Abstract
Most children with coronavirus disease 2019 (COVID-19) infection are asymptomatic or have mild disease. About 5% of infected children will develop severe or critical disease. Rapid identification and treatment are essential for children who are critically ill with signs and symptoms of respiratory failure, septic shock, and Multisystem Inflammatory Syndrome in Children (MIS-C). This article is intended for pediatricians, pediatric emergency physicians, and individuals involved in the emergency care of children. It reviews the current epidemiology of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in children, summarizes key aspects of clinical assessment including identification of high-risk patients and manifestations of severe disease, and provides an overview of COVID-19 management in the emergency department based on clinical severity.
Keywords: COVID-19, pediatrics, emergency care, Multisystem Inflammatory Syndrome in Children, MIS-C, sepsis, critical illness
Introduction, background and epidemiology of SARS-CoV-2 in children
As of June 2021, more than 177 million cases of coronavirus disease 2019 (COVID-19), the infection caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), have been confirmed worldwide, with over 3.8 million deaths. The prevalence of symptomatic COVID-19 infection is lower in children compared to adults.2 Data from several large cohort studies suggest that children account for approximately 2.0% of total COVID-19 infections,3 or more than 3.5 million known COVID-19 infections globally. While the majority of children infected with SARS-CoV-2 have asymptomatic or mild disease, approximately 5–7% will present with or develop severe or critical manifestations of COVID-19 including myocardial dysfunction, shock, acute respiratory distress syndrome (ARDS), altered mental status, multiple organ dysfunction syndrome, or Multisystem Inflammatory Syndrome in Children (MIS-C).4–6
Clinical Assessment and Diagnosis
Initial Evaluation and Triage
Infection prevention and control (IPC) measures should be in place at the first point of in-person contact (e.g., screening and/or triage). This includes personal protective equipment (PPE) for all providers and staff and evaluating children presenting with signs and symptoms of COVID-19 in separate clinical spaces. Outpatient clinics, emergency departments and hospitals should consider developing a clear, clinical pathway to help with patient flow and isolation of patients with suspected COVID-19 infection.
A child with confirmed or suspected COVID-19 infection should be triaged on arrival to determine disease severity, need for immediate stabilization and treatment, and appropriate disposition. Previously healthy children and adolescents with mild symptoms may be candidates for virtual triage and evaluation.7 Children who should be evaluated immediately, however, include: infants <3 months old with fever and older infants and children with more than three days of fever, respiratory distress, or any sign of organ dysfunction such as decreased urine output.8 Patients who are immunocompromised or have a chronic disease such as lung disease or congenital heart disease, or obesity (body mass index [BMI]>40) are at higher risk of severe disease.8
Asymptomatic, Mild and Moderate COVID-19
Asymptomatic COVID-19 infection and mild or non-specific symptoms are more common in children compared to adults.9 Even children with asymptomatic or mild infection can transmit the virus, however.10 By some estimates, 25–73% of children who test positive for SARS-CoV-2 by polymerase chain reaction (PCR) are asymptomatic.10,11 In a study from 28 children’s hospitals across the United States, SARS-CoV-2 PCR positivity rates in asymptomatic children presenting for medical or surgical care varied from 0 to 2.2% (pooled prevalence of 0.65%) and were significantly associated with infection rates in the general population at the time of testing.12
Common symptoms in children include: fever, dry cough, fatigue, and nasal congestion.13 Gastrointestinal symptoms, such as vomiting and diarrhea, are also common in children, far more so than in adults.13 Younger children and infants can present with a wide range of non-specific signs and symptoms including fever, decreased feeding, or lethargy in the absence of respiratory symptoms; therefore, a high index of suspicion for COVID-19 infection is needed.14
Severe and Critical COVID-19
Although rare, children with COVID-19 infection can present with severe manifestations: respiratory failure and ARDS; sepsis and septic shock; acute kidney injury and renal failure; myocarditis, heart failure and cardiac arrest; acute liver failure with cholestasis, severe neurological manifestations such as seizures and stroke; and MIS-C.15–17 It is critical to recognize the ominous signs of impending respiratory failure and/or shock and immediately initiate appropriate support and therapy.
MIS-C is a rare manifestation of SARS-CoV-2 that has been described in children and young adults and is likely related to immune dysregulation and subsequent cytokine storm.4,6,18,19 MIS-C often presents as a post-viral manifestation 2–3 weeks after SARS-CoV-2 infection or after a peak of infections in the community.19,20 Many children with MIS-C do not exhibit respiratory symptoms and may have had a previous, asymptomatic COVID-19 infection.20 Common symptoms of MIS-C include: fever; gastrointestinal symptoms such as abdominal pain, nausea, vomiting, and non-bloody diarrhea, sometimes 1–2 weeks prior to presentation; dermatologic manifestations such as rash and malar erythema that often develop 2–3 days after onset of fever and last for approximately 5 days; mucocutaneous features such as conjunctival injection, periorbital edema and/or distal extremity edema, and strawberry tongue; and cardiovascular involvement including coronary artery aneurysms, myocardial dysfunction, pericarditis, valvulitis, or coronary dysfunction.6,18,19,21,22
SARS-CoV-2 Testing and Diagnostics
Testing for COVID-19 infection typically involves a nucleic acid amplification test (NAAT) such as a reverse transcriptase polymerase chain reaction (RT-PCR), an antigen rapid diagnostic test (RDT), or an antibody (IgM or IgG)/serology test. NAATs are considered to be the gold standard and are more sensitive than antigen testing. Antibody tests can be used to support the diagnosis of COVID-19 in patients with late symptoms (≥ 8 days after symptom onset) or to help assess whether sequelae (e.g., MIS-C) are due to a past infection; however, they cannot be used to rule out or diagnose acute infection active disease. Indications for testing vary by local epidemiology and hospital protocol.
