Abstract
Objective
Extraintestinal manifestations in irritable bowel disease (IBD), Crohn's disease and ulcerative colitis are reported in different system of the body. We aimed to investigate the factors determining disease severity and evaluate extraintestinal manifestations in patients with irritable bowel disease based on disease activity scoring system.
Methods
This cross-sectional study was conducted on all patients with irritable bowel disease referred to clinic and gastroenterology ward of (XXX). Medical history, gastrointestinal complications and incidence of extraintestinal manifestations were recorded. Disease severity in ulcerative colitis was rated based on PUCAI (Pediatric Ulcerative Colitis Activity Index) score and in Crohn's disease was calculated based on PCDAI (Pediatric Crohn's Disease Activity Index) score.
Results
Of 73 children included in our study, 54.80% were diagnosed with ulcerative colitis and 45.20% were diagnosed with Crohn's disease. The most prevalent symptom was weight loss (81.81%), diarrhea (72.72%) and abdominal pain (69.69%) in Crohn's diseases and bloody diarrhea (80%), abdominal pain (77.5%) and weight loss (57.5%) in ulcerative colitis. The average of PCDAI score was 43.44 and PUCAI score was 35.62. The most prevalent extraintestinal manifestation of the disease was arthritis in 7 Crohn's disease patients (21.21%) and 5 patients (12.5%) with ulcerative colitis, oral plague in 5 patients (15.15%) with Crohn's disease and erythema nodosum in 2 patients (6.06%) with Crohn's disease.
Conclusion
The severity of oral plaque was positively associated with the severity of the disease. There was no significant association among other parameters. Scoring systems, to determine the extraintestinal manifestation, should be standardized based on the scoring outcomes.
Keywords: Inflammatory bowel, Pediatric, PCDAI, Gastrointestinal, Irritable bowel
Abbreviations: IBD, inflammatory bowel disease; HLA, human leukocyte antigen; PUCAI, Pediatric Ulcerative Colitis Activity Index; PCDAI, Pediatric Crohn's Disease Activity Index
Highlights
-
•
Crohn’s disease and ulcerative colitis are the most common types of inflammatory bowel disease.
-
•
The severity of oral plaque was positively associated with the severity of the disease.
-
•
The qualitative score of the disease was significantly associated with oral plague.
1. Introduction
Crohn's disease and ulcerative colitis are the most common types of inflammatory bowel disease (IBD) where 15–25% cases initiate in childhood. Some studies have indicated that the prevalence of IBD is greater in younger patients than adults [1]. It can be a chronic condition with serious systemic complications. Environmental factors, epigenetics, gut microbiota and genetic factors are known to play significant role in the etiology of the disease [2]. It is also known to have greater incidence in the regions where hygienic conditions are poor such as regular consumption of contaminated food and water and large family size. Perinatal and early life events such as gastroenteritis or undefined infections, passive smoking and vaccines can increase the risk of IBD in the children [3].
Crohn's disease and ulcerative colitis are considered as systemic diseases due to their extensive extraintestinal manifestations. These signs and symptoms can be presented even before the diagnosis of IBD. Some of the commonly known manifestations are seen as musculoskeletal (ankylosing spondylitis, arthritis, osteoporosis and osteoarthritis), integumentary (erythema nodosum, pyoderma gangrenosum and sweet syndrome), hepatobiliary (cirrhosis, hepatitis and cholelithiasis), hematological (anemia, thrombocytosis, leukocytosis), oral (aphthous stomatitis and angular stomatitis) and ophthalmological complications (uveitis, conjunctivitis and glaucoma) [1]. These complications are seen in 20–40% of the patients [4]. Immune activation during ulcerative colitis and Crohn's disease leads to the production of antibodies that are seen to cross-react with self-antigens such those reported in sclerosing cholangitis [5]. Furthermore, variation in human leukocyte antigen (HLA) genotypes also increases the risk of extraintestinal manifestation [6]. Malabsorption, protein-losing enteropathy, fistulas, and intestinal resection can lead to deficiencies of protein, bile salts, vitamins, and minerals, leading to adverse clinical consequences. Furthermore, medications used to treat IBD can be associated with many non-intestinal and intestinal side effects [7].
