Abstract
Background
The objective of this study was to compare the radiologic and clinical outcomes of HURWA robotic-assisted total knee arthroplasty (TKA) to those of conventional TKA.
Methods
A total of 150 patients were randomized into two groups – 73 and 77 patients underwent robotic-assisted TKA and conventional TKA, respectively. Preoperative and postoperative Western Ontario McMaster University Osteoarthritis Index (WOMAC) score, Hospital for Special Surgery (HSS) score, 36-item Short Form Health Survey (SF-36) score, Knee Society Score (KSS) and range of motion (ROM) were obtained and compared between these two groups. The preoperative and postoperative hip-knee-ankle (HKA) angle and the rate of HKA≤3° in the two groups were also compared.
Results
The postoperative mean HKA angle was 1.801° ± 1.608° of varus for the robotic-assisted TKA group and 3.017° ± 2.735° of varus for the conventional TKA group; these values were significantly different. The alignment rate for mechanical axis lower than 3° in the robotic-assisted TKA group and the conventional TKA group were 81.2% and 63.5%, respectively. Patients undergone robotic-assisted TKA or conventional TKA had similarly improved knee flexion and functional recovery reflected by WOMAC score, HSS score, SF-36 score and KSS.
Conclusion
HURWA robotic-assisted TKA is a safe and effective, resulting in better alignment for mechanical axis than conventional TKA. The improvement in knee flexion and functional recovery after HURWA robotic-assisted TKA were similar to those after conventional TKA. However, longer follow-up is needed to determine whether the improved alignment of mechanical axis will produce better long-term clinical outcomes.
The translational potential of this article
Recently, the robotic-assisted TKA system has been introduced to clinical practice for TKA. Several robotic-assisted TKA systems, including CASPAR, Tsolution, ROSA, ROBODOC and Mako, have been implemented into clinical application.However, the clinical application of these robotic systems was limited due to their technical complexity, insufficient versatility and increased operative time. Until now, there are still no robotic-assisted TKA systems approved by the National Medical Products Administration of China. Therefore, more robotic-assisted TKA systems need to be designed and improved, particularly in China. Through our randomized, multicenter, single blind and parallel controlled trial, we showed that HURWA robot-assisted TKA system is a safe and effective system for TKA, which had improved knee flexion.
Keywords: Total knee arthroplasty, TKA, Osteoarthritis
Abbreviations: TKA, total knee arthroplasty; KOA, Knee osteoarthritis
1. Introduction
Knee osteoarthritis (KOA) is characterized by degradation of articular cartilage [[1], [2], [3], [4]]. KOA is the most frequent type of arthritis, causing progressive pain and physical debilitation [[5], [6], [7]]. A previous study demonstrated that about half of individuals older than 65 years suffered from KOA [8]. The prevalence of KOA is expected to be on the rise due to the expanding aging population [3]. Total knee arthroplasty (TKA) is the best method for the treatment of late-stage KOA [[9], [10], [11], [12]]. In China, over 370,000 TKAs were performed each year with an annual growth rate of 15% [13]. Soft tissue balancing and mechanical alignment play important roles in implant survival rate, patient functionality, and TKA success [[14], [15], [16]]. Previous studies showed that the proportion of hip-knee-ankle (HKA) angle outliers greater than ± 3° in the conventional TKA was 10–20% [17]. This may cause knee prosthesis failure and abnormal load and is strongly associated with limited range of motion and reduced satisfaction [18].
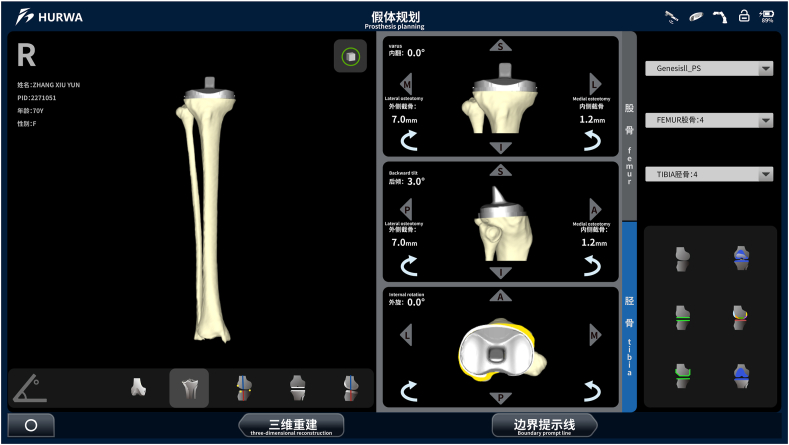
Despite the emergence of patient-specific instrumentation, standard cutting guides, navigation, and accelerometer-based navigation, these new operation approaches are costly [[19], [20], [21]]. Recently, the robotic-assisted TKA system has been introduced to clinical practice for TKA [22]. The robot-assisted system is a new technology which uses computed tomography (CT) data of patients’ lower limb to make a preoperative plan and three -dimensional planning to orientate and size and uses the robotic arm to cut the bone and place for components [23,24]. Several robotic-assisted TKA systems, including CASPAR, Tsolution, ROSA, ROBODOC and Mako, have been implemented into clinical application [[25], [26], [27], [28]]. Previous studies showed that robotic-assisted TKA can offer more accurate bone cuts, precise placement of implants and provide balanced extension and flexion gaps [29,30]. Moreover, robotic-assisted TKA can reduce the extent of bone resection and damage to the soft tissue, which are associated with postoperative pain [31]. However, the clinical application of these robotic systems was limited due to their technical complexity, insufficient versatility and increased operative time [31]. Until now, there are still no robotic-assisted TKA systems approved by the National Medical Products Administration of China. Therefore, more robotic-assisted TKA systems need to be designed and improved, particularly in China. Available types of robotic-assisted TKA include (1) robotic arm designed to provide a haptic interface; (2) handheld robotic burr manually controlled by the surgeon; (3) CT based autonomous system for implant fit and positioning; and (4) motor-powered robotic system that performs precise tibial and femoral cuts. Each type has distinct requirements for manual input from the surgeon and preoperative CT scan and has different compatibility with knee prosthesis. Recently, a new robotic-assisted TKA system (HURWA, BEIJING HURWA-ROBOT Technology Co. Ltd) has been designed (Fig. 1). Our system also uses the CT data of lower limb to perform the preoperative plan and three -dimensional planning to orientate and size and actively uses the robotic arm to cut the bone and place for components. We previously investigated the accuracy and safety of this system in a sheep model and found that it might be an accurate and safe tool for TKA [32]. Moreover, we found that the accuracy of all of the bone resection levels was below 0.6 mm and all of the bone resection angles were below 0.6° in the HURWA robotic-assisted TKA group [33].
Figure 1.
The robot console and the surgical platform of HURWA robot-assisted TKA system.
In the present study, we performed a randomized, multicenter, single-blind, two-arm, parallel-group controlled trial of HURWA robotic-assisted TKA versus conventional TKA to study the effectiveness and safety of this system in humans.
2. Materials and methods
2.1. Study design
Our study was a randomized, multicenter, single blind and parallel controlled trial that was approved by the Institutional Review Board of Peking Union Medical College Hospital (IRB # KS2020328), Affiliated Beijing Chaoyang Hospital of Capital Medical University l (IRB # 2020-10-28-2) and Tianjin Hospital (IRB # 2020-QX-004). All patients had provided written informed consent.
