Abstract
Objective:
To examine variation in the duration of non-work-related sickness absence (NWRSA) across geographical areas and the degree to which this variation can be explained by individual and/or contextual factors.
Methods:
All first NWRSA episodes ending in 2007 and 2010 were analyzed. Individual (diagnosis, age, sex) and contextual factors (healthcare resources, socioeconomic factors) were analyzed to assess how much of the geographical variation was explained by these factors. Median NWRSA durations in quartiles were mapped by counties in Catalonia. Multilevel Cox proportional hazard regression models with episodes nested within counties were fitted to quantify the magnitude of this variation. The proportional change in variance (PCV), median hazard ratios (MHR) and interquartile hazard ratios (IHR) were calculated.
Results:
We found a geographical pattern in the duration of NWRSA, with longer duration in northwestern Catalonia. There was a small, but statistically significant, geographical variation in the duration of NWRSA, which mostly decreased after adjustment for individual factors in both women (PCV = 34.98%, MHR = 1.09, IHR = 1.13 in 2007; PCV = 34.68%, MHR = 1.11, IHR = 1.28 in 2010) and men (PCV = 39.88%, MHR = 1.10, IHR = 1.27 in 2007; PCV = 45.93%, MHR = 1.10, IHR = 1.25 in 2010); only in the case of women in 2010 was there a reduction in county-level variance due to contextual covariates (PCV = 16.18%, MHR = 1.12, IHR = 1.32).
Conclusions:
County-level variation in the duration of NWRSA was small and was explained more by individual than by contextual variables. Knowledge of geographic differences in NWRSA duration is needed to plan specific programs and interventions to minimize these differences.
Keywords: Sick leave, Occupational health, Biological characteristics, Social characteristics, Multilevel analysis
Keywords: Incapacidad temporal, Salud laboral, Características biológicas, Características sociales, Análisis multilevel
RESUMEN
Objetivo:
Examinar la variabilidad de la duración la incapacidad temporal por contingencia común (ITcc) entre áreas geográficas y el grado en que factores individuales y/o contextuales la explican.
Métodos:
Se analizaron los primeros episodios de ITcc finalizados en 2007 y 2010. Se evaluó la variabilidad geográfica explicada por factores individuales (diagnóstico, edad, sexo) y contextuales (recursos sanitarios, socioeconómicos). Se reperesentó gráficamente la duración mediana por comarcas de Cataluña. Se cuantificó la variailidad geográfica de la duración de la ITcc entre comarcas ajustando modelos de regresión multinivel de riesgos proporcionales, con episodios anidados en comarcas. Se calculó el porcentaje de cambio de la varianza (PCV), el razón de riesgo mediano (RRM) y razón de riesgo intercuartílico (RRI).
Resultados:
Se encontró un patrón geográfico en la duración de la ITcc, con mayor duración en el noroeste de Cataluña. La variabilidad geográfica de la duración de la ITcc fue, aunque no elevada, estadísticamente signifitiva, y disminuyó después de ajustar por factores de nivel individual en mujeres (PCV = 34.98%, RRM =1.09, RRI =1.13 en 2007; PCV = 34.68%, RRM =1.11, RRI =1.28 en 2010) y hombres (PCV = 39.88%, RRM =1.10, RRI =1.27 en 2007; PCV = 45.93%, RRM =1.10, RRI =1.25 en 2010); y solo en el caso de las mujeres en 2010 hubo una reducción de la varianza debido a los factores contextuales (PCV = 16.18%, RRM =1.12, RRI =1.32).
Conclusiones:
La variabilidad geográfica de la duración de la ITcc fue pequeña y explicada principalmente por los factores de nivel individual. El conocimiento de las diferencias geográficas en la duración de la ITcc es necesario para planificar programas e intervenciones específicas para reducir al mínimo estas diferencias.
Introduction
Non Work-related Sickness Absence (NWRSA) represents a high economic, social and health care burden,1–3 is determined by multiple factors and its geographical variations may be of great magnitude and could determine its duration.4,5 In addition to the inciting pathology, both individual factors, such as age and gender, and contextual factors related to the groups or geographical areas to which individuals belong, such as socioeconomic circumstances, labor market forces, the organization and quality of the health care delivery system, and the benefits structure, may play important roles as determinants of NWRSA duration.6 Several publications have already pointed out some geographical effects in the duration of NWRSA of individual factor, such as management of episodes, social security system or economic sector in the duration of NWRSA.4,6,7 But few have pointed out geographical variations of contextual factors, such as employment status, socioeconomic status, or medical practice.7–9 Assessing how much of the geographical variability in the duration of NWRSA is explained by these factors can inform resource allocation and the design of interventions and strategies to improve case management.
There is a general lack of studies that simultaneously assess both individual and contextual level factors in relation to NWRSA duration. The analysis of the NWRSA determinants is further hampered by a multiplicity of interacting causes, making it difficult to systematically approach the phenomenon. To circumvent part of these limitations, data from various sources could be combined and analyzed using multilevel statistical models.6,10–12 While a growing number of epidemiology studies apply multilevel regression analysis to the investigation of associations between individual and contextual factors on health outcomes,13 few have studied the effect of health variations between geographical regions regardless of the outcome and even fewer studying variability in survival analysis with duration.14–16
The current global financial crisis which began in 2007 affected the global economy, and spread fast around the world,17 but in Spain began to become aware from 2008 and its consequences have been extended over time to the present. The economic recession has resulted in a substantial increase in unemployment and its consequences have affected not only politically but also affected the economic, social and health system.18 For example, with the economic crisis, in Spain the labour market collapsed, creating conditions of economic hardship for many ordinary people, and tax revenues also fell sharply, leading to a budget deficit of 12% of GDP in 2009. This situation then led to budget cuts, and many areas of public spending as health system were affected.19 Understanding the geographical variations in NWRSA duration due to contextual factors taking into account two different periods in relation to the financial crisis will be more relevant knowledge.