Extraintestinal manifestations of inflammatory bowel disease covers a wide range. Therefore, it is important to study the factors affecting the occurrence of these manifestations and its relationship with the severity of the disease and the use of drugs. The present study was performed to evaluate the prognostic factors and extraintestinal manifestations of inflammatory bowel disease in patients referred to the Pediatric Medical Center.
2. Methods
In this cross-sectional (descriptive-analytical) study, all the children, aged from 2 to 18 years with inflammatory bowel disease referred to the clinic and gastrointestinal ward of the (XXX) from the beginning of April 2019 to the end of September 2019 were enrolled.
The medical records all the patients who have been hospitalized during this period with the diagnosis of inflammatory bowel diseases and have been treated and followed up according to the severity of the disease were extracted. The history and results of clinical examinations for gastrointestinal complications, common extraintestinal complications and other complications of the disease (such as growth disorders, etc.), results of colonoscopy and pathology were extracted from the patients' files and recorded in patients’ forms.
Patients who were diagnosed with indeterminate colitis based PUCAI (Pediatric Ulcerative Colitis Activity Index) criteria and Crohn's disease based on PCDAI (Pediatric Crohn's Disease Activity Index) criteria were included in the study. To evaluate PCDAI score following was used:
-
1
History including abdominal pain, number of watery stools, number and frequency of blood in the stool and patient function.
-
2
Clinical examination including abdominal examination, perianal diseases, extraintestinal manifestations, height and weight, fever.
-
3
The results of laboratory tests including hematocrit, albumin and ESR (erythrocyte sedimentation rate).
The final PCDAI score was reported numerically between 0 and 100. Patients who scored 10–29 were considered mild, patients who scored 30 to 40 were considered moderately ill, and those who scored 40 or higher were considered to have severe disease.
For PUCAI evaluation, information regarding abdominal pain, rectal bleeding, stool consistency, frequency of bowel movements per day, history of need for nocturnal defecation and daily activity level were obtained and the final score was reported numerically between 0 and 85. For patients with ulcerative colitis, a score of 10–29 was considered mild, a score of 30–64 was considered moderate, and a score 65 and above was considered severe.
It should be noted that all the patients who entered the study underwent the same treatment protocol. In cases of inactive Crohn's disease and inactive-to-mild ulcerative colitis, treatment with 5-aminosalicylic acid (5-ASA) was started at a dose of 20 mg/kg/day, increasing to a maximum of 70 mg/kg/day depending on the patient's needs. In cases of mild Crohn's disease, oral prednisolone was added to the above treatment at a dose of 1 mg/kg/day. In moderate to severe cases, oral prednisolone 1 mg/kg/day plus azathioprine 2–2.5 mg/kg/day (or 6-mercaptopurine 1–2 mg/kg/day was prescribed.
The response to the treatment in these patients, recurrence of gastrointestinal symptoms, number of hospitalizations and the need for surgical intervention etc. was evaluated. The data were analyzed using SPSSv19 software. Qualitative data were presented as frequency and quantitative findings were analyzed using chi-square tests. Other findings were presented in the form of tables and graphs.
Unique identifying number is: researchregistry7312.
The methods are stated in accordance with STROCSS 2021 guidelines [8].
3. Results
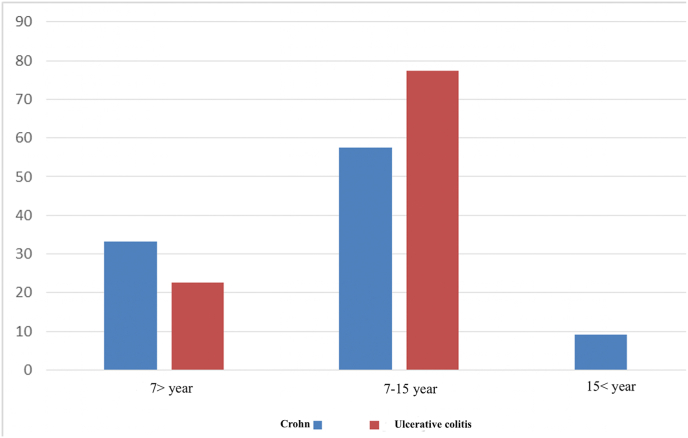
Our study included 73 children with inflammatory bowel disease (IBD) where 33 cases had Crohn's disease (45.20%) and 40 cases (54.80%) had ulcerative colitis. The mean age of patients with Crohn's disease was 9.06 ± 4.94 years and that of patients with ulcerative colitis was 9.10 ± 3.44 years. The overall mean age of patients was 9.08 ± 4.15 years (Fig. 1).
