Abstract
The Rift Valley fever virus (RVFV), a member of the genus Phlebovirus (family Bunyaviridae) is an enveloped negative-strand RNA virus with a tripartite genome. Until 2000, RVFV circulation was limited to the African continent, but the recent deadly outbreak in the Arabian Peninsula dramatically illustrated the need for rapid diagnostic methods, effective treatments, and prophylaxis. A method for quantifying the small RNA segment by a real-time detection reverse transcription (RT)-PCR using TaqMan technology and targeting the nonstructural protein-coding region was developed, and primers and a probe were designed. After optimization of the amplification reaction and establishment of a calibration curve with synthetic RNA transcribed in vitro from a plasmid containing the gene of interest, real-time RT-PCR was assessed with samples consisting of RVFV from infected Vero cells. The method was found to be specific for RVFV, and it was successfully applied to the detection of the RVFV genome in animal sera infected with RVFV as well as to the assessment of the efficiency of various drugs (ribavirin, alpha interferon, 6-azauridine, and glycyrrhizin) for antiviral activity. Altogether, the results indicated a strong correlation between the infectious virus titer and the amount of viral genome assayed by real time RT-PCR. This novel method could be of great interest for the rapid diagnosis and screening of new antiviral compounds, as it is sensitive and time saving and does not require manipulation of infectious material.
The Rift Valley fever (RVF) virus (RVFV), a member of the genus Phlebovirus, belongs to the Bunyaviridae family and possesses a negative-stranded, tripartite RNA genome composed of a large, a medium, and a small (S) segment (for reviews, see references 9 and 37). Like other phleboviruses, the S segment utilizes an ambisense strategy to code for two proteins, the nucleocapsid protein and the nonstructural protein (NSs), which are synthesized from subgenomic viral complementary and viral sense mRNA, respectively.
RVF is a mosquito-borne zoonosis predominantly provoking the death of young animals and abortion (e.g., sheep and goats) (for reviews, see references 24, 39 and 41). The disease was first identified in sheep by Daubney et al. in Kenya in 1931, and it is endemic almost everywhere in subtropical Africa (6). Transmission to humans occurs primarily by contact with infected animal body fluids and by mosquito bites. Infection is usually asymptomatic or associated with a brief self-limited febrile illness. However, complications such as retinitis, encephalitis, or hemorrhagic fever occur in some patients with mortality rates of up to 10 to 12% (21, 28).
The potential of RVF as a disease emerging in new areas was first documented in Egypt in 1977 (16), and since then, epidemics have occurred in Mauritania (1987 to 1988 and 1998), Madagascar (1990 to 1991), Egypt (1993), and eastern Africa (in Kenya, Somalia, and Tanzania) (references 33 and 34 and references therein). Recently, the outbreak on the Arabian Peninsula (in Yemen and Saudi Arabia) represented the first case of RVF outside Africa (2, 4). Epizootics and epidemics are associated with periods of heavy rainfall and the concomitant presence of large numbers of mosquitoes (18). The survival of RVFV during interepizootics is believed to depend on transovarial transmission of the virus in floodwater Aedes mosquitoes (17).
Experimental vaccines are still in development, and no proven specific therapy is available for humans (3, 29). Thus, effective antiviral agents would be useful for treating severe infections or reducing viremia in amplifying hosts, thereby limiting viral propagation by biting arthropods. Currently, diagnosis is based on detection of specific antibodies or virus isolation in animal and mosquito cells (4). Reverse transcription (RT)-PCR techniques have been described and used to detect the RVFV genome in mosquitoes (11) and, recently, in clinical samples (35). In this work we developed a real-time RT-PCR method in order to detect and specifically quantify the virus either from cells or from sera and evaluated the potential of this assay for the diagnosis and screening of antiviral compounds.
MATERIALS AND METHODS
Cells, virus, and mouse sera.
Cells were grown at 37°C in 5% CO2 in 199 culture medium (M199) supplemented with 10% inactivated fetal calf serum. RVFV strains MP12, ZH501, ZH548, ArD38661, 74HB59, and clone 13 and the closely related phleboviruses Toscana, Icoaraci, and Belterra were grown in Vero cells (ATCC CCL-81) by serial passage. Virus titers were determined either by the 50% tissue culture infective dose (TCID50) method (30) or by counting the PFU under the agarose layer.
Mice were inoculated intraperitoneally with 104 PFU of RVFV strain ZH548, and blood was collected at different times postinoculation by veinal puncture at the retro-orbital sinus.
RNA in vitro transcription.
A 750-bp RNA fragment encompassing the complete NSs open reading frame of the RVFV MP12 strain in the genomic sense orientation was transcribed in vitro from the pGem3-NSs plasmid (19) by using the T7 RNA polymerase (Promega) under the conditions recommended by the supplier. The DNA template was eliminated by extensive treatment with RNase-free DNase. Proteins were eliminated by phenol-chloroform extraction, and RNA was concentrated after isopropanol precipitation. The amount of RNA was estimated by spectrophotometry, and known amounts were used to determine the standard curve for real-time RNA quantification.
