Abstract
Background:
The accuracy of existing devices for measuring knee laxity is adversely affected by examiner reliability.
Purpose:
To compare the accuracy of a novel automatic knee arthrometer (AKA) to that of the KT-2000 arthrometer for measuring knee laxity after anterior cruciate ligament (ACL) ruptures.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
We measured anterior displacement and the anterior displacement difference (ADD) at 134 N of anterior force in 221 healthy volunteers and 200 patients with ACL ruptures. All trials were performed by the same 2 examiners. We first analyzed the effects of examiner, side assessed, and device type using the intraclass correlation coefficient (ICC), t test, and F test. We then used the receiver operating characteristic curve to compare the diagnostic value of the measurements between devices.
Results:
In repeated measurements for a single healthy volunteer, there were no differences in the variance of the measurements between sides according to the AKA (standard deviation of right vs left knee for examiner A: 0.43 vs 0.58 mm, respectively [P = .39]; for examiner B: 0.49 vs 0.77 mm, respectively [P = .81]), while the KT-2000 measurements showed differences (standard deviation of right vs left knee for examiner A: 1.47 vs 0.80 mm, respectively [P = .02]; for examiner B: 1.78 vs 0.91 mm, respectively [P = .01]). The ADD assessed by the AKA was not significantly different between examiners A and B (0.50 vs 0.75 mm, respectively; P = .27; ICC = 0.83), but the KT-2000 showed a difference (1.07 vs 2.01 mm, respectively; P = .01; ICC = 0.55). The ADD of 20 healthy volunteers assessed by the AKA was less than that by the KT-2000 (0.98 vs 1.41 mm, respectively; P = .04). When comparing the diagnostic value of the 2 devices in the sample of 200 patients with ACL ruptures and 200 healthy controls, the area under the receiver operating characteristic curve for the AKA was larger than that for the KT-2000 (0.93 vs 0.87, respectively; P ≤ .01), and the threshold values were 1.75 and 2.73 mm, respectively.
Conclusion:
The AKA can be used to determine the degree of knee laxity in ACL injuries and to provide indications for treatment.
Keywords: automatic knee arthrometer, anterior cruciate ligament rupture, knee laxity
The anterior cruciate ligament (ACL) plays an important role in the stability of the knee, as the primary function of the ACL is the restraint of anterior tibial translation. An ACL rupture is a common sports injury with serious long-term negative effects, such as lower extremity dysfunction, low levels of physical activity, and the early development of knee osteoarthritis. 2,6,12,14 The measurement of knee laxity is crucial for treatment strategies and postoperative recovery 15,33 and is commonly obtained by clinical examinations such as the Lachman, anterior drawer, and pivot-shift tests. 20 These tests are not objective, and the results are influenced by the experience of the examiner, patient cooperation, and the duration between the injury and examination. 18,21
Several devices have been investigated to quantify knee laxity, but a gold-standard instrument has not been established. 30 Among these devices, the KT-1000/2000 arthrometer (Medmetric) was first introduced in the early 1980s and is the most widely used knee laxity measurement device. 11,16 However, examiners need to pull the tibia anteriorly by manual force when using the KT-1000/2000, which may be a physical challenge for them, and poor reproducibility and unreliable results have been reported. 17,32
There is a need for a more accurate knee laxity measurement instrument in sports medicine. To this end, we invented an automatic knee arthrometer (AKA) and assembled the device in our university laboratory. It was designed according to the biomechanical characteristics of abnormal anterior tibial displacement in patients with ACL ruptures. This study aimed to assess the reliability and effectiveness of the AKA vs the KT-2000 by comparing (1) the influence of examiner experience and tested side on the measurements and (2) the effectiveness of knee laxity measurements and auxiliary diagnosis of ACL ruptures. We hypothesized that the AKA would have better performance in measuring knee laxity than the KT-2000.
Methods
Study Participants
This study was conducted in accordance with the Declaration of Helsinki and received ethics committee approval. All participants signed an informed consent form. During this study, none of the participants indicated discomfort, and none of the trials were stopped prematurely.
