Abstract
Objective
This study investigates the spatial differences in the occurrence of COVID-19 in Brazilian Tropical Zone and its relationship with climatic, demographic, and economic factors based on data from February 2020 to May 2021.
Methods
A Linear Regression Model with the GDP per capita, demographic density and climatic factors from 5.534 Brazilian cities with (sub)tropical climate was designed and used to explain the spread of COVID-19 in Brazil.
Main results
The model shows evidence that economic, demographic and climate factors maintain a relationship with the variation in the number of cases of COVID-19. The Köppen climate classification defines climatic regions by rainfall and temperature. Some studies have shown an association between temperature and humidity and the survival of SARS-CoV-2. In this cohort study, Brazilian cities located in tropical regions without a dry season (monthly rainfall > 60 mm) showed a greater prevalence than in cities located in tropical regions with a dry season (some monthly rainfall < 60 mm).
Conclusion
Empirical evidence shows that the Brazil's tropical-climate cities differ in the number (contamination rate) of COVID-19 cases, mainly because of humidity. This study aims to alert the research community and public policy-makers to the trade-off between temperature and humidity for the stability of SARS-COV-2, and the implications for the spread of the virus in tropical climate zones.
Keywords: COVID-19, SARS-CoV-2, Brazilian tropical zone, Climate, Economic, Demographic
Graphical abstract
Highlights
-
•
In the Brazilian One Health case, COVID-19 contamination rate in 5,534 cities between February 22, 2020, and May 09, 2021 were analyzed.
-
•
Brazilian cities located in tropical regions (mainly Brazilian Amazonian region), which are warmer and more humid, had greater COVID-19 prevalence than in cities located in the drier (sub)tropical regions.
-
•
The outcomes encourage a closer examination of how the virus spreads in Tropical regions considering, e.g., the trade-off between temperature and humidity for the COVID-19 outbreaks.
1. Introduction
COVID-19 is an infectious respiratory disease caused by the SARS-CoV-2 virus, which can cause rapid death of those affected by the disease, depending on general health conditions and anamnesis. As of Jan 30, 2022, COVID-19 had caused about 5.6 million deaths worldwide. This number has grown rapidly, especially following the appearance of the Omicron variant.
A relevant question around the expansion of SARS-CoV-2 is, What are the main climatic, economic, and/or demographic features that allow a greater expansion of this virus [1]? [2,3] pointed out that a virus similar to SARS-CoV-2, the influenza virus, was affected by the climate.
The Köppen climate classification divides the climatic regions of the Earth by rainfall and temperature. Several studies have shown a relationship between temperature and humidity and the outbreak of COVID-19 [1,[4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [15], [16], [17], [18]]. For many of these studies, the virus outbreak in tropical regions has dashed hopes that the virus would exhibit only minor spread in warmer climates. This study aims to inspire a closer examination of this hypothesis, considering e.g., studies such as [19] which indicated that SARS-CoV-2 incubation has its longest predicted half-life at 30 °C, a higher temperature than originally believed. Other experiments have shown that SARS-CoV-2 survival, depending on temperature, is about five times more likely under wet conditions than under dry conditions [20]. In [21], PRATA et al. showed a trade-off between humidity and temperature (in (sub)tropical Köppen zones) and the spread of COVID-19 for the capital cities of Brazil. In authors investigated the trade-off between humidity and temperature among some cities in Tropical zone of Brazil. Recently studies have shown a relationship between Köppen climate regions and the genomes evolution and spread of SARS-CoV-2 [23].
Another approach to the COVID-19 pandemic considers Gross Domestic Product (GDP) and the population densities. Researchers as GANGEMI, TONACCI [24] and LULBADDA, KOBBEKADUWA, GURUGE [25] show possibilities related to socioeconomic indicators, like the GDP, in the spread of SARS-CoV-2. Hence, this relationship is included in this study.
Brazil is a vast tropical country, with most of its territory located in the range from 5° N to 33° S. The country falls almost entirely into the Tropical classification, with an annual average temperature about 24.3 °C, with a small portion of the country, below 20° S, falling into the Subtropical classification, with an average temperature of 18 °C.