In Catalonia, an autonomous community in Spain, the health needs of all citizens are covered through a public national health care system. NWRSA episodes are certified by primary care physicians in the national health system, and recorded electronically. Case management of a NWRSA episode, including wage replacement benefits, is performed either by the Social Security system or mutual insurance companies (mutuas) that collaborate with the Social Security system. The main responsibility for certifying a NWRSA episode rests on the primary care physicians of the social security System, who establish the start and end dates of the absence. Physicians of the mutual insurance companies can only suggest the end of an episode, based on their evaluation of the case. The existence of this electronic registry offers a unique opportunity to advance our knowledge of the determinants of NWRSA duration, and examine their temporal difference. The general aims of this study were to examine the magnitude of the geographical variability in NWRSA duration across Catalonia and which individual and/or contextual factors may explain this variability, for two specific years, 2007 and 2010, in order to analyze the influence of the financial crisis.
Methods
Data sources and variables
Data were obtained on all first sickness absence episodes ending in the years 2007 and 2010 in Catalonia, two years which may reflect two distinctly different periods in relation to the global financial crisis, which began in Spain around 2008 and currently still continues. All NWRSA episodes of more than three days’ duration are initially certified by a primary care provider of the national health service and electronically registered by the Catalonian Institute of Medical and Health Evaluations (ICAMS, by its Catalan acronym), which provides for 100% capture of all cases. Regarding individual-level data, for each episode we obtained data on start and end dates (from which we computed the duration of the episode), sex, age, 19 economic activity branches according to the International Standard Industrial Classification of All Economic Activities, Rev.4 (Available at: http://unstats.un.org/unsd/cr/registry/regcst.asp?Cl=27), 21 group diagnosis codes according to the International Classification of Diseases, 10th Revision (ICD-10), the entity responsible for case management (National Institute of Social Security or a mutual insurance company), employment status (salaried or self-employed) and 41 non-overlapping homologated territorial demarcations, also known as comarcas similar to counties (Available at: http://web.gencat.cat/ca/temes/catalunya/coneixer/).
We also obtained data on geographical (county-level) contextual variables for health resources, labor market and socioeconomic status. Specifically, we used the number of basic health units20 as a surrogate for the number of primary care centers and physicians of the National Health Service. Unemployment rates of each year by county were obtained from the Catalonian Government Statistics Institute,21 and expressed as percentages of the workforce (16 to 64 years) relative to the total population. As a measure of socioeconomic status, we obtained of each year estimates of “market share”, a comparative index of consumer power produced by a model equivalent to an average index number of variables for a municipality (population, number of telephones, cars, banks, trucks, and retail commercial activities), abstracted from the Annual Economic Yearbook of Spain.22 Each of these three geographical region indicators was expressed in tertiles. We were unable to examine in detail the effect of additional contextual factors due to difficulty in obtaining this limited information.
Statistical analysis
To examine the geographical variability of our main outcome, NWRSA duration, we first created maps of counties and inserted the unadjusted median NWRSA duration in quartiles, separately for women and men and for 2007 and 2010. To quantify the magnitude of the variability between counties we then fitted a series of multilevel Cox proportional hazard regression models with episodes nested within counties,23,24 which included Gaussian-distributed random effects by county.
For each sex and year, we first constructed an empty multilevel survival model (i.e., a model without explanatory covariates). Thereafter, we fit separate models for each of the individual-level variables and then a model including all individual level factors together in a single model. We repeated this strategy for the contextual-level variables. Finally, we fit a model with all the individual and contextual factors together. Geographical variability in NWRSA duration was quantified by the variance of the county-level random effect. To assess the magnitude of change between the empty and the other models, we computed the proportional change in variance (PVC).11 To facilitate interpretation of the geographical differences in NWRSA duration, we computed the median hazard ratio (MHR) and the interquartile hazard ratio (IHR).14,25,26 The MHR is the median value of the hazard ratio between two individuals randomly chosen from two different counties, and takes values ≥ 1, where larger values reflect greater county-level variability in NWRSA duration.10,27 Specifically, the hazard ratio is defined as the ratio of the hazards of the individual in the highest “risk” county to the individual in the lowest “risk” county.14 The IHR measures the differences in NWRSA duration between the 25% of individuals in the highest “risk” county (i.e., shorter NWRSA duration) and the 25% of individuals in the lowest “risk” county (i.e., longer NWRSA duration).25 All models were constructed in R.28
Results
In 2007 there were 580,959 first episodes of NWRSA in Catalonia, with a median duration of 8 days (25th percentile, 4 days; 75th percentile, 24 days). In 2010 there were approximately 20% fewer episodes than in 2007 (466,612 episodes), with the same median duration but a wider interquartile range (median, 8 days; 25th percentile, 3 days; 75th percentile, 33 days) (Tables 1–3).
Table 1.
Distribution and duration of first episodes of non work-related sickness absence by individual factors. Catalonia, 2007 and 2010.
