Abstract
Background
When assessing patients with depressive and anxiety disorders in psychiatric clinical practice, it is common to encounter children and adolescents who have experienced abuse and victimization. To date, it has been clarified that experiences of “childhood abuse” and “childhood victimization” lead to “neuroticism”, and that neuroticism leads to “adult depressive symptoms”. In this study, we analyzed how these four factors are interrelated.
Subjects and Methods
The following self-administered questionnaire surveys were conducted in 576 adult volunteers: Patient Health Questionnaire-9, Eysenck Personality Questionnaire-revised shortened version, Child Abuse and Trauma Scale, and Childhood Victimization Rating Scale. For statistical analysis, Pearson correlation coefficient analysis, t-test, multiple regression analysis, and covariance structure analysis (path analysis) were performed.
Results
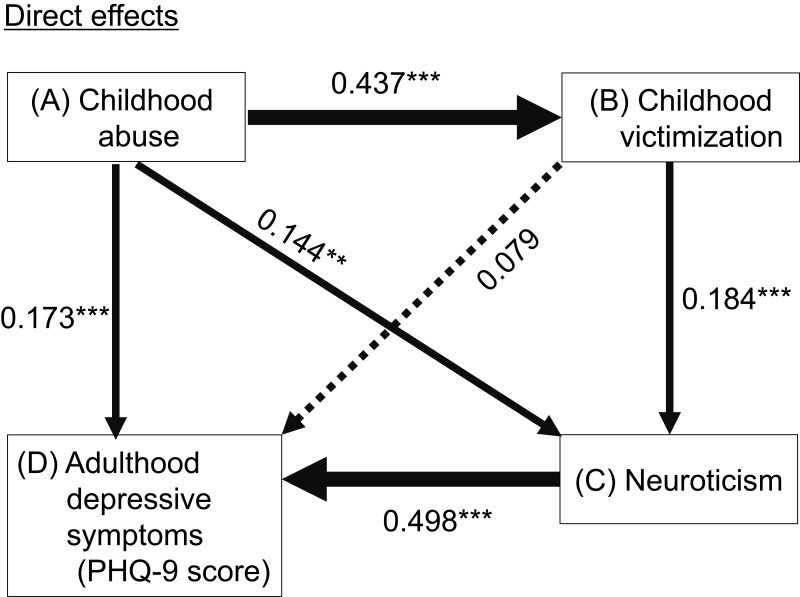
Path analysis showed that the indirect effects of childhood abuse and childhood victimization on depressive symptoms through neuroticism were statistically significant. In addition, the indirect effects of childhood abuse on neuroticism through childhood victimization were statistically significant. Finally, the indirect effects of childhood abuse on depressive symptoms through the combined paths of childhood victimization and neuroticism were statistically significant.
Conclusion
Our results suggest that “childhood abuse (A)” induces changes in the personality trait of “neuroticism (C)” with “childhood victimization (B)” as a mediator, and that these adversities affect the expression of “depressive symptoms in adulthood (D)” through “neuroticism (C)” as a mediator. In other words, to our knowledge, this is the first study to clarify that these four factors are not only individually associated with each other but also cause a chain reaction of A to B to C to D.
Keywords: childhood abuse, childhood victimization, neuroticism, depressive symptoms, path analysis
Introduction
In psychiatric clinical practice, it is common to find that patients with depressive or anxiety disorders have experienced abuse or victimization in their childhood or adolescence, during their assessment. Having the experience of abuse or victimization, which often involves repeated experiences in the mid-to-long term, often leads to Type II trauma, and may cause the loss of a fundamental sense of trust and self-esteem, resulting in long-term mental health problems, including complex post-traumatic stress disorder.1–3 In our many years of experience in child Psychiatry, we have encountered many cases in which children were brought to child psychiatry due to serious abuse or victimization, and developed depressive and anxiety symptoms as they became adults.4–9 However, at present, the mechanism connecting abuse and victimization experienced in childhood with psychiatric symptoms including depressive and anxiety symptoms that develop in adulthood, remain unclear. Clarifying this psychological mechanism will confirm that childhood abuse and victimization can have long-term negative effects in victims. Identification of the risks of such long-term negative effects will help towards the establishment of prevention methods for child abuse and bullying. Furthermore, effective intervention support for children who have experienced child abuse and victimization will enable the prevention of future psychological manifestations.
