Abstract
This paper reports a case of basilar artery occlusion (BAO), a relatively rare event associated with high mortality rate and high risk of disability. A 77-year-old man arrived at our Stroke Unit approximately 14 hours after the onset of symptoms (dysarthria and complete left hemiparesis) with progressive worsening up to coma and with a National Institute Health Stroke Scale (NIHSS) of 22.
The patient was treated and, at discharge, the modified Rankin scale and NIHSS were 2 and 5, respectively. The aim of this paper is to illustrate how revascularization treatment, also after 12 hours, could be a viable option to ensure survival and a good life quality for the patient. Furthermore, it is essential to encourage the publication of a greater number of trials about the posterior circulation emphasizing how many favorable prognosis indicators are now recognized.
Keywords: Neuroradiology, Interventional neuroradiology, Revascularization, Basilar artery occlusion, Stroke
Introduction
Basilar artery occlusion (BAO) is a relatively rare event, accounting for about 1% of strokes, but is strongly associated with a high mortality rate and high risk of disability [1,2].
While there are many randomized and controlled trials about the efficacy and safety of endovascular treatments in occlusion of the anterior circulation vessels, scant literature has been produced regarding occlusion of the basilar artery [3].
In this case report we want to illustrate a BAO case treated over 12 hours with excellent outcome.
Case report
A 77-year-old man, with a history of smoking and hypertension, arrived at our Stroke Unit around 1 PM, after a double transfer from the hospital of the island of residence of the patient and then from one of the spoke units linked to our hub thanks to an inter-company agreement stipulated by our institution with the local ASL (local health companies).
The symptoms onset occurred around 11 PM of the previous day as dysarthria and complete left hemiparesis, with progressive worsening during the transfer to our unit, up to coma (CGS <8) with a National Institute Health Stroke Scale (NIHSS) of 22. He arrived approximately 14 hours after onset and no intravenous or intra-arterial thrombolytic therapy was administered, as he was beyond the standard treatment windows of 4.5 and 6 hours, but had received heparin iv.
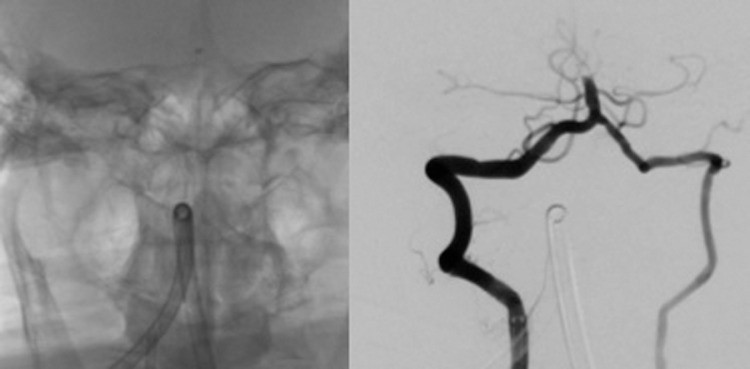
Once intubated was submitted to CT examination which excluded the presence of hemorrhagic areas and revealed the presence of spontaneously hyperdensity of the basilar artery, he was then transported to the angio suite (Fig. 1).
Fig. 1.
CT examination excludes the presence of hemorrhagic areas and reveals the presence of spontaneously hyperdensity of the basilar artery.
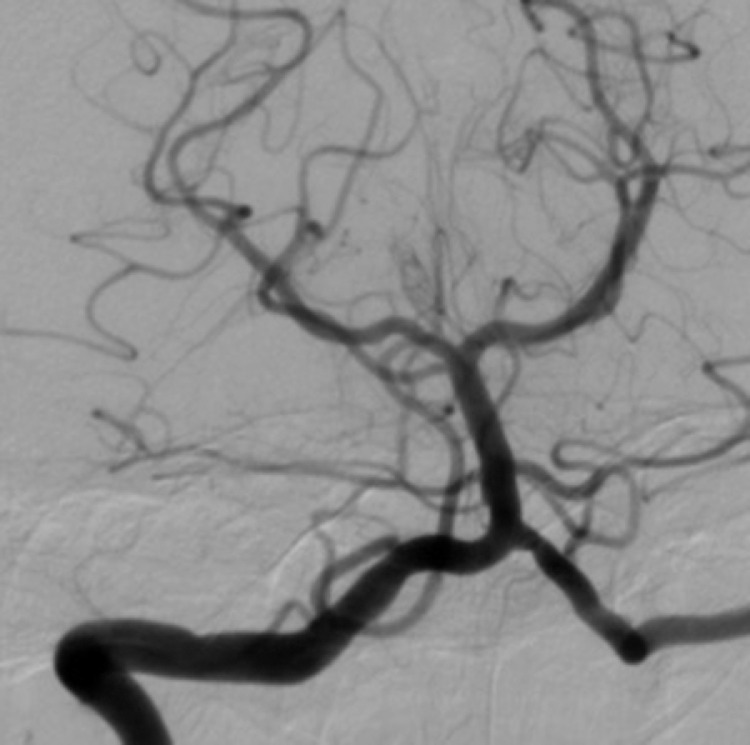
Angiography confirmed a BAO extending from the middle third of the basilar artery to its apex (Fig. 2).
