Abstract
Acceptance and commitment therapy (ACT) is a contemporary behavior-analytic approach to intervening on verbal behavior for the purposes of bringing about socially meaningful overt behavior change. Although originally developed as a behavior-analytic approach to psychotherapy, the conceptual functional analyses and procedures that form the core of ACT have been disseminated broadly outside of clinical psychology, including within the field of applied behavior analysis (ABA). This article discusses the use of ACT within mainstream ABA practice and provides preliminary conceptual functional analyses and practical guidelines for incorporating ACT within the scope of practice of applied behavior analysts.
Keywords: Acceptance and commitment therapy, Acceptance and commitment training, Scope of practice, Applied behavior analysis
Acceptance and commitment therapy (ACT) is a behavior-analytic approach to addressing problematic verbal behavior involved in behavioral rigidity and insensitivity to socially significant contingencies. The overall goal of ACT is to increase psychological flexibility, which consists of engaging in skillful behavior in the presence of aversive experiences in the service of living a rich and meaningful life. A substantial empirical literature has established ACT as an empirically supported treatment. Since 2015, over 15 meta-analyses of ACT methods have been published (for a list, see Hayes, S. C. (n.d.). A meta-analysis in 2012 found 66 ACT component studies (Levin, Hildebrandt, Lillis, & Hayes, 2012), and dozens more such studies have appeared since. Over 60 mediational studies have been published, and most find that changes in the core processes of ACT are functionally important to ACT outcomes https://contextualscience.org/act_studies_with_mediational_data.
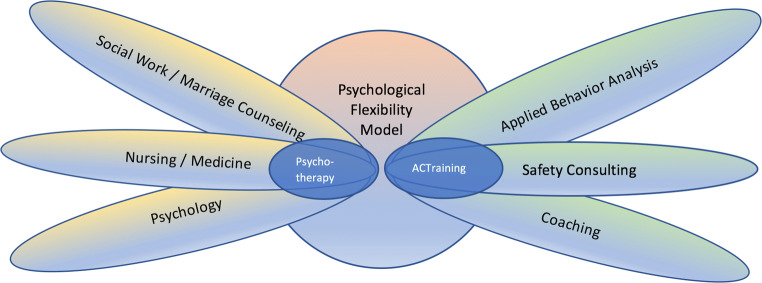
ACT was originally developed and continues to be primarily applied within psychotherapeutic and counseling contexts. However, over the years, a wide range of professions have shown interest in applying ACT outside such settings. For example, nurses and health professionals have successfully used ACT in health coaching sessions to help patients recover from colorectal cancer treatment (Hawkes et al., 2013). Similar efforts have been made by teachers, physical therapists, sports coaches, occupational therapists, dentists, diabetes educators, and professionals from other disciplines (e.g., Kasson & Wilson, 2016; McCracken & Jones, 2012; Pahnke, Lundgren, Hursti, & Hirvikoski, 2014; Szabo & Dixon, 2016). In recent years, interest in ACT from within the applied behavior analysis (ABA) community has continued to grow, and ACT is increasingly integrated into behavior-analytic practice by Board Certified Behavior Analysts (BCBAs). The present article contextualizes this trend in the history and current status of behavior analysis and explores how ACT fits within the scope of practice of BCBAs.
The Behavior-Analytic Roots of ACT
The course of development of ACT illustrates its deep roots in behavior analysis from the outset. ACT research began to emerge in 1981 from Steven Hayes’s lab at the University of North Carolina, Greensboro, a laboratory jointly led by an established behavior-analytic basic researcher, Aaron Brownstein (see Zettle, 2005, for a historical account). This early ACT research sought to address the repertoire-narrowing effects of verbal rules (e.g., Hayes, Brownstein, Haas, & Greenway, 1986; Hayes, Brownstein, Zettle, Rosenfarb & Korn, 1986). A 1982 talk by Steven Hayes at the annual convention of the Association for Behavior Analysis International (ABAI) on rule-governed behavior and psychopathology (Hayes, 1982) led to the first ACT workshop to be held at a scientific meeting. The ABAI workshop, titled “Semantic Therapy, Cognition, Rule-Governed Behavior, and Psychopathology: A Radical Behavioral Approach” (Hayes, 1983), was followed a year later by what is arguably the first article on both ACT and relational frame theory (RFT) in the journal Behaviorism (Hayes, 1984). The first extended presentation of RFT quickly followed at ABAI in 1985 (Hayes & Brownstein, 1985).
Empirical articles on what would later become ACT soon appeared (e.g., Zettle & Hayes, 1986). However, the initial focus in the early development of ACT was on empirical investigations of the rigidity of rule-governed behavior and the link between derived stimulus relations and language development, published in the Journal of the Experimental Analysis of Behavior (e.g., Devany, Hayes, & Nelson, 1986; Hayes, Brownstein, Haas, & Greenway, 1986; Hayes, Brownstein, Zettle, Rosenfarb, & Korn, 1986). As these data converged on RFT as a basic behavioral account of human language and cognition, Hayes and colleagues’ conceptual work focused on the refinement of radical behaviorism as a philosophy of science (Hayes, Hayes, & Reese, 1988) to more adequately address the relation between private events and overt action in a nonmentalistic way (e.g., Hayes & Brownstein, 1986). Over the next 15 years, theoretical and philosophical foundations were clarified (e.g., Hayes & Hayes, 1992), and ACT was refined and manualized (Hayes, McCurry, Afari, & Wilson, 1991).
In the more than 35-year history of the development of ACT, the basic and applied data supporting its implementation as a mainstream psychological intervention have flourished. There are currently over 300 published randomized controlled trials of ACT Hayes, S.C. (2020). As such, ACT has been listed as an empirically supported treatment approach by Division 12 of the American Psychological Association (2016) and by the Department of Veterans Affairs (2016), among other organizations. Data have also been published that are more consistent with behavior-analytic research methods and intervention focuses. Single-case and time-series analyses demonstrating the effectiveness of ACT have been published, in addition to several dozen studies utilizing overt behavioral or physiological measures (e.g., Castro, Rehfeldt, & Root, 2016; Gould, Tarbox, & Coyne, 2018; Szabo, 2019; Szabo, Willis, & Palinski, 2019). This empirical work is increasingly central to topics of concern to most BCBAs. For example, a search of the Web of Science reveals that ACT has been referred to in 32 articles on developmental disabilities or parent training. Indeed, articles in journals published by ABAI over the past 35 years include 98 references to ACT and 650 references to RFT.
There are indications that this body of work is increasingly penetrating the BCBA practice community. A growing number of ACT and RFT presentations are evident at ABA conferences, and in 2018, ABAI hosted a 1-day, single-track special event on ACT immediately postconference. Commercial ACT training workshops aimed at ABA practitioners, as well as a small number of books on applications of ACT to learners with ASD (the most common population served by ABA practitioners), have also emerged (Dixon, 2014; Dixon & Paliliunas, 2017). Recent revisions of BCBA competency standards increasingly point to the theoretical underpinnings and technologies central to ACT, as will be discussed later in the article. Finally, a chapter on RFT and ACT (Critchfield & Rehfeldt, 2020) was included in the most recent edition of the text Applied Behavior Analysis (Cooper, Heron, & Heward, 2020), which is widely considered the classic textbook on ABA.
Several contextual factors seem to be contributing to the increased interest in ACT in behavior analysis. As the number of practicing BCBAs grows exponentially (from just over 6,000 in 2010, to over 33,000 in 2018), so does the demand for evidence-based behavioral technologies that can meet the increasingly diverse needs of consumers seeking ABA-based treatment services. Practitioners often find themselves addressing complex behavioral repertoires that require innovative, higher level programming that goes beyond what they typically receive direct training in during the course of their graduate studies and supervised fieldwork. BCBAs are tasked with designing effective programs for (a) establishing and developing the verbal repertoires of clients and (b) addressing problematic patterns of behavior that tend to emerge with the development of such repertoires. In addition, the majority of a BCBA’s professional activities involve interacting with individuals with complex verbal repertoires (i.e., parents, teachers, staff, colleagues, and other providers), either directly (during observations, training sessions, phone calls, meetings, etc.) or indirectly (via e-mails, treatment plans, written notes, etc.). Thus, a functional understanding of language, as it occurs in typically developing adults, appears critical to a BCBA’s success. In short, the growing interest in ACT by BCBAs seems to be occasioned by client needs and consequated by its effectiveness in addressing those needs.
The growing interest in ACT from within the applied behavior-analytic community poses some potential practical and ethical challenges. ACT as applied within the traditional scope of practice of BCBAs has not been widely disseminated, and most BCBAs have not had significant training or experience in ACT or RFT. Some uses and forms of ACT are properly the realm of clinical psychology or other disciplines, but many others are perfectly suited to the profession of ABA.
ACT as ABA
The acronym “ACT” originally stood for “acceptance and commitment therapy,” but for the last 15 years, the term “acceptance and commitment training” has been used to describe applications of ACT in nonpsychotherapeutic settings (Hayes, Strosahl, & Wilson, 2011; Hayes et al., 2004). A search via Google Scholar shows that the term “acceptance and commitment training” has appeared over 1,000 times in the world’s scientific literature. Although the term “ACT” continues to be used by a wide range of professions, we will use the acronym “ACTraining” to more clearly distinguish between ACT as applied in psychotherapeutic or counseling settings and ACT as applied within the scope of practice of BCBAs. We are not suggesting that the term “ACT” is inappropriate for behavior analysts. We do, however, seek to emphasize the difference between ACT as a training method appropriately integrated into the work of BCBAs versus ACT utilized by psychotherapy or counseling professions.
According to the Behavior Analyst Certification Board (BACB; www.bacb.com), behavior analysis is the “scientific study of principles of learning and behavior,” consisting of the basic natural science of the experimental analysis of behavior and of the application of that natural science, ABA. Specifically, ABA is defined as a systematic approach for influencing socially significant behavior through the application of behavioral principles to the identification and manipulation of reliably related environmental variables. BCBAs provide services to improve organizational functioning (e.g., staff performance, employee training, management and compensation practices), skill deficits (e.g., communication, social behavior, health and wellness behaviors), and socially unacceptable behavior (e.g., aggression, self-injurious behavior). Thus, our most basic proposition is that ACTraining should be based in the same basic natural science and explicitly involve the application of the behavioral principles that extend from that work to the manipulation of the controlling environment in a way that improves socially significant overt behavior. Put simply, ACT as practiced within ABA should meet all of the same standards that define any other practice within ABA (e.g., Baer, Wolf, & Risley, 1968), and we discuss many such examples in this article.
Linkage to Behavioral Principles
ABA is characterized, in part, by its commitment to being conceptually systematic (Baer et al., 1968), meaning that behavior analysts observe and analyze behavior in context and design interventions from an understanding of the functional relationship between behavior and the environment, in terms of behavioral principles. The importance of remaining conceptually systematic is perhaps even greater when adapting interventions that were originally developed for practitioners outside of ABA (e.g., ACT interventions). After ABA practitioners have been substantially trained in the behavior-analytic conceptual analyses that form the core of ACTraining, they can then both (a) adapt traditional ACT methods for incorporation into ABA interventions and (b) create their own ACTraining interventions consistent with their own client-specific functional assessments. Understanding how ACT works in terms of behavioral principles allows the ABA practitioner to implement ACT functionally, rather than simply implementing procedures as pure technology. This is consistent with what ABA practitioners do when they use more mainstream ABA procedures, such as functional communication training, discrete-trial training, or natural environment training.
According to the ACT model, psychological flexibility is the ability to contact the present moment regardless of aversive thoughts and feelings based on the situation and one’s personal values (Hayes et al., 2004). Specifically, one identifies that the thought or feeling is only temporary and engages in behaviors that result in long-term value to one’s life. For instance, a parent may continue to place a tantrum on extinction, although she feels uncomfortable when hearing the crying and whining, to bring about more meaningful interactions with her child in the future. Psychological flexibility can be conceptualized as involving six functionally defined behavioral repertoires, all of which support one another. These six repertoires are typically described in “middle-level terms” (i.e., terms that serve to orient the behavior analyst to particular functional relations between the environment and behavior) and comprise the six points of the ACT hexlaflex: acceptance, defusion, present moment attention, self-as-context, values, and committed action (Hayes, Bond, Barnes-Holmes, & Austin, 2006). In what follows, we describe each of the six dimensions in two ways: (a) as repertoires of behavior that ACT is designed to strengthen and (b) as procedures used to strengthen these repertoires (much the same as “functional communication training” refers both to relations of reinforcement for communication and extinction for challenging behavior and to the procedures used to bring those relations about).
