Abstract
Objective:
Due to limited access to psychiatrists in some emergency departments (EDs), patients presenting to an ED with acute mental illness concerns could wait days either in the ED or as a medicine/surgery admission waiting for a consultation. Telepsychiatry may improve access to care and thereby decrease ED wait times and admission rates.
Methods:
ED visits with a primary diagnosis of mental illness were identified using 2010–2018 Medicare claims. We matched 134 EDs across 22 states who implemented telepsychiatry between 2013–2016 1:1 to a control ED without telepsychiatry on a range of characteristics including availability of in-person psychiatrist consultations. Outcomes included patients’ likelihood of admission to a medical/surgery or psychiatric bed, mental illness spending, prolonged ED length of stay (LOS) (≥2 midnights in ED), 90-day mortality, and outpatient follow-up care. Using a difference-in-difference design, changes in outcomes between the three-year pre- vs. two years post-adoption at our intervention and control EDs were compared.
Results:
There were 172,708 ED visits for mental illness across the 134 matched pairs of EDs. Telepsychiatry adoption was associated with increased admissions to a psychiatric bed (differential increase 4.3%, p<0.001), decreased admissions to a medical/surgical bed (differential decrease 2.0%, p<0.001), increased likelihood of having a prolonged ED LOS (differential increase 3.0%, p<0.001), and increased mental illness spending (differential increase $292, p<0.01).
Conclusions:
Telepsychiatry adoption was associated with a lower likelihood of admission to a medical/surgery bed, but an increased likelihood of admission to a psychiatric bed and prolonged ED LOS.
Between 2006 and 2014, mental illness emergency department (ED) visits increased by 40% and the subset of visits for suicide attempts or suicidal ideation more than quadrupled.1 This growth has exacerbated challenges in providing specialty care for ED patients with mental illness. When caring for patients with acute mental illness, ED physicians rely on consultation from a psychiatrist. Unfortunately, many EDs are not routinely staffed with psychiatrists.2 Patients often wait a long time to be assessed in the ED or may be unnecessarily admitted to a medical/surgery bed awaiting evaluation.3,4
Telepsychiatry, a technology now adopted in 20% of EDs in the United States, could address the gap between psychiatry capacity and growing need in EDs nationally.2 In the telepsychiatry model, the ED provider evaluates the patient and decides whether there is a need for a psychiatrist consultation. The remote psychiatrist interviews the patient via videoconference and provides their recommendations to the ED provider. EDs with limited psychiatrist capacity have introduced telepsychiatry to improve access and quality of care to reduce ED length of stay (LOS), decreasing hospitalizations, and increasing outpatient follow-up care.5,6
Prior studies that evaluate the impact of telepsychiatry have mixed findings in terms of hospital admissions, ED LOS, mental illness outpatient follow-up care, and inpatient spending.6–9 These important studies have had limitations including focusing on just a single health system, geographic area, or telepsychiatry program. Others include not addressing temporal trends over time in outcomes or focusing on patients that received a telepsychiatry consultation as there may be selection bias in who receives a consultation versus those that do not. It remains unclear whether telepsychiatry, as implemented on a national scale across EDs, is associated with improved outcomes for patients with acute mental illness presenting to the ED.
We assessed the impact of telepsychiatry adoption in 134 EDs across 22 states between 2013–2016 on the likelihood of admission to a medical/surgical bed, admission to a psychiatric bed, mental illness spending, ED LOS, mental illness outpatient follow-up care, and mortality.
METHODS
We evaluated the impact of telepsychiatry by comparing patterns of care among patients with a mental illness diagnosis who presented to EDs with telepsychiatry capacity with patients in matched control EDs that did not have telepsychiatry.10 We included all ED visits in our analysis regardless of whether it received a telepsychiatry consultation.
We employed a difference-in-difference approach comparing the change in patterns of care in the three years before to the two years after in EDs that adopted telepsychiatry to those that did not over that same period (“control EDs”).
Telepsychiatry in EDs
Telepsychiatry provides patients with a real-time video telecommunication consultation with a psychiatrist. The psychiatrist conducts a standard history and mental status examination and has access to the medical record. The psychiatrists write a consultant note which provides recommendations for acute management. Management is facilitated by local ED staff, which includes mental health specialists (e.g., social workers). If psychiatric hospitalization is required, the bed search is conducted by local ED staff. EDs may use telepsychiatry for all consultations or consultations when a psychiatrist is unavailable (e.g., evenings, weekends).
Identifying EDs with Telepsychiatry Capacity
There is no comprehensive list of which EDs use telepsychiatry and when it was introduced. We used data from InTouch, a telemedicine company that provides infrastructure for EDs that want to deploy telepsychiatry including software and bedside videoconferencing equipment. The consulting psychiatrists, who are chosen by the local ED, can work within local health systems, academic institutions, or for private companies. InTouch provided the names and dates of telepsychiatry adoption for 134 EDs in 22 states across multiple health systems between 2013–2016. The data did not capture information on how each ED used telepsychiatry (e.g., evenings, weekends, or 24/7) or who their consulting psychiatrists were.
Data Sources and Study Sample
We used 2010–2018 de-identified data for Medicare fee-for-service beneficiaries 18 years and older: outpatient facility and inpatient claims for all beneficiaries and professional claims for a 20% sample. Telepsychiatry was introduced between 2013–6 for each ED studied, which allowed us to look at three-years pre- and two-years post-adoption.