2.2. Patient recruitment
From January 2020 to March 2021, a total of 150 patients were randomized into two groups – 73 patients underwent robotic-assisted TKA and 77 underwent conventional TKA. Patients with primary KOA who underwent TKA using the Legion system (Smith & Nephew, London, UK) were included. The inclusion criteria were as follows: older than 18 years old with primary and unilateral TKA. The exclusion criteria were as follows: Patients with post-traumatic osteoarthritis, infection, severe systemic disease (severe diabetes, severe heart disease, severe liver and/or kidney insufficiency, active tuberculosis infection, hemorrhagic disease), neuromuscular dysfunction of lower limbs (e.g. sequelae of poliomyelitis, myasthenia) and participated in clinical studies of other drugs, biological agents or devices in the last 3 months. All operations were performed by experienced surgeons for the conventional and robotic-assisted groups at three hospitals. All patients who underwent TKA with the robotic-assisted or conventional operations underwent the clinical and radiologic assessment.
2.3. Surgical procedures
Conventional TKA was performed using the Legion system (Smith & Nephew, London, UK) according to the manufacturer's instructions. In brief, 10 mm of tibial bone was resected with the 7° posterior tibial slope. Femoral rotation was followed to three axes: (1) the transepicondylar axis, (2) Whiteside line and (3) 3° of external rotation relative to the posterior aspect of the femoral condyles. Tibial component rotation was aligned with the medial one third of the tibial tubercle.
Robot-assisted TKA was also performed using the Legion system together with the HURWA robotic-assisted TKA system (HURWA, BEIJING HURWA-ROBOT Technology Co. Ltd). Preoperative CT scan of lower limbs was taken for preoperative surgical planning. CT scan of lower limbs files included images of 3 regions (hip, knee, and ankle). These DICOM files were imported into the HURWA software system and segmented to build 3-D bone models. Preoperative surgical planning included varus/valgus angles, flexion/extension angles, internal/external rotation angles, axes and implant alignment planning (Fig. 2 and Fig. 3). After intraoperative registration, bone resection was performed by surgeons with the robotic arm (Fig. 4).
Figure 2.
Preoperatively planned position and posture of a femoral component by the HURWA robot-assisted TKA system.
Figure 3.
Preoperatively planned position and posture of a tibial component by the HURWA robot-assisted TKA system.
Figure 4.
The osteotomy procedure of HURWA robot-assisted TKA system. The surgeon can perform the osteotomy with a cutting saw once the cutting jig that move to the planned position.
2.4. Clinical outcome evaluation
Clinical information, including age, sex, height, body weight and other general information was collected preoperatively. Other clinical information were collected and entered into the database preoperatively and postoperatively by an independent investigator. The primary evaluation index was the rate of malalignment for mechanical axis greater than 3°. The safety objective of this study was based on the rate of intra-operative and postoperative TKA complications. The secondary evaluation indexes included: HSS score, KSS, WOMAC score and operation time. Preoperative clinical scores were collected on the day before surgery and postoperative clinical scores were measured at minimally 3 months after surgery by an independent investigator.
2.5. Radiologic outcome evaluation
Preoperative (within 7 days before the surgery) and postoperative (3 months after the surgery) radiologic data were obtained by two independent investigators. The anteroposterior radiograph of the entire lower extremity during weight bearing and the anteroposterior and lateral radiographs of the knee were performed. Mechanical alignment was determined by measuring the mechanical femorotibial angle (mFTA). The rate of malalignment for mechanical axis greater than 3° was recorded.
2.6. Statistical analysis
Statistical analysis was determined by SPSS (version 25, Inc, Chicago, IL) and P < 0.05 was considered to be statistically significant. Non inferiority one-sided Z-test and confidence interval were used to evaluate the main effectiveness evaluation indexes. Chi-square and Fisher's exact test were performed to assess safety evaluation indexes and secondary evaluation index.
3. Results
The mean follow-up period of all patients was 3 months. There was no significant difference in sex, age, height or weight between the control group and the robot-assisted TKA group (Table 1). All patients were diagnosed as severe osteoarthritis at the stage of middle and late stages. Table 2 summarized the preoperative radiological and clinical data in the two groups. There were no significant differences between these two groups about knee flexion, HSS score, KSS score, WOMAC score and SF-36 score. The preoperative mean hip-knee-ankle (HKA) angle was 8.65° ± 0.49° of varus for the robot-assisted TKA group and 7.96° ± 0.65° of varus for the conventional TKA group (Table 3); these values were not significantly different.
Table 1.
Demographic data.
| Index statistics | Sum(N = 150) | Study group(N = 73) | Control group(N = 77) | Statisticvalue | P value | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | −0.84 | 0.4009 | ||||||
| Number of cases (missing) | 150 | (0) | 73 | (0) | 77 | (0) | ||
| Average value(Standard Deviation) | 68.5 | (7.02) | 68.0 | (7.97) | 69.0 | (6.00) | ||
| Median (Q1, Q3) | 69.0 | (64.0, 73.0) | 68.0 | (63.0, 73.0) | 70.0 | (65.0, 72.0) | ||
| Min, Max | 30.0, | 86.0 | 30.0, | 86.0 | 54.0, | 83.0 | ||
| Age group, n(%) | 0.14 | 0.7040 | ||||||
| <65 years old | 39 | (26.0) | 20 | (27.4) | 19 | (24.7) | ||
| ≥65 years old | 111 | (74.0) | 53 | (72.6) | 58 | (75.3) | ||
| Gender, n(%) | 0.07 | 0.7928 | ||||||
| Male | 28 | (18.7) | 13 | (17.8) | 15 | (19.5) | ||
| Female | 122 | (81.3) | 60 | (82.2) | 62 | (80.5) | ||
| Weight (kg) | −2.05 | 0.0424 | ||||||
| Number of cases (missing) | 150 | (0) | 73 | (0) | 77 | (0) | ||
| Average value(Standard Deviation) | 70.7 | (10.49) | 69.0 | (9.87) | 72.4 | (10.84) | ||
| Median (Q1, Q3) | 70.0 | (65.0, 76.0) | 69.0 | (63.0, 75.0) | 71.0 | (67.0, 78.0) | ||
| Min, Max | 43.5, | 100.0 | 48.0, | 95.0 | 43.5, | 100.0 | ||
| Weight group, n(%) | 4.52 | 0.1044 | ||||||
| <65 kg | 34 | (22.7) | 21 | (28.8) | 13 | (16.9) | ||
| ≥65 kg and <90 kg | 105 | (70.0) | 49 | (67.1) | 56 | (72.7) | ||
| ≥90 kg | 11 | (7.3) | 3 | (4.1) | 8 | (10.4) | ||
| Height (cm) | −2.11 | 0.0363 | ||||||
| Number of cases (missing) | 150 | (0) | 73 | (0) | 77 | (0) | ||
| Average value(standard deviation) | 161.2 | (7.51) | 159.9 | (7.20) | 162.5 | (7.63) | ||
| Median (Q1, Q3) | 160.0 | (156.0, 165.0) | 160.0 | (155.0, 164.0) | 160.0 | (157.0, 165.0) | ||
| Min, Max | 145.0, | 185.0 | 145.0, | 178.0 | 150.0, | 185.0 | ||
| BMI(kg/m2) | −0.86 | 0.3891 | ||||||
| Number of cases (Missing) | 150 | (0) | 73 | (0) | 77 | (0) | ||
| Average value(standard deviation) | 27.2 | (3.32) | 26.9 | (3.26) | 27.4 | (3.38) | ||
| Median (Q1, Q3) | 27.3 | (25.2, 29.1) | 26.8 | (24.6, 28.8) | 27.3 | (25.5, 29.2) | ||
| Min, Max | 16.2, | 38.5 | 20.0, | 38.5 | 16.2, | 35.0 | ||
| BMI group, n(%) | 0.31 | 0.5749 | ||||||
| <28 kg/m2 | 89 | (59.3) | 45 | (61.6) | 44 | (57.1) | ||
| ≥28 kg/m2 | 61 | (40.7) | 28 | (38.4) | 33 | (42.9) | ||
Table 2.