Fig. 1.
Age distribution of patients.
In Crohn's disease, 11 cases (33.3%) were aged under 7 years, 19 cases were aged 7–15 years (57.57%) and 3 cases (9.09%) were aged over 15 years old. In ulcerative colitis, 9 cases (22.5%) were under 7 years, 31 cases (77.5%) were 7–15 years and none of the cases (0%) were above 15 years.
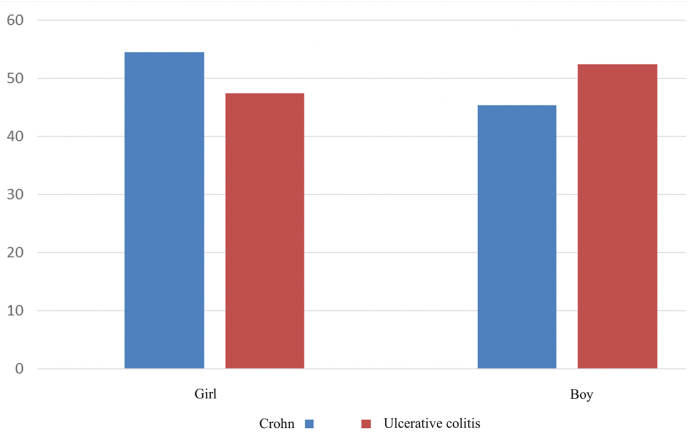
In total, 15 Crohn's patients were boys (45.45%) and 18 were girls (54.54%). Among patients with ulcerative colitis, 21 (52.5%) were boys and 19 (47.5%) were girls. A total of 36 cases were boys and 37 were girls (Fig. 2).
Fig. 2.
Gender distribution of patients in Crohn's disease and ulcerative colitis.
On average, it took 5.58 ± 5.53 months from the onset of symptoms to the diagnosis of the disease in patients with Crohn's disease and 8.17 ± 6.80 months in patients with ulcerative colitis. This period was not significantly different between the two groups (p = 0.571).
In Crohn's disease group, 25 cases (75.75%) had no family history of the disease and 8 cases (24.24%) had family history. In ulcerative colitis, 36 patients (90%) did not have the history and 4 patients (10%) had the history. A total of 61 cases did not have the family history of the disease while 12 patients had the history in the family.
Among Crohn's patients, 27 cases (81.81%) weighed below the 10th percentile whereas 6 cases (18.18%) were above the 10th percentile. In ulcerative colitis group, 13 cases (32.5%) were below the 10th percentile and 27 cases (67.5%) were above. A total of 40 cases were below the 10th percentile weight and 33 cases were above this range.
In Crohn's patients, 17 cases (51.51%) were below 10% of weight and 16 cases (48.48%) were above 10% of weight. In patients with ulcerative colitis, 5 cases (12.5%) were below 10% of weight and 35 cases (87.5%) were above 10%. A total of 22 cases were below the 10% weight percentile and 51 were above the 10% weight percentile.
In Crohn's disease group, 17 cases (51.51%) were below 10th percentile of height and 16 cases (48.48%) were above. Whereas, in ulcerative colitis group, 5 cases (12.5%) were below 10th percentile of height and 35 cases (87.5%) were above. A total of 22 cases were below the 10th percentile of height and 51 were above.
A total of 67 cases (91.78%) had the first manifestation of their disease as gastrointestinal symptoms and in 6 cases (8.21%) extraintestinal symptoms were primarily seen as the first manifestation of IBD.
3.1. Gastrointestinal side effects
Abdominal pain was present in 23 patients (69.69%) and absent in 10 patients (30.30%) in Crohn's disease group. Whereas, in ulcerative colitis, it was present in 31 patients (77.5%) and absent in 9 patients (22.5%).
In Crohn's disease group, anorexia was seen in 17 patients (51.51%) and in 12 patients (30%) with ulcerative colitis. Diarrhea was reported in 24 patients (72.72%) in Crohn's disease group and in 17 patients (42.5%) with ulcerative colitis. Bloody diarrhea was seen in 17 patients (51.51%) in Crohn's disease and in 32 patients (80%) with ulcerative colitis. 13 patients (39.39%) with Crohn's disease and 7 patients (17.5%) with ulcerative colitis were presented with vomiting.