Values
Increasing valued living is described as the primary goal of ACT (Hayes et al., 2011). Behaviorally, values can be conceptually analyzed to be rules that function as verbal motivating operations that increase or decrease the effectiveness of stimuli as reinforcers or punishers, thereby supporting overt behaviors that produce those stimuli. Consider a BCBA who has been avoiding parent training sessions and engaging in negative thoughts (i.e., private verbal behavior) such as “I can’t believe I have to work with another uncooperative parent.” The BCBA may reflect on the situation by clarifying her values. For example, she might assert, “I am going to do whatever I can to ensure this child receives the best care possible, including taking on the challenge of supporting the parents who may not want to do everything I recommend.” If this small values intervention is effective in helping the BCBA engage the parent, the BCBA may then take the opportunity to implement a values intervention with the parent to help the parent move toward her values. For example, the BCBA could suggest the parent write her own unique values statement, such as “I care about being an advocate for my child.” These practices help transform the stimulus function of events that are otherwise aversive and that evoke avoidance responses. When the BCBA or parent in this example articulates an important value, aversive stimuli that participate in equivalence networks with the stated value acquire new, more appetitive stimulus functions. In the context of freshly articulated values, the parent is more likely to ask questions in individualized education plan meetings and the BCBA to make recommendations, even when they might be challenged by the parent.
Overall, values interventions may enable a BCBA to add powerful appetitive functions (or intermediary reinforcers) to an otherwise aversive situation, providing a parent, staff member, client, or teacher with the motivation he or she needs to persevere in the face of adversity. Values interventions thus support rule-following repertoires that are oriented toward larger, longer term positive reinforcers, versus short-term escape (Blackledge & Drake, 2013). For example, during an intake meeting, the BCBA might engage the parent in a values exercise such as “The Three Wishes” (Gould et al., 2018), where the BCBA asks the parent, “If you could have anything in the world for your child, what would it be?” to which the parent might respond with something like “I want my child to be able to express herself and to be safe.” The BCBA might subsequently link all treatment recommendations back to those parent values, potentially increasing the likelihood of securing buy-in and commitment to treatment protocols (e.g., “I want to introduce this augmentative and alternative communication [AAC] device in the service of helping Shanice express her needs and be understood, no matter where she is or who she is talking to.”), as well as reconnecting the parent with his or her values when things get difficult (e.g., “I am willing to go through this, in the service of Shanice being safe from harm, happy, and independent in the future.”).
Present Moment Attention
Present moment attention (often referred to as “mindfulness” or “present moment awareness” in the ACT literature) involves strengthening one’s repertoire of attending to stimuli in the present moment, while weakening one’s repertoire of attending to one’s own verbal behavior with respect to past, future, or imagined events. Present moment attention training thus aims to increase sensitivity to environmental contingencies and weaken unhelpful sources of verbal stimulus control. In practice, this involves evoking and reinforcing attention to different aspects of immediate experience. For example, parents might be taught to discriminate when they are “in the world” (i.e., in contact with direct contingencies) versus “in their heads” (i.e., primarily attending to private verbal stimuli, e.g., “I can’t do this”). The purpose of this training is to facilitate contact with overt environmental stimuli (e.g., the child seeking out the AAC device) that might occasion more adaptive parenting responses that support the child’s treatment (e.g., reinforcing the child’s use of functional communication), as opposed to engaging in avoidance (e.g., obsessively researching treatment articles online) in the presence of aversive private stimuli (e.g., feelings of grief about the child’s diagnosis and worry about the future).
Furthermore, present moment procedures involve training one to pay attention to one’s own attending behavior. In cases where one notices one’s attention wander, one redirects one’s own attending behavior back to present moment stimuli. Put differently, one learns to tact one’s own attending behavior, and the occasion of tacting wandering attention, itself, becomes a discriminative stimulus for redirecting one’s own attention back to the present moment, thus comprising a secondary repertoire of self-managing one’s own ongoing attending behavior (Skinner, 1953, Chapter 15). An everyday example of such behavior that is likely familiar to anyone who drives an automobile is when one suddenly notices that one is not looking at the road while driving and then redirects one’s own attention back to the road.
Acceptance
Acceptance can be thought of as approach behavior (or the absence of avoidance or escape) in the presence of aversive stimuli, thus creating a context for more varied and potentially more adaptive behaviors to occur and then contact natural reinforcers. Thus, an ABA practitioner might train acceptance anytime avoidance is interfering with the task at hand. In practice, this involves weakening rule-governed, negatively reinforced repertoires by directly evoking and reinforcing the ability to approach previously aversive events (public and private). For example, in the context of parent training, a BCBA might train a parent in acceptance while following through with an extinction procedure aimed at producing long-term positive (i.e., values-directed) outcomes, instead of engaging in typical avoidance behavior when the parent contacts aversive private events in the moment (the stress of seeing and hearing the child in distress).
In the context of parent training, BCBAs can model acceptance by saying things like “I know I’m supposed to be the expert, but honestly, doing extinction is really hard for me too. And it’s the stand that I’m willing to take for your child.” BCBAs can directly reinforce parents’ acceptance behavior by creating a supportive context for parents to choose difficult actions and then directly reinforce when they do so. For example, the BCBA might suggest during parent training, “I can see this is frightening to you. You’re worried about getting it wrong. How about we run the extinction procedure together today? You’re not alone. I’ll be here. We’re in this together.” As the parent begins to conduct the procedure, the BCBA might respond by saying, “I know that wasn’t an easy choice, and I’m impressed. Through your actions, you are showing that you are willing to do pretty much whatever it takes to help your child, and that’s pretty awesome. Let’s do this!”
In the case of a BCBA applying ACT procedures to one’s own self-management, if the BCBA is struggling with a challenging parent training situation and experiences aversive private events (e.g., feelings of frustration and thoughts such as “I can’t do this anymore!” or “This is pointless.”), rather than avoiding returning a parent’s phone call, the BCBA might take a few minutes to purposefully observe his or her feelings of frustration and the difficult thoughts he is she is having, and thereby “allow them to be there.” The BCBA might write down his or her thoughts on a Post-it and then state his or her willingness to talk with the parent by connecting to values (“Even though it feels pointless and frustrating, I’m willing to call this parent because I care about doing the best I can for this family, and I care about being a compassionate, responsive behavior analyst.”). Hence, a previously aversive situation now becomes an opportunity to contact reinforcement by behaving in a values-consistent manner.
Defusion
From a commonsense perspective, defusion is the embodiment of perhaps the most central of behavioral concepts: The mind does not control behavior. In contrast to how our mentalistic society has trained us all to believe that the mind causes behavior, and therefore that we should take our thoughts very seriously, defusion procedures are about teaching people to notice their private events for what they really are: just more stimuli in their environment. A behavioral conceptual analysis of defusion is considerably more complex and involves rule-governed behavior. The problem to which defusion is directed is referred to as “fusion” in the ACT literature and means overly rigid control of behavior by rules. Defusion, then, refers to a weakening of overly rigid rule control over behavior, such that other functions (verbally and nonverbally established) can come to bear. Defusion procedures thus seek to disrupt narrow, inflexible functions of a person’s private verbal stimuli (i.e., thoughts), so that a broader, more flexible repertoire of responding to those thoughts as private stimuli might be established. Thus, an ABA practitioner might train defusion anytime thoughts (i.e., private verbal stimuli) dominate attention, producing unworkable patterns of behavior. In practice, this involves training attention to the process of thinking. For example, if a client is continuously distracted from attending to school activities by thoughts that she is going to fail or “is dumb,” the BCBA might teach the child to playfully visualize thinking these negative thoughts as falling down a rabbit hole. Rather than continuing to fall down the hole, the student is taught to verbally “catch herself from dropping farther into the hole.” The student is thus taught to tact her negative thoughts as a “rabbit hole,” a context in which to reorient attention back to the task at hand.
Of course, for less verbally adept students, such talk is too abstract. With such students, it may be helpful to physicalize metaphors. In the previous example, the BCBA might teach the child to respond to her own negative self-talk by literally spreading her arms out to “stop” herself. If the social context of the classroom is not appropriate for the student to spread her arms wide, she could be taught to subtly spread her hands out slightly. In each case, responding to one’s own negative self-talk metaphorically can create a context for more variable behavior, rather than simply avoiding difficult social or academic situations that evoke the negative self-talk.
Defusion procedures generally disrupt the function of unhelpful rules by either adding neutral functions to those rules or by adding humorous functions. An example of adding a neutral function is imagining one’s thoughts as a radio stuck on “negative FM.” For example, consider a parent who tells the BCBA that he or she is having the thought “I can’t do extinction.” The BCBA might say something like
I know doing extinction is unreasonably difficult, and when we do it, our minds will inevitably tell us stuff that isn’t helpful. But what if it was possible to just notice our thoughts as just another thing in our environment, annoying and painful, but not always as directions that we have to follow. If you are willing, try taking a minute and imagining your extinction mind is like a radio that’s stuck on the station “I can’t FM.” It would be really irritating for your radio to be stuck like that, but you wouldn’t have to do whatever the DJ said, right? If you had to, you could keep doing what mattered, even with a really negative DJ talking in the background. Maybe it’s worth trying to imagine that while you implement extinction.
Of course, there is nothing special about the metaphor of a stuck radio station. The BCBA might use any other metaphor that is a familiar example of repeating messages that one does not necessarily have to listen to—for example, a stock market ticker tape, a sign being trailed by an airplane in the sky, or a broken record player.
An example of a defusion exercise that adds humorous functions to maladaptive verbal stimuli is where the BCBA asks the person to repeat the problematic thoughts (i.e., verbal behavior) in a silly voice. For example, if a child with ASD is having difficulty with losing a board game and says, “I can’t lose this game!” the BCBA might say something like
Look, I hate losing too. If you can win, awesome, then win. But when I can’t win, one thing that helps me is to repeat my thought back to myself but in the voice of Yoda from Star Wars. If I’m losing a game, and it’s driving me nuts, I might just say “Lose this game, I can’t!” [while talking in a silly accent that resembles the Yoda character]. Are you willing to give it a shot? Try it—just say something like Yoda.
At first the BCBA may have to provide echoic prompts and contrived reinforcement to teach the child to say his thoughts in a “Yoda voice,” and then fade prompts and reinforcement as the child continues to use the newly learned defusion skill. There is nothing about silly voices, per se, that are necessary for defusion to work. What matters is that, functionally, the practitioner helps the learner engage in some other more flexible and varied behavior in the presence of whatever rules are evoking avoidant behavior. In lay terms, defusion is about teaching learners to “not take their own minds so seriously.”
Self-as-Context
Self-as-context describes an awareness of oneself as the context for all of one’s experiences (i.e., observing that one’s behavior is distinct from other external and internal events; Levin et al., 2012). Behavior analytically, self-as-context might be thought of as a flexible perspective-taking repertoire. Viewed from the standpoint of RFT, self-as-context involves training flexible deictic relations of I/you, here/there, and now/then. In this way, self-as-context procedures involve shaping flexible, self-directed verbal behavior in the presence of private events that vary across time (e.g., memories of the past and concerns for the future), place (e.g., different situations, relationships, roles), and person (e.g., different perspectives on the same event). Thus, an ABA practitioner might train self-as-context anytime rules about the self (i.e., in lay terms, self-conceptualizations like roles, relationships, characteristics, and evaluations) limit flexibility and hinder values-directed overt behavior. For example, if a client defends his disruptive behavior by describing himself as a “class clown,” the BCBA might teach the child to consider (a) the different ways he might describe himself in different situations or at different times in his life and (b) the different ways others in his life (e.g., parent, favorite teacher, or friend) might describe him based on what they see. Similarly, if a father resists a behavior intervention plan and says something like “I’m just a softy; I can’t be strict like that,” the behavior analyst might say something like
I understand what you’re saying. You care about being sensitive to your child’s needs, and I appreciate that. And . . . when we are so focused on being a particular way, like being a softy and not being too strict, we might find ourselves trapped. It can make the current situation more difficult. When I get stuck on particular beliefs about the way I am, sometimes I try reframing it by noticing that these beliefs are just one particular way that I act in certain situations; they don’t necessarily have to dictate my action in all circumstances. There are times when I have the thought that I need to be perfect at my job. One trick I use on myself is to just restate my belief but with some added perspective. For example, I might say, “I notice I’m having the thought that I’m a behavior analyst that is supposed to have it all figured out.” Are you willing to give that a shot and see how it works?