Statistical description of present medical history, knee function and life-quality scores.
| Index Statistics |
Sum(N = 150) | Study group(N = 73) | Control group(N = 77) | statistic value | P value |
|---|---|---|---|---|---|
| Present medical history SOC classification, n(%) | — | — | |||
| Various musculoskeletal and connective tissue diseases | 150 (100.0%) | 73 (100.0%) | 77 (100.0%) | ||
| Present medical history staging | 0.13 | 0.7149 | |||
| Initial stage, n(%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Early stage, n(%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Middle stage, n(%) | 25 (16.7%) | 13 (17.8%) | 12 (15.6%) | ||
| End stage, n(%) | 125 (83.3%) | 60 (82.2%) | 65 (84.4%) | ||
| Affected knee | 2.08 | 0.1489 | |||
| Left lower extremity, n(%) | 83 (55.3%) | 36 (49.3%) | 47 (61.0%) | ||
| Right lower extremity, n(%) | 67 (44.7%) | 37 (50.7%) | 30 (39.0%) | ||
| ROM of affected knee(°) | −0.07 | 0.9437 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 99.9(20.10) | 99.8(20.95) | 100.0(19.40) | ||
| Median number (Q1, Q3) | 100.0 (90.0, 115.0) | 100.0 (90.0, 115.0) | 95.0 (90.0, 110.0) | ||
| Min, Max | 45.0, 140.0 | 45.0, 140.0 | 50.0, 140.0 | ||
| HSS Overall Score | 1.52 | 0.1298 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 63.7(12.81) | 65.3(11.34) | 62.2(13.96) | ||
| Median number (Q1, Q3) | 64.5 (55.0, 73.0) | 66.0 (58.0, 73.0) | 63.0 (55.0, 71.0) | ||
| Min, Max | 31.0, 94.0 | 40.0, 89.0 | 31.0, 94.0 | ||
| HSS overall score group, n(%) | NA | 0.4986 | |||
| ≥85 points | 5 (3.3%) | 2 (2.7%) | 3 (3.9%) | ||
| 70–84 points | 53 (35.3%) | 29 (39.7%) | 24 (31.2%) | ||
| 60–69 points | 45 (30.0%) | 23 (31.5%) | 22 (28.6%) | ||
| <60 points | 47 (31.3%) | 19 (26.0%) | 28 (36.4%) | ||
| KSS Objective score | 1.71 | 0.0899 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 36.8(19.66) | 39.6(18.27) | 34.2(20.66) | ||
| Median number (Q1, Q3) | 34.0 (26.0, 43.0) | 35.0 (29.0, 57.0) | 33.0 (22.0, 39.0) | ||
| Min, Max | −12, 76 | −3, 76 | −12, 76 | ||
| KSS symptom score | −0.39 | 0.6984 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 15.8(3.71) | 15.7(3.53) | 15.9(3.89) | ||
| Median number (Q1, Q3) | 16.5 (13.0, 19.0) | 16.0 (13.0, 18.0) | 17.0 (13.0, 19.0) | ||
| Min, Max | 2, 23 | 6, 23 | 2, 23 | ||
| KSS patients' satisfactory value | −0.38 | 0.7072 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 17.1(6.00) | 16.9(5.60) | 17.2(6.39) | ||
| Median number (Q1, Q3) | 18.0 (14.0, 20.0) | 18.0 (14.0, 20.0) | 18.0 (14.0, 22.0) | ||
| Min, Max | 0, 34 | 0, 30 | 4, 34 | ||
| KSS Score of surgical expectations | 0.08 | 0.9333 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 14.4(1.50) | 14.4(1.54) | 14.4(1.47) | ||
| Median number (Q1, Q3) | 15.0 (15.0, 15.0) | 15.0 (15.0, 15.0) | 15.0 (15.0, 15.0) | ||
| Min, Max | 6, 15 | 6, 15 | 8, 15 | ||
| KSS functional score | 1.65 | 0.1002 | |||
| Number of cases (missing) | 148 (2) | 71 (2) | 77 (0) | ||
| Average value(standard deviation) | 34.8(17.70) | 37.3(16.68) | 32.5(18.40) | ||
| Median number (Q1, Q3) | 35.0 (22.5, 46.0) | 38.0 (27.0, 48.0) | 31.0 (21.0, 44.0) | ||
| Min, Max | −10.0, 84.0 | −10.0, 76.0 | −10.0, 84.0 | ||
| WOMAC Score | −0.04 | 0.9715 | |||
| Number of cases (missing) | 150 (0) | 73 (0) | 77 (0) | ||
| Average value(standard deviation) | 119.0(40.63) | 118.9(40.44) | 119.2(41.07) | ||
| Median number (Q1, Q3) | 117.5 (90.0, 144.0) | 112.0 (88.0, 145.0) | 122.0 (92.0, 141.0) | ||
| Min, Max | 9.0, 238.0 | 28.0, 238.0 | 9.0, 235.0 | ||
| SF-36 health scale score | 1.01 | 0.3142 | |||
| Number of cases (missing) | 149 (1) | 72 (1) | 77 (0) | ||
| Average value(standard deviation) | 49.29(16.568) | 50.71(17.129) | 47.96(16.025) | ||
| Median number (Q1, Q3) | 47.40 (37.70, 61.00) | 47.45 (37.85, 64.20) | 46.60 (37.30, 57.60) | ||
| Min, Max | 18.8, 89.5 | 18.8, 89.5 | 19.7, 87.4 |
Table 3.
Statistical description of preoperative lower limb alignment between the two groups.
| Index Statistics |
Study group (N = 69) | Control group (N = 74) | ||
|---|---|---|---|---|
| Absolute value of lower limb alignment(°) | ||||
| Number of cases(Missing) | 69 | (0) | 74 | (0) |
| Average Value(Standard Deivation) | 8.65 | (0.49) | 7.96 | (0.65) |
| P Value | 0.3917 | |||
The postoperative mean hip-knee-ankle (HKA) angle was 1.801° ± 1.608° (range, 0.15° to 7.75°) of varus for the robot-assisted TKA group and 3.017° ± 2.735° (range, 0.20° to 15.15°) of varus for the conventional TKA group (Table 4); these values were significantly different. The primary effectiveness endpoint is alignment of coronal mechanical axis at 3 months defined as achieving varus-valgus alignment less than ±3° in the frontal plane after TKA. The robot-assisted TKA group showed a 81.2% malalignment for mechanical axis lower than 3° and the conventional TKA group showed a 63.5% malalignment for mechanical axis lower than 3°.
Table 4.
Statistical description of lower limb alignment correction between the two groups.
| Index Statistics |
Study group (N = 69) | Control group (N = 74) | ||
|---|---|---|---|---|
| Absolute value of lower limb alignment(°) | ||||
| Number of cases(Missing) | 69 | (0) | 74 | (0) |
| Average Value(Standard Deivation) | 1.801 | (1.6080) | 3.017 | (2.7352) |
| Median Number(Q1,Q3) | 1.250 | (0.60, 2.55) | 2.450 | (1.10, 4.00) |
| Min,Max | 0.15, | 7.75 | 0.20, | 15.15 |
| Whether lower limb alignment is corrected successfully [1] | ||||
| Yes, n(%) | 56 | (81.2) | 47 | (63.5) |
| No, n(%) | 13 | (18.8) | 27 | (36.5) |
| Correction rate(%) and 95%CI [2] | 81.2 | (69.9, 89.6) | 63.5 | (51.5, 74.4) |
| Lower limb alignment correction assesement Rate(%) and 95%CI [3] | 17.5 | (3.2, 31.9) | ||
| P Value [3] | 0.0207 | |||
In the robot-assisted TKA group, the range of knee flexion was from 60° to 135° and the average range was 114.5 ± 18.41° at 12 weeks after operation. Compared with the baseline data, the range of motion at 12 weeks after operation was significantly increased by 14.4 ± 22.24° in the robot-assisted TKA group (95% CI: 9.0, 19.7). In the conventional TKA group, the range of knee flexion was ranged from 75° to 140° with an average of 111.6° ± 18.75° at 12 weeks postoperatively. Compared with the baseline data, the range of range of motion at 12 weeks postoperatively significantly increased by 11.1° ± 20.33°(95% CI: 6.4, 15.8). There was no significant difference in activity improvement between these two groups (P = 0.2877) (Table 5).