Rectal bleeding was present in 8 patients (24.24%) with Crohn's disease and in 22 patients (55%) with ulcerative colitis. Perinatal disease was seen in 10 patients (30.30%) in Crohn's disease group and in 1 patient (2.5%) with ulcerative colitis.
3.2. Extraintestinal manifestation
7 Crohn's disease patients (21.21%) were presented with arthritis and 5 patients (12.5%) with ulcerative colitis had arthritis. Oral plague was present in 5 patients (15.15%) in Crohn's disease group and none of the patients with ulcerative colitis had oral plague. 2 patients (6.06%) with Crohn's disease had erythema nodosum whereas, erythema nodosum was not seen in patients with ulcerative colitis (0%). Only one case of uveitis was present (3.03%) in Crohn's disease group. Ankylosing spondylitis and pyoderma gangrenosum was only reported in 1 case (2.5%) of ulcerative colitis, respectively.
Fever was observed in 6 (18.18%) Crohn's disease patients and 1 case (2.5%) of ulcerative colitis. Liver involvement was not observed in any of Crohn's patients (0%). Whereas, 5 patients (12.5%) with ulcerative colitis had liver disease and 2 of these (5%) were presented with increase in liver enzymes. Bile duct involvement among Crohn's patients occurred in one patient (3.03%) and among patients with ulcerative colitis, it was seen in 3 (7.5%) patients. One patient (2.5%) with ulcerative colitis was presented with pancreatitis. Gallstones were not observed in any group however, one Crohn's disease patient (3.03%) had kidney stones and amyloidosis, respectively.
Thromboembolism was seen in one patient (3.03%) with Crohn's disease and in two patients (5%) with ulcerative colitis.
The mean score was 43.33 ± 11.56 in Crohn's disease patients and 35.62 ± 14.37 in patients with ulcerative colitis. Comparison of the two groups showed a significant difference (p = 0.015). Qualitative score was also measured in these two groups. In Crohn's disease, 4 cases were mild (12.12%), 7 cases (21.21%) were moderate and 22 cases (66.66%) were severe. Whereas, in patients with ulcerative colitis, 15 cases (37.5%) were mild, 24 cases (60%) were moderate and 1 case (2.5%) was severe.
3.3. Endoscopy and colonoscopy findings
Esophagitis was seen in 19 patients (57.57%) with Crohn's disease and 9 cases (22.5%) of esophagitis were seen in patients with ulcerative colitis. Gastritis was seen in 24 patients (72.72%) with Crohn's disease and in 15 patients (37.5%) with ulcerative colitis. Duodenitis was present in 9 patients (27.27%) with Crohn's disease and 3 patients (7.5%) with ulcerative colitis. Evidence of ulcer on endoscopy was seen in 5 patients (15.15%) with Crohn's disease and 5 patients (12.5%) with ulcerative colitis.
Evidence of erythema on colonoscopy among patients with Crohn's disease and ulcerative colitis was observed in 19 patients (57.57%) and 38 patients (95%), respectively. Mucosal fragility was observed in 11 patients (33.33%) with Crohn's disease and 36 patients (90%), respectively. Absence of vascular pattern in Crohn's disease and ulcerative colitis was seen in 9 patients (27.27%) and 31 patients (77.5%), respectively. Ulcer was seen in 27 patients (81.81%) with Crohn's disease and 34 patients (85%) with ulcerative colitis.
Among Crohn's disease patients, 24 patients (72.72%) had skip lesions in colonoscopy and left colitis and pancreatitis was present in 6 patients (15%) and 15 patients (37.5%) with ulcerative colitis, respectively.
3.4. Usage of drugs
Aminosalicylates were used in the mild stage of the disease in 10 patients (52.63%), in the moderate stage of the disease in 26 patients (83.87%) and in the severe disease in 16 patients (69.56%). Similarly, prednisolone was used by 13 patients (68.42%) with mild pathology, 20 patients (64.51%) with the moderate pathology and 19 patients (82.60%) in the severe disease. Azathioprine was used by 6 patients (31.57%) in the mild group, 8 patients (25.80%) in the moderate group and 4 patients (17.39%) in the severe group and mercaptopurine was used by 4 patients (21.05%) in the mild group, 7 patients (22.58%) in the moderate group and 6 patients (26.08%) in the severe group. Enema was performed for 2 patients (10.52%) in the mild category of the disease and 4 patients (12.90%) with moderate pathology.
