Abstract
Objective
We evaluated the short-term effects of exposure to cleaning products on lung function and respiratory symptoms among professional cleaning women.
Methods
Twenty-one women with current asthma and employed as professional cleaners participated in a 15-day panel study. During 312 person-days of data collection, participants self-reported their use of cleaning products and respiratory symptoms in daily diaries and recorded their forced expiratory volume in 1 s (FEV1) and peak expiratory flow (PEF) three times per day using a handheld spirometer. We evaluated associations of cleaning product use with upper and lower respiratory tract symptoms using Poisson mixed regression models and with changes in FEV1 and PEF using linear mixed regression analyses.
Results
Participants reported using an average of 2.4 cleaning products per day, with exposure to at least one strong irritant (eg, ammonia, bleach, hydrochloric acid) on 56% of person-days. Among participants without atopy, lower respiratory tract symptoms were associated with the use of hydrochloric acid and detergents. Measurements of FEV1 and PEF taken in the evening were 174 mL (95% CI 34 to 314) and 37 L/min (CI 4 to 70), respectively, lower on days when three or more sprays were used. Evening and next morning FEV1 were both lower following the use of hydrochloric acid (−616 and −526 mL, respectively) and solvents (−751 and −1059 mL, respectively). Diurnal variation in FEV1 and PEF increased on days when ammonia and lime-scale removers were used.
Conclusions
The use of specific cleaning products at work, mainly irritants and sprays, may exacerbate asthma.
INTRODUCTION
In the past decade, numerous studies have reported on associations between cleaning-related exposures and asthma and have suggested an important role for the exposure to airway irritants.1–3 Results from recent epidemiological and clinical studies have shown potential links between occupational cleaning-related exposures and exacerbation of existing asthma.4–7 Findings from studies of short-term respiratory health effects following cleaning-related exposures have improved our understanding of how exposures to cleaning products may affect respiratory symptoms and lung function. In a workforce-based study of the short-term effects of cleaning products on asthma symptoms among domestic cleaning workers with pre-existing chronic bronchitis or asthma, Medina-Ramon et al8 concluded that exposure to irritant products may exacerbate respiratory conditions. Similarly, a 12-week prospective study conducted among female homemakers with asthma showed an increased risk of lower respiratory tract symptoms (LRTS) associated with cleaning activities, though no link was found with specific cleaning exposures.9 A case series study of 13 cleaners with and without bronchial hyper-responsiveness showed that inhalation challenge with hypochlorite bleach, even at concentrations below the 8 h occupational exposure standard, can induce a significant decrease in forced expiratory volume in 1 s (FEV1).10 Likewise, exposure to chlorine, which is released when using certain cleaning products,11 has been associated with short-term decrements in lung function among individuals with and without airways hyper-responsiveness.12 13
The Epidemiological Study of Asthma Risk in Cleaning Workers (EPIASLI-2) cohort provided a unique opportunity to assess the relationship between occupational exposure to cleaning products and short-term changes in FEV1 and peak expiratory flow (PEF), objective measures of obstructive respiratory impairment, as well as to evaluate upper respiratory tract symptoms (URTS) and LRTS among female cleaning workers with pre-existing asthma. Nesting our study in the EPIASLI-2 cohort, we conducted a panel study of 21 professional cleaners with asthma in order to evaluate the temporal sequence of short-term respiratory health effects following occupational cleaning product exposures.
METHODS
Study population and design
We recruited participants with asthma from a case–control study of asthma among professional cleaning workers in Barcelona, Spain14 (figure 1). Study design and methods for the study, including the cross-sectional survey and nested case–control study have been described previously.15 16 Briefly, in 2008, 761 cleaning workers employed in 37 cleaning companies in Barcelona completed self-administered questionnaires that included basic information about their work tasks and respiratory health. From this population, we identified 70 adults with asthma symptoms in the previous year or with a history of asthma and recruited those still employed as cleaning workers and who still reported having symptoms or a history of asthma to participate in a case–control study that included a detailed clinic visit.14 Forty-two of the 70 respondents completed the clinic visit and of these, 23 (55%) agreed to participate in a 2-week panel study. These 23 participants each completed a 15-day diary designed to be filled out every night before going to sleep. Following 15 days of data collection, all participants returned the data collection materials to our research centre by mail. After data quality control, we excluded one female participant, due to the poor quality of information, and the only male respondent, which resulted in a final study population of 21 female participants reporting almost complete information in the diaries: 312 person-days (99%). The study was approved by the ethics committee of Parc de Salut Mar, Barcelona and all participants provided written informed consent.
Figure 1.
