Abstract
Background
Thoracic trauma accounts for 20–25% of all trauma-related mortalities and the majority of these deaths occur within few hours of hospitalization. Therefore, prompt diagnosis, assessment of the severity of chest trauma, and immediate treatment are essential to prevent morbidity and mortality. The thorax trauma severity score (TTSS) can be calculated in the emergency room with ease. However, the validity of the TTSS score has still not been evaluated in the Indian setting. This study was conducted with the objective to assess the prognostic role of TTSS to predict the patient’s outcome with thoracic trauma.
Method
A prospective observational cross-sectional study was conducted at the Department of Surgery, Shri Vasantrao Naik Government Medical College, Yavatmal, India, from 1st March 2018 to 31st December 2019. A total of 284 patients, primarily admitted for chest trauma, were included in the study. TTSS was used to assess the severity of the trauma; the outcome (non-hospitalized survivors, hospitalized survivors, and hospitalized non-survivors) was recorded along with the patient’s data and the scoring system. Patients were grouped as per a TTSS score range. Group I includes patients with a TTSS score of 0–5 points, group II patients with a TTSS score of 6–10, group III patients with a TTSS score of 11–15, group IV patients with a TTTS score of 16–20, and group V patients with a TTSS score of 21–25. Fisher’s exact test was used to compare qualitative data. To evaluate the statistical significance of sensitivity and specificity and to choose suitable cut-off points to make decisions, the receiver operator curve (ROC) was used.
Results
The present study included 239 male (84.2%) and 45 female patients (15.8%) with a mean age of 41.57 with a standard deviation of ± 16 years. Sixty-seven (3.9%) patients were non-hospitalized survivors, 202 (71.1%) patients were hospitalized survivors, and 15 (5.3%) patients were hospitalized non-survivors. Two hundred and nineteen (77.1%) patients required conservative management, 49 (17.3%) had unilateral closed thoracostomy, and 11 (3.9%) patients required bilateral thoracostomy. Thoracotomy was required in 3 patients. No mortality was seen in groups I, II, and III. All the 9 patients with TTSS score 21–25 points had fatal prognoses. A TTSS score of 7.5 and above was associated with increased morbidity and mortality in patients with thoracic injuries.
Conclusion
The outcome of thoracic trauma patients can be predicted by using the TTSS. A score of 7.5 and above was associated with morbidity and a score of 20 and above predicted the fatal prognosis.
Keywords: Chest trauma, Thorax trauma severity score, Outcome prediction
Introduction
Thoracic trauma is one of the leading causes of death next only to head injury in polytrauma. It accounts for 20–25% of all trauma-related mortalities in most parts of the developed world. The majority of these deaths occur within few hours of hospitalization and are related to massive hemorrhage, hypoxia, or delay in surgical intervention. Therefore, prompt diagnosis, assessment of the severity of chest trauma, and immediate treatment are essential to prevent morbidity and mortality.
The outcome of thoracic trauma is variable and determined by the interaction between different socio-demographic and anatomical factors [1]. Although life-threatening injuries, like tension pneumothorax, can be managed with minor surgical interventions [2, 3] and few others may require major surgical intervention, the reported mortality in thoracic trauma still ranged from 15 to 25% [4]. Of the many predictors of morbidity and mortality of thoracic trauma reported in the literature, the associated extra-thoracic injuries are found to have a significant impact on the overall outcome of these patients [3].
Several scores have been developed to predict the outcomes of thoracic injuries which include the trauma and injury severity score (TRISS), to be used in polytraumatized patients and Wagner score for the pulmonary contusion [5]. However, TRISS is difficult for the calculation and it may underestimate the thoracic injuries [6]. Therefore, Pape and co-workers (2000) developed a new score, the thorax trauma severity score (TTSS) which combined the patient-related parameters with the anatomical and physiological parameters [7]. The TTSS score includes five parameters — age, PaO2/FiO2, pleural injuries, lung contusion, and rib fractures, and the score ranged from 0 to 25 points.