Cyclosporine, infliximab, adalimumab were prescribed in the mild category of the disease in one case (5.26%), for 4 patient (12.90%) with moderate disease and 3 patients (13.04%) in severe disease (see Table 1).
Table 1.
Relationship between qualitative disease score and study variables.
| Variables | p-value | Variables | p-value |
|---|---|---|---|
| Fever | 0.305 | age categories | 0.738 |
| Liver involvement | 0.130 | History of surgery | 0.393 |
| Bile duct involvement | 0.630 | Number of hospitalizations per year | 0.506 |
| Pancreatitis | 0.237 | History of blood transfusion | 0.548 |
| kidney stone | 0.332 | The process of drugs | 0.321 |
| Amyloidosis | 0.332 | Number of disease control drugs | 0.277 |
| thromboembolism | 0.536 | Arthritis | 0.684 |
| Increase in asymptomatic liver enzymes | 0.569 | Canker Sores | 0.042 |
| Hb | 0.453 | Erythema nodosum | 0.107 |
| CRP | 0.290 | Uveitis | 0.322 |
| ESR | 0.300 | Ankylosing spondylitis | 0.503 |
| Albumin | 0.159 | Pyoderma gangrene | 0.503 |
| Calprotectin | 0.495 |
(p-value less than 0.05 is considered statistically significant).
ACSA (anti saccharomyces cerevisiae antibody) was positive in 24.24% of Crohn's patients and 2.5% of patients with ulcerative colitis. ANCA (Antineutrophilic cytoplasmic antibody) was positive in 3.03% of Crohn's patients and 17.5% of patients with ulcerative colitis (Table 2).
Table 2.
Relationship between ASCA and study variables.
| Variable | p-value | Variables | p-value |
|---|---|---|---|
| age | 0.265 | Gastritis | 0.030 |
| Fever | 0.166 | Uveitis | 0.126 |
| Liver involvement | 0.407 | Ulcer evidence in endoscopy | 0.991 |
| Bile duct involvement | 0.407 | Evidence of erythema on colonoscopy | 0.874 |
| Pancreatitis | 0.687 | History of blood transfusion | 0.678 |
| kidney stone | 0.687 | Evidence of fragility in colonoscopy | 0.223 |
| Amyloidosis | 0.687 | Lack of vascular pattern on colonoscopy | 0.126 |
| thromboembolism | 0.477 | Evidence of skip area in colonoscopy | 0.060 |
| Number of hospitalizations per year | 0.289 | splenic flexure | 0.349 |
| Esophagitis | 0.076 | pancolitis | 0.395 |
(p-value less than 0.05 is considered statistically significant).
The mean quantitative PCDAI score was 43.44 and the mean quantitative mean score of pediatric ulcerative colitis was 35.62. In terms of qualitative score in Crohn's disease, 12.12% were in the mild category, 21.21% in the moderate category and 66.66% in the severe category at the time of diagnosis. In ulcerative colitis, 37.5% were in the mild category, 60% in the moderate category and 2.5% in the severe category.
4. Discussion
In our study, 73 children were studied, of which 54.80% had ulcerative colitis (UC) and 45.20% had Crohn's disease. The mean age of the patients among the two groups was not statistically significant.
The mean time between onset of symptoms and diagnosis in our study was 5.58 months in Crohn's patients and 6.80 months in patients with ulcerative colitis. In our study, there was no significant difference between the two groups of diseases in this regard. In the study by Castro et al. [9], the mean interval between the onset of symptoms and the diagnosis of Crohn's disease was 10.1 months and 5.8 months in ulcerative colitis. In the study of Vahedi et al. [10], the time from the onset of symptoms to the diagnosis of the disease was higher than our study, which was 24.4 months in Crohn's disease and was 22 months in ulcerative colitis.
In our study, 91.78% of patients had first manifestation in the form gastrointestinal symptoms and only 6 cases (8.21%) had primary symptoms as extraintestinal presentation (4 cases of arthritis and 2 cases of arthritis with erythema nodosum). A study by Jose et al., reported a similar figure, with extraintestinal manifestations occurring in 6% of people before diagnosis [11]. In Crohn's patients, Sawczenko's study reported that only 25% of patients were presented with the classic triad; diarrhea, weight loss, and abdominal pain, and 50% of patients did not report diarrhea.
