OBJECTIVES:
The coronavirus disease 2019 pandemic has disrupted critical care services across the world. In anticipation of surges in the need for critical care services, governments implemented “lockdown” measures to preserve and create added critical care capacity. Herein, we describe the impact of lockdown measures on the utilization of critical care services and patient outcomes compared with nonlockdown epochs in a large integrated health region.
DESIGN:
This was a population-based retrospective cohort study.
SETTING:
Seventeen adult ICUs across 14 acute care hospitals in Alberta, Canada.
PATIENTS:
All adult (age ≥ 15 yr) patients admitted to any study ICU.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
The main exposure was ICU admission during “lockdown” occurring between March 16, 2020, and June 30, 2020. This period was compared with two nonpandemic control periods: “year prior” (March 16, 2019, to June 30, 2019) and “pre lockdown” immediately prior (November 30, 2019, to March 15, 2020). The primary outcome was the number of ICU admissions. Secondary outcomes included the following: daily measures of ICU utilization, ICU duration of stay, avoidable delay in ICU discharge, and occupancy; and patient outcomes. Mixed multilevel negative binomial regression and interrupted time series regression were used to compare rates of ICU admissions between periods. Multivariable regressions were used to compare patient outcomes between periods. During the lockdown, there were 3,649 ICU admissions (34.1 [8.0] ICU admissions/d), compared with 4,125 (38.6 [9.3]) during the prelockdown period and 3,919 (36.6 [8.7]) during the year prior. Mean bed occupancy declined significantly during the lockdown compared with the nonpandemic periods (78.7%, 95.9%, and 96.4%; p < 0.001). Avoidable ICU discharge delay also decreased significantly (42.0%, 53.2%, and 58.3%; p < 0.001). During the lockdown, patients were younger, had fewer comorbid diseases, had higher acuity, and were more likely to be medical admissions compared with the nonpandemic periods. Adjusted ICU and hospital mortality and ICU and hospital lengths of stay were significantly lower during the lockdown compared with nonpandemic periods.
CONCLUSIONS:
The coronavirus disease 2019 lockdown resulted in substantial changes to ICU utilization, including a reduction in admissions, occupancy, patient lengths of stay, and mortality.
Keywords: critical care, efficiency, health services, length of stay, mortality, pandemics
The coronavirus disease 2019 (COVID-19) pandemic has contributed to substantial disruptions in healthcare services delivery around the world. In selected jurisdictions, the rapid rise in patients with COVID-19 requiring hospitalization quickly overwhelmed acute care health systems, including critical care services, as seen in New York, northern Italy, and the United Kingdom (1).
The government of Alberta declared a public health emergency in response to the COVID-19 pandemic on March 15, 2020 (total cases in Alberta, Canada, at this time: 97). This triggered the broad implementation of priority public health measures (i.e., physical distancing, contact tracing, increased COVID-19 testing, closure of public institutions [universities, schools, recreational facilities, etc.], restricted public transportation) along with pandemic preparation of the health system (i.e., expanding hospital and ICU capacity, altered staffing models). This was done in anticipation of a substantial surge in COVID-19 cases that would threaten to rapidly exceed existing health system capacity (2).
ICUs in many jurisdictions normally operate at near full capacity and often under strained conditions, with marginal day-to-day flexibility in bed availability to accommodate surges in patients who need ICU support (3). In recognition of this and in anticipation of the potential surge in ICU admissions in the context of the COVID-19 pandemic—concomitant with public health interventions (i.e., lockdown)—scheduled health services were strategically reduced to generate ICU capacity. These health system measures included postponement of nonessential services and scheduled surgeries to rapidly generate ICU and hospital bed capacity. These measures were undertaken and prepared our health system, including ICU capacity, for an anticipated peak surge in hospitalizations to occur in early May 2020; however, this surge in COVID-19–related hospitalizations during the first wave was far smaller than expected (4).
We hypothesized that the COVID-19 lockdown (i.e., reduction in scheduled surgery and other public health measures) translated into large reductions in ICU admissions and ICU utilization, despite no concomitant policy change in ICU admission criteria. Accordingly, we performed a retrospective cohort study to describe the changes in ICU capacity and utilization during the first wave of the COVID-19 pandemic lockdown compared with historical nonpandemic epochs. We further sought to describe the characteristics, course, and outcomes of critically ill patients admitted during this lockdown compared with admissions during historical nonpandemic epochs.