| 2007 (n = 580, 959) |
2010 (n = 466,612) |
|||
|---|---|---|---|---|
| Episodes (%) | MD (P25;75) | Episodes (%) | MD (P25;75) | |
| Sex | ||||
| Male | 295,880 (50.9) | 8 (4;20) | 214,871 (46.0) | 8 (3;31) |
| Female | 285,079 (49.1) | 9 (4;27) | 251,741 (54.0) | 9 (3;36) |
| Age at onset of absence episode (years) | ||||
| 16–28 | 143,287 (24.7) | 6 (3;14) | 85,628 (18.4) | 5 (3;15) |
| 29–35 | 142,249 (24.5) | 7 (4;20) | 115,572 (24.8) | 7 (3;26) |
| 36–45 | 145,119 (25.0) | 8 (4;23) | 126,971 (27.2) | 8 (3;30) |
| >45 | 150,304 (25.9) | 14 (6;42) | 138,441 (29.7) | 15 (5;62) |
| Employment status | ||||
| Salaried workers | 552,620 (95.1) | 8 (4;22) | 441,140 (94.5) | 8 (3;29) |
| Self-employed | 28,339 (4.9) | 30 (14;62) | 25,472 (5.5) | 50 (19;137) |
| Entity managing the sick leave | ||||
| National Institute of Social Security | 274,711 (47.3) | 9 (4;28) | 154,966 (33.2) | 8 (3;33) |
| Insurance company | 306,248 (52.7) | 8 (4;21) | 311,646 (66.8) | 8 (3;33) |
| Economic activity sector | ||||
| Agriculture, forestry and fishing | 4,907 (0.8) | 13 (5;41) | 2,503 (0.5) | 23 (7;75) |
| Mining and quarrying | 901 (0.2) | 7 (4;17) | 579 (0.1) | 8 (4;36) |
| Manufacturing | 128,662 (22.1) | 8 (4;20) | 78,961 (16.9) | 8 (3;29) |
| Electricity, gas, steam and air conditioning | 1,006 (0.2) | 10 (5;24) | 685 (0.1) | 11 (5;33) |
| Water supply; sewerage, waste management | 4,527 (0.8) | 9 (4;26) | 4,375 (0.9) | 8 (3;28) |
| Construction | 60,013 (10.3) | 8 (4;22) | 35,575 (7.6) | 11 (4;51) |
| Wholesale and retail trade; repair of vehicles | 102,063 (17.6) | 8 (4;23) | 79,206 (17.0) | 8 (3;33) |
| Transportation and storage | 28,333 (4.9) | 9 (4;25) | 24,767 (5.3) | 10 (4;40) |
| Accommodation and food service activities | 24,856 (4.3) | 11 (5;31) | 23,941 (5.1) | 12 (4;52) |
| Information and communication | 9,782 (1.7) | 8 (4;19) | 9,800 (2.1) | 7 (3;22) |
| Financial and insurance activities | 8,914 (1.5) | 9 (5;27) | 6,821 (1.5) | 9 (4;32) |
| Real estate activities | 2,903 (0.5) | 10 (5;31) | 2,153 (0.5) | 15 (5;60) |
| Professional, scientific and technical activities | 20,781 (3.6) | 8 (4;20) | 18,395 (3.9) | 8 (3;30) |
| Administrative and support service activities | 45,371 (7.8) | 9 (4;25) | 41,341 (8.9) | 8 (3;35) |
| Public administration and defense | 68,290 (11.8) | 9 (4;26) | 40,145 (8.6) | 8 (4;25) |
| Education | 14,501 (2.5) | 9 (5;23) | 17,962 (3.8) | 8 (4;30) |
| Human health and social work activities | 31,209 (5.4) | 9 (4;28) | 53,069 (11.4) | 8 (3;29) |
| Arts, entertainment and recreation | 6,208 (1.1) | 8 (4;24) | 6,892 (1.5) | 8 (3;34) |
| Other service activities | 17,732 (3.1) | 10 (5;30) | 19,442 (4.2) | 11 (4;47) |
| Total | 580,959 (100.0) | 8 (4;24) | 466,612 (100.0) | 8 (3;33) |
MD: Median duration of the first non work-related sickness absence episodes, in days. P25,75: 25th and 75th percentiles of sickness absence duration, in days.
Table 3.
Distribution and duration of first episodes of non work-related sickness absence by contextual factors. Catalonia, 2007 and 2010.
| 2007 (n = 580, 959) |
2010 (n = 466,612) |
|||
|---|---|---|---|---|
| Episodes (%) | MD (P25;75) | Episodes (%) | MD (P25;75) | |
| Number of basic health areas | ||||
| 2007 | ||||
| ≤ 7 | 96,722 (16.6) | 8 (4;23) | ||
| (7–14] | 98,138 (16.9) | 8 (4;21) | ||
| ≥ 15 | 386,099 (66.5) | 9 (4;24) | ||
| 2010 | ||||
| ≤ 7 | 77,479 (16.6) | 10 (4;40) | ||
| (7–14] | 81,942 (17.6) | 8 (3;34) | ||
| ≥ 15 | 307,191 (65.8) | 8 (3;32) | ||
| Unemployment rate (%) | ||||
| 2007 | ||||
| ≤ 3.6 | 18,131 (3.1) | 9 (5;25) | ||
| (3.6–5.0] | 94,269 (16.2) | 8 (4;23) | ||
| > 5.0 | 468,559 (80.7) | 8 (4;24) | ||
| 2010 | ||||
| ≤ 9.2 | 13,733 (2.9) | 11 (4;38) | ||
| (9.2–11.6] | 225,859 (48.4) | 8 (3;32) | ||
| > 11.6 | 227,020 (48.7) | 9 (3;35) | ||
| Market share (Euros) | ||||
| 2007 | ||||
| ≤ 1,836.80 | 12,584 (2.2) | 9 (5;26) | ||
| (13,836.8–73,561.8] | 69,100 (11.9) | 8 (4;23) | ||
| > 73,561.8 | 499,275 (85.9) | 8 (4;24) | ||
| 2010 | ||||
| ≤ 11,737.7 | 11,101 (2.4) | 12 (5;42) | ||
| (11,737.7–78,457.3] | 55,240 (11.8) | 10 (4;40) | ||
| > 78,457.3 | 400,271 (85.8) | 8 (3;33) | ||
| Total | 580,959 (100.0) | 8 (4;24) | 466,612 (100.0) | 8 (3;33) |
MD: Median duration of the first non work-related sickness absence episodes, in days. P25,75: 25th and 75th percentiles of sickness absence duration, in days.
