Abstract
Background
The aim of this study was to evaluate the care-related quality of life in caregivers of breast cancer patients, to assess its association with breast cancer patients’ health-related quality of life (HRQoL), and to identify its potential predictors.
Methods
Caregivers of breast cancer patients at six and twelve months follow up were identified through the institutes electronic patient reported outcome measurement collection tool. The Care-related Quality of Life Instrument (CarerQoL) was used to obtain CarerQoL utility scores by applying a pre-existent set of Dutch tariffs and the CarerQoL VAS score, which represented the overall happiness of caregivers. The associations between breast cancer patients’ EQ-5D-5L and EORTC QLQ-C30 scores and caregivers’ CarerQoL scores was determined with Spearman’s correlation coefficients. Associations between log transformed CarerQol scores and patient and caregiver characteristics were analyzed with multivariable linear regression analyses.
Results
A total of 116 completed CarerQoL questionnaires were analyzed. Most caregivers were male spouses or partners (81.4%) with a mean age of 55.7 ± 16.4. The median CarerQoL utility score was 92.4/100 and median CarerQoL VAS was 8.0/10. We found weak correlations between CarerQoL VAS scores and patients’ EQ-5D-5L utility score (0.301, p = 0.002) and EQ VAS score (0.251, p = 0.009), and between EORTC QLQ-C30 scores and CarerQol VAS (0.339, p < 0.001) and utility score (0.236, p = 0.015). There was a negative association between chemotherapy and log-transformed CarerQoL utility score (B = − 0.063, p = 0.001) and VAS score (B = − 0.044, p = 0.038) at six months follow-up.
Conclusions
This study provides the first evaluation of the CarerQoL in caregivers of Dutch breast cancer patients. Caregivers’ happiness was associated with breast cancer patients’ HRQoL. Our results can be used as reference values for future care-related quality of life evaluations.
Plain English Summary
Breast cancer patients face many difficulties during their cancer journey and often need the support of their caregivers. Despite the fact that successfully providing informal care can have positive effects on caregivers’ wellbeing, it may also have a negative impact on their quality of life. Monitoring the quality of life using a standardized questionnaire, such as the CarerQoL questionnaire, may result in early detection of possible quality of life issues. In this study, we evaluated 116 caregivers and found overall high CarerQoL scores. The scores showed a positive relation to the patients’ quality of life. Lower CarerQoL scores at six months after surgery were found in caregivers of patients who received chemotherapy. Our research underlines the importance to include caregivers of breast cancer patients in clinical practice, provides reference values for future research, and the results can be used to manage the caregivers’ expectations prior to treatment.
Keywords: Breast cancer, Caregivers, Informal care, Quality of life
Background
In the Netherlands, approximately 23% of the population provides informal care for various health indications [1]. Survival rates for breast cancer patients have improved over the last years [2]. Informal care plays an essential part during their diagnostic and treatment process. Having a social network ensures access to informal care which may even positively affect breast cancer outcomes [3, 4].
The term ‘informal care’ is often interpreted in the context of chronically ill or severely disabled patients in need of daily support and care. However, there is a wide variation in definitions of informal care and it is provided in many forms and in all kinds of situations. Informal care may include support during medical visits, managing wound or drain care, managing medication intake or other activities of daily living, and is performed voluntary by non-professional people without compensation. In addition to physical care, the social-emotional support of caregivers has a positive effect during decision making and processing [5].
As shortening of hospital-based care and early hospital discharge after breast surgery has been shown to improve clinical outcomes [6, 7], support for at-home recovery is often required. Additionally, systemic therapies (e.g. chemotherapy) are increasingly being offered to women with breast cancer, which may cause uncomfortable side effects requiring care at home. Breast cancer patients face many difficult decisions during their cancer journey. These situations illustrate that the burden of caregivers is growing. Caregivers often feel obliged to provide informal care to their relatives. Despite the fact that successfully providing informal care can have positive effects on caregivers’ wellbeing, it may also have a negative impact on their lives [8]. Stress or anxiety induced by continuous caregiving may result in health issues and indirectly affect the care recipient [9, 10]. Monitoring the care-related quality of life of caregivers by using a standardized questionnaire may result in early detection of possible financial, relational or health problems [11, 12]. Thus, engaging caregivers during the treatment of breast cancer patients and optimizing the communication between provider, patient and caregiver may lead to better patient outcomes and breast cancer care.
The primary aim of the current study was to evaluate the care-related quality of life in caregivers of breast cancer patients using the Care-related Quality of Life Instrument (CarerQoL). The primary outcome was the CarerQoL utility score. The second aim was to correlate the CarerQoL utility and VAS scores with health-related quality of life (HRQoL) scores of breast cancer patients and to identify potential predictors.