Fig. 2.
First angiogram from RVA showing occlusion of basilar artery before its bifurcation. Initial angiogram demonstrating occlusion of the basilar artery beyond the PICA.
The basilar apex was supplied by large bilateral posterior communicating arteries, which opacified bilateral superior cerebellar arteries, basilar apex, and bilateral posterior cerebral arteries.
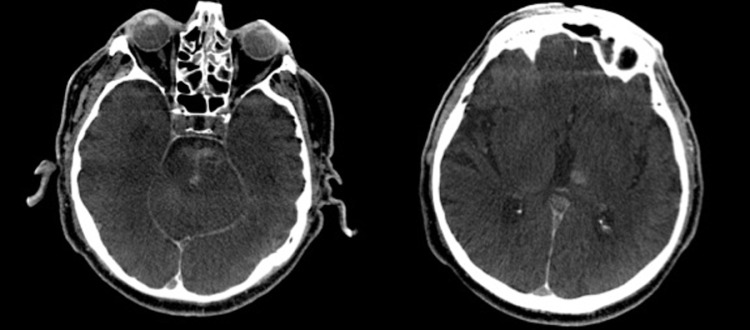
The right vertebral artery was accessed with a 6F Neuron guide catheter (Penumbra) over a 0.060in x 132 mm AXS Catalyst 6 and VBJ was crossed with a 18 Rebar microcatheter up to the basilar thrombus. Two 3-minutes attempts of mechanical thrombectomy and aspiration were performed utilizing two 60mL VacLok vacuum pressure syringes through the AXS Catalyst 6 catheter and the 088 6F Neuron MAX (Penumbra), respectively. The subsequent angiogram demonstrated BAO resolution and distal branch occlusion at P2 of left posterior cerebral artery. Other 2 aspiration attempts were performed at this level with a 139 reperfusion catheter 4MAX (Penumbra) and TICI III was obtained (Fig. 3). The femoral arterial access was closed with manual compression.
Fig. 3.
TICI III complete revascularization of posterior cerebral artery after aspiration with 4MAX catheter.
Post-procedural dynaCT showed hyperperfusion of left hemipons, right cerebral pedicle and left thalamus (Fig. 4). The patient was extubated while still in angiography room and neurologically evaluated, showing mild left extremities weakness and mild dysarthria.
Fig. 4.
Post-procedural dynaCT demonstrating hyperperfusion in pontine and left thalamic regions.