Between July and December 2020, a total of 221 healthy volunteers were included; none of them had a history of knee injuries, and all knees were pain free during the previous 3 months. In addition, 200 patients with ACL ruptures from our institution were enrolled. These patients were diagnosed by sports medicine specialists based on clinical manifestations and imaging results and were hospitalized and awaiting further surgery. We excluded patients aged <18 or >45 years, those with combined multiple knee ligament injuries, and/or those with limited knee range of motion (unable to flex to 20°-30°).
Arthrometer Examinations
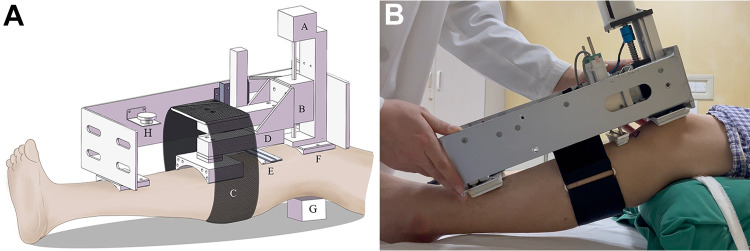
During the AKA examination, the participant lay on an examination bed with the knees flexed at 20° to 30° and with a padded support under both knees. This position is similar to that for the Lachman test to enhance relative tibial displacement. The AKA device consists of an electric slide, force sensor, and displacement sensor. A pad was placed over the patella, secured by both hands of the examiner, and the slider of the electric slide was secured to the participant’s lower leg by a hook-and-loop fastener (Figure 1).
Figure 1.
(A) Diagrammatic drawing and (B) photograph of the automatic knee arthrometer during the examination. A, electric track; B, slider; C, hook-and-loop fastener; D, force sensor; E, displacement sensor; F, patella pad; G, padding; H, emergency terminate button.
Each participant was instructed to relax his or her lower limbs as much as possible, and the test was started by a computer program. The slider (with a 24-V power supply) moved at a constant speed of 0.5 mm/s, pulling the tibia anteriorly. The device was first set to zero to fit the participant’s leg. The slider continuously moved, and relative displacement of the tibia and patella was obtained; displacement was constantly measured by a sensor. The force sensor, situated at the leg-and-slider connection, allowed for simultaneous measurements of the force pulling the tibia. When the force achieved a set value (134 N in this study, but this can be set at 0-300 N by the program), the slider stopped automatically, and the test was complete for one leg (see the Video Supplement for a demonstration of the testing procedure). In case of acute patient discomfort, a button on the upper side of the device could be pushed to terminate the test (Figure 1).
For the KT-2000 arthrometer examination, the participant assumed the same position as for the AKA, and measurements were collected according to the manufacturer’s instructions. Using the right leg as an example, the device was first secured to the lower leg by a hook-and-loop fastener. The patellar side was secured by the left hand of the examiner, and the examiner’s right hand applied tensile force to the device until 134 N was achieved, at which time an indicator light lit up.
For each participant, both legs were examined using both devices. The KT-2000 tests were performed first. If the participant showed no obvious discomfort, then tests with the AKA were performed. The devices were checked to ensure that they were properly fitted each time. The left leg was assessed first for the healthy volunteers, and the uninjured leg was examined first for the patients with ACL ruptures. For both knees, anterior displacement (AD) and the AD difference (ADD) at 134 N were calculated. All data were collected on a computer by plotting a force-displacement curve.
Examiners
There were 2 examiners who performed the trials in the study. Examiner A had 10 years of experience with the KT-2000 and 6 months of experience with the AKA, and examiner B (H.M.) had no experience with either device. Both examiners were right-handed, and neither were involved in the development of the AKA. Before the study, both examiners were trained in the use of the devices.
Study Protocols
Overall, 3 protocols were designed to compare the effectiveness and reproducibility of measuring knee laxity and providing an auxiliary diagnosis of an ACL rupture. As the KT-2000 is one of the regularly used tools before ACL reconstruction (ACLR) at our institution, our tests for patients with ACL ruptures were performed the day before surgery. The patients’ surgery records were reviewed as the gold standard for ACL ruptures, and no misdiagnosis was found. The healthy volunteers were tested as they came to our examination room.
Protocol 1
The 2 examiners performed tests on the same healthy participant (a 28-year-old man) using both devices for 10 consecutive days (ie, 10 times per examiner). For every test, AD of both knees was measured, and the ADD was calculated. We evaluated the effect of which side was measured by comparing the standard deviations of AD for each knee between the devices. In addition, we compared the mean ADD between examiners and evaluated the effect of examiner reliability. Finally, we compared the ADD measured by the same examiner between the devices to evaluate the devices' accuracy in detecting a difference in knee laxity of the healthy participants.