The validity of the TTSS score has still not been evaluated in the Indian setting. Therefore, the study was conducted to assess the prognostic role of TTSS to predict the outcome of thoracic trauma in rural tertiary care hospital of Central India.
Method
A prospective observational cross-sectional study was conducted at the Department of Surgery, Shri Vasantrao Naik Government Medical College, Yavatmal, India. The study was conducted after ethical approval from the Institutional Ethics Committee. The duration of the present study was from 1st March 2018 to 31st December 2019. A total of 284 patients, primarily admitted for chest trauma (both blunt and penetrating chest trauma), were included in the study. Patients with associated minor head injury — Glasgow Coma scale (GCS) score 15 with no loss of consciousness — and mild head injury — GCS score of 14 or 15 with loss of consciousness, extremity injury, and mild abdominal injury — were included.
Patients with severe head injury (having extradural, subdural, subarachnoid, or intraparenchymal hemorrhage and skull bone fracture) or those requiring prior neurosurgical intervention and patients with severe abdominal injury requiring surgical intervention like laparotomy were excluded from the study. Informed and written consent was obtained from the patients and their relatives.
Trauma management
All the patients were attended to in the emergency department immediately and were managed according to the Advanced Trauma Life Support (ATLS) protocol. Subsequently, it was followed by radiological evaluation such as X-ray, focused assessment with sonography in trauma (FAST), and computed tomography (CT) of the brain whenever indicated. Additional investigations, including hematological, biochemical investigation; blood grouping; and cross-matching, arterial blood gas, were done.
Treatment modalities as conservative, tube thoracostomy, and thoracotomy were performed as indicated. Oxygen supplementation, chest physiotherapy, and mechanical ventilation were used if required. For the pain management analgesics (oral/intravenous/intramuscular), intercostal nerve block, epidural analgesia was used. The severity of pain was evaluated with the help of the visual analog scale (VAS). The outcomes (non-hospitalized survivors, hospitalized survivors, and hospitalized non-survivors) were noted. Patients were followed up every week until they attained normal activity.
Patients’ information was recorded in a pre-structured questionnaire, which included their sociodemographic information, characteristics of injury, primary and associated diagnosis, the severity of trauma severity score (TTSS), medical and surgical interventions, and clinical outcomes.
Scoring system
The severity of trauma was assessed using the TTSS as shown in Table 1. Patients were grouped as per a TTSS score range. Group I includes patients with a TTSS score of 0–5, group II patients with a TTSS score of 6–10, group III patients with a TTSS score of 11–15, group IV patients with a TTSS score of 16–20, and group V patients with a TTSS score of 21–25. Association of a TTSS score and outcome were studied.
Table 1.
Items of the thorax trauma severity score (TTSS) [7]
| Grade | PaO2/FiO2 | Rib fractures | Lung contusion | Pleura | Age | Points |
|---|---|---|---|---|---|---|
| 0 | > 400 | 0 | No | No | < 30 | 0 |
| I | 300–400 | 1–3 | Unilobar unilateral | Pneumothorax | 30–41 | 1 |
| II | 200–300 | > 3 unilateral | Unilobar bilateral or bilobar unilateral | Hemothorax (unilateral) or hemo/pneumothorax (unilateral) | 42–54 | 2 |
| III | 150–200 | > 3 bilateral | Bilateral < 2 lobes | Hemothorax (bilateral) or hemo/pneumothorax (bilateral) | 55–70 | 3 |
| IV | < 150 | Flail chest | Bilateral > 2 lobes | Tension pneumothorax | > 70 | 5 |
Note: (a) For calculation of the total score, points allotted to each component are summed. (b) A minimum value is of 0 point (when all the five components have a zero score) and a maximum value is of 25 points (when all the five components have a five score)
Statistical analysis
Quantitative data were presented as mean ± standard deviation (SD) and qualitative data as frequencies and percentages. Data were summarized in the form of proportions, histogram, and table to show relationships of parameters with results. Fisher’s exact test was used to compare qualitative data. A probability value was considered statistically significant only when it was less than 0.05. To evaluate the statistical significance of sensitivity and specificity and to choose suitable cut-off points to make decisions, the receiver operator curve (ROC) was used.
