Abstract
Citrin deficiency belongs to a group of urea cycle disorders that can be identified during newborn screening by measuring citrulline, phenylalanine, methionine, and galactose levels. Early diagnosis of citrin deficiency is beneficial as disease-specific interventions such as permission of food preference and/or supplementation of medium-chain triglyceride can prevent metabolic decompensation. However, there are currently no laboratory tests for the diagnosis of citrin deficiency in routine clinical practice. Our retrospective study investigated the diagnostic characteristics of citrin deficiency during infancy at secondary newborn screening. The present study included 10 patients with citrin deficiency and 35 controls without the condition. The positive likelihood ratios for serum levels of blood urea nitrogen (BUN) levels were 6.8 at the first visit, 3.2 at age ≤ 60 days, and 17.5 at age ≤ 100 days. The serum BUN/creatinine ratio also showed a high positive likelihood ratio (3.9 at first visit, 16.0 at age ≤ 60 days, and 24.5 at age ≤ 100 days). Therefore, the serum BUN or BUN/creatinine ratio may help to identify patients with citrin deficiency during newborn screening. Further studies are required to confirm its diagnostic accuracy in a larger cohort and elucidate the underlying mechanisms involved.
Keywords: Citrin deficiency, Blood urea nitrogen (BUN), BUN/creatinine ratio, Urea cycle disorder
Abbreviations: BUN, blood urea nitrogen; NICCD, neonatal intrahepatic cholestasis by citrin deficiency; ROC, receiver operating characteristic.
1. Introduction
Citrin deficiency belongs to a group of urea cycle disorders and is caused by biallelic pathogenic variants of SLC25A13 genes (MIM 603859) [1], [2]. The subtype classification is based on the symptomatic period in life as follows: neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD, MIM 605814), failure to thrive and dyslipidemia caused by citrin deficiency, and adult-onset type II citrullinemia (MIM 603471) [2], [3], [4], [5]. The symptoms of NICCD include prolonged jaundice, cholestatic liver injury, and growth retardation. After NICCD, obvious symptoms seem to disappear during childhood, but hypoglycemia is frequently noted, especially with hypoketosis or growth failure [6], [7]. Adult-onset type II citrullinemia can manifest as hyperammonemia and encephalopathy in adulthood [8]. Clinical histories could enable a diagnosis, although a diagnosis is ideally made as soon as possible followed by a disease-specific intervention, permission of food preference and/or supplementation of medium-chain triglyceride before the onset of the symptoms [9]. Delayed intervention and persistent cholestasis could result in irreversible complications, such as decompensated liver failure [10]. Newborn screening is the earliest opportunity for diagnosis [11]. High levels of citrulline as well as methionine, phenylalanine, or galactose are associated with increased likelihood of citrin deficiency [11], [12]. However, there are currently few laboratory tests with diagnostic power that are used routinely in clinical practice. Plasma amino acid analysis could help to identify citrin deficiency [13], although genetic analysis of the SLC25A13 gene is essential to diagnose citrin deficiency [14], and these tests do not reveal the results in an outpatient setting.
The present retrospective study investigated the diagnostic characteristics of citrin deficiency during infancy at secondary newborn screening.