Common laboratory findings in children with COVID-19 infection include: leukocytosis, lymphopenia, coagulopathy and elevated inflammatory markers (LDH, CRP, ESR, ferritin, IL-6), D-dimer, and troponin.23 Lymphopenia, elevated WBC count, elevated platelet count, elevated creatine kinase MB, elevated Brain Natriuretic Peptide (BNP), higher levels of CRP, and higher levels of procalcitonin at admission are associated with increased disease severity.11,24,25 Please refer to Figure 1 for an approach to laboratory testing in Acute COVID-19 infection.
1.
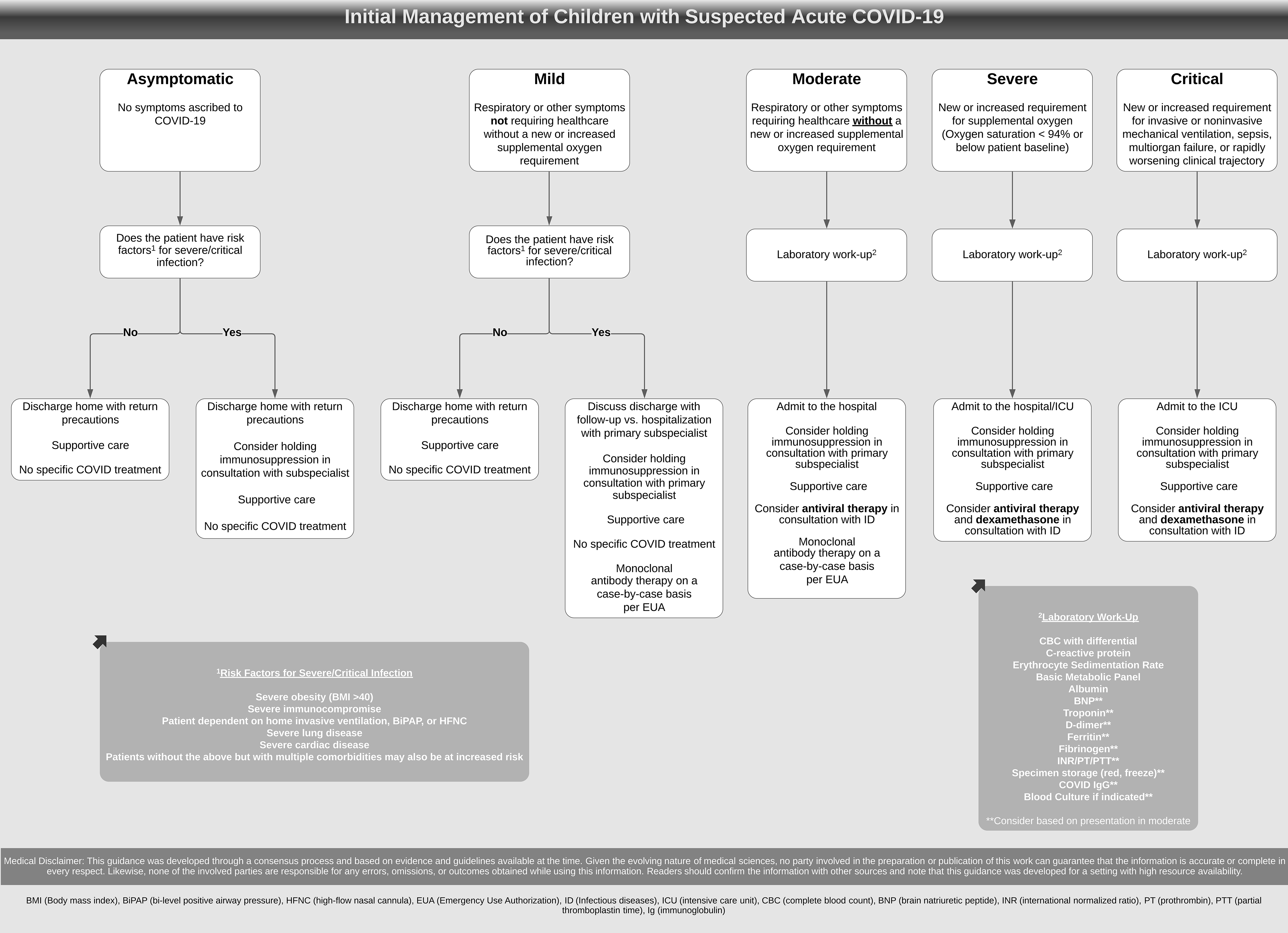
Initial Management of Children with Suspected Acute COVID-19. Adapted and printed with permission from the UCSF Benioff Children’s Hospital Pediatric COVID/MIS-C Guidelines developed by the Pediatric COVID/MISC Working Group (Version 1, Last Updated: 04/01/2021)
Common radiologic findings include peribronchial and bronchial wall thickening as well as basilar and peripheral ground-glass opacities which can be found in both symptomatic and asymptomatic children.13 Normal chest x-rays, however, do not rule out COVID-19 infection.26 Low-risk patients with mild COVID-19 infection do not routinely need chest imaging. Consider obtaining a chest x-ray if there is a high clinical concern for lobar pneumonia, heart failure or tuberculosis; in patients with hypoxia requiring supplemental oxygen, increased work of breathing, or new or sudden decompensation; high clinical suspicion for COVID-19 despite negative testing (possible false negative test); or to check line and/or endotracheal tube placement. Lung ultrasound may also be a reasonable method to detect lung abnormalities in children.27 Routine imaging by computed tomography (CT) is not recommended and may be normal in up to 50% of children with mild COVID-19 infection.28
High-Risk Groups
Among infected children, adolescents >15 years of age are more likely to require hospitalization and intensive care.29 Some studies show that neonates are also more likely to be hospitalized and have severe infection; however, most cases are mild to moderate.3,29 Life-threatening respiratory disease in neonates is rare.30 Adolescents and children with comorbidities, such as congenital heart disease, diabetes, severe obesity (BMI >40), chronic respiratory disease, and immunocompromising conditions, are at higher risk for developing severe COVID-19 disease requiring hospitalization and may need different criteria for admission and/or closer follow-up upon discharge.3,9,24,29,31–34
Differential Diagnosis
The differential for COVID-19 infection is broad for symptomatic infants and children. Other diseases that mimic COVID-19 infection or that can occur concurrently include: tuberculosis, bacterial or viral pneumonia, congestive heart failure, urinary tract infections, bacteremia, and gastrointestinal illnesses.14 Other respiratory viral infections, such as influenza, adenovirus, respiratory syncytial virus (RSV), parainfluenza, and metapneumovirus, and atypical pneumonias (mycoplasma, chlamydia pneumoniae), can also present similarly to COVID-19.
MIS-C may be confused with Toxic Shock Syndrome (TSS), Kawasaki Disease (KD), severe sepsis, or macrophage activation syndromes (MAS), all of which can occur in a post-acute illness setting and involve fever, rash, erythema, edema, conjunctivitis, and oral mucosal changes (e.g., “strawberry tongue”). However, the average age of children with MIS-C is 7–9 years while for KD it is 2 years;21,35,36 MIS-C has more diffuse cardiovascular involvement than KD;19,35,36 and children with MIS-C tend to have a greater elevation in inflammatory markers (CRP, IL-6, fibrinogen) compared to those with TSS or KD.35,36
Management and Disposition
