ABSTRACT
Background
Takotsubo syndrome is a transient stunned myocardium that typically involves the apical and mid-ventricular segments. A variant, called Inverted Takotsubo, concerns the basal and mid-ventricular segments.
Case summary
We present a ruptured ectopic pregnancy that was responsible for a catecholamine surge, which led to this stress-induced cardiomyopathy. Transthoracic echocardiography showed mid-basal segments akinesia and hypercontractility of the apical segments. Biology has shown mild elevated troponin and NT-pro-BNP levels which led to performing a coronary angiography that showed no angiographic stenosis. A left ventricle angiography evoked the diagnosis of inverted Takotsubo. The patient has received Levosimendan to allow progressive weaning of catecholamine inotropes. The clinical evolution was favorable. Echocardiography performed after 3 weeks, showed ad-integrum restitution of the left ventricular function.
Discussion
Takotsubo syndrome should be evoked whenever a context of physical or psychological stress is present. We underline the usefulness of Levosimendan as a nonadrenergic inotrope in this particular context.
How to cite this article
Ghariani A, Dhiab L, Ferhi F, Abdessalem MAB, Mahdhaoui A, Jazia KB, et al. Inverted Takotsubo Following a Ruptured Ectopic Pregnancy, Treated with Levosimendan. Indian J Crit Care Med 2022;26(2):228–230.
Keywords: Echocardiography, Ectopic pregnancy, Heart failure, Levosimendan
INTRODUCTION
Takotsubo syndrome (TS) is a transient stunned myocardium that typically involves the apical segments. A rare entity that concerns the basal and mid-ventricular segments has been recently described as Inverted Takotsubo. This variant is still not completely understood. A ruptured ectopic pregnancy may be responsible for a catecholamine surge that leads to this stress-induced cardiomyopathy, which can easily be missed by physicians.
CASE PRESENTATION
A 30-year-old female patient was presented to the emergency department with lower abdominal pain. She reported no past medical history, nor or psychiatric history. On admission, the patient was pale, her blood pressure was 80/50 mm Hg, and her heart rate was 120 bpm and with cold and clammy extremities.
A pelvic echography revealed an empty uterine cavity with fluid in the pouch of Douglas. Her hemoglobin level was 4.7 g/dL. A ruptured ectopic pregnancy was suspected. During the laparotomy, about 3 L of blood was suctioned. The left tube was successfully resected. The patient received four units of red blood cells. She was then transferred to the Intensive Care Unit. The hemoglobin level was controlled at 10.6 g/dL.
The evolution was initially favorable, then, after 12 hours, the patient developed a shortness of breath. Physical examination showed tachypnea and tachycardia. Oxygen saturation decreased on room air. Cardiac auscultation was normal but pulmonary auscultation revealed bilaterally dispersed crackles. A chest radiography showed an air space opacification in a batwing distribution. The patient's respiratory state kept on deteriorating which eventually led to her reintubation. Inotropic support was initiated secondary to hemodynamic alteration.
The diagnosis of volume overload secondary to rapid transfusion of blood was initially evoked.
The ECG revealed sinus tachycardia, with a prolonged corrected QT interval at 502 ms.
Transthoracic echocardiography (TTE) revealed a severe left ventricular (LV) systolic dysfunction with mid-basal segments akinesia and hypercontractility of the apical segments. Ejection fraction of the LV was estimated at 25% (Supplementary Video 1).
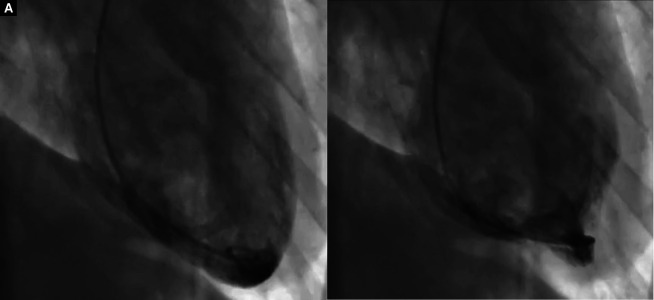
Biology has shown mild elevated troponin and NT-pro-BNP levels which led to perform a coronary angiography. It showed no angiographic stenosis (Supplementary Video 2). A left ventricle angiography evoked the diagnosis of inverted-TS (Fig. 1 and Supplementary Video 3), confirmed by a total inter-TAK diagnosis score of 80 which refers to a probability of 97.3% of a TS.