Protocol 2
A single examiner (examiner A) performed tests on 20 healthy participants (12 male and 8 female; mean age, 26.5 years) using both devices, and the mean ADDs of both knees were calculated. We examined the difference in measurements using each device to determine the device effect.
Protocol 3
A single examiner (examiner A) performed tests on 200 patients with ACL ruptures (132 male and 68 female; mean age, 30.2 years) and 200 healthy participants (113 male and 87 female; mean age, 25.3 years) using each device. Using an ADD at 1.5 and 3.0 mm as threshold values, we compared the effectiveness of the 2 devices in diagnosing ACL ruptures.
Statistical Analysis
The t test was used to compare the mean AD and ADD in protocols 1 and 2; the F test was used to determine the significance of the variance of data spread (ie, the difference in the standard deviations) relative to the mean AD. The intraclass correlation coefficient (ICC) was determined to test the reliability between examiners. In protocol 3, the diagnostic sensitivity and specificity at each threshold (ADD at 1.5 and 3.0 mm) were calculated for both devices. The receiver operating characteristic (ROC) curve was analyzed. The area under the ROC curve (AUC) was calculated, and the difference in the AUC between the 2 devices was assessed by the Z test. Statistical analysis was performed using SPSS software (version 24.0; IBM) and MedCalc (version 19; MedCalc Software).
Results
Protocol 1
A significant effect of side tested was observed with the KT-2000 arthrometer. The standard deviation of the mean measurements on the nondominant side (in which the patella pad was secured by the left hand of the examiner while the right knee of the participant was tested) was significantly larger than the standard deviation on the dominant side (in which the patella pad was secured by the right hand of the examiner while the left knee of the participant was tested), as tested by both the experienced (examiner A) and inexperienced (examiner B) examiners (examiner A: 1.47 vs 0.80 mm, respectively [P = .02]; examiner B: 1.78 vs 0.91 mm, respectively [P = .01]), while the mean values of the right vs left knees were not significantly different (Table 1). This was not the case for the AKA in which both the standard deviations of the means and the mean values themselves were not significantly different between sides (Table 1).
TABLE 1.
Anterior Displacement in a Single Healthy Participant a
| Right Knee, mm | Left Knee, mm | P Value b | P Value c | |
|---|---|---|---|---|
| KT-2000 | ||||
| Examiner A | 3.57 ± 1.47 | 3.43 ± 0.80 | .79 | .02 |
| Examiner B | 3.72 ± 1.78 | 3.47 ± 0.91 | .70 | .01 |
| AKA | ||||
| Examiner A | 3.05 ± 0.43 | 3.13 ± 0.58 | .73 | .39 |
| Examiner B | 3.38 ± 0.49 | 3.08 ± 0.77 | .32 | .81 |
a Data are shown as mean ± SD. Bolded P values indicate statistically significant differences (P < .05). AKA, automatic knee arthrometer.
bP values for the difference in the mean between right and left knees.
cP values for the difference in the SD between right and left knees.
A significant examiner effect was observed with the KT-2000; the mean ADD measured by examiner A was significantly less than that by examiner B (1.07 vs 2.01 mm, respectively; P = .01), and the ICC was 0.55 (P = .04). The mean ADD tested by the AKA showed no difference between examiners A and B (0.50 vs 0.75 mm, respectively; P = .27), and the ICC was 0.83 (P ≤ .01). A significant device effect was observed; the mean ADD tested by the AKA was lower than that by the KT-2000 for both the experienced and inexperienced examiners (examiner A: 0.50 vs 1.07 mm, respectively [P = .01]; examiner B: 0.75 vs 2.01 mm, respectively [P ≤ .01]) (Table 2).
TABLE 2.
Anterior Displacement Difference in a Single Healthy Participant a
| AKA, mm | KT-2000, mm | P Value b | |
|---|---|---|---|
| Examiner A | 0.50 | 1.07 | .01 |
| Examiner B | 0.75 | 2.01 | ≤.01 |
| P value c | .27 | .01 | — |
a Bolded P values indicate statistically significant differences (P < .05). AKA, automatic knee arthrometer.
bP values for the difference between devices tested with the same examiner.
cP values for the difference between examiners with the same device.