Supportive care is the mainstay of therapy for children with COVID-19 infection and should be provided to all pediatric patients.37,38 In general, home medications should be continued, though immunosuppressants should be considered on a case-by-case basis in discussion with the child’s primary medical doctor (PMD) or prescribing subspecialty physician. Figure 1 outlines the initial management of children with suspected acute COVID-19 infection for asymptomatic to critical disease.
Mild and Moderate COVID-19
Mild infection in children is characterized by a generally well-appearing child with respiratory or other mild symptoms without significant tachypnea, hypoxia (oxygen saturation <94%), or a new or increased oxygen requirement. Most patients with mild disease and no significant risk factors do not require laboratory testing, diagnostic imaging, specific monitoring or COVID-19 therapies; rather, they can be managed at home with symptomatic treatment and home isolation. Some children with comorbidities may be candidates for outpatient monoclonal antibody therapy on a case-by-case basis. Certain comorbid conditions (e.g., type one diabetes, adrenal insufficiency) may need adjustment in their medications for these conditions and closer monitoring.
COVID-19 disease severity can progress rapidly; parents and caregivers should be counseled to seek medical care if their child experiences new or progressing symptoms.39 Infants >28 days and young children with more than three days of fever should follow-up with their PMD to assess for bacterial supra-infection and monitor hydration and respiratory status.
Moderate infection is characterized by respiratory or other symptoms, like dehydration, requiring healthcare, but without a new or increased oxygen requirement. Symptom management and supportive care are the foundations of treatment while routine diagnostic imaging and COVID-19-specific therapies are not recommended, though some hospitalized children early in their course may be candidates for monoclonal antibody therapy. Admission to the general inpatient ward with possible infectious disease consultation is recommended. As mentioned above, children with COVID-19 infection can decompensate quickly, so monitoring is recommended.
Severe COVID-19
Severe infection in children is characterized by new or increased oxygen requirement (oxygen saturation <94% or below the patient’s baseline) requiring hospital admission for oxygen therapy, supportive care, COVID-19-specific treatment, and/or monitoring. Hospital admission and possible initiation of Remdesivir and dexamethasone (off-label use) therapy in consultation with appropriate pediatric subspecialty teams (e.g., infectious disease) are recommended. While there is little evidence to support the use or benefit of Remdesivir in children with COVID-19 infection, it is approved in the United States by the Food and Drug Administration (FDA) and used to treat both adults and children >12 years and >40 kg with COVID-19 due to pharmacological rationale. It is not labeled for use in younger or smaller children, though many institutions choose to administer it. Guidelines for the use of Remdesivir have mixed recommendations and evidence continues to evolve.
Goals of supplemental oxygen therapy include: resolution of hypoxia and manageable work of breathing (Figure 2). If the child worsens, develops respiratory failure, or progresses to ARDS, the child should be intubated and mechanically ventilated.40 If the child does not show signs of dehydration and/or is not in shock, a conservative approach to intravenous fluid administration should be used as aggressive fluid resuscitation may worsen oxygenation and pulmonary compliance.40
2.
