Abstract
Background
Recent studies have established that vaccination plays a significant role in reducing COVID-19-related deaths. Here, we investigated differences in COVID-19 case fatality rates (CFRs) among vaccinated and unvaccinated populations, and analyzed whether the age composition of confirmed cases has a significant effect on the variations in the observed CFRs across these groups.
Methods
The study considered 59,853 confirmed cases and 1,687 deaths from COVID-19, reported between January 1 to October 20, 2021, by the Health Department of Londrina, a city in Southern Brazil. We used Negative Binomial regression models to estimate CFRs according to vaccination status and age range.
Results
There are significant differences between the CFR for fully vaccinated and unvaccinated populations (IRR = 0.596, 95% CI [0.460 - 0.772], P < .001). Vaccinated populations experience fatality rates 40.4% lower than non-vaccinated. In addition, the age composition of confirmed cases explains more than two-thirds of the variation in the CFR between these 2 groups.
Conclusions
Our novel findings reinforce the importance of vaccination as an essential public health measure for reducing COVID-19 fatality rates in all age groups. The results also provide means for accurately assessing differences in CFRs across vaccinated and unvaccinated populations. Such assessment is essential to inform and determine appropriate containment and mitigation interventions in Brazil and elsewhere.
Key Words: COVID-19, Vaccination, Demography, Public health
Background
Since the emergence of COVID-19, the world has taken several measures to contain the spread of the disease. Immunization by vaccination has been 1 of the most important contributions to public health in the past century and is responsible for the sharp decline in vaccine-preventable illness worldwide.1 The steady decline in COVID-19 cases and deaths globally after vaccination has corroborated the importance of this public health measure for ending the COVID-19 pandemic.2 However, its success is contingent upon vaccination attitudes and the design of vaccination policies.3
COVID-19 vaccinations in several countries have been shown to be associated with reduced fatality rates.2 In Israel, mass vaccination reduced the risk of COVID-19-related deaths by 72% from 14 to 20 days after the first dose.4 In the United States, a simulation study projected that COVID-19 vaccination programs would reduce COVID-19 deaths by 69.3%.5 In addition to lowering fatality rates, there is evidence that vaccinations are associated with substantial reductions in symptomatic COVID-19 in older adults in England6 and the risk of COVID-19 hospitalization in Scotland.7
Brazil witnessed a widespread distribution of COVID-19 across all regions and was most severely affected by the pandemic.8 , 9 Almost 200,000 COVID-19 deaths were reported just in 2020.10 The country started vaccination campaigns against COVID-19 on January 17, 2021, prioritizing health workers, older adults (starting at age 85 and gradually vaccinating younger age groups), indigenous populations, and institutionalized individuals.11
Recent studies highlighted that vaccination campaigns were critical in reducing COVID-19 incidence among Brazilian healthcare workers,12 , 13 hospital admissions, and deaths among older adults.11 , 14 Overall, vaccinations have proven their efficacy in preventing COVID-19 fatalities.15 Nonetheless, there is lack of studies on the differences in fatality rates across vaccinated and unvaccinated populations, considering the demographic composition of these subgroups. This information is crucial to the ongoing reassessment of public health interventions and policies.
The demographic composition of cases may help explain differences in fatality rates across populations and how transmission unfolds,16 especially among vaccinated and unvaccinated subgroups. This consideration is essential, given that cases and fatalities caused by COVID-19 are concentrated in older age groups who suffer from underlying medical conditions (comorbidities) and are an expressive part of the fully vaccinated population group.
Here, we investigated the differences in COVID-19 case fatality rates among subjects living in a city in Southern Brazil, taking into account their vaccination status and age categories. We also analyzed whether the age composition of confirmed cases has a significant effect on the variations in fatality rates across vaccinated and unvaccinated populations. We hypothesized that vaccination predicts lower fatality rates, regardless of age range.