Distinguishing Between Defusion and Self-As-Context
Behavior analysts new to ACT may find the distinction between defusion and self-as-context unclear. In lay terms, defusion targets unworkable rules and thoughts about the outside world, whereas self-as-context addresses unhelpful rules and thoughts about the self. Said behaviorally, defusion procedures weaken rigid control by rules that describe the environment outside of oneself, whereas self-as-context interventions weaken the influence of rules that describe oneself or others. Both classes of intervention seek to weaken excessively rigid rule control, one with respect to rules in general, and the other with respect to rules influencing perspective-taking behavior.
In practice, it is common for defusion and self-as-context procedures to overlap based on their shared roles in helping trainees identify that their thoughts, whether about themselves or not, do not need to control their actions. Topographically similar procedures could target the defusion repertoire or the self-as-context repertoire to produce functionally different outcomes. For example, when a runner looking to move from running half marathons to full marathons engages in the private verbal behavior “I’m never going to reach 26.2 miles,” she might use the defusion strategy of restating the thought as “I notice that I’m having the thought that I’m never going to reach 26.2 miles.” On a different day, that same runner engaging in the private verbal behavior “Maybe I’m just not the kind of person who runs marathons” might use the self-as-context strategy of restating the thought as “I’m a 40-year-old BCBA noticing myself having the thought that maybe I’m just not the kind of person who runs marathons.” Although they are almost identical topographically, the first example would be conceptualized as a defusion exercise because it is functionally targeting general rules about training, whereas the second would be conceptualized as self-as-context because it is targeting verbal rules about oneself as a person.
When they learn defusion and self-as-context skills, trainees begin to notice their thoughts and to respond to them in defused ways. Trainees can also be taught to recognize the stimuli in the environment that evoke the problematic self-talk, in order to cue themselves to engage flexibly with defusion or self-as-context skills. This is analogous to when BCBAs teach children with autism self-management skills—specifically, to engage in a functionally appropriate replacement behavior over one that is harmful to themselves or others.
Committed Action
Committed action is the ultimate goal of ACT and describes a response class of socially significant overt behaviors that move one in the direction of one’s stated values. All the other five behavioral repertoires described previously serve to create a context for a person to engage in larger and larger patterns of values-directed committed action. Training committed action involves training (a) the discrimination of aspects of the immediate context related to values and (b) the engagement in values-consistent behaviors as appropriate to that context. Throughout treatment, a BCBA might encourage a client to identify and tact the function of his or her current behavior (e.g., “I’m trying to quit the game because it looks like Michelle is going to win.”) and then identify specific behaviors that the child might immediately engage in that are in line with his or her values (e.g., “I want to be a good friend, and friends play games together, even though someone loses.”), in addition to supporting the child in selecting realistic goals to target outside of treatment sessions (e.g., “I want to bring a game that I’m good at next time and teach Michelle.”). The BCBA would also seek to prompt and reinforce the child’s flexibility repertoire more broadly (i.e., defusion, acceptance, present moment awareness, and values), when private events arise that previously derailed values-consistent action.
In the context of parent training, a BCBA might directly instruct that committed action is the desired end point of the training process and set up a context for a parent to create his or her own goals, oriented to his or her own values. For example,
Look, I could tell you what to do and why I think you should do it. But, honestly, that’s not what parent training is about. This process is about me giving you skills to decide what you want to stand for with your child and what you are willing to do about it. We’ve talked already about values, and you chose “helping your child get the most out of life” as your value. I want you to take a few minutes and write down three different ideas you have about small but meaningful ways you could change your behavior this week that would help your child move toward that value. When you are done, let’s get back together and narrow the list down to just one thing that you can commit to doing, the date and time you are going to do it, and who in your life you are going to report it to when you get it done.
The BCBA might then give the parent a worksheet, calendar, or planner or encourage the parent to make his or her own, so that the committed action can be put in writing and then shared with relevant family members, and so on. A variety of ready-made committed action worksheets are available to download for free off of the World Wide Web—for example, the “Mindful Action Plan” (Moran, 2014), and the “Willingness and Action Plan” (Harris, 2008). As we know from the performance management literature, goal setting works much better if it is followed up with feedback on how well the parent met the goals the next time the BCBA and the parent meet, ideally within the next week or two (Alvero, Bucklin, & Austin, 2001).
Combining the Six Processes
The overall goal of ACT is for the trainee to build behavioral flexibility through strengthening the six skill repertoires. Although each skill is conceptualized as equally important, each may not require equal attention at any given time or with any given trainee. As with any other skill acquisition target, the ACT trainer can probe to identify skills that are already at strength in the trainee’s repertoire. The BCBA may ask the trainee to talk about his or her thoughts and emotions as “barriers” to desired behavior change, and based on the trainee’s response, the ACT trainer can then prioritize which ACT skills to train first. We address this process further in the section on functional assessment that follows.
RFT: The Engine That Powers ACT Interventions
The verbal relation expressed in the title of this section is best described as an analogy: RFT is to ACT as engines are to automobiles. Readers unfamiliar with RFT and ACT will no doubt recognize that engines propel cars, and thereby derive that RFT must do the same for ACT. In doing so, readers engage in arbitrarily applicable relational responding (AARR; Hayes, Barnes-Holmes, & Roche, 2001). AARR is verbal behavior in which stimuli unrelated by virtue of form or topography (e.g., the words RFT and engine) are related in accordance with verbal cues that are themselves unconstrained by physical dimensions or properties (e.g., the word “EQUALS”). RFT constitutes the basic account by which humans learn not only to respond to words but also to rapidly build verbal relations, sets of relations, and networks of correlated relational sets.
To illustrate, consider the conditional discriminations one might quickly make given the analogy that RFT is the engine that powers ACT. If RFT powers ACT, then verbal behavior theory powers the picture exchange communication system (Bondy & Frost, 2001), behavioral momentum theory drives several treatments for noncompliance (Mace et al., 1988), and matching theory propels ABA approaches to classroom management (Neef, Mace, Shea, & Shade, 1992). Further, it follows that many ABA interventions are torqued by theories derived from the experimental analysis of human behavior and that practitioners who have an educational background in basic research have a much more powerful engine with which to travel into applied settings.
By itself, RFT has relevance to ABA because it is testable, and those aspects of the theory that have been investigated in basic labs have easily found their way into applied programs of research and practice (e.g., Barron, Verkuylen, Belisle, Paliliunas, & Dixon, 2019; Dixon, Blevins, Belisle, & Bethel, 2019). But the importance of RFT as a theory extends beyond an account of how verbal relations rapidly generate. It also explains the way verbal relations learned in accordance with one type of discriminative cue transform in function as fast as they are initially formed. This feature of verbal learning, referred to in the RFT literature as the transformation of stimulus function, is implicated in a class of psychological suffering that only those with verbal capacity experience, and it is in this way that RFT’s account of human language is the engine of all ACT interventions.
By way of example, imagine that Peter, a 14-year-old, is your most delightful neighbor and is a tremendous musician. Peter is friends and in a band with Zack, whom you have not met, though he also lives in your neighborhood. Zack is close friends with Hank, who you do not know. Because of your previous relationship with Peter, you derive that Zack must be delightful because he is close to Peter, and so must Hank, because he is close to Zack.
Upon talking to your police officer friend, however, you learn that Hanck and a few friends have recently beaten up elderly people in his neighborhood to steal their money and buy musical equipment for their rock band. Immediately, without any further information, you derive that Zack and Peter are the friends Hanck was with when attacking the elderly people. Until this time, you have related to Peter, and by extension to Zack, as delightful, but this one bit of information, in which neither child has been named directly, leads to a transformation of their function from delight to disgust. This change in respondent function is likely to be accompanied by a change in discriminative and reinforcement functions associated with their names. That is, the mention of their names could occasion you to prepare questions for them about how they earned the money for their musical instruments. Any hesitation in their answers would reinforce your decision to ask and provide additional discriminative stimuli for behavior that would be reinforced by their leaving your neighborhood. At that point, it is likely that you will experience pain that reemerges at strength at a much later date when you meet a new teenager who is a gifted guitarist. It is of relevance here that the pain you experience at this point in time is a product of your verbal relating, and not of any interaction with the new person in the current context. Thus, RFT constitutes a basic account of verbal learning, and ACT, as a course of treatment, is designed to deal with the psychological problems that human language produces (McEnteggart, 2018).
The Seven Dimensions of ABA
When asking the question of how ACTraining fits in the scope of practice of ABA, a logical question is how it fits into the seven dimensions that define ABA (Baer et al., 1968). We have written about this elsewhere (Szabo & Tarbox, 2018), but we will touch on some key discussion points here.
Applied and Behavioral
The goal of ACT is to improve socially meaningful, operationally defined overt behaviors that help clients move in the direction of their chosen values. According to the criteria set forth by Baer et al. (1968), ACT is both applied, in that it addresses socially important problems, and behavioral, in that it focuses on changing overt behavior. Private events are addressed in the process but only to teach clients more flexible, productive skills for responding to their own private events, not to change those private events or to give them causal status in any way. For example, a parent might report that he or she has the thought “I can’t just ignore the behavior and watch him cry.” This thought, as a privately occurring self-rule, may indeed have a negative influence on the parent’s implementation of an extinction procedure for his or her child’s attention-maintained behavior, just as an overtly stated rule could. The goal of ACTraining would not be to target the content of that rule, but rather to encourage some variability and flexibility in how the parent engages with it, for the purposes of increasing the probability of implementing attention extinction. That is, the ACT-informed ABA practitioner is concerned with how the rule functions for the parent in that particular context, not with changing or eliminating the rule or any other private behavior. Further, if teaching the parent new ways of responding to that rule does not help improve the parent’s overt behavior of implementing extinction, then the change is insufficiently large and not one that ACT work strives to produce.
Similarly, if a behavior analyst was using a values-based ACTraining intervention aimed at increasing the frequency at which direct care staff fill out their time sheets in a timely manner, the goal of the intervention would be overt behavior change, not a change in private “meaning and purpose,” per se. In order to use a values intervention, the BCBA may hold a staff meeting with direct care staff and talk about the shared values that are meaningful to the staff in their daily work. Imagine in this case the staff identify “helping children achieve their greatest potential” as their highest value for showing up for work. The BCBA leading the meeting might start by acknowledging how difficult and tedious paperwork can be, and then link the overt behavior of filling out time sheets to the value of helping children achieve, by discussing how paperwork allows clients to access continued funding for their treatment, as clients must continue to get treatment if they are to achieve their greatest potential. The BCBA might pose the question “Is it worth it to be bored and irritated out of your mind while you do paperwork, if that’s what it takes to give these kids a better life in the future?” The goal of such a discussion is not to change how staff think about time sheets, but to produce a change in the overt behavior of staff filling out time sheets, especially in the presence of aversive emotional states (e.g., boredom and frustration) and unhelpful self-rules (e.g., “I hate time sheets. I didn’t get into this line of work to spend time on pointless paperwork.”). Again, if the overt behavior does not improve, additional intervention components would need to be added until a socially meaningful change in behavior is produced.
Effective
The insistence within ACT on producing overt behavior change that is large enough to produce a meaningful improvement in the learner’s life is the very definition of the effective dimension of ABA (Baer et al., 1968).
Conceptually Systematic
As we described in the section “Linkage to Behavioral Principles,” ACTraining, when practiced by well-trained behavior analysts who are guided by behavioral principles, is conceptually systematic. The procedures that comprise ACT were conceptualized from the standpoint of behavioral principles from the beginning, and basic behavioral principles are taught in most ACT treatment manuals. Of course, it is possible for poorly trained practitioners to rotely implement ACT procedures as pure technology, without an understanding of how and why they work in terms of behavioral principles. But that is, of course, also possible with any other ABA procedures, such as discrete-trial training and functional communication training. It is probably accurate to say that it is more challenging to conceptually analyze and understand all of ACT in terms of behavioral principles, as compared to more mainstream ABA procedures, but that is likely because the human behavior involved in ACT is relatively more complex, not due to ACT, per se.