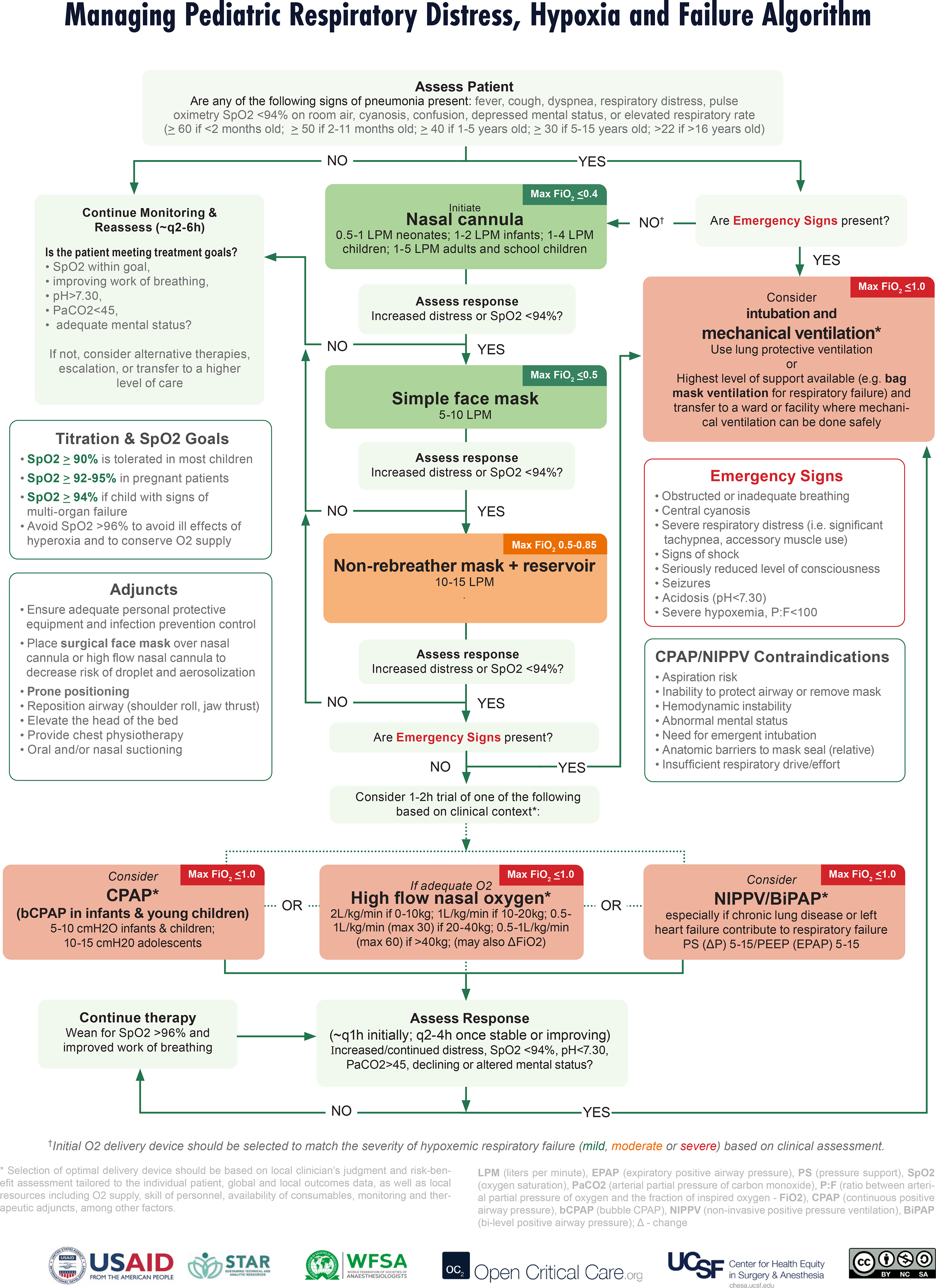
Managing Pediatric Respiratory Distress, Hypoxia and Failure Algorithm. Adapted and printed with permission from Open Critical Care available at: https://opencriticalcare.org/resources/
Critical COVID-19
Respiratory Failure
Critical COVID-19 in children is characterized by a new or increased invasive or non-invasive mechanical ventilation requirement (respiratory failure/ARDS), sepsis, shock, multiorgan failure or rapidly worsening clinical trajectory. Admission to the pediatric intensive care unit (PICU); possible initiation of Remdesivir, corticosteroid therapy and/or prophylactic anticoagulation therapy; and consultation with appropriate pediatric subspecialty teams (e.g., infectious disease, hematology) are recommended (Figure 1). Interventions such as high flow oxygen are being used, although there have not yet been large trials in children with COVID-19. A child with respiratory distress and hypoxia should be closely monitored for signs of clinical deterioration as children can rapidly progress to respiratory failure and shock (Figure 2). Children who develop pediatric acute respiratory distress syndrome should be managed with lung protective ventilation per current guidelines.41,42 Because of the risk of aerosolization with many of the interventions for respiratory failure, such as high flow oxygen, non-invasive positive pressure and frequent suctioning, special attention to IPC protocols is needed along with placing patients in a single, negative pressure room whenever possible.