Table 5.
Statistical description of ROM of subjects in follow-up when compared to baseline.
| Follow up statistics | Study group (N = 69) | Control group (N = 74) |
|---|---|---|
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 100.1 (20.82) | 100.5 (19.31) |
| Median number (Q1, Q3) | 100.0 (90.0, 115.0) | 97.5 (90.0, 115.0) |
| Min, Max | 45, 140 | 50, 140 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (4) | 74 (0) |
| Average value(standard deviation) | 114.5 (18.41) | 111.6 (18.75) |
| Median number (Q1, Q3) | 120.0 (105.0, 130.0) | 115.0 (95.0, 130.0) |
| Min, Max | 60, 135 | 75, 140 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 14.4 (22.24) | 11.1 (20.33) |
| Median number (Q1, Q3) | 15.0 (0.0, 30.0) | 7.5 (−5.0, 25.0) |
| Min, Max | −45, 75 | −35, 70 |
| Average value 95%CI | (9.0, 19.7) | (6.4, 15.8) |
| Adjusted average value(Standard error) [1] | 14.238(2.040) | 11.211(1.970) |
| Adjusted mean difference(95%CI) [1] | 3.027(-2.580,8.634) | |
| P Value [1] | 0.2877 |
The HSS score of the experimental group ranged from 40.0 to 99.0, with an average score of 80.10 ± 12.461. Compared with the baseline data, the postoperative HSS score was significantly increased by 14.38 ± 14.958 (95% CI: 10.78, 17.97). The control group ranged from 39.0 to 98.0 points, with an average of 79.45 ± 11.520 points. Compared with the baseline data, the postoperative HSS score was significantly increased by 16.43 ± 15.113 points (95% CI: 12.92, 19.93). There was no significant difference in the improvement of HSS score between the two groups (P = 0.9862) (Table 6).
Table 6.
Statistical description of HSS overall score of subjects in follow-up when compared to baseline.
| Follow up statistics | Study group (N = 69) | Control group (N = 74) |
|---|---|---|
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 65.7 (11.20) | 63.0 (13.28) |
| Median number (Q1, Q3) | 66.0 (60.0, 73.0) | 64.0 (55.0, 72.0) |
| Min, Max | 40, 89 | 32, 94 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 80.10 (12.461) | 79.45 (11.520) |
| Median number (Q1, Q3) | 83.00 (75.00, 87.00) | 81.00 (74.00, 86.00) |
| Min, Max | 40.0, 99.0 | 39.0, 98.0 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 14.38 (14.958) | 16.43 (15.113) |
| Median number (Q1, Q3) | 14.00 (5.00, 24.00) | 14.00 (7.00, 25.00) |
| Min, Max | −36.0, 45.0 | −17.0, 65.0 |
| Average value 95%CI | (10.78, 17.97) | (12.92, 19.93) |
| Adjusted average value(Standard error) [1] | 15.454(1.397) | 15.421(1.349) |
| P Value [1] | 0.9862 |
Based on the objective knee score, the average score of the experimental group was 70.0 ± 7.31, ranging from 44 to 77. Compared with the baseline data, the average objective knee score of the experimental group was improved to 30.4 ± 20.13; The control group ranged from 27 to 78 with an average of 67.8 ± 10.06; Compared with the baseline data, the average objective score of the control group was improved to 32.5 ± 23.75, and there was no significant difference between the two groups (P = 0.1107) (Table 7).
Table 7.
Statistical description of life quality assessments of subjects in follow-up when compared to baseline.
| Index Follow up Statistics |
Study group (N = 69) | Control group (N = 74) |
|---|---|---|
| Objective Value | ||
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 39.6 (18.40) | 35.2 (20.29) |
| Median number (Q1, Q3) | 35.0 (29.0, 57.0) | 33.0 (23.0, 41.0) |
| Min, Max | −3, 76 | −12, 76 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 70.0 (7.31) | 67.8 (10.06) |
| Median number (Q1, Q3) | 72.0 (66.0, 76.0) | 70.5 (64.0, 76.0) |
| Min, Max | 44, 77 | 27, 78 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 30.4 (20.13) | 32.5 (23.75) |
| Median number (Q1, Q3) | 37.0 (16.0, 44.0) | 36.0 (25.0, 46.0) |
| Min, Max | −11, 62 | −49, 88 |
| Average value 95%CI | (25.6, 35.2) | (27.0, 38.0) |
| Adjusted average value(Standard error) [1] | 32.732(1.055) | 30.371(1.019) |
| P Value[1 | 0.1107 | |
| Symptom Score | ||
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 15.7 (3.60) | 15.9 (3.95) |
| Median number (Q1, Q3) | 16.0 (13.0, 18.0) | 17.0 (13.0, 19.0) |
| Min, Max | 6, 23 | 2, 23 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 12.5 (3.89) | 11.5 (3.57) |
| Median number (Q1, Q3) | 12.0 (9.0, 16.0) | 12.0 (9.0, 13.0) |
| Min, Max | 6, 21 | 6, 23 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | −3.2 (4.86) | −4.4 (5.71) |
| Median number (Q1, Q3) | −4.0 (−7.0, 0.0) | −4.0 (−8.0, −1.0) |
| Min, Max | −12, 7 | −15, 12 |
| Average value 95%CI | (-4.4, −2.1) | (-5.7, −3.1) |
| Adjusted average value(Standard error) [1] | −3.355(0.446) | −4.277(0.431) |
| P值 [1] | 0.1390 | |
| Patients' satisfactory score | ||
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 17.0 (5.46) | 17.4 (6.49) |
| Median number (Q1, Q3) | 18.0 (14.0, 20.0) | 18.0 (12.0, 22.0) |
| Min, Max | 0, 30 | 4, 34 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 25.2 (7.31) | 26.8 (6.26) |
| Median number (Q1, Q3) | 26.0 (20.0, 30.0) | 28.0 (22.0, 30.0) |
| Min, Max | 10, 40 | 14, 40 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 8.3 (8.46) | 9.5 (8.18) |
| Median number (Q1, Q3) | 8.0 (2.0, 16.0) | 10.0 (4.0, 14.0) |
| Min, Max | −14, 30 | −10, 30 |
| Average value 95%CI | (6.3, 10.3) | (7.6, 11.4) |
| Adjusted average value(Standard error) [1] | 8.111(0.801) | 9.626(0.774) |
| P Value[1 | 0.1760 | |
| Value for surgical expectations | ||
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 14.4 (1.58) | 14.5 (1.35) |
| Median number (Q1, Q3) | 15.0 (15.0, 15.0) | 15.0 (15.0, 15.0) |
| Min, Max | 6, 15 | 8, 15 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 8.8 (2.91) | 8.7 (2.41) |
| Median number (Q1, Q3) | 9.0 (6.0, 11.0) | 9.0 (7.0, 9.0) |
| Min, Max | 3, 15 | 3, 15 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | −5.6 (3.12) | −5.8 (2.66) |
| Median number (Q1, Q3) | −6.0 (−8.0, −4.0) | −6.0 (−8.0, −5.0) |
| Min, Max | −12, 2 | −12, 3 |
| Average value 95%CI | (-6.4, −4.9) | (-6.4, −5.1) |
| Adjusted average value(Standard error) [1] | −5.671(0.316) | −5.725(0.305) |
| P Value[1 | 0.9019 | |
| Functional Score | ||
| Baseline | ||
| Number of cases (missing) | 67 (2) | 74 (0) |
| Average value(standard deviation) | 37.4 (17.15) | 33.3 (18.31) |
| Median number (Q1, Q3) | 39.0 (26.0, 49.0) | 31.5 (22.0, 45.0) |
| Min, Max | −10, 76 | −10, 84 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 68 (1) | 74 (0) |
| Average value(standard deviation) | 58.2 (18.19) | 54.7 (19.52) |
| Median number (Q1, Q3) | 60.5 (46.5, 71.0) | 56.5 (40.0, 71.0) |
| Min, Max | 5, 90 | 5, 89 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 66 (3) | 74 (0) |
| Average value(standard deviation) | 21.2 (22.84) | 21.4 (21.91) |
| Median number (Q1, Q3) | 22.0 (5.0, 42.0) | 21.0 (9.0, 33.0) |
| Min, Max | −45, 62 | −38, 81 |
| Average value 95%CI | (15.6, 26.8) | (16.3, 26.5) |
| Adjusted average value(Standard error) [1] | 22.708(2.247) | 20.058(2.121) |
| P Value[1 | 0.3942 |
Based on the symptom score, the score range of the experimental group was 6–21, and the average score was 12.5 ± 3.89. Compared with the baseline data, the average symptom score of the experimental group improved to −3.2 ± 4.86; The control group ranged from 6 to 23, with an average of 11.5 ± 3.75; Compared with the baseline data, the average symptom score of the control group was - 4.4 ± 5.71, and there was no significant difference between the two groups (P = 0.1390) (Table 7).