Our analysis focused on all ED visits to short-term acute care and critical access hospitals with a primary diagnosis of mental illness (substance use disorders were excluded). Mental illnesses were identified and categorized using the Agency for Healthcare Research and Quality Clinical Classification system and ICD-9-CM and ICD-10-CM diagnoses (eAppendix).11 Lower volume mental illness diagnoses were grouped into a single “other” category. Patients could have more than one ED visit in the sample.
Treatment of mental illness may involve transfers from one facility to another. To capture “episodes” across multiple facilities, we linked ED and inpatient claim records with a mental illness primary diagnosis for the same beneficiary if their dates of service overlapped or immediately followed one another.12 For example, if a patient presented to one hospital’s ED, was kept overnight on an observation stay, and then transferred to another hospital’s psychiatric bed for an inpatient stay, this was combined into a single episode and assigned to the first hospital where the patient received care.
Patient and Hospital Characteristics
Using Medicare enrollment files we characterized patients based on age group, gender, dual enrollment in Medicaid, original reason for Medicare enrollment (old age vs. disability/end-stage renal disease), primary diagnosis for ED visit (anxiety disorders, mood disorders, schizophrenia/other psychotic disorders, suicide and self-inflicted injury, other), and having ≥1 inpatient stay or ED visit in 90 days prior to their ED visit. For each patient characteristic, we measured the standardized difference in means between the telepsychiatry and control ED visits to ensure they did not exceed 0.10, a threshold that signifies minimal difference.13
We characterized hospitals based on number of beds, Census region, availability of in-person psychiatrist care in the ED, rurality, location in Medicaid expansion state, and number of baseline mental illness ED visits. Using survey data from the 2018 American Hospital Association (AHA),14 the availability of in-person ED psychiatrist care was based on whether the hospital reported in-person psychiatric consultation services or in-person psychiatric ED care. Hospitals were classified as rural if they were located outside a metropolitan statistical area.15 The number of baseline mental illness ED visits was measured in 2010–2, the three years prior to telepsychiatry adoption in our sample.
Hospital Matching
We performed a 1:1 match based on hospital characteristics that we hypothesized impacted either the adoption of telepsychiatry or study outcomes: hospital size, census region, rural status, state Medicaid expansion status, availability of ED in-person psychiatrist care, and the number of baseline mental illness ED visits (Table 1).
Table 1:
Characteristics of the Matched Telepsychiatry and Control Emergence Departments (EDs)*
| Telepsychiatry Hospitals (N=134) | Matched Control Hospitals (N=134) | All Potential Control Hospitals^ (N=3350) |
||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Availability of In-person Psychiatrist Care in the EDa | ||||||
| No | 86 | 64 | 86 | 64 | 1,948 | 58 |
| Yes | 48 | 36 | 48 | 36 | 1,402 | 42 |
| Hospital Sizea | ||||||
| 0–99 beds | 59 | 44 | 59 | 44 | 1,659 | 50 |
| 100–400 beds | 64 | 48 | 64 | 48 | 1,455 | 43 |
| 400+ beds | 11 | 8 | 11 | 8 | 236 | 7 |
| Rural Hospitala | ||||||
| Metropolitan Area | 90 | 67 | 90 | 67 | 1,800 | 54 |
| Rural Area | 44 | 33 | 44 | 33 | 1,550 | 46 |
| Census Regiona | ||||||
| Northeast | 0 | 0 | 0 | 0 | 434 | 13 |
| Midwest | 33 | 25 | 33 | 25 | 991 | 30 |
| South | 44 | 33 | 44 | 33 | 1,315 | 39 |
| West | 57 | 43 | 57 | 43 | 610 | 18 |
| Medicaid Expansion Statea | ||||||
| No | 57 | 43 | 57 | 43 | 1,274 | 38 |
| Yes | 77 | 57 | 77 | 57 | 2,076 | 62 |
| Number of ED visits per Year at Baseline (mean)** | 120.2 | 119.6 | 131.3 | |||
Standardized difference between telepsychiatry and matched control hospitals = 0.00 for each hospital characteristic, below the 0.10 threshold signifying minimal difference consistent with established methodology
Measured as the mean number of ED visits with a mental illness primary diagnosis per year during the 3-year baseline period of January 1, 2010-December 31, 2012.
This represents the universe of acute care hospitals from which we selected our controls that do not have telepsychiatry services via InTouch in our data and with ≥1 ED visit with a primary mental illness diagnosis in each 6-month period from 2010–2018.
Indicates variable on which exact matching conducted.
Control EDs were sampled from all short-term acute care hospitals and critical access hospitals EDs that did not implement telepsychiatry via InTouch that had ≥1 ED visit with a primary mental illness diagnosis in each 6-month period from 2010–2018. To conduct the match, we used cardinality matching using the R “designmatch” package.16–22
Identification of ED visits in Telepsychiatry and Control Hospitals
ED visits were included in our analyses if they occurred at telepsychiatry or matched control EDs in the three years prior to telepsychiatry adoption or the two years post, with one exception: we excluded visits in the six-month transition period in which telepsychiatry was adopted. Each calendar year was divided into six-month blocks to facilitate the matching. For example, if the ED in Hospital A adopted telepsychiatry in February 2013, and was matched to control Hospital B, then for both hospitals the three-year pre-adoption period would be January 2010 to December 2012, the six-month transition period would be January to June 2013, and the two-year post-adoption period would be July 2013 to June 2015.
Study Outcomes
Our five outcomes were: disposition from the ED (discharge, medical/surgical admission, admission to psychiatric specialty bed), prolonged ED LOS, 90-day mental illness institutional spending (defined below), mental illness outpatient follow-up care, and 90-day mortality. Admission to a psychiatric specialty bed included admission to a psychiatric hospital or a psychiatric unit within an acute care hospital.
Our data only provide the day of admission and discharge and we cannot measure ED LOS in hours. Consistent with prior work,7 we captured prolonged ED LOS with a dichotomous measure of whether the patient spent ≥2 midnights in the ED prior to discharge or admission. ED visits that result in admission do not provide the date of admission to the hospital. In these cases, we measured the number of midnights between presentation to the ED and the date of the first professional claim for a hospital admission note. There was no admission note for 8.2% of ED visits that result in an admission. To address these missing data, we used multiple imputation (Stata’s mi impute) to impute prolonged LOS using the patient characteristics listed above. This outcome was limited to the random 20% of beneficiaries for whom we had professional claims.
Mental illness institutional spending encompassed payments to hospitals for mental illness inpatient and ED care23–26 incurred during the 90 days from ED presentation as our hypothesis was that telepsychiatry would decrease admission rates. Payments to a hospital for admission to a medical/surgical bed would be included in mental illness institutional spending if the primary diagnosis was for mental illness.
Consistent with prior work,27–29 mental illness outpatient follow-up care was the receipt of a visit with a mental illness diagnosis in the primary or secondary diagnostic field with a specialty mental health provider (psychiatrist, psychologist, social worker) within two weeks of ED discharge. Because follow-up care after an inpatient hospitalization would be unlikely to be impacted by an ED telepsychiatry consultation, this measure was limited to the subset of patients discharged from the ED and the 20% random sample of people with professional claims.
Statistical Analysis
We performed a difference-in-differences analysis to measure changes in the outcomes among patients in telepsychiatry EDs versus the matched control EDs. To minimize bias from differential changes over time in the patient population at telepsychiatry and control EDs, we adjusted our estimates for differences in patient characteristics in each time period.
To measure change, we used a series of logistic and linear regression models (appropriate for the outcome) that included an indicator for the post period, for treatment (i.e., telepsychiatry ED), and an interaction of the two terms. We clustered standard errors at the hospital level given care patterns are likely correlated within hospitals. We estimated our models in Stata 15, reporting the average marginal effects of telepsychiatry adoption.
We conducted subgroup analyses to assess heterogeneity of associations among patients with greater severity of illness vs. not (≥1 mental illness hospitalization in prior 90 days). In a sensitivity analysis, we compare the unadjusted vs. adjusted differential changes. We also tested the parallel trends assumption for each outcome in the three years prior to telepsychiatry adoption, a key assumption for difference-in-difference analyses (eAppendix).
This study was conducted between December 15, 2019 through February 1, 2021. The Harvard Faculty of Medicine Institutional Review Board exempted this study from review.
RESULTS
Telepsychiatry and Control EDs
The majority of EDs adapting telepsychiatry lacked in-person psychiatrist care (64%), were located in urban areas (67%), had fewer than 400 hospital beds (92%), and had 120.2 mental illness ED visits per year at baseline (Table 1).
Characteristics of Patients who Present to ED with a Mental Illness Diagnosis
There were 50,420 and 51,445 mental illness ED visits during the 3-year pre-period at telepsychiatry and control EDs, and 35,861 and 34,982 visits during the 2-year post-period, accounting for 2.4% of all ED visits across telepsychiatry and control EDs in the pre- and post-periods. Patient characteristics for visits at telepsychiatry and control EDs were similar in the pre-period (Table 2). However, there were modest differences in the fraction of ED visits with a primary diagnosis of suicidal ideation and intentional self-injury: 7% and 6% of ED visits in the pre- versus 14% and 11% in the post-period at telepsychiatry and control EDs.
Table 2:
Characteristics of Patients who Present to ED with a Mental Illness Diagnosis
| 3 Years Pre-Period | 2 Years Post-Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Telepsychiatry | Control | Std. Diff | Telepsychiatry | Control | Std. Diff | |||||
| N | % | N | % | N | % | N | % | |||
| Number of ED Visits with a Mental Illness Diagnosis | 50,420 | 51,445 | 35,861 | 34,982 | ||||||
| Number of Total ED Visits | 2,121,688 | 2,106,154 | 1,517,705 | 1,476,989 | ||||||
| Sex | ||||||||||
| Female | 27,832 | 55 | 26,881 | 52 | 0.05 | 19,292 | 54 | 18,343 | 52 | 0.03 |
| Male | 22,588 | 45 | 24,564 | 48 | 0.05 | 16,569 | 46 | 16,639 | 48 | 0.03 |
| Age Category | ||||||||||
| 18–29 | 3,436 | 7 | 3,328 | 6 | 0.01 | 2,344 | 7 | 2,365 | 7 | 0.01 |
| 30–39 | 7,645 | 15 | 6,856 | 13 | 0.05 | 5,666 | 16 | 5,145 | 15 | 0.03 |
| 40–49 | 8,994 | 18 | 9,214 | 18 | 0.01 | 6,249 | 17 | 5,943 | 17 | 0.01 |
| 50–59 | 10,364 | 21 | 10,872 | 21 | 0.01 | 7,373 | 21 | 7,065 | 20 | 0.01 |
| 60–64 | 3,553 | 7 | 3,574 | 7 | 0.01 | 2,772 | 8 | 2,905 | 8 | 0.02 |
| 65+ | 16,428 | 33 | 17,601 | 34 | 0.05 | 11,457 | 32 | 11,559 | 33 | 0.02 |
| Original Reason for Medicare Enrollment | ||||||||||
| Older Age | 12,302 | 24 | 13,094 | 25 | 0.04 | 8,226 | 23 | 8,277 | 24 | 0.02 |
| Disability* | 38,118 | 76 | 38,351 | 75 | 0.04 | 27,635 | 77 | 26,705 | 76 | 0.02 |
| Dual Enrollment in Medicaid | 33,352 | 66 | 34,819 | 68 | 0.02 | 24,328 | 68 | 24,287 | 69 | 0.03 |
| Primary Diagnosis** | ||||||||||
| Anxiety disorders | 13,705 | 27 | 13,244 | 26 | 0.02 | 9,926 | 28 | 9,048 | 26 | 0.04 |
| Mood disorders | 15,082 | 30 | 15,336 | 30 | 0.01 | 8,843 | 25 | 9,175 | 26 | 0.04 |
| Schizophrenia and Other Psychotic Disorders | 14,432 | 29 | 16,423 | 32 | 0.07 | 9,508 | 27 | 10,693 | 31 | 0.09 |
| Suicide and Intentional Self-Inflicted Injury | 3,318 | 7 | 2,791 | 6 | 0.05 | 4,925 | 14 | 3,734 | 11 | 0.09 |
| Other*** | 3,883 | 8 | 3,651 | 7 | 0.03 | 2,659 | 7 | 2,332 | 7 | 0.03 |
| ≥1 Inpatient Stay with Mental Illness Primary Diagnosis in 90 Days Prior to ED Visit | 10,286 | 20 | 11,835 | 23 | 0.05 | 8,111 | 23 | 8,617 | 25 | 0.05 |
| ≥1 ED Visit with Mental Illness Primary Diagnosis in 90 Days Prior to ED Visit | 11,278 | 22 | 10,554 | 21 | 0.04 | 9,464 | 26 | 8,196 | 23 | 0.07 |
Beneficiaries with end-stage renal disease were included in this category
Mental illnesses were grouped using the Agency for Healthcare Research and Quality Clinical Classification Software for ICD-9-CM and ICD-10-CM diagnosis (see eAppendix for details).10
Low volume diagnoses were grouped into a single category (see eAppendix for details)
Standardized difference between patients who present to ED with mental illness at telepsychiatry vs. matched control hospitals ≤ 0.07 for each patient characteristic, below the 0.10 threshold signifying minimal difference consistent with established methodology
Differential Change in Adjusted Outcomes at Telepsychiatry and Control EDs
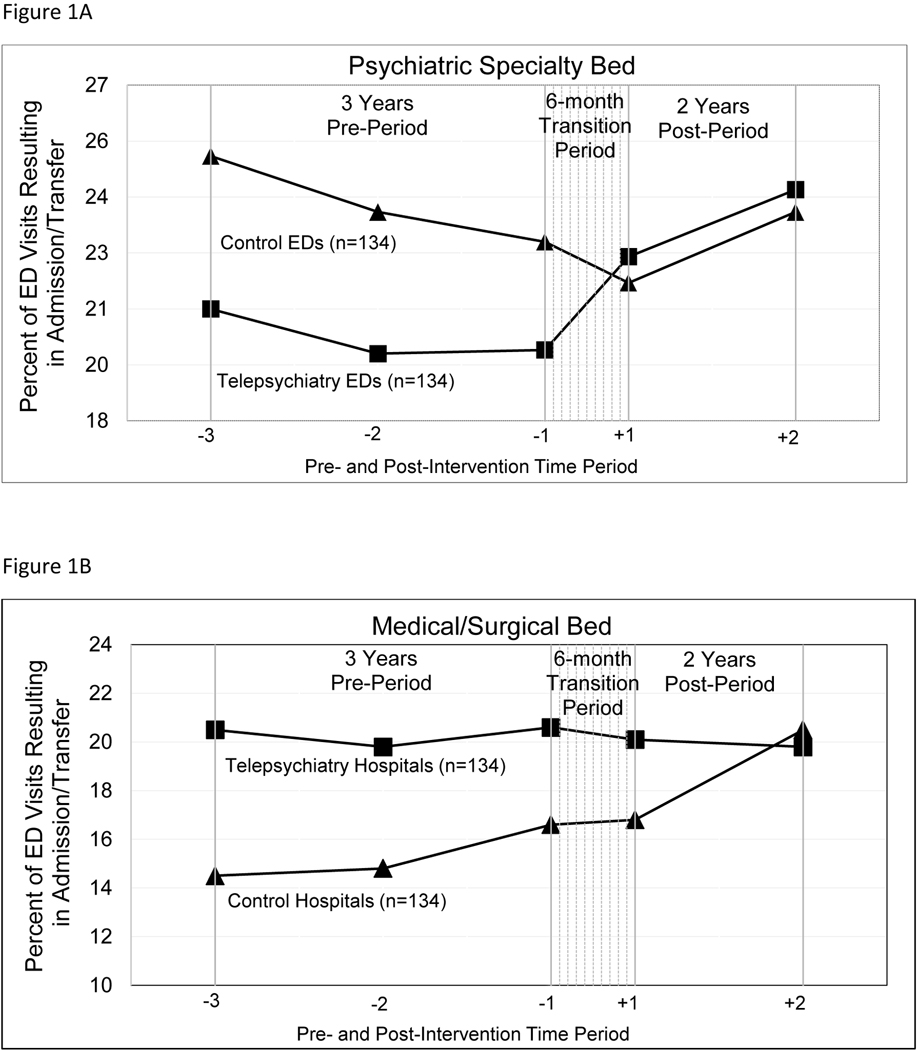
The admission rate to a psychiatric bed in the pre-period was 20.2% at telepsychiatry and 23.8% at control EDs. The admission rate increased by 3.0% at telepsychiatry and decrease by 1.2% at control EDs (Figure 1). After controlling for patient characteristics, there was a net differential increase in admission rate to a psychiatric bed of 4.3% (95% CI=3.5–5.0) at telepsychiatry EDs (Table 3 and Figure 1). In contrast, telepsychiatry adoption was associated with a differential decrease in admission to a medical/surgical bed (−2.0%, 95% CI=−2.8- −1.3). After controlling for changes in patient characteristics, there was a 2.3% differential increase in admission of any type (95% CI=1.5–3.1, p<0.001)
Figure 1a and 1b.