Although the number of episodes in 2010 was slightly higher among women than men (251,741 vs. 214,871), median duration was the same by sex in both years (8 days). The number and duration of NWRSA episodes increased with age. Episodes lasted longer among self-employed workers (median, 30 days in 2007 and 50 days in 2010), as compared to salaried workers (median, 8 days in both 2007 and 2010). Regarding economic activity, the manufacturing category, followed by wholesale and retail trade reported the greatest number of episodes, although agriculture, forestry and fishing had the longest duration in both years (Table 1). Musculoskeletal and respiratory disorders, representing over 20% of all cases in both years, were the most frequent causes of NWRSA, but neoplasms had the longest duration, with pronounced differences as compared to other groups (Table 2).
Table 2.
Distribution and duration of first episodes of non work-related sickness absence by the 21 group diagnosis codes according to the International Classification of Diseases, 10th Revision (ICD-10). Catalonia, 2007 and 2010.
| 2007 (n = 580, 959) |
2010 (n = 466,612) |
|||
|---|---|---|---|---|
| Episodes (%) | MD (P25;75) | Episodes (%) | MD (P25;75) | |
| II Neoplasms | 5,894 (1.0) | 32 (12;92) | 7,722(1.7) | 74 (18;302) |
| I Infectious | 68,552 (11.8) | 4 (3;6) | 53,310 (11.4) | 3 (2;5) |
| III Hematology | 935 (0.2) | 29 (12;67) | 809 (0.2) | 41 (15;95) |
| IV Endocrinology | 1,754 (0.3) | 21 (10;50) | 1,661 (0.4) | 25 (9;64) |
| V Psychiatric | 40,958 (7.1) | 30 (1239) | 35,413 (7.6) | 44 (13;138) |
| VI Neurology | 6,219 (1.1) | 16 (430) | 6,279 (1.3) | 15 (3;65) |
| VII Ophthalmology | 7,532 (1.3) | 9 (530) | 5,733 (1.2) | 9 (4;26) |
| VIII Otolaryngology | 9,493 (1.6) | 8 (4;17) | 6,472 (1.4) | 7 (3;15) |
| IX Cardiovascular | 9,556 (1.6) | 25 (11;60) | 8,874 (1.9) | 30 (11;103) |
| X Respiratory | 145,984 (25.1) | 5 (3;8) | 91,724 (19.7) | 4 (3;7) |
| XI Digestive | 23,733 (4.1) | 8 (4;29) | 23,957 (5.1) | 5 (2;23) |
| XII Dermatology | 7,903 (1.4) | 11 (5;22) | 5,503 (1.2) | 11 (5;25) |
| XIII Musculoskeletal | 118,235 (20.4) | 15 (7;42) | 99,693 (21.4) | 17 (7;61) |
| XIV Genitourinary | 15,921 (2.7) | 10 (5;21) | 14,435 (3.1) | 9 (4;21) |
| XV Pregnancy-puerperium | 8,357 (1.4) | 23 (1037) | 7,901 (1.7) | 27 (9;77) |
| XVI Perinatal period | 279 (0.0) | 11 (4;44) | 222 (0.0) | 18 (4;45) |
| XVII Congenital anomaly | 433 (0.1) | 26 (11;71) | 442 (0.1) | 25 (11;71) |
| XVIII Not classified | 30,521 (5.3) | 6 (3;16) | 30,689 (6.6) | 5 (2;15) |
| XIX Traumatology | 49,808 (8.6) | 17 (8;43) | 39,348 (8.4) | 22 (934) |
| XX External causes | 8,371 (1.4) | 19 (8;43) | 8,185 (1.8) | 21 (8;54) |
| XXI Risk factors | 20,521 (3.5) | 19 (8;43) | 18,240 (3.9) | 25 (931) |
| Total | 580,959 (100.0) | 8 (4;24) | 466,612 (100.0) | 8 (333) |
MD: Median duration of the first non work-related sickness absence episodes, in days. P25,75: 25th and 75th percentiles of sickness absence duration, in days. ICD: International Classification of Diseases.
Figure 1 depicts the differences in unadjusted median duration of NWRSA in quartiles of days for the 41 counties in Catalonia by sex and year. There was a consistent geographical pattern of longer durations in northwestern Catalonia. By gender, there appeared to be less variability in NWRSA duration in 2007 as compared to 2010, reflected in a smaller interquartile range.