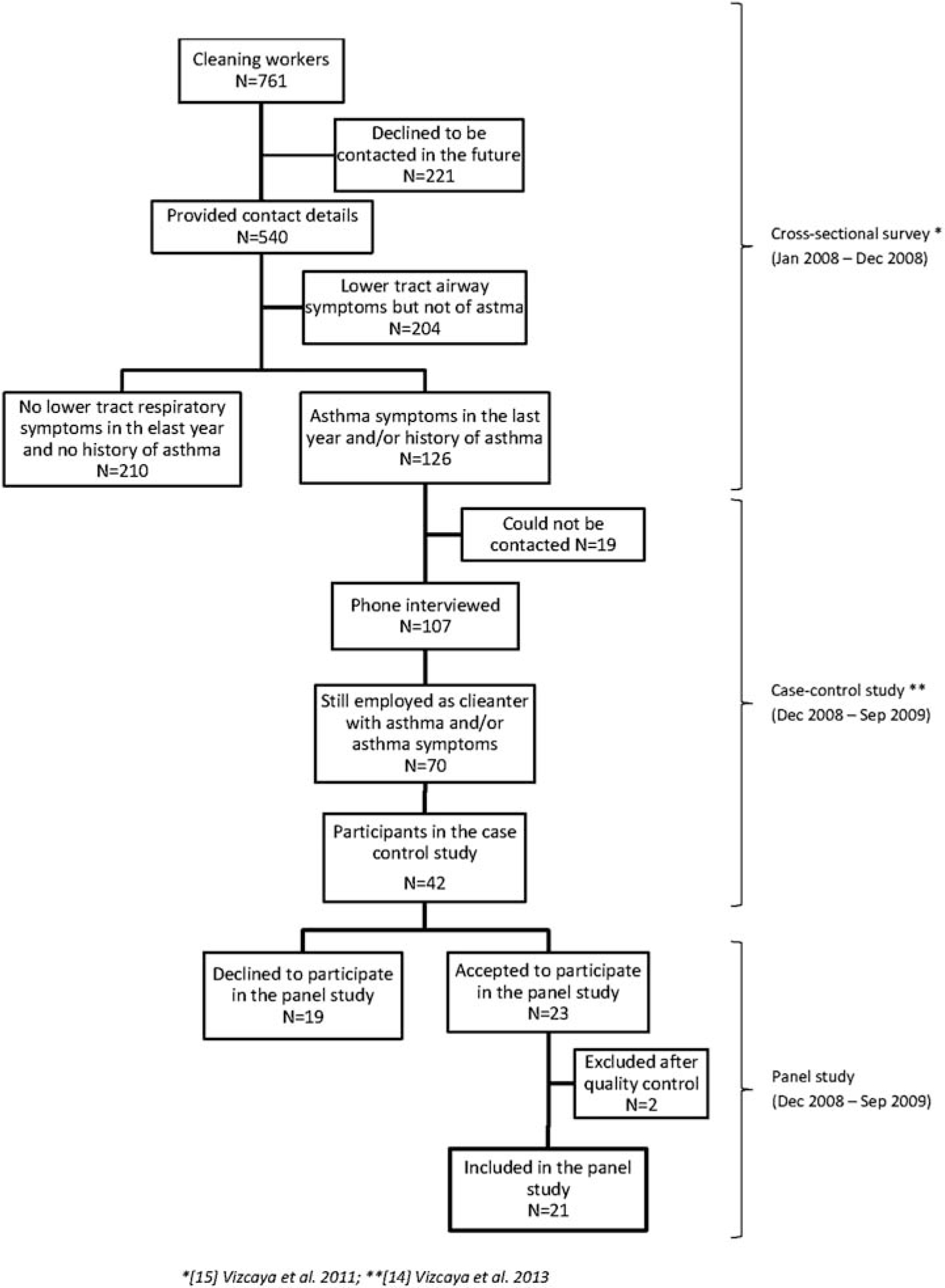
Selection flow chart of the study population.
Cleaning exposures
During the 15-day data collection period, participants recorded the types of cleaning products they used at work as well the form of application (eg, liquid solution or spray). The list of cleaning products evaluated was based on a list considered previously15 and included 14 different generic cleaning agents. We used each participant’s responses to create composite variables indicating the total number of different products and the number of different sprays used. We considered all exposures independent of one another and created a single, unique comparison group consisting of person-days without exposure to any cleaning product, which corresponded with days off work.
Respiratory health outcomes
Study participants recorded daily URTS and LRTS, respectively, using a symptom severity scale that ranged from zero, indicating ‘no symptoms’ to four, indicating ‘a lot’. Symptoms of the upper respiratory tract included a sore throat, a runny nose and watery eyes; symptoms of the lower respiratory tract included breathlessness, wheeze, chest tightness and cough. For each participant, we constructed daily URTS and LRTS summary scores by adding the daily scores assigned to each of the upper and lower symptoms, respectively. The use of a symptom score as an outcome of asthma has a good predictive ability.17 Similar approaches have been used previously.8 18
During the data collection period, PEF, in L/min and FEV1, in mL, were measured three times every day using a portable, handheld PIKO-1 meter (nSpire Health Inc, Longmont, Colorado, USA). Instructions were provided to each participant to complete three consecutive manoeuvres, of which the highest was stored in the morning at wake-up, in the afternoon and in the evening before going to bed every day. We analysed the evening measurements taken on the same day of exposure, daily variation of the same day of exposure and the measurements taken on the morning of the day following the exposure. We calculated daily variation as the daily maximum minus daily minimum divided by the daily mean.
Additional relevant information, including baseline spirometry and atopic status, was collected previously.14 Baseline spirometry was performed before starting the 15-day follow-up with an EasyOne spirometer (NDD Medical Technologies, Zürich, Switzerland) following the American Thoracic Society/European Respiratory Society standardisation19 and results are presented as the percentage of age-predicted and height-specific predicted values.20 21 Atopic status was evaluated using the Phadiatop test (Pharmacia ImmunoCAP; Pharmacia, Uppsala, Sweden).22 Information about the number of cigarettes smoked, use of respiratory medication, having a cold or flu and starting and ending times of the work day was recorded in the diaries.
