Abstract
Background:
To identify prospectively ascertained individual and family factors that are associated with improvement in Bipolar Disorder (BD) among youths who initially presented with poor course.
Methods:
82 youths with BD with persistent poor mood symptomatology (“predominantly ill course”) were compared to 70 youths with BD who at intake had poor course, but showed improvement during the follow-up (“ill with improving course”), (ages 12.3 ± 3.3, vs. 11.7 ± 3.3 years old, at intake). Improvement was measured by the percentage of time euthymic during a mean follow-up of 12.8 years. Youths and parents were interviewed to assess psychopathology, functioning, treatment, and familial functioning and psychopathology.
Results:
Compared to the ill group, since intake, the improving group showed significantly lower subthreshold depression and hypo/mania, Attention Deficit Hyperactivity Disorder, and Disruptive Behavior Disorders. Parental Socioeconomic Status (SES) remained unchanged over time in the ill group, but progressively increased in the improving group. Importantly, the change in SES predated the improvement in the mood trajectory. The most influential variables that predicted improvement were higher SES, and absence of parental BD and Substance Use Disorder (SUD). Parental SUD also negatively affected the parental SES, which was directly associated with worse mood course.
Limitations:
Predominantly self-reported White samples may limit generalizability; other factors potentially associated with outcome (e.g., treatment adherence), were not ascertained.
Conclusions:
In addition to treating mood/comorbid psychopathology in symptomatic BD youths, to improve their prognosis, it is crucial to address their parent’s BD and SUD and promote parental education/employment.
Keywords: Bipolar Disorder, Longitudinal Course, Disease Prognosis, Prospective Cohort Study, Socioeconomic Status, Parental Psychopathology
1. Introduction
Bipolar disorder (BD) is a psychiatric illness that usually onsets before adulthood, affects on average 2% of the population, and is associated with high rates of morbidity, functional impairment, suicidality, and Substance Use Disorder (SUD) (Diler and Birmaher, 2019; Goldstein et al., 2012; Goodwin and Jamison, 2007; Merikangas et al., 2007). Thus, it is important to identify the factors associated with the course and outcome of BD to inform treatment and prevention strategies.
The Course and Outcome of Bipolar Youth (COBY) study is a multi- site, naturalistic, longitudinal research study of youths with BD followed into adulthood (Birmaher et al., 2014). COBY previously reported that youths with BD spectrum disorders (BD-I, BD-II and BD Not-Otherwise Specified, BD-NOS) showed four distinct longitudinal mood trajectories: “predominantly euthymic” (24.0%), “moderately euthymic” (34.6%), “ill with improving course” (19.1%), and “predominantly ill” (22.3%) (Birmaher et al., 2014). As compared to predominantly euthymic course, predominantly ill course was associated with childhood onset of BD, and at intake, more severe depressive and manic symptoms, suicide attempts, and history of sexual abuse. Also, lifetime family history of BD and SUD were associated with worse prognosis (Birmaher et al., 2014).
A study using similar longitudinal methodology to COBY also identified four distinct trajectories of mood symptoms in BD-I/II youths during a 2-year family-focused therapy trial, and reported that poor prognosis was associated with more severe depressive symptoms, suicidality, lower quality of life, and minority race/ethnicity at intake (Weintraub et al., 2019). Other studies in BD youths have also shown that early age of BD onset, long duration, mixed or rapid cycling episodes, psychosis, presence of subsyndromal mood symptoms, comorbid disorders, exposure to negative life events (e.g., abuse), family psychopathology (e.g., mood disorders and SUD), and low socio-economic status (SES) were associated with poor outcome (DelBello et al., 2007; Geller et al., 2004; Wozniak et al., 2011). Finally, in adults with BD, history of severe mood symptoms, comorbid disorders (e.g., anxiety, SUD), early age of mood onset, and exposure to negative life events, have also been associated with worse prognosis (Martino et al., 2017; Mazza et al., 2009; Mitchell et al., 2011; Subramanian et al., 2018).
The above noted studies, including COBY, are informative, but mainly analyzed the effects of variables ascertained at intake on the course of BD. However, with some exceptions, these variables are subject to change over time (e.g., comorbid disorders, SES), and these changes may affect the course of BD. To address this gap, in this manuscript we evaluated the effects of demographic and clinical variables during a mean of 12.8 years of COBY study follow-up.
COBY previously focused on the factors associated with poor outcome for all four trajectories (Birmaher et al., 2014). However, there was a particular group of youths that initially showed a similar trajectory to the “predominantly ill course” group, but after 3 years of follow-up, the youths in this group, on average, progressively joined the group with the best course (the “ill with improving course” group) (Birmaher et al., 2014). Thus, the main objective of this study was to evaluate the intake and longitudinal factors that were associated with this improving course over follow-up. This information will be instrumental for the treatment of BD youths who may present with a poor course.
2. Method
2.1. Participants
The methods of the parent COBY study were described in detail in prior COBY publications (Axelson et al., 2006; Birmaher et al., 2006; Birmaher et al., 2014). Briefly, the parent study included 446 youths, ages 7–17.11 years at intake, with Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) diagnosis of BD-I, BD-II, or a study operationally defined BD-NOS (APA, 1994; Axelson et al., 2006; Birmaher et al., 2014). All youths in this study continued to meet DSM BD criteria during the course of the study, while about 54% of youth with BD-NOS converted to BD--I/II over follow up into young adulthood (Birmaher et al., 2018). Youths from the parent COBY study were mainly recruited from outpatient clinics (67.6%) from the three study sites (University of Pittsburgh Medical Center, Brown University, and the University of California at Los Angeles). Those with schizophrenia, intellectual disability, autism, and mood disorders secondary to substances, medications, or medical conditions, were excluded from the study.
For the current study, 70 youths (mean age 12.3± 3.3 years old) with “ill with improving” course (BD-I/II=40 and BD-NOS=30), and 82 youths (mean age 11.7± 3.3 years old) with “predominantly ill” course (BD-I/II= 54 and BD-NOS=28) were included (Table 1). These two groups are henceforth denominated as “improving group” and “ill group,” respectively. Also, for this study, the analysis of our previous publication was extended from a mean of 8 years to 12.8 years (range: 4–18 years) (Birmaher et al., 2014). Except for greater lifetime prevalence of suicidal ideation, anxiety disorders, and more family history of suicide attempts in the ill group included in this study (p-values < 0.05), there were no other significant clinical or demographic differences between the youths in the current study and the parent COBY study relating to the ill vs improving groups (Birmaher et al., 2014).
Table 1.
