Abstract
Advancement toward competency-based medical education (CBME) has been hindered by inertia and a myriad of implementation challenges, including those associated with assessment of competency, accreditation/regulation, and logistical considerations. The COVID-19 pandemic disrupted medical education at every level. Time-in-training sometimes was shortened or significantly altered and there were reductions in the number and variety of clinical exposures. These and other unanticipated changes to existing models highlighted the need to advance the core principles of CBME. This manuscript describes the impact of COVID-19 on the ongoing transition to CBME, including the effects on training, curricular, and assessment processes for medical school and graduate medical education programs. The authors outline consequences of the COVID-19 disruption on learner training and assessment of competency, such as conversion to virtual learning modalities in medical school, redeployment of residents within health systems, and early graduation of trainees based on achievement of competency. Finally, the authors reflect on what the COVID-19 pandemic taught them about realization of CBME as the medical education community looks forward to a postpandemic future.
COVID-19 produced profound and devastating effects on all elements of modern life including a massive impact on medical education. In undergraduate medical education (UME), the pandemic resulted in removal of students from clinical rotations and cessation of away opportunities 1; meanwhile, graduate medical education (GME) learners were redeployed, their clinical experiences were frequently altered or converted to telehealth, and caseloads were reduced. 2 In this manuscript, we summarize the impact of the first few waves of COVID-19 on implementation and evolution of competency-based medical education (CBME) in the United States. We then consider the consequences for CBME in a postpandemic world.
The Pre–COVID-19 World: CBME Before the Pandemic
The purpose of medical education is to train student physicians to become competent in providing health care services that meet societal needs. For the purposes of the manuscript, we define competent as an individual “possessing the required abilities in all domains in a certain context at a defined stage of medical education or practice.” Competence is defined as “the array of abilities across multiple domains or aspects of physician performance in a certain context; competence is multidimensional and dynamic. It changes with time, experience, and setting.” 3 Traditionally, “time-in-seat” has been used as a poor but feasible and convenient proxy to determine competence among trainees. 4 In contrast, CBME provides a more explicit focus on a learner’s abilities as the outcome achieved throughout training. 4
In recent years, several core principles have been introduced to describe effective implementation of CBME. These include consensus recommendations regarding the definition of CBME, 3 effective methods of assessment, 5 key components to develop CBME curricula, 6 and the role of coaching to promote physician development. 7 A distinct nomenclature is used to describe curriculum and assessment strategies. This includes related but discrete terms such as “competencies,” “milestones,” and “entrustable professional activities (EPAs).” Competencies describe the abilities and attributes of physicians, while milestones depict the developmental stages that physicians progress through within a given competency in developmental, narrative terms. EPAs take a slightly different lens; they describe the work of physicians. 8
Formal incorporation of CBME in medical education programs in North America began with CanMEDS in Canadian training programs, 9 and core competencies of Accreditation Council for Graduate Medical Education (ACGME) and American Board of Medical Specialties in U.S. GME settings. 10 Early efforts to investigate the feasibility of CBME programs include a pilot within an orthopedic residency program in Toronto, 11 the creation of specialty-specific milestones across U.S. GME programs, 12 and the Association of American Medical College’s (AAMC) publication and pilot of the Core EPAs for entering residency. 13 Further efforts led to validation studies of the CanMEDS framework 9 and novel approaches to assessment, 14 analysis of milestone-based data, 15 and the AAMC’s Education in Pediatrics Across the Continuum project. 16 Coaching, an aspect of some of these pilots, is now recognized as an important component in CBME. 7 Through coaching, learners are able to process information received from evaluators and translate that feedback into concrete actions in their progression toward competence.
Despite the rapid embrace and adoption of CBME frameworks, there have been several notable challenges. Assessment in a CBME model requires multiple methods, assessors, selection/training of raters, psychometrics, and group-based decision making. 14 In addition to the assessment-related challenges, other issues include reliance on predictable numbers of residents and fellows to perform for patient care needs, regulatory requirements of the profession, the lack of funding for medical education and research, and complacency on the part of educational leaders and health care systems. 3,6,17 Indeed, in the months and years immediately preceding COVID-19, there was substantial progress toward realization of CBME, but a great deal of further work is still required.
The Disruption: What Happened to Medical Education as a Consequence of COVID-19?
Undergraduate medical education
On March 17, 2020, the AAMC recommended all institutions pause clinical rotations for their medical students immediately. 18 The rationale included concerns over limited personal protective equipment (PPE) and the need for time to develop an action plan and ensure the safety of students and patients. The shutdown concluded around August of 2020, when the AAMC issued guidance for return to in-person activities. 1
The shutdown of clinical training programs and local, state, and federal regulations created a ripple effect for medical education. To facilitate dissemination of information and ideas, AAMC provided informal webinars to generate discussion among educational leaders. Common modifications included front-loading of “nonclinical” components of clerkship experiences, consolidating clerkships, and reducing graduation requirements. 19 Educational leaders stacked didactic sessions and/or administered the National Board of Medical Examiners subject examinations during the pause in patient care activities. To ensure on-time graduation, medical school leaders reduced required lengths of clerkships. These changes coupled with removal or reduction of elective time allowed students to graduate on time, albeit with less clinical experience than prior cohorts.