Methods
Study design and participants
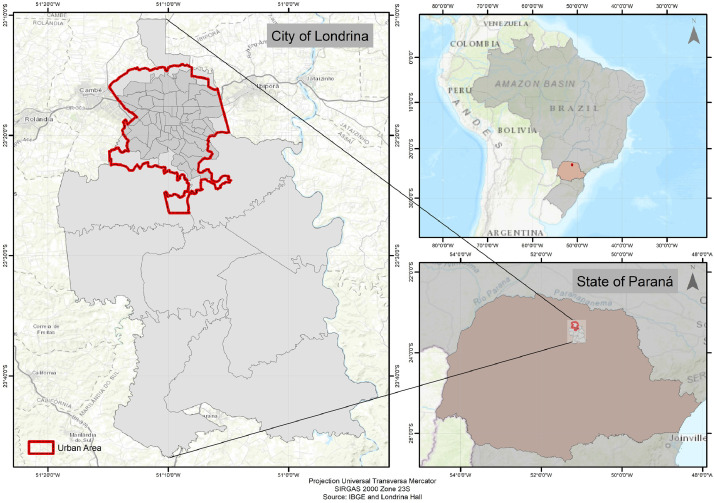
This cohort study draws upon data from the Health Department of Londrina city, the fourth most populous city in Southern Brazil17 (Fig 1 ). The database accrues data on confirmed COVID-19 cases – individuals who tested positive for SARS-CoV-2 – deaths, and vaccination status1 . It is a highly detailed and continuously updated database that allows monitoring the survival trajectory of each individual living in Londrina based on to their demographic characteristics. The main variables of interest in this research were age, sex, vaccination status, and cause of death by COVID-19.
Fig 1.
Geographical delimitation of the studied area – City of Londrina, Paraná – Brazil (2021).
For this investigation, we analyzed baseline data entered into the database between January 1 and October 20, 2021. The initial month coincides with the beginning of the vaccination campaign against COVID-19 in Brazil. COVID-19 case definition followed the World Health Organization (WHO) criteria: a person with a positive Nucleic Acid Amplification Test or a positive SARS-CoV-2 antigen rapid diagnostic tests AND meeting the probable or suspect case definition criteria. In our analysis, death and COVID-19 case counts were cumulative counts up to October 20, 2021. Until this date, Brazilian Health Regulatory Agency (ANVISA) approved the registration of Comirnaty (Pfizer/BioNTech) and Covishield (Oxford/AstraZeneca) vaccines. Coronavac (Sinovac Life Science) and Ad26.COV2.S (Janssen) vaccines obtained an emergency use approval by ANVISA in January and March 2021, respectively.
Although we recognize that each type of vaccine may have different effects on fatality rates, we focused on investigating whether and how subjects with full immunization against COVID-19 differ from those with partial or no vaccination in terms of fatality rates. Therefore, we categorized confirmed cases into 3 distinct groups: unvaccinated, incompletely, and fully vaccinated. We defined incompletely vaccinated as those individuals who received only 1 dose (in the case of 2-dose vaccines) or were less than 14 days after the second dose or after a single-dose vaccine (Janssen). The fully vaccinated category accounts for those who received the second dose (or single-dose vaccine) for 14 days earlier or longer. To overcome the small number of COVID-19 deaths in some age groups, we categorized the age variable into 4 large groups (under 60, 60-69, 70-79, ≥80).
This study was approved by the local Research Ethics Committee (Reference Number: 50261221.3.0000.5231).
Analytical Strategy for decomposing, standardizing, and estimating case fatality rates
The case fatality rate (CFR) is a measure that corresponds to the proportion of individuals with a specific condition who died from that condition during the reference period. In this paper, the CFR metric refers to the ratio of COVID-19 deaths (D) divided by the number of confirmed cases (N): CFR=D/N. We also calculated the CFR as the sum of age-specific CFRs weighted by the proportion of cases in a given age group i. Age-specific CFRs () are given by the following expression: . The proportion of cases in each age group () is given by . Using this notation, the CFR can be written as a weighted average of age-specific CFRs:
-
a)
Decomposition of CFRs
Differences in CFRs could indicate that the risk of dying of COVID-19 among confirmed cases differs between vaccinated and unvaccinated. In addition, differences in CFRs could also imply age compositional differences in confirmed cases, since the risk of dying of COVID-19 is well-documented to increase with age.18 One way to compare demographic variables that belongs to different populations is through decomposition methods. The decomposition of CFRs offers relevant insights for the investigation on whether the age composition of confirmed cases has a significant effect on the variations in fatality rates across vaccinated and unvaccinated populations.