The involvement of childhood stress in the development of depressive symptoms and depressive disorders in adulthood has been widely reported. In addition, childhood stress has been widely acknowledged as a risk factor for the increased severity, resistance to treatment, and prolongation of depressive symptoms and depressive disorders in adulthood.10–12 However, as there is a long time interval between the experience of childhood stress and the onset of depressive symptoms in adulthood, childhood stress is unlikely to have a direct effect on depressive symptoms in adulthood, but is more likely to involve mediators and moderators occurring during this time interval.13 Our previous studies have shown that experiences of childhood abuse affect the onset of depression, the expression of depressive symptoms, and well-being in adulthood, and the effects are mediated by several personality traits.9,14–23 These personality traits include affective temperament, neuroticism, interpersonal sensitivity, self-esteem, and trait anxiety.9,14–23
Among these personality traits, neuroticism has been identified as a forward-looking risk factor for the development of depression.24–26 For this reason, the American Psychiatric Association’s most recent operative diagnostic criteria, Diagnostic and Statistical Manual of Mental Disorders, fifth edition, specifies that neuroticism is a risk factor for major depressive disorders.27 In a study performing structural equation modeling of adult twins, Kendler and Gardner reported that the childhood experience of sexual abuse and neuroticism are two factors that contribute to the severity of clinical depression and symptoms of anxiety and depression.25,26 However, in these studies, the authors did not clarify whether neuroticism was a mediator or not.25,26 We previously demonstrated that the experience of childhood abuse affects the development of depressive symptoms in adulthood through the mediator of neuroticism.18
On the other hand, several studies have shown that the experience of victimization in childhood and adolescence significantly increases the risks of developing depressive and anxiety disorders, as well as suicide-associated problems in adulthood.28–37 Factors mediating the association between bullying and psychiatric disorders have not been reported previously. However, our recent study suggested that the experience of bullying victimization in childhood affects the development of depressive symptoms and major depressive disorders in adulthood, through neuroticism as a mediating factor.38 Therefore, considering our findings of childhood abuse mentioned above, neuroticism may be a common mediator of the effects of overall stress during childhood on the development of depressive symptoms in adulthood.18,22,38
Regarding abuse and victimization, a large-scale cohort study reported that children who experience maltreatment are more likely to be bullied than children who do not.29 Furthermore, this previous study showed the increased risk of mental health problems in young adults, such as anxiety, depression, and self-harm, or suicidality in children who were bullied by their peers, regardless of whether they had a history of being maltreated by adults.29 There are multiple reports that children with a history of abuse at home are more likely to experience victimization in childhood.39,40 The interrelationships among childhood abuse, childhood victimization, and personality traits in the prediction of depressive symptoms have been investigated by several previous studies, and a theoretical basis for personality traits as mediators between childhood adverse stress and depressive symptoms has been proposed.9,15–23,38 Of note, some previous studies suggested that personality traits, including neuroticism, might be mediators between abuse and victimization in childhood and adulthood depressive symptoms in the general adult population.18,22,38 Based on these previous studies and on theory, we hypothesized that the experience of childhood abuse affects neuroticism through the mediating effect of victimization, and these adversities further affect the development of depressive symptoms through the common mediating effect of neuroticism, one after another in a chain reaction. The definitions of these variables in the present study were as follows. The experience of childhood abuse included the following three types of negative experiences in childhood: punishment (unreasonable and severe punishment), sexual abuse (traumatic sexual experiences and witnesses of the sexual mistreatment of other family members), and neglect/negative home atmosphere (physical and emotional neglect, loneliness and lack of attachment, and negative home environment, including parental substance abuse and fighting).41 The definition of “childhood bullying” by Olweus, D., as “repeated physical and psychological acts by a supposedly strong student (or group of students) against a supposedly weak student” is often used internationally.42 However, this study investigates general childhood harm caused by negative behavior, not childhood bullying. Childhood victimization in this study does not necessarily ask whether it is intentional or not, or whether there is a power imbalance. Childhood victimization in our study includes three types of victimization: physical, verbal, and relational victimization by school and/or community members.38 Neuroticism is a tendency for unstable mood and readily feeling miserable, worried, hurt, fed up, nervous, tensed, lonely, guilty, and irritable.43 Depressive symptoms are based on the diagnostic criteria of a major depressive episode of the American Psychiatric Association and composed of nine items of the criteria.44 We used covariance structure analysis (path analysis) in adult volunteers from the community for the verification of our hypothesis, ie, to investigate the interrelationship and mediating effects of the following four factors: childhood abuse experience, childhood victimization experience, neuroticism, and adulthood depressive symptoms.
Subjects and Methods
Subjects
This study was conducted on 576 adult volunteers from the community, who provided their consent and valid responses to the self-administered questionnaires, which were paper-based surveys. One questionnaire was for demographic information, and the four other questionnaires were on childhood abuse, childhood victimization, neuroticism, and depressive symptoms. The volunteers completed all questionnaires at the same time. Between April 2017 and April 2018, questionnaires and the details of this study were distributed to 1237 adults by convenience sampling through our acquaintances at Tokyo Medical University. A total of 597 (48.3%) adult volunteers participated in this study. All participants provided informed consent to participate in this study. After excluding those with missing data, 576 of the volunteers (249 men and 327 women, mean age: 41.6 ± 12.0 years) were analyzed. The inclusion criteria were (a) being 20 years or older, and (b) being capable of agreeing to study participation. The exclusion criteria were (a) having any severe physical illness, and (b) having any organic brain illness. Subjects were informed that participation in this study was not compulsory but entirely voluntary, that their choice not to participate would not create any disadvantage, that the collected information would be anonymized to be personally unidentifiable, and that the information would not be leaked externally. This study was part of a larger study, which investigated stress, personality traits, affective symptoms, sleep, quality of life, well-being, resilience, etc., in adult volunteers by a questionnaire survey.38,45 The study was performed in accordance with the 1964 Declaration of Helsinki (amended in Fortaleza in 2013), with the approval of the Institutional Review Committee of Tokyo Medical University (study approval number: SH3502).
Questionnaires
Patient Health Questionnaire-9 (PHQ-9)
The Japanese version of PHQ-9 is a self-administered rating scale for measuring the severity of depressive symptoms.44,46 The scale consists of 9 question items on a 4-point Likert scale (0 = not at all, 1 = for several days, 2 = more than half the days, and 3 = nearly every day), and the total score of the 9 items was calculated as the PHQ-9 summary score (min: 0 points – max: 27 points). A higher score indicates a higher severity of depressive symptoms. In the present study, Cronbach’s α coefficient calculated for the total score of this scale was 0.854, indicating very high internal consistency. Although major and other depressive episodes can be evaluated by PHQ-9, this study used the PHQ-9 summary score, namely, the severity of depressive symptoms, to analyze the linear association of childhood abuse, victimization, and neuroticism with depressive symptoms in adult volunteers, including many healthy individuals.