Methods
Recruitment of study participants
Two strategies were used for data collection. Firstly, breast cancer patients that reached 6 or 12 months follow-up after surgery and their caregivers were contacted by post including the study’s background and aim. Breast cancer patients were requested to discuss study participation with their caregiver and to eventually make a joint decision. If caregivers were willing to be enrolled, an additional recruitment letter was sent to them. After the informed consent form was signed by both caregiver and researcher, participants received a brief explanation and hyperlink to the questionnaire by email. Two reminders were sent to participants who failed to complete the questionnaire after 2 and 4 weeks. Participants who did not complete the questionnaire were not included in the analysis. Secondly, the CarerQol has been disseminated through the Erasmus University Medical Center’s electronic patient reported outcome measurement (PROM) collection tool (“Zorgmonitor”) in late 2019, as part of standard care for newly diagnosed breast cancer patients and their caregivers [13]. Data from these completed CarerQoL questionnaires at 6 or 12 months postoperatively were also used for analyses. The 6 or 12 months follow up moments for completion of the CarerQoL were already determined in the PROMs collection tool prior to the concept of this study. Therefore, only breast cancer patients at 6 or 12 months post-surgery were approached during the active recruitment to maintain consistency in time since treatment.
Data collection
CarerQoL data were prospectively collected from August 2019 to February 2021 and stored in a “LimeSurvey” database, a secure online survey tool provider [14]. Characteristics of breast cancer patients were retrospectively collected, including age and type of breast surgery. Neo-adjuvant or adjuvant systemic therapy, endocrine therapy and radiotherapy were collected as a dichotomous outcome (yes/no).
Outcome measurements
CarerQoL
The CarerQoL, developed in 2006 [15], is a caregiver reported measure combining a description of the caregiving situation (CarerQol-7D) with a valuation of informal care in terms of quality of life (CarerQol VAS, a visual analogue scale for general happiness). The current study used a Dutch translation of the first version (2006). The translation was performed by the institute for Medical Technology Assessment prior to the conception and design of this study [16].
The CarerQol-7D comprises seven burden dimensions, of which 5 negative and 2 positive, each with 3 possible answer options. This includes (± indicating positive/negative dimension) fulfillment of care giving ( +), relational problems ( −), mental health problems ( −), problems with combining daily activities ( −), financial problems ( −), social support ( +) and physical health problems ( −).Answers on the negative dimensions of the CarerQol-7D receive a value of 0 (a lot), 1 (some) or 2 (no); answers on the positive dimensions receive a value of 0 (no), 1 (some), or 2 (a lot). After summing the values for the seven dimensions, the overall sum score indicates the impact of informal care on caregivers. The higher the score (range 0–14), the better the caregiver experiences providing informal care. The CarerQol utility score is a weighted sum score using utility tariffs, based on preferences of the general public for the different caregiving situations. Dutch tariffs have been published [17]. The CarerQoL VAS score ranges from 0 (worst experience of the caregiver about the informal care situation) to 10 (best experience of the caregiver about the informal care situation). The psychometric properties of the CarerQol have been investigated in previous studies. The CarerQoL demonstrated no floor or ceiling effects, with high feasibility and a reasonable degree of internal consistency in a study that used data of informal carers in Australia [18]. The CarerQoL has been validated in a large heterogeneous cohort of caregivers in the Netherlands, but not for breast cancer caregivers specifically [19–21]. Other validation studies were performed in caregivers of patients with dementia, caregivers of patients in a palliative setting, and in a large cohort of informal caregivers of older persons [22–24].
Health-related quality of life in breast cancer patients
HRQoL of breast cancer patients was measured with the cancer specific European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30) and the EQ-5D-5L [25, 26]. The EORTC QLQ-C30 is a 30-item questionnaire composed of a global quality of life (QoL) subscale, functional subscales and cancer-related symptom scales. Responses to all items were converted to a 0–100 scale. For functional and global QoL scales, higher scores represent a better level of functioning/QoL than lower scores; for symptom-oriented scales, higher scores represent greater symptom severity [25]. The score for global health status was used to compare HRQoL scores in this study. The EORTC QLQ-C30 is validated for oncology clinical research [27]. It has also been validated and found to be responsive in breast cancer patients and therefore commonly used in breast cancer research investigating HRQoL [25, 28, 29].
The EQ-5D-5L is a standardized, non-disease specific instrument to describe the HRQoL using five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), each with five levels of functioning, ranging from no problems to extreme problems [26]. A quality-adjustment weight or “utility” is a number anchored at 0 and 1, with “perfect health” carrying a weight of 1 and death carrying a weight of 0. In this study, the pre-defined EQ-5D-5L value set of the Netherlands was used to compute utility scores based on a specific health state as indicated by a respondent [30]. The EQ VAS score is related to the EQ-5D-5L and used to rate the overall health on a scale from 0 (worst imaginable health state) to 100 (best imaginable health state) [26]. The EQ-5D-5L is widely recognized as a HRQoL measurement tool for cancer patients and has been validated in breast cancer patients [31, 32].