Accordingly, we employed the weighted expression and a mathematical decomposition approach introduced by Kitagawa19 and applied by Dudel et al.18 to separate the difference between 2 CFRs into 2 distinct parts, 1 attributable to the age distribution of cases and the other to age-specific case fatality rates. The method attributes the total difference into these 2 components, leaving no residual. Then, the decomposition approach splits the difference between fully vaccinated and unvaccinated CFRs into:
Where the α-component captures the effect of the age distribution of cases, and the δ-component indicates the part of the difference attributable to age-specific case-fatality. is given by:
while can be calculated as:
Dudel et al.18 provides a step-by-step walk-through of the decomposition and its interpretation that we also employed in this paper.
-
a)
Standardization of CFRs
Despite its value in expressing disease fatality, CFR comparisons among subgroups with different vaccination status needs to be approached with caution. Since CFR is a crude rate, differences in age distributions of confirmed cases and deaths may strongly affect the results. For example, suppose the population is older in a specific vaccination status than another. In that case, the CFR will be higher in the older population, even if the age-specific risk of dying is the same. Here is the relevance of standardization. It is a crucial step to make reliable comparisons between CFRs of populations with different age compositions. One approach to making such a comparison is to adopt the average age distribution of confirmed cases among the 3 vaccination statuses (unvaccinated, incompletely, and fully) as a standard age distribution. The age-standardized case fatality rate (ASCFR) is given by:
Where represents the age-specific CFRs, x refers to the lower limit age of the age group, n is the width of the age intervals, and is the proportion of cases in each age group among the 3 vaccination statuses.
Method for estimating case fatality rates
We employed negative binomial regression models to estimate CFRs for fully, incompletely, or unvaccinated people by age group. The advantage of modeling the number of COVID-19 deaths using a negative binomial model is that it introduces an additional parameter which affords the model more flexibility to deal with overdispersion.20
The underlying assumption of count models for estimating CFRs is the existence of an incidence rate at which the event occurs, which can be multiplied by an exposure time to obtain the number of events that occurred. Therefore, the model includes an additional component, referred to as offset, responsible for controlling the number of COVID-19 deaths by the number of confirmed cases in each selected category. The term offset is included in the logarithmic scale so that it matches with the linking function employed. Thus, the model is given by:
The response variable is the expected number of deaths, and X is a matrix of covariates (vaccination status and age groups). Log(C) is a covariate with a fixed coefficient equal to 1, representing the total number of confirmed cases in the city between the reference period. We adopted the analytical strategy of gradually adding each covariate, starting from a simple model with only age groups (Model 1). Then, we updated the first model with the covariate vaccination status (Model 2). Finally, we presented the last model (Model 3) with age, vaccination status, and an interaction between 2 covariates: age groups and vaccination status. The underlying hypothesis we set to test with this interaction term was whether the differences in fatality rates between vaccinated and unvaccinated varied by age.
