip
The first step in cases of AVA-MG discordance is to exclude errors in the measurement of the LVOTD. Given that the LVOTD is squared in the continuity equation, a minimal error may lead to an important change in AVA. We recommend comparing the measured LVOTD with the predicted LVOTD by using the following formula.
Predicted LVOTD = (5.7 × body surface area) + 12.1
In Case 6, the predicted LVOTD was similar to the measured LVOTD (24 and 25 mm, respectively). Usually, discrepancies >2 mm suggest an inaccurate LVOTD measurement.
Discussion
Low-gradient AS, which is characterized by the combination of a small AVA with a low MG and thus resulting in discordant grading of AS severity, is a challenging entity. Comprehensive echocardiographic and multimodality imaging is key to differentiate the flow-gradient patterns and to confirm the severity of AS1,4 (Figure 1).
The first step is to confirm the accuracy of echocardiographic measurements, especially of LVOTD and flow state, to avoid misclassification. Multiwindow interrogation is essential to obtain an accurate measurement of the MG and Vpeak. The second and more challenging step is to confirm AS severity in each scenario of AVA-MG discordance. Low-dose DSE is recommended only in patients with classic low-flow, low-gradient AS.1,4 However, an AV calcium score could be obtained in all the scenarios of low-gradient AS,1,4 as well as if the severity of AS remains indeterminate after DSE (Figure 1).
Conclusions
Discordant grading of AS severity at TTE is a challenging issue that raises uncertainty about the true severity of AS. A comprehensive echocardiographic assessment and complementary multimodality imaging, including DSE and an AV calcium score by MDCT, are key to confirm AS severity in the different scenarios of AVA-MG discordance.
Funding Support and Author Disclosures
This work was supported by a research grant from Canadian Institutes of Health Research (#FDN-143225). Dr Silva has received support by a grant from the Martin Escudero Foundation. Dr Pibarot has received institutional funding from Edwards Lifesciences, Medtronic, and Pi-Cardia for echocardiography core laboratory services in the field of transcatheter valve therapy of aortic stenosis, with no personal compensation. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Otto C.M., Nishimura R.A., Bonow R.O., et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease. J Am Coll Cardiol. 2021;77(4):e25–e197. doi: 10.1016/j.jacc.2020.11.018. [DOI] [PubMed] [Google Scholar]
- 2.Thaden J.J., Nkomo V.T., Lee K.J., Oh J.K. Doppler imaging in aortic stenosis: the importance of the nonapical imaging windows to determine severity in a contemporary cohort. J Am Soc Echocardiogr. 2015;28(7):780–785. doi: 10.1016/j.echo.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 3.Baumgartner H., Hung J., Bermejo J., et al. EACVI/ASE clinical recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30:372–392. doi: 10.1016/j.echo.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Clavel M.A., Burwash I.G., Pibarot P. Cardiac imaging for assessing low-gradient severe aortic stenosis. J Am Coll Cardiol Img. 2017;10(2):185–202. doi: 10.1016/j.jcmg.2017.01.002. [DOI] [PubMed] [Google Scholar]