Statistical analysis
Descriptive statistics, including frequencies and proportions were used to describe patient and caregiver characteristics. Medians and inter-quartile ranges (IQR) were used to present the results of the overall CarerQoL sum scores. All scores were tested for normality with the Kolmogorov–Smirnov and Shapiro–Wilk test. Scores were not normally distributed and natural log transformation was applied to all CarerQoL, EORTC QLQ-C30 and EQ-5D-5L scores. The distribution of responses to the CarerQoL-7D were calculated in percentages for each of the seven dimensions, and for 6 and 12 months post-surgery separately. Univariate and multivariable linear regression analysis were used to assess the association between kind of relationship with patient, patient’s age, type of surgery, adjuvant breast cancer treatments and log transformed CarerQoL scores. Because of the high number of male caregivers and the missing values of caregivers’ age in most cases, these variables were not included in the regression models. The multivariable linear regression analysis was stratified for time since treatment (6 and 12 months). The effect of the predictors was expressed as beta’s and the total amount of variance explained by the models in R2. The Spearman’s rho was used to describe the correlation of caregivers scores and the EQ VAS and EORTC QLQ-C30 scores of their respective breast cancer patient. The interpretation of the Spearman’s correlation coefficients was based on the following standards: 0.1–0.19 (very weak), 0.2–0.39 (weak), 0.4–0.59 (moderate), 0.6–0.79 (strong), and 0.8–1 (very strong) [33]. Two-sided p-values < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS, Version 25.0 (IBM Corporation, Armonk, NY, USA) and R, Version 1.2.
Ethical considerations
Formal approval from the local Medical Ethics Review Committee was waived as the Dutch Medical Research (Human Subjects) Act did not apply to this study.
Results
Study participants
From July till September 2020, a total of 153 breast cancer patients with their respective caregivers received an invitation to participate in the study. Eventually 34 caregivers responded and signed informed consent, of which two caregivers did not complete the questionnaire after sending two reminders, resulting in a response rate of 22%. Additionally, 84 completed CarerQoL questionnaires were identified in the electronic PROMs collection tool (“Zorgmonitor”). Thus, a total of 116 CarerQoL questionnaires from 2019 to 2020 were analyzed; 67 caregivers in the six months and 49 caregivers in the twelve months post-surgery group. A total of 32 caregivers completed the CarerQoL at both follow-up moments.
The majority of caregivers were male (81.4%) and the median age was 60.5 (IQR 25.0) (Table 1a). Most participants were the care recipient’s spouse or partner with a family consisting either of a partner alone or a partner and children. Median age of breast cancer patients was 54.0 (IQR 25.0) and 39.7% received chemotherapy, either neo-adjuvant or adjuvant, 58.6% received radiotherapy and 46.6% were treated with endocrine therapy (Table 1b). None of the patients had metastatic disease.
Table 1.
a and b. Characteristics of caregivers and breast cancer patients (N = 116), 2019–2021
| (a) | |
|---|---|
| Informal caregivers (N = 116) | |
| Median (IQR) N (%) | |
| Age | 60.5 (25.0) |
| Missing (n = 68) | |
| Gender | |
| Male | 94 (81.0) |
| Female | 18 (15.5) |
| Unknown | 4 (3.4) |
| Relation with breast cancer patient | |
| Spouse/partner | 96 (82.7) |
| Other (parent, child, friend) | 20 (15.4) |
| Family status | |
| Alone | 8 (6.8) |
| Partner | 40 (33.9) |
| Child(ren) | 2 (1.7) |
| Partner and child(ren) | 58 (49.2) |
| Unknown | 10 (8.5) |
| (b) | |
|---|---|
| Breast cancer patient or “care recipient” (N = 116) | |
| Median (IQR) N (%) | |
| Age | 54.0 (25) |
| Type of breast surgery | |
| Lumpectomy | 51 (44.1) |
| Mastectomy | 41 (35.3) |
| Reconstruction | 24 (20.7) |
| Radiotherapy | 68 (58.6) |
| Endocrine therapy | 54 (46.6) |
| Chemotherapy | 46 (39.7) |
| Neo adjuvant chemotherapy | 31 (26.7) |
| Adjuvant chemotherapy | 21 (18.1) |
Primary outcome
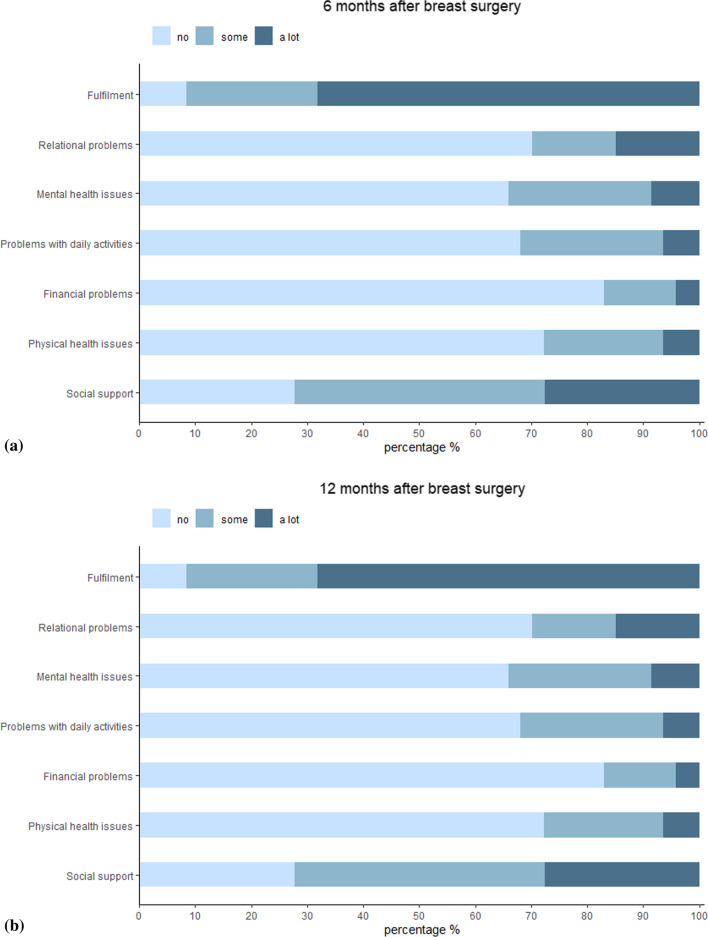
After applying the Dutch set of tariffs to each dimension of the CarerQoL-7D, the median utility score was 92.4/100 (IQR 14.9). According to the positive dimensions, most caregivers experienced some or a lot of fulfillment (98.5% vs. 91.8%) and support when needed (85.1% vs. 71.4%) at six versus twelve months (Fig. 1a and b). Median score for the CarerQol VAS score was 8.0/10 (IQR 1.0) (Table 2).