Protocol 2
The mean ADD of the 20 healthy participants was significantly less with the AKA compared with the KT-2000 (0.98 vs 1.41 mm, respectively; P = .04), showing a device effect as well. One participant had an ADD of 3.53 mm using the KT-2000, which led to a false-positive error at a threshold of 3.0 mm (Figure 2). The number of false positives recorded at the 1.5-mm threshold for the AKA and KT-2000 was 2 and 6, respectively.
Figure 2.
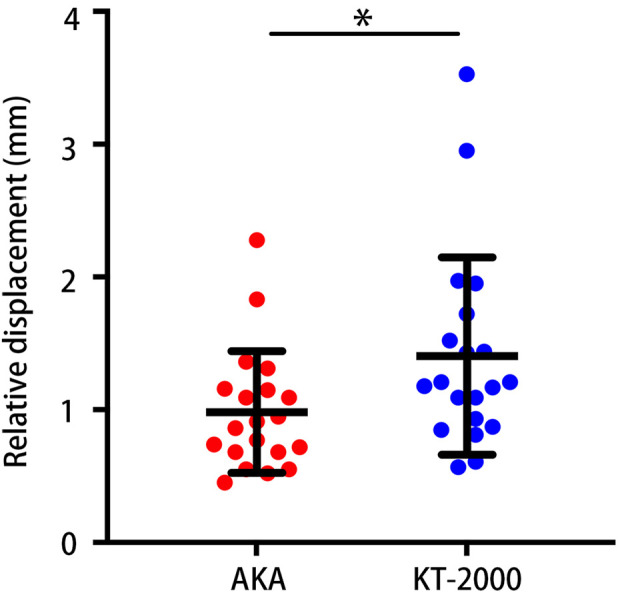
Anterior displacement difference in 20 healthy participants as measured by the automatic knee arthrometer (AKA) and KT-2000 arthrometer. The error bars indicate 95% CIs. *Statistically significant difference (P < .05).
Protocol 3
Figure 3 shows the difference in AD between the healthy and injured knees of a patient with an ACL rupture as tested by the AKA. The diagnostic sensitivity and specificity of the AKA and KT-2000 at differential laxity thresholds of 1.5 and 3.0 mm are shown in Table 3. The sensitivity was similar between the devices, but the specificity of the AKA was higher at both thresholds. The ROC curves of the AKA and KT-2000 for diagnosing ACL ruptures are shown in Figure 4. The AUC of the AKA was 0.93 (P ≤ .01), and the threshold value was 1.75 mm. The AUC of the KT-2000 was 0.87 (P ≤ .01), and the threshold value was 2.73 mm. The difference between the 2 AUCs was significant (0.06; P = .02). A sample of 200 patients from the positive group (patients with ACL ruptures) and 200 from the negative group (healthy controls) achieved 87% power to detect an observed difference in the AUC between the 2 devices using a 2-sided Z test at a significance level of 0.05.
Figure 3.
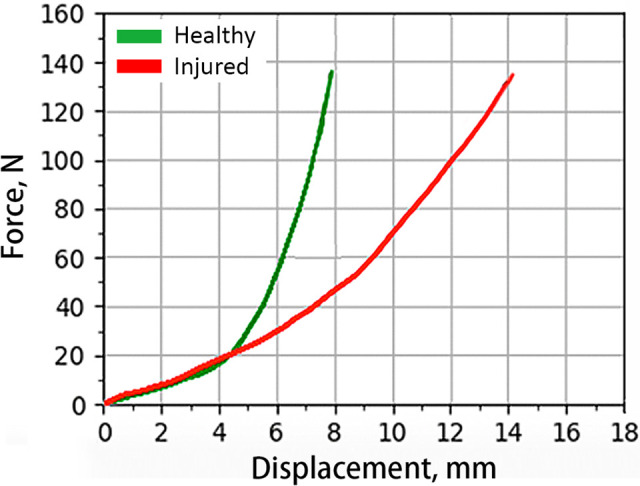
Anterior displacement (AD) at 134 N in the healthy and injured knees of a patient with an anterior cruciate ligament rupture (right knee) as tested by the automatic knee arthrometer. The AD was 7.87 mm in the healthy knee and 14.08 mm in the injured knee, with a difference of 6.21 mm.
