Abstract
Objective:
A quick, efficient, and flexible screening tool is essential for identifying alcohol use disorder in a busy clinical context. The Alcohol Use Disorders Identification Test is the most widely used and validated screening tool in the outpatient context. The psychometric features of the Alcohol Use Disorders Identification Test have yet to be confirmed for Ethiopians. As a result, the purpose of this study was to evaluate the Alcohol Use Disorders Identification Test screening tool’s reliability and validity among medically ill patients in Ethiopia.
Method:
A total of 325 patients who visited the internal medicine outpatient department were included in this study. To diagnose alcohol use disorder based on the Diagnostic and Statistical Manual of Mental Disorders (5th ed.), the psychometric features of the Alcohol Use Disorders Identification Test were compared to the gold standard of Mini International Neuropsychiatry Interview. The reliability was determined by examining internal consistency. The receiver operating characteristic curve was established to calculate sensitivity and specificity of the screening tool. Construct validity was determined using confirmatory factor analysis.
Result:
The translated version of Alcohol Use Disorders Identification Test showed language clarity. Internal consistency was excellent (Cronbach’s α = 0.9). The Alcohol Use Disorders Identification Test provides an excellent receiver operating curve with cut-off point ⩾8 for females (sensitivity = 0.92, specificity = 0.87, positive predictive value = 70.2, negative predictive value = 96.9, likelihood ratio+ = 7.16, and likelihood ratio− = 0.1) and ⩾10 for males (sensitivity = 0.91, specificity = 0.84, positive predictive value = 72.6%, negative predictive value = 95.3%, likelihood ratio+ = 5.57, and likelihood ratio− = 0.10). Confirmatory factor analysis yielded good model fit indices for the two- and three-factor models, with the two-factor model outperforming the others.
Conclusion:
The Alcohol Use Disorders Identification Test has been proven to be a reliable tool for detecting alcohol use in gedofa-speaking medical outpatients.
Keywords: Alcohol Use Disorders Identification Test, validation, medical outpatients, Ethiopia
Introduction
Alcohol has been consumed since prehistories of humans, and it has taken part likely before the invention of bread. 1 The World Health Organization (WHO) estimates that over two billion individuals use alcoholic beverages on a daily basis around the world. Individuals over the age of 15 consume an average of 6.2 L of pure alcohol per year worldwide. Individuals over the age of 15 in Africa consume an estimated 6 L of pure alcohol every year. 2 The report also shows average consumption of alcohol in Ethiopia aged 15 years and older is 4.2 L per capita per year of which 3.5 L of consumption is unrecorded. 2
According to the Ethiopian Central Statistics Authority’s (CSA) 2016 Demographic and Health Poll (DHS), a countrywide survey with a representative sample of 15–49 years old, one-third of women (35%) and roughly half of males (46%) reported drinking alcohol at some point in their life. Among those who have ever consumed alcohol in the previous 30 days, 6% of women and 9% of males consumed alcoholic beverages practically every day. 3
Excessive alcohol intake raises the chance of developing an alcohol use disorder (AUD), which can vary from dangerous and destructive drinking to severe alcohol dependency. 4 The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5), which was last updated in 2013, combines the two Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) disorders of alcohol abuse and alcohol dependence into a single disease known as AUD, which is classified as mild, moderate, or severe. 5 The WHO defines hazardous drinking as an amount or pattern of alcohol intake that puts an individual at risk for negative health consequences.4,6 The WHO also recognizes harmful drinking, which is defined as alcohol intake that has a detrimental impact on physical and mental health.4,6 It is estimated that 4.1% of people aged 15 years and above are suffering from AUD globally, of which 1.8% were harmful drinkers and the rest 2.3% people were dependent to alcohol. AUD affects 3.3% of Africans, with 1.9% reported problematic usage and 1.4% reported alcohol dependency. 2
A variety of screening measures, including self-administered or interviewer-administered questionnaires, have been validated for detecting alcohol-related issues in various clinical contexts. The Alcohol Use Disorders Identification Test (AUDIT) is a well-known screening tool that is widely utilized in many countries and for various target populations. WHO developed and supports the AUDIT questionnaire as a screening tool. 7 It is used all over the world to detect early indicators of dangerous drinking and to detect moderate alcoholism. The questionnaire consists of 10 items in total. The first three questions (Questions 1–3) are targeted at assessing the degree of alcohol intake, the next Questions 4–6 are about dependent symptoms, and Questions 7–10 are about the repercussions of alcohol misuse and difficulties that may be created by excessive alcohol consumption. We can calculate the overall score based on the answers to the 10 AUDIT questionnaire subjects, which can vary from 0 to 40 points. The following is the recommended interpretation of the total score, which is backed up by several studies: 0–7 points—low-risk drinking, 8–19 points—risky or harmful drinking, and 20 points and higher—highly risky drinking with problems and a high likelihood of alcohol dependence. 4
The AUDIT was validated in multinational samples involving Kenya, 7 Zambia, 8 and South Africa. 9 In a research conducted validation of AUDIT screening tool among TB and HIV patients in Zambia primary healthcare center. The study used Mini International Neuropsychiatry Interview (MINI) for Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR) as a gold standard reference. The result showed the AUDIT had high internal consistency reliability (Cronbach’s α = 0.98). 8
Three recent African studies which assessed factor structure of AUDIT have been published in Zambia, Tanzania, and Uganda for different populations.8,10,11 A Tanzanian study revealed that all conceptual models (one-, two-, and three-factor models) fitted well with factor loading ranged from 0.41 to 0.71, suggested that any of these models were acceptable. 10 Confirmatory factor analysis (CFA) of Ugandan and UK study was also indicated that all the three factor models were acceptable, with three-factor model had shown overall superiority than one- and two-factor models.11,12 However, Chishinga et al. 8 investigated only the two-factor model of AUDIT using CFA and reported as the model fitted well in all model fit indices.