RNA extraction.
Vero cells were infected with the MP12 virus at a rate of 0.01 PFU per cell, and virus present in the maintenance medium was collected after 72 h when the cytopathic effect was evident. Cell debris was eliminated by low-speed centrifugation. RNA was extracted according to the manufacturer's instructions either from 200 μl of virus stock by using the RNA Instapur kit (Eurogentec, Seraing, Belgium), from 140 μl of mouse sera by using the Trizol method (Invitrogen Life Technologies SARL, Cergy Pontoise, France), or from 140 μl of human sera by using the QIAamp Viral RNA kit (Qiagen, Courtaboeuf, France). After precipitation with isopropanol, RNA was resuspended in 50 μl of RNase-free water and stored at −80°C.
Design and synthesis of primers and fluorogenic probe.
The available NSs sequences published by Sall et al. (34) were aligned with DNAsis (version 2.6; Hitachi Software Engineering, Olivet, France), and Primer Premier software was used to design the primers and probe (version 4.04; Premier Biosoft International, Palo Alto, Calif.).
The primers S432 (5′-ATG ATG ACA TTA GAA GG GA3′) and NS3m (5′ATG CTG GGA AGT GAT GAG3′), which was modified from the NS3 primer (25), hybridize at positions 432 to 450 and 712 to 729, respectively, in genomic sense RNA, generating a 298-nucleotide DNA fragment. The primers were synthesized by Invitrogen Life Technologies. The TaqMan probe CRSSAr (5′ATT GAC CTG TGC CTG TTGCC3′) was synthesized by Oligo Genset (Paris, France). It contains a fluorescent reporter dye (6-carboxyfluorescein) at the 5′ end and a fluorescent quencher dye (6-carboxy-tetramethyl-rhodamine) at the 3′ end.
RT.
The reaction was carried out at 37°C for 60 min with 10 μl of RNA in a final volume of 30 μl with 200 IU of Moloney murine leukemia virus reverse transcriptase (Invitrogen Life Technologies) and 1 μM forward primer S432 under the conditions recommended by the supplier. Finally, the reaction mixture was heated at 95°C for 10 min to denature the enzyme.
Real-time PCR.
The amplification reaction mixture contained 2 μl of cDNA in a final volume of 20 μl, and the reaction was carried out with the LightCycler fast-start DNA Master hybridization probes kit (Roche Diagnostics, Meylan, France), MgCl2 at a 3.5 mM final concentration, the primers NS3m and S432 at 0.5 μM final concentrations, and the fluorogenic probe CRSSAr at a 0.5 μM final concentration. PCR was carried out in the LightCycler (Roche) for 45 cycles at 95°C for 15 s and 60°C for 1 min.
Assay of antiviral activity of compounds in cell culture.
Glycyrrhizin, ribavirin, and 6-azauridine were purchased from Sigma-Aldrich (St. Quentin-Fallavier, France). Alpha 2b interferon (IFN-α2b) was purchased from Schering-Plough (Herouville St-Clair, France).
Confluent layers of Vero cells in 24-well tissue culture plates were infected with 0.1 ml of diluted viral suspension (0.01 TCID50 per cell), and 2 ml of maintenance medium containing the test compound at an appropriate concentration was added (4 wells per concentration). Five concentrations of the antiviral substances were tested in decreasing order from the maximally tolerated dose, which was the highest dose that did not cause microscopically detectable cytotoxic effects. Four wells were not treated with the drugs and served as controls. After 40 h of incubation, when a maximal infectious RVFV titer was reached in the untreated cells, intra- and extracellular RVFV were obtained by three cycles of freezing and thawing. The viral titer was determined in cell culture (TCID50 per milliliter), and RNA was extracted and used to quantify the RVFV genome by real-time RT-PCR detection (RTD-PCR).
Statistical analysis.
Statistical analysis of the data was carried out using one-way analysis of variance and Spearman's test.
RESULTS
Real-time RTD-PCR of RVFV.
A traditional RT-PCR was already developed for the detection of RVFV in different specimens and proved to be efficient for the diagnosis of human cases during the 1998 Mauritanian outbreak (35). A high level of sensitivity was obtained in a nested RT-PCR assay, which detected 0.5 PFU of MP12 virus and was approximately 100-fold more sensitive than the simple one. In order to meet the requirements of rapid diagnosis and to avoid the risk of contamination, we employed the novel LightCycler instrument (Roche Diagnostics), which associates ultrarapid thermal cycling with TaqMan technology. New primers and a probe were designed in the highly conserved NSs regions previously amplified in the classical RT-PCR.