Fig. 1.
a and b. Distribution of responses to the CarerQol-7D in caregivers of breast cancer patients after 6 and 12 months follow-up (n = 67 and n = 49, respectively)
Table 2.
Median CarerQoL, EQ-5D-5L and EORTC QLQ-C30 scores (N = 116)
| Median (IQR) | 6 months follow-up (N = 67) | 12 months follow-up (N = 49) | |
|---|---|---|---|
| Informal caregivers | |||
| CarerQoL Utility Score | 92.4 (14.9) | 92.3 (14.7) | 93.6 (16.6) |
| CarerQoL VAS Score | 8.0 (1.0) | 7.0 (1.0) | 8.0 (1.0) |
| Breast cancer patients or “care recipient” | |||
| EQ-5D-5L Utility Score | 0.835 (0.137) | 0.818 (0.144) | 0.883 (0.156) |
| EQ VAS Score | 80 (25) | 80 (20) | 80 (26) |
| EORTC QLQ-C30 Global health status | 83.3 (25) | 75 (16.7) | 83.3 (16.7) |
CarerQoL = Carer Quality of Life, VAS = Visual Analogue Scale, IQR = interquartile range
Correlations between caregivers’ and breast cancer patients’ quality of life scores
The CarerQoL VAS score was positively but weakly correlated with the patients’ EQ-5D-5L utility score (0.301, p = 0.002), EQ VAS score (0.251, p = 0.009) and EORTC QLQ-C30 global health status (0.339, p < 0.001). The CarerQoL utility score showed a weak correlation with patient’s EORTC QLQ-C30 global health status (0.236, p = 0.015). See Table 3.
Table 3.
Spearman’s correlation coefficients (N = 116)
| CarerQol VAS Score | CarerQoL utility score | EQ VAS score | EQ-5D-5L utility score | EORTC QLQ-C30 Global health status | |
|---|---|---|---|---|---|
| CarerQoL VAS Score | 0.520 (p < 0.001)* | 0.251 (p = 0.009)* | 0.301 (p = 0.002)* | 0.339 (p < 0.001)* | |
| CarerQoL utility Score | 0.520 (p < 0.001)* | 0.023 (p = 0.810) | 0.148 (p = 0.126) | 0.236 (p = 0.015)* | |
| EQ VAS score | 0.251 (p = 0.009)* | 0.023 (p = 0.810) | 0.678 (p < 0.001)* | 0.608 (p < 0.001)* | |
| EQ-5D-5L Utility score | 0.301 (p = 0.002)* | 0.148 (p = 0.126) | 0.678 (p < 0.001)* | 0.556 (p < 0.001)* |
CarerQoL = Carer Quality of Life, VAS = Visual Analogue Scale. EQ-5D-5L utility and EQ VAS scores and EORTC QLQ-C30 Global health status of breast cancer patients
*Correlation is significant at the level 0.05 (two-tailed)
Univariable and multivariable regression analyses
Data of 116 caregivers at six and twelve months follow up was included in the univariable regression analysis, in which four caregiver characteristics and five patient characteristics were analyzed. Relationship between caregiver and breast cancer patient (partner/spouse versus other) was positively related with caregivers’ log transformed CarerQoL utility score (B = 0.106, p = 0.034). Chemotherapy was associated with the CarerQoL utility score (B = − 0.097, p = 0.019) and to a lesser extent with the CarerQoL VAS score (B = 0.036, p = 0.125). This was also the case for the association between age of breast cancer patient and CarerQoL utility score (B = 0.001, p = 0.034) and CarerQoL VAS score (B = 0.002, p = 0.078).
The multivariable regression analysis revealed chemotherapy as a significant negative predictor for the log transformed CarerQoL utility score (B = − 0.063, p = 0.001) and log transformed CarerQoL VAS score (B = − 0.044, p = 0.038) at 6 months follow-up. Adjusted R2 for the models was 0.188 and 0.165 respectively. At twelve months follow up, results for the log transformed CarerQoL utility score were B = − 0.010 (p = 0.758, Adjusted R2 = 0.126) and B = − 0.042 (i = 0.601, Adjusted R2 = − 0.121) for the CarerQoL VAS score (Table 4).
