Abstract
Background & Aims:
Peripheral artery disease (PAD) is characterized by elevated blood pressure (BP), low nitric oxide availability (NO), and exaggerated pressor responses to sympatho-excitatory stressors. Inorganic nitrate reduces peripheral BP in healthy and chronically diseased populations. The objective of this study was to investigate the effects of eight-weeks of sodium nitrate (NaNO3) supplementation on indices of BP in PAD patients.
Methods & Results:
21 patients with PAD were recruited to participate in this study, undergoing 8-weeks of NaNO3 (n=13; 73±9 years) or placebo (n=8; 69±10 years) supplementation. BP responsiveness to a cold pressor test (CPT) were examined prior to and following the supplementation period. The systolic BP response (change from rest) during the first (26±10 vs. 19±11mmHg) and second minutes (32±10 vs. 26±12mmHg) of CPT were reduced following NaNO3 (P<0.05 for both) but not after placebo (first minute: 22±10 vs. 24±10mmHg, P=0.30; second minute 26±10 vs 27±10mmHg, P=0.72) supplementation.
Conclusion:
Our data suggest that eight-weeks of NaNO3 supplementation reduces BP responsiveness to sympatho-excitatory stimuli.
Clinical Trials Registration Number:
Keywords: Peripheral Arterial Disease, Inorganic Nitrate, Blood Pressure, Nitric Oxide
Introduction
Peripheral arterial disease (PAD), characterized by systemic atherosclerosis, is associated with elevated blood pressure (BP), and low nitric oxide (NO) bioavailability.[1–3] Adequate BP management is crucial in these patients to reduce the risk of major adverse cardiovascular events (MACE).[4, 5] While static (in-office/clinic) BP is used to diagnose hypertension, BP responsiveness to physiological or psychological stressors are stronger predictors of future hypertension [6–10]
Supplementation with inorganic nitrate NO3− effectively reduces clinic/office BP.[11, 12] BP reduction via inorganic NO3− presents a new avenue in the management of BP in subjects with PAD. It is unclear whether inorganic NO3− supplementation improves BP responsiveness in patients with PAD. We hypothesized that NaNO3 supplementation would minimize the exaggerated BP response to sympatho-excitatory stimuli.
Methods
Study Population
Twenty-one patients with PAD participated in the study. Inclusion criteria were clinically diagnosed PAD and the ability to walk without severe leg symptoms. Exclusion criteria included non-atherosclerotic vascular disease, critical limb ischemia, active ischemic ulceration, recent (within six months) revascularization, symptomatic coronary artery disease, heart failure, renal disease, hypotension (resting systolic BP <90mmHg), smoking or history of smoking within one year, and the use of phosphodiesterase V inhibitor drugs. All women enrolled in the study were postmenopausal and not receiving hormone therapy. All subjects completed written, informed consent to participate in study protocols approved by the Institutional Review Board at the University of Iowa. This study was a Registered Clinical Trial (reference identification NCT01983826) with some of the data (e.g., demographics, resting BP, plasma [NO3−] and [NO2−]) reported previously.[13, 14]
Subjects were randomized to either 1g per day of sodium nitrate (NaNO3) or placebo (microcrystalline cellulose) supplementation for eight weeks using a 4:2 block design favoring NaNO3. All investigators were blinded to group randomization. Subjects were requested to follow a low-nitrate diet for the three days preceding all visits, refraining from exercise, alcohol, and caffeine for 24-hours before reporting to the laboratory. Subjects visited the clinical research unit at the University of Iowa Hospital and Clinics for a venous blood draw and then the laboratory for assessment of BP responsiveness to a cold pressor test (CPT).
Blood Pressure Responsiveness
After 10 minutes of seated quiet rest, the left hand of the subject was immersed in ice water (0–4°C) for two minutes. After two minutes of immersion, the hand was placed on a towel for a recovery period of three minutes. Systemic BP was assessed (beat-to-beat) via finger plethysmography (Nexfin, Edwards Lifesciences, Irvine, CA) over the middle phalanx of the right hand. The increases (Δ) in BP from baseline during the first and second minute of the CPT were used for analysis. Each reported value reflects the average BP over the final 30 seconds of each minute (i.e., 30–60 seconds and 90–120 seconds of the CPT).