Neuroticism Subscale of Eysenck Personality Questionnaire-Revised (EPQ-R) (Short Version)
Neuroticism was measured using the subscale of the short version of the self-administered EPQ-R.43 This is a yes-no questionnaire consisting of 12 items (no = 0, yes = 1). A high score indicates that subjects readily have feelings of anxiety, worry, and irritation. The total score of the 12 items was used for the analysis, as the neuroticism score. Cronbach’s α coefficient calculated for this subscale was 0.859, indicating very high internal consistency.
Child Abuse and Trauma Scale (CATS)
CATS is a self-administered questionnaire for retrospectively evaluating a child’s (up to 18-years old) abusive growth environment.41 The Japanese version was translated and validated by Tanabe et al.47 The Japanese version of CATS consists of 38 items in total, and each item was evaluated on a 5-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = very often, and 4 = always). The total score was used for analysis. In the present study, Cronbach’s α coefficient calculated for the total score of this scale was 0.931, indicating very high internal consistency.
Childhood Victimization Rating Scale
As in our previous study,38 this study used a revised version of the scale developed by the National Institute for Educational Policy Research in Japan, which is a scale to evaluate bullying victimization. In our previous study, scores of the victimization scale significantly correlated with neuroticism, the presence of depression, and the severity of depressive symptoms.38 This scale is a self-report questionnaire that asks about the frequency and degree of victimization in the community and school during childhood, on a 5-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = always). The total score of the 5 items was used as the victimization score. The higher the score, the higher the degree of victimization. In the present study, Cronbach’s α coefficient calculated for this scale was 0.862, indicating very high internal consistency. Exploratory factor analysis indicated that this victimization scale had a one-factor structure. Confirmatory factor analysis demonstrated that the 5-item scale had a poor model fit, but the 3-item scale (item numbers 1, 2, and 3 of Appendices 1 and 2) had a very good model fit. (Appendices 1 and 2 show the Japanese and English versions of the scale, respectively.)
Data Analysis
For comparison of demographic information and data from the questionnaire, IBM SPSS Statistics version 26 (IBM, Armonk, NY, USA) was used to either apply the Pearson correlation coefficient or perform the t-test. Furthermore, multiple regression analysis was performed by the forced entry method, using PHQ-9 as a dependent variable and demographic information and each score of the questionnaire (age, sex, education years, current marital status, living alone, presence of offspring, childhood abuse, victimization, and neuroticism) as independent variables.
To analyze the association among factors using path analysis, a model was built in which the experience of being abused at home during childhood is linked with the experience of victimization at school or in the community during childhood, and these childhood experiences aggravate neuroticism and further influence the severity of depressive symptoms in adulthood directly or indirectly. Path analysis was performed by covariance structure analysis with robust maximum likelihood estimation (Mplus version 8.4, Muthén & Muthén, Los Angeles, CA, USA). Two goodness-of-fit indices, namely, the Comparative Fit Index (CFI) and Root Mean Square Error Approximation (RMSEA), were used as goodness-of-fit indices for comprehensive judgment. All coefficients in the covariance structure analysis were standardized. Both direct and indirect effects were analyzed.
Imputation methods were not used for the missing data in this study. Participants with missing data for the four questionnaires of childhood abuse, childhood victimization, neuroticism, and depressive symptoms were excluded from the study, because it was not possible to analyze these subjects in the path analysis.
Results
Demographic Information and CATS, PHQ-9, EPQ-R Neuroticism, and Victimization Scores
Table 1 shows the demographic information, and CATS, PHQ-9, EPQ-R neuroticism, and victimization scores of the 576 subjects. Table 2 shows the association of these parameters with depressive symptoms expressed as PHQ-9 scores; the associations were analyzed using Pearson’s correlation coefficient (r) or the t-test. The PHQ-9 summary score measuring depressive symptoms was higher in women, unmarried individuals, those without children, and those living alone. Age, years of education, employment status, and the presence of physical diseases were not associated with depressive symptoms. The CATS total score, EPQ-R neuroticism score, and victimization score were significantly positively correlated with the severity of depressive symptoms. A p-value of less than 0.05 was considered to be statistically significant.
Table 1.
Background Characteristics, and PHQ-9, CATS, Victimization, and Neuroticism Scores of the Subjects
| Characteristic or Measure | Number or Mean ± SD |
|---|---|
| Age (years) | 41.6 ± 12.0 |
| Sex (men: women) | 249: 327 |
| Years of education | 14.6 ± 1.8 |
| Employment status (employed: non-employed) | 562: 10 |
| Current marital status (married: single) | 377: 194 |
| Presence of offspring (yes: no) | 358: 214 |
| Living alone (yes: no) | 114: 453 |
| Comorbid physical disease (yes: no) | 111: 465 |
| PHQ-9 summary score | 4.1 ± 4.3 |
| CATS total score | 27.3 ± 20.0 |
| EPQ-R neuroticism score | 4.4 ± 3.5 |
| Victimization score | 2.4 ± 3.3 |
Notes: Data are presented as means (Standard Deviation, SD) or numbers.
Abbreviations: PHQ-9, Patient Health Questionnaire-9; CATS, Child Abuse and Trauma Scale; EPQ-R, Eysenck Personality Questionnaire revised.
Table 2.