Figure 1.
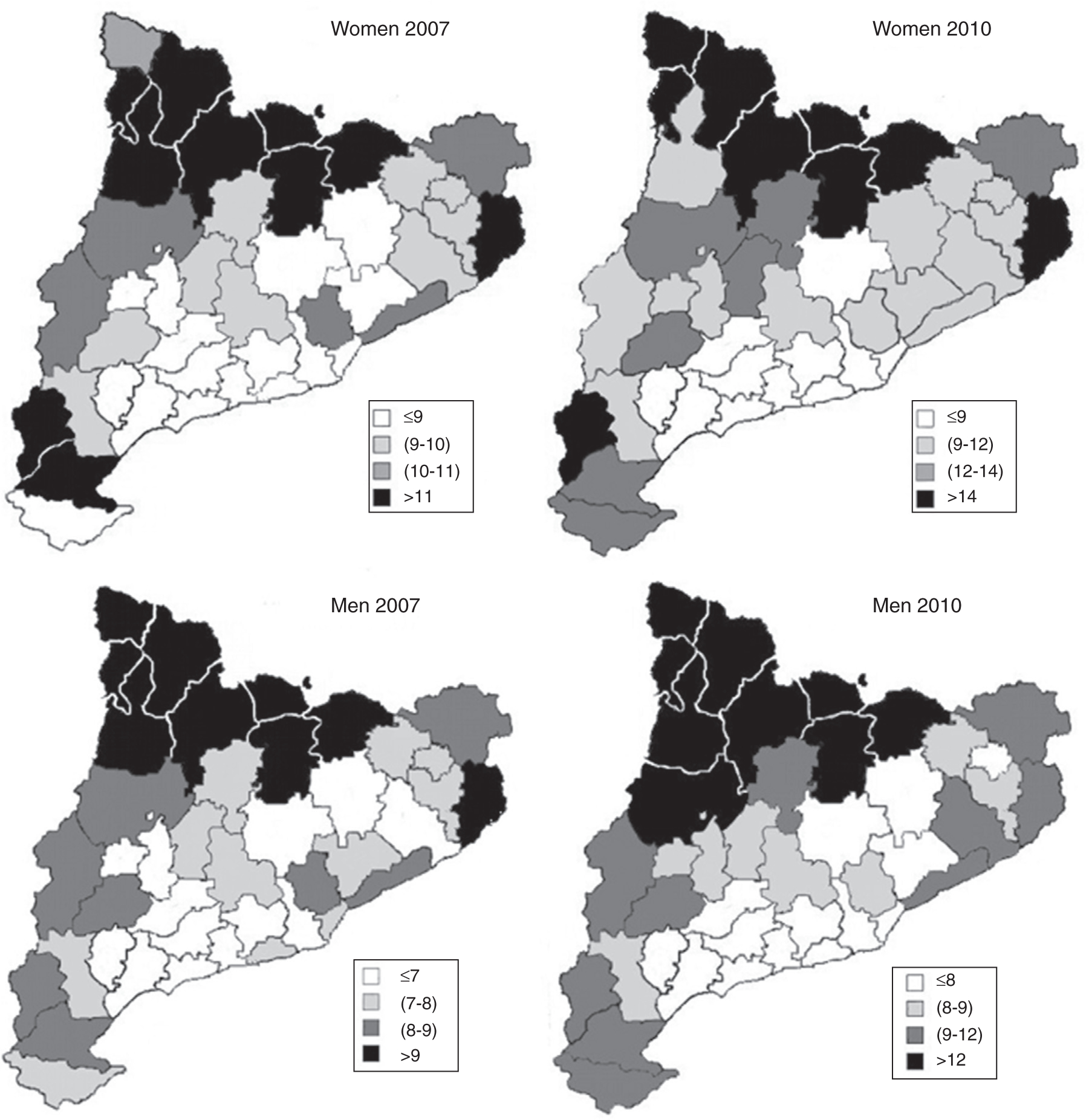
Geographical distribution of non work-related sickness absence (median duration) by counties, by sex and year. Catalonia, 2007 and 2010.
A statistically significant county-level variance was observed in all of the fitted regression models (Table 4). Overall, as shown by empty models estimated separately for each year and sex, there were no major differences between women and men in either year, except for slightly lower geographical variability in NWRSA duration among women in 2007 (county-level variance, 0.0128; MHR = 1.11 and IHR = 1.30), which subsequently increased in 2010. The low MHR and IHR values (i.e., close to 1.0) in women and men by year suggest there was small county-level variability.
Table 4.
Variation in the duration of non albework-related sickness absence episodes between counties, by sex and year. Catalonia, 2007 and 2010.
| Women |
Men |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2007 |
2010 |
2007 |
2010 |
|||||||||||||
| County variance* | PCV | MHR | IHR | County variance* | PCV | MHR | IHR | County variance* | PCV | MHR | IHR | County variance* | PCV | MHR | IHR | |
| Empty model | 0.0128 | 1.11 | 1.30 | 0.0174 | 1.13 | 1.36 | 0.0173 | 1.13 | 1.36 | 0.0172 | 1.13 | 1.35 | ||||
| Individual factors | ||||||||||||||||
| Age | 0.0121 | 5.47 | 1.11 | 1.29 | 0.0166 | 4.05 | 1.13 | 1.35 | 0.0161 | 6.94 | 1.13 | 1.34 | 0.0143 | 16.86 | 1.13 | 1,32 |
| Employment status | 0.0115 | 10.26 | 1.11 | 1.28 | 0.0135 | 21.97 | 1.12 | 1.31 | 0.0155 | 10.40 | 1.13 | 1.33 | 0.0134 | 22.09 | 1.12 | 1,31 |
| Entity managing the sick leave | 0.0125 | 2.34 | 1.11 | 1.29 | 0.0175 | −1.16 | 1.13 | 1.36 | 0.0168 | 2.89 | 1.13 | 1.35 | 0.0172 | 0.00 | 1.13 | 1,35 |
| Economic activity sector | 0.0120 | 6.25 | 1.11 | 1.29 | 0.0159 | 8.09 | 1.13 | 1.34 | 0.0155 | 10.40 | 1.13 | 1.33 | 0.0141 | 18.02 | 1.13 | 1,32 |
| Diagnosis group | 0.0104 | 18.75 | 1.10 | 1.27 | 0.0134 | 22.54 | 1.12 | 1.31 | 0.0137 | 20.81 | 1.12 | 1.31 | 0.0144 | 16.28 | 1.12 | 1,32 |
| All individual factors | 0.0083 | 34.92 | 1.09 | 1.23 | 0.0113 | 34.68 | 1.11 | 1.28 | 0.0104 | 39.88 | 1.10 | 1.27 | 0.0093 | 45.93 | 1.10 | 1.25 |
| Contextual factors | ||||||||||||||||
| Number of basic health areas | 0.0128 | 0.00 | 1.11 | 1.30 | 0.0147 | 15.03 | 1.12 | 1.32 | 0.0172 | 0.58 | 1.13 | 1.35 | 0.0167 | 2.91 | 1.12 | 1,35 |
| Unemployment rate | 0.0127 | 0.78 | 1.11 | 1.30 | 0.0167 | 3.47 | 1.13 | 1.35 | 0.0159 | 8.09 | 1.13 | 1.34 | 0.0178 | −3.49 | 1.13 | 1,36 |
| Market share | 0.0120 | 6.25 | 1.11 | 1.29 | 0.0131 | 24.28 | 1.12 | 1.30 | 0.0166 | 4.05 | 1.13 | 1.35 | 0.0159 | 7.56 | 1.11 | 1,34 |
| All contextual factors | 0.0131 | −2.34 | 1.12 | 1.30 | 0.0145 | 16.18 | 1.12 | 1.32 | 0.0167 | 3.47 | 1.13 | 1.35 | 0.0172 | 0.00 | 1.11 | 1.35 |
| Individual and contextual factors | 0.0086 | 32.50 | 1.09 | 1.24 | 0.0107 | 38.15 | 1.10 | 1.27 | 0.0104 | 39.88 | 1.10 | 1.27 | 0.0098 | 42.79 | 1.10 | 1.26 |
PCV: Proportional change of variance (%); MHR: Median hazard ratio; IHR: Interquartile hazard ratio
Statistically significant variance.
