Abstract
BACKGROUND
Retroperitoneal lipomas are extremely rare tumors and tend to be large in size (> 10 cm) when diagnosed, causing various clinical manifestations. Preoperative diagnosis of retroperitoneal lipomas is difficult. There is a lack of relevant information about the management and prognosis of these benign tumors due to limited reports.
CASE SUMMARY
A 53-year-old woman who complained about progressive abdominal distention and aggravating satiety was referred to the gynecological outpatient department of Peking Union Medical College Hospital. Computerized tomography (CT) revealed an immense mass with fat density, measuring 28.6 cm× 16.6 cm in size. Adjacent organs, including the intestinal tract and uterus, were squeezed to the right side of the abdomen. An exploratory laparotomy was performed with suspicion of liposarcoma. Intraoperatively, a giant yellowish lobulated mass was found occupying the retroperitoneum and it was removed by tumor debulking. Postoperative histopathological results confirmed the diagnosis of retroperitoneal lipoma.
CONCLUSION
Retroperitoneal lipoma is a very rare condition and is difficult to differentiate from well-differentiated liposarcoma. Radiographic investigations, especially CT and magnetic resonance imaging, are important for preoperative diagnosis. Surgical resection is the fundamental treatment, which is difficult due to its size and relation to neighboring structures.
Keywords: Retroperitoneal lipoma, Well-differentiated liposarcoma, Retroperitoneal tumors, Treatment, Prognosis, Case report
Core Tip: Retroperitoneal lipomas are rare benign tumors originating from adipose tissues and they tend to have large sizes. Imaging examinations, especially computerized tomography and magnetic resonance imaging, are fundamental diagnostic tools for these tumors. Surgical resection is the main treatment method. En bloc resection is commonly required. Postoperative histopathology determines the final diagnosis, and immunohistochemical analysis could be useful in the differentiation of liposarcomas. Regular follow-ups are also required for the patients.
INTRODUCTION
Lipomas are a category of benign tumors originating from well-differentiated adipocytes. Their predilection sites are subdermal tissues of the trunk and extremities[1,2]. Retroperitoneal lipomas are a rare condition, with just 22 case reports describing the tumour in adults in the previous literature of PubMed since 1970[3-22]. They account for 2.9% of primary retroperitoneal tumors, approximately 80% of which are known as malignant[6,23,24]. Unlike subcutaneous lipomas, which are related to obesity, hyperlipidaemia, and injuries, retroperitoneal lipomas have an unknown aetiology[5,25-27]. On account of the rarity and limited knowledge of these tumors, further reports and investigations are necessary. In this report, we describe the case of a 53-year-old postmenopausal woman who presented with a massive fatty retroperitoneal mass measuring 28.6 cm× 16.6 cm and weighing 7.126 kg.
CASE PRESENTATION
Chief complaints
A 53-year-old postmenopausal woman who complained about progressive abdominal distention and aggravating satiety was referred to the department of gynaecology in our center.
History of present illness
The patient started to feel intensifying abdominal distention and satiety for the last 2 mo. She also found a significant increase in abdominal circumference and thinning of the limbs. The patient denied other discomforts, including fever, abdominal pain, nausea, and vomiting. The patient had been postmenopausal for 5 years and did not report abnormal vaginal bleeding.
History of past illness
The patient had a 10-year history of hypertension and took Loxone once per day, with stable control of blood pressure. The patient denied any history of diabetes, coronary heart disease, or malignancy. She also reported no drug allergy or other physical impairment. Additionally, the patient did not receive regular physical examinations, and the last medical examination had occurred more than 10 years prior.
Personal and family history
No noteworthy personal or family history was reported by the patient.
Physical examination
The patient’s height was 161 cm, and her weight was 60 kg (body mass index: 23.3, within the normal range). The physical examination revealed a palpable giant abdominal mass reaching the xiphisternum with a rubbery consistency. Other clinical symptoms, including tenderness, rebound tenderness, and mobile turbid sounds, were found.
Laboratory examinations
After hospitalization, the patient received a series of laboratory examinations for testing liver and kidney function, faecal occult blood, blood coagulation factors, electrolyte panel, and tumor biomarkers. The laboratory findings fell within the normal range.