Admission/Transfer to a Medical Bed or Psychiatric Specialty Bed for Telepsychiatry and Control EDs from the 3 Years Pre-Period to 2 Years Post-Period (n=134 ED pairs)
Table 3:
Differential Change in Outcomes at Telepsychiatry and Control EDs (n=134 ED pairs)
| Total Number of ED Visits in Pre and Post Periods | 3 Years Pre-Period | 2 Years Post-Period | Change from Pre- to Post- | Difference-in-Differences*** | 95% Confidence Interval | p-value for difference | |
|---|---|---|---|---|---|---|---|
| ED Visits that Result in Admission/Transfer to a Psychiatric Specialty Bed (%) | 4.30% | (3.5, 5.0) | <0.001 | ||||
| Telepsychiatry | 86,281 | 20.2% | 23.2% | 3.0% | |||
| Control | 86,427 | 23.8% | 22.7% | −1.2% | |||
| ED Visits that Result in Admission/Transfer to a Medical Bed (%) | −2.00% | (−2.8, −1.3) | <0.001 | ||||
| Telepsychiatry | 86,281 | 20.3% | 19.4% | −0.9% | |||
| Control | 86,427 | 15.3% | 16.5% | 1.1% | |||
| Prolonged ED length of stay*^ (%) | 3.00% | (1.8, 4.1) | <0.001 | ||||
| Telepsychiatry | 17,156 | 7.6% | 10.5% | 2.9% | |||
| Control | 16,828 | 9.6% | 9.6% | −0.1% | |||
| Institutional Spending on Mental Illness 90 Days (mean $)** | $292 | (83, 501) | <0.01 | ||||
| Telepsychiatry | 86,281 | $6,939 | $7,734 | $795 | |||
| Control | 86,427 | $7,542 | $8,045 | $503 | |||
| Mortality in 90 Days following ED Presentation (%) | 0.20% | (−0.1, 0.4) | 0.27 | ||||
| Telepsychiatry | 86,281 | 2.0% | 1.9% | −0.1% | |||
| Control | 86,427 | 2.2% | 1.9% | −0.3% | |||
| Mental Illness Outpatient Follow-up Care in 2 Weeks following ED Discharge* (%) | −0.70% | (−3.3, 1.9) | 0.54 | ||||
| Telepsychiatry | 9,494 | 22.9% | 25.4% | 2.6% | |||
| Control | 8,245 | 21.3% | 24.6% | 3.3% |
Smaller sample, because only available in 20% random sample of Medicare beneficiaries
Excessive length of stay defined as a stay in ED that exceeds two midnights
Institutional spending encompassed payments to hospitals for inpatient and ED care incurred during the 90 days from ED presentation
Difference-in-difference estimates adjust for changes in patient characteristics.
Telepsychiatry adoption was associated with a differential increase in the fraction of ED visits with prolonged ED LOS (3.0%, 95% CI=1.8–4.1) and mental illness institutional spending ($292, 95% CI=83–501) (Table 3). In a sensitivity analysis we measured changes in total institutional spending regardless of the primary diagnosis and there was a similar differential increase at telepsychiatry hospitals ($352, 95% CI=66–639).
There was no difference between telepsychiatry and control EDs in 2-week outpatient follow-up visits (−0.7%, 95% CI=−3.3–1.9) and 90-day mortality (0.2%, 95% CI=−0.1–0.4). Our sensitivity analysis found no substantive differences between the unadjusted vs. adjusted differential changes.
In subgroup analyses, among those with greater severity of mental illness vs. not, there was a greater increase in admission to a psychiatric bed (5.3% vs. 3.8%, p<0.001), greater decrease in admission to a medical/surgical bed (−2.4% vs. −1.9%, p<0.001), greater increase in prolonged ED LOS (5.4% vs. 2.5%, p<0.001), and mental illness spending ($700 vs. $216, p=0.02) (Table 4).