This small county-level variability decreased further when individual-level factors were included in the models (Table 4). In 2007, the individual-level variable that produced the greatest decrease in county-level variance was diagnosis code (PVC = 18.75% for women and 20.81% for men). In contrast, in 2010, employment status for both genders (PVC = 21.97% for women and 22.09% for men) and diagnosis code in the case of women (PVC = 22.54%) decreased the most variability. When all individual-level variables were introduced into the models, the decreases in county variance ranged from 34.68% to 45.93%, both in 2010 in women and men, respectively. The MHR and the IHR values differed only slightly with respect to the empty model.
In the models that included only contextual covariates, most decreases in county-level variance were below 10%, except for women in 2010, where the number of basic health units (PVC = 15.03%), market share (PVC = 24.28%) and the model that included all contextual factors (PVC = 16.18%) were higher.
Finally, when both individual- and contextual-level factors were included in the models, the PVC ranged from 32.50% (women in 2007) to 42.79% (men in 2010), and the MHR and IHR were slightly reduced when compared to the empty models for each gender and year.
Discussion
Our study is the first examining the geographic variability of the duration of NWRSA and the first to simultaneously study both individual and contextual factors as a potential explanatory factors of this geographical variability. Furthermore, this study has allowed us to examine the variation of geographical variability in two distinctly different periods in relation to the financial crisis. We found small, but significant, geographical variability in NWRSA duration in Catalonia for both sexes and study years, with longer durations in northwestern Catalonia. This variability was mainly determined by individual-level variables, in particular diagnosis (understandable given the broad range of pathologies leading to lost work-time),29 and employment status. Contextual covariates (i.e., number of basic health units and market share) only seemed to have an effect in women, among whom there was a reduction in county-level variance in 2010.
The effect of socioeconomic and labor market factors on the NWRSA duration is feasible. For example, factors related to the population density or the average travel distance for individuals to access health services could be affecting NWRSA duration. High unemployment, especially during the current global financial crisis, could result in fewer NWRSA episodes but of longer duration because workers may avoid taking work leave unless a condition is quite serious. In a previous study conducted in Norway, Krosktad and colleagues,8 using multilevel analysis, provided evidence that these contextual factors can affect individual NWRSA duration in persons who end up on permanent disability. They concluded that regions with high unemployment, low socioeconomic status, population decline and long commuting distance to public services were at a greater risk of disability. However, in our study, contextual factors seemed to have little influence on county-level variance, possibly due in part to residual confounding or unmeasured variables. In a separate study of sickness absence due to mental health diagnoses, Bratberg and colleagues30 also used a multilevel Cox model with incorporation of contextual factors similar to ours, such as unemployment rate and percentage of aging population, along with a deprivation index reflecting regional living conditions, among others. They found a marginal effect of several contextual factors on risk of progression to permanent disability in women but not men, as in our results, but did not further analyze the variability of these factors.
Among the individual-level determinants, the inciting diagnosis is one of the most important.31,32 In our study, the importance of the diagnosis was reflected in the larger amount of geographical variability explained by diagnosis, which was not surprising given the broad range of pathologies leading to lost work-time. Other variables like age, sex and the state of current or previous health also have an effect.33 Some of these factors (e.g., age, sex, occupation and employment status), are not modifiable, leaving us unable to influence them. But others, such as the diagnosis and entity managing the sickness absence, are amenable to interventions from a public administration standpoint.34,35 The diagnosis variable reflects not only the pathology that initiated the sickness absence episode, but also current approaches to its clinical management (including waiting times for diagnostic evaluations or specific procedures, use of evidence-based treatment guidelines, and return to work practices), all of which can affect NWRSA duration, but whose efficiencies could be improved.36 Likewise, sharing of information on best case managing practices among those entities responsible for handling NWRSA episodes could be promoted.
Another aspect that we should mention was the differences that we found among women and men. In this sense, we must consider the significant gender inequalities in terms of employment and working conditions, and in terms of reconciling family life, that yet exist in Spain, and that it could be influencing the differences observed here.37
Largely, NWRSA duration is a consequence of the effect of prognostic factors that act on its prevalence, with some factors lengthening and others reducing it.3 Despite individual characteristics explained a large proportion of the geographic variability, they still did not fully explain differences between similar individuals among counties. And, some residual geographical variation in NWRSA duration persisted after adjusting for both individual and contextual levels variables. One of the possible explanations for the residual variability in our study, we should consider geographic differences in the proportion of populations with special clinical susceptibility and fragility, who are older or have significant functional limitations, or are in major need of health care resources.
Another factor to consider, and rarely addressed in the sickness absence literature, is geographic differences in medical practice. The medical practice directly affects the diagnosis, but it may also have contextual level effects related to the healthcare resources in the county, efficiencies in the delivery of medical services, the nature of the physician-patient relationship in urban versus rural areas or variations in medical practice patterns.37 Differences in administrative structures, waiting lists for non-urgent procedures, the level of computer and other technical support and in tracking of NWRSA episodes could also be considered.38,39 We had little information on these variables to be able to investigate their effect in detail. In addition to the number of basic health units, we did, however, explore some other county-level health resources, such as number of private sector outpatient centers in each public health sector, and number of hospital beds per 1,000 population, but none of these showed significant effects in preliminary analyses and therefore were not included in the final models (data not shown). The effect medical practice variability on geographical differences in sickness absence patterns will need to be examined in future studies.