Shock
Sepsis and septic shock are rare but potentially life-threatening manifestations of COVID-19 in children and must be promptly recognized and treated.43 Immediate goals when managing pediatric septic shock are to maintain perfusion to the organs and to treat the underlying infection. For improved survival, initiate empiric, broad-spectrum antimicrobial therapy and fluid bolus resuscitation with balanced or buffered crystalloids within 1 hour of recognition and titrate fluid resuscitation to clinical markers of increased perfusion.40,44 Fluid resuscitation may lead to volume overload and capillary leak which may exacerbate respiratory failure, so frequent reassessment for signs of fluid responsiveness and fluid overload during resuscitation is imperative.40,44 If signs of fluid overload are present or signs of shock persist after two fluid boluses, initiate vasoactive therapy for hemodynamic support. Monitor blood pressure frequently and titrate vasoactive medications to the minimum dose necessary to maintain perfusion and prevent side-effects. Inodilators should not be used routinely and are typically not used for septic shock in the absence of cardiac dysfunction.40,44
Children with sepsis frequently show signs of decreased cardiac output, which can be due to hypovolemia or direct myocardial dysfunction.45,46 Acute myocardial dysfunction due to myocardial injury is especially prevalent in children with MIS-C as indicated by higher levels of troponin and brain natriuretic peptide compared to children with non-COVID-19-related sepsis.6,21 Early and thorough cardiac evaluation including ECG, echocardiography (ECHO) and biomarkers (troponin, CK and CK MB, lactate, mixed venous oxygen saturation) on all children who present in shock to rule out cardiac involvement or cause is important. 40,44 In children with suspected MIS-C, early cardiology consultation and specific attention to the coronary arteries on ECHO to rule out aneurysms is recommended. In cases where cardiac dysfunction is suspected or known, reserve fluid resuscitation for patients demonstrating decreased preload, ideally by ECHO, and small volume boluses (5–10ml/kg) over 30–60 minutes should be used with frequent reassessment. In consultation with pediatric cardiology subspecialists, discuss whether inodilators should be initiated and optimize ventilation/gas exchange by providing oxygen therapy with a goal SpO2 >94%. If noninvasive or invasive ventilation are indicated, be aware of the cardio-pulmonary interactions and prepare for the possibility of cardiac arrest on intubation.40,44 Currently, there is insufficient evidence to recommend for or against corticosteroids to treat refractory shock in children with COVID-19; however, corticosteroids may be indicated for the treatment of acute COVID-19 infection. Routine red blood cell transfusions are generally not recommended in hemodynamically stable children with a blood hemoglobin concentration ≥ 7 g/dL.40,44
Cardiac Arrest
The American Heart Association (AHA), in collaboration with the American Academy of Pediatrics (AAP) and the American College of Emergency Physicians (ACEP), published interim guidance for management of pediatric cardiac arrest with suspected/confirmed COVID-19. Pediatric Advanced Life Support (PALS) Algorithms should be followed with several important additions: use appropriate PPE; limit personnel to the minimum number necessary; use a bag-mask device with a filter and tight seal; if intubating, have the person with the highest likelihood of success intubate, use video-assisted laryngoscopy, and use a cuffed endotracheal tube; and, finally, minimize closed-circuit disconnection in intubated patients.47
MIS-C
Like acute COVID-19, MIS-C can present along a spectrum of severity ranging from mild symptoms to shock. The initial management approach for children with suspected MIS-C should focus on stabilization, improving end-organ perfusion, and early cardiac evaluation given the high incidence of myocardial involvement (Figure 3). Treatments for MIS-C target different aspects of the pathophysiology and include antiplatelet therapy like aspirin (off-label use); immunomodulating therapies like intravenous immunoglobulin (IVIg) or Anakinra (off-label use); and anti-inflammatory medications like methylprednisolone (off-label use). If MIS-C is suspected, early consultation or referral to a center with pediatric subspecialist care including critical care, rheumatology, hematology/oncology, cardiology, infectious diseases, and immunology is recommended. For patients with signs of shock, coronary artery dilation, arrhythmia, or cardiac dysfunction, even in the absence of Kawasaki and/or MIS-C-like features, consider urgent transfer to a PICU and urgent consultation of the above subspecialists.48
3.