The results were presented in the form of Incidence Rate Ratios (IRRs). It is a useful and easy-to-interpret metric that allows to compare the incident rate between 2 different groups, for example, vaccinated and non-vaccinated subjects. We used the Akaike Information Criterion (AIC) to select the best regression model among the candidate models to predict the CFRs. Statistical significance was assessed at a 2-sided P value < .05. All analyses were conducted with R software.21
Results
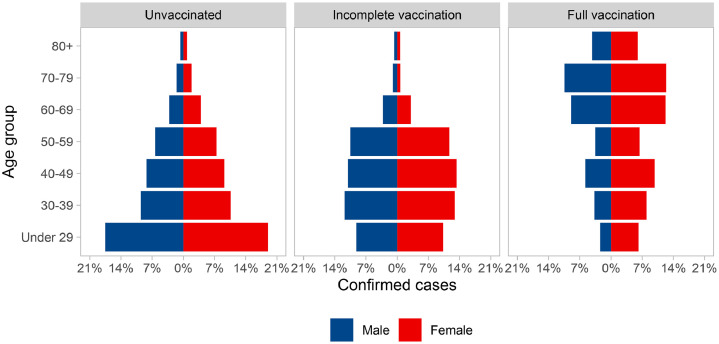
From January 1 to October 20, 2021, the confirmed cases numbered 59,853, of which 2.8% of them (2,238) resulted in death Figure 2. illustrates the distribution of COVID-19 confirmed cases by age, sex, and vaccination status. Note that there is a clear difference in age composition between unvaccinated and vaccinated. Fully vaccinated population has, proportionately, a greater number of older adults. On the other side, the unvaccinated group have a high proportion of individuals under 60 years of age for both sexes, which makes the age structure of this group more rejuvenated than that of the others (Fig 2). These differences have a direct impact on the case fatality rates of the 3 populational subgroups under analysis.
Fig 2.
Distribution of COVID-19 confirmed cases by age, sex, and vaccination status – City of Londrina, Paraná – Brazil (2021).
Table 1 shows the descriptive results for confirmed cases and deaths from COVID-19, according to vaccination status, age, and sex. The values underscore the small number of fatalities for subjects with complete vaccinations, limiting our ability to consider further desegregations or interactions between vaccination status and sex.
Table 1.
COVID-19 deaths, confirmed cases, and case fatality rates (per 1,000) according to vaccination status, age, and sex – City of Londrina, Paraná – Brazil (2021)
| Variable | Unvaccinated |
Incomplete vaccination |
Full vaccination |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | Cases | CFR* | Deaths | Cases | CFR | Deaths | Cases | CFR | |
| Age group | |||||||||
| Under 60 | 498 | 42,431 | 11.74 | 55 | 6,541 | 8.41 | 6 | 2,024 | 2.96 |
| 60-69 | 275 | 3,439 | 79.97 | 39 | 451 | 86.47 | 40 | 939 | 19.76 |
| 70-79 | 272 | 1,624 | 167.49 | 21 | 120 | 175.00 | 114 | 1,011 | 56.32 |
| 80+ | 224 | 723 | 309.82 | 31 | 95 | 326.32 | 112 | 455 | 55.34 |
| Gender | |||||||||
| Male | 724 | 22,708 | 31.88 | 87 | 3,411 | 25.51 | 142 | 1,727 | 70.16 |
| Female | 545 | 25,509 | 21.37 | 59 | 3,796 | 15.54 | 130 | 2,702 | 64.23 |
| Overall | 1,269 | 48,217 | 26.32 | 146 | 7,207 | 20.26 | 272 | 4,429 | 61.41 |
| Age-standardized CFR | 43.51 | 47.33 | 28.7 | ||||||
| Decomposition - Summary | |||||||||
| Case fatality rate (per thousand) among fully vaccinated | 61.41 | ||||||||
| Case fatality rate (per thousand) among unvaccinated | 26.32 | ||||||||
| Difference in CFRs (fully vaccinated minus unvaccinated): | 35.09 | ||||||||
| Proportion of difference explained by age composition of cases (Alpha): | 72% | ||||||||
| Proportion of difference explained by age-specific case fatality (Delta): | 28% | ||||||||
The case fatality rate (CFR) is the ratio between confirmed deaths and confirmed cases.
The overall CFR among fully vaccinated and unvaccinated individuals were 61.41 per thousand and 26.32 per thousand, respectively (Table 1). Subtracting the CFR of fully vaccinated from unvaccinated gives a difference of 35.09. In relative terms, the α-component (proportion of difference explained by age distribution) explains 72% of the difference between these rates. In comparison, the δ-component (proportion of difference explained by age-specific case fatality) only explains 28%. This result indicates that the differences in the age distribution of confirmed cases explain a large part of the variation in CFRs between fully vaccinated and unvaccinated (Table 1).