Background Characteristics, PHQ-9, CATS, Victimization, and Neuroticism Scores of the Subjects, and Their Correlation with and Effects on PHQ-9 Summary Score
| Characteristic or Measure | Correlation with PHQ-9 Summary Score (r) or Effect on PHQ-9 Summary Score (Mean ± SD, t-test) |
|---|---|
| Age (years) | r = –0.032, p = 0.448 |
| Sex (men: women) | Men (3.5 ± 4.1) vs women (4.5 ± 4.3), p = 0.005 (t-test) |
| Years of education | r = –0.073, p = 0.078 |
| Employment status (employed: non-employed) | Employed (4.0 ± 4.2) vs non-employed (3.1 ± 4.9), p = 0.48 (t-test) |
| Current marital status (married: single) | Married (3.5 ± 3.9) vs single (5.2 ± 4.7), p < 0.000 (t-test) |
| Presence of offspring (yes: no) | Yes (3.8 ± 4.1) vs no (4.6 ± 4.5), p = 0.036 (t-test) |
| Living alone (yes: no) | Yes (5.1 ± 4.7) vs no (3.8 ± 4.1), p = 0.011 (t-test) |
| Comorbid physical disease (yes: no) | Yes (4.2 ± 4.6) vs no (4.0 ± 4.2), p = 0.651 (t-test) |
| CATS total score | r = 0.319, p < 0.001 |
| EPQ-R neuroticism score | r = 0.557, p < 0.001 |
| Victimization score | r = 0.277, p < 0.001 |
Notes: Data are presented as means (Standard Deviation, SD) or numbers. r = Pearson’s correlation coefficient.
Abbreviations: PHQ-9, Patient Health Questionnaire-9; CATS, Child Abuse and Trauma Scale; EPQ-R, Eysenck Personality Questionnaire revised.
Multiple Regression Analysis of PHQ-9 Summary Score
Table 3 shows the results of multiple regression analysis of the PHQ-9 summary scores. Multiple regression analysis was performed to determine which of the factors, including childhood abuse, victimization, and neuroticism, had a significant effect on depressive symptoms. In addition to the three factors of CATS total score, EPQ-R neuroticism score, and victimization score, six other factors shown to be associated with depressive symptoms in Table 1 (namely, age, sex, years of education, living alone, presence of children, and marital status) were added as independent variables. The analysis was conducted by the forced entry method. Among the factors, the following four were significantly associated with depressive symptoms: EPQ-R neuroticism score, CATS total score, victimization score, and age. Associations between the other factors and depressive symptoms were not statistically significant. The adjusted R2 was 0.36, ie, this model explains 36% of the variation in depressive symptoms. Multicollinearity was denied. A p-value of less than 0.05 was considered to be statistically significant.
Table 3.
Results of Multiple Regression Analysis of PHQ-9 Summary Scores
| Independent Variable | Beta | p-value | VIF |
|---|---|---|---|
| EPQ-R neuroticism score | 0.494 | < 0.001 | 1.153 |
| CATS total score | 0.153 | < 0.001 | 1.368 |
| Age | 0.114 | 0.010 | 1.703 |
| Victimization score | 0.086 | 0.029 | 1.336 |
| Women | 0.053 | 0.139 | 1.120 |
| Living alone | 0.019 | 0.658 | 1.586 |
| Education years | –0.011 | 0.777 | 1.423 |
| Presence of offspring | –0.048 | 0.320 | 2.012 |
| Married | –0.080 | 0.085 | 1.879 |
Notes: Beta, standardized partial regression coefficient; VIF, variance inflation factor. Dependent variable: PHQ-9 summary score. Nine independent variables: age, sex (men = 0, women = 1), marital status (single = 0, married = 1), presence of offspring (no = 0, yes = 1), living alone (no = 0, yes = 1), education years, CATS total score, EPQ-R neuroticism score, victimization score. Adjusted R2 = 0.36; F = 35.962; p < 0.001.
Path Analysis
Figure 1 and Table 4 show the results of path analysis using the severity of depressive symptoms as the dependent variable. The goodness-of-fit of the path model was CFI = 1.000 and RMSEA = 0.000, which indicates a good fit. The path from childhood abuse to childhood victimization, the path from childhood abuse to neuroticism, and the path from childhood abuse to the severity of depressive symptoms (PHQ-9 score) were all statistically significant. Whereas the path of the direct effect from childhood victimization to depressive symptoms was not significant, the path from childhood victimization to neuroticism and the path from neuroticism to the severity of depressive symptoms were statistically significant. This model explains 35.4% of the variation in the severity of depressive symptoms in adult volunteers.
Figure 1.
Results of the direct effects demonstrated by path analysis between the factors (“childhood abuse”, “childhood victimization”, “neuroticism” and “depressive symptoms in adulthood”) in 576 adult volunteers from the community. The severity of depressive symptoms evaluated by PHQ-9 was the dependent variable. The arrows with solid lines represent statistically significant paths, and the arrow with a broken line shows the nonsignificant path. The numbers beside the arrows show the standardized path coefficients. R2 = 0.354, **p < 0.01, ***p < 0.001.
Table 4.
Standardized Path Coefficients Between Each Variable, and 95% Confidence Intervals in the Path Model: Demonstrating Direct and Indirect Effects
| Direct Effect on | |||
|---|---|---|---|
| From | Victimization | Neuroticism | Depressive Symptoms |
| Childhood abuse | 0.437*** (0.332, 0.541) | 0.144** (0.045, 0.242) | 0.173*** (0.089, 0.256) |
| Victimization | 0.184*** (0.088, 0.280) | 0. 079 (–0.028, 0.186) | |
| Neuroticism | 0.498*** (0.428, 0.568) | ||
| Indirect effect on | |||
| Via | Neuroticism | Depressive Symptoms | |
| Childhood abuse | Victimization | 0.080*** (0.037, 0.124) | 0.034 (–0.013, 0.082) |
| Neuroticism | 0.072** (0.022, 0.121) | ||
| Victimization + neuroticism | 0.040** (0.017, 0.063) | ||
| Victimization | Neuroticism | 0.092*** (0.042, 0.141) | |
Notes: **p < 0.01, ***p < 0.001. Numbers in parentheses indicate lower limits and upper limits of 95% confidence intervals.