Imaging examinations
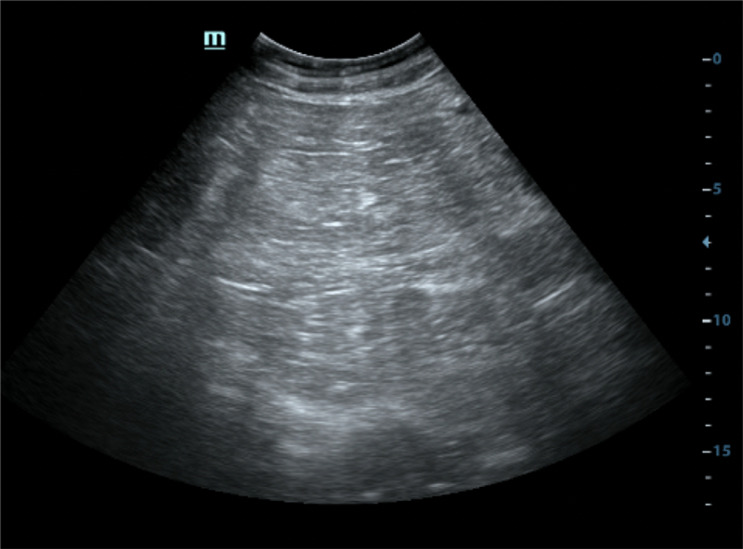
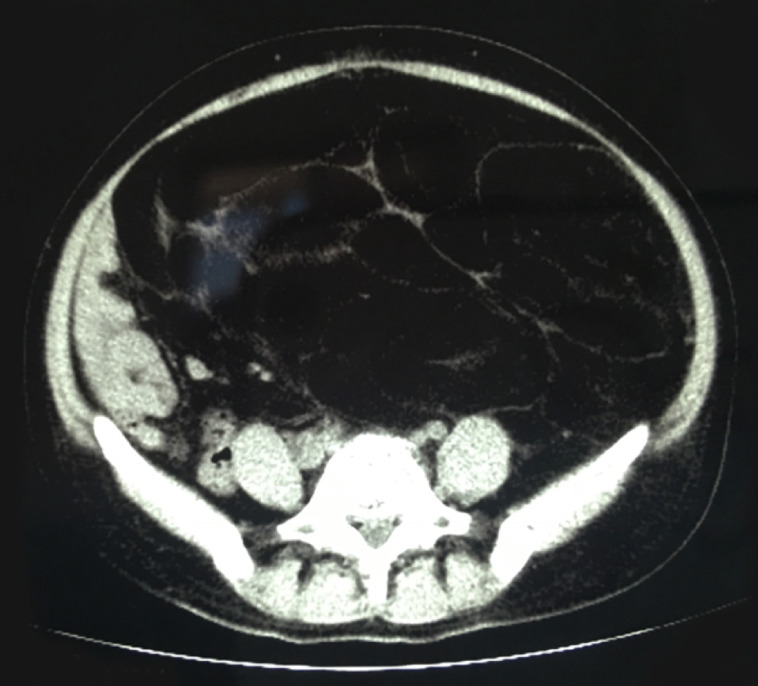
The patient had received a computed tomography (CT) plain scan at another hospital, and was re-evaluated by ultrasonography at our hospital. A massive hyperechoic mass, approximately 30 cm × 17 cm in size, was visualized via ultrasound. The mass was clearly defined and had internal echogenicity, filled with stripe-like structures. Minimal blood signals were detected by colour Doppler ultrasound (Figure 1). A CT plain scan demonstrated a giant homogeneous mass mainly consisting of fatty tissue and thin septa. It measured 16.6 cm × 28.6 cm in volume and pushed the peritoneal contents, such as the bowel loops and uterus, to the right part of the abdomen (Figure 2).
Figure 1.
Abdominal ultrasonography of the mass. A giant hyperechoic mass filling the abdomen was presented on grey-scale ultrasound. The mass had a relative clear margin and internal septas.
Figure 2.
Abdominal computed tomography in the axial plane. Computed tomography imaging showed a giant homogenous mass, mainly consisting of fatty tissue measuring 16.6 cm × 28.6 cm with thin septa, pushing the peritoneal containing such as bowel loops and uterus to the right part of abdomen.