Based on patient satisfaction, the score of the experimental group ranged from 10 to 40, with an average score of 25.2 ± 7.31. Compared with the baseline data, the average satisfaction score of the experimental group was improved to8.3 ± 8.46; The control group ranged from 14 to 40, with an average of 26.8 ± 6.26; Compared with the baseline data, the average satisfaction score of the control group was improved to 9.5 ± 8.18, and there was no significant difference between the two groups (P = 0.1760) (Table 7).
Based on the expected score of surgery, the average score of the experimental group was 8.8 ± 2.91, ranging from 3 to 15. Compared with the baseline data, the average score of the experimental group was improved to-5.6 ± 3.12; The control group ranged from 3 to 15, with an average of 8.7 ± 2.41; Compared with the baseline data, the average score of the control group was - 5.8 ± 2.66, and there was no significant difference between the two groups (P = 0.9019) (Table 7).
Based on the functional score, the score of the experimental group ranged from 5 to 90, and the average score was 58.2 ± 18.19. Compared with the baseline data, the average functional score of the experimental group was improved to 21.2 ± 22.84; The control group ranged from 5 to 89, with an average of 54.7 ± 19.52; Compared with the baseline data, the average functional score of the control group was improved to 21.4 ± 21.91, and there was no significant difference between the two groups (P = 0.3942) (Table 7).∖
The WOMAC scores of the experimental group ranged from 0 to 193, with an average score of 80.6 ± 46.52. Compared with the baseline data, WOMAC score decreased to - 37.8 ± 58.65 (95% CI: - 51.9, - 23.7). The control group ranged from 7 to 206, with an average of 72.1 ± 44.40; Compared with baseline data, WOMAC score decreased by - 45.7 ± 49.38 (95% CI: - 57.2, - 34.3). There was no significant difference in WOMAC score between the two groups (P = 0.2559) (Table 8).
Table 8.
Statistical description of WOMAC overall score of subjects in follow-up when compared to baseline.
| Follow up Statistics | Study group (N = 69) | Control group (N = 74) |
|---|---|---|
| Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 118.4 (40.73) | 117.8 (41.29) |
| Median number (Q1, Q3) | 112.0 (86.0, 145.0) | 119.0 (91.0, 140.0) |
| Min, Max | 28, 238 | 9, 235 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | 80.6 (46.52) | 72.1 (44.40) |
| Median number (Q1, Q3) | 80.0 (44.0, 111.0) | 62.5 (38.0, 92.0) |
| Min, Max | 0, 193 | 7, 206 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 69 (0) | 74 (0) |
| Average value(standard deviation) | −37.8 (58.65) | −45.7 (49.38) |
| Median number (Q1, Q3) | −38.0 (−73.0, −11.0) | −44.0 (−71.0, −13.0) |
| Min, Max | −196, 164 | −181, 81 |
| Average value 95%CI | (-51.9, −23.7) | (-57.2, −34.3) |
| Adjusted average value(Standard error) [1] | −37.563(5.297) | −45.962(5.115) |
| P Value[1 | 0.2559 |
The score of the experimental group ranged from 14.4 to 97.1, with an average score of 61.19 ± 19.906. Compared with the baseline data, the average SF-36 Health Scale score of the experimental group was improved to 10.74 ± 20.409; The control group ranged from 16.7 to 97.3 with an average of 63.05 ± 19.021; Compared with the baseline data, the average SF-36 Health Scale score of the control group was improved to 14.27 ± 21.204, and there was no significant difference between the two groups (P = 0.4511) (Table 9).
Table 9.
Statistical description of SF-36 health scale value of subjects in follow-up when compared to baseline.
| Follow up statistics | Study group (N = 69) | Control group (N = 74) |
|---|---|---|
| Baseline | ||
| Number of cases (missing) | 68 (1) | 74 (0) |
| Average value(standard deviation) | 50.80 (17.431) | 48.50 (16.086) |
| Median number (Q1, Q3) | 48.05 (37.45, 64.20) | 47.65 (37.70, 58.20) |
| Min, Max | 18.8, 89.5 | 19.7, 87.4 |
| POD 12 weeks ± 10 days | ||
| Number of cases (missing) | 69 (0) | 72 (2) |
| Average value(standard deviation) | 61.19 (19.906) | 63.05 (19.021) |
| Median number (Q1, Q3) | 63.60 (47.70, 75.20) | 61.80 (51.30, 77.35) |
| Min, Max | 14.4, 97.1 | 16.7, 97.3 |
| Relative Change of Baseline | ||
| Number of cases (missing) | 68 (1) | 72 (2) |
| Average value(standard deviation) | 10.74 (20.409) | 14.27 (21.204) |
| Median number (Q1, Q3) | 11.15 (−1.35, 24.50) | 14.20 (−1.15, 32.60) |
| Min, Max | −55.0, 54.6 | −50.8, 53.7 |
| Average value 95%CI | (5.80, 15.68) | (9.28, 19.25) |
| Adjusted average value(Standard error) [1] | 11.360(2.197) | 13.677(2.135) |
| P Value[1 | 0.4511 |
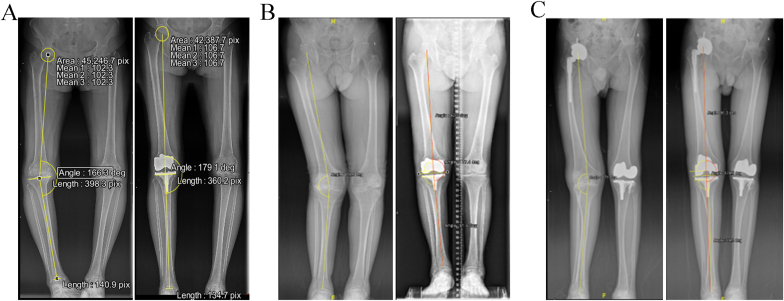
Three typical cases which performed by HURWA robot-assisted TKA system were showed (Fig. 5).
Figure 5.