Table 4:
Subgroup analysis of Patients with and without Severe Illness^^ at Telepsychiatry and Control EDs (n=134 ED pairs)
| Severe mental illness | Total No. of ED Visits in Pre and Post Periods | Change from Pre- to Post-Period at Telepsychiatry EDs (n=134) | Change from Pre- to Post-Period at Control EDs (n=134) | Difference-in-Differences*** | 95% Confidence Interval | p-value for difference |
|---|---|---|---|---|---|---|
| ED Visits that Result in Admission/Transfer to a Psychiatric Specialty Bed (%) | ||||||
| No | 133,859 | 3.10% | −0.80% | 3.80% | (3.1, 4.6) | <0.001 |
| Yes | 38,849 | 2.70% | −2.60% | 5.30% | (3.8, 6.8) | <0.001 |
| ED Visits that Result in Admission/Transfer to a Medical Bed (%) | ||||||
| No | 133,859 | −0.50% | 1.50% | −1.90% | (−2.7, −1.2) | <0.001 |
| Yes | 38,849 | −2.60% | −0.20% | −2.40% | (−4.2, −0.5) | <0.001 |
| Prolonged ED length of stay*^ (%) | ||||||
| No | 26,569 | 2.70% | 0.20% | 2.50% | (1.3, 3.8) | <0.001 |
| Yes | 7,424 | 4.40% | −1.00% | 5.40% | (2.3, 8.4) | <0.001 |
| Institutional Spending on Mental Illness 90 Days (mean $) | ||||||
| No | 133,859 | $817 | $601 | $216 | (9, 423) | 0.04 |
| Yes | 38,849 | $776 | $76 | $700 | (109, 1292) | 0.02 |
| Mortality in 90 Days following ED Presentation (%) | ||||||
| No | 133,859 | −0.10% | −0.30% | 0.20% | (−0.1, 0.5) | 0.23 |
| Yes | 38,849 | 0.00% | 0.00% | 0.00% | (−0.4, 0.4) | 0.96 |
| Mental Illness Outpatient Follow-up Care in 2 Weeks following ED Discharge* (%) | ||||||
| No | 15,338 | 3.20% | 3.80% | −0.60% | (−3.3, 2.0) | 0.6 |
| Yes | 2,401 | 0.20% | −1.30% | 1.50% | (−6.3, 9.3) | 0.7 |
Smaller sample, because only available in 20% random sample of Medicare beneficiaries
Excessive length of stay defined as a stay in ED that exceeds two midnights
Institutional spending encompassed payments to hospitals for inpatient and ED care incurred during the 90 days from ED presentation
As noted in text, more severe mental illness was captured by having one or more inpatient stays in 90 days prior to ED visit.
Difference-in-difference estimates adjust for changes in patient characteristics.
DISCUSSION
In the first large national examination of telepsychiatry in EDs, we find that telepsychiatry adoption was associated with fewer medical/surgery admissions, increased psychiatry admissions, and prolonged ED LOS.
Our finding that the overall admission rate (medical/surgery or psychiatric bed) was higher is consistent with one prior evaluation of telepsychiatry in 13 critical access hospitals.8,9 However, it conflicts with a study of 30 rural South Carolina EDs which found an overall decrease in admissions6 and another of 18 New York ED’s which reported no change in admission30 (both studies did not differentiate by type of admission). It is unclear what drives the conflicting findings. One potential driver may be differences in the patient populations, as other studies did not focus on ED visits among Medicare fee-for-service beneficiaries. Another possibility could be differences in the quality of consultation or selection biases in who received a telepsychiatry consultation. For example, the South Carolina study was limited to EDs being served by one telepsychiatry group and to patients who received a telepsychiatry consultation.
One potential underlying mechanism for the changes we observed is that consulting psychiatrists may have been more likely to recommend admission to a psychiatric bed. We did find a slight differential increase in patients being diagnosed with suicidal ideation and intentional self-injury at the intervention EDs. It is possible that the consulting psychiatrists identified more patients at risk of harming themselves or requiring more intensive psychiatric care, leading to a larger fraction of patients with prolonged ED LOS and increases in spending. Given national shortages of inpatient psychiatric beds,31 finding an inpatient bed for a patient with mental illness could take time. These patients may otherwise have been discharged from the ED, emphasizing that increased admissions to a psychiatric bed could reflect a higher quality of care in EDs with telepsychiatry. We believe the decrease in the rate of medical/surgery admissions is a mark of higher quality care.
Telepsychiatry may be beneficial financially for local EDs. From the perspective of an administrator at an acute care hospital, having fewer psychiatric admissions that are being boarded as medical admissions may be preferable given limited bed supply, and psychiatric admissions could be viewed as less lucrative than a medical/surgery admission. Also, given the low number of mental illness visits per week at many EDs, it may not be financially feasible to have in-person psychiatric capacity, and telepsychiatry may be the only option. Still, the increase in ED LOS and admission rates may lead to overcrowding in EDs.
We found no differential change in outpatient follow-up care. Further changes may be needed to help local ED providers initiate outpatient follow-up between the patient and a local mental health provider.