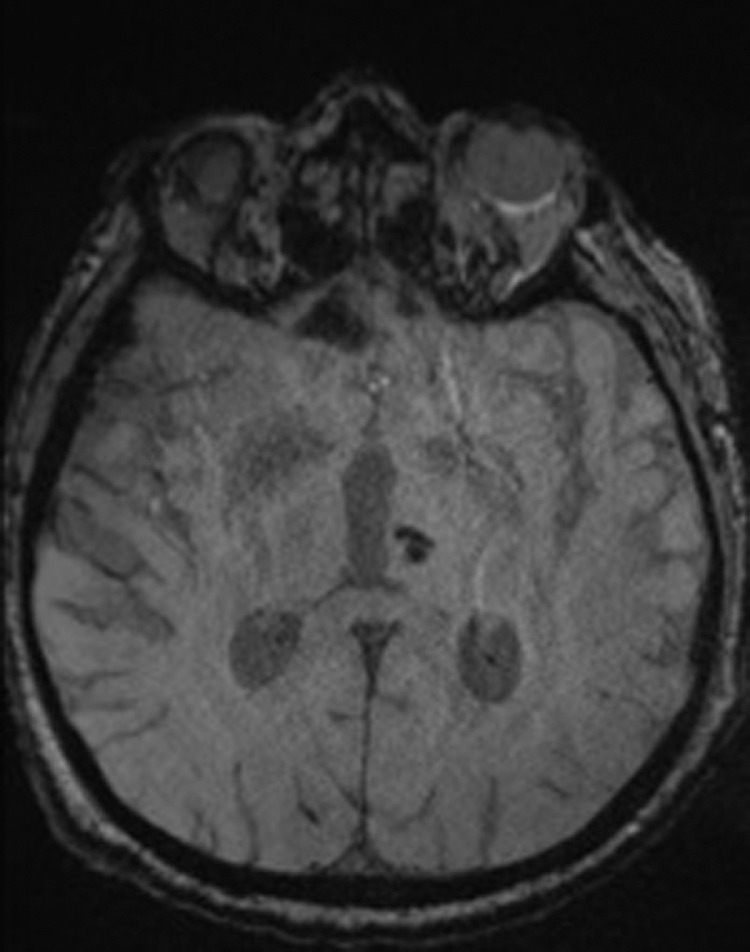
Follow-up MRI revealed hemosiderin from previous post-thrombectomy revascularization at the level of the central portion of the pons and in the left thalamo-capsular region, with stabilized ischemic lesion in the remaining areas pertaining to the basilar (Fig. 5).
Fig. 5.
Hemosiderinic deposit in left thalamus as small post-thrombectomy reperfusion injury.
At discharge, the modified Rankin scale and NIHSS were 2 and 5, respectively.
Discussion
The occlusion of the basilar artery represents an uncommon but dramatic event, usually fatal in the absence of revascularization. It accounts for about 20% of posterior circulation stroke and approximately only 1% of all ischemic strokes. The rate of mortality in BAO can exceed 90% without treatment. In addition, poor clinical outcomes despite successful recanalization are more common in patients with acute BAO than with anterior great vessel occlusion [1,4,5].
Although there are multiple randomized controlled trials that have reported the efficacy and safety of endovascular procedures (EVT) in occlusion of the anterior great vessels, patients with BAO were not included in these studies [3]. For this reason, no protocols have yet been established for the standard treatment of BAO, contrary to what is defined for the anterior vascular circle thanks to the experience of 7 clinical trials [1,2,[6], [7], [8], [9]–10].
The American Heart Association/American Stroke Association guidelines (2015) state that there is reasonable benefit of thrombectomy in BAO, in carefully selected patients with posterior circulation stroke if initiated within the first 6 hours of onset stroke (Class IIb; Level of Evidence C). After 6 hours, the endovascular treatment is to be considerated off-label [11].
Some studies have reported that the time window of EVT can be extended to 16 hours or to 24 hours in selected cases. In particular, in the DEFUSE-3 trial, patients must be selected by performing an MRI with DWI / PWI sequences or with a CT perfusion. The selection criteria are: time to onset of symptoms <16 hours; age <90 years; infarct core <70 mL, penumbra area >15 mL, volume ratio between hypoperfusion area and infarct area >1.8. In the DAWN trial, patients must be selected by performing an MRI with DWI sequences or with a CT perfusion that evaluates only the infarct core.
The time to onset of symptoms have to be <24 hours. The selection criteria are: age <80 years, NIHSS score >10 and infarct core <31 mL; age <80, NIHSS score >20, and infarct core of 31-51 mL; age >80 years, NIHSS score >10, and infarct core <21 mL [12,13].
There are still few data regarding revascularization after 12 hours in BAO and in literature only case reports are present, like in our case.
The purpose of our work is to highlight how the treatment of a basilar artery occlusion is essential to try to guarantee the patient a better quality of life and survival. It is therefore advisable to proceed with revascularization even beyond 6 hours and even when, for clinical reasons (NIHSS >20 and GCS <8, like in our case report), it is not possible to select patients with advanced imaging tests, as indicated by the DEFUSE-3 and DAWN.
Furthermore, another aim of our work is to emphasize how important it is to take into account all known favorable prognostic indicators in addition to the time to onset of symptoms.
In particular, suggested favorable prognostic indicators for BAO revascularization include [[14], [15]–16]:
-
-
the young age;
-
-
low grade NIHSS on admission;
-
-
floating presentation;
-
-
localization of the clot;
-
-
collateral filling of the basilar artery;
-
-
successful recanalization.