Overall, the observed CFR points to a possible difference due to the vaccination status. Fully vaccinated subjects have lower fatality rates than incompletely and unvaccinated people in all age groups. Values from age-standardized CFRs reflect the effect the age composition exerts on this measure. About 54% of the 4,429 confirmed cases fully vaccinated are from individuals over 60-years-of-age (Fig 2). Nonetheless, after standardization, fully vaccinated subjects had the lowest overall CFR.
Table 2 depicts the Incidence Rate Ratio (IRR) of negative binomial regression models to predict CFRs with 95% confidence intervals in brackets. An IRR less than 1 indicates that the incident rate is lower in an exposed group compared to an unexposed group. In cases when IRR is equal to 1, the incident rate is equal among those in an exposed group and those in an unexposed group. Finally, if IRR is greater than 1, this indicates that the incident rate is greater in an exposed group compared to an unexposed group. We provide some examples of its interpretation below.
Table 2.
Incidence Rate Ratios (IRRs) of negative binomial regression models (Incidence Rate Ratios – IRRs) – City of Londrina, Paraná – Brazil (2021)
| Dependent variable: deaths |
|||
|---|---|---|---|
| (Model 1) | (Model 2) | (Model 3) | |
| Intercept | 0.009⁎⁎ | 0.010⁎⁎ | 0.012⁎⁎ |
| (0.007 - 0.012) | (0.008 - 0.013) | (0.009 - 0.016) | |
| Age group | |||
| Under 60 (ref) | 1 | 1 | 1 |
| 60-69 | 7.847⁎⁎ | 8.087⁎⁎ | 6.886⁎⁎ |
| (5.358 - 11.485) | (5.932 - 11.023) | (4.723 - 10.036) | |
| 70-79 | 16.603⁎⁎ | 17.848⁎⁎ | 14.279⁎⁎ |
| (11.320 - 24.354) | (13.060 - 24.395) | (9.792 - 20.815) | |
| 80 + | 32.877⁎⁎ | 35.560⁎⁎ | 26.377⁎⁎ |
| (22.496 - 48.020) | (26.084 - 48.494) | (18.013 - 38.605) | |
| Vaccination status | |||
| Unvaccinated (ref) | 1 | 1 | |
| Incomplete vaccination | 0.932 | 0.714 | |
| (0.710 - 1.220) | (0.456 - 1.110) | ||
| Full vaccination | 0.596⁎⁎ | 0.252⁎ | |
| (0.460 - 0.772) | (0.094 - 0.562) | ||
| Interaction between age group and vaccination status | |||
| Under 60:Unvaccinated (ref) | 1 | ||
| 60-69:Incomplete vaccination | 1.476 | ||
| (0.764 - 2.839) | |||
| 70-79:Incomplete vaccination | 1.439 | ||
| (0.694 - 2.926) | |||
| 80+:Incomplete vaccination | 1.457 | ||
| (0.737 - 2.858) | |||
| 60-69:Full vaccination | 2.087 | ||
| (0.810 - 6.172) | |||
| 70-79:Full vaccination | 2.662⁎ | ||
| (1.072 - 7.670) | |||
| 80+:Full vaccination | 3.193⁎ | ||
| (1.283 - 9.217) | |||
| Degrees of Freedom | 20 | 18 | 12 |
| Log Likelihood | -97.03 | -90.35 | -86.57 |
| Akaike Inf. Crit. | 204.06 | 194.70 | 199.15 |
Note. 95% Confidence Intervals of IRRs are in brackets.
P < .05;
P < .01.
The first model investigated differences in fatality rates controlling only for the covariate relative to age groups. Note that “Under 60” is the reference category. Model 1 shows that there are significant differences in fatality rates between age groups. For example, the fatality rate among subjects under 60 is 7.847 times as high as the rate among subjects with 60-69 years-of-age (C.I 95% [5.358 - 11.485], P < .001). Namely, the older the individuals’ age, the higher their fatality rate (Table 2).