MATERIALS AND METHODS
This study was approved by the Research Ethics Board at the University of Alberta, Edmonton, AB, Canada (File number Pro00101420; July 21, 2020). The need for written informed consent was waived.
Design, Setting, Population
This study was a population-based retrospective cohort study. The study involved all adult (age ≥ 15 yr) patients admitted to any of the 17 adult ICUs across 14 acute care hospitals in Alberta (5) (Supplementary Table 1, http://links.lww.com/CCM/G772). In Alberta (2021 population ~4.43 million [6]), acute care health services are predominantly administered by a single provincial provider, Alberta Health Services (7). Alberta has an estimated baseline-funded ICU bed-base of approximately 9.7 ICU beds per 100,000 population (compared with 13.5 ICU beds per 100,000 population nationwide in Canada and 20 ICU beds per 100,000 population in the United States) (8–10). ICUs generally operate with a “closed” model and are staffed by certified intensivists who are present and available during daytime hours and available afterhours on-call. All 17 adult ICUs in Alberta were able to admit and provide advanced multimodal monitoring and organ support (e.g., mechanical ventilation, vasoactive support) and recommended infection prevention and control standards (i.e., isolation) for patients with suspected or confirmed severe acute respiratory syndrome (SARS) coronavirus 2 infection. Interhospital ICU transfers may occur between sites in response to strained ICU capacity (i.e., no bed available) or to facilitate regional referral for specialized services (i.e., extracorporeal life support) (11).
Primary Exposure
The main exposure was ICU admission during the period of “lockdown” occurring between March 16, 2020 (start of the COVID-19 lockdown in Alberta), and June 30, 2020 (COVID-19 lockdown).
Control Periods
We identified two nonlockdown periods for controls: 1) “year prior”—the same time period (107 d) 1 year prior (March 16, 2019, to June 30, 2019) and 2) “pre lockdown”—the same duration of time (107 d) immediately prior to the COVID-19 lockdown (November 30, 2019, to March 15, 2020).
Outcomes
The primary outcome was the rate (number) of ICU admissions during the COVID-19 lockdown compared with nonlockdown control periods. The secondary outcomes included the following: 1) daily measures of ICU utilization, including patient arrival rate, ICU duration of stay, numbers of patients with and duration of avoidable delay in ICU discharge (avoidable time), and occupancy; 2) description of differences in patient case mix, acuity, and support intensity; and 3) description of patient outcomes, including ICU and hospital mortality, and hospital lengths of stay (LOS).
Data Sources
Data were sourced from an ICU-specific clinical information system/data repository (eCritical/TRACER) and Alberta administrative health datasets, including the Discharge Abstract Database metadata (12, 13). “eCritical” is composed of a bedside system (eCritical MetaVision; iMDsoft, Dusseldorf, Germany), which provides for full electronic interdisciplinary clinical documentation and collation of demographic, diagnostic/case mix, acuity (Acute Physiology and Chronic Health Evaluation [APACHE] II score), laboratory, and device data. “eCritical TRACER” provides a comprehensive, multimodal, and integrated data repository of patient-specific ICU data, enabling creation of reports and specific data extracts for administrative, quality, and research purposes. Data within “eCritical” systems undergo rigorous data quality assurance and audit (14). “eCritical TRACER” has routinely been used to support health services research (15–18). The Discharge Abstract Database provides rich data elements on all hospitalizations in Alberta. It contains patient demographics, diagnoses, discharge disposition, case mix classification (i.e., identifying homogenous patient clusters), and resource intensity weight (indicating the level of a patient’s resource consumption during a hospital stay) (19).
Statistical Analysis
Data were initially explored descriptively. Normally or near normally distributed data are reported as means with sds and compared by Student t test. Nonnormally distributed continuous data are reported as medians with interquartile ranges and were compared by Mann-Whitney U test. Categorical variables were compared using the chi-square test. We used mixed multilevel negative binomial regression to compare the number of ICU admissions and LOS between the COVID-19 lockdown and control periods. We further used interrupted time series and multivariate negative binomial regressions to show temporal trends in ICU admissions related to the COVID-19 lockdown compared with nonlockdown control periods. We used multivariable Cox regressions to compare mortality between COVID-19 lockdown and nonlockdown control periods, respectively.