In the midst of these modifications, medical school leaders sought additional opportunities to keep students engaged. At some institutions, students participated in volunteer efforts, such as distribution or production of PPE. Students were also rapidly trained in telehealth delivery. This form of health care became the only method for direct patient care for many providers and allowed for continued clinical care in a virtual environment.
Promotion, advancement, and graduation were all impacted by the aforementioned changes. United States Medical Licensing Examination Step 2 Clinical Skills (Step 2 CS) was temporarily and, ultimately, permanently canceled. In response to these rapid changes, the Liaison Committee on Medical Education (LCME) encouraged medical schools to reach out for help with maintaining accreditation in the context of a global pandemic. 20
While medical students largely returned to clinical training in the summer of 2020, there were several subsequent challenges. First, academic medical centers generally prohibited undergraduate medical students from caring for patients with suspected or confirmed COVID-19. 1 In parallel, public health authorities required a 10- to 14-day period of mandatory quarantine following exposure. Finally, patient volumes were decreased in many services due to reduction in elective surgeries, near elimination of other viral pathogens, and patients’ avoidance of health care settings. In total, these changes led to periodic student removal and additional reduction in the quantity and type of patient encounters.
In November 2020, the announcement of multiple vaccine options led to significant hope among health care providers throughout the world. Ultimately, most clinical students were offered vaccination in the early months of 2021, allowing for gradual return to “normalcy” with respect to in-person training.
Graduate medical education
Trainees in GME had the opposite experience of undergraduate medical students; many were called to the frontline to care for patients with COVID-19. Residents across specialties were redeployed to help in emergency rooms, medical wards, and intensive care units (ICU), and fellows were allowed to function as attendings in their core specialties. 21 Simultaneously, patients with non–COVID-19 illnesses stopped presenting to clinics and emergency rooms and elective procedures were paused. 22
On March 24, 2020, ACGME created a new framework allowing sponsoring institutions to self-declare “Pandemic Emergency Status,” in which many specialty-specific requirements would be waived. 23 As the COVID-19 pandemic continued, the ACGME transitioned to an application process for a time-limited request to classify a training program as being in the “emergency category,” acknowledging pandemic-related educational disruptions in those programs. 23
The disruption to activities of teaching hospitals meant the usual clinical experiences of residents and fellows were curtailed, surgical case minimums were at risk of not being met, electives were suspended or relinquished to redeployment, and away rotations were paused. 2 New telemedicine requirements allowed supervising physicians to provide “direct supervision” of trainees via telecommunication technology without requiring their physical presence. 24 Finally, social distancing requirements resulted in delays and postponement of United States Medical Licensing Examination Step 3 and specialty/subspecialty board exams for some, as well as edited requirements and timelines for the boards.
Many other facets of GME were disrupted. Teaching conferences transitioned to videoconferencing formats and research opportunities were reduced or shifted to endeavors related to COVID-19. 25 Residents and fellows were frequently unable to present their scholarly work due to cancelation of conferences in the early phases of the pandemic. Later, meetings transitioned to virtual formats, which improved opportunities but inherently limited networking and learning. Studies reported higher rates of stress, burnout, anxiety, and depression among residents and fellows during the pandemic. 26
Training programs adapted to the limitations placed on usual clinical experiences and traditional ways of assessment, spurred by the guidance laid out by ACGME that “... sponsoring institutions and programs must ensure that residents and fellows can successfully complete their programs and become eligible for board certification.” 27 Subspecialty fellowship recruitment and most job interviews were conducted via videoconferencing.
Impact on international medical graduates.
International medical graduates (IMG) constitute almost 25% of licensed physicians in the United States. 28 Certification by the Educational Commission for Foreign Medical Graduates (ECFMG) serves as assurance that an IMG is ready to enter supervised training in the United States. Due to the suspension of the Step 2 CS exam, ECFMG was forced to create new pathways to certification for the 2021 main residency match. Moreover, restrictions limited away and visiting rotations. As a consequence, IMGs and residency programs faced significant additional hurdles.
Ongoing impact of the pandemic.
The early phase of the pandemic had a significant impact on the health of learners, with many becoming ill and at least 5 residents or fellows in U.S. GME programs dying from COVID-19 in the first 6 months. 29 Fortunately, in December 2020, many residents and fellows had access to the newly available vaccines. Fears of PPE shortages were also mitigated by an improved supply chain. Teachers and learners alike became more adept at distance learning and clinical platforms and gained easier access to experts and virtual resources from around the world. Collectively, care for patients with COVID-19 became more routine, and to some extent, less fear-provoking.