Results
Of the total 798 trauma patients who were admitted, 284 patients with primary thoracic trauma were selected for the study as per our selection criteria. Two hundred and thirty-nine were male (84.2%) and 45 (15.8%) were female with a male to female ratio of 5.3:1. The mean age was 41.57 ± 16 years. There were 26 (9.2%) young patients (below 20 years), 43 (15.1%) patients were elderly (above 60 years), and maximum, i.e., 60 patients each were seen in the age group of 21–30 and 31–40 years (Fig. 1).
Fig. 1.
Distribution of age in study population
The commonest mode of injury was a road traffic accident (RTA) comprising of 207 patients (72.9%), followed by accidental fall [36 (12.7%)] and assault [29 (10.2%)]. Twelve patients (4.2%) had a history of an animal attack by a wild pig (6 cases) followed by the bull (4 cases) and tiger (2 cases).
Patients with animal attacks had mostly blunt trauma to the chest (10 cases) which were managed by conservative treatment, and only one patient with wild pig attack required unilateral tube thoracostomy. Two cases with tiger attack had penetrating chest trauma, of which one had hemopneumothorax managed with unilateral tube thoracostomy, while another had massive hemothorax with lung laceration with multiple ribs and scapula fracture which required left thoracotomy with wedge resection of the lung (Fig. 2). No mortality was seen in animal attack patients.
Fig. 2.
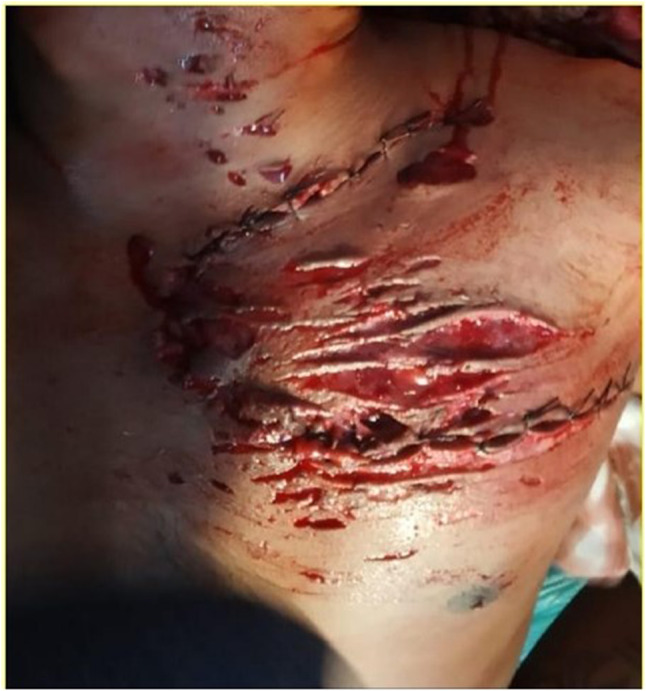
Clinical photograph of patient with tiger attack, having multiple lacerated wounds over neck and chest
In this study, 93.6% of cases with RTA had blunt trauma injury, of which isolated right-sided chest trauma was noted in 52.8% cases, whereas the left side in 41.5%. The bilateral injury was encountered in 16 cases (5.6%).
Other associated injuries were present in 40.14% of patients, of which head injury was most common (25.35%) followed by limb injuries 9.15% (abrasion, contusion, laceration) and abdominal injuries in 5.63% of patients.