Thus, this paper aims to investigate regional differences in the occurrence of COVID-19 in Brazil, and its relationship with climatic, economic, and demographic factors, based on records of identified cases from February 22, 2020, to May 09, 2021. Our sample includes COVID-19 data from 5534, given that 1567 Brazilian cities are located in the tropical zone. The investigation seeks the differences and main determinants of One Health factors of the COVID-19 contagion rate in the Brazilian tropical climate zones.
2. Methodology
The expansion trajectories of COVID-19 in different parts of the planet need to be compared to understand the disease's dynamics under different climatic, demographic, and socio-economic conditions. We start with the following generic model (Formula 1):
| (1) |
The trend of COVID-19's case count is considered as the dependent variable (y), with the independent variables being GDP per capita (x1), demographic density (x2), and climate zone (x3). Specifically, the climate zone variable is the Köppen climate classification, based on the assumption that the taxonomy accounts comprehensively for seasonal and average annual and monthly air temperature and precipitation. Each climatic type is denoted by a code, consisting of uppercase and lowercase letters, whose combination indicates the types (zones) and subtypes (subzones).
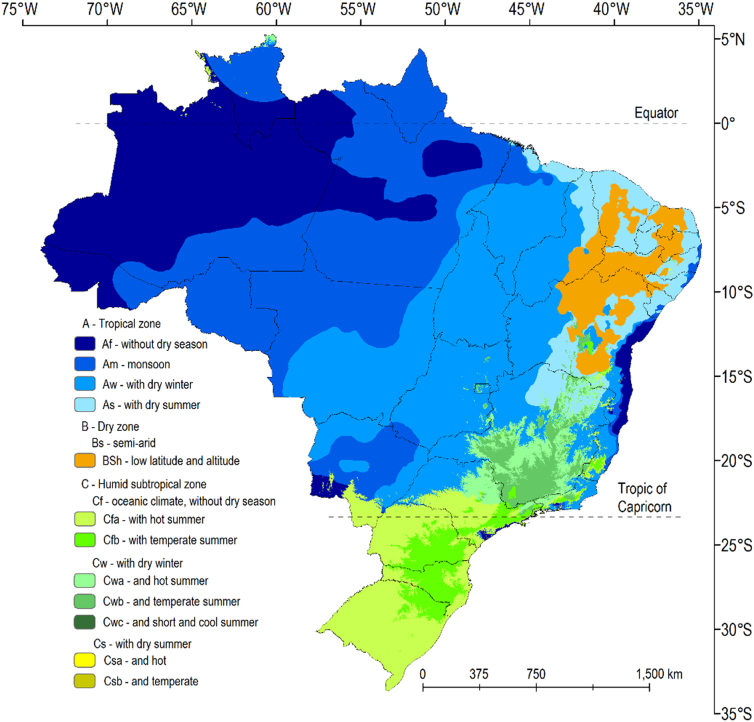
There are five major climate groups in the Köppen classification in Brazil: A - Tropical; B - Dry (arid and semi-arid); C - Subtropical; as shown in Fig. 1. In this article, we focused the tropical subzones as follows: Af – Without Dry Season, Am – Monsoon, and Aw – With Dry Winter. Specifically, the question that must be answered is: are there differences in the COVID-19 contamination rate in relation to One Health factors among Köppen-tropical Brazilian cities?
Fig. 1.
Köppen climate classification for Brazil.
Source: Alvares et al. [26]
The tropical subzones (Af, Am, and Aw) were treated as dummy variables. A sensitivity analysis was performed to evaluate the significance of dozens of One Health factors as covariates of the model, including poverty level, income concentration index, housing conditions, ageing rate and quality and health care index in the cities, GDP per capita, and population density. We hypothesize that climatic, socioeconomic, and health factors should be determinants for the contamination rate.
The climatic and the socioeconomic variables of GDP per capita and population density were selected according to their robustness to the model maintaining a statistical significance of <0.0001 to the contamination rate, for all the random model tests.
It is expected that higher GDP per capita results in higher incidence of COVID-19, because GDP is related to a greater degree of economy-associated movement. In addition, we test whether, in the Brazilian context, the cities' climate affects the occurrence rate of Covid-19.
To operationalize the regression model, the following steps were taken:
-
1.
Selection of the explanatory variables, considering the best theorical or empirical relationships;
-
2.