Three typical cases which performed by HURWA robot-assisted TKA system. A. A case of severe varus deformity. B. A case of severe valgus deformity. C. A case of severe varus deformity that has been performed by THA of right side and TKA of left side.
4. Discussion
KOA is one of the common joint diseases in the elderly and it is also the main cause of knee pain and functional limitation in the elderly [34,35]. TKA is a relative successful and effective method for relieving pain and functional recovery of end-stage knee osteoarthritis, which has been widely carried out worldwide [9,36]. Reconstruction of good lower limb alignment is one of the main purposes of TKA, and it is also an important guarantee of patient satisfaction and prosthesis survival rate after TKA [37,38]. Traditional TKA depends on surgical instruments to complete knee joint parameter measurement, prosthesis model selection and surgical scheme implementation. Although new prosthesis and surgical instruments with more perfect design are constantly coming out, and the surgical technology of the operator is also improving year by year, TKA has not yet become a perfect operation, and its postoperative dissatisfaction rate is as high as 20% [39,40]. The main cause is that TKA has high requirements on the position of prosthesis placement, reconstruction of lower limb force line and maintenance of postoperative stability, while manual operation is difficult to ensure the accuracy and consistency of surgical operation [[41], [42], [43]]. Therefore, poor prosthesis position and poor alignment of lower limb occur from time to time, which seriously affects the stability of knee joint and recovery of motor function and the long-term survival rate and postoperative satisfaction of patients were reduced.
The lower limb force line is relative to the vertical line through the pubic symphysis [44]. It is a line starting from the rotation center of the femoral head and ending at the midpoint of the medial and lateral malleolus. It represents the mechanical transmission line of the lower limb in the load-bearing position. With the continuous improvement of science and technology, as well as the in-depth study of coronal force line, it is generally believed that controlling the lower limb force line after TKA in the coronal plane, genu varus within ±3° is the relative “safe area”, and this standard is used to distinguish the good or bad force line [45].
Many developments in surgical technologies have been achieved in the field of operations. Although robotics has been applicated for about two decades in the other specialties, it has only recently been widely utilized in the field of abdominal surgery. Standard extramedullary and intramedullary guides procedures are the most common technologies for obtaining component alignments for TKA surgery [46,47]. Recently, robotic-assisted TKA surgery has been developed and applicated to ameliorate accuracies in component positioning and bone resection, as well as to improve patient satisfaction and functional outcomes of knee [[48], [49], [50], [51]]. For instance, it has showed that MAKO robotic-assisted TKA ameliorated postoperative pain and perfected implant positioning with equally or slightly superior amelioration of the clinical outcomes, compared to control TKA, at postoperative one year [52]. Sires and their colleagues also found that MAKO robotic-assisted TKA can improve the accuracy of component positioning and the precision of bone resection [53]. Recently, Seidenstein and their colleagues demonstrated that ROSA robotic-assisted TKA improve the precision of bone resection compared to conventional TKA in the cadaveric study [54]. However, more robotic-assisted TKA systems still need to be designed and developed, especially in China.
Recently, one new HURWA robotic-assisted TKA system (Beijing, China) was utilized in TKA surgery. Our previous studies showed that this new robotic-assisted TKA system significantly improve the accuracy of bone resection levels and angles in the Sawbone model [33]. Moreover, we demonstrated that this new system is a safe and accurate tool for TKA surgery in the sheep model [32]. However, clinical experiments are required to confirm the safety and accuracy of this system. Herein, we performed a randomized, multi-centers, single blind and parallel control trial of HURWA robotic-assisted versus conventional TKA to study the effectiveness and safety of this system. We found that the postoperative mean HKA angle was 1.801° ± 1.608° of varus for the robot-assisted TKA group and 3.017° ± 2.735° of varus for the conventional TKA group; these values were significantly different. The robot-assisted TKA group showed a 81.2% malalignment for mechanical axis lower than 3° and the conventional TKA group showed 63.5%. In this study, we used for 4 scoring systems to analyze patient outcomes The WOMAC score is widely used in the analysis of knee osteoarthritis. It has 3 major components, namely, pain, stiffness and physical function. The HSS score is used for evaluating the clinical results of knee arthroplasty and has six major components: pain, function, range of motion, muscle strength, knee flexion deformity, and stability. KSS score system is user-friendly and concise, providing assessment of the following key areas: pain, flexion contracture, extension lag, total range of motion, and stability in the anteroposterior and mediolateral planes. The SF-36 score system is more responsive measure of the overall quality of life of osteoarthritis patients and is frequently used for measuring knee arthroplasty outcomes [55]. Therefore, we chose these four scoring systems. Our study also found that these patients who underwent robot-assisted TKA had improved knee flexion and functional recovery following to HSS score, KSS score, WOMAC score and SF-36 score compared with preoperative, even though there was no significant difference between the conventional TKA group. The reasons may include two aspects: 1. The knee joint performance and function are affected by many factors, such as soft tissue balance, muscle relaxation, bone condition, postoperative rehabilitation exercise, patient complications, etc; 2. The correction of lower limb alignment may not lead to the incremental improvement of clinical efficacy in a short time, or it may be due to the small sample size, which is difficult to observe the difference between groups; Therefore, long-term follow-up or increasing the sample size are needed to further observe the improvement of clinical efficacy. Furthermore, this system did not increase the risk of TKA.
Our study has some major limitations. The sample size in our study is relatively small and more cases are needed to validate this new robotic-assisted TKA system. Secondly, no other robotic-assisted TKA systems were used as the control group. Future studies should provide a head-to-head comparison of safety and efficacy of different robotic-assisted TKA systems. Third, the follow-up time is relative short and long-term follow-up is needed to observe the improvement of clinical efficacy. In summary, HURWA robot-assisted TKA system is a safe and effective system for TKA, which had improved knee flexion and functional recovery compared with preoperative, even though there was no significant difference between the conventional TKA group. Moreover, we found that HURWA robot-assisted TKA has a lot of advantages over conventional TKA including its ability to improve malalignment for mechanical axis. Thus, longer follow-up period is needed to study whether the improve malalignment for mechanical axis will lead to improve long-term survival and better clinical outcomes.
Funding
This study was supported by Beijing Municipal science & technology Commission (No. Z191100007619029 and Z2011100002521007) and National Natural Science Foundation of China (No: 81871829).
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgments
All persons who have made substantial contributions to the work reported in the manuscript (e.g., technical help, writing and editing assistance, general support), but who do not meet the criteria for authorship, are named in the Acknowledgements and have given us their written permission to be named. If we have not included an Acknowledgements, then that indicates that we have not received substantial contributions from non-authors.
Contributor Information
Yuan Lin, Email: linyuan@ccmu.edu.cn.
Jun Liu, Email: drliujun1968@126.com.
Jin Lin, Email: linjinpumc@163.com.