Figs 1A and B.
Left ventricular angiography that shows mid-basal segments akinesia and hypercontractility of the apical segments
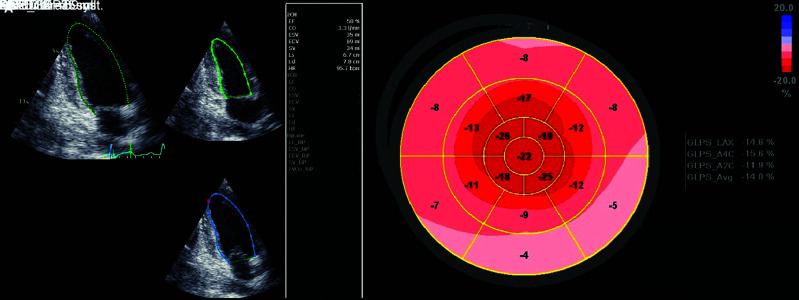
Since the patient was under catecholamine inotropes, we decided to initiate a treatment with Levosimendan. After obtaining oral consent from the patient's husband, a continuous infusion with 0.2 µg/kg/minute for 48 hours was administered to the patient. Weaning of the catecholamine inotropes was possible by the second day of treatment with Levosimendan and the patient was successfully extubated. Clinical evolution was favorable. TTE was performed after 1 week and showed an improvement of the LV systolic function (Fig. 2A). As it is shown in Figure 2B, mild hypokinesia persisted at the basal segments. The patient was discharged from the intensive care unit. Ad-integrum recovery was achieved 3 weeks after this episode where TTE showed good contractility of all LV segments.
Figs 2A and B.
Tranthoracic echocardiography 7 days after admission. (A) It shows an improvement of left ventricular systolic function with ejection fraction estimated at 50%; (B) Global longitudinal strain calculated at −14.0%
DISCUSSION
Our case presents an inverted TS following a ruptured ectopic pregnancy. During the perioperative period, pulmonary edema has been reported after diverse events, including acute lung injury, severe central nervous system trauma (neurogenic pulmonary edema), anaphylaxis, fluid overload, and acute cardiac events. In our case, neither the signs of anaphylaxis nor the evidence of neurogenic pathology or airway obstruction were reported.
A transfusion-related circulatory overload was very likely. TTE was required to help guiding fluid perfusions and especially to exclude unknown valvular heart diseases. Actually, TTE is strongly recommended to assess patients with pulmonary edema. It accurately confirms or excludes cardiogenic-related pulmonary edema in postoperative period and it highlights the type of cardiac dysfunction.1
In our case, TTE revealed mid-basal segments akinesia and hyper-contractility of the apical segments. Thus, Inverted TS was suggested and we performed a coronary angiography with LV angiography to confirm the diagnosis. Risk factors of TS, including neurological and psychiatric disorders, were screened. The patient relatives have infirmed any past medical or psychiatric history.
Stress-induced cardiomyopathy (SIC) mechanism is still not completely elucidated. Many explanations have been evoked but high levels of catecholamines seem to play an important role as triggering factors.2 Nevertheless, high troponin blood levels is disproportional compared to the number of akinetic myocardial segments. Moreover, myocardial adrenergic receptors are unequally distributed. This may explain the variety of SIC presentations in either the mid-ventricular or apical segments.3 Inverted TS is more likely to occur among young female patients. A stress factor is more frequently identified. A larger amount of adrenergic receptors in the basal segments may explain this specific presentation among this population.4
The stress induced by the pain of the ectopic pregnancy may have induced the TS. Moreover, SIC in the perioperative setting has been reported where vasopressors such as norepinephrine were suggested as triggering factors.5
In our case, due to the late diagnosis of inverted TS, catecholamines were initially used to manage the hemodynamic instability. This could have probably exacerbated or prolonged the acute phase of the disease.