Despite the fact that the AUDIT is the most widely used screening tool that has been validated in an outpatient context, even though its psychometric qualities have not been tested for Ethiopians. Therefore, this study intended to fill this gap by assessing psychometrics properties of AUDIT screening tool among medical outpatients in Ethiopia.
Methods
Study design, period, and location
An institutional-based cross-sectional investigation was undertaken. From 1 April 2020 to 30 April 2020, the study was done in Dilla University Referral Hospital (DURH) medical outpatient. The DURH is located in Dilla, Ethiopia, in the South National Regional State. Dilla is located 359 km south of Ethiopia’s capital, Addis Ababa. It is the only referral hospital in the Gedeo Zone, with roughly 500 hospital employees serving a catchment area population of five million people, including the surrounding territories.
Study participants and sampling procedure
Simple random sampling using Medical Registered Number (MRN) as sampling frame was used till the maximum sample was reached. Medical out patients who screened to drink alcohol using single questionnaire for lifetime substance use were studied participants. The study covered all level medical outpatients who had attended DURH, as well as those who were available during the data collection period. Those who were critically unwell were excluded to participate in the study.
Determining a sample size
Sample size was determined using sensitivity and specificity for single validation test formula by considering the following assumption
where n is the required sample size, SN is the anticipated sensitivity, SP is the anticipated specificity, α is the size of the critical region (1 − α is the confidence level), Z1 − α/2 is the standard normal deviate corresponding to the specified size of the critical region (α), and L is the absolute precision desired on either side of sensitivity or specificity.
Based on the above formula, the following assumptions were used for calculating sample size as follows: anticipated sensitivity is 92.7% and anticipated specificity is 80%, α = 0.05, L (desired precision) = 0.05, , and the prevalence is 34.8%, which was taken from South Africa study. 13
Finally, the required sample size using the assumption for sensitivity and specificity of AUDIT screening tool was 299 and 180, respectively. The researcher has taken the required sample of 299 to have larger sample size. Considering 10% non-respondent, the total sample size is 329.
Socio-demographic data
A simple questionnaire was utilized to collect pertinent background information, such as age, gender, marital status, educational level, occupational position, and residence.
Gold standard reference
To identify current AUD, the Mini International Neuropsychiatric Interview (MINI) Version7.0 was employed. 14 The MINI 7.0 is a brief diagnostic structured interview designed to investigate psychiatric disorders using DSM-V diagnostic criteria. It is designed to be used by interviewers who were not experts. For the diagnosis, at least two answers from a total of 11 questions must be answered “yes.”
AUDIT
The WHO established the AUDIT as a straightforward means of screening for AUDs in the previous 12 months. 7 It has 10 questions about recent alcohol usage (Items 1–3), alcohol dependent syndromes (Items 4–6), and alcohol-related disorders (Items 7–10). Eight of ten items are rated on a 5-point scale 0–4; Item numbers 9 and 10 are rated on 3-point scale. The overall score is a number between 0 and 40. A total score of 8 or more is considered a strong predictor of alcoholism. The AUDIT was validated on Kenyan samples from around the world, 7 which has been validated in Zambia 8 and south Africa. 9 A research was conducted for the validation of AUDIT screening tool among TB and HIV patients in Zambia primary healthcare center. The result showed the AUDIT had high internal consistency reliability (Cronbach’s α = 0.98). 8
Data quality assurance
The lead investigator made daily supervision, control, and support data collectors, and each completed questionnaire was examined and the necessary feedback was supplied to interviewers the next morning. Each day, the lead investigator correctly handled, evaluated, and validated the obtained data for completeness and consistency. Only questionnaires which were properly filled and signed by the data collector were accepted.
Statistical analysis
The data were cleaned, coded, and entered into Epi data 3.1. Utilizing double data entry before being exported to the Statistical Package for the Social Sciences version 24 (SPSS 24) for statistical analysis. Frequencies, mean values, and standard deviations were calculated as descriptive statistics. Internal consistency and reliability were determined using Cronbach’s α coefficient. Internal consistency is measured on a scale of zero to one, with a value of 0.7 indicating adequate reliability. High reliabilities (0.95 or greater) are not always desirable because they suggest that things are completely redundant. Inter-rater reliability was assessed using the kappa coefficient.
The diagnostic accuracy of AUDIT was estimated using the Area under the Receiver Operating Curve (AUROC) and threshold scores that give high sensitivity and specificity with the associated 95% confidence interval (CI). Positive predicted value (PPV) and negative predicted value (NPV) and likelihood ratios (LRs) were also calculated for the yielded cut-off score. Positive and negative likelihood ratios (LR+ and LR−) indicated ⩾5 and ⩽0.1, respectively, were considered as acceptable. Construct validity of AUDIT was determined using CFA.
Results
Socio-demographic characteristics
A total of 325 patients took part in the research, with a response rate of 98.8%. The reason for non-interview was urgency for other work. Males comprised 55.4% (n = 180) of the respondents. The mean age of respondents was 32.5 ± 9.1 (SD) years. Of all participants, 52.6% were married followed by single 36.9%. Regarding educational status, 28% (n = 91) and 22.2% (n = 72) respondents had completed primary and secondary school education, respectively. Out of total participant, 20.3% were merchant followed by governmental employee (17.8%, n = 58%). Regarding current living place, majority of participants (63.1%) were residing in urban (Table 1).
Table 1.