Consequences: How the Disruption Impacted CBME
Undergraduate medical education
In an indirect endorsement of the CBME model, the LCME explicitly reinforced learners’ achievement of programmatic objectives as the primary determinant of readiness for advancement. 20 Though the LCME has maintained an outcomes-based approach to curricular and assessment structures, the endorsement of objectives rather than rotational requirements allowed medical schools to focus on achievement of competency.
The need to transition traditional face-to-face teaching to alternative methods such as virtual simulation or telehealth presented another consideration relevant to CBME. Born out of necessity during the pandemic, these educational changes may ultimately produce long-term advantages. For example, there is substantial theoretical literature arguing that learners would benefit from practicing patient care activities in a simulated environment before engaging in direct patient care. This has been proven in clinical practice, through procedural-based task trainers and simulation-based education around high-risk situations, such as codes. 30 This begs the question: Should medical and other health professions students be required to demonstrate competence in the simulated environment before advancing to real-world practice?
An indirect consequence on CBME models involves the impact on assessment and grading. Anecdotally, several schools reported that students performed similar or, in some cases, better on their National Board of Medical Examiners subject examinations when administered before the start of the clinical immersion phase. In addition, medical schools were forced to confront the issue of grading in the midst of limited time for observation. For many, this resulted in conversion to a pass/fail scoring system regarding advancement. In aggregate, these challenges opened the eyes of those in the medical education community to reconsider assessment, grading, and advancement dogma.
Graduate medical education
The advancement of CBME in GME began in 2018 when the ACGME began launching revised milestones, known as Milestones 2.0, which have continued to be launched over the last 4 years. 31 Milestones 2.0 places increased emphasis on the pathway toward competence irrespective of learners’ spending a designated amount of “time-in-seat.” As a consequence of COVID-19, traditional training models that relied heavily on progression happening based on amounts of time spent and volume of patients/clinical conditions were challenged. In response, the ACGME and the American Board of Medical Specialties both issued guidance that reinforced the value of competency attainment by providing the minimum required competency-based assessments needed to make “defensible, high-stakes entrustment” decisions for individual learners. 32 Clinical competency committees (CCCs) were encouraged to review each learner’s current state and to partner with learners in creation of an individual learning plan to address the gaps. 23
The disruptions due to COVID-19 afforded novel ways for direct observation and assessment of residents and fellows. Interprofessional and multidisciplinary teamwork increased during the pandemic, providing new and more frequent opportunities for multisource feedback (i.e., 360-degree feedback) and evaluation. 33 In addition, new opportunities for observation, such as telehealth, emerged. Finally, by necessity, residents and fellows were granted increased responsibility 21 with supervision titrated to entrustability for specific tasks, such as allowing fellows to temporarily take on the role of attendings in their core specialty. 11
The pandemic also elevated the importance of the CCC for programmatic assessment. Fortunately, a body of research on group process and use of CCCs in GME was available to support the essential role of the CCC, which was codified in the summer of 2020 by the release of the third edition of the Clinical Competency Committee Guidebook. 34 Assessment inputs into the CCC to make developmental judgments changed, and the full effects of those changes are not yet known.
UME-to-GME transition
The other major pandemic-related disruption involves the UME-to-GME transition. While some specialties provide “boot camps,” there is no systematic “warm” handoff from UME to GME in the United States. This gap provided difficulty for both the class of 2020 and, perhaps more so, the class of 2021. In 2020, graduating students had completed the bulk of their training by the time the pandemic disruptions hit; many students in the class of 2021, however, experienced reductions in clinical experiences, especially in electives. Recognizing these major challenges of the 2021 transition, the American Association of Colleges of Osteopathic Medicine, AAMC, ACGME, and ECFMG created a transition toolkit to provide guidance and resources for learners and educational program leaders. 35
Reflections: What Can We Learn About CBME in the Aftermath of a Pandemic?
The gaps: Blind spots highlighted by COVID-19
As we consider the history of CBME, the disruption to health professions education caused by COVID-19, and the impact of the pandemic on CBME, it is important to identify the gaps uncovered through our collective experience.
Assessment.
The first gap involves the need for better assessment. Over the past several decades, medical educators have made significant strides toward improving assessment systems, but the pandemic clearly demonstrated continued room for improvement. Most urgently, we need to accelerate measurement of competencies that have proven harder to assess, such as professionalism, interprofessional teamwork, quality improvement and patient safety, care coordination, and cost consciousness. Twenty years since the launch of the Outcome Project in 2001, these competencies are still not routinely assessed, if even taught, in many GME programs. 36
Next, we must reconsider end-of-rotation testing. Outside the United States, in places such as the Netherlands, medical educators have implemented progress testing, which assesses developmental progression across training years. 37 Assessment for learning, combined with coaching systems, represents the future of medical education to better facilitate learner development and assess the quality of our training programs. Simultaneously, we must invest in robust systems to develop faculty. Through the frameworks of competencies, milestones, and EPAs, we have spent substantial effort defining levels of competency and the interim steps required. However, our efforts to develop our raters to measure such achievement requires that we overcome barriers such as time, money, and training.