Among treatment strategies, we may resort to mechanical support devices. If they are not available, low-dose of Levosimendan infusion may be suggested as a positive inotrope in order to avoid catecholamines.6 In fact, TS would be a good circumstance for the use of this inotrope. We should notice that this suggestion is mainly based on expert opinions that are supported by many case reports.
In our case, the patient's husband was informed as soon as we performed the LV angiography and confirmed the diagnosis of inverted TS. We explained to him the possibility to use Levosimendan, letting him know there were no established evidence for the use of this molecule in this situation. He consented immediately and Levosimendan was introduced allowing progressive weaning of catecholamines. By the second day of treatment, the patient was free of inotropic support. She was successfully extubated and discharged from the intensive care after 1 week.
CONCLUSION
Learning objectives through this case are as follows: First, to identify and diagnose TS in uncommon acute pulmonary edema such as following a hemorrhagic shock. We highlight the usefulness of TTE for the differential diagnosis. Second, to use Levosimendan as an alternative inotrope in this situation, especially when mechanical circulatory support is not immediately available.
Footnotes
Source of support: Nil
Conflict of interest: None
ORCID
Anis Ghariani https://orcid.org/0000-0002-1971-0067
Leila Dhiab https://orcid.org/0000-0003-3677-1053
Fehmi Ferhi https://orcid.org/0000-0003-3435-9321
Mohamed AB Abdessalem https://orcid.org/0000-0002-6966-3318
Abdallah Mahdhaoui https://orcid.org/0000-0001-8454-9946
Khaled B Jazia https://orcid.org/0000-0002-9734-6387
Gouider Jeridi https://orcid.org/0000-0003-1726-8495
SUPPLEMENTARY MATERIAL
All the supplementary material from Supplementary videos 1 to 3 are available online on the website of www.ijccm.org
REFERENCES
- 1.Jasudavisius A, Arellano R, Martin J, McConnell B, Bainbridge D. Revue méthodique de l’échocardiographie transthoracique et transœsophagienne en chirurgie non cardiaque: implications pour la formation en échoguidage au chevet en salle d'opération. Can J Anesth. 2016;63(4):480–487. doi: 10.1007/s12630-015-0524-7. [DOI] [PubMed] [Google Scholar]
- 2.Takashi U, Ken K, Takuzo H, Katsuhiro Y, Yoshihiro T, Ichiro N. Emotional stress induces transient left ventricular hypocontraction in the rat via activation of cardiac adrenoceptors: a possible animal model of “tako-tsubo” cardiomyopathy. Circ J. 2002;66(7):712–713. doi: 10.1253/circj.66.712. [DOI] [PubMed] [Google Scholar]
- 3.Ramaraj R, Movahed MR. Reverse or inverted takotsubo cardiomyopathy (reverse left ventricular apical ballooning syndrome) presents at a younger age compared with the mid or apical variant and is always associated with triggering stress. Congest Hear Fail. 2010;16(6):284–286. doi: 10.1111/j.1751-7133.2010.00188.x. [DOI] [PubMed] [Google Scholar]
- 4.Hurst RT, Askew JW, Reuss CS, Lee RW, Sweeney JP, Fortuin FD, et al. Transient midventricular ballooning syndrome. a new variant. J Am Coll Cardiol. 2006;48(3):579–583. doi: 10.1016/j.jacc.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Bainbridge D, Cheng D. La cardiomyopathie provoquée par le stress dans un contexte périopératoire. Can J Anesth. 2009;56(6):397–401. doi: 10.1007/s12630-009-9085-y. [DOI] [PubMed] [Google Scholar]
- 6.Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, et al. Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016;18(1):8–27. doi: 10.1002/ejhf.424. [DOI] [PubMed] [Google Scholar]