Of the 217 patients who required hospitalization, 202 (71.1%) were hospitalized survivors and 15 (5.3%) patients were hospitalized non-survivors. Sixty-seven patients (23.6%) were non-hospitalized survivors. Parameters included in the TTSS score were significantly associated with outcome P-value < 0.001 (Table 2).
Table 2.
Patients’ outcome and distribution of parameters of thorax trauma severity score (TTSS)
| TTSS parameters | Outcomes of patients | p value | |||
|---|---|---|---|---|---|
| Non-hospitalized survivors N = 67 |
Hospitalized survivors N = 202 |
Hospitalized non-survivors N = 15 |
|||
| Pleural involvement | No | 67 | 110 | 0 | < 0.001 |
| Pneumothorax | 0 | 32 | 0 | ||
| Hemothorax or hemo/pneumothorax unilateral | 0 | 49 | 0 | ||
| Hemothorax or hemo/pneumothorax bilateral | 0 | 11 | 11 | ||
| Tension pneumothorax | 0 | 0 | 4 | ||
| Lung contusion | No | 67 | 125 | 0 | < 0.001 |
| Unilobar unilateral | 0 | 27 | 0 | ||
| Unilobar bilateral or bilobar unilateral | 0 | 21 | 0 | ||
| Bilateral < 2 lobes | 0 | 12 | 0 | ||
| Bilateral > 2 lobes | 0 | 17 | 15 | ||
| Rib fractures | No | 67 | 156 | 0 | < 0.001 |
| 1–3 fracture ribs | 0 | 26 | 4 | ||
| 3–6 fracture ribs | 0 | 8 | 0 | ||
| > 3 bilateral fracture ribs | 0 | 8 | 6 | ||
| Flail chest | 0 | 4 | 5 | ||
| PaO2/FiO2 | > 400 | 67 | 109 | 0 | < 0.001 |
| 300–400 | 0 | 40 | 0 | ||
| 200–300 | 0 | 23 | 0 | ||
| 150–200 | 0 | 24 | 0 | ||
| < 150 | 0 | 6 | 15 | ||
| Total | 67 | 202 | 15 | ||
Two hundred and nineteen patients (77.1%) required conservative management, 49 patients (17.3%) had unilateral closed thoracostomy, and 11 patients (3.9%) required bilateral thoracostomy. Thoracotomy was required in 3 patients (1.1%) of which one patient had penetrating chest injury with massive hemothorax and lung laceration by an animal attack (tiger).
The second patient had lung laceration with diaphragm injury (assault with penetrating injury) for which wedge resection of the lung with diaphragm repair was done. These 2 patients were survived. While in the third case, there was massive hemothorax with internal thoracic artery injury (assault with penetrating injury) for which vessel ligation and the evacuation of hemothorax was done but this patient died due to multi-organ failure in an intensive care unit (ICU).
The severity of pain was evaluated by a VAS. In this study, 86.51% of patients were managed with intramuscular or intravenous analgesia alone (non-steroidal anti-inflammatory drugs — inj. diclofenac 75 mg or opioids — inj. tramadol 50 mg in twice a day dose). Intercostal nerve block and epidural analgesia were required in 8.83% and 4.65% patients respectively. Six patients had a VAS score of 8 and four patients had a VAS score of 10.
In group I, 138 patients were having a TTSS score of 0–5 points, of which 67 patients were non-hospitalized survivors and managed only on oral analgesic (non-steroidal anti-inflammatory drugs — tab. diclofenac sodium 50 mg or opioids — tab. tramadol hydrochloride 50 mg in twice a day dose) as per VAS score of patients while 71 patients were hospitalized survivors with an average stay of 1.06 ± 2.12 days. All group I patients were managed with conservative treatment (Table 3).
Table 3.