Statistical methods
The analytical unit of analysis was person-day and we accounted for the potential random effects by participant using mixed regression analyses. For analyses of URTS and LRTS, mean ratios (MR), with 95% CIs, for each cleaning product were calculated as the exponent of the regression coefficient from the Poisson mixed model specified with a log link. For analyses of FEV1 and PEF, mean differences (MD), with 95% CIs, were generated using regression coefficients from linear mixed models. All models were adjusted for age, having a cold or flu, number of cigarettes smoked and use of respiratory medication. For the lung function models, we included height as a covariate at the individual level. To obtain reliable estimates of association, we considered for analysis only those cleaning products with at least five person-days. All analyses were conducted using SAS V.9.3 (SAS Institute Inc, Cary, North Carolina, USA).
RESULTS
Overall, 21 women employed as cleaning workers provided 312 person-days of observation data. The baseline characteristics of the participants and non-participants were not statistically different. Participants were, on average, 45 years old (median: 45; IQR: 39–50) and half reported no history of cigarette smoking (table 1). Eight participants (38%) were categorised as atopic and baseline spirometry indicated lung function values in the range of age-specific and height-specific predicted values.
Table 1.
Demographic and clinical characteristics of the study population
| Demographic characteristics | Study participants N=21 |
|---|---|
|
| |
| Age (years), median (IQR) | 45 (39–50) |
| Smoking status, n (%) | |
| Lifetime non-smoker | 10 (48) |
| Former smoker | 4 (19) |
| Current smoker | 7 (33) |
| Atopy, n (%) | 8 (38) |
| Baseline FVC* (% predicted), median (IQR) | 98 (89–106) |
| Baseline FEV1† (% predicted), median (IQR) | 96 (88–102) |
| (Total IgE)serum>140 UI/mL, n (%) | 6 (29) |
| Baseline asthma score, median (IQR) | 2 (1–3) |
| Characteristics reported during 15 days (312 person-days) of | |
| follow-up | |
| Any LRTS‡, n (%) | 18 (86) |
| Average daily score of LRTS (per person), median (IQR) | 1 (0–2) |
| Any URTS‡, n (%) | 17 (81) |
| Average daily score of URTS (per person), median (IQR) | 1 (0–2) |
| Percentage of working days (per person), median (IQR) | 73 (67–100) |
| Percentage of days using any irritant (per person), median (IQR) | 73 (20–86) |
| Percentage of days using any spray, median (IQR) | 0 (0–60) |
| Daily number of cleaning products used, median (IQR) | 2 (1–4) |
| Daily number of cigarettes smoked,§ median (IQR) | 9 (5–13) |
| Percentage days with respiratory infection, median (IQR) | 0 (0–33) |
| Percentage days taking respiratory medication, median (IQR) | 0 (0–33) |
| Percentage days cleaning at home, median (IQR) | 50 (37–93) |
| Diurnal variation PEF¶ (per person), median (IQR) | 15 (12–18) |
| Diurnal variation FEV1¶ (per person), median (IQR) | 9 (8–14) |
Forced vital capacity.
Forced expiratory volume in the 1 s.
Any LRTS or URTS reported during 15-day follow-up.
Among current smokers.
Daily maximum minus daily minimum divided by daily mean, expressed as a percentage.
FEV1, forced expiratory volume in the 1 s; FVC, forced vital capacity; LRTS, lower respiratory tract symptoms; PEF, peak expiratory flow; URTS, upper respiratory tract symptoms.
Participants performed cleaning work during a median of 73%, or approximately 11 days, of the 15-day follow-up period. The reported mean number of cleaning products used was 2.4 per day (median: 2.0) and exposure to at least one strong irritant (ie, ammonia, bleach, hydrochloric acid) was common (median: 73%; IQR: 20–86; table 2). With the exception of carpet cleaners and waxes, all cleaning products were reported on at least 10 person-days. Waxes and polishes were the least frequently used products, being reported by three participants; bleach, was the most frequently used product, being reported by 15 participants and on 55% of person-days.
Table 2.