Demographic, Clinical, and Family History Comparisons between Improving Group and Ill Group
| Class 3: Improving Group (n=70) | Class 4: Ill Group (n=82) | Test Statistics | ||||
|---|---|---|---|---|---|---|
| Demographics at Intake | Mean | SD | Mean | SD | Stat | p-value |
| Intake Age | 12.3 | 3.3 | 11.7 | 3.3 | t=1.03 | 0.3 |
| Hollingshead Socioeconomic Status | 3.3 | 1.1 | 3.0 | 1.3 | Z=1.65 | 0.1 |
| Age at BD Onset | 8.7 | 3.7 | 7.9 | 3.4 | Z=1.33 | 0.2 |
| N | % | N | % | χ2 Stat | p-value | |
| Sex (% Female) | 33 | 47.1 | 40 | 48.8 | 0.04 | 0.8 |
| Race (% White) | 58 | 82.9 | 65 | 79.3 | 0.32 | 0.6 |
| Living with Both Biological Parents | 27 | 38.6 | 26 | 31.7 | 0.78 | 0.4 |
| Follow-up Stats | Mean | SD | Mean | SD | Stat | p-value |
| Age at Last Assessment | 23.4 | 3.9 | 22.9 | 4.1 | t=0.87 | 0.4 |
| Duration of Follow-up (weeks) | 546.8 | 95.3 | 549.1 | 106.2 | t=0.14 | 0.9 |
| Number of Assessments | 16.6 | 5.2 | 15.3 | 5.8 | t=1.49 | 0.1 |
| Clinical Variables at Intake | N | % | N | % | χ2 Stat | p-value |
| Bipolar Subtype | ||||||
| BD-I | 39 | 55.7 | 47 | 57.3 | Fisher’s Exact Test | 0.1 |
| BD-II | 1 | 1.4 | 7 | 8.5 | ||
| BD Not Otherwise Specified | 30 | 42.9 | 28 | 34.2 | ||
| Any Anxiety Disorder | 34 | 48.6 | 35 | 42.7 | 0.53 | 0.5 |
| Attention Deficit Hyperactivity Disorder | 45 | 64.3 | 59 | 72.0 | 1.03 | 0.3 |
| Disruptive Behavior Disorder | 35 | 50.0 | 49 | 59.8 | 1.45 | 0.2 |
| Psychosis | 18 | 25.7 | 20 | 24.4 | 0.04 | 0.9 |
| Physical/Sexual Abuse | 14 | 20.0 | 20 | 24.4 | 0.42 | 0.5 |
| Follow-up Stats | Mean | SD | Mean | SD | χ2 Stat | p-value |
| Suicide Attempts (rate per 10 years) | 0.53 | 0.9 | 1.76 | 2.9 | 16.82 | <0.0001 |
| Self-Injurious Behavior (rate per 10 years) | 0.61 | 1.3 | 1.82 | 4.2 | 10.44 | 0.001 |
| Family History (Lifetime) | N | % | N | % | χ2 Stat | p-value |
| Depression | 62 | 88.6 | 78 | 95.1 | 2.23 | 0.1 |
| Bipolar Disorder* | 38 | 54.3 | 61 | 74.4 | 6.72 | 0.01 |
| Attention Deficit Hyperactivity Disorder | 41 | 59.6 | 52 | 63.4 | 0.37 | 0.5 |
| Conduct Disorder | 27 | 38.6 | 46 | 56.1 | 4.65 | 0.03 |
| Any Anxiety Disorder | 53 | 75.7 | 69 | 84.2 | 1.69 | 0.2 |
| Substance Use Disorder* | 49 | 70.0 | 72 | 87.8 | 7.37 | 0.007 |
| Suicidal Ideation | 38 | 54.3 | 51 | 62.2 | 0.97 | 0.3 |
Significant when only comparing parent disorders
Improving group= Ill with Improving Course; Ill group= Predominantly Ill Course; BD= Bipolar Disorder; DBD= Disruptive Behavior Disorder (encompasses Oppositional Defiant Disorder [ODD] and/or Conduct Disorder [CD]); SD= Standard Deviation.
2.2. Procedure
The Institutional Review Board for each study site reviewed and approved the study protocol before enrollment of participants. Informed consent and assent were obtained from the participants and parents at intake. Trained COBY research staff administered youth assessments to participants and parents in a semi-structured interview format. At 18, participants chose whether to include reports from parents or secondary informants (e.g., spouse). The research staff reviewed the participant’s symptomatic and psychosocial course with a study investigator (child psychiatrist/psychologist), who was ultimately responsible for the clinical ratings, and confirmed all diagnoses. Similar to our previous studies (Axelson et al., 2011), the consensus scores obtained after interviewing parents, secondary informants, and participants were used for the current analyses.
2.2.1. Measures
2.2.1.1. Mood Trajectory Assessments.
At intake, youths and parents/primary caretakers were directly interviewed for psychiatric disorders and treatment using the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1997). Severity of mood symptomatology was recorded at both intake and follow-up on the Kiddie Mania Rating Scale (K-MRS) (Axelson et al., 2003) and Depression Rating Scale (K-DEP) (Axelson et al., 2011). Week-by-week longitudinal change in psychiatric presentations was assessed using the Adolescent-Longitudinal Interval Follow-up Evaluation (A-LIFE) (Keller et al., 1987). The weekly ratings are quantified using the instrument’s Psychiatric Status Rating (PSR) scale (Keller et al., 1987). The PSR uses numeric values linked to the DSM IV criteria (APA, 1994). For mood disorders, PSR scores range on a Likert scale from 1–6; scores of ≤ 2 indicate euthymia, 3–4 subsyndromal symptoms, and ≥ 5 syndromal symptomatology.
The overall KSADS-PL kappas for psychiatric disorders were ≥0.8. The intraclass correlation coefficients for the K-MRS, the K-DEP, and syndromal/subsyndromal mood disorders ascertained through the A-LIFE PSR, were ≥0.75. The maximum scores for depression and mania on the A-LIFE PSR for the 4 weeks prior to each follow-up assessment, and the maximum scores on the K-MRS and the K-DEP for the same period, showed Spearman correlations of 0.82 (p<0.0001) and 0.77 (p<0.0001), respectively.
2.2.1.2. Functional Assessments.
Current and most severe past global functioning of the youths were assessed at intake and over follow-up using the Children’s Global Assessment Scale (CGAS) (Shaffer et al., 1983) for ages ≤ 21, and the Global Assessment of Functioning (GAF) (Endicott et al., 1976) for ages ≥ 22. Participant’s functioning in specific domains was evaluated longitudinally using the Psychosocial Functioning Schedule (PSF) of the A-LIFE (Keller et al., 1987). Until the youths turned 18 years old, family functioning was also evaluated using the child- and parent-report versions of the Conflict Behavior Questionnaire (CBQ) (Robin and Foster, 1989), and the Family Adaptability and Cohesion Evaluation Scale (FACES)-II (Olson et al., 1982).
2.2.1.3. Demographic and Other Clinical Assessments.
SES was ascertained at intake and over follow-up using the four-factor Hollingshead Scale (Hollingshead, 1975). Until the youths turned 18 years old, both parents and youths completed the Behavior Control Scale (BCS) (Gerson et al., 1996) and the Screen for Child Anxiety Related Emotional Disorders (SCARED) (Birmaher et al., 1999). The youth’s parent was interviewed at intake about his/her psychiatric history using the Structured Clinical Interview for DSM IV Diagnoses (First et al., 1995) and the psychiatric status of first/second-degree relatives using an enhanced version of the Family History Screen (Weissman et al., 2000). Family psychiatric history and parental psychiatric treatment presented in this paper represents the summary of data collected during the full length of the study.
2.3. Statistical Analyses
At intake, between-group (ill group and improving group) demographic, clinical, and family history characteristics were compared using t, Wilcoxon, chi-squared, and Fisher’s exact tests, as appropriate. Demographic variables that potentially changed over time, such as living conditions and SES, were analyzed using mixed linear regression with a random intercept to account for within-participant correlation and fitting an interaction with age (mean-centered) to test whether changes over time predicted future course. If group differences emerged in any variables over follow-up, lag-regressions were fit to assess the temporal relationship between these variables and participants’ mood symptomatology.