Table 4 shows the results of the indirect effects of path analysis. The effect of childhood abuse on neuroticism through the mediating effect of victimization in childhood and the effect of childhood abuse on depressive symptoms in adulthood through the mediating effect of neuroticism were statistically significant. The effect of childhood abuse on depressive symptoms in adulthood through the mediating effects of victimization in childhood and neuroticism was statistically significant. The effect of victimization in childhood on depressive symptoms in adulthood through the mediating effect of neuroticism was also statistically significant. On the other hand, the effect of childhood abuse on depressive symptoms through the mediating effect of victimization in childhood was not statistically significant. A p-value of less than 0.05 was considered to be statistically significant.
The overall effects on depressive symptoms were 0.319 for childhood abuse (p < 0.001) and 0.171 for childhood victimization (p = 0.002). The percentage of mediation in the overall association between childhood abuse and depressive symptoms was 35.1% for the mediation by neuroticism, and 23.2% for the mediation by victimization. The percentage of mediation in the overall association between childhood victimization and depressive symptoms was 53.8% for the mediation by neuroticism.
Discussion
In this study, we showed that “childhood abuse experience (A)”, through the mediating effect of “childhood victimization experience (B)”, influenced “neuroticism (C)”, namely, a change in personality traits, and subsequently increased “adulthood depressive symptoms (D)” through childhood victimization experience and neuroticism as mediators. In other words, this study clarified for the first time that the factors (A, B, C, and D) are not only individually associated with each other, but also triggers chain reaction, ie, A to B to C to D. The findings in this study are consistent with our previous findings mentioned in the Introduction section.
We have previously demonstrated that the Big Five personality traits, which are a major foundation of modern psychological research, and affective temperament are involved in depressive symptoms in adulthood, as mediators of the effects of the experience of childhood abuse.9,17,20,23 Furthermore, we demonstrated that the lack of care, and overprotection in childhood have indirect effects on depressive symptoms in adulthood, through the mediating effect of neuroticism, which is one of the Big Five personality traits.22 We have also shown that the experience of childhood abuse not only has a direct effect on depressive symptoms in adulthood, but also has an indirect effect on them through the mediating effects of neuroticism.18 On the other hand, we have demonstrated that the experience of victimization in childhood and adolescence does not have a direct effect on depressive symptoms in adulthood, but has an indirect effect on depressive symptoms through the mediating effect of neuroticism.38 In this study, we were able to advance our understanding of these associations using path analysis. Our study, together with previous studies all suggest that personality traits, particularly neuroticism, are closely associated with adverse experiences and depression in childhood, and influence depression more directly than adverse childhood experiences. Hence, clinicians should focus on the evaluation of these personality traits to understand the psychopathology of their patients, if their patients have experienced adverse events in childhood.
One of the causes of clinical depression and other psychiatric disorders is stress imposed on the brain during childhood and later development. Genetic factors and the type and timing of adverse experiences are considered to be involved in the onset of depression.48,49 When stress is imposed on an individual through adverse experiences, cortisol is secreted for recovery from the damage; however, it is known that excessive amounts of cortisol are secreted under situations of extreme stress, including abuse and victimization.50–52 As excessive cortisol is neurotoxic, its oversecretion damages or destroys nerve cells. In addition, our previous study demonstrated that neonatal maternal separation attenuates the capacity of adult hippocampal neural precursor cells to differentiate into neurons, by decreasing the expression of retinoic acid receptor α through DNA methyltransferase 1-mediated methylation of its promoter.53 In fact, it has been reported that some brain regions become atrophied in individuals experiencing abuse or victimization.54–60 Therefore, it is expected that the damage caused to the brain will be more severe when an individual experiences victimization in addition to abuse, and there is a possibility that the biological basis of the chain reactions of the four factors shown in this study is damage to the brain caused by childhood adverse experiences.
As mentioned in the Introduction section, childhood abuse is associated with subsequent childhood victimization, and childhood victimization results in a higher rate of development of mental health problems, including depressive and anxiety disorders, and self-harm when individuals reach their adolescence, regardless of whether they experienced childhood abuse.29 This may be owing to the fact that the experience of victimization occurs at a time closer to adulthood than the experience of abuse, and that victimization causes more serious damage to an individual’s self-esteem, as it is harassment that takes place in public.61 Supporting these previous findings, in the present study we showed a close association between childhood abuse and victimization, with a standardized coefficient of 0.437 by path analysis. However, our results did not show that childhood victimization had a stronger effect on the severity of depressive symptoms than childhood abuse, because the overall effect of childhood abuse on depressive symptoms was larger than that of childhood victimization. The difference in age between the individuals analyzed in the previous study and our present study may have contributed to the discrepancy in the results. In the present study, both childhood abuse and childhood victimization increased neuroticism, which is a well-known risk factor for the onset of major depression, and may similarly contribute to the onset of depression in subsequent adulthood.24 This close association between childhood adverse experiences and neuroticism may account for the correlation between childhood abuse and victimization. The effects of childhood abuse and victimization on the onset of depression in subsequent adulthood through the mediating effect of neuroticism should be analyzed prospectively in the future.
A history of abuse at home makes a child more likely to be victims or perpetrators of victimization at school.39,40 Lack of care at home, as in cases of abuse, may delay a family’s ability to detect and respond to the child being a victim or a perpetrator of victimization. Such a psychosocial background is expected to trigger a chain reaction of the four factors shown in this study. Therefore, when treating an adult for depressive symptoms, confirming whether or not the patient experienced abuse and victimization in childhood is clinically meaningful towards providing appropriate medical care to maximize therapeutic effects. Moreover, we believe that providing appropriate support to households with a background of abuse and victimization would prevent the occurrence and aggravation of abuse and victimization, contributing to the prevention of future depressive symptoms in the victims.
