Abstract
Background and Aim
The COVID‐19 is a stigmatizing infectious disease even after healing. Until now, no COVID‐19 stigma scale validated in Tunisian Arabic language among the general population is available. Developing such tools is necessary to detect COVID‐19 stigma and reduce it effectively. Indeed, stigmatization of COVID‐19 patients could increase the spread of this disease and its related mental health issues. We aimed at testing the validity of a translated and modified version of the 12‐item HIV stigma scale among Tunisian COVID‐19 patients.
Methods
A cross‐sectional study was conducted between November and December 2020 among a representative sample of COVID‐19 patients in the governorate of Sousse, Tunisia, after quarantine. The 12‐item HIV stigma scale was translated in Tunisian Arabic and then modified to be adapted to the Tunisian context. The preliminary modified version was administrated to the participants by pretrained medical doctors during phone calls. It consisted on 20 items covering the four stigma dimensions (personalized stigma, disclosure concerns, concerns with public attitudes, and negative self‐image). The psychometric evaluation of this version included internal consistency as well as principal component analysis (PCA).
Results
The responses of 346 COVID‐19 patients were obtained. Their median age was 40 years (interquartile range: 30‐54.5). Females represented 60.4% of them. The PCA resulted in a three factor solution with 14 items. This 14‐item scale demonstrated good internal consistency with a global Cronbach's α of 0.91 and values of 0.94, 0.93, and 0.98 for social stigma, negative self‐image, and disclosure concerns, respectively.
Conclusion
This study provides a reliable and valid instrument for stigma measuring among Tunisian COVID‐19 patients. The use of this scale would contribute in reducing the spread of this new infectious disease and its related mental health issues.
1. BACKGROUND
The COVID‐19 outbreak has provoked rejection of people with certain ethnic backgrounds, health care workers, patients with COVID‐19 infection as well as their families. 1 Indeed, a systematic review on previous infectious outbreaks over the last 20 years revealed a high prevalence of stigma related to this kind of disease. 2 This discriminatory behavior may remain even after recovery. 2 Consequently, COVID‐19 patients may hide their infection episode and avoid medical care which can lead to severe consequences for their physical and mental health. 1 At the collective level, stigma may result in more difficulties in controlling the pandemic spread for public health authorities. 2 , 3 , 4 , 5 A recent meta‐analysis underlined higher prevalence of COVID‐19 stigma in low and middle income countries including Arab countries. 6 However, a variety of tools was used to measure this issue in these countries. 6 , 7 , 8 Actually, little interest was given to develop and valid specific scales measuring COVID‐19‐related stigma among patients worldwide. 9 , 10 Furthermore, several studies focused on stigma toward healthcare providers, while fewer studies assessed stigma among the general population. 9 , 11
At the time of the current study, no Arabic scale was available to measure stigma in the Arab speaking countries. Besides, in the North African region, researchers put more emphasis on the clinical aspects of COVID‐19 infection and overlooked its psychosocial impact. 12 , 13
Providing valid tools to measure COVID‐19 stigma is crucial not only for healthcare professionals but also for policy makers to monitor and reduce the spread of COVID‐19 and its related mental health issues. 2
To address this gap, we translated, adapted, and tested the psychometric properties of the Berger‐HIV stigma scale. 14 This tool would be able to measure COVID‐19 related stigma among the Tunisian general population after quarantine accurately and reliably?
The HIV shares similar characteristics with COVID‐19 in terms of social isolation, fear of contagion and community discrimination. 10 It also evaluate stigma in its various aspects: personalized stigma; disclosure concerns; negative self‐image; and concern with public attitudes. 15 This questionnaire was widely used as screening tool for stigma in previous infectious outbreaks as well as in this current pandemic. 9 , 10 , 16 , 17 Accordingly, we hypotheses that this tool would represent a reliable and accurate tool to measure COVID‐19 related stigma among the Tunisian general population after quarantine.
Accordingly, the aim of the current study was to determine whether a translated and modified version of the 12‐item HIV stigma scale is reliable and accurate among adults with COVID‐19 infection after quarantine in Sousse, Tunisia.
2. METHODS
2.1. Study design
A cross‐sectional study was conducted between the sixth of November and the 12th of December 2020 among patients with confirmed SARS‐COV‐2 infection in the governorate of Sousse (Tunisia) during the third week after diagnosis.
2.2. Study population
Participants were recruited from a dynamic cohort of 375 patients newly diagnosed with COVID‐19 in the governorate of Sousse. This cohort was followed to evaluate compliance with home‐quarantine and the prognosis of COVID‐19 among them. To constitute this cohort, simple random sampling of 15 patients was daily performed among the new declared COVID‐19 cases between the 28th of October and the 28th of November 2020. The daily lists of patients newly diagnosed with COVID‐19 were obtained from the Regional Health Direction of Sousse. These lists contained data about the sociodemographic characteristics, the origin, and contact information. Duplicated patients, those from other governorates and those without contact details were deleted from the lists before performing randomization. The mean of daily number of cases in the region was 67 ± 4 during the study period.
2.3. Inclusion and exclusion criteria
From this cohort of 375 patients, those above the age of 18 years and which gave informed consent were included to the current study. Foreign patients, those who were hospitalized and those with sensorial problems or any clinical condition that could affect comprehension capacities, were not included to the current study.
2.4. Procedure
Three pretrained medical doctors administrated a pretested questionnaire written in Tunisian Arabic to each participant by interview during two phone calls. The first part of the questionnaire, administrated during the first week from diagnosis, served to collect data about the sociodemographic characteristics (age, gender, and profession), the setting of quarantine, the occurrence of new cases of COVID‐19 at home or at work, and the impact of the COVID‐19 on its professional and financial situation. The second part of the questionnaire, administrated during the fourth week from the diagnosis, focused on stigma related to the COVID‐19 episode. Responses of participants were registered electronically using Google forms. To ovoid missing data, all responses were mandatory before sending each completed form.
2.5. Measurement tool
The 40‐item HIV stigma scale 14 was developed and validated by Berger et al in the Sweden context in 2001. The 12‐items short version showed satisfactory construct validity and reliability comparing to psychometric properties of the full‐length scale (Cronbach's α for the subscales were all >0.7). 15 This questionnaire was widely used as screening tool for stigma in previous infectious outbreaks as well as in this current pandemic. 9 , 10 , 16 , 17 Thus, we used this short version with its four subscales intended to evaluate concerns with public attitudes, personalized stigma, negative self‐image, and disclosure concerns. 15 The response format was maintained: a 4‐point Likert scale ranging from strongly disagree (1) to strongly agree (4). Responses were then summed to calculate subscale scores. Higher scores indicate a greater level of Covid‐19‐related stigma.
2.6. Translation and cross‐cultural adaptation of the scale
The cross cultural adaptation of the short version of the HIV stigma scale was ensured as proposed by Guillemin et al. 18 : First, the 12 items were translated from English to Tunisian Arabic by three bilingual experts (Native Tunisian Arab‐speaking people) previously informed about the study purpose. Then the Tunisian Arabic scale version was re‐translated to English by three other professional translators. A group of multidisciplinary experts (security risk management, public health, and medical English), compared the two versions and ensured that the Arabic version was clear, relevant and preserves the original meaning.
2.7. Modification of the scale
After reviewing the literature about tools related to stigma against other diseases 19 , 20 and interviewing 70 COVID‐19 patients diagnosed during October 2020, eight items in Tunisian dialect were added to the translated version (five for concern about public attitudes dimension and three for negative self‐image dimension). The experimental version of the COVD‐19 stigma scale contained 20 items with the same number of dimensions as the original English version of the scale (more details are shown in Appendix 1).
2.8. Validation of the modified scale
2.8.1. Face validity
The experimental version of the stigma scale was pretested on a convenience sample of 30 patients 1 week after the end of their home quarantine to assess the cultural acceptability and the understandability of the items. Unclear items and those that were difficult to understand by two or more patients were reformulated taking into account their comments and the opinion of experts.
2.8.2. Content validity
The experimental version of the stigma scale was given to two other experts who were familiar with psychometric methods for assessment of content validity. They evaluated the items with respect to appropriate wording, grammar, clarity, understandability, and relatedness to Tunisian culture. They were also required to review the items with respect to their relevance.
2.8.3. Construct validity
Confirmatory factor analysis was performed to extract main factors. Independent factors were obtained using principal component analysis (PCA). A factor was considered to be relevant only if its eigenvalue was greater than 1, to indicate that a component explains more variance than any single item. 21 Varimax orthogonal rotation with calculation of the Keizer‐Meyer‐Olkin index (KMO index) was then used to reorganize the representation of items for each selected factor. 22 The Bartlett's test of sphericity served to determine whether there was at least one significant correlation between two of the studied items. 23 Incomplete observations were deleted.
2.8.4. Reliability
The reliability of the questionnaire was assessed, using internal consistency. Cronbach's alpha coefficients, showing how much each of the items in the questionnaire is related to the overall result, indicates acceptable reliability if it is above 0.7. 23
2.9. Data analysis
Data capture and analysis were performed using IBM Statistical Package for the Social Sciences version 10.
Descriptive statistics were reported as frequencies for categorical variables and as means and SDs for quantitative ones. All statistical tests were two‐tailed, and P values <.05 were considered statistically significant.
2.10. Ethics approval and consent to participate
This study was undertaken with respect of the rights and the integrity of people. The study protocol was approved by the Ethical Committee of Farhat Hached University Hospital. Permission from The Regional Health Direction was obtained. Verbal informed consents were obtained beforehand from all participants after providing explanations by the investigators about the aim of the study and confidentiality of the collected data. Participation was voluntary and the participants did not receive any payment. Data were anonymized for this study.
3. RESULTS
3.1. Characteristics of the study sample
A total of 365 adults fulfilled the inclusion criteria. Of these patients, 14 were lost to follow‐up and five did not gave consent to participate to the current study.
The median age of participants was 40 years (interquartile range, 30‐54.5 years), with extremes ranging from 18 to 90 years. Among participants, 60.4% were female and 81.3% had secondary or university educational level. Healthcare providers accounted for 44 (12.7%) of participants. Home quarantine with family members was reported by 250 (78.4%) participants. Contamination of other people at home and at work was reported by 100 (29.1%) and 14 (4.1%) participants, respectively. Because of COVID‐19 illness, 7 (2%) lost their job and 59 (17.1%) reported financial deterioration.
3.2. Measurement of COVID‐19‐related stigma
Descriptive statistics for the scale are presented in Table 1. Missing data were mainly in “concerns about public attitudes” and “personalized stigma” dimensions.
TABLE 1.
Descriptive statistics for items and dimensions in the translated and modified version of the 12‐item short version of the HIV stigma scale
| Items | n | Mean item score a (SD) | Mean subscale score (SD) | Reliability for original items | Reliability with additional items b |
|---|---|---|---|---|---|
| Personalized stigma | 5.64 (1.43) | 0.82 | — | ||
| P1. Some people avoid dealing with me despite my respect of social distancing and wearing mask | 332 | 2.21 (0.73) | |||
| P2. People I care about stopped calling after learning I have COVID‐19 | 336 | 1.75 (0.56) | |||
| P3. I have friends that stopped talking to me after telling them I have COVID‐19 | 336 | 1.70 (0.52) | |||
| Disclosure concerns | 6.86 (2.38) | 0.98 | — | ||
| D1. Telling someone I have COVID‐19 is risky | 344 | 2.29 (0.81) | |||
| D2. I work hard to keep my COVID‐19 a secret | 345 | 2.28 (0.82) | |||
| D3. I did not tell anyone that I have COVID‐19 except my close entourage | 345 | 2.32 (0.82) | |||
| Concerns about public attitudes | 15.95 (4.05) | 0.91 | 0.93 | ||
| C1. People with COVID‐19 are treated like outcasts | 338 | 2.12 (0.71) | |||
| C2. Most people believe a person who has COVID‐19 is dirty | 337 | 2.05 (0.69) | |||
| C3. Most people are uncomfortable around someone with COVID‐19 | 334 | 2.23 (0.72) | |||
| C4. People do not want to use the objects you touch b | 331 | 2.22 (0.72) | |||
| C5. People made you feel that being ill was your mistake b | 337 | 1.84 (0.63) | |||
| C6. People treat you with contempt b | 336 | 1.72 (0.58) | |||
| C7. People told you humiliating comments b | 336 | 1.70 (0.59) | |||
| C8. People avoid dealing with your family members b | 332 | 2.10 (0.69) | |||
| Negative self‐image | 10.71 (2.16) | 0.56 | 0.62 | ||
| N1. I feel guilty because I have COVID‐19 | 345 | 2.01 (0.64) | |||
| N2. People's attitudes about COVID‐19 make me feel worse about myself | 339 | 1.55 (0.51) | |||
| N3. I feel I'm not as good a person as others because I have COVID‐19 | 343 | 1.54 (0.49) | |||
| N4. When you got sick, you felt dirty b | 345 | 1.53 (0.51) | |||
| N5. If anyone from your entourage gets sick, you will feel guilty b | 345 | 2.54 (0.88) | |||
| N6. You feel ashamed because you got sick b | 345 | 1.56 (0.51) |
Possible score for each item 1–4; higher scores reflect a higher level of perceived COVID‐19‐related stigma.
Additional item.
Highest scores were recorded on the questions “I did not tell anyone that I have COVID‐19 except my close entourage” (2.32 ± 0.82) and “Telling someone I have COVID‐19 is risky” (2.29 ± 0.81). We found mean scores of 15.9/32 (±4), 10.7/24 (±2.2), 6.9/12 ± 2.38, and 5.7/12 (±1.4) for concern about public attitudes, negative self‐image, disclosure concerns, and personalized stigma, respectively (Table 1).
3.3. Statistical validation of the questionnaire
3.3.1. Internal consistency
The global reliability for the 20 items scale was at 0.93. Cronbach's alpha was between 0.56 and 0.98 for the questionnaire's dimensions, and the highest reliability was related to disclosure concerns. The reliability of each dimension with original and additional items is displayed in Table 1.
3.3.2. Content Validity
Based on the participants' comments and considering the experts' opinion, items P1, P3, and D3 were modified. Accordingly, “touching me,” “lost friends,” and “very careful who I tell” were changed into “dealing with me despite my respect of social distancing and wearing mask,” “friends stopped talking to me,” and “I did not tell anyone except my close entourage,” respectively.
3.3.3. Construct validity
Table 2 represents the results of the confirmatory factor analysis for the 20‐item stigma scale construct. Three factors explaining 74.7% of the total variance were identified. The eigenvalues of factors 1, 2, and 3 were 8.9, 4.4, and 1.6, respectively. The KMO value of the rotated solution was 0.880. Bartlett's test of sphericity was significant (χ2 [91] = 5764.058, P < .001), which shows a good fit of the data. The rotation converged in five iterations. A closer examination of the scree plot shows that there are only three components that have an eigenvalue greater than 1 and it is depicted by the intersection of the dotted line with the plot line in Figure 1. This is another evidence for a three factor model of the scale.
TABLE 2.
Principal factor analysis with Varimax rotation for the translated and modified version of the 12‐item short version of the HIV stigma scale (n = 332)
| Factors | |||
|---|---|---|---|
| 1 | 2 | 3 | |
| Eigen values | 8.91 | 4.41 | 1.61 |
| Variance explained (%) | 45.6 | 71.2 | 82.8 |
| Items | |||
| C4. People do not want to use the objects you touch | 0.908 | 0.072 | 0.192 |
| C3. Most people are uncomfortable around someone with COVID‐19 | 0.907 | 0.071 | 0.194 |
| P1. Some people avoid dealing with me despite my respect of social distancing and wearing mask | 0.898 | 0.088 | 0.168 |
| C1. People with COVID‐19 are treated like outcasts | 0.768 | 0.101 | 0.375 |
| C2. Most people believe a person who has COVID‐19 is dirty | 0.735 | 0.171 | 0.406 |
| C5. People made you feel that being ill was your mistake a | 0.676 | 0.408 | 0.172 |
| C8. People avoid dealing with your family members a | 0.649 | 0.050 | 0.380 |
| C6. People treat you with contempt a | 0.636 | 0.603 | 0.078 |
| C7. People told you humiliating comments a | 0.592 | 0.592 | 0.067 |
| N4. When you got sick, you felt dirty a | 0.041 | 0.921 | −0.116 |
| N6. You feel ashamed because you got sick a | 0.039 | 0.890 | −0.044 |
| N3. I feel I'm not as good a person as others because I have COVID‐19 | 0.058 | 0.881 | −0.035 |
| N2. People's attitudes about COVID‐19 make me feel worse about myself. | 0.224 | 0.853 | −0.048 |
| P3. I have friends that stopped talking to me after telling them I have COVID‐19 | 0.531 | 0.625 | 0.157 |
| P2. People I care about stopped calling after learning I have COVID‐19 | 0.581 | 0.615 | 0.196 |
| D1. Telling someone I have COVID‐19 is risky | 0.193 | −0.044 | 0.935 |
| D2. I work hard to keep my COVID‐19 a secret | 0.201 | −0.038 | 0.932 |
| D3. I did not tell anyone that I have COVID‐19 except my close entourage | 0.214 | −0.044 | 0.921 |
| N5. If anyone from your entourage gets sick, you will feel guilty a | 0.290 | −0.378 | 0.518 |
| N1. I feel guilty because I have COVID‐19 | 0.259 | 0.142 | 0.464 |
Additional item.
FIGURE 1.
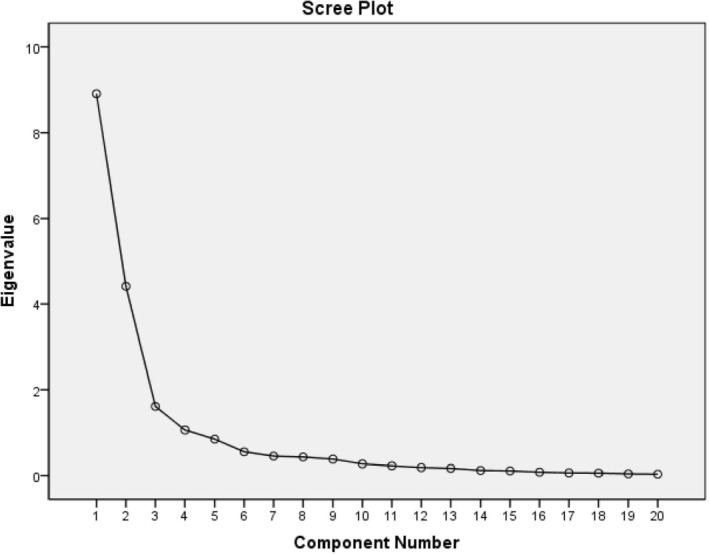
Scree plot of the modified 12‐item version of the HIV stigma scale
The first factor involved as a combination of the original dimension “concerns about public attitudes” (C1, C2, and C3), the first item of the original dimension “personalized stigma” (P1) and three new items (C4, C5, and C8). This factor was renamed as “Social stigma.” The second factor resulted from two items from the original “negative self‐image” dimension (N2 and N3) and two other new items (N4 and N6). This factor was not renamed. The third factor matched the entire original “disclosure concerns” dimension (D1, D2, and D3).
Four items loaded equally on factor one and two (P2, P3, C6, and C7). Two others (N1 and N5) saturated on components one and three (Table 3). These six items were therefore removed: Two items from the original dimension “personalised stigma” (P2 and P3), one from the original dimension “negative self‐image” (N1) and three from the eight added items (two were added to the “concerns about public attitudes” dimension [C6 and C7] and one was added to the “negative self‐image” dimension [N5]).
TABLE 3.
Results of principal factor analysis for 14‐item COVID‐19 stigma scale (n = 335)
| Factors | Reliability | |||
|---|---|---|---|---|
| Social stigma | Negative self‐image | Disclosure concerns | 0.91 | |
| Items | ||||
| Social stigma | 0.94 | |||
| C4. People do not want to use the objects you touch a | 0.942 | 0.078 | 0.126 | |
| C3. Most people are uncomfortable around someone with COVID‐19 | 0.941 | 0.075 | 0.128 | |
| P1. Some people avoid dealing with me despite my respect of social distancing and wearing mask | 0.929 | 0.093 | 0.109 | |
| C1. People with COVID‐19 are treated like outcasts | 0.807 | 0.081 | 0.301 | |
| C2. Most people believe a person who has COVID‐19 is dirty | 0.781 | 0.132 | 0.327 | |
| C5. People made you feel that being ill was your mistake a | 0.672 | 0.038 | 0.342 | |
| C8. People avoid dealing with your family members a | 0.662 | 0.335 | 0.135 | |
| Negative self‐image | 0.93 | |||
| N4. When you got sick, you felt dirty a | 0.067 | 0.952 | −0.103 | |
| N6. You feel ashamed because you got sick a | 0.075 | 0.928 | −0.047 | |
| N3. I feel I'm not as good a person as others because I have COVID‐19 | 0.092 | 0.915 | −0.022 | |
| N2. People's attitudes about COVID‐19 make me feel worse about myself | 0.233 | 0.852 | −0.022 | |
| Disclosure concerns | 0.98 | |||
| D1. Telling someone I have COVID‐19 is risky | 0.255 | −0.070 | 0.939 | |
| D2. I work hard to keep my COVID‐19 a secret | 0.263 | −0.065 | 0.938 | |
| D3. I did not tell anyone that I have COVID‐19 except my close entourage | 0.271 | −0.077 | 0.928 | |
Additional item.
As shown in Table 3, final factor analysis of the remaining 14 items revealed better construct validity than the 20‐item scale. The three factors explained 76% of the total variance. Internal consistency was also high for total score (0.91) and three subscales (Table 3). The 14‐item Arabic version is illustrated in the additional file (Appendix 1).
4. DISCUSSION
Regarding the lack of Tunisian Arabic tool to measure COVID‐19‐related stigma among the general population, we aimed to translate, adapt, and test the HIV‐stigma scale on adults with COVID‐19 infection after quarantine, recruited from the general population in Tunisia. After principal component analysis, the study resulted in a 14‐item stigma scale measuring social stigma, negative self‐image, and disclosure concerns. The scale appeared feasible, reliable for the three subscales, and had good construct validity.
The median age of participants in the current study was 40 years with 61.4% aged between 31 and 64 years. Similar young age range was reported by a national study about the characteristics of COVID‐19 patients and the prognosis of the infection in the Tunisian general population. 24 In the literature, similar results were reported in several case series. 9 , 16 , 17 The proportion of healthcare professionals of 14.8% among participants was also similar to that in the Tunisian national survey. 24
Otherwise, 60.4% of participants were female. In line with our results, several studies reported female predominance among the declared COVID‐19 patients. 9 , 16 Most of cases did not require treatment in a hospital structure and were self‐isolated at home with family members (78.4%). In fact, regarding the lack of confinement centers in Tunisia, home quarantine was the only solution to isolate COVID‐19 patients. 24
Highest scores were recorded on the following questions: “I am very careful about who I tell that I have COVID‐19” and “Telling someone I have COVID‐19 is risky”. These results join those in Pakistan 16 and India 10 showing significantly higher levels of public attitude and disclosure concerns domains. Only a few number of studies was found about COVID‐19 stigma in the general population using nonspecific or nonvalidated tools. 10
The overall reliability for the 14‐item Tunisian scale was at 0.91, suggesting an excellent internal consistency. Similarly, the English version of the stigma scale, originally developed to measure HIV‐related stigma, then adapted to measure post‐SARS stigmatization among 500 Egyptian health care workers had a Cronbach's alpha of 0.91. 9 In line with these results, the reliability of the Ebola‐related stigma questionnaire adapted for COVID‐19 survivors experiencing stigma after their discharge from the hospital in India was at 0.92. 17 The current study revealed Cronbach's alpha coefficients between 0.93 and 0.98 for final questionnaire's dimensions, and the highest reliability was related to disclosure concerns. Consistent with these results, the adapted 12‐item HIV stigma scale showed adequate reliability for the four dimensions (ranged from 0.73 to 0.87) among patients in Pakistan 16 and healthcare workers after quarantine in Vietnam. 25
In view of the emergence of new SARS‐Cov‐2 variants of concerns responsible for reinfection, 26 , 27 higher exposure to stigma is expected. The proposed COVID‐19 stigma tool should be used to early detect this issue among Tunisian COVID‐19 patients and guide its prevention. Further studies are recommended to measure the magnitude and the risk factors of COVID‐19 stigma in Tunisian people. Qualitative studies would allow deeper understanding of this issue. Adequate information of people about this new disease, the ways of its dissemination and avoidance would reduce stigma and emotional disorders among Tunisian people during the current pandemic. Other validation studies are recommended to provide reliable and accurate tools to measure other pandemic‐related mental health issues.
Results of the current research should be viewed in the light of some limitations. First, the predominance of females and participants self‐isolated at home may have interfered with the measure of stigma dimensions and caused selection bias. Nonetheless, a daily random sampling was performed using updated lists of the new declared cases in Sousse. Indeed, this predominance of females and home quarantined patients was observed at the national level. 24 Further investigation on larger samples and different populations is required to confirm our stigma‐related results. Future research should also evaluate if individuals confined in hospital or in a confinement center may experience different levels of COVID‐19 stigma. Second, nonresponse to some items related to the public attitudes dimension may have influenced the psychometric analysis. Disclosure concerns and imposed social distancing could explain nonapplicability of these items. Even so, the response rate for these items was acceptable (at least 95.6% for item S4). Finally, the scarcity of studies focusing on validating Arabic COVID‐19 stigma scale among the general population with similar studied dimensions did not allow comparison of the current findings. 7 , 8
5. CONCLUSION
This study provides the first short format tool for stigma screening among COVID‐19 Tunisian patients with good convergent construct validity and high reliability. The use of this scale would contribute in reducing the spread of this new infectious disease in Tunisia and guide the prevention of COVID‐19‐related mental health issues.
FUNDING
No funding was received for conducting this study.
CONFLICT OF INTEREST
The authors report no actual or potential conflicts of interest. All authors certify responsibility for the manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
AUTHOR CONTRIBUTIONS
Conceptualization: Nawel Zammit, Jihene Maatoug and Hssan Ghannem.
Formal Analysis: Imen Mlouki, Rania Bannour, Ansar Elechi, Rim Ghammam, Sihem Ben Fredj, Hafsia Ladhari, Adel Haddedi, and Mohamed Mizouni Ghodhbani.
Writing—original draft: Imen Mlouki, Nawel Zammit and Jihene Maatoug.
Writing—review and editing: Hssan Ghannem, Rania Bannour, Ansar Elechi, Rim Ghammam, Sihem Ben Fredj, Hafsia Ladhari and Mohamed Mizouni Ghodhbani.
All authors read and approved the final manuscript.
Imen Mlouki had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
Imen Mlouki affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; and that no important aspects of the study have been omitted.
Supporting information
Appendix 1: Supporting Information.
ACKNOWLEDGMENT
We would like to thank all the team members of the Regional Direction of Health in the region of Sousse. All authors declare that the current work submitted to Health Science Reports has been done in accordance to these guidelines and that is has been performed in an ethical and responsible way, with no research misconduct, which includes, but is not limited to data fabrication and falsification, plagiarism, image manipulation, unethical research, biased reporting, authorship abuse, redundant or duplicate publication, and undeclared conflicts of interest.
Mlouki I, Zammit N, Ghammem R, et al. Validity and reliability of a modified short version of a stigma scale for use among Tunisian COVID‐19 patients after quarantine: A cross‐sectional study. Health Sci Rep. 2022;5:e520. doi: 10.1002/hsr2.520
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.A guide to preventing and addressing social stigma associated with COVID‐19 [Internet]. 2021. https://www.who.int/publications/m/item/a-guide-to-preventing-and-addressing-social-stigma-associated-with-covid-19. Accessed September 20, 2021.
- 2. Muhidin S, Vizheh M, Moghadam ZB. Anticipating COVID‐19‐related stigma in survivors and health‐care workers: lessons from previous infectious diseases outbreaks—an integrative literature review. Psychiatry Clin Neurosci. 2020;74(11):617‐618. [DOI] [PubMed] [Google Scholar]
- 3. Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID‐19 pandemic. Front Public Health. 2020;8:577018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kang E, Lee SY, Kim MS, et al. The psychological burden of COVID‐19 stigma: evaluation of the mental health of isolated mild condition COVID‐19 patients. J Korean Med Sci. 2021;36(3):e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bologna L, Stamidis KV, Paige S, et al. Why communities should be the focus to reduce stigma attached to COVID‐19. Am J Trop Med Hyg. 2021;104(1):39‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yuan K, Huang X‐L, Yan W, et al. A systematic review and meta‐analysis on the prevalence of stigma in infectious diseases, including COVID‐19: a call to action. Mol Psychiatry. 2021;1–15. https://www.nature.com/articles/s41380-021-01295-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haddad C, Bou Malhab S, Malaeb D, et al. Stigma toward people with COVID‐19 among the Lebanese population: a cross‐sectional study of correlates and mediating effects. BMC Psychol. 2021;9(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Abuhammad S, Alzoubi KH, Khabour O. Fear of COVID‐19 and stigmatization towards infected people among Jordanian people. Int J Clin Pract. 2021;75(4):e13899. doi: 10.1111/ijcp.13899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mostafa A, Sabry W, Mostafa NS. COVID‐19‐related stigmatization among a sample of Egyptian healthcare workers. PloS One. 2020;15(12):e0244172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moideen S, Uvais NA, Rajagopal S, Maheshwari V, Gafoor TA, Sherief SH. COVID‐19‐related stigma among inpatients with COVID‐19 infection: a cross‐sectional study from India. Prim Care Companion CNS Disord. 2021;23(1):20br02853. https://www.psychiatrist.com/pcc/covid-19/stigma-among-inpatients-with-covid-19/ [DOI] [PubMed] [Google Scholar]
- 11. Nashwan AJ, Al‐Fayyadh S, AL‐Hadrawi H, et al. Development and initial validation of stigma towards healthcare providers working with COVID‐19 patients scale (S19‐HCPs). J Multidiscip Healthc. 2021;14:3125‐3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ben Hassen H, Elaoud A, Ben Salah N, Masmoudi A. A SIR‐Poisson model for COVID‐19: evolution and transmission inference in the Maghreb central regions. Arab J Sci Eng. 2020;23:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Letaief H, Dhaouadi S, Hechaichi A, et al. Evaluation of a COVID‐19 IgM and IgG rapid test and assessment of specific antibody response in COVID‐19 patients, Tunisia 2020 [internet]. In Rev. 2021. https://www.researchsquare.com/article/rs-237568/v1 [Google Scholar]
- 14. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518‐529. [DOI] [PubMed] [Google Scholar]
- 15. Reinius M, Wettergren L, Wiklander M, Svedhem V, Ekström AM, Eriksson LE. Development of a 12‐item short version of the HIV stigma scale. Health Qual Life Outcomes. 2017;15(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Imran N, Afzal H, Aamer I, et al. Scarlett letter: a study based on experience of stigma by COVID‐19 patients in quarantine. Pak J Med Sci. 2020;36(7):1471‐1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dar SA, Khurshid SQ, Wani ZA, et al. Stigma in coronavirus disease‐19 survivors in Kashmir, India: a cross‐sectional exploratory study. PloS One. 2020;15(11):e0240152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guillemin F, Bombardier C, Beaton D. Cross‐cultural adaptation of health‐related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417‐1432. [DOI] [PubMed] [Google Scholar]
- 19. Tavormina MGM, Tavormina R, Nemoianni E, Tavormina G. A questionnaire to assess social stigma. Psychiatr Danub. 2015;27(Suppl 1):S328‐S331. [PubMed] [Google Scholar]
- 20. Park J‐S, Lee E‐H, Park N‐R, Choi YH. Mental health of nurses working at a government‐designated hospital during a MERS‐CoV outbreak: a cross‐sectional study. Arch Psychiatr Nurs. 2018;32(1):2‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Klin P. An Easy Guide to Factor Analysis. London: Routledge; 1994. [Google Scholar]
- 22. Bourque J, Poulin N, Cleaver A. Évaluation de l'utilisation et de la présentation des résultats d'analyses factorielles et d'analyses en composantes principales en éducation. Rev Sci Léducation. 2006;32(2):325‐344. [Google Scholar]
- 23. Using Multivariate Statistics [Internet], 6th ed. California State University ‐ Northridge: Barbara G. Tabachnick, Linda S. Fidell; 2021. https://content/one-dot-com/one-dot-com/us/en/higher-education/program.html [Google Scholar]
- 24. Harizi C, Cherif I, Najar N, et al. Characteristics and prognostic factors of COVID‐19 among infected cases: a nationwide Tunisian analysis. BMC Infect Dis. 2021;21(1):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Duy CD, Nong VM, Van AN, Thu TD, Thu ND, Quang TN. COVID‐19‐related stigma and its association with mental health of health‐care workers after quarantine in Vietnam. Psychiatry Clin Neurosci. 2020;74(10):566‐568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SeyedAlinaghi S, Afsahi AM, MohsseniPour M, et al. Late complications of COVID‐19; a systematic review of current evidence. Arch Acad Emerg Med. 2021;9(1):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. SeyedAlinaghi S, Mirzapour P, Dadras O, et al. Characterization of SARS‐CoV‐2 different variants and related morbidity and mortality: a systematic review. Eur J Med Res. 2021;26(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Supporting Information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