Finally, both UME and GME need to adopt systems thinking in implementing robust programs of assessment. On the UME side, the removal of Step 2 CS coupled with the movement of Step 1 to pass/fail scoring has further accelerated the need for improved measurement of clinical skills. Work is required to create more meaningful alignment of assessment practices between UME and GME to support a more systematic, functional transition.
Continuum (or discontinuum) of education.
The second gap is that we do not have a true continuum of medical education, and there are well-known challenges bringing together the UME, GME, and continuing medical education worlds. These silos of medical education operate with different accrediting bodies, standards and approaches to implementation, and measurement of competence. These differences have been articulated through issues at the junction of UME and GME and have been cited as cause for negative consequences associated with patient care. 38 Current systems to remedy the challenges are largely inadequate. For example, the Medical Student Performance Evaluation functions more as a glorified letter of recommendation than a statement of a learner’s strengths and areas for improvement. 39
In recent years, some have proposed changes to develop and improve upon the continuum. Medical school capstone courses and intern boot camps have been successful. Additionally, some have piloted “warm handoffs” between UME and GME leaders or enhanced feed-forward activities between and within settings. 40 Other models may include the integration of coaching programs across the UME-to-GME continuum. 16
While these efforts are steps in the right direction, there is still much work required. When the pandemic first hit, there were conversations about rapidly transitioning medical students into the residency workforce. However, there was concern regarding the readiness of both systems and learners to make this transition. In reality, learners have never been ready for the transitions from medical school to residency and from residency into practice. 41 This is perhaps an even more significant issue given globalization of the physician workforce. Not only do we need to improve upon the continuum of UME to GME in the United States but we also need to consider how to create a global standard of competence such that trainees from diverse countries are prepared to care for patients in postgraduate training and into practice.&&
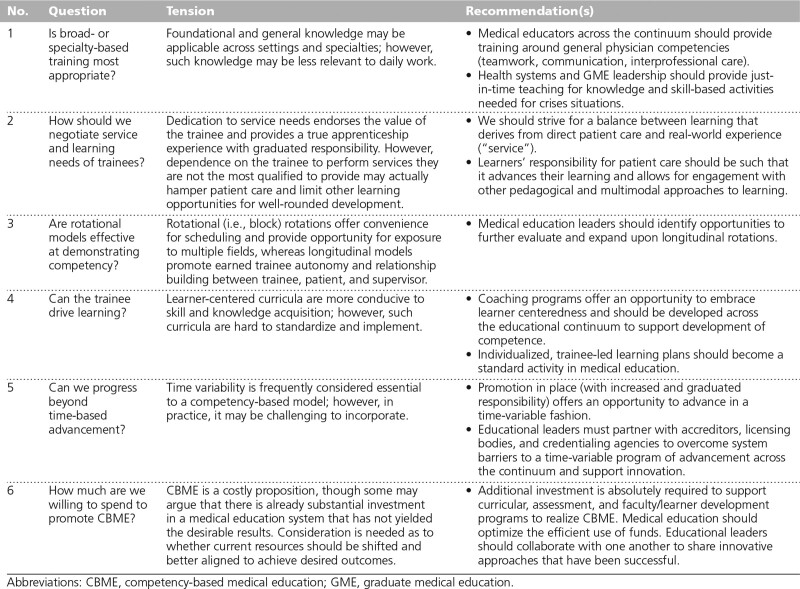
The remaining questions
In this final section, we consider the CBME-related questions that remain for the medical education community following our experience in the COVID-19 pandemic. Table 1 provides a summary of these questions, the tensions inherent within the questions, and proposed recommendations to advance CBME.
Table 1.
Summary of Key Questions, Inherent Tensions, and Proposed Recommendations to Advance CBME Following the COVID-19 Pandemic
Question 1: Is broad- or specialty-based training most appropriate?
Medical education programs have grappled with the polarity of broad-based generalist training and a more narrow-focused specialty training paradigm. 42 Within a few years of postgraduate training, the obstetrics–gynecology resident is unlikely to recall enough general medical information to feel comfortable caring for an elderly man in a medical respiratory ICU. However, in the context of the pandemic, this is exactly what was required. So, in light of the requirements thrust upon our trainees in the pandemic, do we need to revisit the philosophy of our training programs? Is there a set of core competencies we would like all trainees to acquire throughout the continuum?
While there may be value to reevaluating the balance between broad-based and specialty-based training programs, we are reminded of the so-called “forgetting curve” originally described by Ebbinghaus: one’s capacity for new knowledge is countered by its relevance and other competing demands on cognitive capacity. 43 If we were to expand upon broad-based training, it is unlikely to benefit learners if it is not immediately relevant to their practice. However, on the contrary, there is likely some advantage to foundational level knowledge, which can be built upon for a critical situation. For example, interprofessional teamwork, communication skills, and evidence-based and systems-based practice are all essential to the physician regardless of their practice setting; yet, ironically, those competencies remain the most elusive in educational programs across specialties. 36
Overall, we think a middle ground is optimal. For patient care and medical knowledge domains, just-in-time teaching is what is needed to prepare physicians for a national or international crisis in public health. For other domains, the medical education community should provide substantial more focus to ensure that learners possess the communication skills, teamwork abilities, and evidence- and systems-based practice competencies to provide effective health care in the 21st century. The time has come to move beyond medical knowledge as the primary measure of physician competence, particularly in our increasingly diverse, interprofessional, and global communities.