Codification of the variables;
-
3.
Making scatter plots with all variables, pair by pair;
-
4.
Performing univariate analyses of the independent variables, with their respective analyses of residuals;
-
5.
Development of the correlation matrix to assess the collinearity of the independent variables and to define their order of entry in the multi-variable model;
-
6.
Performing the multi-variable analysis, evaluating the significance of the general model, each of the variables and the increment of each one, through the F test and p-value;
-
7.
Deciding on the best model and the best adjustment.
3. Results and discussion
Daily data on the occurrence of COVID-19 in 5534 Brazilian cities were analyzed to verify the hypothesis that a city's Köppen climate classification can estimate the occurrence of COVID-19. The three Köppen tropical subzones each account for a similar land area in the study, as do the aggregated non-tropical zones; see Table 1.
Table 1.
Covid-19 distribution in Brazilian cities – 2020 and 2021.
| Tropical (sub)zone | Number of Cities | % of Cities | % of Total Area (Km2) | Population (mean) | % of Population | Log Contamination Rate (mean) |
|---|---|---|---|---|---|---|
| Af | 101 | 1.83 | 22.6 | 64,163.57 | 3.06 | 4.7583253 |
| Am | 238 | 4.30 | 27.5 | 47,283.78 | 5.32 | 4.3807290 |
| Aw | 1228 | 22.19 | 25.8 | 22,891.70 | 13.29 | 4.3731791 |
| Remainder⁎ | 3967 | 71.68 | 24.1 | 41,777.69 | 78.33 | 4.3140861 |
| Total/Mean | 5534 | 100 | 100 | 38,232.23 | 100 | 4.3381727 |
Brazilian cities localized in other Köppen's (sub)zones.
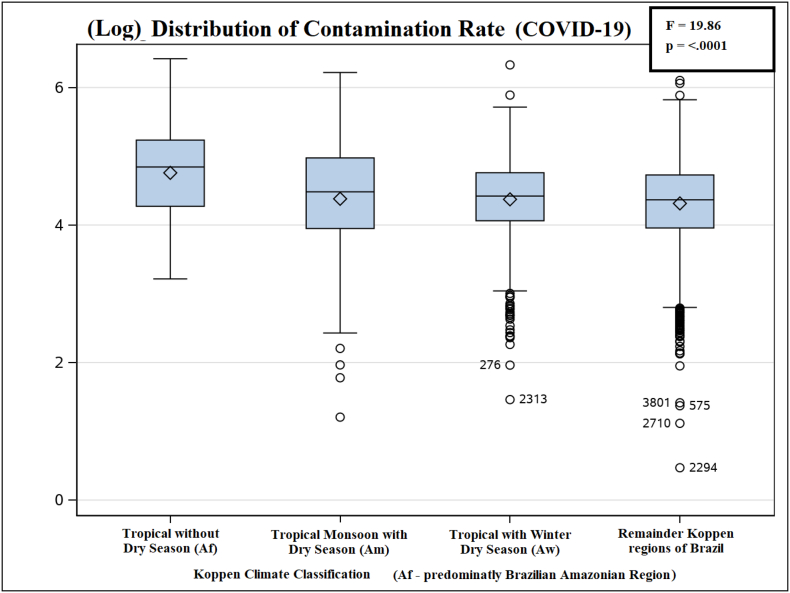
Fig. 2 shows the ANOVA boxplot for the log of COVID-19 contamination rate by Köppen Tropical (sub)zones between February 22, 2020, and May 09, 2021.
Fig. 2.
Log of Covid-19 contamination rate by Köppen Tropical (sub)zones in Brazil.
To control the ANOVA Type-I experimentwise error rate, Tukey's Studentized Range (HSD) test was applied. The Af subzone exhibited statistical significance for the log of Contamination Rate when compared with any of the other subzones; see Table 2.
Table 2.