2. Materials and methods
2.1. Study design
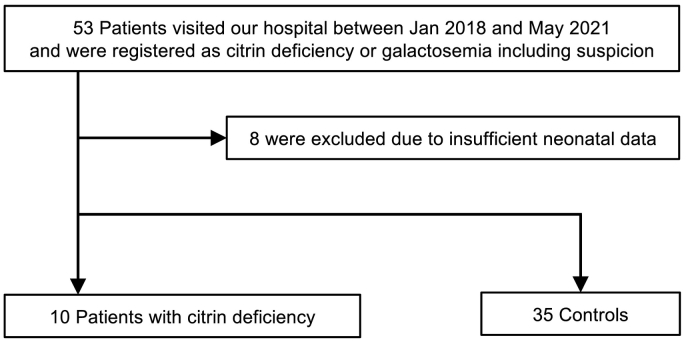
In the present retrospective study, patient data were from the health record data at Tohoku University Hospital. We initially selected 53 patients who visited the hospital between January 2018 and May 2021 who were registered as “citrin deficiency (including suspected)” or “galactosemia (including suspected).” Among these patients, eight were excluded due to insufficient data during the neonatal period, and the remaining 45 patients were finally included in the study (10 in the patient group and 35 in the control group). Patients diagnosed with other diseases because of secondary screening were also included as controls to keep the practicality of the results of this study in secondary screening. The control group included 19 healthy individuals, four with peripheral galactose epimerase deficiency, four with portosystemic shunt, two with hyperphenylalaninemia, two with non-classical galactose-1-phosphate uridylyltransferase deficiency, one with trisomy 21, one with mild argininosuccinate synthetase deficiency, one with carrier of an ASS1 gene pathogenic variant, and one with PHACE syndrome. The laboratory results between the first visit and age 100 days were analyzed with JMP Pro 16.0 (SAS Institute, Cary, NC, USA) using paired t-tests, and P-values <0.05 were considered statistically significant. Receiver operating characteristic (ROC) curves and figures were created using GraphPad Prism 8.4.3 (GraphPad Software, San Diego, CA, USA).
3. Results
3.1. Characteristics of patients with citrin deficiency and controls
The selection criteria are summarized in Fig. 1. Table 1 shows the clinical information of the patients with citrin deficiency and controls at their first visit to our hospital. In all patients, citrin deficiency-induced NICCD was resolved with fat-soluble vitamins, cholagogues, and/or medium-chain triglyceride-containing formula. At the first visit, patients with citrin deficiency had low birth weight and high levels of plasma citrulline, methionine, and threonine/serine ratio compared with the control group, which is agreement with previous reports of citrin deficiency. Blood galactose and plasma phenylalanine levels were higher in patients with citrin deficiency compared with the control group, although this was not statistically significant.
Fig. 1.
Flowchart of participant selection.
Table 1.
Characteristics of patients with citrin deficiency and controls.
| Patients (n = 10) | Controls (n = 35) | P-value | |||
|---|---|---|---|---|---|
| Male/female | 5/5 | 20/15 | |||
| Gestational age (weeks) | 39 ± 1.2 | 39 ± 1.2 | |||
| Birth weight (g) | 2671 ± 237 | 3037 ± 409 | 0.0021 | ||
| Neonatal jaundice | 0/10 | 6/35 | |||
| Newborn screening | |||||
| High citrulline | 5 | 2 | |||
| High galactose and citrulline | 2 | 0 | |||
| High galactose | 1 | 25 | |||
| High galactose-1-phosphate | 0 | 6 | |||
| High phenylalanine | 2 | 2 | |||
| At first visits to our hospital | |||||
| Age (days) | 20.5 ± 13.6 | 19.9 ± 13.2 | |||
| Serum BUN (mg/dL) | 14.4 ± 2.4 | (n = 9) | 8.7 ± 2.6 | (n = 35) | <0.001 |
| Serum creatinine (mg/dL) | 0.27 ± 0.06 | (n = 9) | 0.25 ± 0.07 | (n = 35) | 0.308 |
| Serum BUN/creatinine ratio | 54.8 ± 13.0 | (n = 9) | 38.6 ± 16.5 | (n = 35) | 0.009 |
| Blood galactose (mg/dL) | 18.4 ± 27.1 | (n = 8) | 1.9 ± 3.8 | (n = 31) | 0.152 |
| Plasma citrulline (μM) | 668.4 ± 390.6 | (n = 10) | 39.3 ± 26.7 | (n = 18) | <0.001 |
| Plasma phenylalanine (μM) | 159.0 ± 227.0 | (n = 10) | 76.3 ± 38.1 | (n = 18) | 0.306 |
| Plasma methionine (μM) | 190.6 ± 188.1 | (n = 10) | 39.6 ± 8.9 | (n = 18) | 0.0394 |
| Plasma threonine/serine ratio | 3.78 ± 1.75 | (n = 10) | 1.24 ± 0.66 | (n = 17) | 0.0017 |
Data represent mean ± SD.