In our study, the most common intestinal symptom in Crohn's disease was weight loss, and in ulcerative colitis was dysentery. In the study by Vahedi et al. [10], the most common complaint in Crohn's disease was abdominal pain and in ulcerative colitis was rectal bleeding. The most common intestinal problems in Crohn's disease were fistula, abscess, obstruction and extensive bleeding (with 13.5%, 8.2%, 7.5% and 3.8% prevalence, respectively) and in ulcerative colitis was massive hemorrhage (7.1%). In a study by Stawarski et al. [12], massive intestinal hemorrhage was seen in 11 children with ulcerative colitis and perianal changes were seen in 5 children with Crohn's disease (significantly more than ulcerative colitis). External intestinal fistula, abdominal abscess, intestinal rupture, and ileus were also characteristic complications of Crohn's disease compared with ulcerative colitis.
The most common extraintestinal complication in our study of Crohn's disease and ulcerative colitis was arthritis. There was a statistically significant difference between Crohn's disease and ulcerative colitis among extraintestinal complications in terms of oral plague, fever and liver involvement (p < 0.05). A study by Greuter et al. [13] reported that extraintestinal manifestations are more in Crohn's disease as compared to ulcerative colitis where peripheral arthritis (7.9%) and aphthous stomatitis (7.3%) were the most common manifestations. In the study by Dotson et al. [14], a statistically significant difference in the rate of extraintestinal manifestations between Crohn's disease and ulcerative colitis was reported for aphthous stomatitis, erythema nodosum and sclerosing cholangitis. The study also found that extraintestinal manifestations occurred in approximately 25% of young patients and that 38.2% of patients would have an extraintestinal manifestation or more. In the study of Fallahi et al. [15], the most common extraintestinal manifestations are hepatobiliary disorders and arthritis. Arthritis (26%) and aphthous stomatitis (21%) were the most common manifestations of the disease, in the study by Jose et al. Furthermore, Malaty et al. [16], reported that extraintestinal manifestations occurred in 20% of patients with 48% arthritis, 35% sclerosing cholangitis, and 17% aphthous stomatitis. According to a study by Stawarski et al. [12], 50% of children with ulcerative colitis and 80% of children with Crohn's disease experience at least one case of extraintestinal manifestation and a statistically significant difference was reported between the two groups.
The mean quantitative PCDAI score was 43.44 and the mean quantitative score of pediatric ulcerative colitis was 35.62. In terms of qualitative score in Crohn's disease, 12.12% were in the mild category, 21.21% in the moderate category and 66.66% in the severe category at the time of diagnosis. In ulcerative colitis, 37.5% were in the mild category, 60% in the moderate category and 2.5% in the severe category. A study by Motamed et al. [17], showed that the mean values of PCDAI and PUCAI were 60.62 and 50.95 for patients with Crohn's disease and ulcerative colitis, which showed significant reduction after treatment. In the study by Hyams et al. [18], the mean PCDAI for the mild, moderate, and severe categories of the disease was 19.5, 32.2, and 47.8, respectively. In this study, it was seen that PCDAI of higher than or equal to 30 has acceptable sensitivity and specificity for moderate/severe cases. A decrease in PCDAI of 12.5 or more following therapeutic interventions is a good indication of a clinically significant response.
5. Conclusion
According to the results, it can be said that the qualitative score of the disease was significantly associated with oral plague such that severe disease is associated with severe plaque. In other cases, there was no significant relationship. Therefore, it seems that changes should be made in the “disease activity scoring” system to better communicate the symptoms, severity and complications of the disease.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Sources of funding
No funding was secured for this study.
Author statement
Dr. Parisa Rahmani: conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript.
Dr. Mojtaba Gorgi and Dr. Farzaneh Motamed: Designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript.
Dr. Ghazaleh Rasti and Dr. Parastoo Sharifi: Coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content.
Registration of research studies
1. Name of the registry: N/a.
2. Unique Identifying number or registration ID:
3. Hyperlink to the registration (must be publicly accessible):
Guarantor
Parisa Rahmani.
Consent
Not applicable.
Ethics
The study was approved by the committee of ethics of Tehran's Children's Medical Center.
Availability of data and material
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors deny any conflict of interest in any terms or by any means during the study. All the fees provided by research center fund and deployed accordingly.