The second model incorporates the covariate vaccination status. The model coefficients indicate significant differences in the fatality rate between fully vaccinated and unvaccinated individuals; the CFR for fully vaccinated people is 40.4% lower (IRR = 0.596, 95% CI [0.460 - 0.772], P < .001) than that of non-vaccinated when controlling for age (Table 2).
The third model includes an interaction term between age and vaccination status to enable the analysis as to whether fatality differences between subjects with different vaccination statuses are associated with specific age categories. These differences were age-dependent among older adults with 70-79 or ≥80 years of age at 5% of significance. For example, fully vaccinated subjects older than 80-years-of-age have a fatality rate 20% lower than those unvaccinated with the same age (Table 2).
Table 3 demonstrates the predicted CFR (per thousand) by age groups. The population under 60-years-of age had the lowest fatality rate per thousand confirmed cases in the city, regardless of vaccination status (Table 3). When analyzing the ratio between unvaccinated and fully vaccinated subgroups, individuals under 60-years-of-age had the most significant difference in predicted CFR. In this group, the fatality risk experienced by an unvaccinated person is 7.1-fold higher than in a fully vaccinated subject. Overall, these findings highlight the premise that vaccinated subjects have lower fatality risks than unvaccinated subjects in all age groups.
Table 3.
Predicted Case Fatality rates (per thousand) according to vaccination status – City of Londrina, Paraná – Brazil (2021)
| Predicted CFR* |
Ratio† | |||
|---|---|---|---|---|
| CFR | CI 95% | |||
| Unvaccinated | ||||
| Under 60 | 9.17 | 11.89 | 15.41 | 7.1 |
| 60-69 | 62.40 | 81.85 | 107.36 | 2.2 |
| 70-79 | 129.33 | 169.72 | 222.73 | 1.5 |
| 80+ | 237.55 | 313.52 | 413.79 | 1.3 |
| Incomplete vaccination | ||||
| Under 60 | 5.93 | 8.49 | 12.16 | 4.6 |
| 60-69 | 57.94 | 86.28 | 128.49 | 2.0 |
| 70-79 | 106.39 | 174.43 | 285.97 | 1.3 |
| 80+ | 212.53 | 326.29 | 500.94 | 1.1 |
| Full vaccination | ||||
| Under 60 | 1.30 | 2.99 | 6.91 | - |
| 60-69 | 28.98 | 43.01 | 63.83 | - |
| 70-79 | 83.79 | 113.74 | 154.40 | - |
| 80+ | 185.46 | 252.00 | 342.42 | - |
The case fatality rate (CFR) is the ratio between confirmed deaths and confirmed cases.
Ratio of predicted CFR (Model 3) where age groups of full vaccination are the denominator.
Discussion
This novel study investigated differences in COVID-19 case fatality rates among individuals according to their vaccination status and whether these differences were associated with specific age categories. Regression analysis revealed that COVID-19 vaccination was significantly associated with reduced case fatality rates in all age groups. We also demonstrated that the age composition of confirmed cases significantly affected the variations in fatality rates across vaccinated and unvaccinated populations. Since these groups have different age compositions, it is vital to assess underlying differences in the age distribution of cases with accurate methodologies to enable the most appropriate health response.
Our results strengthen the evidence that vaccination is critical for preventing deaths among infected people. Such evidence is in agreement with previous works that also investigated the impact of COVID-19 vaccination in different geographic regions. Liang et al.2 used observational data from 90 countries and showed that the average CFR reduction approximated 7.6% for a 10% increase in vaccine coverage. In Europe and Israel, vaccination efficacy in terms of protection against deaths was 72%.22 In the United States, COVID-19 vaccination saved an estimated 240,797 lives (95% CI, [200,665-281 230]) in the course of the pandemic23 and was associated with reductions in COVID-19 cases and deaths among older adults.24 Overall, the currently available COVID-19 vaccines effectively prevent severe complications and deaths from COVID-19 in all age groups.25
Our results shed new information on the topic by demonstrating the impact of COVID-19 vaccination on fatality rates, considering the differences in the age composition of infected cases. We posit that age composition matters and is a potential explanation for differences in CFRs among vaccinated and unvaccinated populations. For this reason, we reinforce the importance of applying accurate methodologies for reliable comparisons between these groups when evaluating the impact of COVID-19 vaccination. This consideration is crucial for public health measures. Ignoring the effects of age composition on CFRs can generate misconceptions about the actual effectiveness of vaccination in preventing fatal cases, thwart ongoing pandemic mitigation strategies, and weaken local-level public health responses to protect the most vulnerable groups from the adverse consequences of COVID-19.