References
- 1.Terpstra S.E.S., van der Velde J., de Mutsert R., Schiphof D., Reijnierse M., Rosendaal F.R., et al. The association of clinical and structural knee osteoarthritis with physical activity in the middle-aged population: the NEO study. Osteoarthritis Cartilage. 2021;29(11):1507–1514. doi: 10.1016/j.joca.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Rafiq M.T., Hamid M.S.A., Hafiz E., Chaudhary F.A., Khan M.I. Feasibility and acceptability of instructions of daily care in overweight and obese knee osteoarthritis participants. Curr Rheumatol Rev. 2021;17(4):421–427. doi: 10.2174/1573397117666210727095552. [DOI] [PubMed] [Google Scholar]
- 3.Jansen M.P., Welsing P.M.J., Vincken K.L., Mastbergen S.C. Performance of Knee Image Digital Analysis of radiographs of patients with end-stage knee osteoarthritis. Osteoarthritis Cartilage. 2021;(11):1530–1539. doi: 10.1016/j.joca.2021.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Lau L.C.M., Fan J.C.H., Chung K.Y., Cheung K.W., Man G.C.W., Hung Y.W., et al. Satisfactory long-term survival, functional and radiological outcomes of open-wedge high tibial osteotomy for managing knee osteoarthritis: minimum 10-year follow-up study. J Orthop Transl. 2021;26:60–66. doi: 10.1016/j.jot.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Furlough K., Miner H., Crijns T.J., Jayakumar P., Ring D., Koenig K. What factors are associated with perceived disease onset in patients with hip and knee osteoarthritis? J Orthop. 2021;26:88–93. doi: 10.1016/j.jor.2021.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robbins S.M., Pelletier J.P., Abram F., Boily M., Antoniou J., Martineau P.A., et al. Gait risk factors for disease progression differ between non-traumatic and post-traumatic knee osteoarthritis. Osteoarthritis Cartilage. 2021;29(11):1487–1497. doi: 10.1016/j.joca.2021.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Chen L., Zheng J.J.Y., Li G., Yuan J., Ebert J.R., Li H., et al. Pathogenesis and clinical management of obesity-related knee osteoarthritis: impact of mechanical loading. J Orthop Transl. 2020;24:66–75. doi: 10.1016/j.jot.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park S., Min S., Park S.H., Yoo J., Jee Y.S. Influence of isometric exercise combined with electromyostimulation on inflammatory cytokine levels, muscle strength, and knee joint function in elderly women with early knee osteoarthritis. Front Physiol. 2021;12:688260. doi: 10.3389/fphys.2021.688260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyazaki S., Yoshinaga S., Tsuruta K., Hombu A., Fujii Y., Arakawa H., et al. Total knee arthroplasty improved locomotive syndrome in knee osteoarthritis patients: a prospective cohort study focused on total clinical decision limits stage 3. BioMed Res Int. 2021;2021:3919989. doi: 10.1155/2021/3919989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li D., Bi A.S., Samra S.S., Samra N.S., Wu D., Ma Y. Functional outcomes following total knee arthroplasty without patellar resurfacing: a minimum two-year follow-up retrospective cohort study. Cureus. 2021;13(6) doi: 10.7759/cureus.16036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stobe C., Hoechel S., Muller-Gerbl M., Nowakowski A.M. Systematic effects of femoral component rotation and tibial slope on the medial and lateral tibiofemoral flexion gaps in total knee arthroplasty. J Othop Transl. 2020;24:218–223. doi: 10.1016/j.jot.2019.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeng Y.M., Yan M.N., Li H.W., Zhang J., Wang Y. Does mobile-bearing have better flexion and axial rotation than fixed-bearing in total knee arthroplasty? A randomised controlled study based on gait. J Othop Transl. 2020;20:86–93. doi: 10.1016/j.jot.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng B., Zhu W., Bian Y.Y., Chang X., Cheng K.Y., Weng X.S. China artificial joint annual data report. Chinese Med J. 2020;134(6):752–753. doi: 10.1097/CM9.0000000000001196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bercovy M., Kerboull L., Muller J.H., Saffarini M., Sailhan F. Satisfactory mid- to long-term outcomes of TKA aligned using conventional instrumentation for flexion gap balancing with minimal soft tissue release. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2020 doi: 10.1007/s00167-020-06360-3. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Lee D.H., Park J.H., Song D.I., Padhy D., Jeong W.K., Han S.B. Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2010;18(3):381–387. doi: 10.1007/s00167-009-0983-x. [DOI] [PubMed] [Google Scholar]
- 16.Lim D., Kwak D.S., Kim M., Kim S., Cho H.J., Choi J.H., et al. Kinematically aligned total knee arthroplasty restores more native medial collateral ligament strain than mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2021 doi: 10.1007/s00167-021-06680-y. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Bouche P.A., Corsia S., Dechartres A., Resche-Rigon M., Nizard R. Are there differences in accuracy or outcomes scores among navigated, robotic, patient-specific instruments or standard cutting guides in TKA? A network meta-analysis. Clin Orthop Relat Res. 2020;478(9):2105–2116. doi: 10.1097/CORR.0000000000001324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fournier G., Muller B., Gaillard R., Batailler C., Lustig S., Servien E. Increased survival rate for primary TKA with tibial short extension stems for severe varus deformities at a minimum of 2 years follow-up. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2020;28(12):3780–3786. doi: 10.1007/s00167-020-05848-2. [DOI] [PubMed] [Google Scholar]
- 19.Batailler C., Parratte S. Assistive technologies in knee arthroplasty: fashion or evolution? Rate of publications and national registries prove the Scott Parabola wrong. Arch Orthop Trauma Surg. 2021;141(12):2027–2034. doi: 10.1007/s00402-021-04051-3. [DOI] [PubMed] [Google Scholar]
- 20.Moerenhout K., Allami B., Gkagkalis G., Guyen O., Jolles B.M. Advantages of patient-specific cutting guides with disposable instrumentation in total knee arthroplasty: a case control study. J Orthop Surg Res. 2021;16(1):188. doi: 10.1186/s13018-021-02310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hickey M.D., Anglin C., Masri B., Hodgson A.J. How large a study is needed to detect TKA revision rate reductions attributable to robotic or navigated technologies? A simulation-based power analysis. Clin Orthop Related Res. 2021;479(11):2350–2361. doi: 10.1097/CORR.0000000000001909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marchand K.B., Moody R., Scholl L.Y., Bhowmik-Stoker M., Taylor K.B., Mont M.A., et al. Results of robotic-assisted versus manual total knee arthroplasty at 2-year follow-up. J Knee Surg. 2021 doi: 10.1055/s-0041-1731349. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Batailler C., Fernandez A., Swan J., Servien E., Haddad F.S., Catani F., et al. MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2020;37:299–305. doi: 10.1007/s00167-020-06283-z. [DOI] [PubMed] [Google Scholar]
- 24.Solis M. New Frontiers in Robotic Surgery: the latest high-tech surgical tools allow for superhuman sensing and more. IEEE Pulse. 2016;7(6):51–55. doi: 10.1109/MPUL.2016.2606470. [DOI] [PubMed] [Google Scholar]
- 25.Chan J., Auld T.S., Long W.J., Kreuzer S., Campanelli V., Liebelt R., et al. Active robotic total knee arthroplasty (TKA): initial experience with the TSolution one (R) TKA system. Surg Technol Int. 2020;37:299–305. [PubMed] [Google Scholar]
- 26.Batailler C., Hannouche D., Benazzo F., Parratte S. Concepts and techniques of a new robotically assisted technique for total knee arthroplasty: the ROSA knee system. Arch Orthop Trauma Surg. 2021;141(12):2049–2058. doi: 10.1007/s00402-021-04048-y. [DOI] [PubMed] [Google Scholar]