Each laboratory value of the patient is described in Supplemental Table. BUN, blood urea nitrogen.
3.2. Serum BUN, creatinine, and BUN/creatinine ratio in patients with citrin deficiency and controls
Previous reports suggested a relationship between the urea cycle and creatine metabolism; therefore, we focused on serum BUN and creatinine levels [15], [16]. As expected, serum BUN levels and the BUN/creatinine ratio were significantly elevated in patients with citrin deficiency (14.4 ± 2.5 mg/dL and 54.8 ± 13.7, respectively) compared with controls (8.7 ± 2.7 mg/dL; P < 0.001 and 38.6 ± 16.7; P = 0.009, respectively) at secondary newborn screening (Fig. 2a). Serum BUN levels and the BUN/creatinine ratio were also significantly increased in patients with citrin deficiency (12.2 ± 3.5 mg/dL and 80.29 ± 40.0, respectively) compared with controls (9.0 ± 2.1 mg/dL; P = 0.018 and 48.6 ± 16.1; P = 0.035, respectively) at the time of the lowest serum creatinine levels at age ≤ 60 days (Fig. 2b). Even at age ≤ 100 days, the significant elevations of serum BUN levels and the BUN/creatinine ratio were also found in patients with citrin deficiency (11.7 ± 3.3 mg/dL and 90.9 ± 38.7, respectively) compared with controls (8.5 ± 1.9 mg/dL; P = 0.016 and 47.4 ± 15.9; P = 0.006, respectively). In addition to serum BUN levels and the BUN/creatinine ratio, serum creatinine levels also significantly differed in patients with citrin deficiency (0.15 ± 0.06 mg/dL) compared with the control group (0.19 ± 0.05 mg/dL; P = 0.034) (Fig. 2c) at age ≤ 100 days.
Fig. 2.
Serum BUN and creatinine levels and BUN/creatinine ratio at first visit, age ≤ 60 days, and age ≤ 100 days in patients with citrin deficiency and controls.
The upper, middle, and lower panels show the laboratory data for each patient with citrin deficiency and control at first visit (a), age ≤ 60 days (b), and age ≤ 100 days (c). Bars represent mean ± SD. * P < 0.05 (Student's t-tests).
3.3. Clinical usefulness of serum BUN and BUN/creatinine ratio to as a marker for citrin deficiency
ROC curves were created for patients with citrin deficiency and controls at first visit, age ≤ 60 days, and age ≤ 100 days to assess the usefulness of serum BUN and creatinine levels, and the BUN/creatinine ratio as a marker for citrin deficiency (Fig. 3). The ROC curves indicated their clinical usefulness, particularly serum BUN levels and/or the serum BUN/creatinine ratio. Therefore, the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were calculated (Table 2). At first visit, serum BUN showed good positive and negative likelihood ratios. When the sampling data limits were extended to postnatal days 60 or 100, the serum BUN/creatinine ratio showed better accuracy than serum BUN. In particular, the serum BUN/creatinine ratio at a cutoff level of ≥80 showed excellent accuracy for a definitive diagnosis.
Fig. 3.
ROC curves of serum BUN, creatinine, and BUN/creatinine ratio to differentiate between patients with citrin deficiency and controls.
The upper, middle, and lower panels show each ROC curve at first visit (a), age ≤ 60 days (b), and age ≤ 100 days (c).
Table 2.