Given that the course of mood trajectories between the two study groups diverged on average about 3 years after study intake (Birmaher et al., 2014), an analysis was performed within the improving group to identify the turning point after which improvement began. This was analyzed within each participant via cubic spline-fitting (i.e., spline knot identification). Youths whose improvements were estimated to have begun after the first year of follow-up (n=25) were then subsetted from the dataset, specifically considering the follow-up assessment immediately preceding the identified turning point. These improving group observations (cases) were then matched with observations from the ill group (controls). This was analyzed via a greedy matching algorithm (first using a one-to-one, and then a one-to-many, case-to-control scheme), and an unweighted Euclidean distance between cases/controls, based on age of BD onset, sex, current age, K-DEP, and K-MRS scores. This enabled a comparison between improving and ill youths of the same sex, who were similarly ill at similar ages, and stages of illness progression (Bergstralh and Kosanke, 2007). Conditional logistic regressions compared the two study groups on rates of comorbid illnesses and medication usage, and mixed linear regressions compared the two study groups on dimensional measures of functioning and symptom severity.
The longitudinal courses of symptomatology of the ill vs. improving groups were compared using fitting mixed regressions. Since the differential mood trajectories between ill group vs. improving group were not identified before (e.g., subthreshold/threshold depression vs. mania/hypomania) (Birmaher et al., 2014), we included mood symptomatology in our analyses (in two latent classes that were separated based on the percentage of time euthymic during the follow-up). Models for PSR outcomes were fit via mixed logistic regressions, after dichotomizing percent of follow-up period with threshold symptoms at “0% versus otherwise,” since the distributions of these variables were quite skewed, and non-remediable by mathematical transformation. Square-root transformations were, however, very effective for the K-DEP, K-MRS, SCARED, and CBQ outcome variables, and the remaining clinician and self-reports featured sufficiently normal distributions for mixed linear regression. Before models were fit, outcome variable trajectories were plotted by group to assess the functional form of age effects and examine possible age interactions with the grouping variable. In addition to age effects, longitudinal models covaried for parental SES to account for the groups’ significantly differing SES trajectories. Given that the groups did not significantly differ on any other demographic or clinical factors (all p-values > 0.1), initial models did not covary for any additional variables. Models were then subsequently run further controlling for family history of psychiatric illnesses that differed between groups. Odds ratios (ORs) and 95% confidence intervals (CIs) estimated in logistic regressions were parameterized to compare the ill group’s odds to those of the improving group. These estimates assume mean age values for all but the models with significant group-by-age interactions, for which the ORs are instead estimated at the mean age ± standard deviation (ages 13 and 24).
As noted in the Results Section, SES was an important influential factor in the course of illness. Thus, path analysis was used to test whether SES improvement over follow-up mediated the effects of parental psychiatric diagnoses on youths’ future courses of illness (i.e., ill vs. improving groups), covarying for intake age. To estimate the rate of parental SES improvement by participant, participant-specific slopes were estimated via linear mixed regression fitting a random slope effect (using all observations recorded before age 18), which served as the mediator variable in path analyses. To assess whether any other demographic or clinical factors substantially predicted improvement in the path model, Least Absolute Shrinkage and Selection Operator (LASSO) was implemented. Briefly, a LASSO is a modified form of regression that penalizes overfit models via a regularization parameter that proportionally shrinks the magnitude of estimated predictor coefficients toward zero, and in the case of less important predictors, coefficients shrink all the way to zero. In doing so, predictor selection is implicitly performed, as less important predictors are removed from the model, without the potential biases of other variable selection techniques, such as multiple comparisons and collinearity between predictor variables (Hastie et al., 2009).
Path analyses were performed using Mplus 5, times series and LASSO analyses were performed using R 3.5.1, and all other analyses were performed using SAS 9.4. All tests were conducted at the p < 0.05 level of significance.
Further analyses were conducted to assess the influence of potential confounding factors on the underlying ill and improving group differences; statistical methods implemented include mixed logistic regression, t-tests, Poisson and negative binomial regression, cross-correlation analysis, as well as simple graphical inspection.
3. Results
3.1. Demographic, Clinical, and Family History Between-Group Comparisons at Intake
At intake, in comparison with the ill group, the improving group had significantly less lifetime history of BD, Conduct Disorder (CD), and SUD, in the first/second-degree relatives (Table 1), and less lifetime history of BD and SUD in parents (p-values ≤ 0.03). There were no other between-group demographic or clinical differences at intake.
3.2. Between-Group Comparisons of Variables Ascertained During the First 3 Years of Follow-Up
Since the psychiatric course of the two groups began to separate on average about 3 years after intake (the ill group continued to have persistent psychopathology, while the improving group began to have periods of mood symptom remissions) (Birmaher et al., 2014), demographic and clinical between-group comparisons were first tested during this period (Figure 1). In comparison with the ill group, the improving group had less family history of BD, CD, and SUD at intake, and had continuously lower rates of subthreshold depression and hypo/mania, Attention Deficit Hyperactivity Disorder (ADHD), and Disruptive Behavior Disorder (DBD; incorporating Oppositional Defiant Disorder [ODD] and/or CD). Cubic spline fitting identified 25 youths in the improving group whose turning points were estimated to have begun after the first was year of follow-up. Using the follow-up assessment immediately preceding each participant’s identified turning point, these 25 youths were then matched with youths from the ill group. No significant between-group differences were identified in psychosocial functioning, non-mood symptom severity, rates of comorbid illnesses, and medication usage.
Figure 1. Latent Class Mood Trajectories between Improving Group and Ill Group.
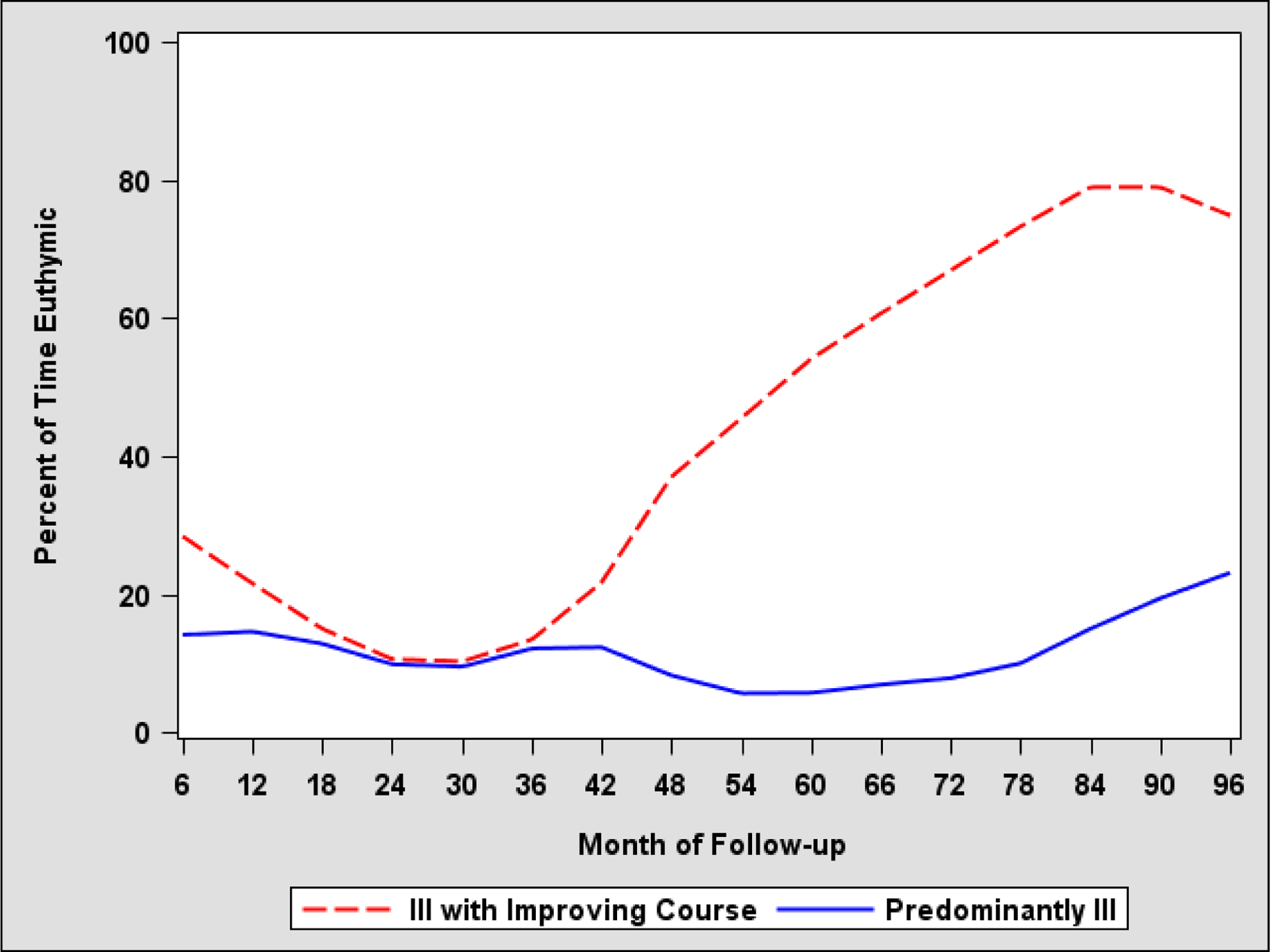
Improving group= Ill with Improving Course; Ill group= Predominantly Ill Course; the Adolescent Longitudinal Interval Follow-Up Evaluation-Intake (A-LIFE).
