Abstract
Objective
Dynamization has already been described as a secondary intervention for delay unions of tibial shaft fractures treated with intramedullary nailing. Although it’s a common procedure, it is not widely supported in the literature. The purpose of this study was to determine the union rate of nail dynamization in cases of delayed union of diaphyseal tibial fractures, and assess the effect of fracture morphology on union rates.
Materials and methods
We retrospectively analyzed a series of 199 consecutive tibial shaft fractures. We recorded the dynamization rate, period from nailing to dynamization, nailing to the union, the fracture pattern (according to AO/ASIF and whether it was closed or open), the callus diameter before dynamization (fracture healing index; FHI) and union/failure rates.
Results
Out of a total of 199 fractures treated during the study period, 41 (20.6%) were dynamized. After applying inclusion and exclusion criteria, 39 patients with 39 fractures were included in the study. The mean time from nailing to dynamization was 18.4 ± 7.2 weeks. The union rate was 92.3% (n = 36) over a mean time of 14.1 ± 5.6 weeks as from dynamization. The overall failure rate was 6.7% (n = 3). There was no significant association between failure and AO/ASIF classification (p > 0.05) or fracture exposure (X2 = 0.19; p = 0.66). The pre-dynamization FHI of ≥ 1.17 was significantly associated with consolidation (p < 0.05).
Conclusion
In cases of delayed union of tibial fractures, dynamization offered a high union rate associated with pre-dynamization FHI, while fracture morphology did not affect the failure rate.
Keywords: Dynamization, Tibial fracture, Delayed union, Intramedullary nailing
Introduction
Tibial shaft fractures are the most common long bone fractures [1]. The Swedish Fracture Register estimates approximately 15.7 fractures per 100,000 individuals per year, while a recent large-scale study reported an incidence of 16.9/100,000 inhabitants in the US [2, 3]. Intramedullary nailing is the treatment of choice for most closed and open (up to Gustilo 3A) tibial shaft fractures with reported union rates over 90% [4, 5]. Complications for this surgical approach include consolidation disorders like delayed union and non-union with rates between 2.2 and 14% respectively [6].
Dynamization has been described as a secondary intervention for these complications. It enhances bone contact and compression at the fracture site, stimulating the osteogenesis [7–9].
After the success obtained with dynamization in experimental animal models, it was subsequently recommended as a routine procedure [8]. However, its indication became more selective after some authors reported complications like shortening and reduction loss, especially in comminuted fractures [9, 10].
Previous studies reported a wide range of successful healings after dynamization [11]. Although, in most of them, femur and tibia fractures, or even delayed and non-union fractures, are assessed jointly [7, 12].
The purpose of this study was to assess the effectiveness (union) after nail dynamization in a delayed union of tibial shaft fractures and to evaluate whether fracture morphology (according to AO/ASIF classification or whether it was closed or open), and callus diameter affected healing or failure rate.
Materials and Methods
After approval from the Institutional Review Board at our hospital, we analyzed all tibial diaphyseal fractures consecutively operated between January 2010 and December 2019.
We included skeletally mature patients initially treated with interlocking nail who underwent dynamization after a diagnosis of delayed union. We excluded patients with metaphyseal-epiphyseal fractures, a history of surgical procedures on the affected leg, pathological fractures, an active surgical site infection, those who had undergone other procedures in addition to dynamization, and cases with incomplete clinical-radiological follow-up information (from fracture to the union).
Delayed union was defined as absence of or minimal radiological signs of healing progress three months after nailing, presence of sparse callus or minimal radiological signs of healing progress at two consecutive monthly follow-ups visits between the third month to the eighth month after nailing [7, 13]. Fracture union was defined as the presence of bridging callus in at least 3 out of 4 cortices and no pain on weight bearing, or a ≥ 10 Radiographic Union Score for Tibial Fracture (RUST) score [14]. Dynamization failure was defined as cases requiring any type of additional post-dynamization intervention to achieve union or lack of healing at 9 months after screw removal.