TABLE 3.
Diagnostic Sensitivity and Specificity at Differential Laxity Thresholds a
| AKA | KT-2000 | |||
|---|---|---|---|---|
| 1.5 mm | 3.0 mm | 1.5 mm | 3.0 mm | |
| Sensitivity, % | 92 | 86 | 91 | 83 |
| Specificity, % | 89 | 95.5 | 67 | 88.5 |
a AKA, automatic knee arthrometer.
Figure 4.
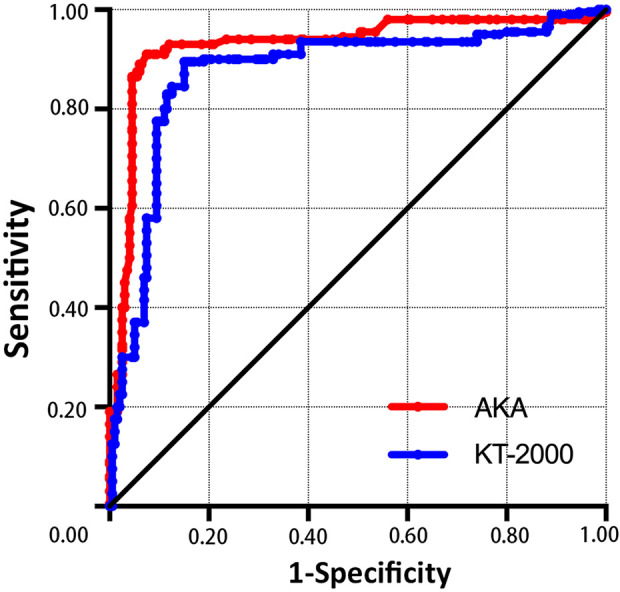
Receiver operating characteristic curves for sensitivity and specificity in the diagnosis of anterior cruciate ligament injuries for the automatic knee arthrometer (AKA) and KT-2000 arthrometer.
Discussion
The present study introduced the AKA, a new device for determining knee laxity, and compared it with an often-used device, the KT-2000 arthrometer. The main result was that the AKA showed superior reproducibility in measuring knee laxity regardless of the examiner's experience (ICC = 0.83; P ≤ .01). At the same time, the AKA provided better effectiveness for an auxiliary diagnosis of ACL ruptures (AUC = 0.93; P ≤ .01) with a lower threshold value (1.75 mm).
Knee laxity measurements in ACL injuries have great value for treatment options. A higher grade of knee laxity probably indicates concomitant injuries in addition to the ACL rupture. Musahl et al 25 found that the medial meniscus functions in a secondary critical role for tibial anterior stability in cadaveric models of ACL ruptures. An anterolateral aspect of capsular and medial collateral ligament injuries was reported to significantly increase knee laxity when combined with ACL ruptures. 8,31 In recent years, a worse prognosis for patients with a high degree of knee laxity after ACL ruptures was suggested. Magnussen et al 22 showed that high-degree anterior knee instability was associated with a significantly increased risk of ACLR failure. Alm et al 4 demonstrated that high-grade anterior knee laxity is a risk factor for revision ACLR failure as well. Cristiani et al 10 reported that a preoperative ADD >5 mm is associated with an increased risk of having abnormal anterior knee laxity at 6 months after primary ACLR. Alm et al 3 defined an ADD >6 mm as measured by the Rolimeter as high-grade knee laxity in patients with graft failure after primary ACLR. They reported that additional lateral extra-articular tenodesis in patients with revision ACLR and high-grade anterior instability significantly reduces the risk of revision failure and improves postoperative functional outcomes. 3 Therefore, knee laxity should be carefully considered before ACLR to provide an indication for targeted treatment of concomitant injuries as well as additional procedures, such as lateral extra-articular tenodesis, augmentation of the anterolateral ligament, or medial stabilization, 4 which may improve the outcomes for patients with high-degree knee laxity. 28
Knee laxity is frequently assessed by surgeons through clinical examinations, including the Lachman, anterior drawer, and pivot-shift tests. 1 However, these tests are manually operated, which is influenced by subjective factors, including the experience of examiners and compliance of patients, leading to varying sensitivities and specificities. The KT-1000/2000 is the most widely used device for measuring knee laxity. The KT-2000 has the same design as the KT-1000, with the addition of a displacement-force curve to present results. 20 Abulhasan et al 1 summarized KT-2000 sensitivity as ranging from 0.50 to 0.97 7,30 and specificity from 0.70 to 0.93. 29,30 They found several reasons accounting for poor reproducibility of the device: the experience level of operators, the amount of force used in tests, and involuntary or defensive hamstring contractions. 1 One disadvantage of the examination process is that anterior force is applied completely manually; thus, the test is significantly influenced by examiner factors. Herein, we introduced and evaluated a novel automatic device that may solve this problem.