FINAL DIAGNOSIS
Based on the clinical manifestations, normal laboratory examinations, and imaging examinations indicating its adipose origin, the clinicians considered the mass to be a giant retroperitoneal lipoma. However, the possibility of malignancy cannot be overlooked due to its large size.
TREATMENT
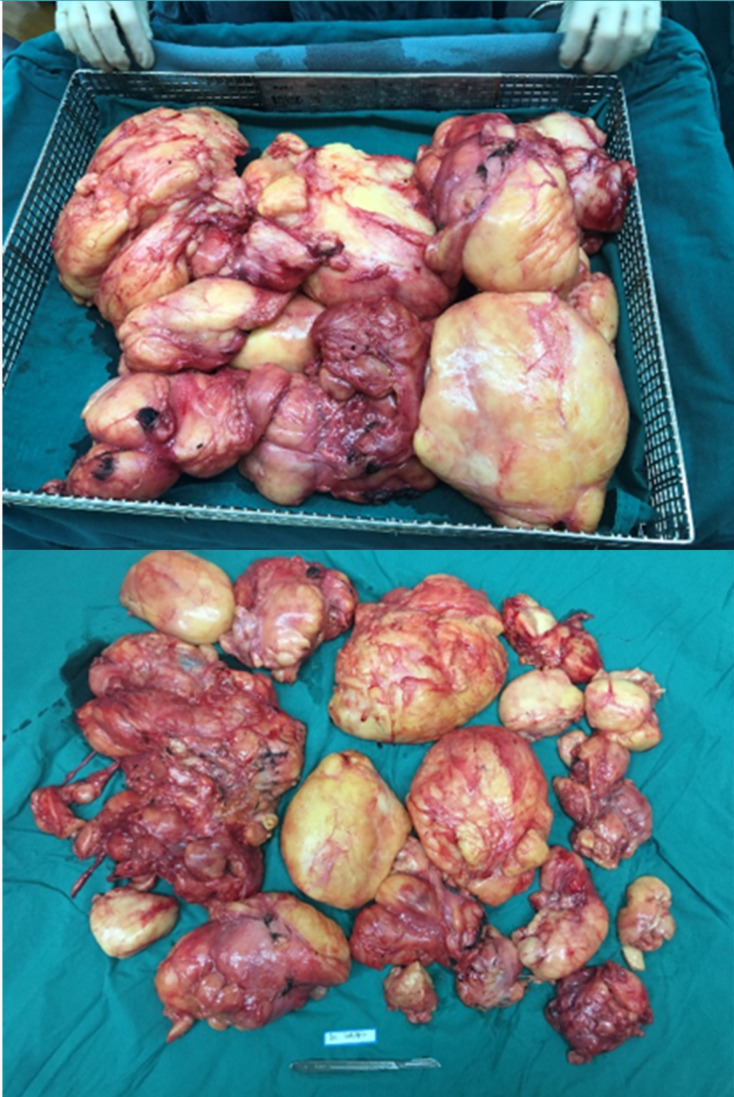
After completing the examinations and preoperative assessments, the patient underwent an exploratory laparotomy with the suspicion of malignancy, most likely retroperitoneal liposarcoma. During the operation, a bulky yellowish tumor originating from perirenal fatty tissues in the left retroperitoneal region was found to occupy the retroperitoneum. The uterus and adnexa were displaced by the mass. The mass adhered to the left psoas major muscle and wrapped around the left ureter, making it unfeasible to perform en bloc resection. After carefully separating the left ureter, we performed tumor debulking and resection of the left adnexa, which was also tightly adhered to the tumor. The total weight of the mass was 7.126 kg (Figure 3). The frozen pathological results suggested that the mass mainly consisted of adipose tissues, and a retroperitoneal lipomatous tumor was considered.
Figure 3.
Macroscopic view of extracted retroperitoneal lipoma. During the operation, a bulky yellowish tumor, originating from the left retroperitoneal region, was found to occupy the retroperitoneum. The mass weighted 7.126 kg.