Surgical Technique
In all cases, dynamization was performed as an outpatient procedure under local anesthesia, sedation and radioscopic guidance (BV Pulsera, Phillips Medical System NL B.V, Netherlands). The proximal locking screw of the intramedullary nail was removed through the previous scar. The proximal dynamic screw was preserved in all cases. In order to restrict activity and control pain, patients were allowed to perform partial weight-bearing with the assistance of a walking cane immediately after surgery for the first week. Thereafter, full weight-bearing was indicated. Postoperative controls were scheduled at 2 and 4 weeks, and then monthly until bone union. After this period, follow-up continued on an annual basis.
Clinical and Radiographic Assessment
Clinical and radiographic records of those patients who met the inclusion criteria were collected. We documented gender, age, affected side, fracture morphology (AO/ASIF classification) and whether the fracture was closed or open (classified according to Gustilo’s method) [15, 16].
Periods from static intramedullary nailing to dynamization, dynamization to the union, and static intramedullary nailing to the union were assessed. The radiation exposure time required for dynamization, measured by the equipment used, was also recorded. The association between fracture type (AO/ASIF and whether it was closed or open) and post-dynamization union/non-union was also analyzed.
The callus diameter was assessed by means of the fracture healing index (FHI) on the basis of pre-dynamization radiographs, according to the method described by Spencer [17] (Fig. 1). The relationship between FHI and post-dynamization union was also assessed.
Fig. 1.

a, b Description of FHI calculates. Line A represents the maximum callus diameter and Line B the normal adjacent bone. Both measurements were taken on AP and lateral radiographs, and at right angles to the tibial axis. FHI = Line A (AP + L)/Line B (AP + L)
All procedure-related complications were recorded (e.g., reduction loss, significant shortening > 10 mm, surgical site infection, wound problems, and residual pain).
The radiographic assessment relied on antero-posterior (AP) and lateral (L) views of the leg. Preoperative radiographs were compared together with all postoperative controls. Measurements were made using software SYNAPSE (Fujifilm Medical System, USA) and, when no digital images were available, measurements were performed manually with a goniometer. Two independent authors evaluated all test results and inconsistencies, if any, were solved by a senior author.
Statistical Analysis
Continuous variables were described as mean and standard deviation. Qualitative variables were described as percentages and a 95% confidence interval (CI) was used. Both groups (pre- and post-dynamization) were compared using a t test for continuous variables and a X2 test (Chi-square test) for categorical variables. Pre-dynamization FHI and bone union were analyzed using ROC curve. The softwares used were Graph Pad Prism 8.0 (San Diego, USA) and MedCalc 12.0 (Ostend, Belgium). Data were entered into an Excel spreadsheet (Microsoft, Redmon, WA, USA) for analysis.
Results
Out of a total of 199 fractures treated during the study period, 41 (20.6%) were dynamized. After applying inclusion and exclusion criteria, 39 patients with 39 fractures were available for full analysis.
Thirty-seven were (94.9%) men. The mean age was 32.4 ± 10.3 years (range 16–50). In 20 (51.3%) cases, the right side was affected. According to the AO/ASIF classification, the most common fracture type was A (58.9%). There were 9 (23.1%) open fractures (Table 1).
Table 1.
Demographic data, fracture morphology and evolution of patients included in the analysis
| Variables | No. (%) | p value |
|---|---|---|
| Age | 32.4 ± 10.3 | – |
| Gender | ||
| Male | 37 (94.9) | – |
| Female | 2 (5.1) | – |
| AO/ASIF | ||
| A | 23 (58.9) | ns |
| B | 10 (25.7) | |
| C | 6 (15.4) | |
| Open–closed | 9 (23.1)–30 (77.9) | ns |
| Gustilo | ||
| II | 3 (33.3) | |
| IIIB | 6 (66.7) | |
| Time interval (weeks) | ||
| IMN–dynamization | 18.4 ± 7.2 | |
| Dynamization–union | 14.1 ± 5.6 | |
| RUST | ||
| Before dynamization | 5.6 ± 1.5 | |
| After dynamization | 10.7 ± 1.5 | < 0.01 |
| Bone union | ||
| Union | 36 (92.3) | |
| Non-union | 3 (7.7) | |
IMN intramedullary nailing, ns not significant
The mean interval between static intramedullary nailing and dynamization was 18.4 ± 7.2 weeks (range 12–30). The union rate was 92.3% (n = 36) over a mean time of 14.1 ± 5.6 weeks (range 5–24) as from dynamization. The mean time between static intramedullary nailing and fracture union was 26.4 ± 5.3 weeks (range 11.4–56.4) (Fig. 2). The mean radiation exposure time required for the dynamization was 2.41 ± 0.6 (range 2–4) seconds.