In our study, an effect for which side was used was found for the KT-2000 but not for the AKA. During the examination by both devices, maintaining the position of the patella pad is the key to accurate measurements of knee laxity, as it is the base point of both anterior force and the measurement. When testing different legs with the KT-2000, the examiner needs to use opposite hands to apply enough counterforce to secure the patella pad. The patella pad is more likely to move when secured by the nondominant hand of the examiner, leading to inconsistency in measurements between the left and right legs of healthy participants. Collette et al 9 also reported this side-dependent effect of the KT-2000, which is consistent with our finding. We believe that this effect can lead to system errors when measuring knee laxity with the KT-2000. On the other hand, the AKA pulls the tibia automatically, as the electric slide operates the pull force instead of the examiner, and the only remaining requirement is to secure the patella pad with both hands at a symmetric position for both knees. In this way, the AKA location is under improved control, and the results show improved reproducibility.
Previous studies have indicated that the experience of the examiner is another factor affecting the reliability of KT-1000/2000 knee laxity measurements. The ICC between examiners has ranged from 0.43 to 0.95. 5,26,27 The KT-2000 provides improved accuracy when used by an experienced examiner and the device is properly positioned and fixed over the joint line. The results of the present study indicate that the AKA had a smaller examiner effect and higher ICC in healthy participants, as the inexperienced examiner achieved the same results as the experienced examiner. It appears that the AKA can be used by examiners with different levels of experience; the results can then be compared with a uniform standard.
We found similar sensitivity but better specificity in the auxiliary diagnosis of ACL ruptures with the AKA compared with the KT-2000 using 1.5 and 3.0 mm as the threshold, respectively. This demonstrated good repeatability of the AKA, leading to fewer false-positive cases in healthy participants. The diagnosis threshold of the KT-2000 is still controversial. 1 Myrer et al, 26 using an ADD >2 mm as a threshold, reported a false-positive rate of 14% with the KT-2000 at a force of 134 N and suggested a threshold >3 mm to avoid false positives. Using a lower threshold will increase the sensitivity of the diagnosis but will significantly reduce the specificity of the KT-2000, while the extent of this for the AKA is not obvious. This phenomenon indicates that, with the KT-2000, the ADD of many healthy participants is between 1.5 and 3.0 mm, while it is <1.5 mm for more participants measured by the AKA. It shows that the AKA has improved repeatability, as we consider that, under ideal conditions, the ADD of a healthy participant is close to 0 mm.
The higher specificity and lower threshold resulted in a larger AUC for the AKA, which indicates a higher auxiliary diagnosis value for ACL ruptures. Clinically, magnetic resonance imaging is the most accurate examination tool to diagnose ACL ruptures. 23 The measurement of knee laxity is affected by the factors of participant, examiner, and arthrometer, leading to varying diagnosis values of knee arthrometers among ACL surgeons. At present, there is no consensus on which device is the most accurate for knee laxity measurements. 24 Except for the KT-1000/2000, several other arthrometers have been introduced. The GNRB arthrometer, developed in 2005, is driven by a microcalculator and has a split drive and measurement design. Robert et al 27 demonstrated that the GNRB has significantly better reproducibility of measurements than the KT-1000. Lerat et al 19 developed a measure for displacement of the tibia with respect to the femur on radiographs under a 9-kg constraint on the tibia; the sensitivity and specificity were 87% and 90%, respectively, at a 6-mm threshold. The Rolimeter is another manual measurement instrument of knee laxity; the sensitivity and specificity reported were 89% and 95%, respectively. 13
In recent years, there has been increasing evidence that the degree of knee laxity has clinical relevance in ACL treatment. To obtain objective results, it is only possible to use an arthrometer to quantify knee laxity precisely. 27 We believe that the higher auxiliary diagnosis value for ACL ruptures is based on the accurate measurement of AD in every examination using the AKA. The automatic force generation and detection structure reduce system errors not only from the examiner, as mentioned, but also the device. The AKA pulls the tibia anteriorly and produces a downward reaction force onto the patella through the electric slide, and the amount of force can be accurately controlled by a computer. The device is like a bottle opener, with the patella as the fulcrum; the slider drives the tibia vertically through the connection, and relative AD is produced. When the examination begins, as the slider moves up and the anterior force increases, the patella pad will be more firmly secured on the patella of the patient through downward counterforce. In contrast to the KT-2000, if there is no reaction force applied by the examiner, the participant’s leg will lift, and displacement of the tibia will not be generated. With a more reasonable design structure, the AKA has better stability during the examination process and reduces system errors caused by subjective and objective factors.