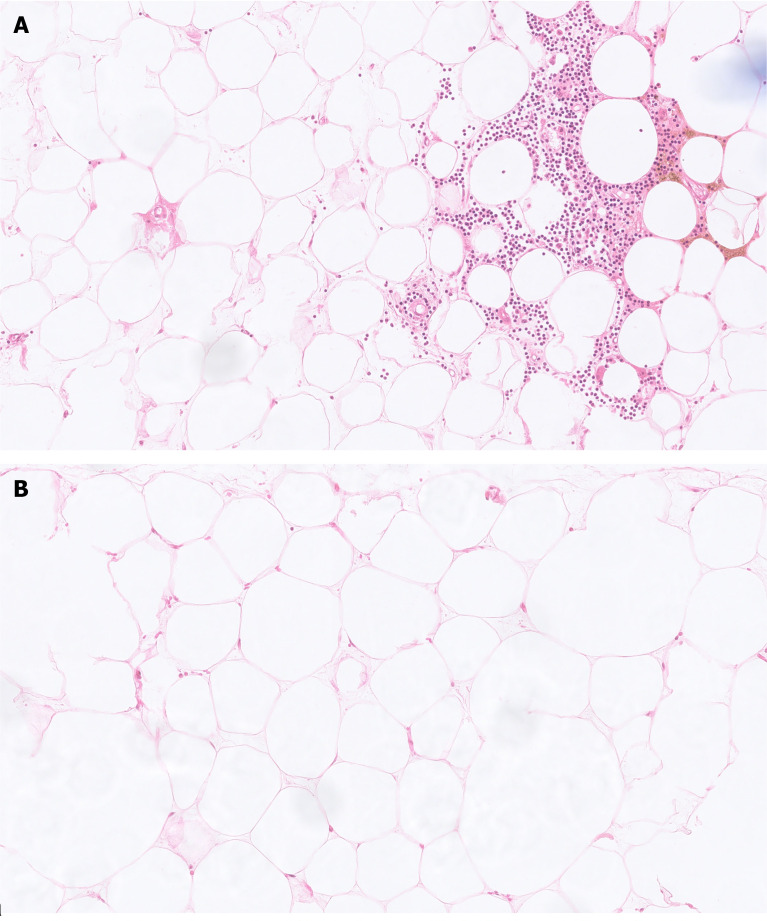
After 1 wk of uneventful hospitalization, the patient was discharged from the hospital with full recovery from her clinical symptoms. The final paraffin pathology showed that the tumor was composed of mature adipose tissues and hematopoietic cells, without cytologic atypia, and confirmed the diagnosis of multiple lipomas and multiple myelolipomas (Figure 4).
Figure 4.
Microscopical picture of the extracted tumors (H&E, 20 ×). A: Myelolipoma was composed of mature adipose adipocytes and hematopoietic cells, without necrosis, atypia, and hyperchromatic cells; B: Conventional lipoma was composed of mature adipocytes.
OUTCOME AND FOLLOW-UP
The patient reported no relevant clinical symptoms after the operation. During a series of follow-ups for 18 mo, the laboratory tests and imaging examinations were normal and indicated no signs of relapse.
DISCUSSION
We herein report a massive retroperitoneal lipoma, which consisted of multiple conventional lipomas and multiple myelolipomas. Retroperitoneal lipomas are rare mesenchymal-originated tumors. It was first reported in 1947[22], and since then, a total of 22 cases have been reported in adults sporadically (Table 1). The peak incidence of adult retroperitoneal lipomas occurs between the ages of 40 and 60, with no discernible gender predisposition. According to the morphologic characteristics, lipomas can be subdivided into conventional lipoma, fibrolipoma, angiolipoma, spindle cell lipoma, pleomorphic lipoma, and myelolipoma[7], of which, almost all myelolipomas have been identified inside the adrenal gland, with just about 50 cases of myelolipomas being identified in extra-adrenal locations, such as the retroperinoneum[28]. The exact underlying aetiology of retroperitoneal lipomas is not well understood. Seeding after fibroid excision, exogenous hormone treatment, or chronic abnormalities in glucose homeostasis have all been blamed for these benign tumors. And genetic factors are thought to have an important role in adipocyte proliferation[5].
Table 1.