We believe that our study is inherently important in that it corroborates the importance of adopting public health policies to mitigate the pandemic that is rooted on sound analysis of vaccine efficacy. However, we concede that our study has also some methodological limitations. The first one relates to the primary measure employed in this research. The CFR might be underestimated because of the time-lag bias associated with local COVID-19 case diagnosis and reports. In addition, the CFR is also influenced by the underreporting of confirmed COVID-19 cases and deaths. We could not also assess other confounding variables such as comorbidities, health behaviors, and educational attainment through the database and incorporate them into the final model. Such information is still unavailable in the database. Despite these limitations, the CFR provides pertinent insight into disease outcomes between vaccinated and unvaccinated populations, and how they are modified by age.
Conclusion
This paper reinforces the importance of vaccination as an essential public health measure for reducing COVID-19 fatality rates. Our work also informs and expands the existing literature by accurately assessing differences in CFRs across vaccinated and unvaccinated populations. Such assessment is crucial to inform and determine appropriate containment and mitigation interventions, such as physical distancing, wearing well-fitting masks, and avoiding crowds.26 These actions can drive down fatality rates as vaccination rates increase. In conclusion, we offer accurate methodologies to assess the impact of vaccination on the COVID-19 pandemic, considering the population's age composition. Such evidence can provide important insights to monitor the spread of COVID-19 in cities in Brazil and around the world.
Acknowledgments
We acknowledge CAPES for the financial support (scholarship), the City Health Secretary of Londrina for providing the data, and the “Núcleo Interdisciplinar de Gestão Pública (NIGEP) – UEL” coordinated by Professor Vera Suguihiro and Professor Saulo Fabiano Amâncio Vieira.
Footnotes
Conflicts of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding/support: This work was supported by CAPES – Coordination for the Improvement of Higher Education Personnel [Financing code 001].
The database used in the paper is not nationally scrutinized; it provides information on the population living in the municipality of Londrina, Paraná - Brazil. The city's Health Department is primarily responsible for maintaining and managing the database. It is not publicly available (only upon request) because it contains personal information about citizens who have tested positive for COVID-19.
References
- 1.Pollard AJ, Bijker EM. A guide to vaccinology: from basic principles to new developments. Nat Rev Immunol. 2021;21:83–100. doi: 10.1038/s41577-020-00479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang LL, Kuo HS, Ho HJ, Wu CY. COVID-19 vaccinations are associated with reduced fatality rates: evidence from cross-county quasi-experiments. J Glob Health. 2021;11:1–9. doi: 10.7189/jogh.11.05019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paul KT, Eberl JM, Partheymüller J. Policy-relevant attitudes toward COVID-19 vaccination: associations with demography, health risk, and social and political factors. Front Public Heal. 2021;9:1–8. doi: 10.3389/fpubh.2021.671896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384:1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clin Infect Dis. 2021;2019:1–8. doi: 10.1093/cid/ciab079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernal JL, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373 doi: 10.1136/bmj.n1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vasileiou E, Simpson CR, Robertson C, et al. Effectiveness of first dose of COVID-19 vaccines against hospital admissions in scotland: National Prospective Cohort Study of 5.4 million people. SSRN Electron J. 2021;2:1–11. [Google Scholar]
- 8.Ranzani OT, Bastos LSL, Gelli JGM, et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9:407–418. doi: 10.1016/S2213-2600(20)30560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castro MC, Kim S, Barberia L, et al. Spatiotemporal pattern of COVID-19 spread in Brazil. Science (80-) 2021;372:821–826. doi: 10.1126/science.abh1558. [DOI] [PubMed] [Google Scholar]