Statistics
Group data are expressed as mean±SD. Baseline characteristics were assessed via independent t-tests or chi-squared analysis for categorical data. BP responses (Δ) to the CPT, as well as plasma NO3−/NO2− were compared between groups over time using a two-way repeated measures ANOVA. For these comparisons, a power analysis indicated 15 subjects were needed per group for adequate power; a detailed description of this analysis can be found elsewhere.[13] All statistical comparisons were completed using SigmaStat software version 12.0 (Systat Software Inc., San Jose, CA). Significance was set a priori at P<0.05.
Results
Table 1 illustrates subject characteristics, comorbidities, and drug regimens within the placebo and NaNO3 groups, along with brachial BP prior to supplementation in either group. Eight weeks of NaNO3 supplementation effectively elevated plasma [NO3−] and [NO2−] compared to placebo, as we have previously reported.[13]
Table 1:
Subject Characteristics
| NaNO3 (n=13) | Placebo (n=8) | P-value | |
|---|---|---|---|
| 73±9 | 69±10 | 0.32 | |
| Female, n (%) | 7 (54) | 2 (25) | 0.20 |
| Body mass index, kg/m2 | 29.2±5.9 | 28.1±3.6 | 0.63 |
| Systolic BP, mmHg | 136±15 | 132±13 | 0.46 |
| Diastolic BP, mmHg | 72±9 | 77±10 | 0.30 |
| ABI | 0.76±0.21 | 0.81±0.14 | 0.57 |
| Medical History, n (%) | |||
| Previous revascularization | 12 (92) | 6 (75) | 0.29 |
| Coronary artery disease | 3 (23) | 0 (0) | 0.15 |
| Type II diabetes mellitus | 4 (31) | 2 (25) | 0.77 |
| Prescription Medication Use, n (%) | |||
| Statin | 12 (92) | 7 (88) | 0.77 |
| ACE inhibitors or ARBs | 6 (46) | 2 (25) | 0.35 |
| Beta-blocker | 6 (46) | 3 (38) | 0.73 |
| Calcium channel blocker | 5 (38) | 2 (25) | 0.55 |
| Anticoagulants | 6 (46) | 2 (25) | 0.35 |
| Insulin | 2 (15) | 1 (13) | 0.90 |
Mean±SD or n (%). BP, blood pressure; ABI, ankle-brachial index; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker.
Blood Pressure Responsiveness
Data related to the BP responses to CPT reflect only 11 out of the 13 subjects within the NaNO3 group due to device malfunction and/or poor finger plethysmography recordings. Figure 1 depicts the change (Δ) in systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) during the CPT prior to and following the interventions. NaNO3 (P<0.01 and <0.05), but not placebo (P=0.30 and 0.72), supplementation reduced ΔSBP during minutes one and two, respectively. No significant group-by-time interactions were observed for ΔDBP (P=0.72 and 0.91) or ΔMAP (P=0.12 and 0.54) during minutes one or two, respectively.