Summary of all case reports describing retroperitoneal lipomas resected in adults
|
Ref.
|
Age
|
Sex
|
Symptoms
|
Imaging methods
|
Tumor size (cm)
|
Tumor weight
|
Follow-up
|
| Cattell et al[22], 1947 | 55 | Female | 10 cm in diameter | ||||
| Cattell et al[22], 1947 | 61 | Female | Epigastric distress and bloating | 12700 g | |||
| Deppe et al[21], 1985 | 24 | Female | Barium enema, CT | 11 × 8 × 3 | NA | ||
| Zhang et al[20], 1987 | 65 | Male | Weight gain, leg edema | NA | 50 cm in diameter | 19500 g | 4 yr |
| Acheson et al[19], 1997 | 76 | Female | Swollen leg | CT, MRI | 20 × 20× 12 | 576 g | |
| Matsubara et al[18], 2000 | 65 | Male | NA | 12 × 13 | NA | ||
| Marshall et al[17], 2001 | 47 | Male | CT | NA | 4990 g | ||
| Forte et al[15], 2002 | 61 | Male | Urinary frequency, urgency and nocturia | CT | |||
| Foa et al[16], 2002 | 52 | Male | 10.5 × 9.5 × 2 | 145 g | |||
| Raftopoulos et al[14], 2002 | 62 | Male | Abdominal pain | CT | 20 × 15 × 10 | 790 g | |
| Martinez et al[12], 2003 | 32 | Female | Abdominal pain | US, barium enema | 20 × 13 × 10 | 3400 g | 17 yr |
| Drop et al[13], 2003 | 60 | Female | Abdominal pain, gastrointestinal symptoms | US, CT | 13 × 12 | ||
| Drop et al[13], 2003 | 72 | Female | Abdominal pain, sickness | US, CT | 12 × 9 × 4 | ||
| Ida et al[11], 2008 | 65 | Male | Painless swelling in left inguinal region | 22 × 14 × 5 | 18 mo | ||
| Ukita et al[10], 2009 | 61 | Female | Gluteal pain | MRI | 25 × 15 | ||
| Singh et al[9], 2011 | 65 | Male | Inguinal pain | 15.6 cm in diameter | NA | ||
| Chander et al[8], 2012 | 36 | Female | 13.6 × 11.2 × 9.1 | 1300 g | |||
| Wei et al[6], 2013 | 25 | Female | US | 20 × 12 × 10 | 1650 g | 6 mo | |
| Saito et al[7], 2013 | 65 | Male | Flank pain | US, CT | 30 cm in diameter | NA | |
| Weniger et al[5], 2015 | 73 | Female | Abdominal swelling, pain, and obstipation | CT | 55 × 40 × 10 | 8950 g | |
| Al-Ali et al[4], 2019 | 34 | Female | Abdominal distention and back pain | US, CT | 45 × 48 × 13 | 1200 g | 6 mo |
| Mitchell et al[3], 2020 | 29 | Female | Abdominal pain, distention, orthopnea | MRI | 28 × 14 × 6 |
CT: Computerized tomography; MRI: Magnetic resonance imaging; US: Ultrasonography; NA: Not available.
Retroperitoneal tumors are often asymptomatic for a long period of time throughout their early clinical course, owing to the vast potential spaces in the retroperitoneum. Local compression of surrounding organs and tissues, which can manifest obstructive urinary/bowel symptoms such as stomach pain, fullness, early satiety, or lower extremity oedema, may occur once the tumors have grown to gigantic sizes. The clinical presentations tend to be variable and nonspecific[4]. Hence, imaging examinations play an essential role in the diagnosis of these lesions.