Table 4.
a and b. Multivariable linear regression coefficients for the log-transformed CarerQoL utility and VAS score after 6 and 12 months follow-up
| CarerQoL utility score | CarerQoL VAS score | |||||
|---|---|---|---|---|---|---|
| Beta | Std. error | Sig | Beta | Std. error | Sig | |
| (a) T = 6 months | ||||||
| Age breast cancer patient | − 7.289E−5 | 0.001 | 0.924 | 0.001 | 0.001 | 0.092 |
| Relationship between caregiver and breast cancer patient | 0.020 | 0.018 | 0.278 | -0.008 | 0.021 | 0.718 |
| Chemotherapy | − 0.063 | 0.018 | 0.001* | − 0.044 | 0.020 | 0.038* |
| Radiotherapy | 0.036 | 0.030 | 0.242 | 0.058 | 0.035 | 0.1 |
| Adjuvant endocrine therapy | − 0.002 | 0.017 | 0.920 | 0.019 | 0.019 | 0.334 |
| Type of surgery | ||||||
| Lumpectomy | Ref | Ref | ||||
| Mastectomy | 0.044 | 0.026 | 0.091 | 0.028 | 0.030 | 0.352 |
| Reconstruction | 0.035 | 0.037 | 0.341 | 0.039 | 0.042 | 0.360 |
| (b) T = 12 months | ||||||
|---|---|---|---|---|---|---|
| Age breast cancer patient | − 3.433E−5 | 0.001 | 0.977 | − 0.001 | 0.003 | 0.778 |
| Relationship between caregiver and breast cancer patient | − 0.002 | 0.028 | 0.954 | − 0.031 | 0.070 | 0.656 |
| Chemotherapy | − 0.010 | 0.031 | 0.758 | − 0.042 | 0.079 | 0.601 |
| Radiotherapy | − 0.061 | 0.051 | 0.237 | − 0.091 | 0.128 | 0.484 |
| Adjuvant endocrine therapy | − 0.009 | 0.028 | 0.735 | 0.018 | 0.070 | 0.797 |
| Type of surgery | ||||||
| Lumpectomy | Ref | Ref | ||||
| Mastectomy | − 0.032 | 0.046 | 0.701 | − 0.011 | 0.115 | 0.925 |
| Reconstruction | − 0.033 | 0.062 | 0.591 | − 0.117 | 0.155 | 0.455 |
*Significance at the level 0.05 (two-tailed)
Discussion
While much effort is generally expended on providing social support for breast cancer patients during treatment, little attention has been paid to the needs of the caregiver in daily practice. The primary aim of this study was to evaluate the quality of life of caregivers of breast cancer patients using the CarerQoL utility and VAS score. In addition, the association with breast cancer patients’ HRQoL and potential predictors of the caregivers’ quality of life were evaluated.
The results of this survey indicates that the overall care-related quality of life of caregivers is good, based on a median CarerQoL utility score of 87.0/100 and VAS score of 8.0/10. The caregivers of breast cancer patients in our cohort formed a homogeneous group, as most caregivers were male spouses or partners. The role of caregiving may be experienced differently between spouses and non-spouses (e.g. close friends or relatives) [35]. Worldwide, caregivers of cancer patients are most often females, experiencing higher levels of caregiving burden. On the contrary, levels of distress may be determined by gender, with females having higher distress levels regardless of their role (e.g. patient or caregiver) [36]. Our results suggest that caregiving does not completely disrupt caregivers’ lives and relationships with breast cancer patients, but could affect the seven dimensions of the social environment in some cases. The question rises to what extent changes in scores are considered to be clinically meaningful. Minimal clinically important differences (MCID) indicate the smallest change in PROM scores which subjects perceive to be important or beneficial, and which would justify an intervention or change in management [37]. MCIDs for the CarerQoL or measures to determine MCIDs for caregivers have not been described previously. The CarerQoL was initially developed for economic evaluations of healthcare, as health care interventions impact both patients and the caregiver burden. When the total societal perspective is evaluated in such cost-effectiveness studies, the optimal approach would be to also include informal care outcomes. However, this may be the most universal questionnaire to evaluate the care-related quality of life in caregivers of cancer patients.
One of the strengths of this study is that the caregivers’ CarerQol scores were correlated to HRQoL scores of breast cancer patients. A positive but weak to moderate correlation was observed between the CarerQoL scores of caregivers and the HRQoL scores of breast cancer patients. It was assumed that care-related quality of life scores of caregivers could reflect the HRQoL of breast cancer patients and vice versa. In caregiving for other diseases, such as Alzheimer or Parkinson’s disease, the caregiver burden was inversely associated with the quality of life of patients [38, 39]. However, our results suggest that although the HRQoL of breast cancer patients diminishes over time, this does not directly impact the care-related quality of life of caregivers. Such observations can possibly be used to manage the caregivers’ expectations prior to treatment.