Diagnostic accuracy of serum BUN and BUN/creatinine ratio to identify patients with citrin deficiency.
| Index | Timing | AUC | Cutoff | Sensitivity | Specificity | Positive LR | Negative LR |
|---|---|---|---|---|---|---|---|
| Serum BUN | First visit | 0.94 | 13 | 0.78 | 0.89 | 6.8 | 0.3 |
| 12 | 0.89 | 0.86 | 6.2 | 0.1 | |||
| 11 | 1.00 | 0.86 | 7.0 | 0.0 | |||
| 10 | 1.00 | 0.71 | 3.5 | 0.0 | |||
| ≤60 days | 0.80 | 13 | 0.30 | 0.91 | 3.2 | 0.8 | |
| 12 | 0.60 | 0.88 | 4.8 | 0.5 | |||
| 11 | 0.70 | 0.75 | 2.8 | 0.4 | |||
| 10 | 0.70 | 0.69 | 2.2 | 0.4 | |||
| ≤100 days | 0.98 | 13 | 0.50 | 0.97 | 17.5 | 0.5 | |
| 12 | 0.50 | 0.94 | 8.8 | 0.5 | |||
| 11 | 0.70 | 0.83 | 4.1 | 0.4 | |||
| 10 | 0.80 | 0.71 | 2.8 | 0.3 | |||
| Serum BUN/creatinine ratio | First visit | 0.78 | 80 | 0.11 | 0.97 | 3.9 | 0.9 |
| 70 | 0.22 | 0.94 | 3.9 | 0.8 | |||
| 60 | 0.33 | 0.91 | 3.9 | 0.7 | |||
| 50 | 0.67 | 0.71 | 2.3 | 0.5 | |||
| ≤60 days | 0.81 | 80 | 0.50 | 0.97 | 16.0 | 0.5 | |
| 70 | 0.50 | 0.88 | 4.0 | 0.6 | |||
| 60 | 0.60 | 0.72 | 2.1 | 0.6 | |||
| 50 | 0.80 | 0.56 | 1.8 | 0.4 | |||
| ≤100 days | 0.85 | 80 | 0.70 | 0.97 | 24.5 | 0.3 | |
| 70 | 0.70 | 0.91 | 8.2 | 0.3 | |||
| 60 | 0.70 | 0.77 | 3.1 | 0.4 | |||
| 50 | 0.80 | 0.57 | 1.9 | 0.4 |
AUC, area under the curve; BUN, blood urea nitrogen; LR, likelihood ratio.
4. Discussion
This retrospective study highlighted the usefulness of serum BUN or BUN/creatinine ratio to identify citrin deficiency in positive cases of newborn screening. Serum BUN levels or the BUN/creatinine ratio showed a high specificity to distinguish between patients with citrin deficiency and controls, suggesting that this laboratory measurement is helpful to accurately determine the probability of citrin deficiency in screening positive case with citrullinemia, hyperphenylalaninemia or galactosemia.
The dynamics of BUN and creatinine in citrin deficiency have not received much attention to date, although a previous study also showed elevated levels of BUN and BUN/creatinine ratio in citrin deficiency [17]. Our patients with citrin deficiency as well as a mouse model of citrin deficiency showed elevated blood urea levels [18]. Although the underlying mechanisms remain unknown, high levels of BUN or BUN/creatinine ratio suggest a pathophysiology associated with citrin deficiency since this tendency may continue into adulthood [17]. Both elevated BUN levels and decreased creatinine levels may be involved in increased catabolism. Low height associated with citrin deficiency [19] may be attributable to persistent increased protein catabolism. Although a high-protein food preference of patients with citrin deficiency could induce elevated levels of BUN elevation, this would not be a primary cause during the early postnatal period as babies cannot spontaneously choose a high-protein formula. Peroxisome proliferator-activated receptor alpha (PPARα), which may be associated with the pathophysiology of citrin deficiency [20], could induce protein catabolism. Pparα knockout mice showed elevated levels of BUN, which is consistent with the phenomenon in citrin deficiency [21]. However, the involvement of creatine metabolism and PPARα is not well understood in citrin deficiency. Low blood creatinine levels could result from decreased body muscle mass due to catabolism. This phenomenon could be related to arginine metabolism. Arginine, which is increased in citrin deficiency [11], is involved in the urea cycle as well as the creatine synthesis pathway. Thus, we hypothesized that the conversion of arginine and glycine to guanidinoacetate and ornithine may be inhibited and the conversion of arginine to urea and ornithine may be promoted in citrin deficiency, although the cause is unknown. The hypothesis could explain the elevated BUN and decreased creatinine levels observed and further studies are required to verify this.