Our analysis has several limitations. First, ED LOS was measured as midnights in the ED as claims data do not provide admission and discharge times. Thus, our analysis captures prolonged ED LOS. Second, we only know that telepsychiatry was available in an ED but do not know how it was used (e.g., during weekends, or 24-hours) and the frequency of its use. We believe this “intention-to-treat” framework is less likely to be biased by selection of which patients receive a telepsychiatry consultation and captures the population level question of what impact adoption of telepsychiatry has on ED patterns of care. Third, our analysis is unable to capture the extent to which in-person psychiatric care is available in each ED. The AHA survey only provides a yes/no question about the availability of such care. Fourth, our analysis does not include measures of whether telepsychiatry improved clinical outcomes for patients presenting with acute mental illness. Fifth, our sample of 134 EDs across 22 states is a convenience sample and we do not know how it generalizes to all EDs with telepsychiatry. Sixth, we do not know the characteristics of psychiatrists involved in providing these services, as these data were not provided. Seventh, our study period includes the transition from ICD9 to ICD10. Prior research shows an increase in identifying intentional self-injury diagnoses following the transition.32 Finally, our findings are limited to Medicare beneficiaries and might not be generalizable to other populations, such as those with commercial insurance or Medicaid but not dual-eligible for Medicare.33
CONCLUSION
Telepsychiatry adoption was associated with fewer medical/surgery admissions, increased psychiatry admissions, and prolonged ED LOS. These changes may reflect higher quality of care if consulting psychiatrists identified more patients requiring inpatient psychiatric care who would have otherwise been discharged. Future work should assess the impact of telepsychiatry on quality of care including longer-term patient outcomes.
Supplementary Material
Highlights:
Telepsychiatry adoption was associated with fewer medical/surgery admissions, increased psychiatry admissions, and a higher likelihood of a prolonged ED length of stay.
These changes may reflect higher quality of care if consulting psychiatrists identified more patients requiring inpatient psychiatric care who would have otherwise been admitted to a medical/surgical bed or discharged from the ED.
Future work should assess the impact of telepsychiatry on hospital finances and longer-term patient outcomes.
ACKNOWLEDGEMENTS
This project was supported by the National Institute on Aging of the National Institutes of Health (K23 AG058806–01) and the National Institute of Mental Health (R01 MH112829–01, T32MH019733). We thank Rebecca Shyu for contributing to manuscript preparation and data analysis efforts.
Footnotes
No authors have conflicts of interest to disclose.
REFERENCES
- 1.Moore BJ, Stocks C, Owens PL. Trends in emergency department visits, 2006–2014. HCUP Statistical Brief #227. Agency for Healthcare Research and Quality, Rockville, MD. Published September 2017. www.hcup-us.ahrq.gov/reports/statbriefs/sb227-Emergency-Department-VisitTrends.pdf [Google Scholar]
- 2.Freeman RE, Boggs KM, Zachrison KS, et al. National study of telepsychiatry use in U.S. emergency departments. Psychiatr Serv. 2020;71(6):540–546. doi: 10.1176/appi.ps.201900237 [DOI] [PubMed] [Google Scholar]
- 3.Weiss AP, Chang G, Rauch SL, et al. Patient- and practice-related determinants of emergency department length of stay for patients with psychiatric illness. Ann Emerg Med. 2012;60(2):162–71.e5. doi: 10.1016/j.annemergmed.2012.01.037 [DOI] [PubMed] [Google Scholar]
- 4.Nicks BA, Manthey DM. The impact of psychiatric patient boarding in emergency departments. Emerg Med Int. 2012;2012:360308. doi: 10.1155/2012/360308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reinhardt I, Gouzoulis-Mayfrank E, Zielasek J. Use of telepsychiatry in emergency and crisis intervention: current evidence. Curr Psychiatry Rep. 2019;21(8). doi: 10.1007/s11920-019-1054-8 [DOI] [PubMed] [Google Scholar]
- 6.Narasimhan M, Druss BG, Hockenberry JM, et al. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatr Serv. 2015;66(11):1167–1172. doi: 10.1176/appi.ps.201400122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kothadia RJ, Jones K, Saeed SA, Torres MJ. The impact of the North Carolina statewide telepsychiatry program (NC-STeP) on patients’ dispositions from emergency departments. Psychiatr Serv. 2020;71(12):1239–1244. doi: 10.1176/appi.ps.201900431 [DOI] [PubMed] [Google Scholar]
- 8.Vakkalanka JP, Harland KK, Wittrock A, et al. Telemedicine is associated with rapid transfer and fewer involuntary holds among patients presenting with suicidal ideation in rural hospitals: a propensity matched cohort study. J Epidemiol Community Health. 2019;73(11):1033–1039. doi: 10.1136/jech-2019-212623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohr NM, Vakkalanka JP, Harland KK, et al. Telemedicine use decreases rural emergency department length of stay for transferred North Dakota trauma patients. Telemed J E Health. 2018;24(3):194–202. doi: 10.1089/tmj.2017.0083 [DOI] [PubMed] [Google Scholar]
- 10.Dimick JB, Ryan AM. Methods for Evaluating Changes in Health Care Policy. JAMA. 2014;312(22):2401–2402. doi: 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- 11.Owens PL, Heslin KC, Fingar KR, Weiss AJ. Co-occurrence of physical health conditions and mental health and substance use conditions among adult inpatient stays, 2010 versus 2014. HCUP Statistical Brief #240. Agency for Healthcare Research and Quality, Rockville, MD. Published June 2018. Revised October 2018. https://www.ncbi.nlm.nih.gov/books/NBK534105/pdf/Bookshelf_NBK534105.pdf [PubMed] [Google Scholar]
- 12.Hula L, Arguella A, Proctor K, Parker J. Recommended method for identifying inpatient hospital stays in the TAF. TAF DQ Brief #5011. Centers for Medicare & Medicaid Services, Baltimore, MD. Published November 2019. https://www.resdac.org/sites/resdac.umn.edu/files/5011_Identifying_IP_Stays.pdf [Google Scholar]
- 13.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–1234. doi: 10.1080/03610910902859574 [DOI] [Google Scholar]
- 14.AMA Physician Masterfile [database online]. American Medical Association. Updated January 1, 2018. Accessed December 20, 2020.