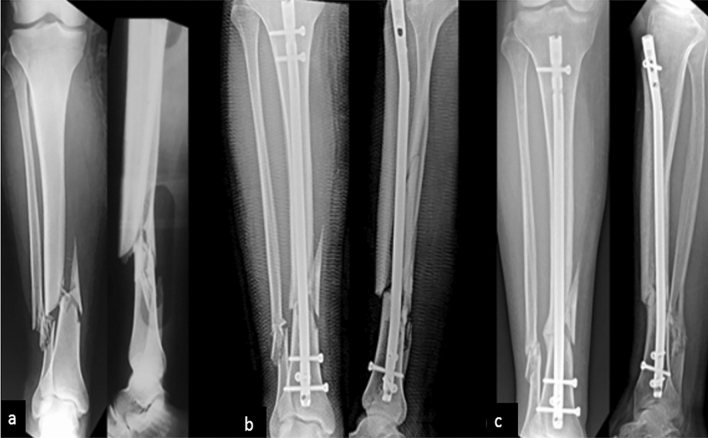
Fig. 2.
Right-leg radiographs, antero-posterior (A-P) and lateral (L) views. a Tibial fracture 42B2 (AO/ASIF). b Fourteen-week follow-up after interlocking nailing without evidence of fracture union. c Twelve-week follow-up after dynamization with union (RUST score of 10)
The mean RUST score increased significantly after dynamization (5.6 ± 1.5 versus 10.7 ± 1.5; p < 0.01). The overall dynamization failure rate was 7.7%.
Regarding fracture morphology, failure percentages were 8.7% for type A fractures (2/23) and 10% for type B fractures (1/10). There were no failures in type C fractures. No significant association was found between fracture type (A, B, or C) and failure (p > 0.05 in each subtype) (Table 2).
Table 2.
Summary of patients who achieved bone union and those who failed after dynamization according to fracture morphology (AO/ASIF classification, open or close fracture) and to pre-dynamization FHI
| Bone unionn-% | Failuren-% | p value | |
|---|---|---|---|
| AO/ASIF | |||
| A | 21 (91.3) | 2 (8.7) | > 0.05 |
| B | 9 (90) | 1 (10) | |
| C | 6 (100) | – | |
| Close | 28 (93.3) | 2 (6.7) | 0.66 |
| Open | 8 (88.9) | 1 (11.1) | |
| FHI | |||
| ≥ 1.17 | 33 (100) | – | < 0.05 |
| < 1.17 | 6 (50) | 3 (50) | |
FHI fracture healing index
Failure percentages were 6.7% (2/30) for closed fractures and 11.1% (1/9) for open fractures. A X2 test showed that there was no statistically significant association between dynamization failure and fracture exposure (open or closed), X2 = 0.19 (p = 0.66).