Socio-demographic characteristics of people attending internal medicine clinic at DURH, southern Ethiopia, 2020 (n = 325).
| Variables | Category | Frequency | |
|---|---|---|---|
| Number (n = 325) | Percent (%) | ||
| Sex | Male | 180 | 55.4 |
| Female | 145 | 44.6 | |
| Age mean (SD, range) | 32.5 (SD = 9.1, range = 18–63) | ||
| Educational status | Uneducated | 47 | 14.5 |
| Able to read and write | 53 | 16.3 | |
| Primary (1–8) | 91 | 28.0 | |
| Secondary (9–12) | 72 | 22.2 | |
| Tertiary (+12) | 62 | 19.1 | |
| Marital status | Single | 120 | 36.9 |
| Married | 171 | 52.6 | |
| Divorced | 25 | 7.7 | |
| Windowed | 9 | 2.8 | |
| Occupation | Employed | 58 | 17.8 |
| Farmer | 55 | 16.9 | |
| Merchant | 66 | 20.3 | |
| House wife | 44 | 13.5 | |
| Daily laborer | 38 | 11.7 | |
| Student | 44 | 13.5 | |
| Unemployed | 20 | 6.2 | |
| Residency | Urban | 205 | 63.1 |
| Rural | 120 | 36.9 | |
SD: standard deviation.
Semantic validity
The translated (gedofa) version of AUDIT was compared with the original version (English) of AUDIT. There were no major discrepancies among each of 10 items which resulted meaning difference. The team which consisted of linguistic professionals from Dilla University and psychiatry professional were finally reached to consensus as the gedofa version of AUDIT is understandable and culturally acceptable for gedofa-speaking populations.
Reliability of AUDIT
Reliability of internal consistency for AUDIT was excellent (Cronbach’s α = 0.90). The inter-item correlation matrix revealed that inter-item correlations ranged from 0.23 between Item 2 (amount in a typical day) and Item 10 (concern of others about drinking) to 0.757 between Item 6 (need alcohol first in the morning) and Item 7 (concern of others about drinking) (feelings of guilty). All 10 items were significantly correlated (r ⩾ 0.30) with at least two other items in the matrix. The corrected item-total correlation coefficient of each item exceeds 0.5, and it ranged from 0.522 to 0.783, indicating as all items are measuring the same construct. Item 6 (need a first drink in the morning) achieved the highest correlation (0.783) with the scale (Table 2).
Table 2.
Reliability and item analyses of AUDIT to detect alcohol use disorder among medical patients in DURH, southern Ethiopia, 2020 (n = 325).
| Scale mean if item deleted | Corrected item-total correlation | Cronbach’s α if item deleted | |
|---|---|---|---|
| Item 1 | 10.23 | 0.532 | 0.897 |
| Item 2 | 11.04 | 0.522 | 0.897 |
| Item 3 | 11.48 | 0.576 | 0.894 |
| Item 4 | 11.99 | 0.730 | 0.884 |
| Item 5 | 12.04 | 0.769 | 0.882 |
| Item 6 | 12.01 | 0.783 | 0.881 |
| Item 7 | 11.97 | 0.761 | 0.882 |
| Item 8 | 12.12 | 0.712 | 0.886 |
| Item 9 | 12.29 | 0.585 | 0.896 |
| Item 10 | 12.35 | 0.579 | 0.896 |
Cronbach’s α: 0.90.
Mean inter-item correlation: 0.48.
Kappa coefficient: 0.93.
Removing of any of the 10 items of the questionnaire did not improve α coefficient value (Table 3). Inter-rater reliability of AUDIT provided a kappa coefficient of 0.93, indicating an excellent agreement between two data collectors.
Table 3.
Inter-item correlation matrix of AUDIT to detect alcohol use disorder among medical patients in DURH, southern Ethiopia, 2020 (n = 325).
| Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Item 1 | ||||||||||
| Item 2 | 0.590 | |||||||||
| Item 3 | 0.603 | 0.622 | ||||||||
| Item 4 | 0.399 | 0.379 | 0.398 | |||||||
| Item 5 | 0.370 | 0.429 | 0.418 | 0.724 | ||||||
| Item 6 | 0.411 | 0.385 | 0.467 | 0.729 | 0.711 | |||||
| Item 7 | 0.400 | 0.349 | 0.391 | 0.637 | 0.687 | 0.757 | ||||
| Item 8 | 0.404 | 0.347 | 0.486 | 0.546 | 0.600 | 0.704 | 0.693 | |||
| Item 9 | 0.395 | 0.258 | 0.272 | 0.469 | 0.547 | 0.431 | 0.503 | 0.414 | ||
| Item 10 | 0.381 | 0.230 | 0.307 | 0.466 | 0.468 | 0.471 | 0.491 | 0.461 | 0.637 |
Criterion validity of AUDIT
Criterion ROC analysis was used to determine the validity of AUDIT in detecting AUDs. The area under the curve for DSM-V was 0.94 when the overall score of AUDIT was compared to the gold standard measure of MINI 7.0 (95% CI = 0.91–0.96). The most appropriate cut-off point for concurrently optimizing sensitivity and specificity is 8. The sensitivity and specificity were 94% and 84%, respectively, with 70% PPV and 97% NPV at this cut-off point. For AUDIT 8 with Youden’s Index (0.77), the LR+ and LR− were 5.67 and 0.08, respectively. Lowering the cut-off value to 7 indicated that the specificity, PPV and LR+ would relatively decrease to 80%, 65.7%, and 4.7, respectively. When cut-off value was raised to 9, the sensitivity became fall to 88% and LR− considerably increased to 0.14. Figures 1 and 2 displayed the ROC curve of AUDIT 0.93 (95% CI = 0.90–0.97) for males and 0.96 (95% CI = 0.92–0.99) for female separately.
Figure 1.
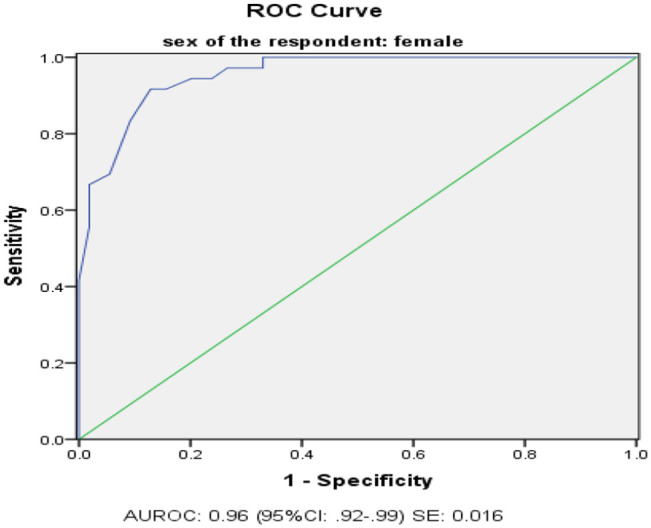
Receiving operating characteristics (ROC) curve of AUDIT for identifying alcohol use disorders among female participants in 2020.
Figure 2.
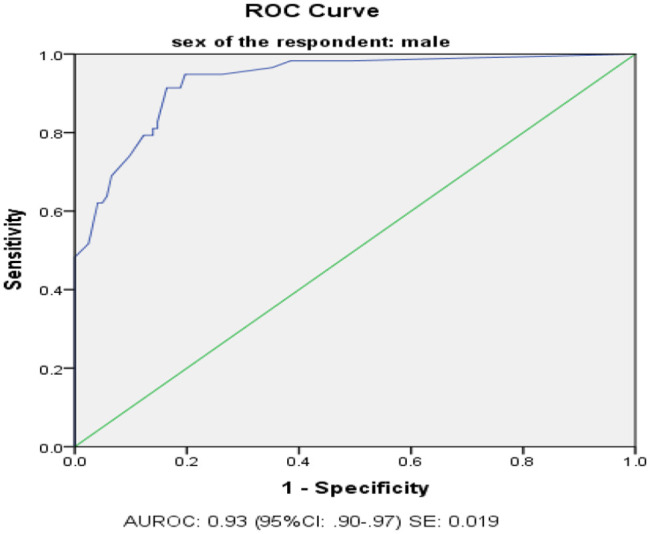
Receiving operating characteristics (ROC) curve of AUDIT for identifying alcohol use disorders among male participants in 2020.
The appropriate cut-off score for male was 10, yielded sensitivity of 0.91, specificity of 0.84, PPV of 72.6%, NPV of 95.3%, LR+ of 5.57, and LR− of 0.10. The optimum cut-off score for female was 8, provided that sensitivity of 0.92, specificity of 0.87, PPV of 70.2, NPV of 96.9, LR+ of 7.16, and LR− of 0.1 (Table 4).
Table 4.
Diagnostic properties of AUDIT to detect alcohol use disorder among medical patients in DURH, southern Ethiopia, 2020 (n = 325).
| AUDIT cut-off score | Sensitivity | Specificity | PPV | NPV | LR+ | LR− | Youden’s Index | |
|---|---|---|---|---|---|---|---|---|
| Total | 5 | 0.96 | 0.70 | 56.6 | 97.6 | 3.20 | 0.06 | 0.66 |
| 6 | 0.95 | 0.77 | 62.2 | 97.3 | 4.05 | 0.07 | 0.71 | |
| 7 | 0.94 | 0.80 | 65.7 | 96.9 | 4.70 | 0.08 | 0.74 | |
| 8 | 0.94 | 0.84 | 69.8 | 97.0 | 5.67 | 0.08 | 0.77 | |
| 9 | 0.88 | 0.86 | 71.6 | 94.7 | 6.17 | 0.14 | 0.74 | |
| 10 | 0.83 | 0.89 | 75.0 | 92.8 | 7.35 | 0.19 | 0.72 | |
| 11 | 0.77 | 0.91 | 78.3 | 90.6 | 8.80 | 0.26 | 0.68 | |
| 12 | 0.76 | 0.91 | 78.0 | 90.2 | 8.68 | 0.27 | 0.67 | |
| 13 | 0.76 | 0.92 | 78.9 | 90.2 | 9.21 | 0.27 | 0.67 | |
| 14 | 0.71 | 0.92 | 77.9 | 88.7 | 8.70 | 0.31 | 0.63 | |
| Area under the curve for men = 0.93 (95% CI = 0.90–0.97); SE = 0.019 | ||||||||
| For male | 5 | 0.97 | 0.65 | 56.6 | 97.5 | 2.74 | 0.05 | 0.61 |
| 6 | 0.95 | 0.74 | 63.2 | 96.8 | 3.62 | 0.07 | 0.69 | |
| 7 | 0.95 | 0.76 | 65.5 | 96.9 | 3.98 | 0.07 | 0.71 | |
| 8 | 0.95 | 0.80 | 69.6 | 97.0 | 4.81 | 0.06 | 0.75 | |
| 9 | 0.91 | 0.81 | 69.7 | 95.7 | 4.84 | 0.11 | 0.73 | |
| 10 | 0.91 | 0.84 | 72.6 | 95.3 | 5.57 | 0.10 | 0.75 | |
| 11 | 0.83 | 0.85 | 72.7 | 91.2 | 5.59 | 0.20 | 0.68 | |
| 12 | 0.81 | 0.85 | 72.3 | 90.4 | 5.47 | 0.22 | 0.66 | |
| 13 | 0.81 | 0.86 | 73.4 | 90.5 | 5.83 | 0.22 | 0.67 | |
| 14 | 0.79 | 0.86 | 73.0 | 89.7 | 5.71 | 0.24 | 0.65 | |
| Area under the curve for men = 0.93 (95% CI = 0.90–0.97); SE = 0.019 | ||||||||
| For female | 5 | 0.94 | 0.76 | 56.7 | 97.6 | 3.95 | 0.07 | 0.71 |
| 6 | 0.94 | 0.80 | 60.7 | 97.8 | 4.67 | 0.07 | 0.74 | |
| 7 | 0.92 | 0.84 | 66.0 | 96.8 | 5.88 | 0.10 | 0.76 | |
| 8 | 0.92 | 0.87 | 70.2 | 96.9 | 7.16 | 0.10 | 0.79 | |
| 9 | 0.83 | 0.91 | 75.0 | 94.3 | 9.05 | 0.18 | 0.74 | |
| 10 | 0.69 | 0.95 | 80.6 | 90.4 | 12.62 | 0.32 | 0.64 | |
| 11 | 0.67 | 0.98 | 92.3 | 89.9 | 37.06 | 0.34 | 0.65 | |
| 12 | 0.58 | 0.98 | 92.3 | 89.9 | 32.39 | 0.42 | 0.57 | |
| 13 | 0.56 | 0.98 | 92.3 | 89.9 | 30.89 | 0.45 | 0.54 | |
| 14 | 0.42 | 1.00 | 91.3 | 87.7 | – | 0.58 | 0.42 | |
| Area under the curve for women = 0.96 (95% CI = 0.92–0.99); SE: 0.016 | ||||||||
PPV: positive predictive value; NPV: negative predictive value; LR: likelihood ratio; CI: confidence interval; SE: standard error.
Bold indicated an optimum cut-off point corresponding with diagnostic properties.
Construct validity of AUDIT
CFA
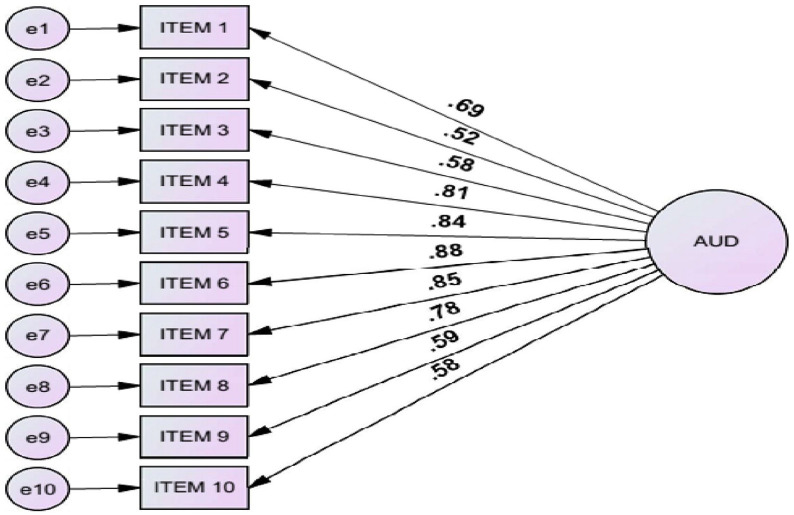
CFA was used to assess the fitness of AUDIT for one-factor, two-factor, and three-factor models which are proposed in prior research works. For each factor solution, the acceptable model fit was determined using model fit indices. The value of chi-square test with degree of freedom for all three factor solutions indicated significant test statics (p-value = 0.00). However, because chi-square is sensitive for high sample sizes, the result should be interpreted with caution as a poor fit model. The one-factor model did not give an acceptable model fit for the data (comparative fit index (CFI) of 0.81, a Tucker–Lewis index (TLI) of 0.82, and root mean squared error approximation (RMSEA) of 0.13). Factor loading were ranged from 0.60 (frequency of drinking) to 0.85 (need a morning drink) (Figure 3).
Figure 3.
One-factor model of AUDIT with corresponding factor loading of items in DURH medical patients 2020 (n = 325).
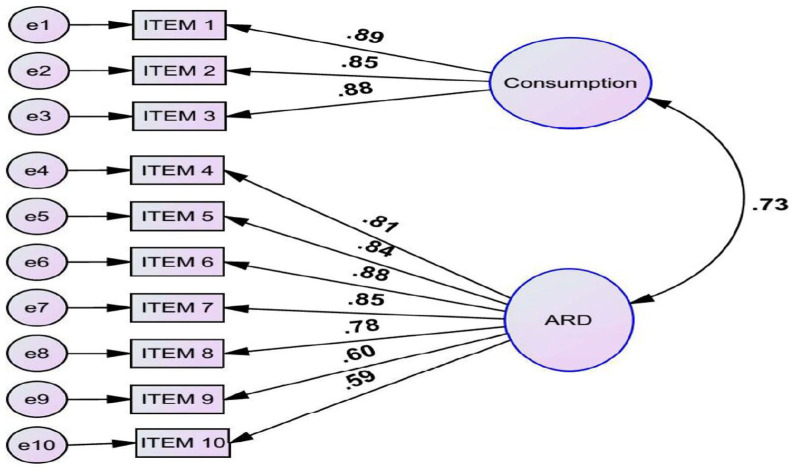
The factor two and three models had shown improvement considerably to all fit indices than factor one model. The standardized factor loading for each item was also parallel with factor two models. The two-factor models, which represent alcohol consumption (Items 1–3) and alcohol-related problem, provided acceptable fit indices in CFI and TLI indices. The value of RMSEA (0.08) was also at the edge. In factor two model, all the items loaded above 0.5 which ranged from 0.59 Item 10 (concern of others) to 0.89 Item 1 (frequency of drinking). Internal consistency of the two subscales provided 0.82 and 0.90 for alcohol consumption and alcohol-related problems, respectively (Figure 4).
Figure 4.
Two-factor model of AUDIT with corresponding factor loading of items in DURH medical patients 2020 (n = 325).
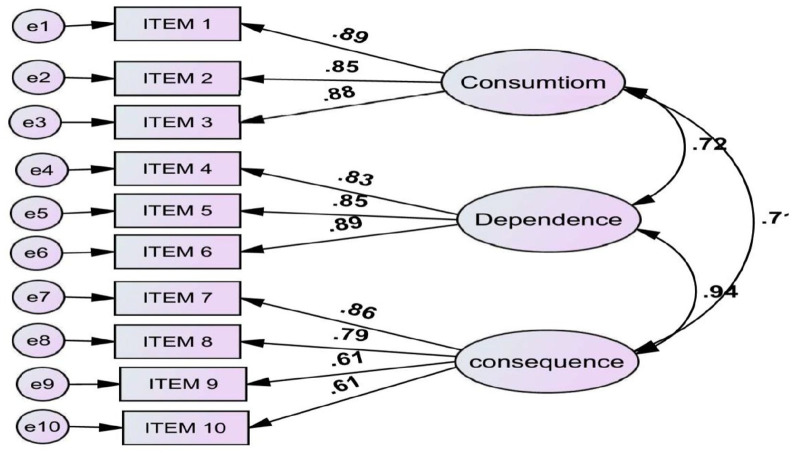
The three-factor model, which exemplifies the AUDIT developer factors, provided almost equivalent fit indices with factor two models. The estimated correlation between alcohol consumption and dependence was 0.72 and between alcohol consumption and consequence was 0.71. However, the correlation between alcohol dependence and consequence was very high (r = 0.94, p < 0.001) which revealed that there was an extensive overlap between two factors. Internal consistency for this model was (Cronbach’s α = 0.82, 0.87, and 0.81) respectively for alcohol consumption, dependence, and alcohol-related problems as indicated in Figure 5.
Figure 5.
Three-factor model of AUDIT with corresponding factor loading of items in DURH medical patients 2020 (n = 325).
Hence, selection of the paramount model fit should be determined based on comparison of parsimony value. As a result, factor two models provided more parsimony normed fit index (PNFI) (0.55) and parsimony comparative fit index (PCFI) (0.57) than factor three models with PNFI (0.54) and PCFI (0.52). Furthermore, the two component model showed that high correlation between alcohol dependence and alcohol consequence (r = 0.94) indicated that the two-factor model had an adequate factor structure (Table 5).
Table 5.
Fit indices for alternating models of AUDIT, estimated correlation among factors, and internal consistency for each subscale to detect alcohol use disorder among medical patients in DURH, southern Ethiopia, 2020 (n = 325).
| Indices of model fit | Factor one | Factor two | Factor three |
|---|---|---|---|
| Chi-square | 249.91 | 133.75 | 123.82 |
| Degree of freedom | 35 | 34 | 32 |
| p-value | 0.00 | 0.00 | 0.00 |
| CFI | 0.81 | 0.92 | 0.92 |
| TLI | 0.82 | 0.92 | 0.93 |
| RMSEA | 0.13 | 0.08 | 0.07 |
| PNFI | 0.51 | 0.55 | 0.54 |
| PCFI | 0.52 | 0.57 | 0.52 |
| Estimated correlations among factors | |||
| Factor one | 1 | – | – |
| Factor two | 0.73 | 1 | – |
| Factor three | 0.71 | 0.94 | 1 |
| Cronbach’s α for each subscale | |||
| Factor one model | 0.90 | – | – |
| Factor two model | 0.82 | 0.90 | |
| Factor three model | 0.82 | 0.87 | 0.81 |
CFI: comparative fit index; TLI: Tucker–Lewis Index; RMSEA: root mean squared error approximation; PNFI: parsimony normed fit index; PCFI: parsimony comparative fit index.
Discussion
The purpose of this study was to demonstrate that the AUDIT has psychometric properties for detecting AUD among gedofa-speaking medical patients. This result confirmed that AUDIT has excellent internal consistency, showing that the scale as a whole has well-represented the hypothesized construct, with a Cronbach’s coefficient of 0.90.
A comprehensive examination of AUDIT published after 2002 indicated a comparable median reliability coefficient of 0.83, ranging from 0.75 to 0.97. 15 However, the reliability found in this study is higher than the study done in Persia (Cronbach’s α = 0.77) and Malaysia (Cronbach’s α = 0.82).16,17 Small sample numbers in Persia and Malaysia (N = 70 and N = 52, respectively) might be explain the discrepancy. The high Cronbach’s α coefficients obtained in this study for each subscale of the AUDIT’s two and three components model were similar to those discovered in previous research published in Brazil, Australia, and the United States.18,19
The ROC of AUDIT has shown an area under curve of 0.94 (95% CI = 0.91–0.96) which was similar with a Japanese validation study of Fujii et al. 20 among medical outpatients found AUROC of 0.97. Chishinga et al. 8 was also found comparable AUROC of 0.96 among Zambian HIV and TB patients. This implies that the tool has high degree of performance to distinguish AUDs among medical outpatients. However, it was higher than the study done in Russia (AUROC = 0.80). 21 This may be due to the difference of gold standard reference tool (they used composite international diagnostic interview for alcohol as a gold standard).
The result recorded excellent diagnostic properties at an optimal cut-off point of 8 which is similar with initially recommended cut-off point by the tool inventors. Seven similar cut-off points were also reported in Persian and Russian version of AUDIT.16,21 The cut-off threshold in this study was slightly lower than the optimal cut-off score of 9 for both sexes reported in a study in Nepal. 22 This might be due to the difference in gold standard tool which was structural clinical interview diagnosis (SCID vs MINI). This study provided different cut-off scores among gender with 10 for males and 8 for females. Reinert and Allen 23 in their systematic review supported the need of different cut-off scores for males and females and suggested as cut-off value is lower in females than in males. This study’s indicated cut-off value for both sexes is consistent with a Korean study of medical outpatients. 24
The result recorded satisfactorily high sensitivities, specificities, and NPV for both sexes but moderate PPV (72.6% for males and 70.2% for females). This indicates that those who screened positive about one-third of patients were actually false positive cases. The estimated value of PPV in this study was poorer than Nepal study (90.3% for males and 80.1% for females). 22 In contrast, many previous research works published in different settings reported as AUDIT had lower value of PPV with satisfactory other diagnostic parameters. Chang-Gi Kim et al. 24 reported lower PPV (73.85% for males and 58.06% for females) of Korean outpatients and Perula de Torres et al. were also reported 53% of PPV for Spanish patients with adequate sensitivity, specificity, and NPV. 25 The findings of this investigation resemble those of the previous studies.
The factor component of AUDIT items were originally organized into three dimensions by developers: alcohol intake (Items 1–3), alcohol dependency (Items 4–6), and hazardous drinking (Items 7–10). 7 Further analyses of internal structure of AUDIT for the one, two, and three dimensions model were determined by CFA. The result of CFA reveled that factor two models had shown improvement considerably to all fit indices than factor one and three models. These two-factor structure model is consistent to findings of previous studies performed in Tanzania, Zambia, and Malaysia.8,10,17 In addition, a systematic review examined seven studies on factorial structure of AUDIT arrived at a conclusion that the two-factor model was preferable. 15
In comparison to the two and three component models, the one-factor model produced poor model fit indices in all parameters in this study which is consistent with other studies in Uganda and the United Kingdom.11,12 Despite the fact that the one-factor model had a low model fit, the empirical findings show that it had excellent internal consistency and acceptable factor loading for each item. Lima et al. 18 suggested as poor model for one-factor structure does not detract the application of single-factor structure of AUDIT items to quantify a global assessment of AUDs.
Limitations of the study
This study was examined only in medical outpatients who visited DURH. Hence, the result may differ in other clinical setting like general hospital and other primary healthcare setting. In addition, generalizability of the result to other language-speaking patients other than gedofa should be taken in caution since the language by itself is varied in wording and cultural acceptability across the country.
Interview technique was applied to respondents in where their attendants were with them. This might result in social desirability bias. Self-administered technique is recommended once semantic validity has been done. However, this approach could not be applicable in low literacy population group.
Conclusion
To the best of the researcher knowledge, this study is the first validation study of AUDIT among Ethiopian populations speaking gedofa language. The result exhibited as AUDIT can be used as reliable and valid tool to detect AUDs in a busy medical outpatient setting. Diagnostic performance of AUDIT against MINI provided an AUROC of 0.94.
An optimal cut-off score is ⩾8 for females and ⩾10 for males. At this cut-off point, the tool provides satisfactory sensitivity, specificity, and NPV but modest PPV for both sexes. The correlation between each subscale of two-factor model was acceptable. High item loading of each item and its excellent internal consistency would make the structure applicable for global assessment of AUDs.
Recommendations
The following recommendations are forward to the concerned stakeholders:
To medical outpatient clinicians: comorbidity of AUDs among medical outpatients has to be taken into consideration and screening of AUDs with AUDIT is recommended to all patients.
To Dilla University Referral Hospital: advocacy and training of AUDIT screening tool for clinicians working in medical outpatient clinic is recommended. Through this, quality of service and integration of inter departments will be guaranteed.
For future researchers: the finding of this study is recommended to use as a validated tool to researchers who are interested in AUDs in medical setting. Furthermore, validation of AUDIT across different languages and settings is an eligible area to be studied in the future.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121221077568 for Psychometric properties of Alcohol Use Disorder Identification Test screening tool among medical outpatients in Dilla University Referral Hospital, southern Ethiopia, 2020 by Endashaw Habtamu and Derebe Madoro in SAGE Open Medicine
Acknowledgments
The authors of this study would like to express their gratitude to the entire employees of the hospital administration. Dilla University’s, College of Health and Medicine, deserves our gratitude. Finally, the authors want to express their gratitude to all of the participants for their cooperation and assistance in gathering the essential information.
Footnotes
Author contributions: E.H. conceived the research idea, wrote the proposal, conducted the analysis, and finalized the paper. D.M. came up with the research concept, wrote the manuscript, revised the proposal, and double-checked the data analysis and write-up. Finally, the final paper was read and approved by all of the authors.
Ethical approval: The study was carried out after getting ethical approval from Dilla University’s College of Health Science and Medicine’s ethical review board with ethical approval number of du/234/8/111, as well as a permission letter obtained from the medical director of Dilla University’s Referral Hospital.
Informed consent: After explaining the study’s goal, we got written informed consent from all study participants. The information gathered was kept private throughout the investigation and was solely used for the purpose of the study.
ORCID iD: Derebe Madoro  https://orcid.org/0000-0001-6901-2892
https://orcid.org/0000-0001-6901-2892
Supplemental material: Supplemental material for this article is available online.
References
- 1. Keller M. A historical overview of alcohol and alcoholism. Cancer Res 1979; 39: 2822–2829. [PubMed] [Google Scholar]
- 2. World Health Organization (WHO). Global status report on alcohol and health 2014. Geneva: WHO Press, 2014. [Google Scholar]
- 3. Central Statistical Agency. Demographic and health survey 2016. Addis Ababa, Ethiopia; Rockville, MD: CSA and ICF, 2017. [Google Scholar]
- 4. Babor TF, Higgins-biddle JC, Saunders JB, et al. The alcohol use disorders identification yest: guidelines for use in primary care. 2nd ed. Geneva: Department of Mental Health and Substance Dependence, World Health Organization, 2001. [Google Scholar]
- 5. Pataki CS, Sussman N, Sadock BJ, et al. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. New York: Lippincott Williams & Wilkins, 2013, pp. 591–595. [Google Scholar]
- 6. Study C, Gordon AJ, Saitz R. Identification and management of alcohol use disorders in primary care. J Clin Outcomes Manag 2010; 11(7): 444–460. [Google Scholar]
- 7. Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction 1993; 88(6): 791–804. [DOI] [PubMed] [Google Scholar]
- 8. Chishinga N, Kinyanda E, Weiss HA, et al. Validation of brief screening tools for depressive and alcohol use disorders among TB and HIV patients in primary care in Zambia. BMC Psychiat 2011; 11: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pengpid S, Peltzer K, Skaal L, et al. Screening and brief interventions for hazardous and harmful alcohol use among hospital outpatients in South Africa: results from a randomized controlled trial. BMC Public Health 2013; 13: 644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ricardo J, Vissoci N, Hertz J, et al. Cross-cultural adaptation and psychometric properties of the AUDIT and CAGE questionnaires in Tanzanian Swahili for a traumatic brain injury population. Alcohol Alcohol 2018; 53: 112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blair AH, Pearce ME, Katamba A, et al. The Alcohol Use Disorders Identification Test (AUDIT): exploring the factor structure and cutoff thresholds in a representative post-conflict population in Northern Uganda 2017; 52: 318–327. [DOI] [PubMed] [Google Scholar]
- 12. Shevlin M, Smith GW. The factor structure and concurrent validity of the alcohol use disorder identification test based on a nationally representative. Alcohol Alcohol 2007; 42(6): 582–587. [DOI] [PubMed] [Google Scholar]
- 13. Pengpid S, Peltzer K, Heever H, et al. Prevalence of alcohol use and associated factors in urban hospital outpatients in South Africa. Int J Environ Res Public Health 2011; 8: 2629–2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sheehan D, Janavas J, Harnett-Sheehan K, et al. Mini international neuropsychiatric interview Tampa, USA, 2009. https://eprovide.mapi-trust.org/instruments/mini-international-neuropsychiatric-interview
- 15. Meneses-gaya C, De Zuardi AW, Loureiro SR, et al. Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. Psychol Neurosci 2009; 2(1): 83–97. [Google Scholar]
- 16. Zavar A, Jarahi L, Alimoradi B, et al. The Alcohol Use Disorders Identification Test (AUDIT): reliability and validity of the Persian version. Asia Pacific J Med Toxicol 2015; 4: 37–42. [Google Scholar]
- 17. Yee A, Adlan ASA, Rashid RR, et al. Validation of the alcohol use disorders identification test (AUDIT)—Bahasa Malaysia version among a group of alcohol users. J Subst Use 2014; 20: 229–233. [Google Scholar]
- 18. Lima CT, Freire ACC, Silva APB, et al. Concurrent and construct validity of the audit in an urban Brazilian sample. Alcohol Alcohol 2005; 40(6): 584–589. [DOI] [PubMed] [Google Scholar]
- 19. Wade D, Ph D, Varker T, et al. Examination of the latent factor structure of the Alcohol Use Disorders Identification Test in two independent trauma patient groups using confirmatory factor analysis. J Subst Abuse Treat 2012; 43(1): 123–128. [DOI] [PubMed] [Google Scholar]
- 20. Fujii H, Nishimoto N, Yamaguchi S, et al. The Alcohol Use Disorders Identification Test for Consumption (AUDIT-C) is more useful than pre-existing laboratory tests for predicting hazardous drinking: a cross-sectional study. BMC Publ Health 2016; 16: 379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mathew TA, Shields AL, Golubchikova VT, et al. Performance of the alcohol use disorders identification test among tuberculosis patients in Russia. NIH Public Access 2011; 45(4): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pradhan B, Chappuis F, Baral D, et al. The alcohol use disorders identification test (AUDIT): validation of a Nepali version for the detection of alcohol use disorders and hazardous drinking in medical settings. Subst Abuse Treat Prev Policy 2012; 7: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reinert DF, Aleen JP. The Alcohol Use Disorders Identification Test: an update of research findings. Alcohol Clin Exp Res 2007; 31(2): 185–199. [DOI] [PubMed] [Google Scholar]
- 24. Kim C, Kim JS, Jung J, et al. Reliability and Validity of Alcohol Use Disorder Identification Test-Korean revised version for screening at-risk drinking and alcohol use disorders. Korean J Fam Med 2014; 35(1): 2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Angel L, Torres P, De Rebollo EM, et al. Diagnostic usefulness of the Alcohol Use Disorders Identification Test (AUDIT) questionnaire for the detection of hazardous drinking and dependence on alcohol among Spanish patients. Eur J Gen Pract 2009; 15: 15–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121221077568 for Psychometric properties of Alcohol Use Disorder Identification Test screening tool among medical outpatients in Dilla University Referral Hospital, southern Ethiopia, 2020 by Endashaw Habtamu and Derebe Madoro in SAGE Open Medicine