3.3. Between-Group Comparisons of Variables Ascertained During the Entire Length of the Follow-Up
In comparison with the ill group, the rates of subthreshold major depression, threshold and subthreshold hypo/mania, ADHD, and DBD, remained significantly lower throughout the follow-up (range 4–18 years, mean = 12.8 years) in the improving group (Table 2, Figure S.1., Figure S.2.). The improving group had approximately one third the rates of self-injurious behaviors and suicide attempts as compared to the ill group (rate ratios=3.3 and 3.0, respectively; p-values ≤ 0.001; Table 1). Except for threshold hypo/mania, which became nonsignificant, adjusting for between-group differences in family psychopathology yielded similar results.
Table 2.
Clinical Characteristics between Improving Group and Ill Group over the Length of the Follow-Up
| Categorical Disorders | Mixed Logistic Regressions | Controlling for Family History*** | Age at which contrasts became significant | ||||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | Effects | F-Stat | p-value | F-Stat | p-value | ||
| Threshold Major Depression* | Age 13: 1.7 (1.0, 2.9) | Group | 16.94 | <0.0001 | 13.38 | 0.0003 | ≥ 13 |
| Subthreshold or Worse Major Depression | 4.6 (2.7, 8.0) | Group | 30.57 | <0.0001 | 28.54 | <0.0001 | (at all ages) |
| Threshold Hypo/mania | 1.8 (1.0, 3.2) | Group | 4.35 | 0.04 | 1.49 | 0.1375 | (at all ages) |
| Subthreshold or Worse Hypo/mania | 3.2 (1.9, 5.5) | Group | 17.76 | <0.0001 | 16.25 | <0.0001 | (at all ages) |
| Anxiety* | Age 16: 1.4 (0.7, 2.7) | Group | 9.33 | 0.002 | 6.16 | 0.01 | ≥ 16 |
| Attention Deficit Hyperactivity Disorder (ADHD) | 2.3 (1.1, 4.5) | Group | 5.57 | 0.02 | 5.21 | 0.02 | (at all ages) |
| Disruptive Behavior Disorder (DBD) | 2.0 (1.0, 3.6) | Group | 4.44 | 0.03 | 4.58 | 0.03 | (at all ages) |
| Substance Use Disorder (SUD) | 1.7 (0.8, 3.8) | Group | 1.78 | 02 | 0.10 | 0.8 | - |
| Effect | F-stat | p-value | F-stat | p-value | ||
|---|---|---|---|---|---|---|
| K-DEP** | Group | 16.75 | <0.0001 | 14.48 | 0.0001 | ≥ 12 |
| K-MRS** | Group | 9.64 | 0.002 | 8.56 | 0.004 | ≥ 13 |
| SCARED - Child Report** | Group | 2.77 | 0.1 | 2.16 | 0.1 | - |
| SCARED - Parent Report** | Group | 2.80 | 0.09 | 2.70 | 0.1 | ≥ 15 |
| BCS | Group | 0.26 | 0.6 | 0.24 | 0.6 | - |
| CGAS/GAF | Group | 23.8 | <0.0001 | 24.74 | <0.0001 | ≥ 12 |
| PSF Total Score | Group | 24.39 | <0.0001 | 22.18 | <0.0001 | ≥ 13 |
| CBQ Child about Father** | Group | 0.38 | 0.5 | 0.17 | 0.7 | - |
| CBQ Child about Mother** | Group | 0.48 | 0.5 | 0.13 | 0.7 | - |
| CBQ Parent | Group | 0.36 | 0.6 | 0.02 | 0.9 | - |
| FACES Cohesion - Child Report | Group | 0.04 | 0.8 | 0.53 | 0.5 | - |
| FACES Adaptability - Child Report | Group | 1.09 | 0.3 | 1.36 | 0.2 | - |
| FACES Cohesion - Parent Report | Group | 0.04 | 0.8 | 0.20 | 0.6 | - |
| FACES Adaptability - Parent Report | Group | 0.80 | 04 | 0.58 | 0.5 | - |
Models featured a quadratic age effect and group interaction with the linear age term.
Square-root transformed.
Results are controlled for the family history of Bipolar Disorder (BD), Conduct Disorder (CD), and Substance Use Disorder (SUD).
Significant p values<0.05 are shown in bold. Kiddie Depression Rating Scale= K-DEP and Kiddie Mania Rating Scale (K-MRS); Improving group= Ill with Improving Course; Ill group= Predominantly Ill Course; Children’s Global Assessment Scale= C-GAS) and Global Assessment of Functioning= GAF; Screen for Child Anxiety Related Emotional Disorders= SCARED; Psychiatric Status Rating (PSR) and Psychosocial Functioning Schedule (PSF) of the Adolescent Longitudinal Interval Follow-Up Evaluation-Intake (A-LIFE); Behavior Control Scale (BCS); Conflict Behavior Questionnaire= CBQ; Family Adaptability and Cohesion Evaluation Scale= FACES-II.
There were several between-group differences that were identified as youths aged (Table 2). Group rates of threshold major depression became significantly different, with increasing ORs from 1.7 (95% CI=1.0–2.9) at age 13, to 3.7 (95% CI=2.2–6.2) at age 24. Similarly, rates of anxiety became significantly different, with increasing ORs from 1.4 (95% CI=0.7–2.7) at age 16, to 4.2 (95% CI=2.2–8.1) at age 24. Regarding dimensional psychopathology, mixed linear regressions showed that the ill group began having more severe depression (K-DEP, at age 12), mania (K-MRS, at age 13), parental reported anxiety (parental-SCARED, at age 15), and lower functioning (CGAS, at age 12, and A-LIFE PSF, at age 13), in comparison with the improving group (p-values ≤ 0.01, Table 2). All the above comparisons remained significant after adjusting for between-group differences in family psychopathology. Lag regressions assessed whether changes in any of the non-mood variables above preceded changes in mood symptoms. Results showed that the temporal relationship was bidirectional between anxiety and mood symptoms, indicating that anxiety and mood symptoms largely covaried together over follow-up. Conversely, results indicated that changes in mood symptoms preceded changes in functioning over follow-up.
There were no between-group differences in SES at intake (Table 1). However, in comparison with the ill group, whose SES remained constant over the follow-up, the improving group showed significant increases in SES that separated the groups by age 14 (F=4.69, p-value=0.03; Table 3, Figure S.1.). Results were similar when dichotomizing SES as low (Hollingshead Levels 1–3) vs. high (Hollingshead Levels 4–5) (F=6.59, p-value=0.01). Groups were further compared over follow-up on the individual components used to determine SES scores: education level, occupation level, and employment status of the head of the household, and their spouse/significant other. As compared to the ill group, the improving group had significant improvements in the occupation level of the head of household, as well as the education level and employment status of the spouse/significant other of the parent (all p-values ≤ 0.01, Table 3). We identified a significant temporal relationship between increases in the level of SES and the improving group’s course of illness, which suggested that the increases in SES preceded the improvement in youths’ mood symptomatology (one-lag regression effect F=9.55, p-value=0.002). Covarying for age at intake, each one-level increase in SES nearly doubled the estimated odds of improvement in the course of illness (OR=1.9, 95% CI=1.2–3.1, p-value=0.02). In contrast, the youths’ current mood symptomatology did not significantly influence future SES improvement (F=0.00, p-value=0.98).
Table 3.
Analyses of Parental Socioeconomic Status between Improving Group and Ill Group
| Parental SES Model | Parameter Estimate | F stat | p-value | |
|---|---|---|---|---|
| Effects | Group | 0.32 | 3.25 | 0.0719 |
| Age (Centered) | 0.12 | 201.63 | <0.0001 | |
| Class*Age | 0.04 | 4.69 | 0.0306 | |
| SES Component Models | Effect | F stat | p-value | |
| Head of Household | Education Level | Group | 0.31 | 0.6 |
| Age (Centered) | 0.08 | 0.8 | ||
| Class*Age | 0.09 | 0.8 | ||
| Occupation Level | Group | 0.00 | 1.0 | |
| Age (Centered) | 17.01 | <0.0001 | ||
| Class*Age | 7.24 | 0.007 | ||
| Employed | Group | 0.19 | 0.7 | |
| vs. | Age (Centered) | 1.86 | 0.2 | |
| Unemployed | Class*Age | 0.03 | 0.9 | |
| Spouse/Significant Other | Education Level | Group | 0.14 | 0.7 |
| Age (Centered) | 14.44 | 0.0002 | ||
| Class*Age | 6.12 | 0.01 | ||
| Occupation Level | Group | 0.38 | 0.5 | |
| Age (Centered) | 9.22 | 0.003 | ||
| Class*Age | 0.11 | 0.7 | ||
| Employed | Group | 1.75 | 0.2 | |
| vs. | Age (Centered) | 0.02 | 0.89 | |
| Unemployed | Class*Age | 7.62 | 0.006 | |
Significant p-values<0.05 are shown in bold.
Improving group= Ill with Improving Course; Ill group= Predominantly Ill Course; SES= Hollingshead Socioeconomic Status.
3.4. Predictors of Improvement
In addition to SES improvement, LASSO logistic regression identified parental SUD and BD, but not the youth clinical variables, such as anxiety or ADHD, as influential predictors of improvement. Path analysis was then used to test whether SES improvement mediated the effects of parental SUD and BD on youths’ odds of improvement (Figure 2). Estimated direct paths indicated that both the presence of parental BD and parental SUD halved youths’ estimated odds of illness course improvement, though both direct effects were marginally nonsignificant (parental BD: OR=0.5, 95% CI=0.27–1.10, p-value=0.09; parental SUD: OR=0.5, CI=0.26–1.06, p-value=0.07). There was, however, a statistically significant effect of parental SUD on SES change (the mediator) before adulthood (Cohen’s d=0.5, p=0.004). There was also a significant direct effect of the SES on estimated odds of improvement in illness course (standardized OR=1.5, CI=1.02–2.17, p-value=0.04).
Figure 2. Mediation Model.
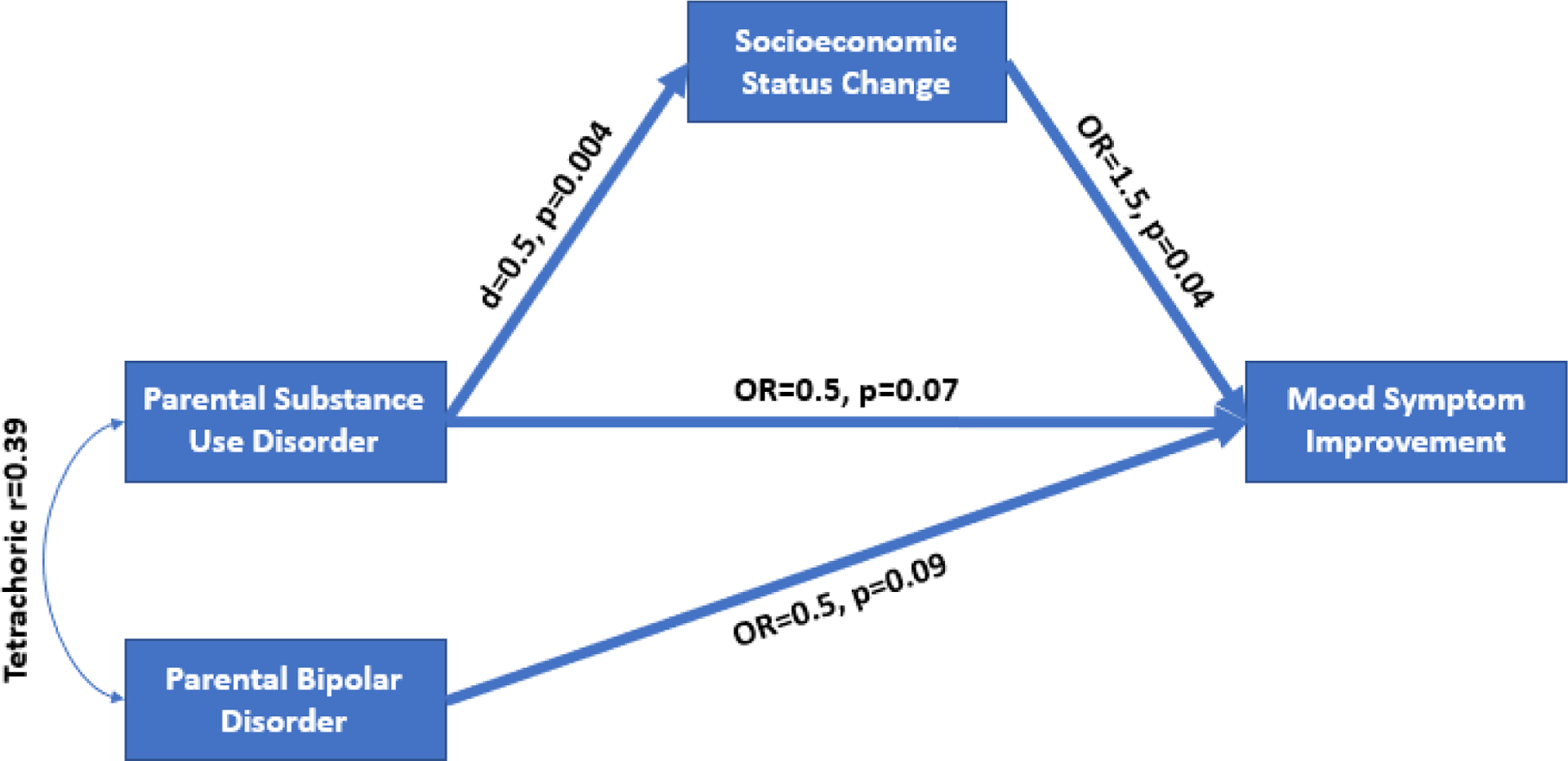
The path model above found that both the presence of parental bipolar disorder (BD) and substance use disorder (SUD) halved youths’ estimated odds of illness course improvement, though both direct effects were marginally nonsignificant (parental BD= odds ratio (OR)=0.5, 95% confidence interval (CI)=0.27–1.10, p-value=0.09; parental SUD= OR=0.5, CI=0.26–1.06, p-value=0.07). There was, however, a statistically significant effect of parental SUD on socioeconomic status (SES) change (mediator) during participants’ youth/adolescence (Cohen’s d=0.5, p=0.004), as well as a significant effect of the SES on estimated odds of improvement in illness course (standardized OR=1.5, CI=1.02–2.17, p-value=0.04).