There are some methodological considerations to take into account when interpreting our findings. First, information on individual behavioral risk factors, comorbidities and health care utilization, all of this could potentially affect NWRSA duration, was not available. Second, most NWRSA incidence and duration studies that have used multilevel models have included individual and work-related factors,40,41 but we did not have much information on the latter to compare our findings with that research. Moreover, we did not know the reason for case closure of each NWRSA episode, which could have allowed more insight on NWRSA duration, as we would have been able to analyze whether the case was closed due to cure or improvement of the worker, death or default, or a shift into permanent disability status.42
In summary, NWRSA is a major and complex public health issue that carries a significant economic burden,2,3 and has negative effects for employees, employers and society in general.1 Because of its complexity, the theoretical framework of its determinants should take into account the diverse and overlapping levels considered influential, including inciting medical diagnosis, individual factors, work-related variables, and aspects related to healthcare services, socioeconomics and sociopolitical factors.43,44 In this regard, our study contributes to a better understanding of sources of variability in the duration of sickness absence by using multilevel analysis that allows simultaneous examination of the effects of many of these individual and contextual level factors. Further studies are necessary and encouraged, aimed at better conceptualizing and assessing these effects in terms of health care, social system and labor market legislation.45 Among these, one could examine variations in medical practice, as this could identify factors associated with inefficiencies in delivery of services, along with possible misuse or overuse of sickness absence benefits.37 Although the data derive from Catalonia, our methodological approach and results are generalizable to similar situations in sickness absence research in other countries. Increasing our knowledge on the role of these factors in determining the geographic differences in NWRSA duration will also increase our ability to design actions to minimize regional differences.
What is already known on this subject
Non work-related sickness absence (NWRSA) varies according to different individual and contextual factors.
These factors have geographical effects on the duration of NWRSA.
Prior studies have analyzed these effects due to individual factors, but few or none have examined those due to contextual factors.
What this study adds
This study contributes to a better understanding of sources of variability in NWRSA duration.
Geographical variability in NWRSA duration was found. Northwest Catalonia had longer NWRSA durations.
This variability was mainly explained by individual factors, but there was also some effect in women in 2010 due to contextual factors.
Acknowledgments
The authors would like to thanks the Institut Català d’Avaluacions Mèdiques i Sanitàries for providing the database. The authors would like to thank Ana María García for his help with the writing of the manuscript.
Funding
This study was partially funded by grants from the Fondo de Investigación Sanitaria (PI11/01470), the Canadian Institutes for Health Research (CIHR) and the Institut Català d’Avaluacions Mèdiques i Sanitàries.
Footnotes
Conflicts of interest
None declared.
References
- 1.Alexanderson K Sickness absence: a review of performed studies with focused on levels of exposure and theories utilized. Scand J Soc Med. 1998;26:241–9. [DOI] [PubMed] [Google Scholar]
- 2.Alexanderson K, Norlund A. Swedish Council on technology assessment in health care (SBU). Chapter 12. Future need for research. Scand J Public Health Suppl. 2004;63:256–8. [DOI] [PubMed] [Google Scholar]
- 3.Block FS, Prins R, editors. Who returns to work and why? A six-country study on work incapacity and reintegration. New Brunswick. New Jersey: Transaction Publishers; 2001. [Google Scholar]
- 4.Ballesteros M, Serra C, Martínez JM, et al. Comparación del coste de la incapacidad temporal por contingencia común en 2006 entre las provincias de Barcelona y Madrid. Rev Esp Salud Pública. 2009;83:453–61. [DOI] [PubMed] [Google Scholar]
- 5.Roelen CAM, Koopmans PC, Anema JR, et al. Recurrence of medically certified sickness absence according to diagnosis: a sickness absence register study. J Occup Rehabil. 2010;20:113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torá I, Martínez JM, Delclos J, et al. Duración de los episodios de incapacidad temporal por contingencia común según regiones sanitarias en Cataluña. Rev Esp Salud Pública. 2010;84:61–9. [DOI] [PubMed] [Google Scholar]
- 7.Karlsson NE, Casrtensen JM, Gjesdal S, et al. Risk factors for disability pension in a population-based cohort of men and women on long-term sick leave in Sweden. Eur j Public Health. 2008;18:224–31. [DOI] [PubMed] [Google Scholar]
- 8.Krosktad S, Magnus P, Skrondal A, et al. The importance of social characteristics of communities for the medically based disability pension. Eur J Public Health. 2004;14:406–12. [DOI] [PubMed] [Google Scholar]
- 9.Virtanen M, Kivimakï M, Elovainio M, et al. Local economy and sickness absence: a panel data study. Health Econ. 2005;14:25–31.15386668 [Google Scholar]
- 10.Merlo J Multilevel analytical approaches in social epidemiology: measures of health variation compared with traditional measures of association. J Epidemiol Community Health. 2003;57:550–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merlo J, Chaix B, Yang M, et al. A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiol Community Health. 2005;59:1022–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–92. [DOI] [PubMed] [Google Scholar]
- 14.Chaix B, Rosvall M, Merlo J. Assessment of the magnitude of geographical variations and socioeconomic contextual effects on ischeamic heart disease mortality: a multilevel survival analysis of a large Swedish cohort. J Epidemiol Community Health. 2007;61:349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merlo J, Chaix B, Yang M, et al. A brief conceptual of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59: 443–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merlo J, Yang M, Chaix B, et al. A brief conceptual tutorial on multilevel analysis in sosial epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Community Health. 2005;59:729–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai FJ, Chan CC. The impact of the 2008 financial crisis on psychological work stress among financial workers and lawyers. Int Arch Occup Environ Health. 2011;84:445–52. [DOI] [PubMed] [Google Scholar]
- 18.Astell-Burt T, Feng X. Health and the 2008 economic recession: evidence from the United Kingdom. Plos One. 2013;8:e56674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Day P Spain underperformed euro zone for 1st time in 2010. Reuter’s. 2010. [Google Scholar]
- 20.Decret 105/2005. Diari Oficial de la Generalitat de Catalunya. Decret 105/2005, de 31 de maig, de delimitació de les regions sanitàries i dels sectors sanitaris del Servei Català de Salut. DOGC Núm. 4397–2.June.2005. [Google Scholar]
- 21.IDESCAT (Institut d’Estadística de Catalunya). Generalitat de Catalunya. Available at: www.idescat.cat. Accessed May 23, 2013.