Some limitations of this study should be considered. First, the results may be influenced by memory bias of childhood events, as this study is based on self-administered questionnaires that rely on the subjects’ memory. Second, as the subjects of this study are adult volunteers, including many healthy subjects, the results may not be generalizable to patients with clinical depression. Third, the nature of the cross-sectional design of this study limits the conclusion of the causal association. Although the path model used in this study is acceptable considering the chronological order of the targets of the questionnaires, a possibility that the chain reaction occurs in the opposite direction cannot be denied. Long-term prospective studies will hence be necessary to confirm the causal associations of a chain reaction of the four factors demonstrated in this study.
Conclusion
The results of this study suggest that individuals who have experienced abuse during childhood are at increased risk of experiencing victimization. In addition, our results suggest that when individuals who have experienced abuse in their childhood also experience victimization, these experiences of abuse and victimization aggravate neuroticism in a chain reaction. Thus, victimization and neuroticism may affect depressive symptoms during adulthood as mediators.
Acknowledgments
The authors did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors for this research. We thank Dr. Nobutada Takahashi of Fuji Psychosomatic Rehabilitation Institute Hospital, Dr. Hiroshi Matsuda of Kashiwazaki Kosei Hospital, Dr. Yasuhiko Takita (deceased) of Maruyamasou Hospital, and Dr. Yoshihide Takaesu of Izumi Hospital for their collection of data of the subjects. We thank Dr. Helena Popiel of the Department of International Medical Communications, Tokyo Medical University, for editorial review of the manuscript. Jiro Masuyaa and Masahiko Ichikia are co-first authors for this study.
Author Contributions
All authors made substantial contributions to the conception and design of the study, acquisition of the data, or analysis and interpretation of the data; took part in drafting the manuscript or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
Jiro Masuya has received personal compensation from Otsuka Pharmaceutical, Eli Lilly, Astellas, and Meiji Yasuda Mental Health Foundation, as well as grants from Pfizer. Masahiko Ichiki has received personal compensation from Otsuka Pharmaceutical, Pfizer, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Meiji Seika Pharma, Janssen Pharmaceutical, Takeda Pharmaceutical Company, MSD, Dainippon Sumitomo Pharma, and Eisai; grants from Otsuka Pharmaceutical, Eli Lilly, Eisai, Shionogi, Takeda Pharmaceutical, MSD, and Pfizer; and is a member of the advisory board of Meiji Seika Pharma. Takeshi Inoue has received personal fees from Mochida Pharmaceutical, Takeda Pharmaceutical, Eli Lilly, Janssen Pharmaceutical, MSD, Taisho Toyama Pharmaceutical, Yoshitomiyakuhin, and Ono Pharmaceutical; a grant from Astellas; and grants and personal fees from Otsuka Pharmaceutical, Sumitomo Dainippon Pharma, Mitsubishi Tanabe Pharma, Kyowa Pharmaceutical Industry, Pfizer, Shionogi, Tsumura, Novartis Pharma, Eisai, Daiichi Sankyo and Meiji Seika Pharma; and is a member of the advisory boards of Pfizer, Novartis Pharma, and Mitsubishi Tanabe Pharma. The other authors do not have any actual or potential conflicts of interest to declare.
References
- 1.Terr LC. Childhood traumas: an outline and overview. Am J Psychiatry. 1991;148(1):10–20. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. International statistical classification of diseases and related health problems 11th version; 2018. Available from: https://icd.who.int/en. Accessed February 3, 2022.
- 3.Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Trauma Stress. 1992;5(3):377–391. doi: 10.1002/jts.2490050305 [DOI] [Google Scholar]
- 4.Brown J, Cohen P, Johnson JG, et al. Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1490–1496. doi: 10.1097/00004583-199912000-00009 [DOI] [PubMed] [Google Scholar]
- 5.Rehan W, Antfolk J, Johansson A, et al. Experiences of severe childhood maltreatment, depression, anxiety and alcohol abuse among adults in Finland. PLoS One. 2017;12(5):1–12. doi: 10.1371/journal.pone.0177252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Springer KW, Sheridan J, Kuo D, et al. The long-term health outcomes of childhood abuse - An overview and a call to action. J Gen Intern Med. 2003;18(10):864–870. doi: 10.1046/j.1525-1497.2003.20918.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Comijs HC, Exel E, Van der Mast RC, et al. Childhood abuse in late-life depression. J Affect Disord. 2013;147(1–3):241–246. doi: 10.1016/j.jad.2012.11.010 [DOI] [PubMed] [Google Scholar]
- 8.Christ C, De Waal MM, Dekker JJM, et al. Linking childhood emotional abuse and depressive symptoms: the role of emotion dysregulation and interpersonal problems. PLoS One. 2019;14(2):e0211882. doi: 10.1371/journal.pone.0211882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayashi Y, Okamoto Y, Takagaki K, et al. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry. 2015;15(1):244. doi: 10.1186/s12888-015-0636-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386–389. doi: 10.1126/science.1083968 [DOI] [PubMed] [Google Scholar]
- 11.Chapman DP, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 12.Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335 [DOI] [PubMed] [Google Scholar]
- 13.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- 14.Kanai Y, Takaesu Y, Nakai Y, et al. The influence of childhood abuse, adult life events, and affective temperaments on the well-being of the general, nonclinical adult population. Neuropsychiatr Dis Treat. 2016;12:823–832. doi: 10.2147/NDT.S100474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toda H, Inoue T, Tsunoda T, et al. The structural equation analysis of childhood abuse, adult stressful life events, and temperaments in major depressive disorders and their influence on refractoriness. Neuropsychiatr Dis Treat. 2015;11:2079–2090. doi: 10.2147/NDT.S82236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Toda H, Inoue T, Tsunoda T, et al. Affective temperaments play an important role in the relationship between childhood abuse and depressive symptoms in major depressive disorder. Psychiatry Res. 2016;236:142–147. doi: 10.1016/j.psychres.2015.12.016 [DOI] [PubMed] [Google Scholar]
- 17.Nakai Y, Inoue T, Toda H, et al. The influence of childhood abuse, adult stressful life events and temperaments on depressive symptoms in the nonclinical general adult population. J Affect Disord. 2014;158:101–107. doi: 10.1016/j.jad.2014.02.004 [DOI] [PubMed] [Google Scholar]
- 18.Ono K, Takaesu Y, Nakai Y, et al. Associations among depressive symptoms, childhood abuse, neuroticism, and adult stressful life events in the general adult population. Neuropsychiatr Dis Treat. 2017;13:477–482. doi: 10.2147/NDT.S128557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uchida Y, Takahashi T, Katayama S, et al. Influence of trait anxiety, child maltreatment, and adulthood life events on depressive symptoms. Neuropsychiatr Dis Treat. 2018;14:3279–3287. doi: 10.2147/NDT.S182783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higashiyama M, Hayashida T, Sakuta K, et al. Complex effects of childhood abuse, affective temperament, and subjective social status on depressive symptoms of adult volunteers from the community. Neuropsychiatr Dis Treat. 2019;15:2477–2485. doi: 10.2147/NDT.S209100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayashida T, Higashiyama M, Sakuta K, et al. Subjective social status via mediation of childhood parenting is associated with adulthood depression in non-clinical adult volunteers. Psychiatry Res. 2019;274:352–357. doi: 10.1016/j.psychres.2019.02.061 [DOI] [PubMed] [Google Scholar]
- 22.Ono Y, Takaesu Y, Nakai Y, et al. The influence of parental care and overprotection, neuroticism and adult stressful life events on depressive symptoms in the general adult population. J Affect Disord. 2017;217:66–72. doi: 10.1016/j.jad.2017.03.058 [DOI] [PubMed] [Google Scholar]
- 23.Otsuka A, Takaesu Y, Sato M, et al. Interpersonal sensitivity mediates the effects of child abuse and affective temperaments on depressive symptoms in the general adult population. Neuropsychiatr Dis Treat. 2017;13:2559–2568. doi: 10.2147/NDT.S144788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161(4):631–636. doi: 10.1176/appi.ajp.161.4.631 [DOI] [PubMed] [Google Scholar]
- 25.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am. J. Psychiatry. 2014;171(4):426–435. doi: 10.1176/appi.ajp.2013.13101375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kendler KS, Gardner CO. A longitudinal etiologic model for symptoms of anxiety and depression in women. Psychol Med. 2011;41(10):2035–2045. doi: 10.1017/S0033291711000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Arlington VA: American Psychiatric Association; 2013. [Google Scholar]
- 28.Bowes L, Joinson C, Wolke D, et al. Peer victimisation during adolescence and its impact on depression in early adulthood: prospective cohort study in the United Kingdom. BMJ. 2015;350:h2469. doi: 10.1136/bmj.h2469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lereya ST, Copeland WE, Costello EJ, et al. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. 2015;2(6):524–531. doi: 10.1016/S2215-0366(15)00165-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schaefer JD, Moffitt TE, Arseneault L, et al. Adolescent victimization and early-adult psychopathology: approaching causal inference using a longitudinal twin study to rule out noncausal explanations. Clin Psychol Sci. 2018;6(3):352–371. doi: 10.1177/2167702617741381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arseneault L. Annual research review: the persistent and pervasive impact of being bullied in childhood and adolescence: implications for policy and practice. J Child Psychol Psychiatry. 2018;59(4):405–421. doi: 10.1111/jcpp.12841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klomek AB, Sourander A, Elonheimo H. Bullying by peers in childhood and effects on psychopathology, suicidality, and criminality in adulthood. Lancet Psychiatry. 2018;2(10):930–941. doi: 10.1016/S2215-0366(15)00223-0 [DOI] [PubMed] [Google Scholar]
- 33.Copeland WE, Wolke D, Angold A, et al. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry. 2013;70(4):419–426. doi: 10.1001/jamapsychiatry.2013.504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geoffroy MC, Boivin M, Arseneault L, et al. Childhood trajectories of peer victimization and prediction of mental health outcomes in midadolescence: a longitudinal population-based study. CMAJ. 2018;190(2):E37–E43. doi: 10.1503/cmaj.170219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takizawa R, Maughan B, Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am J Psychiatry. 2014;171(7):777–784. doi: 10.1176/appi.ajp.2014.13101401 [DOI] [PubMed] [Google Scholar]
- 36.Herba CM, Ferdinand RF, Stijnen T, et al. Victimisation and suicide ideation in the TRAILS study: specific vulnerabilities of victims. J Child Psychol Psychiatry. 2008;49(8):867–876. doi: 10.1111/j.1469-7610.2008.01900.x [DOI] [PubMed] [Google Scholar]