Associations of cleaning-related occupational exposures with upper and LRTS among 21 professional female cleaners, for the entire study population and stratified by atopic status
| All study participants (N = 312 person-days) |
With atopy (N=119 person-days) |
Without atopy (N=193 person-days) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Cleaning product exposures | N* | URTS score MR (95% CI) | LRTS score MR (95% CI) | N | URTS score MR (95% CI) | LRTS score MR (95% CI) | N | URTS score MR (95% CI) | LRTS score MR (95% CI) |
|
| |||||||||
| No use of any productt | 112 | 1.0 | 1.0 | 46 | 1.0 | 1.0 | 66 | 1.0 | 1.0 |
| Bleach | 172 | 1.7 (1.1 to 2.7) | 1.4 (0.9 to 2.1) | 69 | 2.0 (1.0 to 3.9) | 1.2 (0.7 to 2.0) | 103 | 1.4 (0.7 to 2.8) | 1.8 (0.9 to 3.6) |
| Liquid soap/detergent | 121 | 1.6 (1.0 to 2.5) | 1.8 (1.1 to 3.0) | 35 | 2.3 (1.0 to 5.1) | 1.2 (0.6 to 2.3) | 86 | 1.3 (0.7 to 2.3) | 3.2 (1.4 to 7.5) |
| Air freshener | 65 | 1.6 (1.0 to 2.7) | 1.4 (0.8 to 2.5) | 20 | 2.5 (1.1 to 5.6) | 1.1 (0.5 to 2.4) | 45 | 1.2 (0.6 to 2.4) | 1.8 (0.8 to 3.9) |
| Degreaser | 61 | 1.7 (0.9 to 3.3) | 1.5 (0.9 to 2.6) | 16 | 1.5 (0.4 to 5.5) | 1.0 (0.4 to 2.6) | 45 | 1.8 (0.8 to 4.0) | 2.2 (1.1 to 4.2) |
| Multiuse product | 58 | 1.4 (0.9 to 2.3) | 1.0 (0.6 to 1.8) | 24 | 2.1 (1.0 to 4.6) | 1.3 (0.6 to 2.5) | 34 | 1.1 (0.6 to 1.9) | 0.5 (0.2 to 1.2) |
| Limescale remover | 40 | 2.0 (1.2 to 3.5) | 1.3 (0.6 to 2.4) | 26 | 2.7 (1.2 to 6.2) | 1.2 (0.5 to 2.9) | 14 | 1.4 (0.6 to 3.2) | 1.5 (0.6 to 3.8) |
| Glass cleaner | 40 | 1.6 (1.0 to 2.5) | 1.0 (0.5 to 1.8) | 26 | 2.4 (1.1 to 5.4) | 1.2 (0.5 to 2.5) | 14 | 1.1 (0.6 to 2.0) | 0.5 (0.2 to 1.8) |
| Dust mop product | 37 | 1.5 (0.9 to 2.5) | 1.0 (0.5 to 2.1) | 8 | 2.7 (1.1 to 6.5) | 1.3 (0.5 to 3.2) | 29 | 1.0 (0.5 to 2.0) | 0.5 (0.1 to 2.2) |
| Powder soap/detergent | 31 | 2.5 (1.2 to 5.0) | 1.5 (0.6 to 3.8) | 16 | 7.2 (1.0 to 54.3) | 0.3 (0.0 to 4.2) | 15 | 2.5 (1.2 to 5.6) | 2.8 (1.0 to 8.0) |
| Ammonia | 21 | 2.3 (0.6 to 8.9) | 0.4 (0.1 to 1.4) | 19 | 2.8 (0.6 to 13.0) | 0.5 (0.1 to 2.0) | 2 | – | – |
| Solvent | 20 | 2.3 (0.3 to 16) | 2.4 (0.6 to 9.2) | 11 | 5.2 (0.3 to 98.4) | 0.8 (0.0 to 12.2) | 9 | 11.0 (0.3 to 455.1) | 4.6 (0.7 to 29.4) |
| Hydrochloric acid | 16 | 3.4 (0.8 to 14) | 1.9 (0.9 to 4.3) | 3 | – | – | 13 | 12.0 (1.1 to 136.3) | 2.5 (1.0 to 6.5) |
| Wax/polishes | 8 | 2.4 (0.9 to 6.2) | 1.4 (0.5 to 3.5) | 5 | 2.0 (0.7 to 5.6) | 1.3 (0.4 to 3.9) | 3 | – | – |
| Carpet cleaner | 2 | – | – | 0 | – | – | 2 | – | – |
| Any irritant | 175 | 1.7 (1.1 to 2.6) | 1.4 (0.9 to 2.1) | 69 | 2.0 (1.0 to 3.9) | 1.2 (0.7 to 2.0) | 106 | 1.4 (0.7 to 2.8) | 1.8 (0.9 to 3.6) |
| Number of different products | |||||||||
| 1–3 | 103 | 1.4 (0.9 to 2.3) | 1.3 (0.9 to 2.0) | 36 | 1.0 (0.3 to 3.2) | 1.3 (0.7 to 2.4) | 67 | 1.3 (0.8 to 2.4) | 1.8 (0.9 to 3.6) |
| ≥4 | 97 | 1.6 (1.0 to 2.5) | 1.5 (0.9 to 2.3) | 37 | 2.5 (1.1 to 5.6) | 1.1 (0.5 to 2.2) | 60 | 1.3 (0.7 to 2.3) | 1.6 (0.8 to 3.3) |
| Number of different sprays | |||||||||
| 1–2 | 48 | 1.7 (0.9 to 2.9) | 1.4 (0.8 to 2.4) | 11 | 2.5 (1.0 to 6.5) | 0.8 (0.3 to 2.1) | 37 | 1.4 (0.6 to 3.1) | 1.8 (0.9 to 3.7) |
| ≥3 | 23 | 1.6 (1.0 to 2.6) | 1.4 (0.7 to 2.7) | 10 | 2.8 (1.2 to 6.7) | 1.3 (0.6 to 2.9) | 13 | 1.1 (0.6 to 2.1) | 0.6 (0.1 to 3.4) |
N denotes the number of person-days with reported use of each product.
Referent category. Numbers represent mean ratios (with 95% CIs) generated using exponentiated coefficients from logistic mixed models adjusted for age, having a cold or flu, number of cigarettes smoked and use of respiratory medication. A random intercept for participant was included in the models.