Generality
The goal of establishing generalized behavior change is at the heart of all ACT work, in that the goal is never to establish specific topographies of behavior under specific instances of stimulus control. Rather, the goal of ACTraining is to strengthen generalized operant repertoires that are then portable for learners to take into any relevant aspects of their daily lives. For example, if parents are trained to monitor their own behavior in implementing their child’s behavior plan in the service of helping their child live more independently (comprising present moment, values, and committed action repertoires), then parents might also track their daily behavior of putting away their own smartphones while playing with their child, in the service of fostering intimacy and joy in daily life (also present moment, values, and committed action repertoires).
ACTrainers also address generalization within the training process itself and look for trainees to derive their own untrained examples of behavioral flexibility. For example, if an ABA therapist is sharing with his or her BCBA during a supervision meeting that he or she is stressed out by driving in traffic and not sure if he or she can take it anymore, the BCBA might try to promote an acceptance repertoire by saying something like “I wonder if trying not to feel stressed while driving in rush hour traffic might be a little bit like trying to avoid drowning by struggling in quicksand.” In assessing generalization, the trainer might look for the ABA therapist to demonstrate a derived extension of the metaphor; for example,
So you are telling me I need to open myself up to the traffic and just lay flat on top of it? That sounds insane, but I guess it actually makes sense, in a nonliteral way. Maybe instead of fighting my way through traffic like I have been, I can try floating through it on a surfboard.
Or perhaps the ABA therapist might derive a new metaphor that is functionally the same; for example,
Quicksand—OK, I get it, or maybe it’s like trying to stay dry with an umbrella in a hurricane. Maybe I’ll put an umbrella on the passenger seat of my car to prompt me to practice acceptance of stress while driving.
Of course, inducing people to merely talk like an ACT trainer is not the goal of ACTraining; changes in socially relevant overt therapist behavior must also be evaluated, such as decreases in staff callouts or turnover related to burnout.
To sum up, producing generalization is so fundamental to all ACT work that it cannot be considered a distinct phase or goal of treatment, separate from initial acquisition. The demonstration of generalization across aversive events, across and within ACT self-management repertoires, and across committed actions is evidence of mastery.
Analytic
ACTraining is analytic in the sense that BCBAs practicing ACTraining are equally responsible for evaluating whether or not ACTraining procedures were responsible for observed behavior changes, just as they are with any other ABA procedures. Careful data collection and some attempt at single-case experimental design, even in the context of everyday practice, are as critical to ACTraining as they are to any other area of specialty within ABA practice.
Technological
Perhaps the least straightforward dimension of ABA is the status of ACTraining as technological. Like any other scientific procedure, it is critical for ACTraining procedures to be clearly defined so that they are replicable. It is likely fair to state that this is a dimension in which ACTraining requires further development, perhaps largely due to the fact that it is a relatively new area of practice within ABA. Still, manualized protocols for ACTraining inside ABA exist (Gould et al., 2018; Szabo, 2019; Szabo et al., 2019), as well as curricula with clearly defined exercises (Dixon, 2014; Dixon & Paliliunas, 2018).
To recap, we suggest that ABA practitioners use ACT as a tool with which to target socially important, observable, measurable behavior and hold themselves accountable for analyzing the extent to which their results are due to their intervention, and not some other environmental event. ABA practitioners using ACT should further demonstrate that their results are powerful enough that others should see their relevance and durable enough to warrant moving on to other goals. They should then make certain to write out what they do in a way that allows anyone with the instructions and adequate training to perform the treatment and obtain similar results. Lastly, ABA practitioners should be prepared to describe to other professionals the basic principles (i.e., reinforcement, AARR, etc.) that are the necessary and sufficient ingredients to explain the strength of the intervention results obtained.
ACTraining and the BACB Task List
One way to organize a discussion of scope of practice of a discipline is to reference the description of practice provided by the profession’s credentialing body. The fifth edition of the BACB Task List (BACB, 2017), hereafter simply referred to as the Task List, provides an overview of the knowledge and skills that serve as the foundation for the BCBA and Board Certified Assistant Behavior Analyst examinations. The Task List is organized in two major sections: “Foundations,” which includes underlying principles and knowledge, and “Applications,” which includes skills and procedures. When implementing ACTraining inside ABA, all of the Task List items are relevant, because one is, indeed, practicing ABA. ACTraining is best conceptualized as a supplement to more mainstream ABA practices, not as a replacement for anything on the Task List. However, some of the items on the Task List are especially relevant to the six sets of functional relations and procedures that constitute ACT work. In what follows, we note several of these Task List items and discuss how they are the active ingredients in ACTraining.
Functional Assessment
Conducting descriptive functional assessments is included in the Task List (BACB, 2017, Content Area F-7), and taking a functional approach to changing behavior has been considered a best practice for at least a few decades in the realm of assessment and treatment of challenging behavior (Iwata, Dorsey, Slifer, Bauman, & Richman, 1982). Functional assessment is also the foundation ACT, given that it is an intervention based on a functional analysis of language and avoidant overt behavior. Functional assessment of such behavior may include direct descriptive observations (e.g., antecedent-behavior-consequence data), as well as indirect descriptive assessment (e.g., interviews). Assessment efforts in ACTraining attempt to identify socially meaningful overt approach behaviors that are happening too infrequently and other escape-maintained behaviors that are occurring too frequently. For example, a trainer may engage in too much small talk while observing a trainee because it results in avoiding having to give meaningful corrective feedback on the trainee’s performance that could be improved. If a clinical director identified this pattern of behavior through direct observation, she might then follow up with an interview of the trainer, asking why he did not provide feedback during his session with the trainee, and perhaps asking if there was anything in particular he was thinking (i.e., a covert rule) that might be getting in the way. The trainer might identify something along the lines of “It’s the trainee’s first week, and I’m afraid that if I overwhelm him with too much feedback, he might quit.” Such a statement might identify a rule that supports the maladaptive avoidant behavior of excessive small talk and suppresses the adaptive overt behavior of giving effective feedback.
In addition to generally attempting to recognize and assess avoidant behavior, ACT functional assessments focus on identifying problematic functional relations that map onto the behavioral conceptual interpretations of the six ACT processes described in the “Linkage to Behavioral Principles” section of this article. Developing procedures for functional analysis inside of ACT is still in substantial need of empirical research, but a brief description of some common practices is warranted. When conducting indirect functional assessments by interviewing clients, the behavior analyst can look for evidence that might suggest one or more of the six ACT processes to be relevant. To identify acceptance as a potential area to target, the BCBA looks for verbal behavior that tacts aversive experiences for the trainee. For example, when a BCBA asks a parent to describe the difficulty with implementing extinction, the parent might reply, “I just can’t take him being upset.” To identify defusion as a potential area to target, the BCBA looks for a description of rules the trainee may be rigidly adhering to. For example, a parent might report, “I just know it’s not going to work; nothing ever works for him.” To identify self-as-context, the BCBA looks for verbal behavior focused on statements about who the trainee is; for example, the parent might say something like “I believe what you are suggesting works for some parents, but I think I’m just not that kind of parent.” To identify present moment attention as a potentially fruitful repertoire to target, the BCBA listens for descriptions of attending behavior that are focused on the past or the future; for example, “I just can’t focus on this behavior plan; all I’m thinking about is how frustrated I am that he has been acting like this for years and hasn’t gotten better.” To identify values as a potential repertoire to work on, the BCBA looks for verbal behavior that describes a lack of perceived positive reinforcement for the desired behavior; for example, the parent might say something like “I just don’t get why we are doing this.” Finally, to identify committed action as a potential area to target, the BCBA looks for the trainee describing a lack of clarity on which overt behaviors to engage in toward his or her stated values. For example, the parent might say something like “I just don’t even know where to start; it all just seems like too much.”
In sum, using both direct and indirect descriptive functional assessments of the problematic functional relations that could be interfering with values-directed behavior, the BCBA then identifies behaviors and relations that can be targeted with ACT procedures, as part of the Task List components described throughout this article. More future research is needed to identify potential procedures for conducting brief experimental functional analyses for prescribing ACTraining strategies.
Rule-Governed Behavior
The Task List requires that BCBAs define, provide examples of, and use rules to change behavior (BACB, 2017, Content Area G-6). Given that BCBAs primarily interact with highly verbal humans (i.e., parents and staff), it is impossible for BCBAs to avoid rule-governed behavior. The functional distinctions among types of rule-governance (i.e., pliance, tracking, augmenting) emerged from the earliest work on ACT and RFT itself (e.g., Hayes, Zettle, & Rosenfarb, 1989). ABA practitioners can thus readily adopt conceptual analyses and procedures from the ACT literature to establish or diminish rule-governed behavior and to accomplish other Task List goals such as to foster generalization or to facilitate maintenance.
Establishing flexible rule control in circumstances where rigid rules are not workable is clearly within the scope of practice of BCBAs. Procedures designed to foster defusion are examples of methods focused on rule-governed behavior that ABA practitioners can adopt from ACT. For example, while training a parent of a child with autism to implement extinction with the child, the parent might say to the BCBA, “I can’t ignore this! He needs to understand he doesn’t get to call all the shots around here!” The BCBA might use defusion strategies to diminish the impact of ineffective rules of this kind. In this case, the behavior analyst might say,
I know this is really difficult. So much of what I’m asking you to do goes against how you’ve learned to parent. I wonder if you’d be willing to notice with me, out loud, during our practice today, when I’m saying one thing, and you’re having thoughts like “Nope! That won’t ever work!” or “That isn’t right! He can’t just get away with this!” And if I notice you look stuck, I could ask what your mind is up to.
If the parent agrees, the BCBA would model, instruct, prompt, and reinforce not only the parent adhering to the planned ignoring procedure, but also the parent noticing the presence and function of his or her covert verbal behavior. Such an intervention could be one for rule-governed behavior to the extent that it effectively prompts the parent to engage in alternative, variable forms of rule-deriving (e.g., tracking the effectiveness of ignoring) and sets the occasion for variable forms of overt behavior, rather than the parent immediately avoiding implementing extinction, as he or she has in the past.
Eilers and Hayes (2015) used defusion procedures to weaken maladaptive rules surrounding rigidity and accompanying challenging behavior in children with autism. The participants displayed rigidity with routines—for example, having to go first or not letting a train track be dissembled—with overt verbal rules (e.g., “The track can’t break!”) and overt challenging behaviors that occurred if adults did not follow their rules. The defusion procedure consisted of teaching the children to state their rules repeatedly in silly voices while their rules were broken (e.g., other children played with the train track or took it apart). Results showed, in the first experiment, that combining defusion with exposure effectively decreased problem behavior and, in the second experiment, that defusion combined with exposure was more effective than exposure alone. An analysis in terms of rule-governed behavior would suggest this procedure would work because it adds additional functions to the rules and because it creates the opportunity for the learner to engage in other behaviors (as opposed to following the rule), which can then come in contact with adult-delivered consequences (e.g., praise), as well as natural consequences (e.g., playing with others in varied and fun ways). Therefore, defusion likely works because it decreases the effectiveness of rules to control behavior in old ways and helps establish alternative behaviors.
At times, staff or practitioner behavior suggests rigid rules that tend to reduce sensitivity to direct contingencies by interfering with effective overt behaviors, including behaviors relevant to their work. For example, a staff member might report to the supervising behavior analyst, “I really don’t think there’s anything else I can do with this parent. She’s just so stubborn and needs everything to be her way.” If the supervisor then observes the staff member failing to reinforce the parent’s appropriate questions or attempts during skills training, the supervisor might hypothesize that a rigid self-rule may be undermining successful staff behavior. In addition to fostering defusion, the ABA supervisor might train perspective-taking to weaken the dominance of rigid rules about oneself or others and establish more flexible behavior in the face of whatever contexts typically evoke the problematic rule. For example, the next time the staff member expresses similar frustration, the supervisor might say, “I wonder what it is that keeps her coming back here and trusting you when she’s clearly struggling to do it right.” This, and the discussion that follows, might be an intervention on rule-governed behavior, to the extent that it evokes the staff member taking the perspective of the parent. For example, the staff member’s affect might soften, and he or she might say, “I mean she really loves her kid. She’s probably really scared and wants him to be OK. She just gets so frustrated!” If the intervention functions as intended, it will then set the occasion for the staff member to discriminate both the parent’s affect and the staff member’s effective responding, such that the staff member can respond with greater sensitivity during training. Such an intervention would also likely be made more effective if the BCBA helped the staff member set a measurable goal for committed action—for example, “catching the parent doing well” and praising her.