Tukey's Studentized Range (HSD) test for the Log of Contamination Rate by Köppen (sub)zones of Brazilian cities – 2020 and 2021.
| Köppen Sub(zones) Comparison |
Difference Between Means |
Simultaneous 95% Confidence Limits |
||
|---|---|---|---|---|
| Af – Am | 0.37760 | 0.19188 | 0.56331 | *** |
| Af – Aw | 0.38515 | 0.22326 | 0.54703 | *** |
| Af – Remainder | 0.44424 | 0.28666 | 0.60182 | *** |
| Am – Aw | 0.00755 | −0.10321 | 0.11831 | |
| Am – Remainder | 0.06664 | −0.03772 | 0.17101 | |
| Aw – Remainder | 0.05909 | 0.00802 | 0.11016 | *** |
Comparisons significant at the 0.05 level are indicated by ***.
Likewise, statistically significant regression coefficients were found, in logarithmic space, between the COVID-19 contamination rate cases in Tropical Brazilian's cities, with the GDP per capita (0.33), demographic density (0.04), and Köppen climate zones: Af (0.71), Am (0.24) and Aw (0.12). The overal model parameters are shown in Table 3.
Table 3.
Regression model for Covid 19 dissemination in Brazilian cities – 2020 and 2021.
| Variable | Coefficient | Pr > |t| |
|---|---|---|
| Intercept | 0.90660 | <0.0001 |
| Log GDP per capita | 0.33102 | <0.0001 |
| Log Population Density | 0.04178 | <0.0001 |
| Af subzone | 0.71945 | <0.0001 |
| Am subzone | 0.24425 | <0.0001 |
| Aw subzone | 0.12127 | <0.0001 |
| F value | 209.82 | |
| R2 | 0.1595 | |
The regression model restates the initial hypothesis that, in Brazilian cities with greater economic dynamism, represented by the highest GDP per capita, there were more cases of COVID-19 per capita.
Some limitations of the research should be pointed out. The data about cities do not identify information about the sites where patients were infected. This should be an important factor, especially because enclosed environments are known to promote superspreading events. Also, other One Health factors should be considered, such as density in residences, the abundance of high-rise buildings, and the use of masks. In Brazil, interpersonal distancing rules and mask use were established in a heterogeneous manner for each city; this variation may be considered in future work.
4. Conclusions
In this Brazilian study, the hypothesis that “One Health factors among Brazil's Köppen Tropical cities can impact the proliferation of Covid-19” was accepted.
As interpersonal distancing rules and other preventive measures differed between Brazilian cities, locations with large economic movement scale (indicated by greater GPD) exhibited higher COVID-19 case counts. When considering climatic zones, there is a tendency towards infection with Covid-19 in cities located in tropical subzone Af, which spans the Brazilian Amazonian region.
Even though many studies have shown a relationship between temperature and humidity with COVID-19, it is worth examining the virus's spread in tropical regions more closely, since the epidemic of COVID-19 (mainly in Amazonian region of Brazil) has astonished researchers and public policy-makers who had hoped that the virus would have a smaller impact in warmer climates. To improve investigations about the surprising fact that SARS-CoV-2 can spread so well in warmer and humid regions, this study aims to encourage research towards further examination of, e.g., the trade-off between temperature and humidity for the incidence of COVID-19, primarily in Tropical zones.
Author contributions
David Prata conceived and designed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft. Conceptualization, Formal analysis, project administration, supervision, validation, writing review.
Waldecy Rodrigues conceived and designed the experiments, analyzed the data, authored or reviewed drafts of the paper, and approved the final draft. Writing original draft, conceptualization, formal analysis.
Paulo Henrique De Souza Bermejo conceived and designed the experiments, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Marina Moreira performed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Wainesten Camargo performed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Daniela Trevisan performed the experiments, prepared figures and/or tables, and approved the final draft. Data curation, forma analysis, visualization, editing.
Humberto Fizzera performed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Rafael Camargo and Gentil Barbosa performed the experiments, prepared figures and/or tables, and approved the final draft.
Cleyton Alvares oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors acknowledge the financial support of the Ministry of Health of Brazil.
Contributor Information
David Prata, Email: ddnprata@uft.edu.br.
Waldecy Rodrigues, Email: waldecy@uft.edu.br.
Daniela Mascarenhas de Queiroz Trevisan, Email: danielatrevisan@uft.edu.br.
Wainesten Camargo, Email: wainesten@uft.edu.br.
Humberto Frizzera, Email: humberto.frizzera@uft.edu.br.