Ultrasound is generally used for the initial diagnosis and screening of abdominal masses. Radiography, especially CT and magnetic resonance imaging (MRI), is a crucial diagnostic tool for further evaluation of retroperitoneal tumors. The characteristics of adipose tissues are consistent on CT and MRI, but they differ on ultrasonography depending on the physical properties and histologic types. The fatty content is the fundamental feature to identify fat-containing retroperitoneal tumors during imaging examinations. Typical lipomas appear as extensive hyperechoic lesions on ultrasound, while they appear as homogeneous fat-containing masses with thin septa on CT and MRI. Retroperitoneal lipomas are difficult to identify preoperatively since they mimic liposarcomas, which account for the majority of fat-containing retroperitoneal tumors. Liposarcomas present heterogeneous signal intensity and variable appearances on MRI and CT due to the varying subtypes, which included well-differentiated liposarcoma (WDLPS), dedifferentiated liposarcoma, myxoid/round cell liposarcoma, pleomorphic liposarcoma, and mixed liposarcoma. The increased vascularity in liposarcomas that present as low-intensity signals on T1-weighted images can be used for differentiation. However, both lipomas and WDLPS are accompanied by a large amount of fat and minimal soft tissue and have identical appearances on CT and MRI, making it hard to distinguish lipomas from well-differentiated liposarcomas preoperatively.
Due to the large size, the measurement of retroperitoneal tumors by preoperative imaging examinations can be inaccurate. Despite their typical presentations on CT and MRI, both imaging modalities may not rule out the possibility of WDLPS[29]. Approximately 80% of retroperitoneal tumors appear to be malignant, most of which are soft-tissue sarcomas, a category of very uncommon neoplasms, with an overall incidence of 0.3% to 0.4% per 100000 people[10]. Liposarcomas account for 41% of sarcomas, and the majority of the cases are malignant from the start. A few outliers arise from benign lipomas in the early stages[30]. The final diagnosis of lipomas depends on histopathology. Tissue for pathology can be acquired by fine-needle aspiration or core-needle biopsy, but it is nearly impossible to distinguish lipoma-like WDLPS and lipomas due to the limited tissue sample obtained by these methods for detecting atypia and hyperchromatic cells. Postoperative histopathology remains the gold standard for diagnosis. Histologic characteristics for WDLPS include mature adipocytes punctuated with big atypical hyperchromatic cells. However, WDLPS are likely to be misdiagnosed, because atypia may be localized, especially in deep lesions with tiny samples. Murine double minute (MDM2, located at 12q14-15) and cyclin-dependent kinase 4 gene are regularly amplified in WDLPS, which cannot be observed in benign lipomas. Hence, fluorescence in situ hybridization has emerged as a promising method for differential diagnosis[11,16,18].
It is of great importance to discern tumor characteristics intraoperatively and make decisions about the resection extent subsequently. In cases of the pathological diagnosis of liposarcoma, resection with negative margins (R0) is crucial. If infiltrative growth is detected by frozen pathology, a broad excision should be performed. Surgeons should also tailor personalized surgical strategies for patients with important involved adjacent structures who are unsuitable for an entire resection. Commonly, en bloc removal of the involved structures is required[3,5]. The prognosis and recurrence risk for patients with benign retroperitoneal lipomas are unclear due to the limited number of case reports. Patients are often recommended to receive regular clinical and radiologic follow-ups.
CONCLUSION
Retroperitoneal lipomas are rare benign tumors originating from adipose tissues and they tend to have large sizes. Imaging examinations, especially CT and MRI, are fundamental diagnostic tools for these tumors. Surgical resection is the main treatment method. En bloc resection is commonly required. Postoperative histopathology determines the final diagnosis, and immunohistochemical analysis could be useful in the differentiation of liposarcomas. Regular follow-ups are also required for the patients.
ACKNOWLEDGEMENTS
The authors are deeply grateful to Dr. Zhao H and Dr. Shi J for their help in reviewing the postoperative pathology.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict-of-interest statement: No conflict of interests exists to any of the authors.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: August 21, 2021
First decision: November 17, 2021
Article in press: January 8, 2022
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dhali A, Meglio LD S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Wang JL
Contributor Information
Zhi-Yan Chen, Department of Obstetrics and Gynecology, Peking Union Medical College Hospital, Beijing 100730, China.
Xian-Long Chen, Department of Pathology, Peking Union Medical College Hospital, Beijing 100730, China.
Qi Yu, Department of Obstetrics and Gynecology, Peking Union Medical College Hospital, Beijing 100730, China.
Qing-Bo Fan, Department of Obstetrics and Gynecology, Peking Union Medical College Hospital, Beijing 100730, China. qbfan@sohu.com.