- 10.Zimmermann IR, Sanchez MN, Frio GS, et al. Trends in COVID-19 case-fatality rates in Brazilian public hospitals: a longitudinal cohort of 398,063 hospital admissions from 1st March to 3rd October 2020. PLoS One. 2021;16:1–15. doi: 10.1371/journal.pone.0254633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Victora C, Castro MC, Gurzenda S, Medeiros AC, França GVA, Barros AJD. Estimating the early impact of vaccination against COVID-19 on deaths among elderly people in Brazil: Analyses of routinely-collected data on vaccine coverage and mortality. EClinicalMedicine. 2021;38 doi: 10.1016/j.eclinm.2021.101036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Toniasso SCC, Fernandes FS, Joveleviths D, et al. Reduction in COVID-19 prevalence in healthcare workers in a university hospital in southern Brazil after the start of vaccination. Int J Infect Dis. 2021;109:283–285. doi: 10.1016/j.ijid.2021.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hitchings MDT, Ranzani OT, Torres MSS, et al. Effectiveness of CoronaVac among healthcare workers in the setting of high SARS-CoV-2 Gamma variant transmission in Manaus, Brazil: a test-negative case-control study. Lancet Reg Heal - Am. 2021;1:1–9. doi: 10.1016/j.lana.2021.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alencar CH, Cavalcanti LP de G, de Almeida MM, et al. High effectiveness of sars-cov-2 vaccines in reducing covid-19-related deaths in over 75-year-olds, Ceará State, Brazil. Trop Med Infect Dis. 2021;6:4–9. doi: 10.3390/tropicalmed6030129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Villela DAM, de Noronha TG, Bastos LS, et al. Effectiveness of mass vaccination in Brazil against severe COVID-19 cases. MedRxiv. 2021;1:1–25. [Google Scholar]
- 16.Dowd JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci U S A. 2020;117:9696–9698. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Instituto Brasileiro de Geografia e Estatística. Estimated population of Londrina, Parana - Brazil (2021). IBGE Cid 2021:1. Accessed April 5, 2022. https://cidades.ibge.gov.br/brasil/pr/londrina/panorama.
- 18.Dudel C, Riffe T, Acosta E, van Raalte A, Strozza C, Myrskylä M. Monitoring trends and differences in COVID-19 case-fatality rates using decomposition methods: Contributions of age structure and age-specific fatality. PLoS One. 2020;15:1–11. doi: 10.1371/journal.pone.0238904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kitagawa EM. Components of a difference between two rates. J Am Stat Assoc. 1955;50:1168–1194. [Google Scholar]
- 20.Roback P, Legler J. Chapman and Hall/CRC Press; New York: 2021. Poisson Regression. Beyond Mult. Linear Regres. Appl. Gen. Linear Model. Multilevel Model. R. [Google Scholar]
- 21.R Core Team. R: A Language and Environment for Statistical Computing 2021.
- 22.Jabłońska K, Aballéa S, Toumi M. The real-life impact of vaccination on COVID-19 mortality in Europe and Israel. Public Health. 2021;198:230–237. doi: 10.1016/j.puhe.2021.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vilches TN, Moghadas SM, Sah P, et al. Estimating COVID-19 infections, hospitalizations, and deaths following the US vaccination campaigns during the pandemic. JAMA Netw. Open. 2022;797:2020–2023. doi: 10.1001/jamanetworkopen.2021.42725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McNamara LA, Wiegand RE, Burker RM, et al. Estimating the early impact of the US COVID-19 vaccination programme on COVID-19 cases, emergency department visits, hospital admissions, and deaths among adults aged 65 years and older: an ecological analysis of national surveillance data. Lancet. 2022;399(10320):152–160. doi: 10.1016/S0140-6736(21)02226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henry DA, Jones MA, Stehlik P, Glasziou PP. Effectiveness of COVID-19 vaccines: findings from real world studies. Med. J. Aust. 2021;215:149–151. doi: 10.5694/mja2.51182. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization, COVID-19 advice for the public: Getting vaccinated,” 2021. [Online]. Accessed April 5, 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice.