Abstract
Background
The impact of a postoperative diagnosis of COVID-19 in patients undergoing total joint arthroplasty (TJA) remains unknown. The objective of this study is to characterize the effect of COVID-19 infection following TJA on perioperative complication rates.
Methods
The Mariner database was queried for patients undergoing total hip and total knee arthroplasty from January 2018 to April 2020. TJA patients who were diagnosed with COVID-19 within 90 days postoperatively were matched in a 1:3 fashion based on age, gender, iron deficiency anemia, payer status, and Charlson Comorbidity Index with patients who were not diagnosed with COVID-19. Preoperative comorbidity profiles and complications within 3 months of surgery were compared. Statistical analysis included chi-squared tests and multivariate logistic regression with outcomes considered significant at P < .05.
Results
Of the 239 COVID-19 positive patients, 132 (55.2%) underwent total hip arthroplasty. On multivariate analysis, COVID-19 diagnosis was associated with increased odds of deep vein thrombosis (odds ratio [OR] 4.86, 95% confidence interval [CI] 2.10-11.81, P < .001), pulmonary embolism (OR 6.27, 95% CI 2.57-16.71, P < .001), and all complications (OR 3.36, 95% CI 2.47-4.59, P < .001). Incidence of deep vein thrombosis/pulmonary embolism was greater the closer in time the COVID-19 diagnosis was to the surgical procedure (10.24 times at 1 month, 7.87 times at 2 months, and 1.42 times at 3 months; P < .001). A similar relationship was observed with all complications.
Conclusion
Postoperative COVID-19 infection is associated with higher rates of cardiopulmonary complications, thromboembolic disease, renal injury, and urinary tract infections in patients undergoing hip and knee arthroplasty. COVID-19 infection earlier in the postoperative period is associated with a higher risk of complications.
Keywords: COVID-19, coronavirus, total knee arthroplasty, total hip arthroplasty, total joint arthroplasty, thromboembolism
The 2020 global pandemic caused by the novel coronavirus, SARS-CoV-2, severely affected the delivery of healthcare in the United States [1,2]. Abruptly, efforts and resources were focused on the treatment and prevention of Coronavirus Disease 2019 (COVID-19). To that end, elective surgeries were cancelled or significantly limited [[3], [4], [5], [6], [7], [8]]. Total joint arthroplasty (TJA) is one of the most common elective procedures, with more than 1 million procedures completed annually in the United States prior to the COVID-19 pandemic [9,10]. Surgical volumes surrounding TJA dropped precipitously during the pandemic [11]. Bedard et al [12] estimated that approximately 30,000 primary and 3000 revision TJA cases would be cancelled each week while COVID-19 restrictions for elective surgery were in place, highlighting the extraordinary toll on healthcare systems and patients alike [13].
Development of perioperative protocols, utilization of ambulatory surgery centers, and the rollout of COVID-19 vaccinations have allowed for safe reintroduction of elective procedures, including TJA [13]. The return to prepandemic surgical volumes is beneficial to patients with hip and knee osteoarthritis who have been delayed in receiving care, which has been linked to increased mortality and comorbidities [14]. Although extensive measures have been instituted to ensure the safety of the surgical encounter for TJA, perioperative COVID-19 infection appears to increase patient morbidity. A large, international, multicenter cohort study found that a recent diagnosis of COVID-19 was associated with a statistically significant increased risk of pulmonary complications and mortality in specific patient populations, including male sex and patients over 70 [15]. Investigators from the United Kingdom assessed the independent association of COVID-19 on postoperative mortality in patients undergoing orthopedic and trauma surgery and found that perioperative COVID-19 infections nearly doubled the mortality risk postoperatively [16].
It remains unclear how postoperative COVID-19 infection affects complication rates among patients undergoing TJA. The purpose of the present study is to characterize the effect of coronavirus infection following hip and knee arthroplasty. Additionally, we sought to determine if the timing of coronavirus infection impacts morbidity.
Methods
The Mariner administrative claims database was queried using the PearlDiver Patient Record Database (PearlDiver Inc, Fort Wayne, IN; www.pearldiverinc.com). This database houses deidentified patient information from a variety of payer types including commercial, Medicare, Medicaid, government, and cash payers from 2018 to 2020. Data regarding patient demographics, medical comorbidities, postoperative complications, insurance coverage, geographic information, and procedural volumes were queried using International Classification of Disease Ninth and Tenth Revision (ICD-9 and ICD-10) codes, Current Procedural Terminology (CPT) codes, and National Drug Codes. This study was granted exemption from the Institutional Review Board as PearlDiver uses deidentified patient information and therefore is compliant with the Health Insurance Portability and Accountability Act.
A retrospective analysis of patients undergoing total hip arthroplasty (THA) and total knee arthroplasty (TKA), referred to collectively as TJA was performed from January 2018 to April 2020. All patients who underwent THA and TKA were identified using the Current Procedural Terminology codes 27130 and 27447, respectively. Patients who were not active within the database for at least 6 months prior and 3 months after their TJA procedure were excluded.
The cohort of patients who were diagnosed with COVID-19 following TJA was determined using the ICD-10 diagnosis code, ICD-10-D-U07.1. The “First instance” coding language was used to capture patients with a new diagnosis of COVID-19. Longitudinal tracking and sequential coding within the PearlDiver database allowed us to identify 90-day adverse events including superficial surgical site infection, prosthetic joint infection, deep vein thrombosis (DVT), pulmonary embolism (PE), acute kidney injury (AKI), cardiac arrest, wound disruption, postoperative hematoma, nerve injury, pneumonia, blood transfusion, and urinary tract infection diagnosed within 3 months. The “All complications” variable represents the pooled risk of one of the above complications. Pneumonia was excluded from pooled analysis to prevent overinflation secondary to pneumonia diagnosis codes in COVID-positive patients. The corresponding ICD-9/10 diagnosis codes which were used to define these diagnoses can be found in the Appendix.
Patients newly diagnosed with COVID-19 within 3 months following TJA were included in the experimental group. A 1:3 matched cohort analysis was performed with COVID-naïve patients based on procedure (THA or TKA), age, gender, iron deficiency anemia, payer status, and Charlson Comorbidity Index to derive a control cohort of TJA patients who underwent TJA between 2018 and 2020 and were not diagnosed with COVID-19 prior to or in the 3 months following surgery. Demographic characteristics and complication rates were compared between matched and unmatched cohorts. In order to evaluate the effect of timing of a COVID-19 diagnosis on postoperative complications, 3 groups were formed on the basis of duration in months between TJA and COVID-19 diagnosis: within 1 month, between 1 and 2 months, and between 2 and 3 months.
Descriptive statistics with t-tests were performed to report the incidence of postoperative complications. Chi-squared tests were used to evaluate the difference in categorical variables while Student’s t-tests were used to determine differences in continuous variables, such as age. Multivariate regression was performed to identify the risk of developing postoperative complications if diagnosed with COVID-19 within 3 months of TJA and resulting odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. The temporal relationship between COVID-19 infection and TJA was assessed by binary logistic regression. Univariate and multivariate analysis was performed using the open-source R tool (www.r-project.org) housed within PearlDiver. Statistical significance was defined as P < .05.
Results
A total of 239 patients diagnosed with COVID-19 within 3 months following primary TJA were identified and matched with 713 control patients. Of the 239 COVID-19 positive patients, 132 (55.2%) underwent THA and 107 (44.8%) underwent TKA. After matching, the COVID-19 positive cohort and their matched controls demonstrated no significant differences with respect to demographic and medical comorbidities (Table 1 ).
Table 1.
Demographic Comparison of Patients Diagnosed With COVID-19 Within 3 mo of TJA and Controls Not Diagnosed With COVID, Unmatched and Matched Data.
| Matched |
Unmatched |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TJA, COVID+, n (%) | TJA, No COVID, n (%) | P-Value | TJA, COVID+, n (%) | TJA, No COVID, n (%) | P-Value | |||||
| Total | 239 | 713 | Reference | 312 | 5368 | Reference | ||||
| THA | 132 | 55.2% | 395 | 55.4% | 1.000 | 194 | 62.2% | 2209 | 41.2% | <.001a |
| Demographics | ||||||||||
| Age, mean, SD | 72.9 | 8.4 | 72.6 | 8.3% | 1.000 | 73.0 | 9.7% | 66.4 | 9.9% | <.001a |
| Gender | 1.000 | .711 | ||||||||
| Male | 88 | 36.8% | 261 | 36.6% | 125 | 40.1% | 2085 | 38.8% | ||
| Female | 151 | 63.2% | 452 | 63.4% | 187 | 59.9% | 3283 | 61.2% | ||
| Plan | .317 | .036a | ||||||||
| Commercial | 136 | 57.0% | 391 | 54.9% | 169 | 54.2% | 3361 | 62.6% | ||
| Medicaid | 15 | 6.2% | 32 | 4.5% | 18 | 5.8% | 259 | 4.8% | ||
| Medicare | 80 | 33.5% | 277 | 38.9% | 116 | 37.2% | 1636 | 30.5% | ||
| Comorbidities | ||||||||||
| Hypertension | 173 | 72.4% | 502 | 70.4% | .617 | 237 | 76.0% | 3558 | 66.3% | <.001a |
| COPD | 33 | 13.8% | 93 | 13.0% | .848 | 55 | 17.6% | 854 | 15.9% | .468 |
| CHF | 3 | 1.3% | 3 | 0.4% | .348 | 5 | 1.6% | 198 | 3.7% | .076 |
| Smoking | 5 | 2.1% | 11 | 1.5% | .779 | 7 | 2.2% | 300 | 5.6% | .016 |
| CKD | 43 | 18.0% | 130 | 18.2% | 1.000 | 79 | 25.3% | 639 | 11.9% | <.001a |
| Diabetes | 76 | 31.8% | 232 | 32.5% | .895 | 109 | 34.9% | 1731 | 32.2% | .355 |
| Obesity | 59 | 24.7% | 161 | 22.6% | .562 | 76 | 24.4% | 1259 | 23.5% | .766 |
| Depression | 54 | 22.6% | 123 | 17.3% | .082 | 76 | 24.4% | 804 | 15.0% | <.001a |
| Hypothyroidism | 38 | 15.9% | 107 | 15.0% | .819 | 50 | 16.0% | 817 | 15.2% | .761 |
| PVD | 29 | 12.1% | 109 | 15.3% | .275 | 57 | 18.3% | 639 | 11.9% | .001a |
| Coagulopathy | 11 | 4.6% | 39 | 5.5% | .724 | 21 | 6.7% | 229 | 4.3% | .055a |
| Cancer | 46 | 19.2% | 126 | 17.7% | .652 | 75 | 24.0% | 778 | 14.5% | <.001a |
| Iron deficiency anemia | 32 | 13.2% | 62 | 8.7% | .058 | 50 | 16.0% | 399 | 7.4% | <.001a |
| Liver disease | 12 | 5.0% | 36 | 5.0% | 1.000 | 19 | 6.1% | 267 | 5.0% | .457 |
| Alcohol use | 9 | 3.8% | 14 | 2.0% | .185 | 12 | 3.8% | 124 | 2.3% | .125 |
TJA, total joint arthroplasty; THA, total hip arthroplasty; SD, standard deviation; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; CKD, chronic kidney disease; PVD, peripheral vascular disease.
Indicates statistical significance of P < .05.
On univariate analysis, patients diagnosed with COVID-19 infection postoperatively had a significantly higher risk of complications including DVT (5.9% vs 1.3%), PE (5.9% vs 1.0%), AKI (22.6% vs 6.9%), cardiac arrest (2.9% vs 0.3%), pneumonia (55.2% vs 4.8%), transfusion (7.1% vs 2.2%), urinary tract infection (19.2% vs 10.8%), and all complications, excluding pneumonia (48.1% vs 21.7%; Table 2 ).
Table 2.
Complication Rate Comparison of Patients Diagnosed With COVID-19 Within 3 mo of TJA and Controls Not Diagnosed With COVID, Unmatched and Matched Data.
| Matched |
Unmatched |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TJA, COVID+, n (%) | TJA, No COVID, n (%) | P-Value | TJA, COVID+, n (%) | TJA, No COVID, n (%) | P-Value | |||||
| Total patients | 239 | 713 | Reference | 312 | 5368 | Reference | ||||
| Superficial surgical site infection | 3 | 1.3% | 6 | 0.8% | .853 | 4 | 1.3% | 76 | 1.4% | 1.000 |
| Prosthetic joint infection | 3 | 1.3% | 2 | 0.3% | .198 | 5 | 1.6% | 21 | 0.4% | .008a |
| Deep vein thrombosis | 14 | 5.9% | 9 | 1.3% | <.001a | 14 | 4.5% | 144 | 2.7% | .088 |
| Pulmonary embolism | 14 | 5.9% | 7 | 1.0% | <.001a | 16 | 5.1% | 55 | 1.0% | <.001a |
| Acute kidney injury | 54 | 22.6% | 49 | 6.9% | <.001a | 72 | 23.1% | 271 | 5.0% | <.001a |
| Cardiac arrest | 7 | 2.9% | 2 | 0.3% | .001a | 9 | 2.9% | 3 | 0.1% | <.001a |
| Wound disruption | 8 | 3.3% | 13 | 1.8% | .257 | 12 | 3.8% | 114 | 2.1% | .070 |
| Postoperative hematoma | 0 | 0.0% | 0 | 0.0% | 1.000 | 0 | 0.0% | 37 | 0.7% | .267 |
| Nerve injury | 0 | 0.0% | 0 | 0.0% | 1.000 | 0 | 0.0% | 0 | 0.0% | 1.000 |
| Pneumonia | 132 | 55.2% | 34 | 4.8% | <.001a | 168 | 53.8% | 158 | 2.9% | <.001a |
| Transfusion | 17 | 7.1% | 16 | 2.2% | <.001a | 24 | 7.7% | 242 | 4.5% | <.001a |
| Urinary tract infection | 46 | 19.2% | 77 | 10.8% | .001a | 62 | 19.9% | 450 | 8.4% | <.001a |
| All complicationsb | 115 | 48.1% | 155 | 21.7% | <.001a | 155 | 49.7% | 1096 | 20.4% | <.001a |
TJA, total joint arthroplasty.
Bold values indicate statistical significance of P < .05.
Indicates statistical significance of P < .05.
Includes rate of all complications, excluding pneumonia.
On multivariate analysis, COVID-19 infection was associated with an increased odds of DVT (OR 4.86, 95% CI 2.10-11.81), PE (OR 6.27, 95% CI 2.57-16.71), AKI (OR 4.03, 95% CI 2.65-6.17), cardiac arrest (OR 10.71, 95% CI 2.57-51.92), pneumonia (OR 25.38, 95% CI 16.66-39.65), urinary tract infection (OR 1.99, 95% CI 1.33-2.97), and all complications (OR 3.36, 95% CI 2.47-4.59; Table 3 ).
Table 3.
Multivariate Analysis of Risk of Complication for Patients Who Were Diagnosed With COVID-19 Within 3 mo of TJA.
| Complication | OR (95% CI) | P-Value |
|---|---|---|
| Superficial surgical site infection | 1.50 (0.31-5.71) | .571 |
| Prosthetic joint infection | 4.51 (0.74-27.17) | .099 |
| Deep vein thrombosis | 4.86 (2.10-11.81) | <.001a |
| Pulmonary embolism | 6.27 (2.57-16.71) | <.001a |
| Acute kidney injury | 4.03 (2.65-6.17) | <.001a |
| Cardiac arrest | 10.71 (2.57-51.92) | .003a |
| Wound disruption | 1.86 (0.73-4.47) | .172 |
| Hematoma | N/A | N/A |
| Nerve injury | N/A | N/A |
| Pneumonia | 25.38 (16.66-39.65) | <.001a |
| Urinary tract infection | 1.99 (1.33-2.97) | <.001a |
| All complicationsb | 3.36 (2.47-4.59) | <.001a |
TJA, total joint arthroplasty; OR, odds ratio; CI, confidence interval; N/A, not applicable.
Bold values indicate statistical significance of P < .05.
Indicates statistical significance of P < .05.
Includes rate of all complications, excluding pneumonia.
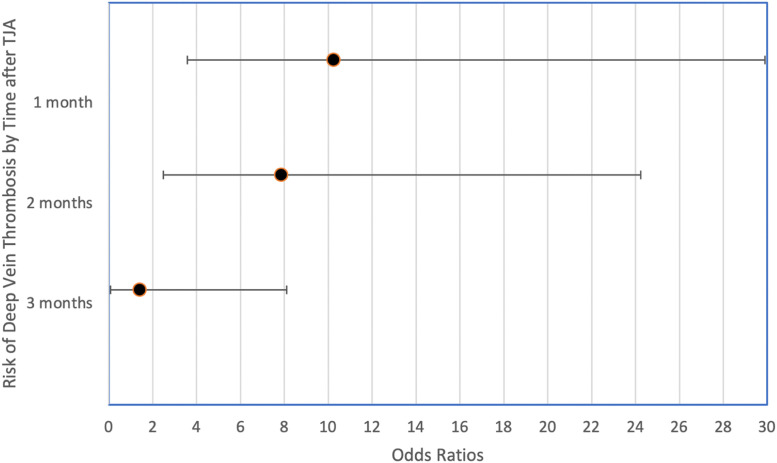
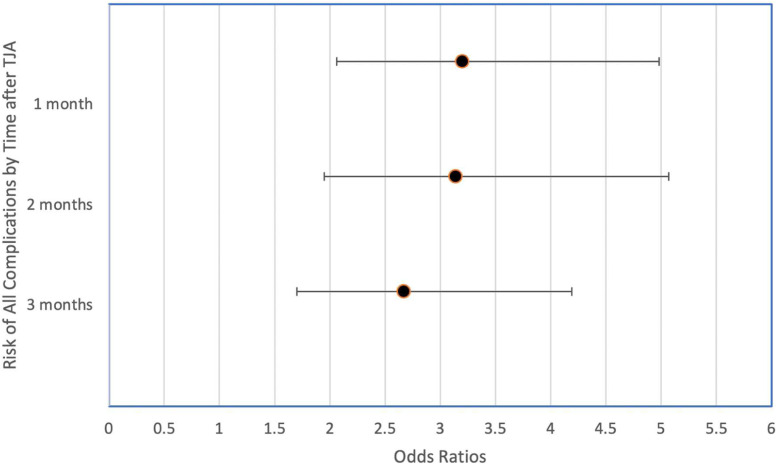
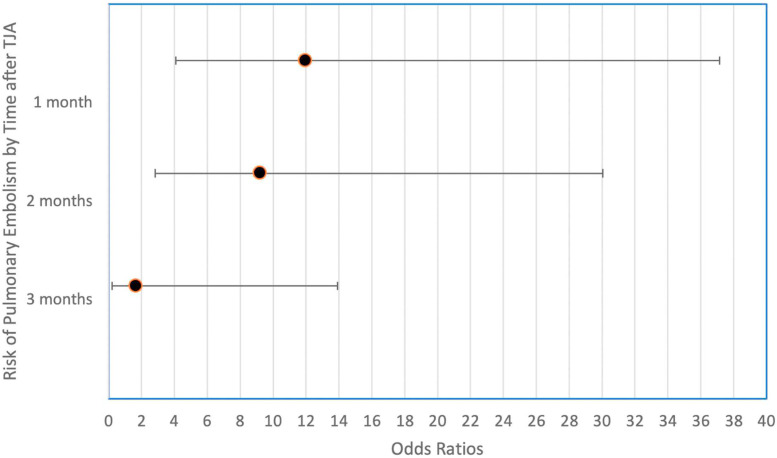
The timing of COVID-19 infection demonstrated a temporal relationship with TJA, with infection closer in time to TJA resulting in greater odds of thromboembolic as well as all complications. The incidence of DVT was greater the closer in time the COVID-19 diagnosis was to the surgical procedure (10.24× at 1 month, 7.87× at 2 months, and 1.42× at 3 months, P < .001; Table 4 , Fig. 1 ). A similar relationship was observed for PE (11.96× at 1 month, 9.20× at 2 months, and 1.65× at 3 months, P < .001; Table 4, Fig. 2 ) and all complications (3.20× at 1 month, 3.14× at 2 months, and 2.67× at 3 months; Table 4, Fig. 3 ).
Table 4.
Temporal Relationship of COVID-19 Diagnosis Following TJA and the Odds of Suffering Venous Thromboembolic Event (DVT/PE) and Any Complication.
| Time After TJA of COVID-19 dx | DVT |
PE |
Any Complication |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| 1 mo | 10.24 (3.59-29.90) | <.001a | 11.96 (4.07-37.14) | <.001a | 3.20 (2.06-4.98) | <.001a |
| 2 mo | 7.87 (2.48-24.24) | <.001a | 9.20 (2.82-30.03) | <.001a | 3.14 (1.95-5.07) | <.001a |
| 3 mo | 1.42 (0.08-8.10) | .747 | 1.65 (0.20-13.92) | .644 | 2.67 (1.70-4.19) | <.001a |
TJA, total joint arthroplasty; OR, odds ratio; CI, confidence interval; DVT, deep vein thrombosis; PE, pulmonary embolism.
Indicates statistical significance of P < .05.
Fig. 1.
Temporal relationship of COVID-19 diagnosis following TJA and the odds of suffering deep vein thrombosis.
Fig. 2.
Temporal relationship of COVID-19 diagnosis following TJA and the odds of suffering all complications.
Fig. 3.
Temporal relationship of COVID-19 diagnosis following TJA and the odds of suffering pulmonary embolism.
Discussion
The results of this study demonstrate significant morbidity associated with postoperative COVID-19 infection. Patients who had a COVID-19 infection in the early postoperative period had significantly higher rates of venous thromboembolic events (VTEs), AKI, cardiac arrest, pneumonia, and urinary tract infection associated with COVID-19 diagnosis following TJA. Additionally, timing was important with COVID-19 infections earlier in the postoperative period having a greater risk than those that occurred later. As elective joint arthroplasty has resumed, this analysis provides important information regarding the impact of a postoperative COVID-19 diagnosis on perioperative complications.
DVT and PE were more common in COVID-19 positive patients compared to matched controls. Although we were unable to assess the rate of complications in COVID-19 positive patients who did not undergo TJA given the limitations of the database, a recent meta-analysis of 64,503 patients demonstrated the incidence of DVT and PE among COVID-19 positive patients to be 11.2% and 7.8%, respectively [17]. Similarly, other authors have reported a significantly higher risk of thromboembolic events associated with COVID-19 infection. Di Minno et al [18] completed a large-scale meta-analysis showing that COVID-19 positive patients were at a higher risk of VTE, including intensive care unit patients and those on antithrombotic prophylaxis. Colling and Kanthi [19] studied the COVID-19 associated coagulopathy and hypothesized that the hypercoagulable state is secondary to an imbalance between coagulation and inflammation. This imbalance is believed to arise from immune system activation leading to endothelial injury, loss of antithrombotic mechanisms, excess thrombin production, and poor fibrinolysis and thrombosis [19].
The present investigation finds that the proximity of COVID-19 diagnosis to the time of TJA demonstrated a temporal relationship, with COVID-19 diagnosis 1 month from TJA increasing the risk of both VTE and overall complication rate relative to COVID-19 diagnosis at 2 and 3 months postoperatively. Additional research is required to determine whether more aggressive anticoagulation regimens are indicated for TJA patients who are diagnosed with COVID-19 in the early postoperative period.
Although the matching process was successful for a majority of Charlson Comorbidity Index variables, there was a significantly higher frequency of deficiency anemia in the COVID-positive cohort (13.8% vs 7.7%, P = .007). In a study conducted in Italy, Bergamaschi et al [20] found that the prevalence of anemia (due to iron deficiency, inflammation, or other causes) was significantly higher in COVID-19 patients compared to the matched control. Although iron deficiency anemia does not directly influence mortality or pulmonary complications, it does usually affect elderly patients which makes up the vast majority of TJA patients. Having associated comorbidities while recovering from surgery can place more physiological demand on patients postoperatively leading to more complications [21].
There are several limitations to the present study. First, while the total number of patients included in the study provides statistical power for analysis, the cohort size of this study was relatively small given both the recency and rarity of post-TJA COVID infection. Second, inherent in all administrative claims datasets is the reliance upon accurate documentation and coding. Third, database limitations precluded matching based on year of TJA, thus COVID-naive patients who underwent TJA dating back to 2018 were included to allow for successful matching. It would be expected that matches from earlier years would have experienced more complications, as surgical safety has since improved. Thus, it is possible that the observed risk of complications following COVID diagnosis is greater than we report. In addition, the database used for this investigation contained data on patients who underwent TJA. Therefore, we were unable to determine the incidence of the studied complications in patients who were COVID-19 positive but did not undergo TJA. Fourth, although we reported a higher incidence of thromboembolic events associated with COVID-19 diagnosis, we did not have information regarding DVT prophylaxis, although we would assume that matched cohorts would be subject to similar perioperative management. Fifth, the database utilized does not contain information regarding patient-reported outcome measures to subjectively evaluate differences in COVID-19-positive patients and control patients. Finally, software limitations prevented us from determining vaccination status among the study groups. Further research is needed to determine the effect of the COVID-19 vaccine on reducing complication rates in TJA patients.
COVID-19 has drastically altered access to healthcare. As surgical volumes begin to return to normal levels, it is important to understand the effect of postoperative coronavirus infection. In this matched cohort study, we identified higher rates of cardiopulmonary complications, thromboembolic disease, renal injury, and urinary tract infections in TJA patients postoperatively after COVID-19 infection. Moreover, morbidity increased with the proximity of COVID-19 diagnosis to arthroplasty. Patients and caregivers should consider strategies to decrease the risk of COVID-19 infection in the early postoperative period.
Conclusion
Postoperative COVID-19 infection is associated with higher rates of cardiopulmonary complications, thromboembolic disease, renal injury, and urinary tract infections in patients undergoing hip and knee arthroplasty. COVID-19 infection earlier in the postoperative period is associated with a higher risk of complications. These findings highlight the importance of preventing COVID-19 infection among patients recovering from TJA.
CRediT authorship contribution statement
Enrico M. Forlenza: Conceptualization, Methodology, Funding acquisition, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Investigation. John D.D. Higgins: Conceptualization, Methodology, Funding acquisition, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Investigation. Robert A. Burnett: Conceptualization, Methodology, Funding acquisition, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Investigation. Joseph Serino: Conceptualization, Methodology, Funding acquisition, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Investigation. Craig J. Della Valle: Writing – original draft, Writing – review & editing, Investigation.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2021.10.023.
Appendix A. Supplementary Data
Appendix
Appendix A.
Diagnoses Codes Associated With Various Postoperative Complications.
| Complication | Corresponding ICD-9/10 Diagnosis Code |
|---|---|
| Superficial surgical site infection | ICD-10-D-L0889, ICD-10-D-L089, ICD-10-D-T814XXA, ICD-10-D-L03119, ICD-10-D-L03129, ICD-10-D-L03319, ICD-10-D-L03329 |
| Prosthetic joint infection | ICD-10-D-K6811, ICD-10-D-T8579XA, ICD-10-D-T8450XA, ICD-10-D-T8460XA, ICD-10-D-T847XXA, ICD-10-D-T8579XA |
| Acute kidney injury | ICD-9-D-5845, ICD-9-D-5846, ICD-9-D-5847, ICD-9-D-5848, ICD-9-D-5849, ICD-10-D-N17:ICD-10-D-N179 |
| Cardiac arrest | ICD-9-D-4275, ICD-9-D-42741, ICD-10-D-I46:ICD-10-D-I469 |
| Deep vein thrombosis | ICD-9-D-4532, ICD-9-D-4533, ICD-9-D-4534, ICD-9-D-45382, ICD-9-D-45384, ICD-9-D-45385, ICD-9-D-45386, ICD-10-D-I26:ICD-10-D-I2699 |
| Nerve injury | ICD-9-D-9550, ICD-9-D-9551, ICD-9-D-9552, ICD-9-D-9553, ICD-9-D-9554, ICD-9-D-9555, ICD-9-D-9556, ICD-9-D-9557, ICD-9-D-9558, ICD-9-D-9559, ICD-9-D-9074, ICD-10-D-S440, ICD-10-D-S4400, ICD-10-D-S4400XA, ICD-10-D-S4400XD, ICD-10-D-S4400XS, ICD-10-D-S4401, ICD-10-D-S4401XA, ICD-10-D-S4401XD, ICD-10-D-S4401XS, ICD-10-D-S4402, ICD-10-D-S4402XA, ICD-10-D-S4402XD, ICD-10-D-S4402XS, ICD-10-D-S441, ICD-10-D-S4410, ICD-10-D-S4410XA, ICD-10-D-S4410XD, ICD-10-D-S4410XS, ICD-10-D-S4411, ICD-10-D-S4411XA, ICD-10-D-S4411XD, ICD-10-D-S4411XS, ICD-10-D-S4412, ICD-10-D-S4412XA, ICD-10-D-S4412XD, ICD-10-D-S4412XS, ICD-10-D-S442, ICD-10-D-S4420, ICD-10-D-S4420XA, ICD-10-D-S4420XD, ICD-10-D-S4420XS, ICD-10-D-S4421, ICD-10-D-S4421XA, ICD-10-D-S4421XD, ICD-10-D-S4421XS, ICD-10-D-S4422, ICD-10-D-S4422XA, ICD-10-D-S4422XD, ICD-10-D-S4422XS, ICD-10-D-S443, ICD-10-D-S4430, ICD-10-D-S4430XA, ICD-10-D-S4430XD, ICD-10-D-S4430XS, ICD-10-D-S4431, ICD-10-D-S4431XA, ICD-10-D-S4431XD, ICD-10-D-S4431XS, ICD-10-D-S4432, ICD-10-D-S4432XA, ICD-10-D-S4432XD, ICD-10-D-S4432XS, ICD-10-D-S444, ICD-10-D-S4440, ICD-10-D-S4440XA, ICD-10-D-S4440XD, ICD-10-D-S4440XS, ICD-10-D-S4441, ICD-10-D-S4441XA, ICD-10-D-S4441XD, ICD-10-D-S4441XS, ICD-10-D-S4442, ICD-10-D-S4442XA, ICD-10-D-S4442XD, ICD-10-D-S4442XS, ICD-10-D-S445, ICD-10-D-S4450, ICD-10-D-S4450XA, ICD-10-D-S4450XD, ICD-10-D-S4450XS, ICD-10-D-S4451, ICD-10-D-S4451XA, ICD-10-D-S4451XD, ICD-10-D-S4451XS, ICD-10-D-S4452, ICD-10-D-S4452XA, ICD-10-D-S4452XD, ICD-10-D-S4452XS, ICD-10-D-S448, ICD-10-D-S448X, ICD-10-D-S448X1, ICD-10-D-S448X1A, ICD-10-D-S448X1D, ICD-10-D-S448X1S, ICD-10-D-S448X2, ICD-10-D-S448X2A, ICD-10-D-S448X2D, ICD-10-D-S448X2S, ICD-10-D-S448X9, ICD-10-D-S448X9A, ICD-10-D-S448X9D, ICD-10-D-S448X9S, ICD-10-D-S449, ICD-10-D-S4490, ICD-10-D-S4490XA, ICD-10-D-S4490XD, ICD-10-D-S4490XS, ICD-10-D-S4491, ICD-10-D-S4491XA, ICD-10-D-S4491XD, ICD-10-D-S4491XS, ICD-10-D-S4492, ICD-10-D-S4492XA, ICD-10-D-S4492XD, ICD-10-D-S4492XS |
| Pneumonia | ICD-9-D-4800:ICD-9-D-4809, ICD-9-D-481, ICD-9-D-4820, ICD-9-D-4821, ICD-9-D-48230, ICD-9-D-48231, ICD-9-D-48232, ICD-9-D-48239, ICD-9-D-48240, ICD-9-D-48241, ICD-9-D-48242, ICD-9-D-48249, ICD-9-D-48281, ICD-9-D-48282, ICD-9-D-48283, ICD-9-D-48284, ICD-9-D-48289, ICD-9-D-4829, ICD-9-D-4830, ICD-9-D-4831, ICD-9-D-4838, ICD-9-D-4841, ICD-9-D-4843, ICD-9-D-4845, ICD-9-D-4846, ICD-9-D-4847, ICD-9-D-4848, ICD-9-D-485, ICD-9-D-486, ICD-10-D-J12:ICD-10-D-J189 |
| Pulmonary embolism | ICD-9-D-4151:ICD-9-D-4159, ICD-10-D-I26:ICD-10-D-I269 |
| Urinary tract infection | ICD-9-D-5990, ICD-10-D-N390 |
| Wound disruption | ICD-9-D-99830, ICD-9-D-99831, ICD-9-D-99832, ICD-9-D-99833, ICD-10-D-T8130XA, ICD-10-D-T8130XD, ICD-10-D-T8130XS, ICD-10-D-T8131XA, ICD-10-D-T8131XD, ICD-10-D-T8131XS, ICD-10-D-T8132XA, ICD-10-D-T8132XD, ICD-10-D-T8132XS, ICD-10-D-T8133XA, ICD-10-D-T8133XD, ICD-10-D-T8133XS |
| Postoperative hematoma | ICD-9-D-99811, ICD-9-D-99812, ICD-9-D-99813, ICD-10-D-D7801, ICD-10-D-D7802, ICD-10-D-D7821, ICD-10-D-D7822, ICD-10-D-E3601, ICD-10-D-E3602, ICD-10-D-E89810, ICD-10-D-E89811, ICD-10-D-G9731, ICD-10-D-G9732, ICD-10-D-G9751, ICD-10-D-G9752, ICD-10-D-H59111, ICD-10-D-H59112, ICD-10-D-H59113, ICD-10-D-H59119, ICD-10-D-H59121, ICD-10-D-H59122, ICD-10-D-H59123, ICD-10-D-H59129, ICD-10-D-H59311, ICD-10-D-H59312, ICD-10-D-H59313, ICD-10-D-H59319, ICD-10-D-H59321, ICD-10-D-H59322, ICD-10-D-H59323, ICD-10-D-H59329, ICD-10-D-H9521, ICD-10-D-H9522, ICD-10-D-H9541, ICD-10-D-H9542, ICD-10-D-I97410, ICD-10-D-I97411, ICD-10-D-I97418, ICD-10-D-I9742, ICD-10-D-I97610, ICD-10-D-I97611, ICD-10-D-I97618, ICD-10-D-I97620, ICD-10-D-J9561, ICD-10-D-J9562, ICD-10-D-J95830, ICD-10-D-J95831, ICD-10-D-K9161, ICD-10-D-K9162, ICD-10-D-K91840, ICD-10-D-K91841, ICD-10-D-L7601, ICD-10-D-L7602, ICD-10-D-L7621, ICD-10-D-L7622, ICD-10-D-M96810, ICD-10-D-M96811, ICD-10-D-M96830, ICD-10-D-M96831, ICD-10-D-N9961, ICD-10-D-N9962, ICD-10-D-N99820, ICD-10-D-N99821, ICD-10-D-T888XXA |
| Transfusion | ICD-9-P-9904, ICD-10-P-3023, ICD-10-P-30230AZ, ICD-10-P-30230G0, ICD-10-P-30230G2, ICD-10-P-30230G3, ICD-10-P-30230G4, ICD-10-P-30230H0, ICD-10-P-30230H1, ICD-10-P-30230J0, ICD-10-P-30230J1, ICD-10-P-30230K0, ICD-10-P-30230K1, ICD-10-P-30230L0, ICD-10-P-30230L1, ICD-10-P-30230M0, ICD-10-P-30230M1, ICD-10-P-30230N0, ICD-10-P-30230N1, ICD-10-P-30230P0, ICD-10-P-30230P1, ICD-10-P-30230Q0, ICD-10-P-30230Q1, ICD-10-P-30230R0, ICD-10-P-30230R1, ICD-10-P-30230S0, ICD-10-P-30230S1, ICD-10-P-30230T0, ICD-10-P-30230T1, ICD-10-P-30230V0, ICD-10-P-30230V1, ICD-10-P-30230W0, ICD-10-P-30230W1, ICD-10-P-30230X0, ICD-10-P-30230X2, ICD-10-P-30230X3, ICD-10-P-30230X4, ICD-10-P-30230Y0, ICD-10-P-30230Y2, ICD-10-P-30230Y3, ICD-10-P-30230Y4, ICD-10-P-30233AZ, ICD-10-P-30233G0, ICD-10-P-30233G2, ICD-10-P-30233G3, ICD-10-P-30233G4, ICD-10-P-30233H0, ICD-10-P-30233H1, ICD-10-P-30233J0, ICD-10-P-30233J1, ICD-10-P-30233K0, ICD-10-P-30233K1, ICD-10-P-30233L0, ICD-10-P-30233L1, ICD-10-P-30233M0, ICD-10-P-30233M1, ICD-10-P-30233N0, ICD-10-P-30233N1, ICD-10-P-30233P0, ICD-10-P-30233P1, ICD-10-P-30233Q0, ICD-10-P-30233Q1, ICD-10-P-30233R0, ICD-10-P-30233R1, ICD-10-P-30233S0, ICD-10-P-30233S1, ICD-10-P-30233T0, ICD-10-P-30233T1, ICD-10-P-30233V0, ICD-10-P-30233V1, ICD-10-P-30233W0, ICD-10-P-30233W1, ICD-10-P-30233X0, ICD-10-P-30233X2, ICD-10-P-30233X3, ICD-10-P-30233X4, ICD-10-P-30233Y0, ICD-10-P-30233Y2, ICD-10-P-30233Y3, ICD-10-P-30233Y4, ICD-10-P-30240AZ, ICD-10-P-30240G0, ICD-10-P-30240G2, ICD-10-P-30240G3, ICD-10-P-30240G4, ICD-10-P-30240H0, ICD-10-P-30240H1, ICD-10-P-30240J0, ICD-10-P-30240J1, ICD-10-P-30240K0, ICD-10-P-30240K1, ICD-10-P-30240L0, ICD-10-P-30240L1, ICD-10-P-30240M0, ICD-10-P-30240M1, ICD-10-P-30240N0, ICD-10-P-30240N1, ICD-10-P-30240P0, ICD-10-P-30240P1, ICD-10-P-30240Q0, ICD-10-P-30240Q1, ICD-10-P-30240R0, ICD-10-P-30240R1, ICD-10-P-30240S0, ICD-10-P-30240S1, ICD-10-P-30240T0, ICD-10-P-30240T1, ICD-10-P-30240V0, ICD-10-P-30240V1, ICD-10-P-30240W0, ICD-10-P-30240W1, ICD-10-P-30240X0, ICD-10-P-30240X2, ICD-10-P-30240X3, ICD-10-P-30240X4, ICD-10-P-30240Y0, ICD-10-P-30240Y2, ICD-10-P-30240Y3, ICD-10-P-30240Y4, ICD-10-P-30243AZ, ICD-10-P-30243G0, ICD-10-P-30243G2, ICD-10-P-30243G3, ICD-10-P-30243G4, ICD-10-P-30243H0, ICD-10-P-30243H1, ICD-10-P-30243J0, ICD-10-P-30243J1, ICD-10-P-30243K0, ICD-10-P-30243K1, ICD-10-P-30243L0, ICD-10-P-30243L1, ICD-10-P-30243M0, ICD-10-P-30243M1, ICD-10-P-30243N0, ICD-10-P-30243N1, ICD-10-P-30243P0, ICD-10-P-30243P1, ICD-10-P-30243Q0, ICD-10-P-30243Q1, ICD-10-P-30243R0, ICD-10-P-30243R1, ICD-10-P-30243S0, ICD-10-P-30243S1, ICD-10-P-30243T0, ICD-10-P-30243T1, ICD-10-P-30243V0, ICD-10-P-30243V1, ICD-10-P-30243W0, ICD-10-P-30243W1, ICD-10-P-30243X0, ICD-10-P-30243X2, ICD-10-P-30243X3, ICD-10-P-30243X4, ICD-10-P-30243Y0, ICD-10-P-30243Y2, ICD-10-P-30243Y3, ICD-10-P-30243Y4, ICD-10-P-30250G0, ICD-10-P-30250G1, ICD-10-P-30250H0, ICD-10-P-30250H1, ICD-10-P-30250J0, ICD-10-P-30250J1, ICD-10-P-30250K0, ICD-10-P-30250K1, ICD-10-P-30250L0, ICD-10-P-30250L1, ICD-10-P-30250M0, ICD-10-P-30250M1, ICD-10-P-30250N0, ICD-10-P-30250N1, ICD-10-P-30250P0, ICD-10-P-30250P1, ICD-10-P-30250Q0, ICD-10-P-30250Q1, ICD-10-P-30250R0, ICD-10-P-30250R1, ICD-10-P-30250S0, ICD-10-P-30250S1, ICD-10-P-30250T0, ICD-10-P-30250T1, ICD-10-P-30250V0, ICD-10-P-30250V1, ICD-10-P-30250W0, ICD-10-P-30250W1, ICD-10-P-30250X0, ICD-10-P-30250X1, ICD-10-P-30250Y0, ICD-10-P-30250Y1, ICD-10-P-30253G0, ICD-10-P-30253G1, ICD-10-P-30253H0, ICD-10-P-30253H1, ICD-10-P-30253J0, ICD-10-P-30253J1, ICD-10-P-30253K0, ICD-10-P-30253K1, ICD-10-P-30253L0, ICD-10-P-30253L1, ICD-10-P-30253M0, ICD-10-P-30253M1, ICD-10-P-30253N0, ICD-10-P-30253N1, ICD-10-P-30253P0, ICD-10-P-30253P1, ICD-10-P-30253Q0, ICD-10-P-30253Q1, ICD-10-P-30253R0, ICD-10-P-30253R1, ICD-10-P-30253S0, ICD-10-P-30253S1, ICD-10-P-30253T0, ICD-10-P-30253T1, ICD-10-P-30253V0, ICD-10-P-30253V1, ICD-10-P-30253W0, ICD-10-P-30253W1, ICD-10-P-30253X0, ICD-10-P-30253X1, ICD-10-P-30253Y0, ICD-10-P-30253Y1, ICD-10-P-30260G0, ICD-10-P-30260G1, ICD-10-P-30260H0, ICD-10-P-30260H1, ICD-10-P-30260J0, ICD-10-P-30260J1, ICD-10-P-30260K0, ICD-10-P-30260K1, ICD-10-P-30260L0, ICD-10-P-30260L1, ICD-10-P-30260M0, ICD-10-P-30260M1, ICD-10-P-30260N0, ICD-10-P-30260N1, ICD-10-P-30260P0, ICD-10-P-30260P1, ICD-10-P-30260Q0, ICD-10-P-30260Q1, ICD-10-P-30260R0, ICD-10-P-30260R1, ICD-10-P-30260S0, ICD-10-P-30260S1, ICD-10-P-30260T0, ICD-10-P-30260T1, ICD-10-P-30260V0, ICD-10-P-30260V1, ICD-10-P-30260W0, ICD-10-P-30260W1, ICD-10-P-30260X0, ICD-10-P-30260X1, ICD-10-P-30260Y0, ICD-10-P-30260Y1, ICD-10-P-30263G0, ICD-10-P-30263G1, ICD-10-P-30263H0, ICD-10-P-30263H1, ICD-10-P-30263J0, ICD-10-P-30263J1, ICD-10-P-30263K0, ICD-10-P-30263K1, ICD-10-P-30263L0, ICD-10-P-30263L1, ICD-10-P-30263M0, ICD-10-P-30263M1, ICD-10-P-30263N0, ICD-10-P-30263N1, ICD-10-P-30263P0, ICD-10-P-30263P1, ICD-10-P-30263Q0, ICD-10-P-30263Q1, ICD-10-P-30263R0, ICD-10-P-30263R1, ICD-10-P-30263S0, ICD-10-P-30263S1, ICD-10-P-30263T0, ICD-10-P-30263T1, ICD-10-P-30263V0, ICD-10-P-30263V1, ICD-10-P-30263W0, ICD-10-P-30263W1, ICD-10-P-30263X0, ICD-10-P-30263X1, ICD-10-P-30263Y0, ICD-10-P-30263Y1, ICD-10-P-30273H1, ICD-10-P-30273J1, ICD-10-P-30273K1, ICD-10-P-30273L1, ICD-10-P-30273M1, ICD-10-P-30273N1, ICD-10-P-30273P1, ICD-10-P-30273Q1, ICD-10-P-30273R1, ICD-10-P-30273S1, ICD-10-P-30273T1, ICD-10-P-30273V1, ICD-10-P-30273W1, ICD-10-P-30277H1, ICD-10-P-30277J1, ICD-10-P-30277K1, ICD-10-P-30277L1, ICD-10-P-30277M1, ICD-10-P-30277N1, ICD-10-P-30277P1, ICD-10-P-30277Q1, ICD-10-P-30277R1, ICD-10-P-30277S1, ICD-10-P-30277T1, ICD-10-P-30277V1, ICD-10-P-30277W1, ICD-10-P-30280B1, ICD-10-P-30283B1 |
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. China Novel Coronavirus I. Research T A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. China Medical Treatment Expert Group for C Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haffer H., Schomig F., Rickert M., Randau T., Raschke M., Wirtz D., et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in University Hospitals in Germany: results of a Nationwide Survey. J Bone Joint Surg Am. 2020;102:e78. doi: 10.2106/JBJS.20.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain V.K., Vaishya R. COVID-19 and orthopaedic surgeons: the Indian scenario. Trop Doct. 2020;50:108–110. doi: 10.1177/0049475520921616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liebensteiner M.C., Khosravi I., Hirschmann M.T., Heuberer P.R., Board of the AGASoA, Joint S., et al. It is not 'business as usual' for orthopaedic surgeons in May 2020- the Austrian-German-Swiss experience. J Exp Orthop. 2020;7:61. doi: 10.1186/s40634-020-00272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace C.N., Kontoghiorghe C., Kayani B., Chang J.S., Haddad F.S. The impact of COVID-19 on trauma and orthopaedic surgery in the United Kingdom. Bone Jt Open. 2020;1:420–423. doi: 10.1302/2633-1462.17.BJO-2020-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong J.S.H., Cheung K.M.C. Impact of COVID-19 on orthopaedic and trauma Service: an Epidemiological study. J Bone Joint Surg Am. 2020;102:e80. doi: 10.2106/JBJS.20.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurtz S.M., Ong K.L., Lau E., Bozic K.J. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–630. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 10.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 11.Brown T.S., Bedard N.A., Rojas E.O., Anthony C.A., Schwarzkopf R., Barnes C.L., et al. The effect of the COVID-19 pandemic on electively scheduled hip and knee arthroplasty patients in the United States. J Arthroplasty. 2020;35:S49–S55. doi: 10.1016/j.arth.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bedard N.A., Elkins J.M., Brown T.S. Effect of COVID-19 on hip and knee arthroplasty surgical volume in the United States. J Arthroplasty. 2020;35:S45–S48. doi: 10.1016/j.arth.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Connor C.M., Anoushiravani A.A., DiCaprio M.R., Healy W.L., Iorio R. Economic Recovery after the COVID-19 pandemic: resuming elective orthopedic surgery and total joint arthroplasty. J Arthroplasty. 2020;35:S32–S36. doi: 10.1016/j.arth.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nuesch E., Dieppe P., Reichenbach S., Williams S., Iff S., Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collaborative C Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clement N.D., Hall A.J., Makaram N.S., Robinson P.G., Patton R.F.L., Moran M., et al. IMPACT-Restart: the influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Joint J. 2020;102-B:1774–1781. doi: 10.1302/0301-620X.102B12.BJJ-2020-1395.R2. [DOI] [PubMed] [Google Scholar]
- 17.Tan B.K., Mainbourg S., Friggeri A., Bertoletti L., Douplat M., Dargaud Y., et al. Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis. Thorax. 2021;76:970–979. doi: 10.1136/thoraxjnl-2020-215383. [DOI] [PubMed] [Google Scholar]
- 18.Di Minno A., Ambrosino P., Calcaterra I., Di Minno M.N.D. COVID-19 and venous thromboembolism: a meta-analysis of literature studies. Semin Thromb Hemost. 2020;46:763–771. doi: 10.1055/s-0040-1715456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colling M.E.K. Yogendra. COVID–19-associated coagulopathy: an exploration of mechanisms. Vasc Med. 2020;25:471–478. doi: 10.1177/1358863X20932640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergamaschi G., Borrelli de Andreis F., Aronico N., Lenti M.V., Barteselli C., Merli S., et al. Internal Medicine Covid C Anemia in patients with Covid-19: pathogenesis and clinical significance. Clin Exp Med. 2021;21:239–246. doi: 10.1007/s10238-020-00679-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joosten E. Iron deficiency anemia in older adults: a review. Geriatr Gerontol Int. 2018;18:373–379. doi: 10.1111/ggi.13194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.