References
- 1.Jang H.-J., Kang B., Choe B.-H. The difference in extraintestinal manifestations of inflammatory bowel disease for children and adults. Transl. Pediatr. 2019;8(1):4–15. doi: 10.21037/tp.2019.01.06. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Béres N.J., Kiss Z., Sztupinszki Z., et al. Altered mucosal expression of microRNAs in pediatric patients with inflammatory bowel disease. Dig. Liver Dis. 2017;49(4):378–387. doi: 10.1016/j.dld.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Strisciuglio C., Giugliano F., Martinelli M., et al. Impact of environmental and familial factors in a cohort of pediatric patients with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2017;64(4) doi: 10.1097/MPG.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 4.Agrawal D., Rukkannagari S., Kethu S. Pathogenesis and clinical approach to extraintestinal manifestations of inflammatory bowel disease. Minerva Gastroenterol. Dietol. 2007;53(3):233–248. [PubMed] [Google Scholar]
- 5.Danese S., Semeraro S., Papa A., et al. Extraintestinal manifestations in inflammatory bowel disease. World J. Gastroenterol. 2005;11(46):7227. doi: 10.3748/wjg.v11.i46.7227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vavricka S.R., Schoepfer A., Scharl M., Lakatos P.L., Navarini A., Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm. Bowel Dis. 2015;21(8):1982–1992. doi: 10.1097/mib.0000000000000392. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jose F.A., Heyman M.B. Extraintestinal manifestations of inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2008;46(2):124–133. doi: 10.1097/MPG.0b013e318093f4b0. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathew G., Agha R., Albrecht J., et al. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Ann. Med. Surg. 2021;72 doi: 10.1016/j.amsu.2021.103026. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castro M., Papadatou B., Baldassare M., et al. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996–2003) Inflamm. Bowel Dis. 2008;14(9):1246–1252. doi: 10.1002/ibd.20470. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 10.Vahedi H., Merat S., Momtahen S., et al. 2009. Epidemiologic Characteristics of 500 Patients with Inflammatory Bowel Disease in Iran Studied from 2004 through 2007. [PubMed] [Google Scholar]
- 11.Jose F.A., Heyman M.B. Extraintestinal manifestations of inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2008;46(2):124. doi: 10.1097/MPG.0b013e318093f4b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stawarski A., Iwańczak B., Krzesiek E., Iwańczak F. Intestinal complications and extraintestinal manifestations in children with inflammatory bowel disease. Pol. Merkur. Lek.: organ Polskiego Towarzystwa Lekarskiego. 2006;20(115):22. [PubMed] [Google Scholar]
- 13.Greuter T., Bertoldo F., Rechner R., et al. Extraintestinal manifestations of pediatric inflammatory bowel disease: prevalence, presentation, and anti-TNF treatment. J. Pediatr. Gastroenterol. Nutr. 2017;65(2):200–206. doi: 10.1097/MPG.0000000000001455. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 14.Dotson J.L., Hyams J.S., Markowitz J., et al. Extraintestinal manifestations of pediatric inflammatory bowel disease and their relation to disease type and severity. J. Pediatr. Gastroenterol. Nutr. 2010;51(2):140–145. doi: 10.1097/MPG.0b013e3181ca4db4. [DOI] [PubMed] [Google Scholar]
- 15.Fallahi G.-H., Moazzami K., Tabatabaeiyan M., et al. Clinical characteristics of Iranian pediatric patients with inflammatory bowel. Acta Gastro-Enterol. Belg. 2009:72. [PubMed] [Google Scholar]
- 16.Malaty H.M., Abraham B.P., Mehta S., Garnett E.A., Ferry G.D. The natural history of ulcerative colitis in a pediatric population: a follow-up population-based cohort study. Clin. Exp. Gastroenterol. 2013;6:77. doi: 10.2147/CEG.S40259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Motamed F., Famouri F., Najafi M., et al. Response to induction therapy in a pediatric population of inflammatory bowel disease. Z. Gastroenterol. 2010;48:748–752. doi: 10.1055/s-0028-1109969. 07. [DOI] [PubMed] [Google Scholar]
- 18.Hyams J., Markowitz J., Otley A., et al. Evaluation of the pediatric crohn disease activity index: a prospective multicenter experience. J. Pediatr. Gastroenterol. Nutr. 2005;41(4):416–421. doi: 10.1097/01.mpg.0000183350.46795.42. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.