- 27.Liow M.H., Xia Z., Wong M.K., Tay K.J., Yeo S.J., Chin P.L. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014;29(12):2373–2377. doi: 10.1016/j.arth.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 28.Schafer P., Mehaidli A., Zekaj M., Padela M.T., Rizvi S.A., Chen C., et al. Assessing knee anatomy using Makoplasty software a case series of 99 knees. J Orthop. 2020;20:347–351. doi: 10.1016/j.jor.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sires J.D., Wilson C.J. CT validation of intraoperative implant position and knee alignment as determined by the MAKO total knee arthroplasty system. J Knee Surg. 2020;34(10):1133–1137. doi: 10.1055/s-0040-1701447. [DOI] [PubMed] [Google Scholar]
- 30.Sires J.D., Craik J.D., Wilson C.J. Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. 2021;34(7):745–748. doi: 10.1055/s-0039-1700570. [DOI] [PubMed] [Google Scholar]
- 31.Blum C.L., Lepkowsky E., Hussein A., Wakelin E.A., Plaskos C., Koenig J.A. Patient expectations and satisfaction in robotic-assisted total knee arthroplasty: a prospective two-year outcome study. Arch Orthop Trauma Surg. 2021;141(12):2155–2164. doi: 10.1007/s00402-021-04067-9. [DOI] [PubMed] [Google Scholar]
- 32.Chen X., Li Z., Zhang X., Yan J., Ding L., Song Y., et al. A new robotically assisted system for total knee arthroplasty: a sheep model study. The international journal of medical robotics + computer assisted surgery : MRCAS. 2021;17(4):e2264. doi: 10.1002/rcs.2264. [DOI] [PubMed] [Google Scholar]
- 33.Li Z., Chen X., Zhang X., Yan J., Song Y., Huo Y., et al. Better precision of a new robotically assisted system for total knee arthroplasty compared to conventional techniques: a sawbone model study. The international journal of medical robotics + computer assisted surgery : MRCAS. 2021;17(4) doi: 10.1002/rcs.2263. [DOI] [PubMed] [Google Scholar]
- 34.Malanga G., Niazi F., Kidd V.D., Lau E., Kurtz S.M., Ong K.L., et al. Knee osteoarthritis treatment costs in the medicare patient population. Am Health Drug Benefits. 2020;13(4):144–153. [PMC free article] [PubMed] [Google Scholar]
- 35.Fekete H., Guillemin F., Pallagi E., Fekete R., Lippai Z., Luteran F., et al. Evaluation of osteoarthritis knee and hip quality of life (OAKHQoL): adaptation and validation of the questionnaire in the Hungarian population. Ther Adv Musculoskel Dis. 2020;12 doi: 10.1177/1759720X20959570. 1759720X20959570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Durmus Iskender M., Caliskan N. Effect of acupressure and abdominal massage on constipation in patients with total knee arthroplasty: a randomized controlled study. Clin Nurs Res. 2021 doi: 10.1177/10547738211033917. 10547738211033917. [DOI] [PubMed] [Google Scholar]
- 37.Kawaguchi K., Inui H., Taketomi S., Yamagami R., Takagi K., Kage T., et al. Rotational kinematics differ between mild and severe valgus knees in total knee arthroplasty. Knee. 2021;28:81–88. doi: 10.1016/j.knee.2020.10.010. [DOI] [PubMed] [Google Scholar]
- 38.Putnis S.E., Neri T., Coolican M.R.J. Total knee arthroplasty in a transtibial amputee. J Orthop Case Rep. 2020;10(3):15–18. doi: 10.13107/jocr.2020.v10.i03.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bian T., Shao H., Zhou Y., Huang Y., Song Y. Does psychological distress influence postoperative satisfaction and outcomes in patients undergoing total knee arthroplasty? A prospective cohort study. BMC Muscoskel Disord. 2021;22(1):647. doi: 10.1186/s12891-021-04528-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rantasalo M., Palanne R., Vakkuri A., Olkkola K.T., Madanat R., Skants N. Use of a tourniquet and spinal anesthesia increases satisfactory outcomes after total knee arthroplasty: a randomized study. J Bone Joint Surg Am. 2021;103(20):1890–1899. doi: 10.2106/JBJS.20.02080. [DOI] [PubMed] [Google Scholar]
- 41.Huang G., Xia J., Wang S., Wei Y., Wu J., Chen F., et al. Total knee arthroplasty using trochlear groove as guide for position of femoral component in severe knee osteoarthritis. BMC Surg. 2016;16(1):33. doi: 10.1186/s12893-016-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sicat C.S., Chow J.C., Kaper B., Mitra R., Xie J., Schwarzkopf R. Component placement accuracy in two generations of handheld robotics-assisted knee arthroplasty. Arch Orthop Trauma Surg. 2021;141(12):2059–2067. doi: 10.1007/s00402-021-04040-6. [DOI] [PubMed] [Google Scholar]
- 43.Tan J., Zou D., Zhang X., Zheng N., Pan Y., Ling Z., et al. Loss of knee flexion and femoral rollback of the medial-pivot and posterior-stabilized total knee arthroplasty during early-stance of walking in Chinese patients. Front Bioeng Biotechnol. 2021;9 doi: 10.3389/fbioe.2021.675093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peng H., Ou A., Huang X., Wang C., Wang L., Yu T., et al. Osteotomy around the knee: the surgical treatment of osteoarthritis. Orthop Surg. 2021;13(5):1465–1473. doi: 10.1111/os.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aquili A., Cane P.P., Fravisini M., Farinelli L., Procaccini R., Gigante A.P. Extramedullary femoral alignment system in total knee arthroplasty: accuracy in relation of severity and different types of varus. J Orthop. 2021;24:86–90. doi: 10.1016/j.jor.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang T., Chuang P., Lee C., Lin S., Huang K., Shen S., et al. Total knee arthroplasty in patients with Ranawat type-II valgus arthritic knee with a marked coronal femoral bowing deformity: comparison between computer-assisted surgery and intra-articular resection. J Orthop Surg Res. 2016;11(1):88. doi: 10.1186/s13018-016-0422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nam D., Cross M., Deshmane P., Jerabek S., Kang M., Mayman D. Radiographic results of an accelerometer-based, handheld surgical navigation system for the tibial resection in total knee arthroplasty. Orthopedics. 2011;34(10):e615–e621. doi: 10.3928/01477447-20110826-12. [DOI] [PubMed] [Google Scholar]
- 48.Banger M., Johnston W., Razii N., Doonan J., Rowe P., Jones B., et al. Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: a prospective randomized controlled trial. Bone Joint Lett J. 2020;(11):1511–1518. doi: 10.1302/0301-620X.102B11.BJJ-2020-1166.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scholl L., Hampp E., de Souza K., Chang T., Deren M., Yenna Z., et al. How does robotic-arm assisted technology influence total knee arthroplasty implant placement for surgeons in fellowship training? J Knee Surg. 2020;35(2):198–203. doi: 10.1055/s-0040-1716983. [DOI] [PubMed] [Google Scholar]
- 50.Kayani B., Konan S., Tahmassebi J., Oussedik S., Moriarty P., Haddad F. A prospective double-blinded randomised control trial comparing robotic arm-assisted functionally aligned total knee arthroplasty versus robotic arm-assisted mechanically aligned total knee arthroplasty. Trials. 2020;21(1):194. doi: 10.1186/s13063-020-4123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xia R., Zhai Z., Zhang J., Yu D., Wang L., Mao Y., et al. Verification and clinical translation of a newly designed “Skywalker” robot for total knee arthroplasty: a prospective clinical study. J Orthop Transl. 2021;29:143–151. doi: 10.1016/j.jot.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Batailler C., Fernandez A., Swan J., Servien E., Haddad F., Catani F., et al. MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020;29(11):3585–3598. doi: 10.1007/s00167-020-06283-z. [DOI] [PubMed] [Google Scholar]
- 53.Sires J., Craik J., Wilson C. Accuracy of bone resection in MAKO total knee robotic-assisted surgery. J Knee Surg. 2019;34(7):745–748. doi: 10.1055/s-0039-1700570. [DOI] [PubMed] [Google Scholar]
- 54.Seidenstein A., Birmingham M., Foran J., Ogden S. Better accuracy and reproducibility of a new robotically-assisted system for total knee arthroplasty compared to conventional instrumentation: a cadaveric study. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2021;29(3):859–866. doi: 10.1007/s00167-020-06038-w. [DOI] [PubMed] [Google Scholar]
- 55.Liow M.H.L., Goh G.S., Wong M.K., Chin P.L., Tay D.K., Yeo S.J. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2017;25(9):2942–2951. doi: 10.1007/s00167-016-4076-3. [DOI] [PubMed] [Google Scholar]