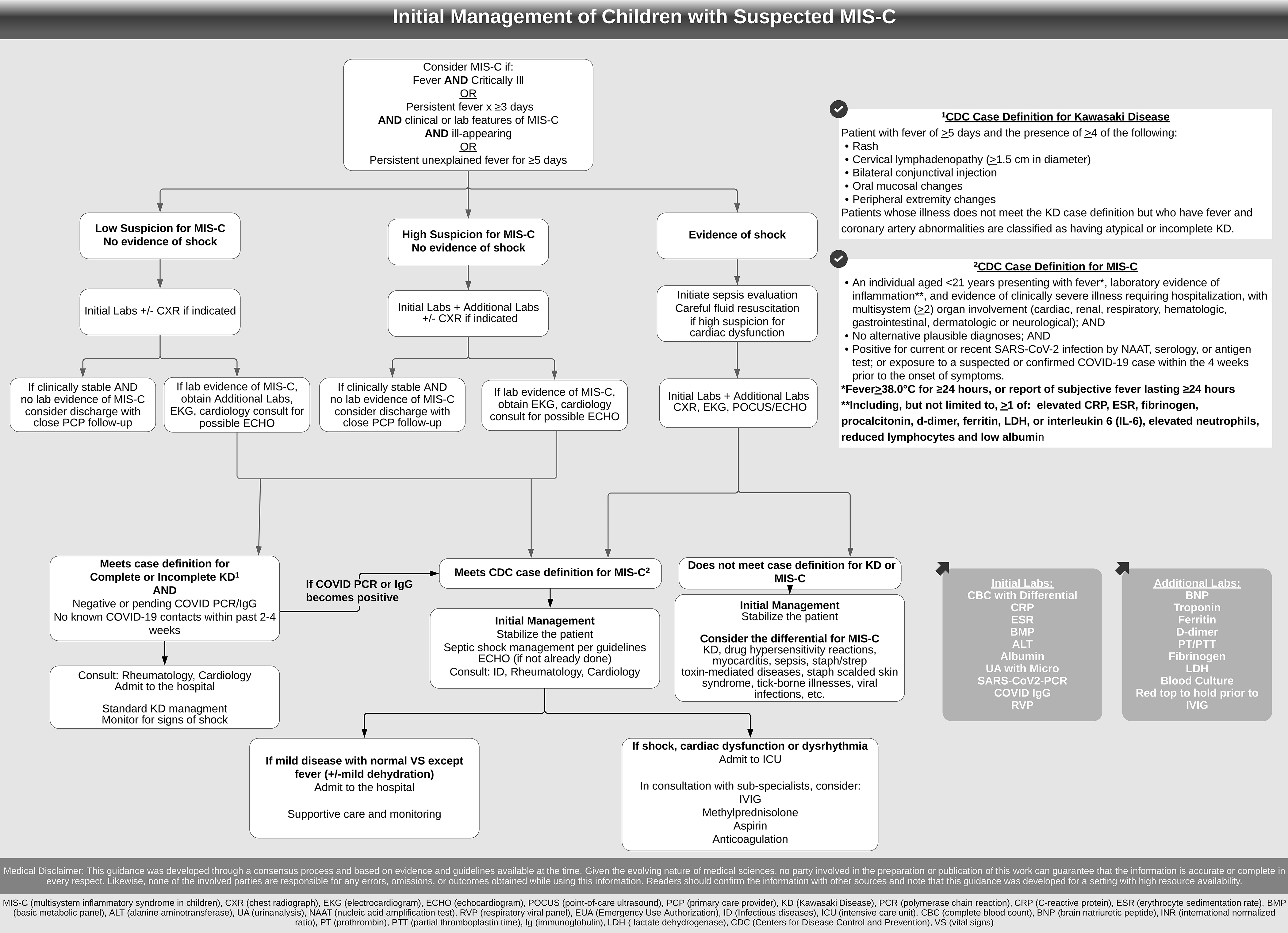
Initial Management of Children with Suspected MIS-C. Adapted and printed with permission from the UCSF Benioff Children’s Hospital Pediatric COVID/MIS-C Guidelines developed by the Pediatric COVID/MISC Working Group (Version 1, Last Updated: 04/01/2021)
Published outcomes
Hospitalization rates, need for ICU-level care, and mortality tend to be lower in children than adults, but are highly variable depending on testing patterns, case definitions and resources. According to data from the US Department of Health, as of September 2020, children represented 1.7% of total SARS-CoV-2 hospitalizations and 0.07% of total deaths.49 These rates may vary by age and geographic location. One large retrospective cohort study that included people <25 years of age in the US found that 7% of SARS-CoV-2-infected children required hospitalization, and of those hospitalized, 28% required ICU-level care and 9% required mechanical ventilation. Case fatality rate was 0.2%.50 Children with MIS-C tend to require ICU-level care more often (74% vs. 44%) and have a slightly higher probability of mortality compared to acute COVID-19 (1.9% vs. 1.4%).21 Among children with MIS-C and decreased left ventricular systolic function, over 90% had normalized function within 30 days.21
Summary
While COVID-19 disease severity is lower in children compared to adults, symptoms in children can be atypical and vary widely. COVID-19 infection should be considered when a child presents with respiratory, gastrointestinal or neurological complaints, especially when community infection rates are high. Children can still experience severe and critical disease including shock, ARDS, sepsis, and MIS-C. Early recognition and management of respiratory failure, septic shock, and myocardial dysfunction are essential. While MIS-C has overlapping features with other diseases such as KD and TSS, it is characterized by a greater elevation of inflammatory markers and diffuse cardiac involvement. Supportive care is the mainstay of therapy for children with COVID-19 infection and MIS-C and additional therapies such as Remdesivir, corticosteroids, prophylactic anticoagulation, aspirin, and immunomodulating therapies should be considered in severe and critical disease in consultation with appropriate pediatric subspecialty team(s). While death is rare in children with COVID-19 infection, children with severe and critical infection or MIS-C should be closely monitored as they can rapidly deteriorate and progress to respiratory failure and shock.
5. Multiple choice questions.
- MIS-C may be confused with Kawasaki Disease (KD), but children with MIS-C tend to have these distinguishing factors:
- Older average age and diffuse myocardial involvement
- Hispanic or African descent and coronary artery aneurysms
- Younger average age and of Hispanic or African descent
- Non-Hispanic white descent and diffuse myocardial involvement
- Signs of septic shock in children may include:
- Altered mental status
- Bradycardia or tachycardia
- Tachypnea
- Warm or cool skin
- All of the above
- Common presenting symptoms in children with COVID-19 infection include all of the following EXCEPT:
- Fever
- Cough
- Liver failure
- Gastrointestinal symptoms
- Fatigue
- Severe presentations of COVID-19 infection in children include:
- Respiratory failure and ARDS
- Septic shock
- Renal failure
- Myocarditis
- All of the above
- The mainstay of therapy for children with COVID-19 infection is:
- Steroids
- Supportive care
- Antivirals
- Antibiotics
- Anticoagulation
Target Audience:
This article is for pediatric emergency physicians, emergency physicians, pediatricians, family physicians, and other healthcare providers caring for acutely ill children in emergency departments and urgent care settings.