For all experiments, the threshold limit was set above the noise band, and the threshold cycle (CT) value was determined. The conditions of the amplification for salt and primer requirements were optimized with RVFV MP12 RNA; those yielding the lowest CT values were selected. Thus, in our standard conditions, the concentrations of the forward and reverse primers and the probe were 500 nM, and the concentration of MgCl2 was 3 mM.
The sensitivity and specificity of the RVFV genome detection were evaluated by using serial dilutions of a known amount of RNA transcribed in vitro from plasmid pGem-NSs. The detection and quantification were linear over the range of concentrations examined, from at least 106 to 100 copies per run (data not shown). To test the reproducibility of the results, four aliquots of the same samples were independently amplified during the same cycles (Table 1). The intra-assay coefficient of variation (CV) calculated by using the CT values (1) was found to vary between 0.2 and 1.8%, depending on the quantity of RNA. Moreover, the data reported in Table 1 indicate that the sensitivity limit was 50 to 100 copies.
TABLE 1.
Sensitivity and intraexperimental variability of RVFV strain MP12 synthetic RNAa
| No. of synthetic RNAb copies | Detection rate (%) | CT (mean ± SD) | CV (%) |
|---|---|---|---|
| 5 × 106 | 100 | 17.79 ± 0.20 | 1.1 |
| 5 × 105 | 100 | 22.22 ± 0.31 | 1.4 |
| 5 × 104 | 100 | 25.98 ± 0.47 | 1.8 |
| 5 × 103 | 100 | 29.81 ± 0.06 | 0.2 |
| 5 × 102 | 100 | 32.70 ± 0.36 | 1.1 |
| 102 | 100 | 35.14 ± 0.26 | 0.7 |
| 5 × 101 | 25 | 37.25c | NDd |
Standard deviations and CV were calculated by using the CT values.
RNA was diluted with water, and four identical samples were assayed in the same experiment.
Standard deviation was not determined.
ND, not determined.
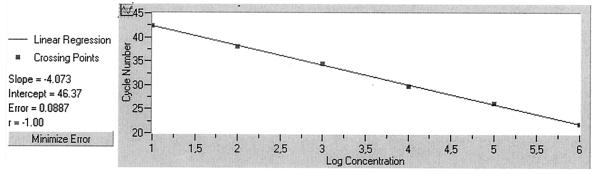
To assay RNAs from RVFV stock, serial dilutions of samples in MP12-infected cell culture supernatants containing from 106 to 10 TCID50 · ml−1 were reverse transcribed and amplified. We observed a linear response over 106 TCID50 · ml−1, and the method could detect less than 10 TCID50 · ml of RVFV−1 (Fig. 1). Moreover, we also tested variation with time by assaying the same samples in three different experiments carried out with a 1-day interval. The interassay CV calculated by using the CT values was found to vary between 0.9 and 3.0%, depending on the quantity of RNA (Table 2).
FIG. 1.
Standard curve obtained with 10-fold serial dilutions of viral RVFV RNA. CT values are plotted against different RNA amounts extracted from the infectious virus (titers running from 106 to 10 TCID50 · ml−1).
TABLE 2.
Interexperimental variability of RVFV RNA quantificationa
| Sample no. | No. of RVFV RNA copies/sample on day:
|
No. of copies/sample (mean ± SD) | CV (%) | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| 1 | 3.5 × 107 | 1.8 × 107 | 3.2 × 107 | 2.8 × 107 ± 0.20 | 0.9 |
| 2 | 1.2 × 107 | 6.7 × 106 | 1.4 × 107 | 1.1 × 107 ± 0.13 | 0.55 |
| 3 | 1.6 × 107 | 6.7 × 106 | 1.5 × 107 | 1.2 × 107 ± 0.26 | 1.1 |
| 4 | 7.7 × 107 | 3.1 × 107 | 4.8 × 107 | 5.2 × 107 ± 0.66 | 3.0 |
| 5 (blank) | Not detected | Not detected | Not detected | ||
Four identical samples from the supernatants of Vero cells infected with RVFV strain MP12 were analyzed in four separate experiments with a 1-day interval. Synthetic RNAs were included in each experiment to determine the RNA copy numbers. CV were calculated by using the CT values.
To test the specificity of the amplification, we carried out the reaction with RNAs from RVFV strains clustered in the three groups referred to as West Africa, East-Central Africa, and Egypt (31, 32, 34). These strains were ZH501, ZH548, ArD38661, 74HB59, and clone 13. We also included RNAs from closely related phleboviruses (Toscana, Icoaraci, and Belterra) and RNA extracted from uninfected AP61 or Vero cells (usually used for RVFV replication). All of the RVFV strains, except for the avirulent clone 13 strain lacking the amplified NSs sequence (25), were detected, thus confirming that the primers and probe hybridized in conserved regions of the RVFV genome. No amplification was observed for other phleboviruses or cellular RNAs (not shown).
Since real-time RT-PCR is utilized for accurate quantification, we compared the infectious titer of MP12 stock, and the concentrations of genome equivalents were determined by using the calibration curve established with in vitro-transcribed RVFV RNA amplified during the same experiment. The concentration of S genome equivalent measured by real-time RT-PCR is approximately 3 to 3.5 log higher than the infectious virus titer measured in cell culture (Table 3).
TABLE 3.
Real-time quantification of RVFV RNA extracted from MP12-infected Vero cell supernatant or from sera of infected mice collected at different times postinfection
| Source, infection status, and time (h) postinfection | Virus titera | Quantification (log RNA copies · ml−1) |
|---|---|---|
| Vero cell supernatant | ||
| Infected with MP12 | 6.0 | 9.0 |
| 5.6 | 8.5 | |
| 4.6 | 7.5 | |
| 3.4 | 6.5 | |
| 1.6 | 5.1 | |
| 1.7 | 5.1 | |
| Not infected | Not detected | Not detected |
| Mouse sera | ||
| Infected with 2H548 | ||
| 24 | 4.6 | 6.8 |
| 33 | 5.9 | 8.6 |
| 48 | >8.5 | 10.0 |
| Not infected | Not detected | Not detected |
Virus titers are expressed in PFU per milliliter for mouse serum samples and in TCID50 per milliliter for Vero cell samples.
Because real-time RT-PCR is of special importance for diagnosis, we evaluated the method by using sera from mice experimentally infected with the virulent strain ZH548 and collected at different times postinoculation. Viremia was determined by plaque assay, and after RNA extraction and amplification, the concentrations of genome equivalents were calculated (Table 3). The values obtained were in good correlation with the infectious titers. In addition, seven human serum samples artificially contaminated with the MP12 strain were successfully amplified (data not shown).
Evaluation of antiviral activity.
The screening of antiviral agents is generally tedious as it requires testing a wide range of drug concentrations followed by a large number of virus titrations. Thus, we used real-time RT-PCR to quantify RVFV yielded in the presence of the drugs. We tested ribavirin, IFN-α, 6-azauridine, and glycyrrhizin, which are already commercialized and used in patients for their antiviral or antitumor activity. They were known to inhibit the in vitro replication of another phlebovirus, sandfly fever Sicilian virus (SFSV) (5), and ribavirin was previously shown to have an inhibitory effect on RVFV replication in infected cells (27).
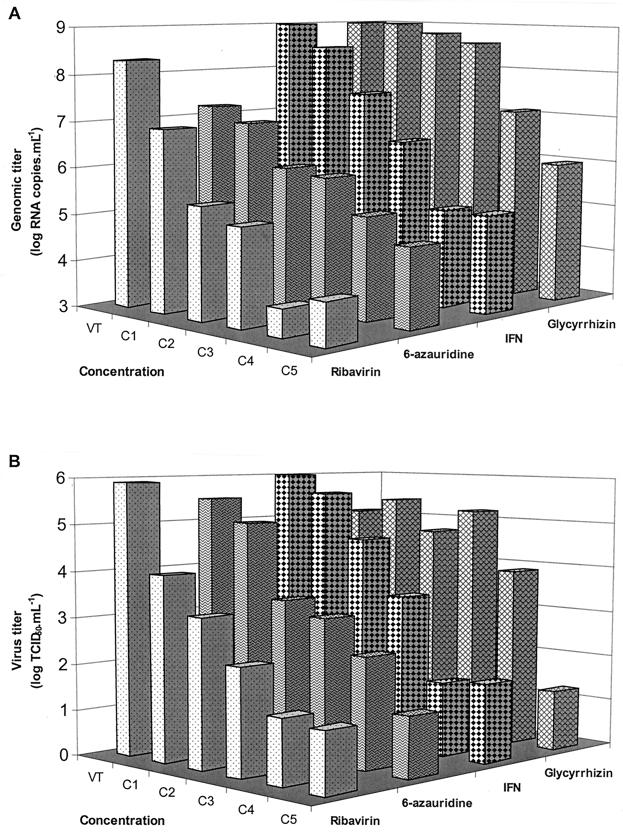
A preliminary experiment was performed to determine the maximal tolerated dose of each drug. At this concentration, these compounds inhibited virus production by >4.0 log (Table 4). The effects of decreasing concentrations were determined by two methods, titration of RVFV by TCID50 and RT-PCR of genome equivalent (Fig. 2). At the lowest concentrations tested, ribavirin (62.5 μg · ml−1), IFN-α (1 IU · ml−1), and 6-azauridine (0.3 μg · ml−1) were still active. The virus titer reductions were 1.9, 0.5, and 0.5 log, respectively, and the genome titer reductions were 1.4, 0.5, and 0.6 log, respectively. Glycyrrhizin had lower antiviral activity; viral replication was inhibited only at relatively high concentrations.
TABLE 4.
Effects of antiviral compounds on RVFV production assessed by infectious virus assay or genome detection
| Compound | Final concentrationd | Virus titer reductionb (log TCID50 · ml−1) | Genomic titer reductionb (log RNA copies · ml−1) |
|---|---|---|---|
| Glycyrrhizin | 156 | NRa | NR |
| 312 | NR | NR | |
| 625 | NR | NR | |
| 1,250 | 1.2 | 2.0 | |
| 2,500 | >4.1c | 3.0 | |
| IFN-α | 1 | 0.5 | 0.5 |
| 10 | 1.5 | 1.5 | |
| 100 | 2.7 | 2.5 | |
| 1,000 | 4.5 | 3.9 | |
| 10,000 | 4.4 | 3.9 | |
| Ribavirin | 62.5 | 1.9 | 1.4 |
| 125 | 2.7 | >2.9 | |
| 250 | 3.6 | >3.2 | |
| 500 | >4.6 | >4.7 | |
| 1,000 | >4.6 | >4.4 | |
| 6-Azauridine | 0.3 | 0.5 | 0.6 |
| 0.6 | 2.1 | 1.5 | |
| 1.3 | 2.4 | 1.7 | |
| 2.5 | 3.1 | 2.2 | |
| 5.0 | >4.5 | 2.6 |
NR, no reduction measured.
Reduction in virus titers and genome concentration between RVFV yields in treated and untreated Vero cells.
Greater than signs are used if the titers obained with an antiviral compound were below the sensitivity threshold.
Concentrations of glycyrrhizin, ribavirin, and 6-azauridine are expressed in micrograms per milliliter. Concentrations of IFN-α are expressed in international units per milliliter.
FIG. 2.
Effect of antiviral compounds on the RVFV (strain MP12) yield measured by either genomic (A) or virus (B) titer. Antiviral compound concentrations, increasing from C1 to C5, are given in Table 4. VT is the virus control (infected nontreated cells).
IFN-α and ribavirin caused a concentration-dependent reduction in the virus yield (by analysis of variance, P < 0.5). The reductions in virus titer and in genome equivalent were analyzed statistically by using the Spearman test. The two methods led to strongly correlated results (P < 0.01). Altogether, our data clearly indicate that this method should be recommended to detect and quantify viral replication.
DISCUSSION
Currently, besides recognizing clinical and biological features, the diagnosis of a human RFV infection is based on the detection of specific immunoglobulin M and immunoglobulin G antibodies or virus isolation in mammalian or mosquito cells or in the brains of suckling mice (7, 13, 22). Recently Sall et al. described a single-tube RT-PCR that allows for the detection of RVFV in clinical samples (35).
The RT-PCR is often used as a method of detection for a great number of arboviruses, which facilitates phylogenetic studies (14, 36).
Here we describe, for the first time, a method of RTD-PCR which allows the identification and quantification of RVFV RNA. This new technique is a significant improvement in PCR cycling, since it is a closed system in which the formation of amplified product is measured in real time, avoiding risks of contamination. It has been used for immediate identification of a viral agent during the early acute phase of illness and for monitoring the virus load in treated patients infected by the hepatitis B and C viruses and by herpesvirus and cytomegalovirus (1, 12, 15, 20, 40). Moreover, when compared to other quantification methods, RTD-PCR was often revealed to be more sensitive (1, 26).
The sensitivity of the assay is dependent on several factors, such as the sample source, the nucleic acid extraction method, and the thermal cycling conditions. In our hands, RNA extraction with phenol chloroform led to better results than adsorption elution on the column of the QIAamp Viral RNA kit (Qiagen). Likewise, we increased the sensitivity of the RT step by adding glycogen to the samples. The sensitivity of this RVFV assay was evaluated using synthetic and viral RNA and was shown to be less than 100 RNA copies per run or less than 10 TCID50 · ml−1, which is equivalent to the sensitivity of the traditional RT-PCR already described (11, 35). It is worth noting that the genomic titer measured by real-time RT-PCR was found to be between 2 and 3 log higher than the virus titer measured in cell culture. For the dengue virus, it was also found that each infectious PFU represents at least 100 or more genomic equivalents (10), and we found a 3 log difference with the Puumala virus (8). This difference may be due to the presence of noninfectious viral RNA, or the RVFV S segment may be overexpressed in the cells.
The specificity of the real-time RT-PCR was successfully tested with different RVFV clusters and the closely related phleboviruses Belterra, Toscana, and Icoaraci, and as expected, the method failed to detect the clone 13 strain. The use of a cDNA synthesis step allows us to overcome the limitations of Tth. Theoretically, RTD-PCR is a one-step procedure employing a single enzyme, the Tth provided by the LightCycler RNA Master hybridization probe (Roche Diagnostics). This enzyme displays RT activity at a recommended temperature of 61°C and polymerase activity at a recommended temperature of 72°C. However, we found that these conditions were suboptimal. Other kits now in development will probably overcome this problem.
In order to screen potent antiviral drugs in cell culture, it is necessary to appreciate their ability to inhibit virus replication at noncytotoxic concentrations and then to determine their concentration-dependent activity. As a reference method, the titration of infectious virus is currently used to evaluate antiviral activity. It requires a time-consuming cell culture as support for the quantification of the virus either by evaluating PFU per milliliter or TCID50 milliliter (5, 38). In this study, we obtained a good correlation when viral genomes were quantified by RTD-PCR. The latter method reduced the time required for an experiment from 1 week to 4 h, and it avoided manipulation of dangerous infectious material which required a biosafety level 3 laboratory.
Among several antiviral compounds, four were selected for their inhibitory effects on RVFV replication and for their abilities to be used in human therapeutics. Ribavirin, 6-azauridine, and IFN-α were proven to be very active at low concentrations and led to a reduction of the virus titer depending on the concentration, whereas glycyrrhizin became active at the highest concentrations tested. Among these compounds, only ribavirin and IFN-α had previously been investigated for their effects on RVFV (23, 27). Intravenous ribavirin has been shown to effectively treat other viral hemorrhagic fevers, including Lassa fever, hemorrhagic fever with renal syndrome, and Crimean-Congo hemorrhagic fever. Furthermore, the Saudi Arabian Ministry of Health recently evaluated the feasibility of a randomized, placebo-controlled trial using intravenous ribavirin in patients with suspected severe RVF infection (4). 6-Azauridine and glycyrrhizin were shown to be effective against a related phlebovirus, SFSV. It would be interesting to evaluate the efficacy of a combination of two or three compounds as was done for SFSV (5).
In conclusion, RTD-PCR detection and quantification of RVFV would be useful as a routine diagnostic test for identifying the virus in the early stage of the disease and for following up antiviral therapy. The technique should be used now in large field experiments to confirm its clinical ability. It also gives a new way to estimate the in vitro efficiency of potential antiviral substances and to detect unusual antiviral resistance.
ACKNOWLEDGMENTS
This work was supported by research grants from the Service de Santé des Armées and from the Délégation Générale à l'Armement (grant no. 00CO014; PEA 980-814).
We thank Corinne Rothlisberger, Danielle Gratier, Josette Guimet, Henri Blancquaert, and Pierre Vialat for technical assistance.
REFERENCES
- 1.Abe A, Inoue K, Tanaka T, Kato J, Kajiyama N, Kawaguchi R, Tanaka S, Yoshiba M, Kohara M. Quantitation of hepatitis B virus genome DNA by real-time detection PCR. J Clin Microbiol. 1999;37:2899–2903. doi: 10.1128/jcm.37.9.2899-2903.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmad K. More deaths from Rift Valley fever in Saudi Arabia and Yemen. Lancet. 2000;356:1422. doi: 10.1016/S0140-6736(05)74068-X. [DOI] [PubMed] [Google Scholar]
- 3.Caplen H, Peters C J, Bishop D H L. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66:2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Outbreak of Rift Valley fever—Saudi Arabia, August-October, 2000. Morb Mortal Wkly Rep. 2000;49:905–908. [PubMed] [Google Scholar]
- 5.Crance J M, Gratier D, Guimet J, Jouan A. Inhibition of sandfly fever Sicilian virus (Phlebovirus) replication in vitro by antiviral compounds. Res Virol. 1997;148:353–365. doi: 10.1016/s0923-2516(97)89132-7. [DOI] [PubMed] [Google Scholar]
- 6.Daubney R, Hundson J R, Garnham P C. Enzootic hepatitis or Rift Valley fever. An undescribed virus disease of sheep, cattle and man from East Africa. J Pathol Bacteriol. 1931;34:545–579. [Google Scholar]
- 7.Digoutte J P, Jouan A, Le Guenno B, Riou O, Philippe B, Meegan J, Ksiazek T G, Peters C J. Isolation of the Rift Valley fever virus by inoculation into Aedes pseudoscutellaris cells: comparison with other diagnostic methods. Res Virol. 1989;140:31–41. doi: 10.1016/s0923-2516(89)80082-2. [DOI] [PubMed] [Google Scholar]
- 8.Garin D, Peyrefitte C, Crance J M, Le Faou A, Jouan A, Bouloy M. Highly sensitive Taqman PCR detection of Puumala hantavirus. Microbes Infect. 2001;3:739–745. doi: 10.1016/s1286-4579(01)01424-1. [DOI] [PubMed] [Google Scholar]
- 9.Giorgi C. Molecular biology of phleboviruses. In: Elliott R M, editor. The Bunyaviridae. New York, N.Y: Plenum Press; 1996. pp. 105–128. [Google Scholar]
- 10.Houng H S H, Hritz D, Kanesa-Thasan N. Quantitative detection of dengue 2 virus using fluorogenic RT-PCR based on 3′-noncoding sequence. J Virol Methods. 2000;86:1–11. doi: 10.1016/s0166-0934(99)00166-4. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim M S, Turell M J, Knauert F K, Loft R S. Detection of Rift Valley fever in mosquitoes by RT-PCR. Mol Cell Probes. 1997;11:49–53. doi: 10.1006/mcpr.1996.0075. [DOI] [PubMed] [Google Scholar]
- 12.Kessler H H, Mühlbauer G, Rinner B, Stelzl E, Berger A M, Dörr H-W, Santner B, Marth E, Rabenau H. Detection of herpes simplex virus DNA by real-time PCR. J Clin Microbiol. 2000;38:2638–2642. doi: 10.1128/jcm.38.7.2638-2642.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knauert F K, Meegan J M, Jouan A, Ksiazek T G, Le Guenno B, Sarthou J L, Peters C J, Digoutte J P. Assessment of an rDNA probe filter hybridization assay for the detection of Rift Valley fever virus RNA in human serum samples from the Mauritanian epidemic. Res Virol. 1989;140:47–57. doi: 10.1016/s0923-2516(89)80084-6. [DOI] [PubMed] [Google Scholar]
- 14.Kuno G. Universal diagnostic RT-PCR protocol for arboviruses. J Virol Methods. 1998;72:27–41. doi: 10.1016/s0166-0934(98)00003-2. [DOI] [PubMed] [Google Scholar]
- 15.Lallemand F, Desire N, Rozenbaum W, Nicolas J-C, Marechal V. Quantitative analysis of human herpesvirus 8 viral load using a real-time PCR assay. J Clin Microbiol. 2000;38:1404–1408. doi: 10.1128/jcm.38.4.1404-1408.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laughlin L W, Meegan J M, Strausbaugh L J, Morens D M, Watten R H. Epidemic Rift Valley fever in Egypt: observations of the spectrum of illness. Trans R Trop Med Hyg. 1979;73:630–633. doi: 10.1016/0035-9203(79)90006-3. [DOI] [PubMed] [Google Scholar]
- 17.Linthicum K J, Davies F G, Kairo A, Bailey C L. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J Hyg (London) 1985;95:197–205. doi: 10.1017/s0022172400062434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linthicum K J, Anyamba A, Tucker C J, Kelley P W, Myers M F, Peters C J. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science. 1999;285:397–400. doi: 10.1126/science.285.5426.397. [DOI] [PubMed] [Google Scholar]
- 19.Lopez N, Muller R, Prehaud C, Bouloy M. The L protein of Rift Valley Fever virus can rescue viral ribonucleoproteins and transcribe synthetic genome-like RNA molecules. J Virol. 1995;69:3972–3979. doi: 10.1128/jvi.69.7.3972-3979.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Machida U, Kami M, Fukui T, Kazuyama Y, Kinoshita M, Tanaka Y, Kanda Y, Ogawa S, Honda H, Chiba S, Mitani K, Muto Y, Osumi K, Kimura S, Hirai H. Real-time automated PCR for early diagnosis and monitoring of cytomegalovirus infection after bone marrow transplantation. J Clin Microbiol. 2000;38:2536–2542. doi: 10.1128/jcm.38.7.2536-2542.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meegan J M, Bailey C L. Rift Valley fever. In: Monath T P, editor. The arboviruses: epidemiology and ecology. Boca Raton, Fla: CRC Press; 1988. pp. 51–76. [Google Scholar]
- 22.Meegan J M, Le Guenno B, Ksiazek T, Jouan A, Knauert F, Digoutte J P, Peters C J. Rapid diagnosis of Rift Valley fever: a comparison of methods for the direct detection of viral antigen in human sera. Res Virol. 1989;140:59–65. doi: 10.1016/s0923-2516(89)80085-8. [DOI] [PubMed] [Google Scholar]
- 23.Morrill J C, Czarniecki C W, Peters C J. Recombinant human interferon-γ modulates Rift Valley fever virus infection in the rhesus monkey. J Interferon Res. 1991;11:297–304. doi: 10.1089/jir.1991.11.297. [DOI] [PubMed] [Google Scholar]
- 24.Morrill J C, McClain D J. Epidemiology and pathogenesis of Rift Valley fever and other phleboviruses. In: Elliott R M, editor. The Bunyaviridae. New York, N.Y: Plenum Press; 1996. pp. 281–293. [Google Scholar]
- 25.Muller R, Saluzzo J F, Lopez N, Dreier T, Turell M, Smith J, Bouloy M. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am J Trop Med Hyg. 1995;53:405–411. doi: 10.4269/ajtmh.1995.53.405. [DOI] [PubMed] [Google Scholar]
- 26.Pas S D, Fries E, De Mans R A, Osterhaus A D M E, Niesters H G M. Development of a quantitative real-time detection assay for hepatitis B virus DNA and comparison with two commercial assays. J Clin Microbiol. 2000;38:2897–2901. doi: 10.1128/jcm.38.8.2897-2901.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peters C J, Reynolds J A, Slone T W, Jones D E, Stephen E L. Prophylaxis of Rift Valley fever with antiviral drugs, immune serum, an interferon inducer, and a macrophage activator. Antivir Res. 1986;6:285–297. doi: 10.1016/0166-3542(86)90024-0. [DOI] [PubMed] [Google Scholar]
- 28.Peters C J, Linthicum K J. Rift Valley fever. In: Beron G W, Steele J H, editors. Handbook series in zoonoses. Section B: viral zoonoses. Boca Raton, Fla: CRC Press; 1994. pp. 125–138. [Google Scholar]
- 29.Pittman P R, Liu C T, Cannon T L, Makuch R S, Mangiafico J A, Gibbs P H, Peters C J. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine. 2000;18:181–189. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- 30.Reed L J, Muench H. A simple method of estimating fifty percent end points. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 31.Sall A A, de A. Zanotto P M, Zeller H G, Digoutte J P, Thiongane Y, Bouloy M. Variability of the NSs protein among Rift Valley fever virus isolates. J Gen Virol. 1997;78:2853–2858. doi: 10.1099/0022-1317-78-11-2853. [DOI] [PubMed] [Google Scholar]
- 32.Sall A A, de A. Zanotto P M, Sene O K, Bouloy M. Molecular epidemiology and emergence of Rift Valley fever. Mem Inst Oswaldo Cruz. 1998;93:609–614. doi: 10.1590/s0074-02761998000500009. [DOI] [PubMed] [Google Scholar]
- 33.Sall A A, de A. Zanotto P M, Vialat P, Sene O K, Bouloy M. Origin of 1997–98 Rift Valley fever outbreak in East Africa. Lancet. 1998;352:1596–1597. doi: 10.1016/s0140-6736(05)61043-4. [DOI] [PubMed] [Google Scholar]
- 34.Sall A A, de A. Zanotto P M, Sene O K, Zeller H G, Digoutte J P, Thiongane Y, Bouloy M. Genetic reassortment of Rift Valley Fever virus in nature. J Virol. 1999;73:8196–8200. doi: 10.1128/jvi.73.10.8196-8200.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sall A A, Thonnon J, Sene O K, Fall A, Ndiaye M, Baudez B, Mathiot C, Bouloy M. Single-tube and nested reverse transcriptase-polymerase chain reaction for detection of Rift Valley fever virus in human and animal sera. J Virol Methods. 2001;91:85–92. doi: 10.1016/s0166-0934(00)00252-4. [DOI] [PubMed] [Google Scholar]
- 36.Scaramozzino N, Crance J-M, Jouan A, DeBriel D A, Stoll F, Garin D. Comparison of Flavivirus universal primer pairs and development of a rapid, highly sensitive heminested reverse transcription-PCR assay for detection of flaviviruses targeted to a conserved region of the NS5 gene sequences. J Clin Microbiol. 2001;39:1922–1927. doi: 10.1128/JCM.39.5.1922-1927.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmaljhon C. Bunyaviridae: the viruses and their replication. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott Raven Publishers; 1996. pp. 1447–1471. [Google Scholar]
- 38.Sidwell R W, Huffman J H, Barnett B B, Pifat D Y. In vitro and in vivo Phlebovirus inhibition by ribavirin. Antimicrob Agents Chemother. 1988;32:331–336. doi: 10.1128/aac.32.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Swanepoel R, Coetzer J A W. Rift Valley fever. In: Coetzer J A W, Thompson G R, Tustin R C, editors. Infectious diseases of livestock with special reference to southern Africa. Cape Town, South Africa: Oxford University Press Southern Africa; 1994. pp. 688–717. [Google Scholar]
- 40.Takeuchi T, Katsume A, Tanaka T, Abe A, Inoue K, Tsukiyama-Kohara K, Kawaguchi R, Tanaka S, Kohara M. Real-time detection system for quantification of hepatitis C virus genome. Gastroenterology. 1999;116:636–642. doi: 10.1016/s0016-5085(99)70185-x. [DOI] [PubMed] [Google Scholar]
- 41.Zeller H, Bouloy M. Infections by viruses of the families Bunyaviridae and Filoviridae. Rev Sci Tech Off Int Epizoot. 2000;19:79–91. doi: 10.20506/rst.19.1.1208. [DOI] [PubMed] [Google Scholar]