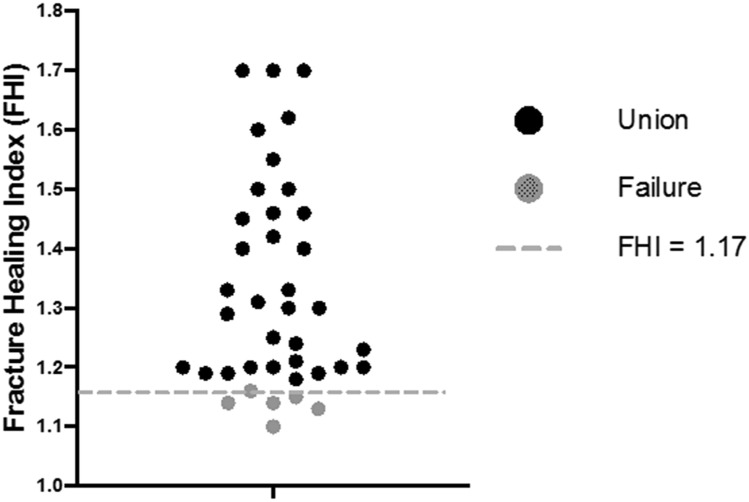
When analyzing the association between FHI and fracture union, a statistically significant difference was observed between fractures with FHI < 1.17 and those with an index higher than this value. The latter healed in all cases (p < 0.05), while only 50% (3 out of 6) of those with FHI < 1.17 did (Fig. 3). FHI ≥ 1.17 showed a positive predictive value of 100% of bone union after dynamization, with 91.67% sensitivity and 100% specificity (Fig. 4).
Fig. 3.
Description of pre-dynamization FHI values and bone union or failure after dynamization
Fig. 4.
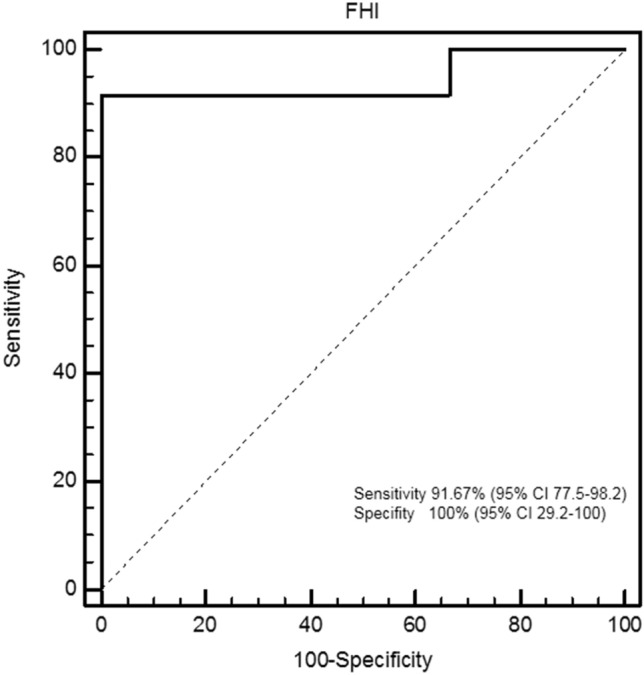
ROC curve showing FHI optimized at 1.17. Area under the curve = 0.94; standard error = 0.041; 95% confidence interval 0.821–0.992
No procedure-related complications were recorded.
Three patients did not achieve bone union after dynamization and required additional procedures: 42B2 fracture dynamized after 14 weeks and two 42A3 fractures (1 Gustilo 3B) dynamized after 12 and 17 weeks, respectively. In all three cases, nail exchange was performed with a reamed larger diameter nail. Both type A fractures also required a fibular osteotomy. All three cases achieved union after the re-intervention.
Discussion
Dynamization is a surgical alternative for the initial treatment of delayed bone union, which may even be used in non-union [7, 11, 12]. Union rates after the dynamization of a tibial fracture range between 54 and 95.8% [7, 18]. Although it is a common procedure, it is not widely supported by the literature [13, 14].
In 1993, Wu et al. reported a union rate of 64% after dynamization in a series of 11 tibial fractures without radiographic signs of consolidation after 4 months [7]. Since then, several authors have studied the effectiveness of dynamization in tibial fractures after interlocking nailing [18, 19]. In this series, the union rate after dynamization was 92.3%, which is consistent with the results published by Manjunatha et al., Jain et al., and Perumal et al. [13, 18, 19].