The present study has some limitations. First, the results of this study cannot be applied to patients with factors that affect serum BUN and/or creatinine, such as gastrointestinal bleeding. Second, the data were based on experiences in our institute and the sample size was not sufficient to set a validation cohort. Third, all patients with citrin deficiency in the present study had NICCD due to the use of infant laboratory data. Therefore, these results cannot be applied to all patients with citrin deficiency. Despite these limitations, our selection criteria for patients with citrin deficiency and controls minimized a sampling bias, and the significance of our in clarifying the laboratory findings to approach a definitive diagnosis of citrin deficiency remained unaffected.
5. Conclusion
Serum BUN levels and/or the BUN/creatinine ratio may be useful to identify patients with citrin deficiency during newborn screening. Further studies are required to confirm the diagnostic accuracy in other cohorts and elucidate the underlying mechanism involved.
The following is the supplementary data related to this article.
Laboratory data of patients with citrin deficiency at first visits to our hospital
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Ethics statement
This study was approved by the Ethics Committee of Tohoku University Hospital (approval number: 2021-1-497) and used opt-out consent.
Authors' contributions
TS and YW collected data and drafted the initial manuscript. All authors conceptualized and designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
References
- 1.Ferreira C.R., Rahman S., Keller M., et al. An international classification of inherited metabolic disorders (ICIMD) J. Inherit. Metab. Dis. 2020;44:164–177. doi: 10.1002/jimd.12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobayashi K., Sinasac D.S., Iijima M., et al. The gene mutated in adult-onset type II citrullinaemia encodes a putative mitochondrial carrier protein. Nat. Genet. 1999;22(2):159–163. doi: 10.1038/9667. [DOI] [PubMed] [Google Scholar]
- 3.Ohura T., Kobayashi K., Tazawa Y., et al. Neonatal presentation of adult-onset type II citrullinemia. Hum. Genet. 2001;108(2):87–90. doi: 10.1007/s004390000448. [DOI] [PubMed] [Google Scholar]
- 4.Song Y.-Z., Deng M., Chen F.-P., et al. Genotypic and phenotypic features of citrin deficiency: five-year experience in a chinese pediatric center. Int. J. Mol. Med. 2011;28(1):33–40. doi: 10.3892/ijmm.2011.653. [DOI] [PubMed] [Google Scholar]
- 5.Palmieri L., Pardo B., Lasorsa F.M., et al. Citrin and aralar1 are Ca(2+)-stimulated aspartate/glutamate transporters in mitochondria. EMBO J. 2001;20(18):5060–5069. doi: 10.1093/emboj/20.18.5060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arai-Ichinoi N., Kikuchi A., Wada Y., Sakamoto O., Kure S. Hypoglycemic attacks and growth failure are the most common manifestations of citrin deficiency after 1 year of age. J. Inherit. Metab. Dis. 2021;44:838–846. doi: 10.1002/jimd.12390. [DOI] [PubMed] [Google Scholar]
- 7.Wada Y., Arai-Ichinoi N., Kikuchi A., Sakamoto O., Kure S. Hypoketotic hypoglycemia in citrin deficiency: a case report. BMC Pediatr. 2020;20(1):444. doi: 10.1186/s12887-020-02349-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayasaka K., Numakura C. Adult-onset type II citrullinemia: current insights and therapy. Appl. Clin. Genet. 2018;11:163–170. doi: 10.2147/TACG.S162084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayasaka K. Metabolic basis and treatment of citrin deficiency. J. Inherit. Metab. Dis. 2020;44:110–117. doi: 10.1002/jimd.12294. [DOI] [PubMed] [Google Scholar]