- 37.Sourander A, Jensen P, Rönning JA, et al. What is the early adulthood outcome of boys who bully or are bullied in childhood? The Finnish “from a boy to a man” study. Pediatrics. 2007;120(2):397–404. doi: 10.1542/peds.2006-2704 [DOI] [PubMed] [Google Scholar]
- 38.Tachi S, Asamizu M, Uchida Y, et al. Victimization in childhood affects depression in adulthood via neuroticism: aPath analysis study. Neuropsychiatr Dis Treat. 2019;15:2835–2841. doi: 10.2147/NDT.S220349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baldry AC. Bullying in schools and exposure to domestic violence. Child Abuse Negl. 2003;27(7):713–732. doi: 10.1016/S0145-2134(03)00114-5 [DOI] [PubMed] [Google Scholar]
- 40.Shields A, Cicchetti D. Parental maltreatment and emotion dysregulation as risk factors for bullying and victimization in middle childhood. J Clin Child Adolesc Psychol. 2001;30(3):349–363. doi: 10.1207/S15374424JCCP3003_7 [DOI] [PubMed] [Google Scholar]
- 41.Sanders B, Becker-Lausen E. The measurement of psychological maltreatment: early data on the child abuse and trauma scale. Child Abuse Negl. 1995;19(3):315–323. doi: 10.1016/S0145-2134(94)00131-6 [DOI] [PubMed] [Google Scholar]
- 42.Olweus D. Bullying at school: basic facts and effects of a school based intervention program. J Child Psycho Psychiat. 1994;35(7):1171–1190. doi: 10.1111/j.1469-7610.1994.tb01229.x [DOI] [PubMed] [Google Scholar]
- 43.Eysenck S, Eysenck H, Barrett PA. A revised version of the psychoticism scale. Pers Individ Dif. 1985;6(1):21–29. doi: 10.1016/0191-8869(85)90026-1 [DOI] [Google Scholar]
- 44.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 45.Seki T, Shimura A, Miyama H, et al. Influence of parenting quality and neuroticism on perceived job stressors and psychological and physical stress response in adult workers from the community. Neuropsych Dis Treat. 2020;16:2007–2015. doi: 10.2147/NDT.S260624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muramatsu K, Miyaoka H, Kamijima K, et al. The patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol Rep. 2007;101(3 Pt 1):952–960. doi: 10.2466/pr0.101.3.952-960 [DOI] [PubMed] [Google Scholar]
- 47.Tanabe H, Ozawa S, Goto K Psychometric properties of the Japanese version of the Child Abuse and Trauma Scale (CATS). The 9th Annual Meeting of the Japanese Society for Traumatic Stress Studies; Kobe, Japan; March 6, 2010. [Google Scholar]
- 48.Teicher MH, Tomada A, Andersen SL. Neurobiological consequences of early stress and childhood maltreatment: are results from human and animal studies comparable? Ann N Y Acad Sci. 2006;1071(1):313–323. doi: 10.1196/annals.1364.024 [DOI] [PubMed] [Google Scholar]
- 49.Teicher MH, Anderson CM, Polcari A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc Natl Acad Sci USA. 2012;109(9):E563–572. doi: 10.1073/pnas.1115396109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heim C, Newport DJ, Heit S, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284(5):592–597. doi: 10.1001/jama.284.5.592 [DOI] [PubMed] [Google Scholar]
- 51.Heim C, Newport DJ, Mletzko T, et al. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33(6):693–710. doi: 10.1016/j.psyneuen.2008.03.008 [DOI] [PubMed] [Google Scholar]
- 52.Rudolph KD, Troop-Gordon W, Granger DA. Individual differences in biological stress responses moderate the contribution of early peer victimization to subsequent depressive symptoms. Psychopharmacology. 2011;214(1):209–219. doi: 10.1007/s00213-010-1879-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boku S, Toda H, Nakagawa S, et al. Neonatal maternal separation alters the capacity of adult neural precursor cells to differentiate into neurons via methylation of retinoic acid receptor gene promoter. Biol Psychiatry. 2015;77(4):335–344. doi: 10.1016/j.biopsych.2014.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Andersen SL, Tomada A, Vincow ES, et al. Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. J Neuropsychiatry Clin Neurosci. 2008;20(3):292–301. doi: 10.1176/jnp.2008.20.3.292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teicher MH, Samson JA, Polcari A. Sticks, stones, and hurtful words: relative effects of various forms of childhood maltreatment. Am J Psychiatry. 2006;163(6):993–1000. doi: 10.1176/ajp.2006.163.6.993 [DOI] [PubMed] [Google Scholar]
- 56.Tomoda A, Suzuki H, Rabi K, et al. Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. Neuroimage. 2009;47(Suppl 2):T66–71. doi: 10.1016/j.neuroimage.2009.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tomoda A, Polcari A, Anderson CM, et al. Reduced visual cortex gray matter volume and thickness in young adults who witnessed domestic violence during childhood. PLoS One. 2012;7(12):e52528. doi: 10.1371/journal.pone.0052528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tomoda A. Preliminary evidence of neurobiological and behavioral consequences of exposure to childhood maltreatment on regional brain development. No to Hattatsu. 2011;43(5):345–351. Article in Japanese. [PubMed] [Google Scholar]
- 59.Tomoda A, Navalta CP, Polcari A, et al. Childhood sexual abuse is associated with reduced gray matter volume in visual cortex of young women. Biol Psychiatry. 2009;66(7):642–648. doi: 10.1016/j.biopsych.2009.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Quinlan EB, Barker ED, Luo Q, et al. Peer victimization and its impact on adolescent brain development and psychopathology. Mol Psychiatry. 2020;25(11):3066–3076. doi: 10.1038/s41380-018-0297-9 [DOI] [PubMed] [Google Scholar]
- 61.Delara EW. Bullying Scars: The Impact on Adult Life and Relationships. 1st ed. Oxford University Press; 2016. [Google Scholar]