3.5. Effects of Other Potential Confounders
Analyses were carried out to explore potential confounding factors that could explain the divergence in trajectories of psychopathology between the two groups. First, since youths may potentially under- or over-report their symptoms, the presence or absence of a parent/secondary informant (as described above) was analyzed. No between-group differences in the likelihood of having a secondary informant at any age were found (F=0.48, p-value=0.5). The second potential confounding factor analyzed was “living status after age 18,” since moving out of a conflictual household could potentially improve the youths’ symptoms. However, no between-groups differences were observed (youths moved out of parental homes at an average of 21 years old for both groups, t=0.14, p-value=0.9). Controlling for the number of assessments after youths left their homes after age 18 years old did not change the results in Table 1 and 2. Finally, considering that COBY is a naturalistic study in which the treatment is confounded by indication, the effects of psychosocial and pharmacological treatments were explored. Psychosocial treatment did not significantly differ between the two groups over follow-up. When we analyzed the percentages of follow-up time using various medication classes, none of the group or interaction effects were statistically significant (all p-values >0.25), except that youths in the ill group were more likely to use benzodiazepine medications than those in the improving group after age 18 (group effect: F=2.14, p-value=0.1; interaction: F=4.38, p-value=0.04). Cross-correlation analysis indicated that changes in symptoms and medication use occurred approximately simultaneously. However, it is important to note that the above results were from an observational study, and treatment was not systematically provided.
4. Discussion
To our knowledge, this is the first prospective BD study that compared the demographic and clinical variables between BD participants who were predominantly ill throughout follow-up, and those who were ill during the early course of the illness, but progressively improved during the follow-up. Compared to the ill group, the improving group showed lower rates of family history of BD, CD, and SUD at intake, and significantly less subthreshold depression, subthreshold hypo/mania, ADHD, and DBD over the mean 12.8 years of follow-up, including the first 3 years before the two groups diverged. As they aged toward adulthood, threshold depression was a significant differentiating factor in the groups’ diverging mood trajectories, as it showed a gradual decline in the improving group, but an increase in the ill group. There were also between-group differences in non-mood presentations that emerged over time, including improvements in global functioning, SES, and anxiety symptoms in the improving group, as compared to the ill group (in general, these contrasts became significant after ages 12–16). However, time series analyses indicated that SES improvements were the only changes that preceded changes in mood symptoms. Further, the LASSO only selected parental SES, BD, and SUD as the most influential factors on course and outcome. In fact, parental BD and SUD halved the estimated odds of improvement, as compared to those youths whose parents did not have these disorders. However, these effects, while univariately significant, were marginally significant in the full path model, possibly due to the large degree of comorbidity between these two parental disorders. Parental SUD also negatively affected the family SES, which in turn was directly associated with worse mood course in youths. Importantly, the change in SES predated the improvement in the mood trajectory; the converse was not true. There were no between-group differences in the likelihood of having a secondary informant at any age, living status after age 18, and psychosocial and medication treatments, except for more benzodiazepine medications in the ill group after age 18.
In this study, there were significant differences in trajectories of depression, mania, anxiety, ADHD, and CD between the improving and ill groups (Figure S.1.). For example, subthreshold depression and hypo/mania were significantly lower in the improving group from the beginning of the study and over the duration of the follow-up, suggesting that persistent subsyndromal mood symptoms are associated with worse prognosis. These findings are consistent with previous studies in BD that reported association of poor outcome with depression (Chang, 2009; Diler and Birmaher, 2019), mania (Diler, 2007; Diler and Birmaher, 2019; Geller et al., 2008), anxiety (Diler and Birmaher, 2019; Duffy et al., 2014; Sala et al., 2014), and ADHD and CD (Yen et al., 2016). However, for the two groups of BD youths selected for this study, these symptoms during the first 3 years of follow-up were not as influential in predicting better course as family SES and parental psychopathology.
It is well established that income-related SES disadvantage is a world-wide problem that worsens as children age and is associated with poorer overall health (van Zwieten et al., 2018). Parental income, education, and occupation (the components of SES) have substantial influences on psychopathology in youths, and some studies have reported their negative impact on the risk of depression (Bjorkenstam et al., 2017) and severity of BD (Kohler-Forsberg et al., 2020; Wozniak, 2020). Preliminary findings reported that increasing amounts of time spent in low-income conditions was linked with higher risk for schizophrenia (Hakulinen et al., 2019), and increasing the household income may lower the risk of youth crime (Akee et al., 2010), and SUD (Costello et al., 2010), thus highlighting the importance of interventions that improve social determinants of health (SDOH) early in the life-course (van Zwieten et al., 2018). Important barriers to SDOH improvement include the incomplete understanding of the dynamic associations between SES disadvantages and the development of psychopathology (van Zwieten et al., 2018), and the lack of specific and temporal correlates of SDOH (Shanahan et al., 2008), especially during the course of BD. Longitudinal studies in youth with BD reported that low SES was associated with poor outcome (DelBello et al., 2007; Geller et al., 2004; Wozniak et al., 2011). Although mechanisms are not clear for this association, it has been speculated that low SES affects the individual’s health (social causation), that health affects SES (health selection), and common background factors may influence both SES and health (indirect selection) (Hoffmann et al., 2018). Given the prospective nature of our study, our findings are able to add to the literature that improvements in SES variables preceded the improvement of mood symptoms in BD. We identified that improvement of SES was accounted for by the occupation level of the head of household, as well as the education level and employment status of the spouse/significant other of the parent. Each one level increase in SES nearly doubled the estimated odds of improvement. Furthermore, the association between SDOH and parental diagnoses of BD and SUD may be critical, as parental psychopathology may be associated with less parental monitoring, poorer family functioning, and consequently, more severe psychopathology in offspring (Birmaher et al., 2014). Similarly, previous studies have reported an important link between parental depression and poor outcome in adolescent depression (Brent et al., 1998), and successful treatment of depressed mothers was associated with improvement in functioning and psychopathology in their children (Wickramaratne et al., 2011). While living with their family, youth-family conflict and adaptability scores, and treatment interventions were not different between our study groups, both parental BD and SUD halved the estimated odds for improvement in youths’ mood symptoms between the two study groups. Importantly, the negative effect of parental SUD on mood symptoms was mediated by SES, suggesting the potential benefit for early interventions to target improving both SES and psychopathology in parents.
4.1. Limitations
The parent COBY study has limitations that should be considered when interpreting results from this study. First, while COBY is a longitudinal study, data were collected retrospectively at each assessment, and therefore subject to recall bias. Second, few youths with BD-II were included. Third, medications were prescribed under naturalistic conditions, limiting causal interpretation of our findings. Also, other important factors potentially associated with outcome, including medication dosages and blood levels, adherence to treatment, and quality of treatment, were not ascertained. Finally, as most youths were White and were recruited primarily from university settings, the generalizability of the observations to other populations remains uncertain.