Perhaps the most straightforward way in which ACTraining involves rule-governed behavior is in the link between values and committed action. As described earlier, values interventions involve describing long-delayed, global classes of positive reinforcers (e.g., “my child being able to live a full and meaningful life”), and committed action involves stating specific behaviors one is going to engage in, the antecedent conditions under which one is going to do them, and how the behaviors are connected to a chosen value. For example, a parent might write down on a parent training worksheet,
I am committing to running at least three 10-minute natural environment training sessions per week with my child, on Monday, Wednesday, and Friday evenings, to work on generalizing the mands she is learning in her ABA program, because learning language is going to help her live a fuller and more meaningful life in the long run.
Such a committed action statement is a relatively straightforward example of Skinner’s (1969) definition of a complete rule, which describes the antecedent (Monday, Wednesday, and Friday nights), the behavior (running sessions), and the consequence (the child living a meaningful life).
Derived Stimulus Relations and Equivalence
The Task List requires that BCBAs be able to define and give examples of derived stimulus relations and use equivalence-based instruction (BACB, 2017, Content Area G-12). Derived stimulus relations and equivalence have always been foundational to ACT work. One example is in addressing experiential avoidance. Experiential avoidance is overt or covert behavior that has the function of avoiding uncomfortable thoughts, feelings, or situations (Gould et al., 2018). Such behaviors can lead to successfully avoiding difficult situations temporarily, but generally do not result in positive long-term effects. For instance, the parent uncomfortable with following through with demands to address her child’s problem behavior may cancel a parent training session. By canceling the session, she may avoid spending the hour contriving opportunities to follow through with demands or have to wait out the tantrum; however, this avoidance will only create a temporary solution and does not address the long-term goal. The next day, week, and month later, the child’s tantrums may persist, and precious learning opportunities may be lost.
Measures of experiential avoidance (e.g., Bond et al., 2011) are highly predictive of behavioral trajectories over several years (e.g., Spinhoven, Drost, de Rooij, van Hemert, & Penninx, 2014), including overt measures such as work absence (e.g., Bond et al., 2011). Research on equivalence classes and derived stimulus relations shows that experiential avoidance is due in part to the equivalence relation derived between emotions and verbal evaluations. For example, the statement “anxiety is bad” has long been an item on the most common self-report measure of experiential avoidance (Bond et al., 2011; Hayes et al., 2004). Laboratory tests of the strength of equivalence relations show that people who are highly experientially avoidant are more likely to have derived a strong “anxiety–bad” equivalence relation (Levin, Haeger, & Smith, 2017). The strength of this equivalence relation in turn predicts actual behavioral performance in anxiety-producing tasks and moderates the relationship between increased physiological arousal and premature task termination. In effect, this equivalence relation undergirds a verbal rule that is known to have a dramatic negative impact on response flexibility and sensitivity to direct consequences of responding (see Chawla & Ostafin, 2007, for a review). Because rule-based insensitivity to direct consequences of responding transfers through equivalence relations (Monestes, Greville, & Hooper, 2017), it makes sense for behavior analysts to undermine the aversive functions of anxiety that were transferred via the “anxiety–bad” relation.
One way that a behavior analyst might undermine the functions within such a relation would be to contrive an exercise that produces anxiety that is at the same time humorous and playful. Szabo (2019) showed children that tantrummed when game rules were changed during ABA sessions a bowl of ice and asked if they thought whether it would be painful to hold their hand at the bottom of the bowl. Participants replied that they thought it would be painful, and the experimenter then said, “In a moment, I’m going to ask you to do that. What are you feeling now?” The participants said that they felt nervous and related it to the nervousness they felt when game rules were changed and made more difficult. After this initial equivalencing task, the participants were then asked to hold a hand under the ice for as long as they could and instructed “not to allow themselves to feel cold under any circumstances.” Participants were timed, and there was no immediate feedback. Next, they were asked to draw a hamburger with all the things they liked on it. Then they were asked if, in order to be able to have this amazing burger, they would allow someone to put some broccoli on it, and they were asked to draw this too. This exercise was debriefed and followed with a second effort at holding a hand under the ice, except this time the participants were instructed to be curious and marvel at the sensation of being cold. Again, they were timed, and the event was debriefed. In the second instance, children held their hand in the ice for nearly twice as long and said that it was fun. They were then asked if they thought that sometimes things that they were asked to do could be more difficult and scarier than what they had done in the past, and more fun too. The importance of the exercise was that it added new context to the initial “anxiety–bad” relation in a functionally novel manner, thus transforming it from a rigid relation to one that could be shaped, given the right context.
Motivating Operations
The Task List (BACB, 2017, Content Area G-2) states that behavior analysts define motivating operations and use them in their daily practice to help maximize the effectiveness of reinforcers for adaptive behaviors and minimize the potency of reinforcers for maladaptive behaviors. Experimental research has shown that stimuli involved in stimulus equivalence classes can function as establishing stimuli, or “motivational augmentals” that alter the function of delayed consequences and immediately evoke overt behavior with respect to these outcomes (Ju & Hayes, 2008). A BCBA making use of an augmental with an athlete whose preparation is waning a few weeks before a competition might say, “Can you imagine how good it will feel to be at your best during the comp?” thereby increasing the salience of the remote outcomes of participating in athletic drills (Szabo et al., 2019).
Values work is one such example drawn from ACT. Values are a particular variety of stimuli that verbally establish or enhance the functions of other stimuli. Said in another way, values can function as augmentals. For example, ABA practitioners could help parents identify values (e.g., intimacy and belonging) and then generate goals and objectives for treatment based on those values (e.g., spending time playing with their child each day). Each potential procedure could then be examined in terms of not only how it might meet a particular goal or objective but also how it serves the value. For example, during the first stage of behavioral skills training (i.e., discussing the rationale of the procedure one is about to train) for an extinction procedure for tantrums, an ABA practitioner might describe how implementing extinction opens up the possibility for intimacy and belonging. In addition, throughout training, the ABA practitioner might return to this value (e.g., “This next part will be a really tough part of the intimacy journey.”). Such an intervention could serve to improve engagement in difficult extinction procedures, to the extent that this transforms the aversive functions of implementing extinction. Put more simply, values interventions may function as verbally mediated motivating operations, through the transformation of stimulus functions, due to the derived relational responding involved. In addition, BCBAs might establish themselves and the treatment setting as valuable through pairing, because the reinforcing and motivating functions of values might transfer to everything else present, including the treatment team. In this way, the context of treatment might start to function as a motivating operation for increased engagement in values-directed behavior. A recent multiple-baseline study demonstrated, for example, that the use of ACT procedures for increasing values clarity was associated with increases in overt values-directed parent behavior in parents of children with autism (Gould et al., 2018). Importantly, in this study, gains were not only maintained posttraining, but the greatest effects were observed more than 6 months posttraining.
Self-Management
The Task List requires that behavior analysts know how to use self-management procedures (BACB, 2017, Content Area G-20). Skinner (1953) conceptualized self-management as involving secondary repertoires of behavior that are acquired and maintained because they help one’s normal ongoing behavior be successful (i.e., more likely to be reinforced). A simple example is how the behavior of making a grocery list increases the probability that the behavior of shopping will result in reinforcement. Similarly, the behavior of using a calendar at work increases the probability of engaging in the behavior of showing up for meetings one is required to attend, and therefore increases the probability of reinforcement. The six repertoires of behavior that make up the ACT hexaflex can usefully be considered six self-management skills, in that strengthening each of them may help an individual be more successful at obtaining long-term positive reinforcement, referred to as “values.”
Present moment training procedures can be used by ABA practitioners to train individuals in the self-management behavior of noticing one’s own attending behavior. For example, parents might be trained to tact when they are “here and now,” versus when they are “in their heads,” in the context of managing their child’s behavior. The rationale for this is that, if parents are attending primarily to present moment stimuli (their child’s behavior and their own behavior), they are going to be more successful at implementing a behavior intervention plan than if they are attending primarily to other stimuli (e.g., their own private verbal behavior about how hard it is). Such training often starts with a less stressful and less effortful approximation, such as engaging in daily tasks with greater attention to sensory stimuli, such as washing dishes while noticing the temperature of the water, noticing the feeling of the soap on the hands, noticing the sounds of the dishes colliding with one another in the sink, and so on. The purpose of this training is to alter actions of observation and labeling (i.e., the behavior of attending) that augment or diminish stimulus control over other behaviors.
Szabo (2019) asked children who were preoccupied with thoughts about games with difficult rules to walk quietly and in sync with an experimenter, who alternately took large slow steps, wide slow steps, tiny rapid steps, fast large steps, and so on. Following this, participants were asked to continue to walk in silence but to list all the smells, sounds, colors, and textures that they came into contact with that they had not previously noticed. In the debrief, participants were encouraged to list times when this could be useful, including times when things were uncomfortable for them in other respects. Later, they practiced (a) noticing what they wanted to do the moment that rules to their favorite games were made more difficult by their instructor, (b) asking for a turn at changing the rules, and (c) observing the outcome. In this experiment, the practice of pausing and bringing attention to the present moment served as a precursor to effective self-management. As an adjunct to other direct contingency management procedures, this mindfulness strategy was effective at bringing learners’ behavior under relevant stimulus control.
The use of mindfulness methods to foster self-management has been shown to be beneficial with populations commonly served by behavior analysts. For example, mindfulness strategies have been shown to help those with developmental disabilities successfully maintain their community placement (e.g., Singh et al., 2007), improve parent training outcomes (Blackledge & Hayes, 2006), decrease challenging behavior of adolescents with autism spectrum disorder (Brazeau et al., 2017), and improve client affect after mindfulness training for staff (Castro et al., 2016; Chancey et al., 2019).
The committed action components of ACTraining also fall squarely under the category of self-management. Many committed action procedures train learners to state the behaviors they intend to engage in, what particular value they are in the service of, when they are going to engage in the behaviors, how they are going to track the behaviors themselves, and whom they are going to report to—for example, the “Mindful Action Plan” worksheet (Moran, 2014). Stating goals, self-monitoring progress toward goals, and reporting on progress to others are key defining components of self-management in classic ABA texts (Cooper et al., 2020).
Goal Setting
Setting socially meaningful behavior change goals is featured on the Task List (BACB, 2017, Content Area F-3) and, when done in collaboration with a client, is another well-documented procedure in behavior-analytic research to promote behavior change. Controlled research has found that goal setting is more powerful in producing actual behavior change when it is combined with values work (Chase et al., 2013). If the function of behavior that achieves treatment goals is centered around avoidance, the BCBA may inadvertently strengthen an avoidant repertoire. For example, setting the goal of “my child always being happy” might lead the parent to allow the child to continuously engage in perseverative play or problematic self-stimulatory behavior, and avoid following through with skill development targets aimed at broadening the child’s play repertoire. In contrast, the BCBA might promote and maintain adaptive, more flexible repertoires of parent behavior by framing treatment goals in terms of parent values. Teaching the child to play with a variety of toys and games may initially evoke strong emotions and a variety of avoidant behaviors on the part of the child. That said, the parent may be willing to persevere with implementing the treatment program if the BCBA frames the goal in terms of expanding the child’s interests, finding more things he enjoys, and giving him more choices with respect to how he spends his time, ultimately leading to a richer, more joyful life. The BCBA might also frame the play goals in terms of fostering dignity by teaching the child to interact appropriately with age-appropriate toys and games, and connection to their community, by increasing the child’s ability to interact with and share experiences with others.
Client Preference and Social Validity
The Task List requires that behavior analysts recommend intervention goals based on client preference and social validity (BACB, 2017, Content Area H-3). Assessing a person’s individual values always requires asking the person what matters to him or her, which is the heart and soul of social validity (Wolf, 1978). In addition, ACTraining work always involves asking individuals to come up with their own committed actions, based on what they believe moves them toward their values, which is again a clear example of building social validity assessment into the identification of the goals of intervention.
Modeling
The Task List includes the use of modeling as a foundational behavior-analytic procedure (BACB, 2017, Content Area G-5). When incorporating ACT into daily ABA practice, behavior analysts should model flexible behavior when interacting with others. Behavior analysts can model acceptance with respect to their own and others’ difficult private events that arise during the course of treatment. For example, when introducing a new behavior intervention plan that evokes distress and challenging behavior in the child (i.e., produces an extinction burst), the behavior analyst can model acceptance, values, and committed action for staff by tacting that discomfort and not escaping or avoiding. In doing so, the behavior analyst might say something like
Honestly, this could be a really tough session. You don’t need to feel like you have it all figured out. I’m actually kind of apprehensive too. But I know that following through for this learner is the best way we can work toward a better future for him, so I’m doing it.
A BCBA might also model acceptance, values, and committed action when choosing to discuss difficult topics with a parent, such as pursuing a conversation about the child’s current or future placement, prognosis, or treatment trajectory; fulfillment of treatment hours; the parent’s treatment-interfering behaviors; and so on. For example, the BCBA might say,
It’s really important to me to maintain a good relationship with you . . . and it is easier for me to avoid talking about things that are difficult or tell you things that will be hard to hear . . . but by avoiding feeling uncomfortable or upsetting you, I would be choosing being comfortable, over fighting for you and Max’s future and doing the best job I can for you both. So . . . even though it is going to be really difficult I would like to talk to you about [topic].
A behavior analyst can model defusion by tacting her private experience when working with parents. For example, she might say,
I notice I’m having the thought that I’m not being very helpful to you right now, and it’s getting in the way of me actually listening and figuring this out with you. Would it be OK if we pause for a second and start over?
Or a behavior analyst might smile humbly and say to a parent during a complex conversation where they are not making progress,
Hang on a second, my “Behavior Analyst Always Has to Be Right” theme song is playing in my head again. That’s probably not the most helpful thing right now. Let’s see how we can compromise so we can make a plan to move forward.
Using Single-Case Experimental Designs
ABA research and practice have always been concerned with empirically evaluating the effectiveness of interventions (Baer et al., 1968), and the use of single-case designs for this purpose is codified in Content Area D-5 of the Task List (BACB, 2017). The need to carefully evaluate the effectiveness of treatment is equally critical for ABA interventions that do or do not incorporate ACT. The methods used to evaluate whether it was actually an ACT intervention that produced behavior change are the same as those used for evaluating any other ABA intervention component, and rely primarily on single-case designs. At the very minimum, ABA practitioners look for large and immediate changes from baseline to treatment (Kazdin, 2011). For greater rigor, the practitioner might look at the other clients in her caseload and replicate the evaluation in a multiple-baseline across-clients design or employ some other single-case experimental design strategy. Ideally, the BCBA may attempt a component analysis to determine whether individual ACT components were effective in bringing about socially meaningful overt behavior change.
Competently Managing Emotional Behavior
In the context of ABA procedures that incorporate ACT, clients’ values-incongruent behaviors are discussed openly, and clients are asked to approach difficult thoughts or feelings. At these times, clients may sometimes engage in emotional behavior. Some BCBAs express concern that eliciting clients’ emotions could be construed as talk therapy, out of bounds for a behavior analyst, and outside their scope of competence. When young children with autism or adults with developmental disabilities react emotionally to behavioral programs, BCBAs do not express the concern that they may be acting outside their scope of practice or competence. The stance we advocate for BCBAs practicing in ACT inside ABA is that emotional behavior should be considered from both an operant and a respondent standpoint, for both typically developing adults and individuals with developmental disabilities.
Although clients may display emotional behavior during ACTraining, the approach that an ABA ACTrainer takes is distinct from that of many psychotherapists. In the context of emotional behavior, we recommend a behavior analyst show empathy and then move forward with the ACTraining skills that have been described in this article, which focus on establishing new self-management skills, rather than intentionally emotionally evocative intrapersonal exploration that is more common in psychotherapy. To illustrate the point, consider the following dialogue, in the context of a hypothetical parent training interaction between a BCBA and a parent, in which the BCBA works on acceptance of aversive private events, as well as implements a defusion procedure (i.e., “Sing Your Thoughts”):
Behavior analyst (BA): It’s difficult. Jake screams and curses at you. Then he ignores you for hours after you’ve pushed him to work with you.
Parent (P): I hate it.
BA: And your partner doesn’t follow your lead, so Jake goes to him for affection, leaving you to be the “villain.”
P: (Tears up)
BA: What’s going on for you right now?
P: I feel like a bad mom.
BA: Can you say a little more about that?
P: It’s just, ever since Jake was diagnosed, that’s all I ever say to myself. (Continues to tear up) That I’m a bad mom.
BA: Sounds like this is very old for you. You’ve been saying this to yourself for a long time.
P: Yeah, maybe since he was a baby and nothing seemed to go right with him.
BA: (Choosing not to go deeper into the past) So, I wonder if you’d be willing to try something rather unusual with me. Something very different.
P: (Sniffling) What do you mean?
BA: I sometimes get emotional when I think of the years I wasted before learning to take care of myself. I was overweight and inactive. I get this thought “I’m a horrible person for doing this to myself.”
P: Like my “Bad Mom.”
BA: Exactly.
P: So what do you do?
BA: Well, here’s what I’d like you to try. This is what I do, and like I said, it works for me, but I don’t know if it will work for you. I’d like you to try this.
P: What are we going to do?
BA: Tell me a song that you like. A song that really is meaningful to you.
P: Um. How about “Piano Man”?
BA: By Billy Joel? OK. Excellent. Can you sing a few bars for me?
P: (Reluctantly sings a few bars)
BA: (Joins her in a few bars)
P: (Smiling through her tears) OK. Now what?
BA: Well, for me, the next bars I sing might go like this,
“Now Jen was a graduate student and thought,
‘I’ll eat, sleep, and drink when I please,’
But after 6 years, she was all beer and cheese,
And her doctorate was nowhere in sight . . .”
P: (Laughs with BA)
BA: So now I want you to try this thing. You know your own refrain: “I’m a bad mom.” I’ll bet there’s more that comes with it.
P: Yeah, like it’s all my fault, even if I know it’s not. And I’m cold, and Jake just puts up with me.
BA: I hear you. Thank you for trusting me enough to share that with me. Can you now do this thing? Can you sing “Piano Man” but with those words?
P: For real?
BA: Yes.
P: (Pauses, then sings) “Sing us a song, you’re the world’s worstest mom, sing us a song tonight . . .” (Tears up and smiles) “’Cause we’re all in the mood to be laughing at you, and you’ve got it coming, don’t you?” (Laughs through her tears)
BA: (Laughing with her and tearing up) Yes. That’s it. What’s opening up for you now?
P: It’s like it still hurts . . .
BA: There’s an “and” somewhere in there.
P: Yeah—and it’s OK.
BA: What’s OK?
P: Maybe I can be thinking all that and still . . . do things that Jake doesn’t like if it means he might one day be more able to be independent because I persevered.
BA: I love it. Now, in the name of the value you just took a stand for, would you be willing to set a goal for action over the next 45 minutes with Jake and some kind of reinforcer you’ll give yourself for completing the task?
P: Sure. How about I do 10 maintenance trials each of two different programs that you’ve been working on with Jake? Then maybe I’ll go for a 5-minute walk around the block by myself to unwind?
BA: Sounds great. Let’s do it.
Inside this brief dialogue, the behavior analyst used behavioral skills training, first offering a rationale for the coming exercise, modeling, and then providing practice, reinforcement, and feedback. She allowed the parent to experience a range of emotions that started with self-pity and worked through sadness into humor and self-determination. The behavior analyst did not shy away from the emotion, nor did she lean in to elicit more intense emotional responding. Importantly, there was a moment when the parent wanted to introspect further into the past and deeper into the content of her verbal behavior about herself, and the behavior analyst did not go in this direction. Instead, the behavior analyst redirected the parent at that moment to an activity aimed at transforming the function of these rigid self-statements.
An ACT-based psychotherapist may or may not have done too much different, but the quality could have been more intense or more emotionally evocative. A psychotherapist might have asked questions regarding other contexts in which “I’m bad” might be showing up, or further explored childhood experiences that may have resulted in the parent learning the “I’m bad” verbal repertoire. This would be quite helpful for a client coming in for talk therapy about a general sense of helplessness in her life, but inappropriate for a BCBA helping a parent who feels helpless in her ability to implement behavior intervention plans with her child. The BCBA’s role is limited to that which the client has consented to and hired the BCBA to work on—in this case, the context of aiding the parent to implement her part of her child’s ABA treatment, and this is where the therapist in the previous transcript started and finished. When emotions were uncovered, the context was shifted toward playful levity, creating a context for the parent’s commitment to implement her child’s program. The next step for the BCBA would be to establish contingencies of reinforcement for this parent to follow through on her commitment and a method of measuring her performance during and after the session.
Was it necessary in the previous example to talk to the mother about her negative thoughts and emotions, as opposed to just instructing her to implement the behavior plan? When might a BCBA choose to address negative thoughts and feelings while practicing ACTraining? We suggest that BCBAs only address particular private events if and when there is some evidence that the client’s verbal behavior surrounding those private events may be getting in the way of engaging in socially important overt behavior. For example, when a behavior analyst asks a parent why he did not implement extinction, if the parent says, “Implementing extinction makes me feel like a bad father,” then the words “bad father” might be worth addressing, to show empathy and compassion for a parent who is suffering, among other reasons. If, instead, the parent expressed that he is “just too busy,” then ACTraining might work on developing some flexibility around verbal behavior about being too busy. In short, ACTraining does not necessitate addressing emotions just for their own sake. Negative private events are addressed in the same situations in which overt stimuli would be addressed: when there is reason to believe they may be interfering with progress in changing overt behavior.
A final note regarding private events warrants mention. Human beings talk about thoughts and feelings, and behavior analysts work with human beings. It is impossible to avoid talking about thoughts and feelings, and if we try, we run the risk of appearing cold and uncompassionate (Taylor, LeBlanc, & Nosik, 2018). If we do not use empirically derived behavior-analytic procedures for talking about private events, such as ACTraining, then we are left with nothing more than what we have all learned from our culture to talk about thoughts and feelings: mentalism. Therefore, ironically, the harder behavior analysts try to avoid talking about the mind, the more we may actually end up doing so mentalistically, rather than behaviorally. The concepts and procedures of ACTraining provide a behavior-analytic approach for BCBAs to talk to others about private events when doing so is in the service of socially meaningful overt behavior change.
Scope of Practice Versus Scope of Competence
It is important to distinguish between scope of practice and scope of competence (Brodhead, Quigley, & Wilczynski, 2018). Figure 1 is a diagram that depicts the larger psychological flexibility model that ACT comprises, as well as examples of specific disciplines that practice either ACT within psychotherapy, on the left half of the diagram, or ACTraining, on the right half of the diagram. Of course, the actual practices of the hundreds of thousands of professionals across these disciplines do not fit perfectly into these categories, but we propose that this diagram provides a useful framework for identifying ACTraining inside of ABA and how it is related to but separate from ACT as implemented inside psychotherapy across many different disciplines.
Fig. 1.
Related but distinct domains of practicing ACT as psychotherapy versus ACT as training, across multiple distinct but related professions.
We have been making the case in this article that ACTraining methods fit within the behavioral conceptual system and overlap substantively with the Task List and are therefore within the scope of practice of behavior analysts. However, just because ACTraining is within the professional scope of practice of BCBAs, it does not mean it is within the scope of competence of any particular BCBA. Similarly, both ABA for young children with autism and performance management consulting to Fortune 500 companies are within the scope of practice of behavior analysts, but if one has only had training and mentorship in one, then one is certainly not competent to practice the other. ABA practitioners must seek out specialized training and mentorship from competent trainers in order to use any ABA procedure, including ACT.
The goal of BCBAs is the deployment of conceptually and empirically sound methods of behavior change. Thus, the evolution of the scope of practice of BCBAs has occurred, and must continue to occur, with care and with the agreement and involvement of the science and profession, in careful and respectful interaction with other related professions. ACTraining inside ABA must stand up to the criteria proposed by Baer et al. (1968). The present discussion is not designed to promote any particular future vision of the responsible practice of BCBAs. Rather, the goal is to show that ACTraining is already within the scope of practice of BCBAs. Much further research and development are going to be needed to determine the type and amount of training, mentorship, and supervision that are required to produce excellent ACTraining performance inside of ABA. Of course, the same is also still true of most other specialties within ABA. Little or no research has been published that has demonstrated the type, amount, and quality of training necessary, nor any reliable outcome measure of competence, to produce a clinician who is competent to implement experimental functional analyses of severe behavior, treatment of feeding disorders, or organizational behavior management consulting. In all of these arenas, just as in ACTraining, when a practitioner expands into a new specialty, she must seek out extensive, high-quality training, supervision, and mentorship, until she is deemed competent to practice independently, ideally by others who are already doing so. Of course, even after one is competent to practice in any specialty, it is one’s ethical responsibility to seek out continued peer mentorship, supervision, and professional development.
When to Refer Out
The BACB Professional and Ethical Compliance Code for Behavior Analysts (BACB, 2014) states that individual behavior analysts practice only within their own scopes of competence (Section 1.02) and must refer clients to other providers when the BCBA is not able to address client needs appropriately (Section 2.03). Because ACT addresses problematic private events, behavior analysts often, and properly, wonder when it would be more appropriate to refer a client out for the services of a licensed psychologist or other mental health worker, versus implementing ACTraining inside of ABA services herself. This article attempts to identify when and how ACTraining is within the scope of practice of behavior analysts, and it is the duty of the individual behavior analyst to identify her own scope of competence. When a behavior analyst believes that a client demonstrates a need for ABA services outside the BCBA’s scope of competence, the client should be referred to another BCBA who possesses the necessary area of competence. However, when the BCBA believes the client demonstrates the need for mental health services (which are by definition outside the scope of practice of BCBAs who are not also licensed in another mental health profession), then the BCBA should refer the client to an appropriate mental health professional. However, as we have been discussing, this does not mean that the behavior analyst needs to cease all contact with the client or refuse to discuss private events. For example, a parent who is struggling with depression, is receiving psychotherapy for depression, and also has a child in an ABA program will likely still need to participate in that child’s ABA program. A BCBA who incorporates ACTraining into the parent training approach may be more effective in training that parent to implement the child’s behavior plan, even though the BCBA is in no way treating the parent’s depression. Using ACTraining, the behavior analyst may help the client develop flexibility and values-oriented behavior around the specific targets that are, indeed, within the scope of ABA services.
The left column of Table 1 lists examples of everyday challenges that are commonplace in the delivery of ABA services. The middle column lists overly simplified examples of how a BCBA might use ACTraining to be more effective in her work, still well within the scope of practice of ABA. The right column lists overly simplified examples of how a clinical psychologist might address these same challenges within the scope of his or her practice. These examples are overly simplified for the purposes of illustrating a discrimination; we do not in any way suggest that all practitioners fall into one of these two simplistic caricatures, nor do we suggest that we speak for all clinical psychologists or BCBAs. In addition, a third group of practitioners has largely not been addressed in this article, for the sake of clarity and space, and they are similarly left out of this table: specifically, practitioners who are both behavior analysts and also licensed mental health professionals, who practice behavior-analytic ACT as psychotherapy with their clients. This distinction, too, is an important one, but a sufficient discussion of this is beyond the scope of the current article.
Table 1.
Practical Challenges Addressed from ACTraining Compared to Psychotherapy Perspectives
| Trainee Presentation | ABA Practitioner | Psychotherapy Practitioner |
|---|---|---|
| A parent of a child with autism who is being trained to manage the child’s behavior reports being depressed. | Refer the parent to a clinical psychologist. If the parent is still willing to participate in training, then consider including ACT components in behavioral skills training to help the parent engage in overt behaviors while having negative feelings. Assess the effectiveness by measuring changes in overt parent implementation of behavior management procedures. | Treat core symptoms of depression. Measure effectiveness by assessing depressive symptomology. |
| A BCBA is supervising a staff member, and the staff member reports that distress over her marital strife is getting in the way of her doing her job. | Refer the staff member to a psychologist for couples therapy. Consider implementing ACT components into behavioral supervision to train the staff member in self-management strategies for still engaging in excellent overt performance while feeling distress. | Deliver couples therapy with the goal of decreasing marital discord. |
| A BCBA is engaging an adolescent with autism in social skills training, and the adolescent reports that he feels like a loser because he has no friends. | Consider referring the adolescent to a clinical psychologist for assessment for potential depression if the reports continue. In the context of social skills training, adapt ACT components to help the adolescent learn new and variable rules about himself in the context of social relations. | If the adolescent’s negative affect rises to the level of depression, treat the adolescent for depression with psychotherapy. |
Final Thoughts
We have attempted to provide both conceptual and practical guidance on how ABA practitioners can begin to incorporate ACT into their daily practice as behavior analysts. Naturally, like any important distinction within professional practice, it is unlikely that reading a single article will ensure appropriate practice. Therefore, we offer six simple rules:
Understand the behavioral principles that undergird any behavioral procedure used, including methods drawn from ACT. That is, as behavior analysts, we must remain conceptually systematic at all times in our practice.
Maintain an approach to treatment that fits your role as a BCBA, including a focus on overt behavior change.
Seek consultation from experienced ABA practitioners who understand the distinction between ACT as practiced within ABA treatment settings and ACT as practiced in other settings. Seek out appropriate training and mentorship, including behavioral skills training that continues until you demonstrate proficient implementation without assistance.
Look for and be guided by empirical behavioral literature in your application of ACT as a BCBA.
Empirically evaluate what you do, and reconsider immediately if the data are not positive.
Know when to refer out. Incorporating the functional analyses and procedures within ACT can enhance one’s behavior-analytic practice, but it is not a panacea. Just as a BCBA must know when to refer a client out when one is not competent to solve a conventional problem of overt behavior (e.g., feeding disorder, severe self-injurious behavior), one must be sensitive to when it is appropriate to refer a client out when the client is struggling with private events that are outside one’s scope of competence, regardless of whether one is trained in ACT.
In conclusion, we believe that the future of ACT within ABA is a bright one. The rich and complex functional analyses of verbal behavior and derived relations, along with the implications these analyses have for helping clients make meaningful overt behavior changes, have much to contribute to the practice of ABA. As with any new area of growth within the field, the dissemination of ACT within ABA will not be without its bumps. However, by staying close to the philosophy, principles, and procedures that comprise ABA, we believe that the gradual and careful adoption of ACT functional analyses and treatment procedures within ABA will yield benefits for behavior analysts and those whose lives we touch.
Author Note
The authors would like to thank Drs. Evelyn Gould, Emily Sandoz, Steven C. Hayes, and Courtney Tarbox for their contributions throughout the manuscript.
Compliance with Ethical Standards
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
The authors declare that this article did not involve research with human subjects and therefore was not reviewed by a research ethics committee.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alvero AM, Bucklin BM, Austin J. An objective review of the effectiveness and essential characteristics of performance feedback in organizational settings (1985–1998) Journal of Organizational Behavior Management. 2001;21(1):3–29. doi: 10.1300/J075v21n01_02. [DOI] [Google Scholar]
- American Psychological Association. (2016). Psychological treatments. Retrieved from the Society of Clinical Psychology Division 12 website: https://www.div12.org/treatments/
- Baer, DM., Wolf, M. M., & Resley, T. R. (1968). Some current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis, 1(1), 91. [DOI] [PMC free article] [PubMed]
- Barron BF, Verkuylen L, Belisle J, Paliliunas D, Dixon MR. Teaching “then-later” and “here-there” relations to children with autism: An evaluation of single reversals and transformation of stimulus function. Behavior Analysis in Practice. 2019;12:167–175. doi: 10.1007/s40617-018-0216-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behavior Analyst Certification Board . Professional and ethical compliance code for behavior analysts. Littleton, CO: Author; 2014. [Google Scholar]
- Behavior Analyst Certification Board . BCBA/BCaBA task list. 5. Littleton, CO: Author; 2017. [Google Scholar]
- Blackledge JT, Hayes SC. Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child and Family Behavior Therapy. 2006;28:1–18. doi: 10.1300/j019v28n0. [DOI] [Google Scholar]
- Blackledge, J.T., & Drake, C.E (2013). Acceptance and commitment theraphy: Empirical and theoritical considerations. In S. Dymond & Roche (Eds.), Advances in relational frame theory: Research and application (p.219–252). Oakland, CA: New Harbinger Publiations, Inc.
- Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42, 676–688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed]
- Bondy A, Frost L. The picture exchange communication system. Behavior Modification. 2001;25:725–744. doi: 10.1177/0145445501255004. [DOI] [PubMed] [Google Scholar]
- Brazeau K, Rehfeldt RA, Mazo A, Smalley S, Krus S, Henson L. On the efficacy of mindfulness, defusion, and behavioral skills training on job interviewing skills in dually-diagnosed adults with developmental disorders. Journal of Contextual Behavioral Science. 2017;6(2):145–151. doi: 10.1016/j.jcbs.2017.04.002. [DOI] [Google Scholar]
- Brodhead, M.T., Quigley, S.P., & Wilczynski, S.M. (2018). A call for discussion about scope of competence in behavior analysis. Behavior Analysis in Practice, 11(4), 424–435. [DOI] [PMC free article] [PubMed]
- Castro M, Rehfeldt RA, Root WB. On the role of values clarification and committed actions in enhancing the engagement of direct care workers with clients with severe developmental disorders. Journal of Contextual Behavioral Science. 2016;5(4):201–207. doi: 10.1016/j.jcbs.2016.09.003. [DOI] [Google Scholar]
- Chancey C, Weihl C, Root WB, Rehfeldt RA, McCauley D, Takeguchi K, Pritchard J. The impact of mindfulness skills on interactions between direct care staff and adults with developmental disabilities. Journal of Contextual Behavioral Science. 2019;12:160–169. doi: 10.1016/j.jcbs.2018.07.004. [DOI] [Google Scholar]
- Chase JA, Houmanfar R, Hayes SC, Ward TA, Vilardaga JP, Follette VM. Values are not just goals: Online ACT-based values training adds to goal-setting in improving undergraduate college student performance. Journal of Contextual Behavioral Science. 2013;2:79–84. doi: 10.1016/j.jcbs.2013.08.002. [DOI] [Google Scholar]
- Chawla, N., & Ostafin, B. D. (2007). Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. Journal of Clinical Psychology, 63, 871–890. 10.1002/jclp.20400 [DOI] [PubMed]
- Cooper, J.O., Heron, T.E., & Heward, W.L. (2002). Applied Behavior analysis. Hoboken, NJ:
- Critchfield, T., & Rehfeldt, R. A. (2020). Engineering emergent learning with nonequivalence relations. In J. O. Cooper, T. E. Heron, & W. L. Heward (Eds.), Applied behavior analysis (3rd ed.) 497–526. London, UK: Pearson.
- Department of Veterans Affairs. (2016). VA/DoD clinical practice guideline for the management of major depressive disorder: Version 3.0. Retrieved from: https://www.healthquality.va.gov/guidelines/MH/mdd/VADoDMDDCPGFINAL82916.pdf
- Devany JM, Hayes SC, Nelson RO. Equivalence class formation in language-able and language-disabled children. Journal of the Experimental Analysis of Behavior. 1986;46:243–257. doi: 10.1901/jeab.1986.46-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon MR. ACT for children with autism and emotional challenges. Carbondale, IL: Shawnee Scientific Press; 2014. [Google Scholar]
- Dixon, M.R. & Paliliunas, D. (2017). AIM: A behavior analytic curriculum for social-emotional development in children. Carbondale, IL: Shawnee Scientific Press.
- Dixon MR, Blevins A, Belisle J, Bethel B. Teaching children with autism extended verbal utterances under audience control in the context of show-and-tell. Behavior Analysis in Practice. 2019;12:194–198. doi: 10.1007/s40617-018-0250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dollard J, Miller NE. Personality and psychotherapy: An analysis in terms of learning, thinking, and culture. New York, NY: McGraw-Hill; 1950. [Google Scholar]
- Eilers HJ, Hayes SC. Exposure and response prevention therapy with cognitive defusion exercises to reduce repetitive and restrictive behaviors displayed by children with autism spectrum disorder. Research in Autism Spectrum Disorders. 2015;19:18–31. doi: 10.1016/j.rasd.2014.12.014. [DOI] [Google Scholar]
- Estes, W. K., & Skinner, B. F. (1941). Some quantitative properties of anxiety. Journal of Experimental Psychology, 29(5), 390–400. 10.1037/h0062283
- Gould ER, Tarbox J, Coyne L. Evaluating the effects of acceptance and commitment training on the overt behavior of parents of children with autism. Journal of Contextual Behavioral Science. 2018;7:81–88. doi: 10.1016/j.jcbs.2017.06.003. [DOI] [Google Scholar]
- Harris, R. (2008). The willingness and action plan. Retrieved from thehappinesstrap.com/upimages/Willingness_and_Action_Plan.pdf
- Hayes, S.C. (n.d.). State of the ACT Evidence. Retrieved from: https://contextualscience.org/state_of_the_act_evidence
- Hayes, S. C. (1982, May). Rule-governed behavior and psychopathology. Invited address presented at the meeting of the Association for Behavior Analysis International, Milwaukee, WI.
- Hayes, S. C. (1983, May). Semantic therapy, cognition, rule-governed behavior, and psychopathology: A radical behavioral approach. Invited workshop presented at the meeting of the Association for Behavior Analysis International, Milwaukee, WI.
- Hayes, S. C. (1984). Making sense of spirituality. Behaviorism, 12, 99–110. https://www.jstor.org/stable/27759047
- Hayes, S.C. (2020). ACT Randomized Controlled Trials Since 1986. Retrieved from : https://contextualscience.org/ACT_Randomized_Controlled_Trials
- Hayes SC, Barnes-Holmes D, Roche B, editors. Relational frame theory: A post-Skinnerian account of human language and cognition. New York, NY: Kluwer Academic/Plenum Publishers; 2001. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Bond F, Barnes-Holmes D, Austin J, editors. Acceptance and mindfulness at work: Acceptance and commitment therapy, relational frame theory, and organizational behavior management. Binghamton, NY: Haworth; 2006. [Google Scholar]
- Hayes, S. C., & Brownstein, A. J. (1985, May). Verbal behavior, equivalence classes, and rules: New definitions, data, and directions. Invited address presented at the meeting of the Association for Behavior Analysis International, Columbus, OH.
- Hayes, S. C., & Brownstein, A. J. (1986). Mentalism, behavior-behavior relations and a behavior analytic view of the purposes of science. The Behavior Analyst, 9, 175–190. 10.1007/BF03391944 [DOI] [PMC free article] [PubMed]
- Hayes SC, Brownstein AJ, Haas JR, Greenway DE. Instructions, multiple schedules, and extinction: Distinguishing rule-governed from schedule controlled behavior. Journal of the Experimental Analysis of Behavior. 1986;46:137–147. doi: 10.1901/jeab.1986.46-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Brownstein AJ, Zettle RD, Rosenfarb I, Korn Z. Rule-governed behavior and sensitivity to changing consequences of responding. Journal of the Experimental Analysis of Behavior. 1986;45:237–256. doi: 10.1901/jeab.1986.45-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Cone JD. Reduction in residential consumption of electricity through simple monthly feedback. Journal of Applied Behavior Analysis. 1981;14:81–88. doi: 10.1901/jaba.1981.14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, S. C., & Hayes, L. J. (1992). Some clinical implications of contextualistic behaviorism: The example of cognition. Behavior Therapy, 23(2), 225–249. 10.1016/S0005-7894(05)80383-1
- Hayes SC, Hayes LJ, Reese HW. Finding the philosophical core: A review of Stephen C. Pepper’s World hypotheses. Journal of the Experimental Analysis of Behavior. 1988;50:97–111. doi: 10.1901/jeab.1988.50-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, McCurry SM, Afari N, Wilson K. Acceptance and . . . A therapy manual for the treatment of emotional avoidance. Reno: Context Press; 1991. [Google Scholar]
- Hayes, S. C., Strosahl, K. D., Wilson, K. G., Bissett, R. T., Pistorello, J., Toarmino, D., et al. (2004). Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record, 54, 553–578. 10.1007/BF03395492
- Hayes SC, Zettle RD, Rosenfarb I. Rule following. In: Hayes SC, editor. Rule-governed behavior: Cognition, contingencies, and instructional control. New York, NY: Plenum; 1989. pp. 191–220. [Google Scholar]
- Hayes, S.C., Strosahl, K.D., & Wilson, K.G. (2011). Acceptance and commitment therapy: The process and practice of mindful change. New York: Guilford Press.
- Hawkes, A. L., Chambers, S.K., Pakenham, K.I., Patrao, T.A., Baade, P.D., Lynch, B.M., Aitken, J.F., Meng, X., & Courneya, K.S., (2013). Effects of a telephone-delivered multiple health behavior change intervention (CanChange) on health and behavioral outcomes in survivors of colorectal cancer: a randomzed controlled trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncolgy, 31(28), 2313–2321. 10.1200/JCO.2012.45.5873 [DOI] [PubMed]
- Iwata, B. A., Dorsey, M. F., Slifer, K. J., Bauman, K. E., & Richman, G. S. (1982). Toward a functional analysis of self-injury. Analysis and Intervention in Developmental Disabilities, 2(1), 3–20. 10.1016/0270-4684(82)90003-9
- Ju, W.C., & Hayes, S.C. (2008). Verbal stablishing stimuli: Testing the motivative effect of stimuli in a derived relation with consequences. The Psychological Record, 58(3), 339–363
- Kanfer, F. H. (1961). Comments on learning in psychotherapy. Psychological Reports, 9(3), 681–699. 10.2466/pr0.1961.9.3.681
- Kasson EM, Wilson AN. Preliminary evidence on the efficacy of mindfulness combined with traditional classroom management strategies. Behavior Analysis in Practice. 2016;10:242–251. doi: 10.1007/s40617-016-0160-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin, A.E. (2011). Single-case research designs: Methods for clinical and applied settings (2nd ed.). Oxford: Oxford University Press
- Kohlenberg, R. J., Tsai, M., & Dougher, M. J. (1993). The dimensions of clinical behavior analysis. The Behavior Analyst, 16(2), 271–282. 10.1007/BF03392636 [DOI] [PMC free article] [PubMed]
- Krasner, L. (1963). Reinforcement, verbal behavior and psychotherapy. American Journal of Orthopsychiatry, 33, 601–613. 10.1111/j.1939-0025.1963.b01008.x [DOI] [PubMed]
- Levin ME, Haeger J, Smith GS. Examining the role of implicit emotional judgments in social anxiety and experiential avoidance. Journal of Psychopathology and Behavioral Assessment. 2017;39:264–278. doi: 10.1007/s10862-016-9583-5. [DOI] [Google Scholar]
- Levin ME, Hildebrandt MJ, Lillis J, Hayes SC. The impact of treatment components suggested by the psychological flexibility model: A meta-analysis of laboratory-based component studies. Behavior Therapy. 2012;43:741–756. doi: 10.1016/j.beth.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Luciano, C., Ruiz, F. J., Torres, R. M. V., Martín, V. S., Martínez, O. G., & López, J. C. L. (2011). A relational frame analysis of defusion interactions in acceptance and commitment therapy: A preliminary and quasi-experimental study with at-risk adolescents. International Journal of Psychology and Psychological Therapy, 11, 165–182. https://www.redalyc.org/pdf/560/56019292001.pdf
- Mace FC, Hock ML, Lalli JS, West BJ, Belfiore P, Pinter E, Kirby Brown D. Behavioral momentum in the treatment of noncompliance. Journal of Applied Behavior Analysis. 1988;21:123–141. doi: 10.1901/jaba.1988.21-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuda A, Hayes SC, Sackett CF, Twohig MP. Cognitive defusion and self-relevant negative thoughts: Examining the impact of a ninety year old technique. Behaviour Research and Therapy. 2004;42:477–485. doi: 10.1016/j.brat.2003.10.008. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Jones R. Treatment for chronic pain for adults in the seventh and eighth decades of life: A preliminary study of acceptance and commitment therapy (ACT) Pain Medicine. 2012;13(7):860–867. doi: 10.1111/j.1526-4637.2012.01407.x. [DOI] [PubMed] [Google Scholar]
- McEnteggart, C.A., (2018). Brief Tutorial on Acceptance an Commiment Theraphy as Seen Throuh the Lense of Derived Simulus Relations. Perspectives on Behavioral Science, 41, 215–227. 10.1007/s40614-018-0149-6 [DOI] [PMC free article] [PubMed]
- Monestes JL, Greville WJ, Hooper N. Derived insensitivity: Rule-based insensitivity to contingencies propagates through equivalence. Learning and Motivation. 2017;59:55–63. doi: 10.1016/j.lmot.2017.08.003. [DOI] [Google Scholar]
- Moran, D. J. (2014). Mindful action plan. Retrieved from contextualscience.org/files/49%20FriAM%20-%20Batten%20and%20Moran-%20XXXX.pdf
- Neef NA, Mace FC, Shea MC, Shade D. Effects of reinforcer rate and reinforcer quality on time allocation: Extensions of matching theory to educational settings. Journal of Applied Behavior Analysis. 1992;25:691–699. doi: 10.1901/jaba.1992.25-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahnke J, Lundgren RT, Hursti T, Hirvikoski T. Outcomes of an acceptance and commitment therapy-based skills training group for students with high-functioning autism spectrum disorder: A quasi-experimental pilot study. Autism. 2014;18:953–964. doi: 10.1177/1362361313501091. [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Winton ASW, Adkins AD, Singh J, Singh AN. Mindfulness training assists individuals with moderate mental retardation to maintain their community placements. Behavior Modification. 2007;31:800–814. doi: 10.1177/0145445507300925. [DOI] [PubMed] [Google Scholar]
- Skinner BF. Science and human behavior. New York, NY: Macmillan; 1953. [Google Scholar]
- Skinner, B.F., (1969). Contingencies of reinforcement: A theoritical analysis. NJ: Prentice Hall.
- Spinhoven P, Drost J, de Rooij M, van Hemert AM, Penninx BW. A longitudinal study of experiential avoidance in emotional disorders. Behavior Therapy. 2014;45:840–850. doi: 10.1016/j.beth.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Szabo TG. Acceptance and commitment training for reducing inflexible behaviors in children with autism. Journal of Contextual Behavioral Science. 2019;12:178–188. doi: 10.1016/j.jcbs.2019.03.001. [DOI] [Google Scholar]
- Szabo, T. G., & Dixon, M. R., (2016). Contextual behavior science and education. In R.D. Zettle S.C. Hayes, D. Barnes-Holmes, & A. Biglan (Eds.), Wiley Handbook of Contextual Behavioral Science (422–458). Medford, MA: Wiley
- Szabo, T., & Tarbox, J. (2018). Acceptance and commitment training and the scope of practice of BCBAs [Web log post]. https://bsci21.org/acceptance-and-commitment-training-and-the-scope-of-practice-of-bcbas [DOI] [PMC free article] [PubMed]
- Szabo, T. G., Willis, P. G., & Palinski, C. J. (2019). Watch me try: Improving athletic performance of young adults with ASD. Advances in Neurodevelopmental Disorders. Advance online publication. https://rdcu.be/bQKlb
- Taylor, B. A., LeBlanc, L. A., & Nosik, M. R. (2018). Compassionate care in behavior analytic treatment: Can outcomes be enhanced by attending to relationships with caregivers? Behavior Analysis in Practice. Advance online publication.10.1007/s40617-018-00289-3 [DOI] [PMC free article] [PubMed]
- Villatte M, Villatte J, Hayes SC. Mastering the clinical conversation: Language as intervention. New York, NY: Guilford; 2015. [Google Scholar]
- Wolf, M. M. (1978). Social validity: The case for subjective measurement or how applied behavior analysis is finding its heart. Journal of Applied Behavior Analysis, 11(2), 203–214. 10.1901/jaba.1978.11-203 [DOI] [PMC free article] [PubMed]
- Zettle RD. The evolution of a contextual approach to therapy: From comprehensive distancing to ACT. International Journal of Behavioral Consultation and Therapy. 2005;1(2):77–89. doi: 10.1037/h0100736. [DOI] [Google Scholar]
- Zettle, R. D., & Hayes, S. C. (1986). Dysfunctional control by client verbal behavior: The context of reason giving. The Analysis of Verbal Behavior, 4, 30–38. 10.1007/BF03392813 [DOI] [PMC free article] [PubMed]