Question 2: How should we negotiate the service and learning needs of trainees?
The reallocation and quarantine of resident providers led to an unmasking of the issue that residents are depended upon to provide direct patient care in health care systems. They are relied upon to gather initial histories, to identify problems in the early morning hours, and to make rounds while attending physicians are busy in the operating room or in clinic. In the educational context, they are also counted on to serve as the frontline teachers for medical students. In direct contrast, medical students were sidelined completely from clinical scenarios, suggesting that they are expendable in meeting patient care needs.
These observations in the setting of a national crisis illustrate a major challenge with CBME implementation in the United States. When compared with our neighbors in Canada, educational programs in the United States have struggled to implement CBME, in part, due to a lack of opportunities for direct observation. The process of direct observation is almost exclusively for learning and feedback and requires some degree of redundancy in patient care responsibilities. Because residents see patients with indirect and physically separate supervision, their responsibilities are often integral to the effective and efficient delivery of patient care. On the other hand, medical students are present exclusively for educational purposes.
This raises the challenging conundrum of service versus education, or rather, “right” service. “Right” service is that which helps deliver effective patient care and promotes the professional development of the learner. On the one hand, some may argue that trainees are present for the purpose of education alone and they should not be considered such an integral part of the workforce that their removal leads to a critical deficiency. However, there is a downside to a strict educational focus for philosophical and practical reasons. Philosophically, medicine is a profession based on the idea of a service apprenticeship. In that context, trainees are learning the profession through graduated responsibility. Practically, if trainees were completely redundant to the care of patients, there would be substantial costs to the system that may inadvertently threaten the future of medical education training programs. Overall, we feel a balance is required. As some have suggested, in UME, we must advocate for increased service-based focus of our medical students to open their untapped potential as value-added providers. 44 However, we must counterbalance this by ensuring that learners, particularly on the GME side, are not given so much responsibility for patient care activities that either their learning opportunities are impeded or that patient outcomes are threatened.
Question 3: Are rotational models effective at demonstrating competency?
In traditional UME and GME programs, learning is typically segmented to block rotations. In medical schools, blocks are often discipline specific (e.g., internal medicine, surgery, pediatrics). For this setting, this regimen is more traditional than requirement; however, such is not the case in residency. In GME, the ACGME and the specialty certification boards set requirements on the type, number, and duration of several experiences.
For years, some have argued against the rotational model of training. In UME, longitudinal integrated clerkships counter the traditional model by placing students in a single setting and integrating their patient care activities. Longitudinal integrated clerkships have substantial benefits, including better trust between patients and learners, increased learner responsibility, and more advanced professional identity formation among learners. 45 By design, rotational models require learners to transition abruptly between specialties and subspecialties, and, as a result, they can be fraught with difficulties and may hinder learner progression toward competence. 46
The COVID-19 pandemic further questioned this model. In the UME setting, rotations were drastically modified, consolidated, or eliminated. As a consequence, medical education programs were forced to determine whether learners met programmatic objectives in other rotations, and in many cases, they had. Students could demonstrate they cared for patient case types in different clerkship contexts, reducing the need for specific rotations. These observations question whether rotations support the development of competency or whether they hamper its development by creating artificial timelines. In summary, rotational models have pragmatic advantages; however, longitudinal models can provide several notable advantages for competency development. As such, expansion of longitudinal programming should be explored further to advance CBME.
Question 4: Can the trainee drive learning?
The movement toward coaching programs was instrumental in shifting dynamics for learning from a faculty-centered model to a learner-centered concept. In many ways, the pandemic has furthered this movement. The ACGME’s UME-to-GME transition document endorsed momentum toward learner centeredness by including reflective questions for students to consider as they started residency. 35 In the circumstances surrounding COVID-19, this was both valuable for the learner’s demonstration of competence and for their confidence going into a situation with unknown outcomes and unclear expectations. Coaching programs must be expanded across the educational continuum to promote CBME.
Question 5: Can we progress beyond time-based advancement?
Time variability is frequently described as a defining feature of CBME. 47 However, it is simultaneously one of the most significant barriers to its realization. 17 This conundrum has raised some to question how integral the time-variable component is to CBME: is it a defining feature or is it valuable but not imperative?