5. Conclusions
Despite the above limitations, the COBY study provides a unique opportunity to identify prospectively ascertained individual and family factors that are associated with improvement in BD among youths who initially presented with poor course. Our findings suggest that, in addition to treating sub/syndromal mood psychopathology and comorbid disorders in BD youths who remain symptomatic, efforts need to focus on improving parental BD and SUD, as well as fostering better parental education and employment; factors that may increase the likelihood that their children with BD will have a better prognosis. Practical implications may include early family involvement in youth with BD, including thorough review of psychopathology, as well as implementing evidence-based interventions and social/case management services, not only to improve psychopathology, but also to foster education and give opportunity for better employment. Given the significant biological and environmental changes that occur from childhood into young adulthood (Pan et al., 2017; Schneider et al., 2012; Subramanian et al., 2017), our findings can help characterize the longitudinal factors associated with the improving course of BD and identify the critical time frames for effective interventions.
Supplementary Material
HIGHLIGHTS.
Improvement factors in symptomatic bipolar disorder (BD) youths were identified.
Predominantly ill course youths were compared to ill with improving course youths.
Improving youths had lower mood/comorbid symptomatology over 12.8 follow-up years.
Parental increases in socioeconomic status (SES) predated youth mood improvements.
Higher SES, absence of parental BD and substance use, predicted improvement.
Acknowledgements
The authors wish to thank Mr. Merranko and Dr. Iyengar for serving as the statistical experts for this research, the COBY/PROBY studies’ participants and their families for their participation, and the associated study research teams. The authors would also like to acknowledge Stacia Friedman-Hill, PhD, and Shelli Avenevoli, PhD, of NIMH, for their continued encouragement and support.
Role of the Funding Source
This research was supported by the National Institute of Mental Health (NIMH), Course and Outcome of Bipolar Youth (COBY) study grants MH059929 (PI Boris Birmaher, MD), MH059691 (PIs Martin B., Keller, MD, and Shirley Yen, PhD), and MH05977 (PI Michael Strober, PhD), and Predicting Adult Outcomes in Bipolar Youth (PROBY) study grants MH112544 (PI Boris Birmaher, MD), and MH112543 (PI Shirley Yen, PhD). The funding sources had no role in the design or conduct of this study: collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Declaration of Competing Interest
Dr. Diler has received research support from the National Institutes of Mental Health (NIMH). Dr. Hafeman has received grants from NIMH and the Klingenstein Third Generation Foundation. Dr. T. Goldstein has received grants from NIMH, the American Foundation for Suicide Prevention (AFSP), and the Brain and Behavior Foundation, and royalties from Guilford Press. Dr. B. Goldstein has received research support from Brain Canada, the Canadian Institutes for Health Research, the Heart and Stroke Foundation, NIMH, the Sunnybrook Hospital Department of Psychiatry, and the University of Toronto Department of Psychiatry. Dr. Axelson has received grants from NIMH, and personal fees from Janssen Research and Development, LLC, and UpToDate. Dr. Ryan has received grants from the National Institutes of Health (NIH). Ms. Hower has received funding from NIMH, and honoraria from the US Department of Defense (DOD) and the University of California at San Diego (UCSD) School of Medicine. Dr. Strober has received research support from NIMH, and as the Resnick Endowed Chair in Eating Disorders at the University of California, Los Angeles (UCLA). Dr. Keller has received research support from NIMH. Dr. Yen has received research support from NIMH, AFSP, and the National Center for Complementary and Integrative Health (NCCIH), and has served as a consultant at Janssen Global Services. Dr. Hunt has received honorarium from Wiley Publishers and has received support from the NIMH. Dr. Weinstock has received funding from the NCCIH, NIMH, the NIH Office of Behavioral and Social Sciences Research, and the National Institute of Justice (NIJ). Dr. Birmaher has received grants from NIMH, and royalties from Random House, UpToDate, and Lippincott, Williams, and Wilkins. Dr. Iyengar, Mr. Merranko, and Ms. Gill report no financial relationships with commercial interests.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data Statement
The research data is confidential, and therefore is unsuitable to post.
References
- Akee RK, Copeland WE, Keeler G, Angold A, Costello EJ, 2010. Parents’ Incomes and Children’s Outcomes: A Quasi-Experiment. Am Econ J Appl Econ 2, 86–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA, 1994. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.. American Psychiatric Association; Washington, DC. [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M, 2006. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry 63, 1139–1148. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N, 2003. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. Journal of child and adolescent psychopharmacology 13, 463–470. [DOI] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Strober MA, Goldstein BI, Ha W, Gill MK, Goldstein TR, Yen S, Hower H, Hunt JI, Liao F, Iyengar S, Dickstein D, Kim E, Ryan ND, Frankel E, Keller MB, 2011. Course of subthreshold bipolar disorder in youth: diagnostic progression from bipolar disorder not otherwise specified. Journal of the American Academy of Child & Adolescent Psychiatry 50, 1001–1016 e1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergstralh E, Kosanke J, 2007. Computerized matching of cases to controls using the greedy matching algorithm with a fixed number of controls per case, GMATCH. [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M, 2006. Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry 63, 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M, 1999. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38, 1230–1236. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Gill MK, Axelson DA, Goldstein BI, Goldstein TR, Yu H, Liao F, Iyengar S, Diler RS, Strober M, Hower H, Yen S, Hunt J, Merranko JA, Ryan ND, Keller MB, 2014. Longitudinal trajectories and associated baseline predictors in youths with bipolar spectrum disorders. Am J Psychiatry 171, 990–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Merranko JA, Goldstein TR, Gill MK, Goldstein BI, Hower H, Yen S, Hafeman D, Strober M, Diler RS, Axelson D, Ryan ND, Keller MB, 2018. A Risk Calculator to Predict the Individual Risk of Conversion From Subthreshold Bipolar Symptoms to Bipolar Disorder I or II in Youth. J Am Acad Child Adolesc Psychiatry 57, 755–763 e754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorkenstam E, Pebley AR, Burstrom B, Kosidou K, 2017. Childhood social adversity and risk of depressive symptoms in adolescence in a US national sample. J Affect Disord 212, 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Kolko D, Birmaher B, Baugher M, Bridge J, Roth C, Holder D, 1998. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry 37, 906–914. [DOI] [PubMed] [Google Scholar]
- Chang K, 2009. Challenges in the diagnosis and treatment of pediatric bipolar depression. Dialogues in Clinical Neuroscience 11, 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Copeland W, Angold A, 2010. Association of family income supplements in adolescence with development of psychiatric and substance use disorders in adulthood among an American Indian population. JAMA 303, 1954–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM, 2007. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode.[see comment]. American Journal of Psychiatry 164, 582–590. [DOI] [PubMed] [Google Scholar]
- Diler RS, 2007. Pediatric Bipolar Disorder: A Global Perspective. Nova Science Publishers, Inc., New York. [Google Scholar]