- 10.Okano Y., Ohura T., Sakamoto O., Inui A. Current treatment for citrin deficiency during NICCD and adaptation/compensation stages: strategy to prevent CTLN2. Mol. Genet. Metab. 2019;127(3):175–183. doi: 10.1016/j.ymgme.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Ohura T., Kobayashi K., Tazawa Y., et al. Clinical pictures of 75 patients with neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD) J. Inherit. Metab. Dis. 2007;30(2):139–144. doi: 10.1007/s10545-007-0506-1. [DOI] [PubMed] [Google Scholar]
- 12.Naito E., Ito M., Matsuura S., et al. Type II citrullinaemia (Citrin Deficiency) in a neonate with hypergalactosaemia detected by mass screening. J. Inherit. Metab. Dis. 2002;25(1):71–76. doi: 10.1023/a:1015198103395. [DOI] [PubMed] [Google Scholar]
- 13.Shigetomi H., Tanaka T., Nagao M., Tsutsumi H. Early detection and diagnosis of neonatal intrahepatic cholestasis caused by citrin deficiency missed by newborn screening using tandem mass spectrometry. Int. J. Neonatal. Screen. 2018;4(1):5. doi: 10.3390/ijns4010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kikuchi A., Arai-Ichinoi N., Sakamoto O., et al. Simple and rapid genetic testing for citrin deficiency by screening 11 prevalent mutations in SLC25A13. Mol. Genet. Metab. 2012;105(4):553–558. doi: 10.1016/j.ymgme.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 15.Boenzi S., Pastore A., Martinelli D., et al. Creatine metabolism in urea cycle defects. J. Inherit. Metab. Dis. 2012;35(4):647–653. doi: 10.1007/s10545-012-9494-x. [DOI] [PubMed] [Google Scholar]
- 16.Ingoglia F., Chong J.-L., Pasquali M., Longo N. Creatine metabolism in patients with urea cycle disorders. Mol. Genet. Metabol. Rep. 2021;29 doi: 10.1016/j.ymgmr.2021.100791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Komatsu M., Kimura T., Yazaki M., et al. Steatogenesis in adult-onset type II citrullinemia is associated with down-regulation of PPARalpha. Biochim. Biophys. Acta. 2015;1852(3):473–481. doi: 10.1016/j.bbadis.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saheki T., Iijima M., Li M.X., et al. Citrin/mitochondrial glycerol-3-phosphate dehydrogenase double knock-out mice recapitulate features of human citrin deficiency. J. Biol. Chem. 2007;282(34):25041–25052. doi: 10.1074/jbc.M702031200. [DOI] [PubMed] [Google Scholar]
- 19.Numakura C., Tamiya G., Ueki M., et al. Growth impairment in individuals with citrin deficiency. J. Inherit. Metab. Dis. 2019;42(3):501–508. doi: 10.1002/jimd.12051. [DOI] [PubMed] [Google Scholar]
- 20.Tobón-Cornejo S., Vargas-Castillo A., Leyva-Martínez A., et al. PPARα/RXRα downregulates amino acid catabolism in the liver via interaction with HNF4α promoting its proteasomal degradation. Metabolism. 2021;116 doi: 10.1016/j.metabol.2021.154705. [DOI] [PubMed] [Google Scholar]
- 21.Kersten S., Mandard S., Escher P., et al. The peroxisome proliferator-activated receptor α regulates amino acid metabolism. FASEB J. 2001;15(11):1971–1978. doi: 10.1096/fj.01-0147com. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Laboratory data of patients with citrin deficiency at first visits to our hospital