Rafael Carvalho, Email: rafael.lima@uft.edu.br.
Gentil Barbosa, Email: gentil@uft.edu.br.
Clayton Alvares, Email: ca.alvares@unesp.br.
Paulo H. De Souza Bermejo, Email: paulobermejo@next.unb.br.
References
- 1.Bukhari Q., Jameel Y. 2020. Will Coronavirus Pandemic Diminish by Summer?. Available at SSRN 3556998. [Google Scholar]
- 2.Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3(10) doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barreca A.I., Shimshack J.P. Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States. Am. J. Epidemiol. 2012;176(suppl_7):S114–S122. doi: 10.1093/aje/kws259. [DOI] [PubMed] [Google Scholar]
- 4.Auler A.C., Cássaro F.A.M., Da Silva V.O., Pires L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., Wang B., Fu S., Niu T., Yan J., Shi Y., Ren X., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Núñez-Delgado A. What do we know about the SARS-CoV-2 coronavirus in the environment? Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yip C., Chang W.L., Yeung K.H., Yu I.T. Possible meteorological influence on the severe acute respiratory syndrome (SARS) community outbreak at Amoy Gardens, Hong Kong. J. Environ. Health. 2007;70(3):39–47. [PubMed] [Google Scholar]
- 11.Thai P.Q., Choisy M., Duong T.N., Thiem V.D., Yen N.T., Hien N.T., Weiss D.J., Boni M.F., Horby P. Seasonality of absolute humidity explains seasonality of influenza-like illness in Vietnam. Epidemics. 2015;13:65–73. doi: 10.1016/j.epidem.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Ng S., Cowling B.J. Association between temperature, humidity and ebolavirus disease outbreaks in Africa, 1976 to 2014. Eurosurveillance. 2014;19(35):20892. doi: 10.2807/1560-7917.es2014.19.35.20892. [DOI] [PubMed] [Google Scholar]
- 13.Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014;88(14):7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moriyama M., Ichinohe T. High ambient temperature dampens adaptive immune responses to influenza a virus infection. Proc. Natl. Acad. Sci. 2019;116(8):3118–3125. doi: 10.1073/pnas.1815029116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang P., Goggins W.B., Chan E.Y. A time-series study of the association of rainfall, relative humidity and ambient temperature with hospitalizations for rotavirus and norovirus infection among children in Hong Kong. Sci. Total Environ. 2018;643:414–422. doi: 10.1016/j.scitotenv.2018.06.189. [DOI] [PubMed] [Google Scholar]
- 18.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kratzel A., Steiner S., Todt D., V'kovski P., Brueggemann Y., Steinmann J., Steinmann E., Thiel V., Pfaender S. Temperature-dependent surface stability of SARS-CoV-2. J. Inf. Secur. 2020;81(3):452–482. doi: 10.1016/j.jinf.2020.05.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhardwaj R., Agrawal A. Likelihood of survival of coronavirus in a respiratory droplet deposited on a solid surface. Phys. Fluids. 2020;32(6) doi: 10.1063/5.0012009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prata D., Rodrigues W., De Souza Bermejo P.H., Moreira M., Camargo W., Lisboa M., Rossone Reis G., de Araujo H.X. The relationship between (sub)tropical climates and the incidence of COVID-19. PeerJ. 2021;9:e:10655. doi: 10.7717/peerj.10655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bajaj P., Arya P.C. Evolution and spread of SARS-CoV-2 likely to be affected by climate. Clim. Change Ecol. 2021;100005 [Google Scholar]
- 24.Gangemi S., Billeci L., Tonacci A. Rich at risk: socio-economic drivers of COVID-19 pandemic spread. Clin. Mol. Allergy. 2020;18(1):1–3. doi: 10.1186/s12948-020-00127-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lulbadda K.T., Kobbekaduwa D., Guruge M.L. The impact of temperature, population size and median age on COVID-19 (SARS-CoV-2) outbreak. Clin. Epidemiol. Global Health. 2021;9:231–236. doi: 10.1016/j.cegh.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alvares C.A., Stape J.L., Sentelhas P.C., Gonçalves J.D.M., Sparovek G. Köppen’s climate classification map for Brazil. Meteorol. Z. 2013;22(6):711–728. [Google Scholar]