- 15.Medicare telehealth payment eligibility analyzer. Health Resources & Services Administration. Updated January 1, 2021. Accessed December 20, 2020. https://data.hrsa.gov/tools/medicare/telehealth
- 16.Kilcioglu C, Zubizarreta JR. Maximizing the information content of a balanced matched sample in a study of the economic performance of green buildings. Ann Appl Stat. 2016;10(4):1997–2020. doi: 10.1214/16-AOAS962 [DOI] [Google Scholar]
- 17.Zubizarreta JR, Keele L. Optimal multilevel matching in clustered observational studies: a case study of the effectiveness of private schools under a large-scale voucher system. J Am Stat Assoc. 2017;112(518):547–560. doi: 10.1080/01621459.2016.1240683 [DOI] [Google Scholar]
- 18.Visconti G, Zubizarreta JR. handling limited overlap in observational studies with cardinality matching. Observational Studies. 2018;4:2017–2249. [Google Scholar]
- 19.Zubizarreta JR. Using mixed integer programming for matching in an observational study of kidney failure after surgery. J Am Stat Assoc. 2012;107(500):1360–1371. doi: 10.1080/01621459.2012.703874 [DOI] [Google Scholar]
- 20.Zubizarreta JR, Small DS, Rosenbaum PR. Isolation in the construction of natural experiments. Ann Appl Stat. 2014;8(4):2096–2121. doi: 10.1214/14-AOAS770 [DOI] [Google Scholar]
- 21.Keele L, Titiunik R, Zubizarreta JR. Enhancing a geographic regression discontinuity design through matching to estimate the effect of ballot initiatives on voter turnout. J R Stat Soc Ser A Stat Soc. 2015;178(1):223–239. doi: 10.1111/rssa.12056 [DOI] [Google Scholar]
- 22.Zubizarreta JR, Small DS, Goyal NK, Lorch S, Rosenbaum PR. Stronger instruments via integer programming in an observational study of late preterm birth outcomes. Ann Appl Stat. 2013;7(1):25–50. doi: 10.1214/12-AOAS582 [DOI] [Google Scholar]
- 23.Barnett ML, Wilcock A, McWilliams JM, et al. Two-year evaluation of mandatory bundled payments for joint replacement. N Engl J Med. 2019;380(3):252–62. doi: 10.1056/NEJMsa1809010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finkelstein A, Ji Y, Mahoney N, Skinner J. Mandatory Medicare bundled payment program for lower extremity joint replacement and discharge to institutional postacute care: interim analysis of the first year of a 5-year randomized trial. JAMA. 2018;320(9):892–900. doi: 10.1001/jama.2018.12346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dummit L, Smathers K, Bright OJ, et al. CMS comprehensive care for joint replacement model: performance year 1 evaluation report. The Lewin Group. Published August 2018. https://innovation.cms.gov/files/reports/cjr-firstannrpt.pdf [Google Scholar]
- 26.Haas DA, Zhang X, Kaplan RS, Song Z. Evaluation of economic and clinical outcomes under Centers for Medicare & Medicaid Services mandatory bundled payments for joint replacements. JAMA Intern Med. 2019;179(7):924–931. doi: 10.1001/jamainternmed.2019.0480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patel SY, Huskamp HA, Busch AB, Mehrotra A. Telemental health and US rural–urban differences in specialty mental health use, 2010–2017. Am J Public Health. 2020;110(9):1308–1314. doi: 10.2105/AJPH.2020.305657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehrotra A, Huskamp HA, Souza J, et al. Rapid growth in mental health telemedicine use among rural Medicare beneficiaries, wide variation across states. Health Aff. 2017;36(5):909–917. doi: 10.1377/hlthaff.2016.1461 [DOI] [PubMed] [Google Scholar]
- 29.Huskamp HA, Busch AB, Souza J, et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Aff. 2018;37(12):1940–1947. doi: 10.1377/hlthaff.2018.05134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhong C, Freeman RE, Boggs KM, et al. Receipt of telepsychiatry and emergency department visit outcomes in New York state. Psychiatr Q. Published online February 15, 2021. doi: 10.1007/s11126-021-09886-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Slade E, Domino ME. Are there enough inpatient psychiatric beds? In: Goldman HH, Frank RG, Morrissey JP, eds. The Palgrave Handbook of American Mental Health Policy. Springer International Publishing; 2020:129–169. doi: 10.1007/978-3-030-11908-9_6 [DOI] [Google Scholar]
- 32.Stewart C, Crawford PM, Simon GE. Changes in coding of suicide attempts or self-harm with transition from ICD-9 to ICD-10. Psychiatr Serv. 2017;68(3):215. doi: 10.1176/appi.ps.201600450 [DOI] [PubMed] [Google Scholar]
- 33.Hazlett SB, McCarthy ML, Londer MS, Onyike CU. Epidemiology of Adult Psychiatric Visits to U.S. Emergency Departments. Academic Emergency Medicine. 2004;11(2): 193–195. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.