LRTS, lower respiratory tract symptoms; MR, mean ratios.
The average daily summary scores for URTS and LRTS were 1.26 and 1.24, respectively. During the 15-days follow-up, 17 (81%) participants reported at least one URTS and 18 (86%) reported at least one LRTS. URTS were associated with the use of any cleaning agent, use of four different products or more, and specifically with bleach (MR: 1.7; 95% CI 1.1 to 2.7), glass cleaner (MR: 1.6; 95% CI 1.0 to 2.5), powder detergent (MR: 2.5; 95% CI 1.2 to 5.0), liquid detergent (MR: 1.6; 95% CI 1.0 to 2.5), limescale remover (MR: 2.0; 95% CI 1.2 to 3.5) and air freshener (MR: 1.6; 95% CI 1.0 to 2.7). These associations were generally stronger when analyses were limited to individuals with atopy and attenuated among those without atopy. For LRTS, elevated MRs were observed for the use of liquid detergents (1.8; 95% CI 1.1 to 3.0), hydrochloric acid (1.9; 95% CI 0.9 to 4.3), degreasers (1.5; 95% CI 0.9 to 2.6) and bleach (1.4; 95% CI 0.9 to 2.1). In contrast to our findings for analysis of URTS, associations with LRTS were stronger among individuals without atopy.
Associations between cleaning products and metrics of lung function were consistent with the findings on respiratory symptoms (table 3). Average FEV1 for person-days with no use of any product was 2.5 L on the evening following the exposure and 2.4 L the following morning. Average PEF for person-days with no use of any product was 357 L/min on the evening following the exposure and 353 L/min the following morning. Largest reductions in evening FEV1 were observed on days with exposure to hydrochloric acid (MD: −616 mL; 95% CI −843 to −390) and solvents (MD: −751; 95% CI −1092 to −411). The use of cleaning sprays was also associated with lower evening FEV1, showing a dose–response pattern across categories of the number of sprays used (ptrend=0.01). Results of analyses of evening PEF, morning FEV1 and morning PEF showed similar effects to those observed for evening FEV1. In particular, the use of solvents was associated with a large reduction in FEV1 (MD: −1059 mL (−1392 to −726) and PEF (MD: −212 mL (−339 to −85). Diurnal variation of both FEV1 and PEF increased on days with exposure to certain cleaning agents. The highest variations were observed with the use of ammonia (MD: 13; 95% CI 6 to 19 for FEV1; MD: 17; 95% CI 6 to 28 for PEF).
Table 3.
Short-term effects of cleaning-related exposures on FEV1 and PEF among 21 professional female cleaners (n=312 person-days)
| Evening following exposure |
Morning following exposure |
Diurnal variation |
||||
|---|---|---|---|---|---|---|
| Cleaning product exposures | FEV1 (mL) | PEF (L/min) | FEV1 (mL) | PEF (L/min) | FEV1 (mL) | PEF (L/min) |
|
| ||||||
| No use of any product* | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Bleach | −84 (−209 to 42) | −16 (−40 to 8) | −46 (−178 to 86) | −10 (−37 to 17) | 2.7 (−1.1 to 6.6) | 4.0 (−1.7 to 9.7) |
| Liquid soap/detergent | −108 (−229 to 14) | −13 (−39 to 13) | −106 (−241 to 30) | −14 (−43 to 16) | 4.9 (1.5 to 8.4) | 5.9 (0.7 to 11.1) |
| Air freshener | −127 (−285 to 30) | −6 (−40 to 27) | −141 (−307 to 24) | 1 (−39 to 41) | 7.2 (2.6 to 11.8) | 8.6 (1.5 to 15.8) |
| Degreaser | −197 (−358 to −35) | −22 (−53 to 8) | −383 (−514 to −252) | 3 (−39 to 45) | 2.1 (−2.4 to 6.5) | 0.1 (−6.5 to 6.6) |
| Multiuse product | 3 (−136 to 142) | −4 (−31 to 23) | −25 (−176 to 126) | −11 (−44 to 22) | 6.8 (2.4 to 11.2) | 7.8 (1.1 to 14.4) |
| Limescale remover | −134 (−306 to 37) | −13 (−57 to 30) | 139 (−79 to 357) | 8 (−42 to 58) | 9.3 (4.4 to 14.1) | 13.0 (5.4 to 20.6) |
| Glass cleaner | 6 (−146 to 158) | −10 (−41 to 20) | −24 (−164 to 116) | −2 (−41 to 36) | 6.4 (1.7 to 11.2) | 6.7 (−0.9 to 14.3) |
| Dust mop product | −101 (−243 to 41) | −12 (−48 to 25) | −96 (−258 to 66) | −22 (−65 to 20) | 4.7 (0.1 to 9.3) | 7.3 (−0.5 to 15.1) |
| Powder soap/detergent | −115 (−330 to 100) | −4 (−57 to 49) | −523 (−712 to −334) | 11 (−66 to 88) | 8.5 (2.3 to 14.7) | 11.4 (2.5 to 20.3) |
| Ammonia | −22 (−275 to 231) | −23 (−82 to 36) | −168 (−389 to 53) | −40 (−112 to 32) | 12.7 (6.0 to 19.4) | 17.0 (5.9 to 28.0) |
| Solvent | −751 (−1092 to −411) | −114 (−233 to 5) | −1059 (−1392 to −726) | −212 (−339 to −85) | 0.6 (−6.5 to 7.6) | 6.5 (−9.2 to 22.1) |
| Hydrochloric acid | −616 (−843 to −390) | −21 (−102 to 61) | −526 (−758 to −293) | 104 (−3 to 212) | 1.1 (−4.4 to 6.6) | 1.1 (−11.1 to 13.4) |
| Wax/polishes | −300 (−499 to −101) | −26 (−86 to 35) | −23 (−291 to 245) | −13 (−85 to 60) | 4.9 (−3.4 to 13.1) | 0.8 (−14.3 to 16.0) |
| Carpet cleaner | −245 (−578 to 89) | −32 (−130 to 66) | −181 (−643 to 282) | −34 (−154 to 87) | 4.7 (−11.2 to 20.6) | 7.2 (−21.5 to 35.9) |
| Any irritant Number of different products |
−86 (−212 to 39) | −16 (−40 to 7) | −50 (−181 to 81) | −10 (−38 to 17) | 2.8 (−1.0 to 6.6) | 4.0 (−1.6 to 9.7) |
| 1–3 | −76 (−211 to 59) | −21 (−46 to 5) | −52 (−196 to 91) | −14 (−43 to 16) | −0.0 (−4.1 to 4.0) | 0.7 (−5.3 to 6.8) |
| >4 | −75 (−211 to 61) | −6 (−32 to 20) | −39 (−185 to 108) | −3 (−33 to 27) | 5.4 (1.4 to 9.3) | 6.8 (0.8 to 12.7) |
| Number of different sprays | ||||||
| 1–2 | −166 (−305 to −27) | −5 (−37 to 28) | −150 (−317 to 18) | −1 (−42 to 39) | 1.8 (−3.1 to 6.7) | 4.3 (−3.1 to 11.7) |