Another strength is using the CarerQoL Instrument to evaluate the care-related quality of life in caregivers of breast cancer patients, as this has never been described in the literature before. Translating the results of previous caregiver-related studies into daily practice remains challenging. For example, outcomes based on a review of Lopes et al. are only useful to a certain extent as objective measurements are lacking [35]. In three other studies, the psychosocial impact of caregiving in women with advanced breast cancer in a palliative setting or recurrent disease was described [40–42]. Overall, they conclude that patient’s physical and emotional factors can predict the caregivers’ quality of life. According to the Short Form 36 questionnaire, better quality of life scores in patients and caregivers were found if the caregiver was spouse. Formal comparisons with our results was difficult, as this current cohort did not include metastasized or recurrent breast cancer and one study did not use validated questionnaires. The breast cancer patients that were linked to the caregivers in this study made up a small and heterogeneous group according to the treatment characteristics. Treatment strategies for breast cancers have different symptom burden and duration of therapy, which may have an impact on the intensity of care provided by caregivers. This may also influence the tasks and medical support carried out by caregivers. Our results suggest that chemotherapy in breast cancer patients was negatively associated with quality of life scores of caregivers, but previous research found inconsistent results [43–45]. According to a study of Nijboer et al., numerous background characteristics of the caregiver may influence the quality of life, including age, gender, living situation, socioeconomic status and type of relationship between care recipient and caregiver [46]. Another study investigated potential determinants that influence the quality of life of Chinese caregivers of specifically breast cancer patients. Quality of life was measured with the Short Form-36 questionnaire. Although they found several significant associated predictors (income, educational level and symptom severity) which were unfortunately not included in our analyses, similar non-significant correlations for overlapping variables were found [43]. As chemotherapy may contribute to symptom severity, this may explain the negative association with our CarerQoL scores at six months follow up and that the effect on quality of life is normalized after one year. The relationship with breast cancer patients was not investigated, as only spouses were included in their study.
Study limitations
Several limitations were identified in this study. Firstly, although several reminders were sent to participants to complete the questionnaire, one third responded. The low response rate may be due to the fact that caregivers did not directly identify themselves as such. As previously mentioned, caregivers often experience the provision of informal care as an obligation to their family, and something that goes without saying. This may have resulted in some selection bias. On the other side, by disseminating the survey directly to caregivers, we maybe have reached more persons lending informal care who would normally not define themselves as caregivers, for instance because their burden is low. The suboptimal response rate could have influenced the normal distribution of CarerQoL scores, for which log transformation was applied. It is possible that the caregivers with a low burden and relatively good quality of life may be more likely to complete a survey. However, caregivers that have a higher burden may be more self-conscious of their care-related problems, recognize the importance of such research, and are willing to participate in a survey.
Secondly, the lack of socio-demographic characteristics of caregivers prevents to precisely describe the cohort that was studied. Educational level and current work situation can be important explanatory factors of the care-related quality of life. Such variables were only registered for those caregivers that completed the questionnaire after active recruitment and not during standard breast cancer care. Due to the low response rate, these data were not sufficient enough to use in the analysis.
Lastly, the questionnaires were only administered to caregivers of patients of a tertiary hospital with a specialized academic breast cancer center in which more younger women or advanced stages of breast cancer are treated. Therefore, the results may not be generalizable to patients of general hospitals.
Clinical implications
Results highlight the need to include caregivers of breast cancer patients in clinical practice, and provide reference values in a predefined cohort of caregivers of breast cancer patients. The CarerQoL has already been implemented in the institutes electronic PROM collection tool since 2019. Providing feedback and discussing questionnaire outcomes is important to maintain adherence and to act upon if quality of life is diminishing. However, physicians usually do not have a doctor-patient relationship with the caregiver. An implication for clinical practice could be exchanging the CarerQoL outcomes with general practitioners. They could evaluate the quality of life scores of caregivers but also provide additional support or care for the caregiver if needed. In addition, caregivers could benefit from self-management tasks in managing their own quality of life. The CarerQoL may be a suitable tool in optimizing self-management to prevent caregiver-related health issues.
Conclusions
This is the first study that evaluated the CarerQoL Instrument in caregivers of breast cancer patients. Most caregivers felt happy as they were satisfied and experienced fulfillment in their role as caregiver. A minority of the caregivers indicated some problems in their relationship, mental and physical health, finances, or daily activities. Caregivers’ happiness was associated with breast cancer patients’ HRQoL. Chemotherapy was a negative predictor for logtransformed CarerQoL utility and VAS scores as six months follow-up. Results of this study can be used as a reference for future quality of life evaluations in caregivers of breast cancer patients.
Acknowledgements
The authors wish to thank all caregivers for participation.
Authors' contributions
Conceptualization, M.E.C. and L.B.K.; data acquisition, M.E.C.; writing—original draft preparation, M.E.C., A.O.; writing—review and editing, M.E.C., A.O., M.E.E.B., C.V., H.L. and L.B.K.; supervision, L.B.K. All authors have read and agreed to the final version of the manuscript.
Funding
This research received no external funding.
Availability of data and materials
Data shall only be shared with researchers upon reasonably request, at the discretion of the principal investigator.
Code availability
Not applicable.
Declarations
Ethics approval and Consent to participate
Formal approval from the local Medical Ethics Review Committee was waived as the Dutch Medical Research (Human Subjects) Act did not apply to this study. Written informed consent was obtained in all subjects before participation in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schellingerhout R. The informal caregiver. In: J Timmermans (Ed), Informal care Care of and to informal carers. 2003:33–57.
- 2.van der Meer DJ, Kramer I, van Maaren MC, van Diest PJ, S CL, Maduro JH, et al. Comprehensive trends in incidence, treatment, survival and mortality of first primary invasive breast cancer stratified by age, stage and receptor subtype in the Netherlands between 1989 and 2017. Int J Cancer. 2021;148(9):2289–303. [DOI] [PMC free article] [PubMed]
- 3.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 4.Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24(7):1105–1111. doi: 10.1200/JCO.2005.04.2846. [DOI] [PubMed] [Google Scholar]
- 5.Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision-making and treatment received among older breast carcinoma patients. Cancer. 2006;106(4):957–965. doi: 10.1002/cncr.21680. [DOI] [PubMed] [Google Scholar]
- 6.Bundred N, Maguire P, Reynolds J, Grimshaw J, Morris J, Thomson L, et al. Randomised controlled trial of effects of early discharge after surgery for breast cancer. BMJ. 1998;317(7168):1275–1279. doi: 10.1136/bmj.317.7168.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells M, Harrow A, Donnan P, Davey P, Devereux S, Little G, et al. Patient, carer and health service outcomes of nurse-led early discharge after breast cancer surgery: a randomised controlled trial. Br J Cancer. 2004;91(4):651–658. doi: 10.1038/sj.bjc.6601998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schulz R, Newsom J, Mittelmark M, Burton L, Hirsch C, Jackson S. Health effects of caregiving: the caregiver health effects study: an ancillary study of the Cardiovascular Health Study. Ann Behav Med. 1997;19(2):110–116. doi: 10.1007/BF02883327. [DOI] [PubMed] [Google Scholar]
- 9.van Ryn M, Sanders S, Kahn K, van Houtven C, Griffin JM, Martin M, et al. Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psychooncology. 2011;20(1):44–52. doi: 10.1002/pon.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goren A, Gilloteau I, Lees M, DaCosta DM. Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer. 2014;22(6):1637–1646. doi: 10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 11.Lefranc A, Perol D, Plantier M, Chatelain P, de Rohan-Chabot H, Schell M. Assessment of informal caregiver's needs by self-administered instruments: a literature review. Eur J Pub Health. 2017;27(5):796–801. doi: 10.1093/eurpub/ckx103. [DOI] [PubMed] [Google Scholar]
- 12.Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM. Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage. 2003;26(4):922–953. doi: 10.1016/S0885-3924(03)00327-0. [DOI] [PubMed] [Google Scholar]
- 13.GemsTracker. 2011 [updated 17–09–2020. https://gemstracker.org/.
- 14.LimeSurvey. [updated 21–10–2020. https://www.limesurvey.org/.
- 15.Brouwer WB, van Exel NJ, van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006;15(6):1005–1021. doi: 10.1007/s11136-005-5994-6. [DOI] [PubMed] [Google Scholar]
- 16.Hoefman RJ VEN, Brouwer WBF. iVICQ. iMTA Valuation of Informal Care Questionnaire 2013 [updated 17–09–2020. https://www.imta.nl/carerqol/].
- 17.Hoefman RJ, van Exel J, Rose JM, van de Wetering EJ, Brouwer WB. A discrete choice experiment to obtain a tariff for valuing informal care situations measured with the CarerQol instrument. Med Decis Making. 2014;34(1):84–96. doi: 10.1177/0272989X13492013. [DOI] [PubMed] [Google Scholar]
- 18.McCaffrey N, Bucholc J, Rand S, Hoefman R, Ugalde A, Muldowney A, et al. Head-to-head comparison of the psychometric properties of 3 carer-related preference-based instruments. Value Health. 2020;23(11):1477–1488. doi: 10.1016/j.jval.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Hoefman RJ, van Exel J, Brouwer WB. Measuring the impact of caregiving on informal carers: a construct validation study of the CarerQol instrument. Health Qual Life Outcomes. 2013;11:173. doi: 10.1186/1477-7525-11-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoefman RJ, van Exel NJ, Looren de Jong S, Redekop WK, Brouwer WB. A new test of the construct validity of the CarerQol instrument: measuring the impact of informal care giving. Qual Life Res. 2011;20(6):875–87. [DOI] [PMC free article] [PubMed]
- 21.Hoefman RJ, van Exel NJ, Foets M, Brouwer WB. Sustained informal care: the feasibility, construct validity and test-retest reliability of the CarerQol-instrument to measure the impact of informal care in long-term care. Aging Ment Health. 2011;15(8):1018–1027. doi: 10.1080/13607863.2011.575351. [DOI] [PubMed] [Google Scholar]
- 22.Voormolen DC, van Exel J, Brouwer W, Skoldunger A, Goncalves-Pereira M, Irving K, et al. A validation study of the CarerQol instrument in informal caregivers of people with dementia from eight European countries. Qual Life Res. 2021;30(2):577–588. doi: 10.1007/s11136-020-02657-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoefman R, Al-Janabi H, McCaffrey N, Currow D, Ratcliffe J. Measuring caregiver outcomes in palliative care: a construct validation study of two instruments for use in economic evaluations. Qual Life Res. 2015;24(5):1255–1273. doi: 10.1007/s11136-014-0848-8. [DOI] [PubMed] [Google Scholar]