Figure 1:
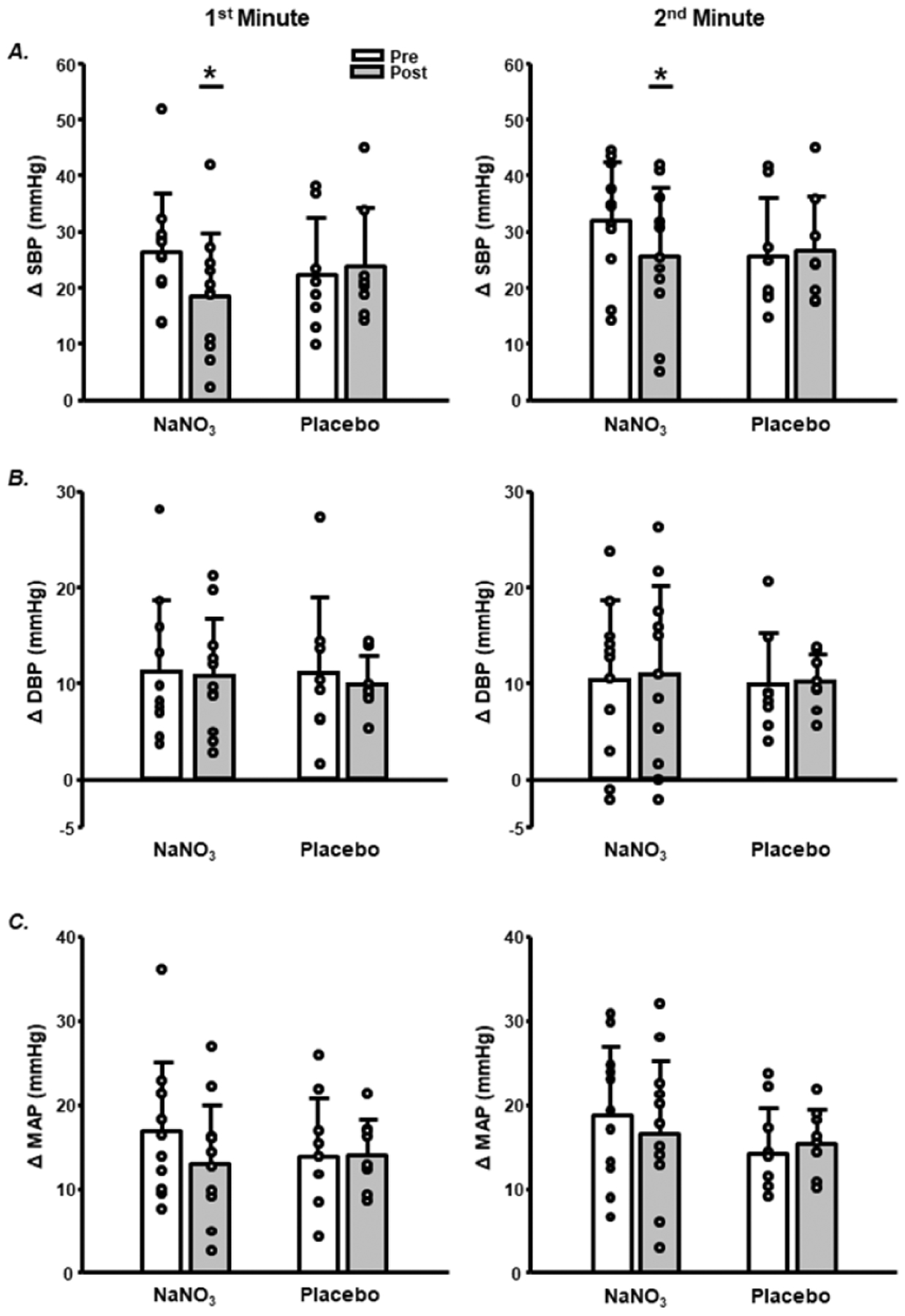
Change (Δ) from baseline in A. systolic blood pressure (SBP), B. diastolic blood pressure (DBP), and C. mean arterial pressure (MAP) during the first (left column) and last minute (right column) of cold pressor testing pre- and post-supplementation. NaNO3; sodium nitrate. Group data (bars) are mean±SD with circles representing individual responses. *P<0.05 pre-vs. post.
Discussion
This study examined the effects of eight weeks of NaNO3 supplementation on BP responsiveness in patients with PAD. Previously, we reported improvements in resting brachial SBP, but not brachial DBP or MAP in this same PAD cohort following eight weeks of NaNO3.[13, 14] Within the current study, NaNO3 supplementation improved systolic BP responsiveness to sympatho-excitatory stimuli (CPT) in patients with PAD (Figure 1).
Blood Pressure Responsiveness
Hemodynamic responses to sympatho-excitatory stimuli such as mental arithmetic or CPT are exaggerated in older and hypertensive adults relative to young adults.[9, 10] Exaggerated hemodynamic responses to physiological stressors may predispose aging populations to MACE, and may predict development of hypertension.[6, 7] Recent evidence has demonstrated that an acute dose of NO3− (beetroot juice) reduces muscle sympathetic nerve activity (MSNA) in young healthy adults,[15] while enhancing nitric oxide production via L-citrulline reduces the pressor response to a CPT in normotensive men.[16] Within the current study eight weeks NaNO3 reduced systolic BP during CPT relative to pre-measurements (Figure 1), with no changes observed in the placebo group. Conversely, NaNO3 supplementation did not have any effect on measures of diastolic BP or MAP relative to placebo. Exaggerated BP responses to physiological stimuli (e.g., exercise, cold stress) are linked to development of hypertension and increase risk for future MACE.[9, 10] Supplementation with NaNO3 reduces exaggerated systolic BP responses to sympatho-excitation in PAD patients. This suggests that NaNO3 supplementation could be a novel way to reduce risk for future MACE, opening this concept for future investigation.
Experimental Considerations
This study was not designed to examine the mechanisms contributing to how BP is reduced with inorganic NO3−. Animal models indicate that inorganic NO3− (10mmol/L; 14 days in drinking water) attenuates both age-[17] and experimentally-induced hypertension (Angiotensin II + L-NAME)[18] through reductions in NADPH oxidase-mediated oxidative stress, and modulation of angiotensin II receptors within the rostral ventrolateral medulla and kidney, associated with a reduction in sympathetic nerve activity. It could be speculated that the improvements in BP responsiveness to sympatho-excitatory stimuli with NaNO3 supplementation within the current study are perhaps due to these mechanisms, however translation of these mechanistic studies to humans are lacking.
Conclusion
This study sought to examine the effects of eight weeks of supplementation with NaNO3 on BP responsiveness in patients with PAD. Eight weeks of NaNO3 supplementation reduces systolic BP responsiveness to sympatho-excitatory stimuli. Taken together, these results suggest that while NaNO3 supplementation may have positive benefits on BP, these effects are not universally observed across various indices of BP in patients with PAD.
PAD is associated with exaggerated blood pressure responses
Patients with PAD have low nitric oxide (NO) availability
Inorganic nitrate reduces blood pressure and increases NO in healthy individuals
8 weeks of inorganic nitrate in PAD patients reduces BP responses to a cold stress.
Acknowledgements & Funding
This work was supported by the American Heart Association [13GRNT16490002, DPC] and National Institutes of Health Clinical and Translational Science Award [U54TR001356].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests
The authors have no competing interests or conflicts to report.
References
- [1].de Haro Miralles J, Martinez-Aguilar E, Florez A, Varela C, Bleda S, Acin F. Nitric oxide: link between endothelial dysfunction and inflammation in patients with peripheral arterial disease of the lower limbs. Interactive cardiovascular and thoracic surgery. 2009;9:107–12. [DOI] [PubMed] [Google Scholar]
- [2].Fowkes FG, Aboyans V, Fowkes FJ, McDermott MM, Sampson UK, Criqui MH. Peripheral artery disease: epidemiology and global perspectives. Nature reviews Cardiology. 2017;14:156–70. [DOI] [PubMed] [Google Scholar]
- [3].Jiang J, Zheng JP, Li Y, Gan Z, Jiang Y, Huang D, et al. Differential contribution of endothelium-derived relaxing factors to vascular reactivity in conduit and resistance arteries from normotensive and hypertensive rats. Clinical and experimental hypertension (New York, NY : 1993). 2016;38:393–8. [DOI] [PubMed] [Google Scholar]
- [4].Clement DL, De Buyzere ML, Duprez DA. Hypertension in peripheral arterial disease. Current pharmaceutical design. 2004;10:3615–20. [DOI] [PubMed] [Google Scholar]
- [5].Fudim M, Hopley CW, Huang Z, Kavanagh S, Rockhold FW, Baumgartner I, et al. Association of Hypertension and Arterial Blood Pressure on Limb and Cardiovascular Outcomes in Symptomatic Peripheral Artery Disease: The EUCLID Trial. Circulation Cardiovascular quality and outcomes. 2020;13:e006512. [DOI] [PubMed] [Google Scholar]
- [6].Wood DL, Sheps SG, Elveback LR, Schirger A. Cold pressor test as a predictor of hypertension. Hypertension. 1984;6:301–6. [DOI] [PubMed] [Google Scholar]
- [7].Schindler TH, Hornig B, Buser PT, Olschewski M, Magosaki N, Pfisterer M, et al. Prognostic value of abnormal vasoreactivity of epicardial coronary arteries to sympathetic stimulation in patients with normal coronary angiograms. Arteriosclerosis, thrombosis, and vascular biology. 2003;23:495–501. [DOI] [PubMed] [Google Scholar]
- [8].Schultz MG, Picone DS, Nikolic SB, Williams AD, Sharman JE. Exaggerated blood pressure response to early stages of exercise stress testing and presence of hypertension. Journal of science and medicine in sport. 2016;19:1039–42. [DOI] [PubMed] [Google Scholar]
- [9].Monahan KD, Feehan RP, Sinoway LI, Gao Z. Contribution of sympathetic activation to coronary vasodilatation during the cold pressor test in healthy men: effect of ageing. The Journal of physiology. 2013;591:2937–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Matsukawa T, Gotoh E, Uneda S, Miyajima E, Shionoiri H, Tochikubo O, et al. Augmented sympathetic nerve activity in response to stressors in young borderline hypertensive men. Acta physiologica Scandinavica. 1991;141:157–65. [DOI] [PubMed] [Google Scholar]
- [11].Ashor AW, Lara J, Siervo M. Medium-term effects of dietary nitrate supplementation on systolic and diastolic blood pressure in adults: a systematic review and meta-analysis. Journal of hypertension. 2017;35:1353–9. [DOI] [PubMed] [Google Scholar]
- [12].Siervo M, Lara J, Ogbonmwan I, Mathers JC. Inorganic nitrate and beetroot juice supplementation reduces blood pressure in adults: a systematic review and meta-analysis. The Journal of nutrition. 2013;143:818–26. [DOI] [PubMed] [Google Scholar]
- [13].Bock JM, Treichler DP, Norton SL, Ueda K, Hughes WE, Casey DP. Inorganic nitrate supplementation enhances functional capacity and lower-limb microvascular reactivity in patients with peripheral artery disease. Nitric oxide : biology and chemistry / official journal of the Nitric Oxide Society. 2018;80:45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kruse NT, Ueda K, Hughes WE, Casey DP. Eight weeks of nitrate supplementation improves blood flow and reduces the exaggerated pressor response during forearm exercise in peripheral artery disease. American journal of physiology Heart and circulatory physiology. 2018;315:H101–H8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Notay K, Incognito AV, Millar PJ. Acute beetroot juice supplementation on sympathetic nerve activity: a randomized, double-blind, placebo-controlled proof-of-concept study. American journal of physiology Heart and circulatory physiology. 2017;313:H59–H65. [DOI] [PubMed] [Google Scholar]
- [16].Figueroa A, Trivino JA, Sanchez-Gonzalez MA, Vicil F. Oral L-citrulline supplementation attenuates blood pressure response to cold pressor test in young men. American journal of hypertension. 2010;23:12–6. [DOI] [PubMed] [Google Scholar]
- [17].Hezel M, Peleli M, Liu M, Zollbrecht C, Jensen BL, Checa A, et al. Dietary nitrate improves age-related hypertension and metabolic abnormalities in rats via modulation of angiotensin II receptor signaling and inhibition of superoxide generation. Free radical biology & medicine. 2016;99:87–98. [DOI] [PubMed] [Google Scholar]
- [18].Guimaraes DD, Cruz JC, Carvalho-Galvao A, Zhuge Z, Marques SM, Naves LM, et al. Dietary Nitrate Reduces Blood Pressure in Rats With Angiotensin II-Induced Hypertension via Mechanisms That Involve Reduction of Sympathetic Hyperactivity. Hypertension. 2019;73:839–48. [DOI] [PubMed] [Google Scholar]