| >3 | −174 (−314 to −34) | −37 (−69 to −4) | − | − | 3.3 (−2.7 to 9.2) | 1.6 (−7.5 to 10.8) |
Referent category. Numbers represent mean difference (with 95% CIs) generated using linear mixed models adjusted for age, having a cold or flu, height, number of cigarettes smoked and use of respiratory medication. A random intercept for participant was included in the models.
FEV1, forced expiratory volume in the 1 s; PEF, peak expiratory flow.
DISCUSSION
Our study evaluated associations between exposure to cleaning products and acute respiratory health effects among women employed as professional cleaners and identified plausible respiratory symptom exacerbations following the use of irritant cleaning products. Our results also suggest that lung function may be affected rapidly following the use of irritant cleaning products, such as hydrochloric acid and solvents, and that the observed decrease may persist, or even worsen, on the morning following the exposure. These findings should be interpreted cautiously and in the light of the strengths and limitations of our study described below. If the observed association reflects the true effects of cleaning product exposures on respiratory health, then these findings highlight the potential for improvements in workplace health and safety practices designed to limit exposures to irritant chemicals in cleaning products that affect respiratory health.
These results extend the findings of previous clinical studies about the short-term adverse respiratory effects10 12 and contrast the findings of two panel studies in which associations between cleaning product exposures and lung function were not observed.8 9 The contrast between our results and those published by Medina-Ramon et al8 and Bernstein et al9 in particular suggest that differences in the patterns of non-occupational and occupational cleaning exposures may result in important differences in respiratory health. The American Thoracic Society’s statement on work-exacerbated asthma recently described a potential link between the use of cleaning products and work-aggravated asthma7 and increased airways reactivity has been suggested as a main adverse effect of exposure to respiratory irritant products.1 23–25 Our results for LRTS suggest that short-term exposure to irritant cleaning agents among cleaning workers may exacerbate pre-existing asthma, especially among individuals without atopy. Similar results have been reported for domestic cleaners;8 however, no indicative effect modification by atopy was observed in the population of domestic cleaners, in which there was a notably lower prevalence of atopy (16%) compared to that in our study population (38%). Our findings for URTS support those of Bernstein et al,9 showing an increased risk following exposure to cleaning products. To the best of our knowledge, there are no additional analyses of short-term respiratory effects of exposure to cleaning products stratified by atopic status with which to compare our findings.
Decreases in lung function measured on the day of and day following exposure were large for several specific exposures and, broadly speaking, were larger among participants without atopy than participants with atopy (see online supplementary tables S1 and S2). The stronger observed effects among persons without atopy may be due to the different exposure patterns. If individuals with higher sensitivity to cleaning products, especially products with strong odours, tend to change their environment or behaviours (eg, increase ventilation, use of masks) while using the products, then the actual dose of exposure to these products may be lower than the dose received by individuals with lower sensitivity. To evaluate the likelihood of this hypothesis, we evaluated exposure frequency data from the case–control study in which our panel was nested and found that non-atopic cases used the majority of cleaning products for more hours per day and days per week than non-atopic cases (data not shown). At the time we conducted our analysis, we found no previous study reporting a similar finding, and thus any hypothesis suggesting that differences in respiratory health outcomes may be attributed to differences in patterns of exposure rather than, or in addition to, differences in susceptibility should be considered carefully. Improvements in exposure assessment methods, including the addition of information about the extent to which cleaners with and without atopy change their behaviours in response to the onset of symptoms, would improve our ability to interpret the differences observed by atopic status. The large effects observed on lung function for certain exposures, such as solvents, must be considered cautiously. The small numbers of participants with specific exposures may have reduced the accuracy of the point estimates and have led to the wide CIs we observed. Thus, owing to the uncertainty of the values presented here, these results should be interpreted carefully. Despite the small numbers and the resulting estimates that were, in some cases, unexpectedly large, our findings provide evidence suggestive of adverse effects on lung function following acute exposure to cleaning products among cleaning workers with asthma.
Future studies of the acute respiratory health effects of cleaning products, including studies with larger numbers of participants and longer durations of data collection, may provide information with which to evaluate the precision and validity of the estimates presented here. Since our results suggest that cleaning workers may experience respiratory health effects measurable on the morning following cleaning product exposures, these findings provide justification for particular attention to the assessment of exposures and outcomes across two or more days and the evaluation of lagged effects.
Our data collection did not include information with which to evaluate the aetiology of the participants’ baseline symptomatology, but this lack of information did not affect our evaluation of the short-term respiratory effects of exposure to cleaning products. Work-exacerbated asthma requires pre-existing asthma or asthma symptoms that are worsened by conditions at work.7 Our definition of asthma at baseline was based on reliable survey questions about asthma symptoms and asthma history, and the symptomatic status was confirmed twice in two different interviews14 15 to reduce the likelihood of misclassification. If any of the participants we classified as asthmatic was in fact not asthmatic, then our findings may deviate from the true association among asthmatic women. To rule out other comorbidities similar to asthma, we evaluated the prevalence of chronic obstructive pulmonary disease (COPD) in our study population and found that our initial study cohort of cleaning workers with asthma included few (3 out of 42) cases with COPD.14 Indeed, the potential misclassification of the underlying disease does not invalidate our results, which focus on self-reported symptoms and objective measures of lung function. We conducted multiple statistical comparisons, and therefore a multiple testing scenario should be considered when interpreting our results. Overall, we expect multiple testing to have little impact on our study for several reasons. First, in order to diminish the effect of conducting multiple independent statistical tests, we used a single reference group for all comparisons in our study. Second, the exposures considered in our analyses were planned a priori and not driven by the results. Third, our analyses did not generate any inverse associations; if multiple testing had notably impacted our results, one would expect to observe both positive and inverse associations. Nonetheless, our analyses generated a large number of statistically significant associations, some of which may be type I errors.
Our findings are bolstered by the major strengths of our study. The present study is nested within a cohort of cleaners, a workforce dominated by women and by individuals with a narrow socioeconomic status, relative to the general population. As a result, we expect little residual confounding in our results due to socioeconomic status, and we do not anticipate that selection or participation in our study was differential with respect to sociodemographic factors. We adjusted our regression models for other confounders: number of cigarettes smoked, presence of flu or cold and respiratory medication. The latter variable was a dichotomous variable and did not provide any additional information about the type of medication used. Additional information about medication types, dosages and frequencies of use may notably improve our understanding of the extent to which the associations reported here may be affected by specific medications. We also consider it unlikely that differential recall of exposures or symptoms affected our results, since participants completed diaries and responded to questions about their cleaning exposures daily. In fact, the use of daily diaries highlights a particular strength of our study: the panel design. This design provided a time framework that allows us to draw causal conclusions about the short-term effects of cleaning exposures in respiratory symptoms and lung function, although if pre-existing health conditions (eg, atopy or symptoms of asthma) influence the exposure, then such factors must be taken into account. Our finding that cleaning workers use numerous products per day is unsurprising. However, since few workers used just one product per day, we were unable to disentangle the independent effects of specific cleaning products. By using a single reference category of non-exposed person-days in our statistical models, all estimates of effect generated in our analysis can be interpreted relative to a single, unexposed referent category. To test the robustness of our results, we restricted the analysis of lung function and cleaning products to person-days with any LRTS reported. Findings were consistent, suggesting that changes in lung function are due to physiological changes rather than in the expiratory manoeuvre or random variability.
Overall, our findings indicate that exposure to cleaning products affects respiratory health, including the short-term exacerbation of symptoms, decline in obstructive lung function parameters and bronchial reactivity. However, our results must be interpreted in the context of multiple comparisons and thus need replication to be confirmed. These results support the importance of developing workplace health and safety practices designed to limit the use of irritant chemicals in cleaning products. Our findings also indicate a need for improvement in our understanding of the mechanisms by which exposure to cleaning products induces or exacerbates respiratory disease.
Supplementary Material
What this paper adds.
Women employed as professional cleaners commonly use bleach, liquid detergents and other respiratory irritant cleaning products on the job.
Bleach, glass cleaner, detergents, limescale remover and air fresheners are associated with upper respiratory tract symptoms, and these associations are stronger among women with atopy than among women without atopy.
Specific cleaning products are associated with decreases in forced expiratory volume in 1 s and peak expiratory flow on the evening of and morning after exposure that are largely not statistically significant.
These results support the importance of developing workplace health and safety practices designed to limit exposures to irritant chemicals in cleaning products.
Acknowledgements
The authors thank Drs Paul Henneberger and Kjell Torén for their helpful comments on this paper. They also thank the participant companies and workers.