- 24.Lutomski JE, van Exel NJ, Kempen GI, Moll van Charante EP, den Elzen WP, Jansen AP, et al. Validation of the Care-Related Quality of Life Instrument in different study settings: findings from The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS). Qual Life Res. 2015;24(5):1281–93. [DOI] [PubMed]
- 25.McLachlan SA, Devins GM, Goodwin PJ. Validation of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (QLQ-C30) as a measure of psychosocial function in breast cancer patients. Eur J Cancer. 1998;34(4):510–517. doi: 10.1016/S0959-8049(97)10076-4. [DOI] [PubMed] [Google Scholar]
- 26.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bottomley A, Aaronson NK, European Organisation for R, Treatment of C. International perspective on health-related quality-of-life research in cancer clinical trials: the European Organisation for Research and Treatment of Cancer experience. J Clin Oncol. 2007;25(32):5082–6. [DOI] [PubMed]
- 28.Osoba D, Zee B, Pater J, Warr D, Kaizer L, Latreille J. Psychometric properties and responsiveness of the EORTC quality of Life Questionnaire (QLQ-C30) in patients with breast, ovarian and lung cancer. Qual Life Res. 1994;3(5):353–364. doi: 10.1007/BF00451727. [DOI] [PubMed] [Google Scholar]
- 29.Michels FA, Latorre Mdo R, Maciel MS. Validity, reliability and understanding of the EORTC-C30 and EORTC-BR23, quality of life questionnaires specific for breast cancer. Rev Bras Epidemiol. 2013;16(2):352–363. doi: 10.1590/S1415-790X2013000200011. [DOI] [PubMed] [Google Scholar]
- 30.Versteegh MVK, Evers S, de Wit GA, Prenger R, Stolk E. Dutch tariff for the five-level version of EQ-5D. Value Health. 2016;19(4):343–352. doi: 10.1016/j.jval.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 31.Lee CF, Ng R, Luo N, Wong NS, Yap YS, Lo SK, et al. The English and Chinese versions of the five-level EuroQoL Group's five-dimension questionnaire (EQ-5D) were valid and reliable and provided comparable scores in Asian breast cancer patients. Support Care Cancer. 2013;21(1):201–209. doi: 10.1007/s00520-012-1512-x. [DOI] [PubMed] [Google Scholar]
- 32.Pickard AS, De Leon MC, Kohlmann T, Cella D, Rosenbloom S. Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Med Care. 2007;45(3):259–263. doi: 10.1097/01.mlr.0000254515.63841.81. [DOI] [PubMed] [Google Scholar]
- 33.Dancey CP, Reidy J. Statistics without maths for psychology. Pearson/Prentice Hall, Harlow (2007).
- 34.Nunnally J, Bernstein I. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- 35.Lopes VB, Lobo APA, Da Silva Junior GB, Melo AK, Lamboglia CG, Silva C. The experience of male spouses in the context of breast cancer: a systematic review of the literature. Psychol Health Med. 2018;23(1):89–98. doi: 10.1080/13548506.2017.1332374. [DOI] [PubMed] [Google Scholar]
- 36.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134(1):1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- 37.Beaton DE, Boers M, Wells GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheumatol. 2002;14(2):109–114. doi: 10.1097/00002281-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkin Relat Disord. 2006;12(1):35–41. doi: 10.1016/j.parkreldis.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 39.Conde-Sala JL, Garre-Olmo J, Turro-Garriga O, Lopez-Pousa S, Vilalta-Franch J. Factors related to perceived quality of life in patients with Alzheimer's disease: the patient's perception compared with that of caregivers. Int J Geriatr Psychiatry. 2009;24(6):585–594. doi: 10.1002/gps.2161. [DOI] [PubMed] [Google Scholar]
- 40.Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coristine M, Crooks D, Grunfeld E, Stonebridge C, Christie A. Caregiving for women with advanced breast cancer. Psychooncology. 2003;12(7):709–719. doi: 10.1002/pon.696. [DOI] [PubMed] [Google Scholar]
- 42.Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, et al. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol. 2002;20(19):4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 43.Zhu P, Fu JF, Wang B, Lin J, Wang Y, Fang NN, et al. Quality of life of male spouse caregivers for breast cancer patients in China. Asian Pac J Cancer Prev. 2014;15(10):4181–4185. doi: 10.7314/APJCP.2014.15.10.4181. [DOI] [PubMed] [Google Scholar]
- 44.Siegel K, Raveis VH, Mor V, Houts P. The relationship of spousal caregiver burden to patient disease and treatment-related conditions. Ann Oncol. 1991;2(7):511–516. doi: 10.1093/oxfordjournals.annonc.a058005. [DOI] [PubMed] [Google Scholar]
- 45.Shaffer KM, Jacobs JM, Nipp RD, Carr A, Jackson VA, Park ER, et al. Mental and physical health correlates among family caregivers of patients with newly-diagnosed incurable cancer: a hierarchical linear regression analysis. Support Care Cancer. 2017;25(3):965–971. doi: 10.1007/s00520-016-3488-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999;86(4):577–588. doi: 10.1002/(SICI)1097-0142(19990815)86:4<577::AID-CNCR6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data shall only be shared with researchers upon reasonably request, at the discretion of the principal investigator.
Not applicable.