Association of TTSS with outcome
| Group | TTSS score | No. of patients N = 284 |
Non-hospitalized survivor N = 67 |
Hospitalized survivors N = 202 |
Hospitalized non-survivors (%) N = 15 |
|---|---|---|---|---|---|
| I | 0–5 | 138 | 67 | 71 | 0 (0%) |
| II | 6–10 | 90 | 0 | 90 | 0 (0%) |
| III | 11–15 | 24 | 0 | 24 | 0 (0%) |
| IV | 16–20 | 23 | 0 | 17 | 6 (26.08%) |
| V | 21–25 | 09 | 0 | 00 | 9 (100%) |
Of the 90 patients in group II (TTSS 6–10 points), 81 were managed with conservative treatment with an average hospital stay of 6.14 ± 2.39 days, while 8 patients required unilateral thoracostomy and one patient was managed with bilateral thoracostomy.
In group III (TTSS 11–15 points), 22 of the 24 patients were managed with unilateral tube thoracostomy with an average stay of 12.59 ± 4.35 days and 2 patients required thoracotomy who survived after intervention with an average stay of 24 days. No mortality was seen in groups I, II, and III.
Seventeen of the 23 patients in group IV were managed with unilateral thoracostomy with an average stay of 15.24 ± 4.63 days. Five patients required bilateral thoracostomy amongst which four patients died after an average stay of 21.4 days. One patient died in the emergency room and another one after 15 days of hospitalization. A total of 6 patients died resulting in 26.08% mortality in group IV (TTSS 16–20 points).
Group V (TTSS 21–25 points) includes nine patients, of which two patients required unilateral thoracostomy, who died after an average of 13 days of hospital stay. Amongst the 6 patients who died after an average stay of 20.2 ± 8.94 days, bilateral thoracostomy was done in 5 patients and thoracotomy was done in 1 patient. One patient of group V died in the emergency room.
All the nine patients in group V died resulting in 100% mortality in higher TTSS score (21–25 points). The association of the severity of TTSS with the outcome of the patients tested with Fischer’s exact test was found to be statistically significant (Table 3).
A total of 45 patients (15.84%) required ICU care. Twenty-eight patients were managed in ICU care without the need of mechanical ventilation and 15 patients (5.3%) needed mechanical ventilation, including 2 patients who died in the emergency room despite giving mechanical ventilation.
In the present study, 15 out of 284 patients died (5.3%). All these patients had higher TTSS more than 16. In group IV (TTSS 16–20 points), mortality was seen in 6 patients (26.08%). We analyzed these six patients separately; 2 out of 6 patients were presented with tension pneumothorax which was diagnosed clinically and treated by needle thoracostomy followed by tube thoracostomy but one of them died in the emergency room due to late presentation in extremis. Another one survived with emergency room management but had a lung contusion which later progressed to acute respiratory distress syndrome (ARDS) leading to death after 15 days of hospital stay. The remaining four patients in group IV had bilateral chest injury with bilateral hemothorax managed with bilateral tube thoracostomy; these patients had pneumonia and sepsis after an average hospital stay of 21.4 ± 2.41 days.
In group V (TTSS 21–25 points), all the 9 patients died. One patient died in the emergency room due to hypovolaemic shock resulting from massive hemothorax. Two patients were having tension pneumothorax who survived with emergency room treatment but later had ARDS due to lung contusion leading to death after an average hospital stay of 13 days. Five patients had bilateral chest injuries with flail chest with bilateral hemopneumothorax managed with bilateral tube thoracostomy; these patients had pneumonia and sepsis after an average hospital stay of 21.4 ± 6.1 days (Table 3).
One patient in group V had a massive hemothorax due to internal thoracic artery injury (assault with penetrating injury) managed by emergency thoracotomy with ligation of vessels. The patient had atelectasis and septicemia in the post-operative period and died due to multi-organ failure in ICU after 16 days of hospital stay.
We concluded that patients with a TTSS of 7.5 points and above were associated with increased morbidity and mortality with thoracic injuries (Fig. 3).
Fig. 3.