As we consider this question, it is helpful to first describe how, despite perceptions to the contrary, the medical education community has frequently challenged a fixed time frame for training. In World War II, many medical students graduated in 3 years to fulfill critical shortages within the health care workforce. In recent years, many schools have continued with the tradition of consolidating the MD program, albeit for a variety of reasons, such as reducing financial burden on learners and improving the primary care workforce in rural health care settings. 48 Finally, many, if not all, medical schools have truncated the basic science curriculum from the traditional 2-year model to 1 or 1.5 years. Collectively, these successful initiatives all highlight that there is nothing magical about the 4-year degree and other time-based traditions in medical school education.
The relationship between time-based advancement and competency achievement is somewhat more complex on the GME side. In an early CBME model within an orthopedic residency in Toronto, the time-variable component was removed because of logistical issues associated with staffing. 11 And in the United States, time variability is challenged when board certification decisions have come into play. 49 Yet, at the same time, advancement happens de facto within GME programs, wherein supervising physicians may relinquish supervision, allowing trainees independence based on the supervising physician’s personal and often informal assessment of each trainee’s competency. Experiences during the COVID-19 pandemic reinforced that time-variable, competency-based advancement is possible on a relatively large scale, particularly if advancement takes place within programs or, to some extent, across the UME-to-GME continuum.
The COVID-19 pandemic also provided an optimal opportunity to test competency-based advancement into practice. However, limitations posed by specialty and subspecialty boards markedly limited this opportunity, and thus, even when there were significant needs to increase the workforce, we were simply unable to do so. In lieu, we asked retired physicians to come out of practice, reallocated practicing physicians to other specialties, and asked for volunteers to travel out of state to help meet the demand. It is clear that, to make progress in the junction between GME and practice, we will need to work with specialty boards, credentialing bodies, and our institutions to advance to a competency-based model.
Question 6: How much are we willing to spend to promote CBME?
Finally, it is important to discuss the direct and indirect costs of CBME. The costs of CBME include time, money, and infrastructure to create necessary administrative structures, rigorous (and bias-free) methods of assessment, technology platforms (e.g., dashboards, portfolios), curricula, faculty development programs, and political buy-in from institutions and accrediting/licensing bodies. 17 The inherent question becomes: How willing are we (educators, learners, and society) to engage in the costly reform efforts necessary to promote the optimization of the CBME model?
We think this is the wrong question. Perhaps a better question is: How willing are we to maintain the status quo? To support GME programs alone, the public provides upward of $20 billion/year for salary/benefits and large indirect costs to cover other expenses within health care institutions. Is there not already an expectation that our trainees are being directly observed, provided with feedback, and assessed on their readiness to advance in their training? Further investment is certainly needed; however, it is simultaneously worth asking what we need to do to provide the return on investment that our communities expect and deserve? With relatively small financial investment, but a relatively large investment in collaboration, there are increasing examples of innovation to advance programs, learning experiences, and assessment methods to enhance our promise to produce competent physicians. 50
Conclusion
Eventually, the COVID-19 pandemic will come to a close. While we all look forward to a return to “normalcy,” we hope that the accelerated momentum toward CBME during the pandemic will not be wasted. Many of the gaps in CBME may be distilled down to our ongoing difficulties with curricular structure, assessment, and faculty development. As we look forward to the postpandemic world, the foundation has been laid for successful CBME delivery. By addressing the remaining challenges and answering the key questions, we believe that the medical education community may finally deliver on its promise to train physicians who have demonstrated, through measurable outcomes-based assessment, that they are competent to practice the art and science of medicine.
Footnotes
Funding/Support: M.S. Ryan receives salary support to serve as cross-continuum consultant for the Association of American Medical Colleges. E.S. Holmboe receives royalties from Elsevier publishing.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Eric S. Holmboe, Email: eholmboe@acgme.org.
Subani Chandra, Email: sc3328@cumc.columbia.edu.
References
- 1.Association of American Medical Colleges. Important guidance for medical students on clinical rotations during the coronavirus (COVID-19) outbreak [press release]. https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak. Published March 17, 2020. Accessed October 29, 2021.
- 2.Potts JR, 3rd. Residency and fellowship program accreditation: Effects of the novel coronavirus (COVID-19) pandemic. J Am Coll Surg. 2020;230:1094–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank JR, Snell LS, ten Cate O, et al. Competency-based medical education: Theory to practice. Med Teach. 2010;32:638–645. [DOI] [PubMed] [Google Scholar]
- 4.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. [DOI] [PubMed] [Google Scholar]
- 5.Holmboe ES, Sherbino J, Long DM, Swing SR, Frank JR. The role of assessment in competency-based medical education. Med Teach. 2010;32:676–682. [DOI] [PubMed] [Google Scholar]
- 6.Van Melle E, Frank JR, Holmboe ES, Dagnone D, Stockley D, Sherbino J; International Competency-based Medical Education Collaborators. A core components framework for evaluating implementation of competency-based medical education programs. Acad Med. 2019;94:1002–1009. [DOI] [PubMed] [Google Scholar]
- 7.Sawatsky AP, Huffman BM, Hafferty FW. Coaching versus competency to facilitate professional identity formation. Acad Med. 2020;95:1511–1514. [DOI] [PubMed] [Google Scholar]
- 8.ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ. 2013;5:157–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Royal College of Physicians and Surgeons of Canada. History of CanMEDS. https://www.royalcollege.ca/rcsite/canmeds/about/history-canmeds-e. Accessed November 2, 2021.