This study had limitations. First, patients with acute ACL injuries with significant limited range of motion were excluded; there was a selection bias among the ACL rupture population. Second, we recruited healthy participants based on history; less obvious injuries may lead to abnormal knee laxity. Last, the results of both devices were influenced by the degree of participants’ muscle tension/relaxation during the examination; therefore, the results might be influenced by the emotional/mental state of the participants, especially regarding that the KT-2000 examinations were performed first.
Conclusion
This study introduced the AKA, a novel knee laxity arthrometer with a more efficient design structure. Its advantages compared with the KT-2000 are as follows: easy to operate, independent of the side tested, and independent of examiner experience, leading to more accurate measurements of AD and a higher auxiliary diagnosis value. The AKA may be used to determine the degree of knee laxity in ACL injuries and to provide indications for treatment.
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671211051301.
Supplementary Material
Acknowledgment
The authors are grateful to the participants for taking part in the study.
Footnotes
Final revision submitted April 28, 2021; accepted July 14, 2021.
Ethical approval for this study was obtained from Peking University Third Hospital (IRB00006761).
One or more of the authors has declared the following potential conflict of interest or source of funding: X.N. and Y.A. are the co-inventors of the automatic knee arthrometer used in this study. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abulhasan J, Snow M, Anley C, Bakhsh M, Grey M. An extensive evaluation of different knee stability assessment measures: a systematic review. J Funct Morphol Kinesiol. 2016;1(2):209–229. [Google Scholar]
- 2. Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9):2242–2252. [DOI] [PubMed] [Google Scholar]
- 3. Alm L, Drenck TC, Frosch KH, Akoto R. Lateral extra-articular tenodesis in patients with revision anterior cruciate ligament (ACL) reconstruction and high-grade anterior knee instability. Knee. 2020;27(5):1451–1457. [DOI] [PubMed] [Google Scholar]
- 4. Alm L, Krause M, Frosch KH, Akoto R. Preoperative medial knee instability is an underestimated risk factor for failure of revision ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2458–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson AF, Lipscomb AB. Preoperative instrumented testing of anterior and posterior knee laxity. Am J Sports Med. 1989;17(3):387–392. [DOI] [PubMed] [Google Scholar]
- 6. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 7. Bach BR, Jr, Warren RF, Flynn WM, Kroll M, Wickiewiecz TL. Arthrometric evaluation of knees that have a torn anterior cruciate ligament. J Bone Joint Surg Am. 1990;72(9):1299–1306. [PubMed] [Google Scholar]
- 8. Ball S, Stephen JM, El-Daou H, Williams A, Amis AA. The medial ligaments and the ACL restrain anteromedial laxity of the knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(12):3700–3708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Collette M, Courville J, Forton M, Gagniere B. Objective evaluation of anterior knee laxity: comparison of the KT-1000 and GNRB(R) arthrometers. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2233–2238. [DOI] [PubMed] [Google Scholar]
- 10. Cristiani R, Forssblad M, Engstrom B, Edman G, Stalman A. Risk factors for abnormal anteroposterior knee laxity after primary anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(8):2478–2484. [DOI] [PubMed] [Google Scholar]
- 11. Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–407. [DOI] [PubMed] [Google Scholar]
- 12. Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42(5):1247–1255. [DOI] [PubMed] [Google Scholar]
- 13. Ganko A, Engebretsen L, Ozer H. The Rolimeter: a new arthrometer compared with the KT-1000. Knee Surg Sports Traumatol Arthrosc. 2000;8(1):36–39. [DOI] [PubMed] [Google Scholar]