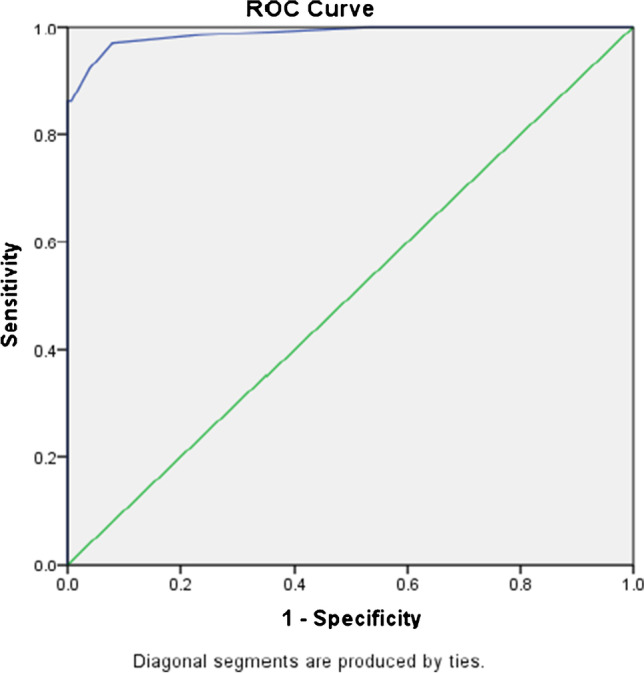
The receiver operator curve (ROC) of the predictability of thorax trauma severity score (TTSS) with area under curve equals 0.988
Discussion
Uses of scoring systems in trauma victims are of immense value in treating them. The ideal trauma scoring system should have a precise definition of injury parameters and an accurate prediction of outcomes. It should provide a prediction of morbidity and mortality associated with trauma.
At present different scoring systems for predicting the outcome of trauma are available. Some of these have an anatomical description of injuries whereas few are based on physiological parameters. The most commonly used scoring system to predict the outcome after trauma is based on combine anatomical and physiological parameters. Injury severity score (ISS) and TRISS were popular as a global polytrauma scale and proved to be useful over a period of time but consideration of patient’s age, associated comorbidity, genetic predisposition, or immunological differences bring extreme difficulty in creating a universally acceptable and applicable scoring system [8].
Chrysou et al. in their study concluded that the mortality rate in patients with polytrauma having blunt chest trauma did not correlate with the severity of chest injury but rather with the severity of associated head injury [9]. To predict the outcome in thoracic trauma, a scale that preferentially includes thoracic trauma parameters is required.
The TTSS is a specific scale made for thoracic trauma, prepared originally for patients with severe thoracic trauma which combines both anatomical and physiological parameters. Identification of trauma patients at risk of pulmonary complications, using parameters available during the initial emergency medical evaluation, was the basic purpose of scale [7].
In the present study, higher TTSS was associated with high mortality. Mortality occurred in 15 patients (5.3%) and all those had higher TTSS ranging from 16 to 22. Subhani et al. found 9.8% mortality in their study and increased mortality was seen in patients with high TTSS scores [10], and similar results were reported in the study of Elbaih et al. having ten patients (33.3%) with 0–5 score, eight patients (26.6%) with 6–10 score, six (20%) with 11–15, four (13.3%) with 16–20, and two patients (6.7%) with > 21 with the highest score attributed to high risk of mortality. All of those who had 11–20 scores were admitted to ICU and 2 patients having scores > 21–25 had early death [11]. Similarly, Aukema et al. reported that the patients who died of thoracic-related complications had higher TTSS than patients who survived (P < 0.001, CI 95%) [12].
We found that mortality was more in patients having bilateral lung contusion involving more than two lobes, which is consistent with Subhani et al. showing mortality in 10.6% patients (28) with unilateral lung contusion and 41.6% patients (110) with bilateral lung contusion [10].