There is no consensus regarding the ideal time for dynamization. It is usually performed 8–12 weeks after interlocking nailing to allow for the formation of enough fibrous callus to prevent excess mobility at the fracture site [12, 13, 20]. In this study, the mean time between nailing and dynamization was 18.4 weeks, in consistency with Perumal et al. who dynamized a series of 20 tibial fractures after a mean interval of 19.1 weeks [13]. Vaughn et al. and Wu et al. reported lower union rates (54% and 64%) with late dynamization (after 25.6 and 31.2 weeks, respectively) [7, 12]. Although the union rates of late dynamization appear to be lower, these and other authors state they could not find a significant association between dynamization time and union rate [7, 12, 13, 21].
In accordance with the literature, the failure rate of this series ranges between 5 and 46% [12, 13]. Although type B fractures (AO/ASIF) were most frequently related to failure, we did not find a statistically significant association between fracture patterns and failure rates [12, 21, 22]. Perumal et al., however, reported a significant association between dynamization failure and comminuted fractures (type C) [13]. On the other hand, consistently with the series of Chalidis et al. and Litrenta et al., open fractures showed higher indexes of failure, though not significant [13, 22].
In this series, there were no procedure-related complications. Reduction loss, shortening or instability reported in other publications could result from the dynamization technique. Some authors remove all locking screws from one of the fracture fragments, losing the rotational and longitudinal control offered by interlocking nails [6, 7, 10, 22]. In our series, the design of the intramedullary nails used had the oval hole only in the proximal side of the nail, so that by removing only the static screw and leaving the dynamic screw, we kept at least one locking screw in each fragment. This allowed us to control axial displacement and neither fracture presented reduction loss or significant shortening.
According to previous reports that state that the callus diameter reflects biological potential of the fracture, FHI ≥ 1.17 showed a positive predictive value of 100% bone healing after dynamization in our series, with 91.67% sensibility and 100% specificity [12, 13].
Finally, in this study, dynamization was not characterized for being a technically demanding intervention. It was performed as an outpatient procedure without associated complications.
The limitations of this study are those inherent to retrospective studies. A more accurate statistical analysis was not possible because of the small sample size; therefore, the lack of statistical significance observed for some variables could be due to a Beta error. To the best of our knowledge, however, there are not many larger series in the literature regarding this subject.
Conclusion
In this study, dynamization as a treatment for delayed union of tibial fractures had a success rate of 92.3%. Fracture morphology did not appear to have an impact on dynamization failure rate. Callus diameter (FHI) was a useful predictor of post-dynamization bone union. Further properly designed studies with more patients are necessary to determine the effectiveness of this treatment technique.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TLD, SG and LPA. The first draft of the manuscript was written by GG, CAP and HdS. All authors read and approved the final manuscript.
Funding
This work has not received funding.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures followed were in accordance with ethical standards of the British Hospital of Buenos Aires committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Praemer A, Furner S, Rice DP. Musculoskeletal conditions in the United States. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1992. [Google Scholar]
- 2.Wennergren D, Bergdahl C, Ekelund J, Juto H, Sundfeldt M, Moller M. Epidemiology and incidence of tibia fractures in the Swedish Fracture Register. Injury. 2018;49(11):2068–2074. doi: 10.1016/j.injury.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Anandasivam NS, Russo GS, Swallow MS, Basques BA, Samuel AM, Ondeck NT, Chung SH, Fischer JM, Bohl DD, Grauer JN. Tibial shaft fracture: A large-scale study defining the injured population and associated injuries. J Clin Orthop Trauma. 2017;8(3):225–231. doi: 10.1016/j.jcot.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keon OJ, Hoon J, Wug OC, Biswal S. Treatment of femoral and tibial diaphyseal non-unions using reamed intramedullary nailing without bone graft. Injury. 2008;39(8):952–959. doi: 10.1016/j.injury.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 5.Duan, X., Al‐Qwbani, M., Zeng, Y., Zhang, W., & Xiang, Z. (2012). Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database of Systematic Reviews. [DOI] [PMC free article] [PubMed]
- 6.Phieffer LS, Goulet JA. Delayed unions of the tibia. Instructional Course Lectures. 2006;55:389–401. [PubMed] [Google Scholar]
- 7.Wu CC, Shih CH. Effect of dynamization of a static interlocking nail on fracture healing. Canadian Journal of Surgery. 1993;36(4):302–306. [PubMed] [Google Scholar]
- 8.Glatt V, Evans CH, Tetsworth K. A concert between biology and biomechanics: The influence of the mechanical environment on bone healing. Frontiers in Physiology. 2017;7:678. doi: 10.3389/fphys.2016.00678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. Journal of Bone and Joint Surgery. American Volume. 1985;67(5):709–720. doi: 10.2106/00004623-198567050-00005. [DOI] [PubMed] [Google Scholar]
- 10.Rupp M, Biehl C, Budak M, Thormann U, Heiss C, Alt V. Diaphyseal long bone non-unions—Types, aetiology, economics, and treatment recommendations. International Orthopaedics. 2018;42(2):247–258. doi: 10.1007/s00264-017-3734-5. [DOI] [PubMed] [Google Scholar]
- 11.Papakostidis C, Psyllakis I, Vardakas D, Grestas A, Giannoudis PV. Femoral-shaft fractures and non-unions treated with intramedullary nails: The role of dynamization. Injury. 2011;42(11):1353–1361. doi: 10.1016/j.injury.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 12.Vaughn J, Gotha H, Cohen E, Fantry AJ, Feller RJ, Van Meter J, Hayda R, Born CT. Nail dynamization for delayed union and non-union in femur and tibia fractures. Orthopedics. 2016;39(6):1117–1123. doi: 10.3928/01477447-20160819-01. [DOI] [PubMed] [Google Scholar]
- 13.Perumal R, Shankar V, Basha R, Jayaramaraju D, Rajasekaran S. Is nail dynamization beneficial after twelve weeks—An analysis of 37 cases. Journal of Clinical Orthopaedics and Trauma. 2018;9(4):322–326. doi: 10.1016/j.jcot.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whelan DB, Bhandari M, Stephen D, Kreder H, McKee MD, Zdero R, Schemitsch EH. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. Journal of Trauma. 2010;68(3):629–632. doi: 10.1097/TA.0b013e3181a7c16d. [DOI] [PubMed] [Google Scholar]
- 15.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. Journal of Orthopaedic Trauma. 2018;32(Suppl 1):S1–S170. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 16.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. Journal of Bone and Joint Surgery. American Volume. 1976;58(4):453–458. doi: 10.2106/00004623-197658040-00004. [DOI] [PubMed] [Google Scholar]
- 17.Spencer RF. The effect of head injury on fracture healing. A quantitative assessment. Journal of Bone and Joint Surgery. British Volume. 1987;69(4):525–528. doi: 10.1302/0301-620X.69B4.3611151. [DOI] [PubMed] [Google Scholar]
- 18.Manjunatha A, Santhosha J. Evaluation of results after dynamization of interlocking nail in diaphyseal fractures of femur and tibia. National Journal of Clinical Orthopaedics. 2019;3(4):75–79. doi: 10.33545/orthor.2019.v3.i4b.181. [DOI] [Google Scholar]
- 19.Jain G, Taneja D, Bangani P. Effect of dynamization in delayed union tibia shaft fracture. Indian Journal of Orthopaedics Surgery. 2017;3(4):372–377. [Google Scholar]
- 20.Tigani D, Fravisini M, Stagni C, Pascarella R, Boriani S. Interlocking nail for femoral shaft fractures: Is dynamization always necessary? International Orthopaedics. 2005;29(2):101–104. doi: 10.1007/s00264-004-0627-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Litrenta J, Tornetta P, 3rd, Vallier H, et al. Dynamizations and exchanges: Success rates and indications. Journal of Orthopaedic Trauma. 2015;29(12):569–573. doi: 10.1097/BOT.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 22.Chalidis BE, Petsatodis GE, Sachinis NC, Dimitriou CG, Christodoulou AG. Reamed interlocking intramedullary nailing for the treatment of tibial diaphyseal fractures and aseptic non-unions. Can we expect an optimum result? Strategies in Trauma and Limb Reconstruction. 2009;4(2):89–94. doi: 10.1007/s11751-009-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]