RESULTS
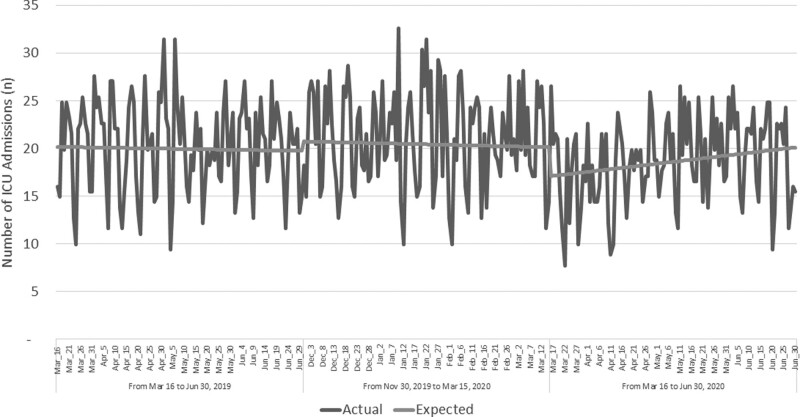
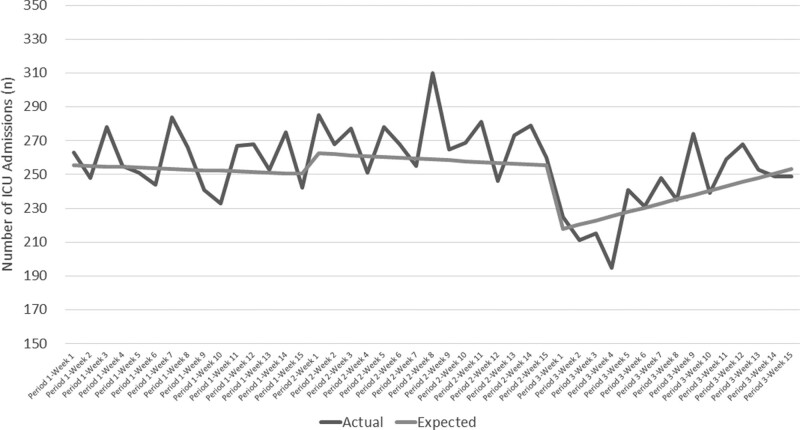
There were 3,649 ICU admissions during the lockdown (34.1 [8.0] ICU admissions/d), compared with 4,125 (38.6 [9.3] ICU admission per day) during the prelockdown and 3,919 (36.6 [8.7] ICU admissions per day) during the year prior, respectively (Fig. 1). During the lockdown, there were only a total of 381 patients hospitalized and 88 admitted to ICU cumulatively with a diagnosis of COVID-19 (median age 61 yr; women 39%; median APACHE II score 19) (data not shown). There was a significant decline in the numbers of daily ICU admissions occurring during the lockdown compared with the nonlockdown periods (Table 1 and Fig. 2).
Figure 1.
Number of ICU admissions per day per 100 funded beds by the three periods: lockdown, pre lockdown, and the year before.
Table 1.
Association Between the Lockdown and ICU Admissions During the Lockdown Compared With Nonlockdown Periods
| Relative Difference in Number of ICU Admission Per Day Between Periods | Incidence Rate Ratioa | p | 95% CI | |
|---|---|---|---|---|
| Low | High | |||
| Lockdown vs pre lockdown | 0.904 | 0.001 | 0.853 | 0.957 |
| Lockdown vs year prior | 0.926 | 0.070 | 0.852 | 1.006 |
| Difference in Number of ICU Admissions Per Day Between Periods | Coefficient b | p | 95% CI | |
| Low | High | |||
| Lockdown vs pre lockdown | –3.9 | 0.045 | –7.6 | –0.1 |
| Lockdown vs year prior | –2.6 | 0.224 | –6.8 | 1.6 |
aFull multilevel multivariate negative binomial regressions will be provided upon request.
bFull Interrupted Time Series Analysis models will be provided upon request.
Figure 2.
Number of ICU admissions per week by the three periods: lockdown, pre lockdown, and the year before.
Average bed occupancy decreased significantly during the lockdown compared with the nonlockdown periods (Table 2) (Supplementary Table 2, http://links.lww.com/CCM/G773). The proportion of patients with avoidable ICU discharge delay and the average avoidable time experienced by patients was significantly lower during the lockdown compared with the nonlockdown periods (Supplementary Table 3, http://links.lww.com/CCM/G774; and Supplementary Table 4, http://links.lww.com/CCM/G775).
Table 2.
Patient Characteristics, Organ Support, and Outcomes
| Characteristics | Year Prior | Pre Lockdown | Lockdown |
|---|---|---|---|
| From March 16, 2019, to June 30, 2019 (the Same Time as Lockdown Period But in 2019) | From November 30, 2019, to March 15, 2020 (107 d Right Before the Lockdown) | From March 16, 2020, to June 30, 2020 (107 d of Lockdown) | |
| n | 3,919 | 4,125 | 3,649 |
| Age, mean (sd) | 59.2 (16.5) | 58.3 (16.6) | 56.8 (16.6) |
| Male sex (%) | 61.4 | 61.2 | 64.7 |
| ICU type (%) | |||
| Adult cardiovascular surgical ICU | 23.6 | 23.9 | 21.7 |
| Adult ICU | 76.4 | 76.1 | 78.3 |
| Patient types (%) | |||
| Elective surgery | 24.8 | 19.8 | 16.8 |
| Emergency surgery | 14.3 | 11.9 | 13.0 |
| Medical (nonoperative) | 56.2 | 50.9 | 50.8 |
| Others | 4.7 | 17.4 | 19.4 |
| Comorbidities (%) | 45.8 | 39.8 | 36.4 |
| Dialysis | 2.8 | 2.4 | 2.4 |
| Congestive heart failure | 9.8 | 8.4 | 7.4 |
| Respiratory insufficiency | 10.9 | 10.7 | 8.6 |
| Immune suppression | 7.0 | 6.4 | 5.0 |
| Cirrhosis | 4.4 | 3.7 | 4.7 |
| Hepatic failure | 2.2 | 1.7 | 2.5 |
| AIDS | 0.4 | 0.2 | 0.3 |
| Metastatic cancer | 2.8 | 2.4 | 2.1 |
| Leukemia/lymphoma | 1.7 | 1.3 | 1.2 |
| Diabetes | 23.2 | 19.9 | 18.7 |
| Organ support | |||
| APACHE II, mean (sd) | 19.3 (8.5) | 19.6 (8.8) | 19.8 (9.0) |
| APACHE III, mean (sd) | 65.8 (30.7) | 66.6 (32.4) | 67.9 (32.7) |
| Mechanical ventilation (%) | 73.4 | 74.0 | 71.0 |
| Vasoactive support (%) | 57.2 | 57.2 | 56.2 |
| Renal replacement therapy (%) | 7.9 | 8.1 | 8.5 |
| ICU operations | |||
| Occupancy (%), mean (sd) | 96.4 (25.2) | 95.9 (24.5) | 78.7 (24.9) |
| Avoidable time (%)a | 58.3 | 53.2 | 42.0 |
| Avoidable time (hr), mean (sd) | 15.7 (30.9) | 21.3 (52.3) | 11.8 (86.1) |
| Avoidable time (hr), median (IQR) | 2.4 (0.0–21.5) | 2.8 (0.0–24.5) | 0.4 (0.0–5.0) |
| Total avoidable time (d) | 2,570 | 3,666 | 1,797 |
| Outcomes | |||
| Lengths of stay, median (IQR) | |||
| ICU | 2.9 (1.4–6.0) | 3.0 (1.3–5.9) | 2.5 (1.1–4.9) |
| Hospital | 10.0 (5.0–20.0) | 8.8 (5.0–17.0) | 8.0 (4.0–16.0) |
| ICU mortality (%) | 11.3 | 11.1 | 11.2 |
| Hospital mortality (%) | 16.1 | 15.2 | 15.1 |
APACHE = Acute Physiology and Chronic Health Evaluation, IQR = interquartile range.
aAvoidable time is defined as the proportion of total ICU patient-hours accounted for by avoidable ICU discharge delay. Avoidable discharge delay is defined as the time difference between the date/time of decision for transfer and when the patient was actually discharged from the ICU, less 4 hr.
During the lockdown, patients admitted to ICU were younger, had fewer comorbid diseases, had a higher acuity, and were more likely to be medical (nonoperative) admissions compared with the nonlockdown periods. There was a reduction in scheduled surgery admissions; however, there was no change in emergency surgery admissions (Table 2). Mortality in ICU and in hospital decreased substantially during the lockdown compared with both nonlockdown periods (Table 3). ICU LOS and hospital LOS were also shorter during the lockdown compared with the nonlockdown periods (Table 3) (Supplementary Table 5, http://links.lww.com/CCM/G776).
Table 3.
Association Between Lockdown and Death and Lengths of Stay
| Mortality | Hazard Ratioa | p | 95% CI | |
|---|---|---|---|---|
| Low | High | |||
| Lockdown vs pre lockdown | ||||
| Death in ICU | 0.663 | < 0.001 | 0.558 | 0.789 |
| Death in hospital | 0.714 | < 0.001 | 0.600 | 0.849 |
| Lockdown vs year prior | ||||
| Death in ICU | 0.720 | < 0.001 | 0.604 | 0.857 |
| Death in hospital | 1.102 | 0.269 | 0.928 | 1.309 |
| Lengths of Stay | Incidence Rate Ratioa | p | 95% CI | |
| Low | High | |||
| Lockdown vs pre lockdown | ||||
| ICU length of stay | 0.881 | < 0.001 | 0.840 | 0.925 |
| Hospital length of stay | 0.933 | 0.012 | 0.884 | 0.985 |
| Lockdown vs year prior | ||||
| ICU length of stay | 0.813 | < 0.001 | 0.772 | 0.856 |
| Hospital length of stay | 0.736 | < 0.001 | 0.694 | 0.779 |
aFull multilevel multivariate Cox regressions for death and negative binomial regressions for length of stay will be provided upon request.
DISCUSSION
We performed a retrospective population-based cohort study to describe the health system and patient-level impact of public health interventions aimed to generate ICU capacity during the first wave of the COVID-19 pandemic lockdown. First, we found that our provincial health system was able to rapidly adapt to prepare for a surge in ICU-related COVID-19 admissions, given suitable lead time, as evidenced by changes in several metrics of ICU capacity and operations. This is relevant when considering that Alberta has a lower number of ICU beds per capita compared with other Canadian provinces; however, it is important to also highlight that this was within the context of a wave 1 surge having a limited impact on provincial hospital and critical care capacity (Supplementary Table 6, http://links.lww.com/CCM/G777). Second, we found the absolute numbers of ICU admissions declined significantly during COVID-19 lockdown. The decline was consistent across all health zones in the province. However, we did observe a positive trend in ICU admissions toward the tail of the lockdown period, which is likely attributed to gradual easing of public health measures and resumption of selected scheduled services. Third, we showed a concomitant large increase in ICU capacity (i.e., drop in average occupancy) and a reduction in avoidable time spent in ICU, which is likely attributed to corresponding reductions in hospital occupancy and the ability to more rapidly transition patients to the ward (i.e., reduced ICU exit block). Fourth, we found patients spent, on average, less time in ICU and in the hospital. Furthermore, we found reductions in both ICU and hospital mortality during the lockdown, despite comparable acuity of illness, compared with nonlockdown epochs. Fifth, we showed that ICU admissions support for scheduled surgery likely represented the most significant change during the COVID-19 lockdown when compared with the two nonpandemic epochs. This correlated with public health interventions aimed to strategically reduce scheduled surgeries across the province. However, we found that the rate of ICU admissions for emergency surgery remained similar during the initial lockdown when compared with the two nonpandemic epochs. Finally, we found differences in patient demographics and case mix, with the patients admitted during the COVID-19 lockdown being younger and having a lower burden of chronic comorbid illness compared with nonlockdown epochs.
Context With Prior Literature
One implication of the dramatic reductions in ICU admissions during the first wave of the COVID-19 pandemic could be that patients with critical illness were not presenting to hospital or undergoing scheduled procedures that would generally necessitate support in ICU settings (i.e., cardiac and other scheduled major surgeries). Although there have been limited data available on the impact of ICU services during the initial phases of the COVID-19 lockdown, our data support this possibility. This trend in reduced ICU utilization was found to occur in both pediatric and adult ICU settings (20, 21). Young et al (21) described significant reductions in daily unplanned ICU admissions during the initial phase of COVID-19 lockdown in a single center adult ICU in a study from New Zealand. Graciano et al (20) described a 48.2% decline in ICU admissions during the initial phase of COVID-19 lockdown compared with the same period in the preceding year, driven predominantly by marked reductions in respiratory illnesses. Similarly trends in hospital presentation for several medical emergencies also declined substantially, including acute stroke (22) and acute myocardial infarction (23), among others (24). On the contrary, rates of out-of-hospital cardiac arrest were found to increase during the early phase of COVID-19 lockdowns and may have represented delay in hospital presentation for COVID-19–related and nonrelated acute conditions (25).
The COVID-19 lockdown was associated with significant reductions in both ICU and hospital mortality for critically ill patients, a finding that persisted in analysis that adjusted for case mix and illness acuity, when compared with the nonlockdown epochs. This may have been attributed to fewer patients with critical illness or changes to clinician decision-making to forego ICU care for selected patients. This could also be plausibly related to reduced patient-to-intensivist ratios during the lockdown, given that no changes to operational or intensivist staffing models were known to have occurred (26). Indeed, this may indirectly support observations of higher mortality risk during periods of strained ICU capacity (16, 27). Recently, Bravata et al (28) found critically ill patients with COVID-19 admitted to strained ICUs, defined by a high burden of COVID-19 activity, had a greater risk of hospital mortality.
Implications for Clinicians and Policy
Guidelines recommended that health systems plan, model, and reorganize their ICU structure and resources (i.e., beds, supplies, human resources) to generate added ICU capacity in readiness for potential surge increases in COVID-19–related critical illness (7). This approach was sensible and widely adopted, given the uncertainty of the potential demand on critical care services for COVID-19–related admissions coupled with the uncertainty of the effectiveness of government-imposed public health measures and the profound impact of COVID-19 surges on healthcare resources observed in other countries. Prior data implied a major limitation on the implementation of surge capacity would be the relative day-to-day strain on the existing hospital and ICU capacity (29). However, during the initial lockdown period across the province, ICU capacity did not require surge beyond “basic presurge” (0% increase from baseline) to “phase 1” (minor surge—34% increase from baseline). Indeed, the occupancy of many ICUs during this time were at unprecedented low levels, implying that admissions to ICU and overall ICU utilization were considerably reduced, despite no systemic or operational change in the criteria for ICU admission or in the availability of critical care services. For example, during the 107-day initial lockdown, cumulatively there were 381 patients with COVID-19 hospitalized and only 88 admitted to any of 17 adult ICUs across Alberta (average and peak percent COVID test positivity was 2.0% and 7.7% in Alberta, similar to other Canadian jurisdictions and lower than many other countries) (Supplementary Table 6, http://links.lww.com/CCM/G777).
There may be important learnings from our early health system response to create surge capacity during the COVID-19 pandemic that may be applicable to other jurisdictions and during future pandemics (30). The measures instituted across the health system were intended to provide surge capacity while mitigating the need for the implementation of pandemic triage protocols (7, 31). However, the ICU capacity generated during the initial COVID-19 lockdown greatly exceeded actual need. It remains uncertain how the health system would have further responded had there been a substantial increase in the demand for critical care services during this period. However, these measures may have had two important implications. First, this may have translated into negative consequences and severe limitations in the public’s access to acute care health services during the initial phases of the COVID-19 pandemic when the incremental demand for critical care services remained minimal. These unintended consequences were shown to occur during the lockdown imposed during the SARS outbreak in 2003 in the Greater Toronto Area (32). Importantly, our study showed that the health system was able to respond to the impending threat by rapidly creating substantial critical care capacity in a relatively short period of time. Although this was not accompanied by a concomitant increased demand for critical care services during wave 1 of the COVID-19 pandemic, this exercise provided important insights and informed how to strategically scale critical capacity in response to pandemic modeling during subsequent waves. Second, this may also represent an opportunity to realize greater health system efficiency and understand where acute care may be better optimized and/or even unnecessary (30, 33). For example, recent data suggest that a marked decline in emergency department visits in a large health region in Germany for cardiovascular-related events during government-imposed lockdown was for “discretionary” admissions, such as dizziness/syncope, heart failure, and chronic obstructive pulmonary disease exacerbations rather than for diagnoses that are associated with unavoidable admissions, such as acute coronary syndrome, stroke, or cardiac arrest, rates of which remained similar (33). This is perhaps analogous to prior nonpandemic work showing a substantial variation in ICU utilization for patients with low or similar risk-adjusted mortality, implying opportunity for improved quality and efficiency (34, 35). In addition, the substantial decline in avoidable time prior to ICU discharge (i.e., reduced ICU exit block) observed during the lockdown epoch can be viewed as better efficiency (i.e., patient flow) and utilization of constrained ICU resources. Implementation of policies to reduce exit block and to facilitate more timely transition of patients to the ward, and strategic expansion of ward-bed capacity could realize considerable improvements in efficiency and cost savings (5).
Although our study provides detailed insight into the critical care response to the initial COVID-19 lockdown, we recognize it has limitations. First, our study was retrospective and does not enable drawing causal conclusions between the COVID-19 lockdown and historical epochs in terms of changes in ICU operations and patient case mix. Second, we did not have concomitant detailed data on hospital occupancy during the study periods. Third, although population based, our study reflects a single large integrated health system and may not be generalizable to other jurisdictions. Finally, we recognize that during wave 1 of the COVID-19 pandemic, jurisdictions likely experienced widely varying case counts, rates of hospitalization, and critical care utilization, driven by a mix of differing approaches to implementation of public health measures and surge capacity planning. As such, comparisons with the health system response in Alberta may not be directly applicable.
CONCLUSIONS
In this retrospective study, we found marked reductions in numbers of ICU admissions and avoidable time among those awaiting ICU discharge during the initial COVID-19 lockdown compared with historical epochs. The reduction was associated with substantial differences in measures of ICU utilization, efficiency, patient case mix, and outcomes.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supported, in part, by Strategic Clinical Networks, Alberta Health Services, Edmonton, AB, Canada.
Dr. Bagshaw received funding from Baxter and CAN Diagnostics. He is supported by a Canada Research Chair in Critical Care Nephrology. Dr. Stelfox is supported by an Alberta Innovates Population Health Investigator Award and Canadian Institutes of Health Research Embedded Clinician Researcher Award. Dr. Opgenorth disclosed that she is employed as Project Manager at University of Alberta. The remaining authors have disclosed that they do not have any potential conflicts of interest.
This work was performed at the University of Alberta, Edmonton, AB, Canada.
REFERENCES
- 1.Uppal A, Silvestri DM, Siegler M, et al. : Critical care and emergency department response at the epicenter of the COVID-19 pandemic. Health Aff (Millwood). 2020; 39:1443–1449 [DOI] [PubMed] [Google Scholar]
- 2.Government of Alberta: COVID-19 Info for Albertans. Edmonton, AB, Canada, Government of Alberta, 2020. Available at: https://www.alberta.ca/coronavirus-info-for-albertans.aspx. Accessed November 25, 2020 [Google Scholar]
- 3.Tran DT, Thanh NX, Opgenorth D, et al. : Association between strained ICU capacity and healthcare costs in Canada: A population-based cohort study. J Crit Care. 2019; 51:175–183 [DOI] [PubMed] [Google Scholar]
- 4.Alberta Health: COVID-19 Info for Albertans. Edmonton, AB, Canada, Alberta Health, 2021. Available at: https://www.alberta.ca/coronavirus-info-for-albertans.aspx. Accessed November 25, 2020 [Google Scholar]
- 5.Bagshaw SM, Tran DT, Opgenorth D, et al. : Assessment of costs of avoidable delays in intensive care unit discharge. JAMA Netw Open. 2020; 3:e2013913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Government of Alberta: Population Statistics Edmonton, 2021. Available at: https://www.alberta.ca/population-statistics.aspx#:~:text=Alberta%20added%208%2C176%20residents%20in,2021%2C%20Alberta’s%20population%20was%204%2C436%2C258. Accessed November 25, 2020
- 7.Aziz S, Arabi YM, Alhazzani W, et al. : Managing ICU surge during the COVID-19 crisis: Rapid guidelines. Intensive Care Med. 2020; 46:1303–1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Institute for Health Information: Care in Canadian ICUs. Ottawa, ON, Canada, Canadian Institute for Health Information (CIHI), 2016 [Google Scholar]
- 9.Fowler RA, Abdelmalik P, Wood G, et al. ; Canadian Critical Care Trials Group; Canadian ICU Capacity Group: Critical care capacity in Canada: Results of a national cross-sectional study. Crit Care. 2015; 19:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wunsch H, Angus DC, Harrison DA, et al. : Variation in critical care services across North America and Western Europe. Crit Care Med. 2008; 36:2787–2793, e1 [DOI] [PubMed] [Google Scholar]
- 11.Parhar KKS, Lequier L, Blackwood J, et al. : Optimizing provision of extracorporeal life support during the COVID-19 pandemic: Practical considerations for Canadian jurisdictions. CMAJ. 2020; 192:E372–E374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alberta Health: Interactive Drug Benefit List. Edmonton, AB, Canada, Alberta Health, 2017. Available at: http://www.ab.bluecross.ca/dbl/publications.php. Accessed November 25, 2020 [Google Scholar]
- 13.Alberta Health: Overview of Administrative Health Datasets, 2018. Available at: https://open.alberta.ca/dataset/657ed26d-eb2c-4432-b9cb-0ca2158f165d/resource/38f47433-b33d-4d1e-b959-df312e9d9855/download/Research-Health-Datasets.pdf. Accessed November 25, 2020
- 14.Brundin-Mather R, Soo A, Zuege DJ, et al. : Secondary EMR data for quality improvement and research: A comparison of manual and electronic data collection from an integrated critical care electronic medical record system. J Crit Care. 2018; 47:295–301 [DOI] [PubMed] [Google Scholar]
- 15.Bagshaw SM, Stelfox HT, Iwashyna TJ, et al. : Timing of onset of persistent critical illness: A multi-centre retrospective cohort study. Intensive Care Med. 2018; 44:2134–2144 [DOI] [PubMed] [Google Scholar]
- 16.Bagshaw SM, Wang X, Zygun DA, et al. : Association between strained capacity and mortality among patients admitted to intensive care: A path-analysis modeling strategy. J Crit Care. 2018; 43:81–87 [DOI] [PubMed] [Google Scholar]
- 17.Stelfox HT, Brundin-Mather R, Soo A, et al. : A multicentre controlled pre-post trial of an implementation science intervention to improve venous thromboembolism prophylaxis in critically ill patients. Intensive Care Med. 2019; 45:211–222 [DOI] [PubMed] [Google Scholar]
- 18.Stelfox HT, Soo A, Niven DJ, et al. : Assessment of the safety of discharging select patients directly home from the intensive care unit: A multicenter population-based cohort study. JAMA Intern Med. 2018; 178:1390–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canadian Institute for Health Information: Case Mix. Ottawa, ON, Canada, Canadian Institute for Health Information (CIHI), 2018 [Google Scholar]
- 20.Graciano AL, Bhutta AT, Custer JW: Reduction in paediatric intensive care admissions during COVID-19 lockdown in Maryland, USA. BMJ Paediatr Open. 2020; 4:e000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young PJ, Gladwin B, Psirides A, et al. : Unplanned admissions to the Wellington hospital intensive care unit before, during and after New Zealand’s COVID-19 lockdown. N Z Med J. 2020; 133:95–103 [PubMed] [Google Scholar]
- 22.Kansagra AP, Goyal MS, Hamilton S, et al. : Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med. 2020; 383:400–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Solomon MD, McNulty EJ, Rana JS, et al. : The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020; 383:691–693 [DOI] [PubMed] [Google Scholar]
- 24.Bhambhvani HP, Rodrigues AJ, Yu JS, et al. : Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern Med. 2021; 181:272–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baldi E, Sechi GM, Mare C, et al. ; Lombardia CARe Researchers: Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med. 2020; 383:496–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gershengorn HB, Harrison DA, Garland A, et al. : Association of intensive care unit patient-to-intensivist ratios with hospital mortality. JAMA Intern Med. 2017; 177:388–396 [DOI] [PubMed] [Google Scholar]
- 27.Gabler NB, Ratcliffe SJ, Wagner J, et al. : Mortality among patients admitted to strained intensive care units. Am J Respir Crit Care Med. 2013; 188:800–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bravata DM, Perkins AJ, Myers LJ, et al. : Association of intensive care unit patient load and demand with mortality rates in US Department of Veterans Affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 2021; 4:e2034266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schull MJ, Stukel TA, Vermeulen MJ, et al. : Surge capacity associated with restrictions on nonurgent hospital utilization and expected admissions during an influenza pandemic: Lessons from the Toronto severe acute respiratory syndrome outbreak. Acad Emerg Med. 2006; 13:1228–1231 [DOI] [PubMed] [Google Scholar]
- 30.Moynihan R, Johansson M, Maybee A, et al. : COVID-19: An opportunity to reduce unnecessary healthcare. BMJ. 2020; 370:m2752. [DOI] [PubMed] [Google Scholar]
- 31.Wunsch H, Hill AD, Bosch N, et al. : Comparison of 2 triage scoring guidelines for allocation of mechanical ventilators. JAMA Netw Open. 2020; 3:e2029250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schull MJ, Stukel TA, Vermeulen MJ, et al. : Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007; 176:1827–1832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stöhr E, Aksoy A, Campbell M, et al. : Hospital admissions during COVID-19 lock-down in Germany: Differences in discretionary and unavoidable cardiovascular events. PLoS One. 2020; 15:e0242653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gershengorn HB, Iwashyna TJ, Cooke CR, et al. : Variation in use of intensive care for adults with diabetic ketoacidosis*. Crit Care Med. 2012; 40:2009–2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Viglianti EM, Bagshaw SM, Bellomo R, et al. : Hospital-level variation in the development of persistent critical illness. Intensive Care Med. 2020; 46:1567–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.