In our study, most of the patients were managed with simple procedures without any life-threatening complications. Sixty-seven patients (23.6%) were non-hospitalized survivors, 202 patients were hospitalized survivors, and 15 patients were hospitalized non-survivors. Unilateral thoracostomy was required in 49 patients (17.3%) and bilateral thoracostomy in 11 patients (3.9%). Three patients (1.1%) had thoracotomy and 5.3% of patients required mechanical ventilation. In the study of Zahran et al., 148 patients (49.3%) had closed thoracostomy or observation in the inpatient ward, mechanical ventilation was required in 44 patients (14.7%), and only 4 patients (1.3%) required thoracotomy [13] which is comparable to our study. With the advancement of imaging systems, new therapeutics, and minimally invasive procedures, this trend in managing chest trauma can be explained which had a direct impact in decreasing the morbidity and mortality of thoracic trauma injuries [14].
Our study showed that the TTSS value of 7.5 points or above points had 96.9% sensitivity and 92.1% specificity to morbidity and mortality of patients of isolated thoracic trauma after exclusion of associated severe extra thoracic injuries. This result is comparable with Elbaih and co-workers, who found that the TTSS value of 7 or above was 100% sensitive and 100% specific to poor prognosis [11]. Similarly, Rezk and associates found that the TTSS value of 8 or above had a sensitivity of 92.3% and a specificity of 100% in the prediction of poor outcome and mortality [15]. In another study by Casas et al., the TTSS of 8 points had a sensitivity of 80% and a specificity of 94% to predict complications and death [16]. In the study of Pressley et al., the TTSS of 7 or 8 predicted increased risk of mortality, admission to ICU, and intubation [17]. Similarly in the study of Zahran et al., the TTSS of 7 points and above was associated with increased morbidity, and a score of 20 points and above predicted prolonged mechanical ventilation and a fatal prognosis [13].
In our study, the area under the curve was 0.988 showing that the TTSS has a strong predictive value for morbidity and mortality. In a study by Hildebrand and associates, they found the TTSS to be the best predictive value as compared to CT-dependent Wagner score for pulmonary contusion and CT-independent scoring system [18]. Whereas for predicting the mortality of severe thoracic trauma, Moon and associates found that TRISS was superior to TTSS [19]. However, this scoring system was not developed for isolated thoracic trauma and this may underestimate the importance of chest trauma in predicting mortality, also the study was conducted in a retrospective manner where the possibility of selection biases could not be ruled out.
In our study, we found that a TTSS score of 7.5 and above was associated with an increased probability of ICU stay and need of mechanical ventilation, and 100% mortality was seen in patients with a TTSS score of more than 20. This is comparable with the study of Balkan and associates, who found that there was an association between morbidity, mortality, and need for mechanical ventilation [20]. Similarly, a study conducted by Mommsen et al. concluded that the TTSS is an independent predictor of mortality amongst the thoracic trauma scores examined [5].
Conclusion
The TTSS is helpful in predicting the outcome in thoracic trauma patients. A score of 7.5 and above was associated with increased morbidity and the patient requires close monitoring. A score of 20 and above predicted high mortality.
Funding
None.
Declarations
Informed consent
Taken in writing.
Institutional Ethics committee approval
Taken.
Conflict of interest
No.
Statement of human and animal rights
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bozorgi F, Mirabi A, Chabra A, Mirabi R, Hosseininejad S-M, Zaheri H. Mechanisms of traumatic injuries in multiple trauma patients. Int J Med Invest. 2018;7:7–15. [Google Scholar]
- 2.Marx J, Walls R, Hockberger R. Rosen’s emergency medicine - concepts and clinical practice e-book 9th ed. Elseveir Health Sciences; 2017. 382–391.