- Diler RS, Birmaher B, 2019. Bipolar Disorders in Children and Adolescents, in: Ray JM (Ed.), IACAPAP e-Textbook of Child and Adolescent Mental Health. International Child and Adolescent Psychiatry and Allied Professionals, Geneva, pp. 1–7. [Google Scholar]
- Duffy A, Horrocks J, Doucette S, Keown-Stoneman C, McCloskey S, Grof P, 2014. The developmental trajectory of bipolar disorder. Br J Psychiatry 204, 122–128. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J, 1976. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Archives of general psychiatry 33, 766–771. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B, 1995. The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II): Multisite test-retest reliability study. Journal of Personality Disorders 9, 92–104. [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B, 2008. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome.[see comment]. Archives of General Psychiatry 65, 1125–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Tillman R, Craney JL, Bolhofner K, 2004. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype.[see comment]. Archives of General Psychiatry 61, 459–467. [DOI] [PubMed] [Google Scholar]
- Gerson AC, Gerring JP, Freund L, Joshi PT, Capozzoli J, Brady K, Denckla MB, 1996. The Children’s Affective Lability Scale: a psychometric evaluation of reliability. Psychiatry Res 65, 189–198. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Ha W, Axelson DA, Goldstein BI, Liao F, Gill MK, Ryan ND, Yen S, Hunt J, Hower H, Keller M, Strober M, Birmaher B, 2012. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch Gen Psychiatry 69, 1113–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR, 2007. Manic-depressive illness: Bipolar Disorders and Recurrent Depression, 2nd ed. Oxford University Press, New York. [Google Scholar]
- Hakulinen C, Webb RT, Pedersen CB, Agerbo E, Mok PLH, 2019. Association Between Parental Income During Childhood and Risk of Schizophrenia Later in Life. JAMA psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastie T, Tibshirani R, Friedman J, 2009. The elements of statistical learning: prediction, inference and data mining, 2nd Edition ed. New York: Springer-Verlag. [Google Scholar]
- Hoffmann R, Kröger H, Pakpahan E, 2018. Pathways between socioeconomic status and health: Does health selection or social causation dominate in Europe?, Advances in Life Course Research. Advances in Life Course Research 36, 23–36. [Google Scholar]
- Hollingshead AA, 1975. Four-factor index of social status. Yale University, New Haven, CT. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N, 1997. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC, 1987. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of general psychiatry 44, 540–548. [DOI] [PubMed] [Google Scholar]
- Kohler-Forsberg O, Sylvia LG, Ruberto VL, Kuperberg M, Shannon AP, Fung V, Overhage L, Calabrese JR, Thase M, Bowden CL, Shelton RC, McInnis M, Deckersbach T, Tohen M, Kocsis JH, Ketter TA, Friedman ES, Iosifescu DV, McElroy S, Ostacher MJ, Nierenberg AA, 2020. Familial severe psychiatric history in bipolar disorder and correlation with disease severity and treatment response. J Affect Disord 273, 131–137. [DOI] [PubMed] [Google Scholar]
- Martino DJ, Igoa A, Scapola M, Marengo E, Samame C, Strejilevich SA, 2017. Functional Outcome in the Middle Course of Bipolar Disorder: A Longitudinal Study. J Nerv Ment Dis 205, 203–206. [DOI] [PubMed] [Google Scholar]
- Mazza M, Mandelli L, Di Nicola M, Harnic D, Catalano V, Tedeschi D, Martinotti G, Colombo R, Bria P, Serretti A, Janiri L, 2009. Clinical features, response to treatment and functional outcome of bipolar disorder patients with and without co-occurring substance use disorder: 1-year follow-up. J Affect Disord 115, 27–35. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC, 2007. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication.[erratum appears in Arch Gen Psychiatry. 2007 Sep;64(9):1039]. Archives of General Psychiatry 64, 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PB, Hadzi-Pavlovic D, Loo CK, 2011. Course and outcome of bipolar disorder. Curr Top Behav Neurosci 5, 1–18. [DOI] [PubMed] [Google Scholar]
- Olson DH, Portner J, Bell RQ, 1982. FACES II: Family Adaptability and Cohesion Evaluation Scales, Minnesota: Family Social Science, University of Minnesota. [Google Scholar]
- Pan LA, Goldstein TR, Rooks BT, Hickey M, Fan JY, Merranko J, Monk K, Diler RS, Sakolsky DJ, Hafeman D, Iyengar S, Goldstein B, Kupfer DJ, Axelson DA, Brent DA, Birmaher B, 2017. The Relationship Between Stressful Life Events and Axis I Diagnoses Among Adolescent Offspring of Probands With Bipolar and Non-Bipolar Psychiatric Disorders and Healthy Controls: The Pittsburgh Bipolar Offspring Study (BIOS). J Clin Psychiatry 78, e234–e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Foster SL, 1989. Negotiating parent-adolescent conflict. Guilford, New York. [Google Scholar]
- Sala R, Strober MA, Axelson DA, Gill MK, Castro-Fornieles J, Goldstein TR, Goldstein BI, Ha W, Liao F, Iyengar S, Yen S, Hower H, Hunt J, Dickstein DP, Ryan ND, Keller MB, Birmaher B, 2014. Effects of comorbid anxiety disorders on the longitudinal course of pediatric bipolar disorders. J Am Acad Child Adolesc Psychiatry 53, 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider MR, Delbello MP, McNamara RK, Strakowski SM, Adler CM, 2012. Neuroprogression in bipolar disorder. Bipolar Disord 14, 356–374. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S, 1983. A children’s global assessment scale (CGAS). Archives of general psychiatry 40, 1228–1231. [DOI] [PubMed] [Google Scholar]
- Shanahan L, Copeland W, Costello EJ, Angold A, 2008. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry 49, 34–42. [DOI] [PubMed] [Google Scholar]
- Subramanian K, Sarkar S, Kattimani S, Philip Rajkumar R, Penchilaiya V, 2017. Role of stressful life events and kindling in bipolar disorder: Converging evidence from a mania-predominant illness course. Psychiatry Res 258, 434–437. [DOI] [PubMed] [Google Scholar]
- Subramanian K, Sarkar S, Kattimani S, Rajkumar RP, 2018. Influence of age at onset on the course and outcome of bipolar I disorder: Findings from a retrospective study. Asian J Psychiatr 31, 135–136. [DOI] [PubMed] [Google Scholar]
- van Zwieten A, Saglimbene V, Teixeira-Pinto A, Howell M, Howard K, Craig JC, Wong G, 2018. The Impact of Age on Income-Related Health Status Inequalities from Birth to Adolescence: A Systematic Review with Cross-Country Comparisons. J Pediatr 203, 380–390 e314. [DOI] [PubMed] [Google Scholar]
- Weintraub MJ, Schneck CD, Axelson DA, Birmaher B, Kowatch RA, Miklowitz DJ, 2019. Classifying Mood Symptom Trajectories in Adolescents With Bipolar Disorder. J Am Acad Child Adolesc Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M, 2000. Brief screening for family psychiatric history: the family history screen. Archives of general psychiatry 57, 675–682. [DOI] [PubMed] [Google Scholar]
- Wickramaratne P, Gameroff MJ, Pilowsky DJ, Hughes CW, Garber J, Malloy E, King C, Cerda G, Sood AB, Alpert JE, Trivedi MH, Fava M, Rush AJ, Wisniewski S, Weissman MM, 2011. Children of depressed mothers 1 year after remission of maternal depression: findings from the STAR*D-Child study. Am J Psychiatry 168, 593–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wozniak J, 2020. Further evidence of high level of persistence of pediatric bipolar-I disorder from childhood onto young adulthood: a six-year follow up. Journal of the American Academy of Child & Adolescent Psychiatry 59, S309–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wozniak J, Petty CR, Schreck M, Moses A, Faraone SV, Biederman J, 2011. High level of persistence of pediatric bipolar-I disorder from childhood onto adolescent years: a four year prospective longitudinal follow-up study. J Psychiatr Res 45, 1273–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Stout R, Hower H, Killam MA, Weinstock LM, Topor DR, Dickstein DP, Hunt JI, Gill MK, Goldstein TR, Goldstein BI, Ryan ND, Strober M, Sala R, Axelson DA, Birmaher B, Keller MB, 2016. The influence of comorbid disorders on the episodicity of bipolar disorder in youth. Acta Psychiatr Scand 133, 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