References
- 1.Terada T. Giant fibrolipoma of the spermatic cord. Pathol Int . 2010;60:330–332. doi: 10.1111/j.1440-1827.2010.02521.x. [DOI] [PubMed] [Google Scholar]
- 2.Johnson CN, Ha AS, Chen E, Davidson D. Lipomatous Soft-tissue Tumors. J Am Acad Orthop Surg . 2018;26:779–788. doi: 10.5435/JAAOS-D-17-00045. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell K, Fuller K, Thomay A, Shapiro R. Diagnosis and Surgical Management of a Retroperitoneal Lipoma in Pregnancy. Case Rep Obstet Gynecol . 2020;2020:6309417. doi: 10.1155/2020/6309417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Ali MHM, Salih AM, Ahmed OF, Kakamad FH, Mohammed SH, Hassan MN, Sidiq SH, Mustafa MQ, Najar KA, Abdullah IY. Retroperitoneal lipoma; a benign condition with frightening presentation. Int J Surg Case Rep . 2019;57:63–66. doi: 10.1016/j.ijscr.2019.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weniger M, D’Haese JG, Kunz W, Pratschke S, Guba M, Werner J, Angele MK. En-bloc resection of a giant retroperitoneal lipoma: a case report and review of the literature. BMC Res Notes . 2015;8:75. doi: 10.1186/s13104-015-1038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei D, Shen L, Yang K, Fang F. Giant retroperitoneal lipoma in a pregnant patient. J Obstet Gynaecol . 2013;33:522. doi: 10.3109/01443615.2013.788621. [DOI] [PubMed] [Google Scholar]
- 7.Saito S. Retroperitoneal lipoma presenting with nutcracker-like phenomenon. Case Rep Urol . 2013;2013:893242. doi: 10.1155/2013/893242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chander B, Krishna M, Thakur S, Mahajan N, Vij A, Diwakaran J. Extremely rare giant retroperitoneal fibrolipoma: a case report. J Cancer Res Ther . 2012;8:314–316. doi: 10.4103/0973-1482.99002. [DOI] [PubMed] [Google Scholar]
- 9.Singh G, Bharadwaj RN, Purandare SN, Gore CR, Dubhashi SP, Vaidya S, Patil A, Kompally GR. Giant retroperitoneal lipoma presenting as inguinal hernia. Indian J Surg . 2011;73:187–189. doi: 10.1007/s12262-010-0210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ukita S, Koshiyama M, Ohnaka M, Miyagawa N, Yamanishi Y, Nishimura F, Nagura M, Kim T, Hirose M, Shirase T, Kobayashi H, Ozasa H. Retroperitoneal lipoma arising from the urinary bladder. Rare Tumors . 2009;1:e13. doi: 10.4081/rt.2009.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ida CM, Wang X, Erickson-Johnson MR, Wenger DE, Blute ML, Nascimento AG, Oliveira AM. Primary retroperitoneal lipoma: a soft tissue pathology heresy? Am J Surg Pathol . 2008;32:951–954. doi: 10.1097/pas.0b013e318160cfbf. [DOI] [PubMed] [Google Scholar]
- 12.Martinez CA, Palma RT, Waisberg J. Giant retroperitoneal lipoma: a case report. Arq Gastroenterol . 2003;40:251–255. doi: 10.1590/s0004-28032003000400010. [DOI] [PubMed] [Google Scholar]
- 13.Drop A, Czekajska-Chehab E, Maciejewski R. Giant retroperitoneal lipomas--radiological case report. Ann Univ Mariae Curie Sklodowska Med . 2003;58:142–146. [PubMed] [Google Scholar]
- 14.Raftopoulos I, Lee T, Byrne MP. Image of the month: retroperitoneal lipoma. Arch Surg . 2002;137:865–866. doi: 10.1001/archsurg.137.7.865. [DOI] [PubMed] [Google Scholar]