- 10.Swing S. ACGME launches outcomes assessment project. JAMA. 1998;279:1492–1492. [Google Scholar]
- 11.Nousiainen MT, Mironova P, Hynes M, et al. ; CBC Planning Committee. Eight-year outcomes of a competency-based residency training program in orthopedic surgery. Med Teach. 2018;40:1042–1054. [DOI] [PubMed] [Google Scholar]
- 12.Edgar L, McLean S, Hogan SO, Hamstra S, Holmboe ES. The Milestones Guidebook: Version 2020. Chicago, IL: Accreditation Council for Graduate Medical Education; 2020. https://www.acgme.org/globalassets/milestonesguidebook.pdf. Accessed November 2, 2021. [Google Scholar]
- 13.Englander R, Flynn T, Call S, et al. Toward defining the foundation of the MD degree: Core Entrustable Professional Activities for Entering Residency. Acad Med. 2016;91:1352–1358. [DOI] [PubMed] [Google Scholar]
- 14.Lockyer J, Carraccio C, Chan MK, et al. ; ICBME Collaborators. Core principles of assessment in competency-based medical education. Med Teach. 2017;39:609–616. [DOI] [PubMed] [Google Scholar]
- 15.Li ST, Tancredi DJ, Schwartz A, et al. ; Association of Pediatric Program Directors (APPD) Longitudinal Educational Assessment Research Network (LEARN) Validity of Resident Self-Assessment Group. Competent for unsupervised practice: Use of pediatric residency training milestones to assess readiness. Acad Med. 2017;92:385–393. [DOI] [PubMed] [Google Scholar]
- 16.Andrews JS, Bale JF, Jr, Soep JB, et al. ; EPAC Study Group. Education in Pediatrics Across the Continuum (EPAC): First steps toward realizing the dream of competency-based education. Acad Med. 2018;93:414–420. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins RE, Welcher CM, Holmboe ES, et al. Implementation of competency-based medical education: Are we addressing the concerns and challenges? Med Educ. 2015;49:1086–1102. [DOI] [PubMed] [Google Scholar]
- 18.Association of American Medical Colleges. AAMC releases recommendations on coronavirus [press release]. https://www.aamc.org/news-insights/press-releases/aamc-releases-recommendations-coronavirus. Published March 11, 2020. Accessed November 2, 2021.
- 19.Association of American Medical Colleges. AAMC building better curriculum webinars. https://www.aamc.org/what-we-do/mission-areas/medical-education/curriculum-inventory/establish-your-ci/webinars. Accessed November 2, 2021.
- 20.Liaison Committee on Medical Education. Covid-19 updates and resources. https://lcme.org/covid-19. Accessed November 2, 2021.
- 21.Manson DK, Shen S, Lavelle MP, et al. Reorganizing a medicine residency program in response to the COVID-19 pandemic in New York. Acad Med. 2020;95:1670–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American College of Surgeons. COVID-19: Elective case triage guidelines for surgical care. http://www.facs.org/covid-19/clinical-guidance/elective-case. Published March 24, 2020. Accessed November 2, 2021.
- 23.Accreditation Council for Medical Education ACGME resident/fellow education and training considerations related to coronavirus (COVID-19) [press release]. https://www.acgme.org/newsroom/2020/3/acgme-residentfellow-education-and-training-considerations-related-to-coronavirus-covid-19. Published March 13, 2020. Accessed November 2, 2021.
- 24.Accreditation Council for Graduate Medical Education. ACGME response to COVID-19: Clarification regarding telemedicine and ACGME surveys. https://www.acgme.org/newsroom/blog/2020/3/acgme-response-to-covid-19-clarification-regarding-telemedicine-and-acgme-surveys. Published March 20, 2020. Accessed November 2, 2021.
- 25.U.S. Department of Health and Human Services. Office for Human Research Protections. OHRP guidance on coronavirus. HHS.gov. https://www.hhs.gov/ohrp/regulations-and-policy/guidance/ohrp-guidance-on-covid-19/index.html. Published April 8, 2020. Accessed November 2, 2021.
- 26.Sanghavi PB, Au Yeung K, Sosa CE, Veesenmeyer AF, Limon JA, Vijayan V. Effect of the coronavirus disease 2019 (COVID-19) pandemic on pediatric resident well-being. J Med Educ Curric Dev. 2020;7:2382120520947062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Accreditation Council for Medical Education. Sponsoring institution emergency categorization. https://www.acgme.org/COVID-19/Sponsoring-Institution-Emergency-Categorization. Accessed November 2, 2021.
- 28.Association of American Medical Colleges. Active physicians who are international medical graduates (IMGs) by specialty, 2019. https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-who-are-international-medical-graduates-imgs-specialty-2019. Accessed November 2, 2021.