- 3.Mirka H, Ferda J, Baxa J. Multidetector computed tomography of chest trauma: indications, technique and interpretation. Insights Imaging. 2012;3:433–449. doi: 10.1007/s13244-012-0187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters S, Nicolas V, Heyer CM. Multidetector computed tomography-spectrum of blunt chest wall and lung injuries in polytraumatized patients. Clin Radiol. 2010;65:333–338. doi: 10.1016/j.crad.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Mommsen P, Zeckey C, Andruszkow H, et al. Comparison of different thoracic trauma scoring systems in regards to prediction of post-traumatic complications and outcome in blunt chest trauma. J Surg Res. 2012;176:239–247. doi: 10.1016/j.jss.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 6.de Alencar Domingues C, de Souza Nogueira, Settervall CHC, de Sousa RMC. Performance of Trauma and Injury Severity Score (TRISS) adjustments: an integrative review. Rev Esc Enferm USP. 2015;49:138–46. [DOI] [PubMed]
- 7.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. [DOI] [PubMed]
- 8.Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35:347–358. doi: 10.1016/S0020-1383(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 9.Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25:42. doi: 10.1186/s13049-017-0384-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Subhani SS, Muzaffar MS, Khan MI. Comparison of outcome between low and high thoracic trauma severity score in blunt trauma chest patients. J Ayub Med Coll Abbottabad. 2014;26:474–477. [PubMed] [Google Scholar]
- 11.Elbaih A, Elshaboury I, Kalil N, El-Aouty H. Evaluation of thoracic trauma severity score in predicting the outcome of isolated blunt chest trauma patients. Int J Surg Med. 2016;2:100–106.
- 12.Aukema TS, Beenen LF, Hietbrink F, Leenen LP. Validation of the Thorax Trauma Severity Score for mortality and its value for the development of acute respiratory distress syndrome. Open Access Emerg Med. 2011;3:49–53. doi: 10.2147/OAEM.S22802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zahran MR, Elwahab AAEMA, El Nasr MMA, et al. Evaluation of the predictive value of thorax trauma severity score (TTSS) in thoracic-traumatized patients. Cardiothorac Surg. 2020. 10.1186/s43057-020-0015-7.
- 14.Trinkle JK, Richardson JD, Franz JL, Grover FL, Arom KV, Holmstrom FM. Management of flail chest without mechanical ventilation. Ann Thorac Surg. 1975;19:355–363. doi: 10.1016/S0003-4975(10)64034-9. [DOI] [PubMed] [Google Scholar]
- 15.Rezk ME, El Nahas AM, Mohamed M, Saad DA. Assessment of isolated blunt chest trauma patients in Benha University Hospital according to thoracic trauma severity score. Am J Cardiovasc Thorac Surg. 2020;5:1–8.
- 16.Casas IM, Marchante MAA, Paduraru M, Fabregues Olea AI, Nolasco A, Medina JC. Thorax Trauma Severity Score: is it reliable for patient’s evaluation in a secondary level hospital? Bull Emerg Trauma. 2016;4:150–5. [PMC free article] [PubMed]
- 17.Pressley CM, Fry WR, Philp AS, Berry SD, Smith RS. Predicting outcome of patients with chest wall injury. Am J Surg. 2012;204:910–913. doi: 10.1016/j.amjsurg.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 18.Hildebrand F, van Griensven M, Garapati R, et al. Diagnostics and scoring in blunt chest trauma. Eur J Trauma. 2002;28:157–167. doi: 10.1007/s00068-002-1192-1. [DOI] [Google Scholar]
- 19.Moon SH, Kim JW, Byun JH, et al. The thorax trauma severity score and the trauma and injury severity score: do they predict in-hospital mortality in patients with severe thoracic trauma? A retrospective cohort study. Medicine (Baltimore). 2017;96:e8317. [DOI] [PMC free article] [PubMed]
- 20.Balkan ME, Oktar GL, Kayi-Cangir A, Ergül EG. Emergency thoracotomy for blunt thoracic trauma. Ann Thorac Cardiovasc Surg. 2002;8:78–82. [PubMed] [Google Scholar]