- 15.Forte F, Maturo G, Catania A, Sorrenti S, Gemma D, Foti N, Vanni B, Virgili G, Vespasiani G, De Antoni E. Retroperitoneal lipoma. Unusual presentation with detrusor instability. Minerva Urol Nefrol . 2002;54:131–133. [PubMed] [Google Scholar]
- 16.Foa C, Mainguené C, Dupré F, Coindre JM, Huguet C, Kober C, Pedeutour F. Rearrangement involving chromosomes 1 and 8 in a retroperitoneal lipoma. Cancer Genet Cytogenet . 2002;133:156–159.. doi: 10.1016/s0165-4608(01)00573-8. [DOI] [PubMed] [Google Scholar]
- 17.Marshall MT, Rosen P, Berlin R, Greenson N. Appendicitis masquerading as tumor: a case of two diagnoses. J Emerg Med . 2001;21:397–399. doi: 10.1016/s0736-4679(01)00422-x. [DOI] [PubMed] [Google Scholar]
- 18.Matsubara N, Yoshitaka T, Matsuno T, Ikeda M, Isozaki H, Tanaka N, Shimizu K. Multiple tumors and a novel E2F-4 mutation. A case report. Digestion . 2000;62:213–216. doi: 10.1159/000007816. [DOI] [PubMed] [Google Scholar]
- 19.Acheson A, McIlrath E, Barros D'Sa AA. Pelvic lipoma causing venous obstruction syndrome. Eur J Vasc Endovasc Surg . 1997;14:149–150. doi: 10.1016/s1078-5884(97)80213-4. [DOI] [PubMed] [Google Scholar]
- 20.Zhang SZ, Yue XH, Liu XM, Lo SL, Wang XZ. Giant retroperitoneal pleomorphic lipoma. Am J Surg Pathol . 1987;11:557–562. [PubMed] [Google Scholar]
- 21.Deppe G, Malviya VK, Hercule J, Gleicher N. Retroperitoneal pelvic lipoma. J Natl Med Assoc . 1985;77:574–576. [PMC free article] [PubMed] [Google Scholar]
- 22.Cattell RB, Warren KW. Retroperitoneal lipoma. Surg Clin North Am . 1947;27:659–665. doi: 10.1016/s0039-6109(16)32148-x. [DOI] [PubMed] [Google Scholar]
- 23.Pai MR, Naik R, Raghuveer CV. Primary retroperitoneal tumors a 25 year study. Indian J Med Sci . 1995;49:139–141. [PubMed] [Google Scholar]
- 24.Armstrong JR, Cohn I. Primary malignant retroperitoneal tumors. Am J Surg . 1965;110:937–943. doi: 10.1016/0002-9610(65)90181-9. [DOI] [PubMed] [Google Scholar]
- 25.Rubinstein A, Goor Y, Gazit E, Cabili S. Non-symmetric subcutaneous lipomatosis associated with familial combined hyperlipidaemia. Br J Dermatol . 1989;120:689–694. doi: 10.1111/j.1365-2133.1989.tb01357.x. [DOI] [PubMed] [Google Scholar]
- 26.Self TH, Akins D. Dramatic reduction in lipoma associated with statin therapy. J Am Acad Dermatol . 2008;58:S30–S31. doi: 10.1016/j.jaad.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 27.Pires Botelho da Costa JS, Reis JC, Valença-Filipe R. Giant atypical lipoma of the thigh. Dermatol Surg . 2014;40:213–214. doi: 10.1111/dsu.12397. [DOI] [PubMed] [Google Scholar]
- 28.Cho J, Kinsey D, Kimchi ET, O'Carroll KS, Nguyen V, Alsabbagh M, Gaballah A. Retroperitoneal extra-adrenal myelolipoma misdiagnosed as liposarcoma: A case report. Radiol Case Rep . 2021;16:364–368. doi: 10.1016/j.radcr.2020.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shaaban AM, Rezvani M, Tubay M, Elsayes KM, Woodward PJ, Menias CO. Fat-containing Retroperitoneal Lesions: Imaging Characteristics, Localization, and Differential Diagnosis. Radiographics . 2016;36:710–734. doi: 10.1148/rg.2016150149. [DOI] [PubMed] [Google Scholar]
- 30.Vijay A, Ram L. Retroperitoneal liposarcoma: a comprehensive review. Am J Clin Oncol . 2015;38:213–219. doi: 10.1097/COC.0b013e31829b5667. [DOI] [PubMed] [Google Scholar]