- 14. Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA. Nonsurgical or surgical treatment of ACL injuries: knee function, sports participation, and knee reinjury. The Delaware-Oslo ACL cohort study. J Bone Joint Surg Am. 2014;96(15):1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37(2):e103–e108. [DOI] [PubMed] [Google Scholar]
- 16. Klasan A, Putnis SE, Kandhari V, Oshima T, Parker DA. Anterior knee translation measurements after ACL reconstruction are influenced by the type of laximeter used. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3639–3646. [DOI] [PubMed] [Google Scholar]
- 17. Kowalk DL, Wojtys EM, Disher J, Loubert P. Quantitative analysis of the measuring capabilities of the KT-1000 knee ligament arthrometer. Am J Sports Med. 1993;21(5):744–747. [DOI] [PubMed] [Google Scholar]
- 18. Leblanc MC, Kowalczuk M, Andruszkiewicz N, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2805–2813. [DOI] [PubMed] [Google Scholar]
- 19. Lerat JL, Moyen BL, Cladiere F, Besse JL, Abidi H. Knee instability after injury to the anterior cruciate ligament: quantification of the Lachman test. J Bone Joint Surg Br. 2000;82(1):42–47. [DOI] [PubMed] [Google Scholar]
- 20. Lubowitz JH, Bernardini BJ, Reid JB, 3rd. Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008;36(3):577–594. [DOI] [PubMed] [Google Scholar]
- 21. Lucie RS, Wiedel JD, Messner DG. The acute pivot shift: clinical correlation. Am J Sports Med. 1984;12(3):189–191. [DOI] [PubMed] [Google Scholar]
- 22. Magnussen RA, Reinke EK, Huston LJ, et al. Effect of high-grade preoperative knee laxity on 6-year anterior cruciate ligament reconstruction outcomes. Am J Sports Med. 2018;46(12):2865–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marom N, Greditzer HG, 4th, Roux M, et al. The incidence of Kaplan fiber injury associated with acute anterior cruciate ligament tear based on magnetic resonance imaging. Am J Sports Med. 2020;48(13):3194–3199. [DOI] [PubMed] [Google Scholar]
- 24. Murgier J, Beranger JS, Boisrenoult P, Steltzlen C, Pujol N. Prospective comparative study of knee laxity with four different methods in anterior cruciate ligament tears. Int Orthop. 2018;42(8):1845–1851. [DOI] [PubMed] [Google Scholar]
- 25. Musahl V, Citak M, O’Loughlin PF, et al. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591–1597. [DOI] [PubMed] [Google Scholar]
- 26. Myrer JW, Schulthies SS, Fellingham GW. Relative and absolute reliability of the KT-2000 arthrometer for uninjured knees: testing at 67, 89, 134, and 178 N and manual maximum forces. Am J Sports Med. 1996;24(1):104–108. [DOI] [PubMed] [Google Scholar]
- 27. Robert H, Nouveau S, Gageot S, Gagniere B. A new knee arthrometer, the GNRB: experience in ACL complete and partial tears. Orthop Traumatol Surg Res. 2009;95(3):171–176. [DOI] [PubMed] [Google Scholar]
- 28. Sonnery-Cottet B, Daggett M, Fayard JM, et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament-deficient knee. J Orthop Traumatol. 2017;18(2):91–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Steiner ME, Brown C, Zarins B, et al. Measurement of anterior-posterior displacement of the knee: a comparison of the results with instrumented devices and with clinical examination. J Bone Joint Surg Am. 1990;72(9):1307–1315. [PubMed] [Google Scholar]
- 30. van Eck CF, Loopik M, van den Bekerom MP, Fu FH, Kerkhoffs GM. Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of instrumented knee laxity tests. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1989–1997. [DOI] [PubMed] [Google Scholar]
- 31. Vincent JP, Magnussen RA, Gezmez F, et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):147–152. [DOI] [PubMed] [Google Scholar]
- 32. Wiertsema SH, van Hooff HJ, Migchelsen LA, Steultjens MP. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008;15(2):107–110. [DOI] [PubMed] [Google Scholar]
- 33. Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45(14):3233–3242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.