Learning objectives:
After reading this article the reader should be able to:
Recognize the common, uncommon, and severe presentations of COVID-19 infection in children
Identify children with COVID-19 at higher risk for severe disease
Manage COVID-19 in the emergency department according to illness severity
Conflicts of Interest and Source of Funding:
TK (K23AI1440.29) and EC (NCT03892915) receive salary support from the National Institutes of Health. For the remaining authors none were declared.
Contributor Information
Dr. Teresa B. Kortz, Department of Pediatrics, Critical Care Medicine, University of California, San Francisco, CA, USA; Affiliate Faculty for the Institute of Global Health Sciences, University of California, San Francisco, CA, USA.
Dr. Emilia Connolly, Partners In Health/Abwenzi Pa Za Umoyo, Malawi; Division of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA; Division of Hospital Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Dr. C. Lee Cohen, Department of Pulmonary and Critical Care, Brigham and Women’s Hospital, Boston, MA USA; Broad Institute of Harvard and MIT, Boston, MA USA.
Dr. Rebecca E. Cook, Partners In Health-Liberia; Division of Pediatric Global Health, Massachusetts General Hospital, Boston MA USA; Department of Internal Medicine & Pediatrics, Harvard Medical School, Boston MA USA.
Dr. Jennifer A. Jonas, Department of Pediatrics, Weill Cornell Medicine, New York City, NY.
Dr. Michael S. Lipnick, Department of Anesthesia and Critical Care, University of California, San Francisco, CA, USA; Affiliate Faculty for the Institute of Global Health Sciences, University of California, San Francisco, CA, USA.
Dr. Niranjan Kissoon, Department of Pediatrics, Global Child Health BC Children’s Hospital University of British Columbia, Vancouver, Canada; Child & Family Research Institute (CFRI), Vancouver, Canada; Division of Critical Care, BC Children’s Hospital University of British Columbia, Vancouver, Canada.
Literature Cited
- 1.University CfSSaEaJH. COVID-19 Dashboard. June 18, 2021. 2021. https://coronavirus.jhu.edu/map.html (accessed June18 2021).
- 2.Leidman E, Duca LM, Omura JD, Proia K, Stephens JW, Sauber-Schatz EK. COVID-19 Trends Among Persons Aged 0–24 Years - United States, March 1-December 12, 2020. MMWR Morb Mortal Wkly Rep 2021; 70(3): 88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellino S, Punzo O, Rota MC, et al. COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy. Pediatrics 2020; 146(4). [DOI] [PubMed] [Google Scholar]
- 4.Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med 2020; 383(4): 334–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godfred-Cato S, Bryant B, Leung J, et al. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep 2020; 69(32): 1074–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020; 395(10237): 1607–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reid S, Bhatt M, Zemek R, Tse S. Virtual care in the pediatric emergency department: a new way of doing business? Cjem 2021; 23(1): 80–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feketea GM, Vlacha V. A Decision-Making Algorithm for Children With Suspected Coronavirus Disease 2019. JAMA pediatrics 2020; 174(12): 1220–2. [DOI] [PubMed] [Google Scholar]
- 9.Wald ER, Schmit KM, Gusland DY. A Pediatric Infectious Disease Perspective on COVID-19. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2021; 72(9): 1660–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poline J, Gaschignard J, Leblanc C, et al. Systematic SARS-CoV-2 screening at hospital admission in children:a French prospective multicenter study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. The Lancet Infectious diseases 2020; 20(6): 689–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sola AM, David AP, Rosbe KW, Baba A, Ramirez-Avila L, Chan DK. Prevalence of SARS-CoV-2 Infection in Children Without Symptoms of Coronavirus Disease 2019. JAMA pediatrics 2021; 175(2): 198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castagnoli R, Votto M, Licari A, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review. JAMA pediatrics 2020; 174(9): 882–9. [DOI] [PubMed] [Google Scholar]
- 14.Mithal LB, Machut KZ, Muller WJ, Kociolek LK. SARS-CoV-2 Infection in Infants Less than 90 Days Old. J Pediatr 2020; 224: 150–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nepal G, Rehrig JH, Shrestha GS, et al. Neurological manifestations of COVID-19: a systematic review. Critical care (London, England) 2020; 24(1): 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perez A, Cantor A, Rudolph B, et al. Liver involvement in children with SARS-COV-2 infection: Two distinct clinical phenotypes caused by the same virus. Liver Int 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saeed A, Shorafa E. Status epilepticus as a first presentation of COVID-19 infection in a 3 years old boy; Case report and review the literature. IDCases 2020; 22: e00942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones VG, Mills M, Suarez D, et al. COVID-19 and Kawasaki Disease: Novel Virus and Novel Case. Hosp Pediatr 2020; 10(6): 537–40. [DOI] [PubMed] [Google Scholar]
- 19.Panupattanapong S, Brooks EB. New spectrum of COVID-19 manifestations in children: Kawasaki-like syndrome and hyperinflammatory response. Cleve Clin J Med 2020. [DOI] [PubMed] [Google Scholar]