- 29.Byrne LM, Holmboe ES, Kirk LM, Nasca TJ. GME on the frontlines-health impacts of COVID-19 across ACGME-accredited programs. J Grad Med Educ. 2021;13:145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86:706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edgar L, Roberts S, Holmboe E. Milestones 2.0: A step forward. J Grad Med Educ. 2018;10:367–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Accreditation Council on Graduate Medical Education. Guidance statement on Competency-Based Medical Education during COVID-19 residency and fellowship disruptions [press release]. https://www.acgme.org/newsroom/2020/9/guidance-statement-on-competency-based-medical-education-during-covid-19-residency-and-fellowship-disruptions/. Published September 22, 2020. Accessed December 17, 2021.
- 33.Kumaraiah D, Yip N, Ivascu N, Hill L. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catalyst Innovations in Care Delivery. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0158. Published April 28, 2020. Accessed November 2, 2021. [Google Scholar]
- 34.Andolsek K, Padmore J, Hauer KE, Ekpenyong A, Edgar L, Holmboe E. Clinical Competency Committees. A Guidebook for Programs. 3rd ed. Chicago, IL: Accreditation Council for Graduate Medical Education; 2020. https://www.acgme.org/globalassets/acgmeclinicalcompetencycommitteeguidebook.pdf. Accessed November 2, 2021. [Google Scholar]
- 35.Accreditation Council for Graduate Medical Education. Transition to residency. https://acgme.org/COVID-19/Transition-to-Residency. Accesesd November 2, 2021.
- 36.Weiss KB, Co JPT, Bagian JP; CLER Evaluation Committee. Challenges and opportunities in the 6 focus areas: CLER National Report of Findings 2018. J Grad Med Educ. 2018;10(suppl 4):25–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vleuten CPMVD, Verwijnen GM, Wijnen WHFW. Fifteen years of experience with progress testing in a problem-based learning curriculum. Med Teach. 1996;18:103–109. [Google Scholar]
- 38.Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD. “July effect”: Impact of the academic year-end changeover on patient outcomes: A systematic review. Ann Intern Med. 2011;155:309–315. [DOI] [PubMed] [Google Scholar]
- 39.Hook L, Salami AC, Diaz T, Friend KE, Fathalizadeh A, Joshi ART. The revised 2017 MSPE: Better, but not “outstanding.” J Surg Educ. 2018;75:e107–e111. [DOI] [PubMed] [Google Scholar]
- 40.Sozener CB, Lypson ML, House JB, et al. Reporting achievement of medical student milestones to residency program directors: An educational handover. Acad Med. 2016;91:676–684. [DOI] [PubMed] [Google Scholar]
- 41.Lyss-Lerman P, Teherani A, Aagaard E, Loeser H, Cooke M, Harper GM. What training is needed in the fourth year of medical school? Views of residency program directors. Acad Med. 2009;84:823–829. [DOI] [PubMed] [Google Scholar]
- 42.Weisz G. The emergence of medical specialization in the nineteenth century. Bull Hist Med. 2003;77:536–575. [DOI] [PubMed] [Google Scholar]
- 43.Ebbinghaus H. Memory: A contribution to experimental psychology. Ann Neurosci. 2013;20:155–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gonzalo JD, Dekhtyar M, Hawkins RE, Wolpaw DR. How can medical students add value? Identifying roles, barriers, and strategies to advance the value of undergraduate medical education to patient care and the health system. Acad Med. 2017;92:1294–1301. [DOI] [PubMed] [Google Scholar]
- 45.Hudson JN, Poncelet AN, Weston KM, Bushnell JA, A Farmer EA. Longitudinal integrated clerkships. Med Teach. 2017;39:7–13. [DOI] [PubMed] [Google Scholar]
- 46.Bernabeo EC, Holtman MC, Ginsburg S, Rosenbaum JR, Holmboe ES. Lost in transition: The experience and impact of frequent changes in the inpatient learning environment. Acad Med. 2011;86:591–598. [DOI] [PubMed] [Google Scholar]
- 47.Lucey CR, Thibault GE, ten Cate O. Competency-based, time-variable education in the health professions: Crossroads. Acad Med. 2018;93(suppl 3):S1–S5. [DOI] [PubMed] [Google Scholar]
- 48.Cangiarella J, Fancher T, Jones B, et al. Three-year MD programs: Perspectives from the Consortium of Accelerated Medical Pathway Programs (CAMPP). Acad Med. 2017;92:483–490. [DOI] [PubMed] [Google Scholar]
- 49.American Medical Association. AMA Reimagining Residency initiative. https://www.ama-assn.org/education/improve-gme/ama-reimagining-residency-initiative. Accessed November 2, 2021.
- 50.Frank JR, Snell L, Englander R, Holmboe ES; ICBME Collaborators. Implementing competency-based medical education: Moving forward. Med Teach. 2017;39:568–573. [DOI] [PubMed] [Google Scholar]