- 22.La Caixa Estudios y Análisis Económico. Anuario Económico de España. Available at: http://www.anuarioeco.lacaixa.comunicacions.com/java/X?cgi=caixa.anuari99.util.ChangeLanguage&lang=esp. Accessed Jul 09, 2014.
- 23.Oakes DA. Frailty models for multilevel event times. In: Lein JP, Goel PK, editors. In survival data, state of the art. Dordrecht: Kluwer Academic Publishers; 1992. [Google Scholar]
- 24.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. Springer Verlag: New York; 2000. [Google Scholar]
- 25.Chaix B, Rosvall M, Merlo J. Recent increase of neighborhood socioeconomic effects on ischemic heart disease mortality: a multilevel survival analysis of two large Swedish cohorts. Am J Epidemiol. 2007;165:22–6. [DOI] [PubMed] [Google Scholar]
- 26.Lian M, Schootman M, Doubeni CA, et al. Geographic variation in colorectal cancer survival and the role of small-area socioeconomic deprivation: a multilevel survival analysis of the NIH-AARP diet and health study cohort. Am J Epidemiol. 2011;174:828–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161:81–8. [DOI] [PubMed] [Google Scholar]
- 28.Therneau T Survival analysis, including penalized likelihood. Package ‘survival’, version 2.36–14; 2012. Available at: http://cran.r-project.org/web/packages/survival/survival.pdf. Accessed Jul 09, 2014. [Google Scholar]
- 29.Delcós J, García S, López JC, et al. Duración de la incapacidad temporal por contingencia común por grupos diagnósticos. Arch Prev Riesgos Labor. 2010;13:180–7. [Google Scholar]
- 30.Bratberg E, Gjesdal S, Maeland JG. Sickness absence with psychiatric diagnoses: individual and contextual predictors of permanent disability. Health Place. 2009;15:308–14. [DOI] [PubMed] [Google Scholar]
- 31.Maeland JG, Havik OE. Return to work after a myocardial infarction: the influence of background factors, work characteristics and illness severity. Scand J Soc Med. 1986;14:183–95. [DOI] [PubMed] [Google Scholar]
- 32.Reiso H, Nygård JF, Jørgensen GS, et al. , Bruusgaard D. Back to work: predictors of return to work among patients with back disorders certified as sick: a two-year follow-up study. Spine (phila Pa 1976). 2003;28:1468–73. [DOI] [PubMed] [Google Scholar]
- 33.Marmot M, Feeney A, Shipley M, et al. Sickness absence as a measure of health status and functioning: from the UK Whitehall II study. J Epidemiol Community Health. 1995;49:124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benavides FG, Torá I, Martínez JM, et al. Evaluación de la gestión de los casos de incapacidad temporal por contingencia común de más de 15 días en Cataluña. Gac Sanit. 2010;24:215–9. [DOI] [PubMed] [Google Scholar]
- 35.Delclós J, Gimeno D, Torá I, et al. Distribución de la duración de la incapacidad temporal por contingencia común por diagnóstico médico (Cataluña, 2006–2008). Gac Sanit. 2013;21:81–3. [DOI] [PubMed] [Google Scholar]
- 36.Allebeck P, Mastekaasa A. Swedish council on technology assessment in health care (SBU). Chapter 3. Causes of sickness absence: research approaches and explanatory models. Scand J Public Health Suppl. 2004;63:36–43. [DOI] [PubMed] [Google Scholar]
- 37.Campos-Serna J, Ronda-Pérez E, Artazcoz L, et al. Desigualdades de género en salud laboral en España. Gac sanit. 2012;26:343–51. [DOI] [PubMed] [Google Scholar]
- 38.Peiró S, Bernal-Delgado E. Variaciones de la práctica médica: apoyando la hipótesis nula en tiempos revueltos. Rev Esp Salud Pública. 2012;86:213–7. [DOI] [PubMed] [Google Scholar]
- 39.von Knorring M, Sundberg L, Löfgren A, et al. Problems in sickness certification of patients: a qualitative study on views of 26 physicians in Sweden. Scand J Prim Health Care. 2008;26:22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marnetoft SU, Selander J, Akerström B, et al. A comparison of perceived health, attitudes to work, leisure time, and social welfare systems among people in a rural area in the north of Sweden and among people in the city of Stockholm. Work. 2007;28:153–64. [PubMed] [Google Scholar]
- 41.Labriola M Conceptual framework of sickness absence and return to work, focusing on both the individual and the contextual level. Work. 2008;30:377–87. [PubMed] [Google Scholar]
- 42.Labriola M, Lund T, Christensen KB, et al. Multilevel analysis of individual and contextual factors as predictors of return to work. J Occup Environ Med. 2006;48:1181–8. [DOI] [PubMed] [Google Scholar]
- 43.Duran X, Martínez JM, Benavides FG. Occupational facors associated with the potential years of working life lost due to a non-work related permanent disability. Work. 2013;45:305–9. [DOI] [PubMed] [Google Scholar]
- 44.Loisel P, Côté P, Durand MJ, et al. Training the next generation of researchers in work disability prevention: the Canadian Work Disability Prevention CIHR Strategic Training Program. J Occup Rehabil. 2005;15:273–84. [DOI] [PubMed] [Google Scholar]
- 45.Pransky G, Gatchel R, Linton SJ, et al. Improving return to work research. J Occup Rehabil. 2005;15:453–7. [DOI] [PubMed] [Google Scholar]