- 20.Belay ED, Abrams J, Oster ME, et al. Trends in Geographic and Temporal Distribution of US Children With Multisystem Inflammatory Syndrome During the COVID-19 Pandemic. JAMA pediatrics 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldstein LR, Tenforde MW, Friedman KG, et al. Characteristics and Outcomes of US Children and Adolescents With Multisystem Inflammatory Syndrome in Children (MIS-C) Compared With Severe Acute COVID-19. Jama 2021; 325(11): 1074–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young TK, Shaw KS, Shah JK, et al. Mucocutaneous Manifestations of Multisystem Inflammatory Syndrome in Children During the COVID-19 Pandemic. JAMA Dermatol 2021; 157(2): 207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.González-Dambrauskas S, Vásquez-Hoyos P, Camporesi A, et al. Pediatric Critical Care and COVID-19. Pediatrics 2020; 146(3). [DOI] [PubMed] [Google Scholar]
- 24.Kainth MK, Goenka PK, Williamson KA, et al. Early Experience of COVID-19 in a US Children’s Hospital. Pediatrics 2020; 146(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zachariah P, Johnson CL, Halabi KC, et al. Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA pediatrics 2020; 174(10): e202430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong HYF, Lam HYS, Fong AH, et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 2020; 296(2): E72–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Denina M, Scolfaro C, Silvestro E, et al. Lung Ultrasound in Children With COVID-19. Pediatrics 2020; 146(1). [DOI] [PubMed] [Google Scholar]
- 28.Merkus P, Klein WM. The value of chest CT as a COVID-19 screening tool in children. Eur Respir J 2020; 55(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeBiasi RL, Song X, Delaney M, et al. Severe Coronavirus Disease-2019 in Children and Young Adults in the Washington, DC, Metropolitan Region. J Pediatr 2020; 223: 199–203.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mark EG, Golden WC, Gilmore MM, et al. Community-Onset Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Young Infants: A Systematic Review. J Pediatr 2021; 228: 94–100.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fernandes DM, Oliveira CR, Guerguis S, et al. Severe Acute Respiratory Syndrome Coronavirus 2 Clinical Syndromes and Predictors of Disease Severity in Hospitalized Children and Youth. J Pediatr 2021; 230: 23–31.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ho C, Ng NBH, Lee YS. Caring for Pediatric Patients with Diabetes amidst the Coronavirus Disease 2019 Storm. J Pediatr 2020; 223: 186–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shekerdemian LS, Mahmood NR, Wolfe KK, et al. Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA pediatrics 2020; 174(9): 868–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simpson M, Collins C, Nash DB, Panesar LE, Oster ME. Coronavirus Disease 2019 Infection in Children with Pre-Existing Heart Disease. J Pediatr 2020; 227: 302–7.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang L, Tang K, Levin M, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. The Lancet Infectious diseases 2020; 20(11): e276–e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Whittaker E, Bamford A, Kenny J, et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. Jama 2020; 324(3): 259–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chiotos K, Hayes M, Kimberlin DW, et al. Multicenter Interim Guidance on Use of Antivirals for Children With Coronavirus Disease 2019/Severe Acute Respiratory Syndrome Coronavirus 2. Journal of the Pediatric Infectious Diseases Society 2021; 10(1): 34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Larson DT, Sherner JH, Gallagher KM, et al. Clinical Outcomes of COVID-19 with Evidence-Based Supportive Care. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Venturini E, Palmas G, Montagnani C, et al. Severe neutropenia in infants with severe acute respiratory syndrome caused by the novel coronavirus 2019 infection. J Pediatr 2020; 222: 259–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kache S, Chisti MJ, Gumbo F, et al. COVID-19 PICU guidelines: for high- and limited-resource settings. Pediatr Res 2020; 88(5): 705–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 2015; 16(5): 428–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khemani RG, Smith L, Lopez-Fernandez YM, et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. The Lancet Respiratory medicine 2019; 7(2): 115–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liguoro I, Pilotto C, Bonanni M, et al. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr 2020; 179(7): 1029–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med 2020; 46(Suppl 1): 10–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ceneviva G, Paschall JA, Maffei F, Carcillo JA. Hemodynamic support in fluid-refractory pediatric septic shock. Pediatrics 1998; 102(2): e19. [DOI] [PubMed] [Google Scholar]
- 46.Ranjit S, Natraj R, Kandath SK, Kissoon N, Ramakrishnan B, Marik PE. Early norepinephrine decreases fluid and ventilatory requirements in pediatric vasodilatory septic shock. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine 2016; 20(10): 561–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Topjian A, Aziz K, Kamath-Rayne BD, et al. Interim Guidance for Basic and Advanced Life Support in Children and Neonates With Suspected or Confirmed COVID-19. Pediatrics 2020. [DOI] [PubMed] [Google Scholar]
- 48.Henderson LACS, Friedman KG, Gorelik M, Lapidus SK, Bassiri H, et al. American College of Rheumatology Clinical Guidance for Pediatric Patients with Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2 and Hyperinflammation in COVID-19. Version 2. Arthritis Rheumatology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sisk B, Cull W, Harris JM, Rothenburger A, Olson L. National Trends of Cases of COVID-19 in Children Based on US State Health Department Data. Pediatrics 2020; 146(6). [DOI] [PubMed] [Google Scholar]
- 50.Bailey LC, Razzaghi H, Burrows EK, et al. Assessment of 135 794 Pediatric Patients Tested for Severe Acute Respiratory Syndrome Coronavirus 2 Across the United States. JAMA pediatrics 2021; 175(2): 176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]