Funding
This study was funded by Instituto de Salud Carlos III/European Regional Development Fund, grant number PI 06/1378. The authors acknowledge partial funding of this research by CIBER Epidemiología y Salud Pública (CIBERESP), Spain.
Footnotes
Competing interests None declared.
Patient consent Obtained.
Ethics approval Ethics committee of Parc de Salut Mar, Barcelona.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol 2010;20:542–50; quiz 2p following 550. [PubMed] [Google Scholar]
- 2.Zock JP, Vizcaya D, Le Moual N. Update on asthma and cleaners. Curr Opin Allergy Clin Immunol 2010;10:114–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jaakkola JJ, Jaakkola MS. Professional cleaning and asthma. Curr Opin Allergy Clin Immunol 2006;6:85–90. [DOI] [PubMed] [Google Scholar]
- 4.Berger Z, Rom WN, Reibman J, et al. Prevalence of workplace exacerbation of asthma symptoms in an urban working population of asthmatics. J Occup Environ Med 2006;48:833–9. [DOI] [PubMed] [Google Scholar]
- 5.Blanc PD, Ellbjar S, Janson C, et al. Asthma-related work disability in Sweden. The impact of workplace exposures. Am J Respir Crit Care Med 1999;160:2028–33. [DOI] [PubMed] [Google Scholar]
- 6.Saarinen K, Karjalainen A, Martikainen R, et al. Prevalence of work-aggravated symptoms in clinically established asthma. Eur Respir J 2003;22:305–9. [DOI] [PubMed] [Google Scholar]
- 7.Henneberger PK, Redlich CA, Callahan DB, et al. An official American Thoracic Society statement: work-exacerbated asthma. Am J Respir Crit Care Med 2011;184:368–78. [DOI] [PubMed] [Google Scholar]
- 8.Medina-Ramon M, Zock JP, Kogevinas M, et al. Short-term respiratory effects of cleaning exposures in female domestic cleaners. Eur Respir J 2006;27:1196–203. [DOI] [PubMed] [Google Scholar]
- 9.Bernstein JA, Brandt D, Rezvani M, et al. Evaluation of cleaning activities on respiratory symptoms in asthmatic female homemakers. Ann Allergy Asthma Immunol 2009;102:41–6. [DOI] [PubMed] [Google Scholar]
- 10.Sastre J, Madero MF, Fernandez-Nieto M, et al. Airway response to chlorine inhalation (Bleach) among cleaning workers with and without bronchial hyperresponsiveness. Am J Ind Med 2011;54:6. [DOI] [PubMed] [Google Scholar]
- 11.Medina-Ramon M, Zock JP, Kogevinas M, et al. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case-control study. Occup Environ Med 2005;62:598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D’Alessandro A, Kuschner W, Wong H, et al. Exaggerated responses to chlorine inhalation among persons with nonspecific airway hyperreactivity. Chest 1996;109:331–7. [DOI] [PubMed] [Google Scholar]
- 13.Stav D, Stav M. Asthma and whirlpool baths. N Engl J Med 2005;353:1635–6. [DOI] [PubMed] [Google Scholar]
- 14.Vizcaya D, Mirabelli MC, Orriols R, et al. Functional and biological characteristics of asthma in cleaning workers. Respir Med 2013;107:673–83. [DOI] [PubMed] [Google Scholar]
- 15.Vizcaya D, Mirabelli MC, Anto JM, et al. A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup Environ Med 2011;68:914–19. [DOI] [PubMed] [Google Scholar]
- 16.Mirabelli MC, Vizcaya D, Marti Margarit A, et al. Occupational risk factors for hand dermatitis among professional cleaners in Spain. Contact Dermatitis 2012;66:188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sunyer J, Pekkanen J, Garcia-Esteban R, et al. Asthma score: predictive ability and risk factors. Allergy 2007;62:142–8. [DOI] [PubMed] [Google Scholar]
- 18.Delfino RJ, Gong H, Linn WS, et al. Respiratory symptoms and peak expiratory flow in children with asthma in relation to volatile organic compounds in exhaled breath and ambient air. J Expo Anal Environ Epidemiol 2003;13:348–63. [DOI] [PubMed] [Google Scholar]
- 19.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. [DOI] [PubMed] [Google Scholar]
- 20.Roca J, Burgos F, Sunyer J, et al. References values for forced spirometry. Eur Respir J 1998;11:1354–62. [DOI] [PubMed] [Google Scholar]
- 21.Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993;16:5–40. [PubMed] [Google Scholar]
- 22.Vidal C, Gude F, Boquete O, et al. Evaluation of the phadiatop test in the diagnosis of allergic sensitization in a general adult population. J Investig Allergol Clin Immunol 2005;15:124–30. [PubMed] [Google Scholar]
- 23.White CW, Martin JG. Chlorine gas inhalation: human clinical evidence of toxicity and experience in animal models. Proc Am Thorac Soc 2010;7:257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leuenberger P, Schindler C, Schwartz J, et al. Occupational exposure to inhalative irritants and methacholine responsiveness. Scand J Work Environ Health 2000;26:146–52. [DOI] [PubMed] [Google Scholar]
- 25.Strapkova A, Nosal’ova G, Hanacek J. Effects of irritants on airways reactivity. Cent Eur J Public Health 1996;4(Suppl):54–5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