In light of this we agree with a recent study that underestimates the relationship between reperfusion time and prognosis, in favor of the diagnostic indicators described above [3] even if Mokin et al. [17] point out the key role of time to treatment on the clinical outcome rate. They report high success rate in patients with thrombectomy starts within the first 6 hours compared to patients treat beyond the 6-hour window. Additionally, a negative outcome rate is reported more beyond the 9-hour window.
Guarantor
The scientific guarantor of this publication is M.T.
Statistics and biometry
One of the authors (F.T.) has significant statistical expertise.
Patient consent
Written informed consent was obtained from all subjects (patient) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been reported in previous studies.
Footnotes
Acknowledgments: The authors state that this work has not received any funding.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009;8(8):724–730. doi: 10.1016/S1474-4422(09)70173-5. Epub 2009 Jul 3. PMID: 19577962. [DOI] [PubMed] [Google Scholar]
- 2.Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. 2015;77(3):415–424. doi: 10.1002/ana.24336. Epub 2015 Jan 13. PMID: 25516154. [DOI] [PubMed] [Google Scholar]
- 3.Kwak HS, Park JS. Mechanical thrombectomy in basilar artery occlusion: clinical outcomes related to posterior circulation collateral score. Stroke. 2020;51(7):2045–2050. doi: 10.1161/STROKEAHA.120.029861. Epub 2020 Jun 17. PMID: 32568658. [DOI] [PubMed] [Google Scholar]
- 4.Chaudry I, Feng W, Holmstedt C, Turner R, Adams R, Turk AS. Delayed basilar artery recanalization 100 hours after symptom onset. J Neurointerv Surg. 2010;2(4):345–347. doi: 10.1136/jnis.2010.002576. Epub 2010 Jul 23. PMID: 21990643. [DOI] [PubMed] [Google Scholar]
- 5.Möhlenbruch M, Stampfl S, Behrens L, Herweh C, Rohde S, Bendszus M, et al. Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol. 2014;35(5):959–964. doi: 10.3174/ajnr.A3796. Epub 2013 Nov 28. PMID: 24287087; PMCID: PMC7964527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. doi: 10.1056/NEJMoa1411587. Epub 2014 Dec 17. Erratum in: N Engl J Med. 2015 Jan 22;372(4):394. PMID: 25517348. [DOI] [PubMed] [Google Scholar]
- 7.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–1018. doi: 10.1056/NEJMoa1414792. Epub 2015 Feb 11. PMID: 25671797. [DOI] [PubMed] [Google Scholar]
- 8.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. doi: 10.1056/NEJMoa1414905. Epub 2015 Feb 11. PMID: 25671798. [DOI] [PubMed] [Google Scholar]
- 9.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–2306. doi: 10.1056/NEJMoa1503780. Epub 2015 Apr 17. PMID: 25882510. [DOI] [PubMed] [Google Scholar]
- 10.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–2295. doi: 10.1056/NEJMoa1415061. Epub 2015 Apr 17. PMID: 25882376. [DOI] [PubMed] [Google Scholar]
- 11.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020–3035. doi: 10.1161/STR.0000000000000074. Epub 2015 Jun 29. PMID: 26123479. [DOI] [PubMed] [Google Scholar]
- 12.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–718. doi: 10.1056/NEJMoa1713973. Epub 2018 Jan 24. PMID: 29364767; PMCID: PMC6590673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21. doi: 10.1056/NEJMoa1706442. Epub 2017 Nov 11. PMID: 29129157. [DOI] [PubMed] [Google Scholar]
- 14.Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005;76(9):1238–1241. doi: 10.1136/jnnp.2004.049924. PMID: 16107358; PMCID: PMC1739786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cross DT, 3rd, Moran CJ, Akins PT, Angtuaco EE, Diringer MN. Relationship between clot location and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol. 1997;18(7):1221–1228. PMID: 9282845; PMCID: PMC8338023. [PMC free article] [PubMed] [Google Scholar]
- 16.Cross DT, 3rd, Moran CJ, Akins PT, Angtuaco EE, Derdeyn CP, Diringer MN. Collateral circulation and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol. 1998;19(8):1557–1563. PMID: 9763394; PMCID: PMC8338690. [PMC free article] [PubMed] [Google Scholar]
- 17.Mokin M, Sonig A, Sivakanthan S, Ren Z, Elijovich L, Arthur A, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke. 2016;47(3):782–788. doi: 10.1161/STROKEAHA.115.011598. PMID: 26888533. [DOI] [PubMed] [Google Scholar]