Abstract
Background
Pulmonary embolism is a known complication of coronavirus disease 2019 (COVID-19). Epidemiological population data focusing on pulmonary embolism-related mortality is limited.
Methods
Veneto is a region in Northern Italy counting 4,879,133 inhabitants in 2020. All ICD-10 codes from death certificates (1st January 2018 to 31st December 2020) were examined. Comparisons were made between 2020 (COVID-19 outbreak) and the average of the two-year period 2018–2019. All-cause, COVID-19-related and the following cardiovascular deaths have been studied: pulmonary embolism, hypertensive disease, ischemic heart disease, atrial fibrillation/flutter, and cerebrovascular diseases.
Results
In 2020, a total of 56,412 deaths were recorded, corresponding to a 16% (n = 7806) increase compared to the period 2018–2019. The relative percentage increase during the so-called first and second waves was 19% and 44%, respectively. Of 7806 excess deaths, COVID-19 codes were reported in 90% of death certificates. The percentage increase in pulmonary embolism-related deaths was 27% (95%CI 19–35%), 1018 deaths during the year 2020, compared to 804 mean annual deaths in the period 2018–2019. This was more evident among men, who experience an absolute increase of 147 deaths (+45%), than in women (+67 deaths; +14%). The increase was primarily driven by deaths recorded during the second wave (+91% in October–December). An excess of deaths, particularly among men and during the second wave, was also observed for other cardiovascular diseases, notably hypertensive disease, atrial fibrillation, cerebrovascular disease, and ischemic heart disease.
Conclusions
We observed a considerable increase of all-cause mortality during the year 2020. This was mainly driven by COVID-19 and its complications. The relative increase in the number of pulmonary embolism-related deaths was more prominent during the second wave, suggesting a possible underdiagnosis during the first wave.
1. Introduction
Since the beginning of the severe acute respiratory syndrome coronavirus (SARS-CoV)-2 pandemic, a dramatic increase in the number of deaths was reported. However, recent studies suggested that this increase cannot be attributed to coronavirus disease (COVID)-19-related deaths alone [1]. At the same time, other studies have demonstrated a decrease in hospital admissions for acute cardiovascular disease such as acute myocardial infarction, acute heart failure, or stroke [2], [3], [4]. This phenomenon is not yet fully understood. It may reflect fewer patients with acute cardiovascular events presenting to medical attention for fear of in-hospital infection, a delay of potentially life-saving elective investigations and interventions for cardiovascular disease, or COVID-19 representing a competing risk for the occurrence of acute cardiovascular syndromes. Indeed, an overall concomitant increase in the number of deaths from cardiovascular causes, notably arterial ones, has been described in other studies [5], [6], [7].
Pulmonary embolism is a frequent complication of COVID-19, particularly among hospitalized patients [8]. Physicians and the general population became aware of the prothrombotic potential of COVID-19 early in 2020 [9]. Despite this, the real magnitude of the burden of pulmonary embolism on a population level is still unclear. The reasons are various. The COVID-19 pandemic may have led to a reduction in the use of imaging tests for diagnostic workup [8], [10]. Furthermore, a broader and more aggressive use of pharmacological preventative measures for venous thromboembolism may have partly reduced this risk, as recently shown by trials conducted in the hospital and ambulatory setting [11], [12]. One nationwide French study illustrated that the number of pulmonary embolism-related hospitalizations and in-hospital fatality increased in 2020, particularly during the COVID-19 waves [13].
It is of outstanding interest to analyze data from regions in Europe and North America with high mortality rates during the first two COVID-19 waves, including Northern Italy and the province of New York, to investigate whether the overload of the health care systems or differences regarding patient characteristics and/or complication rates may partly explain the increased mortality. In this context, data on pulmonary embolism-related mortality in the same period is sparse and we do not currently have any large-scale analysis investigating the impact of excess mortality from COVID-19 in relation to pulmonary embolism events. Veneto, a large high-income region of Italy characterized by a homogeneous healthcare system, geography, and demographic structure, was the first European region hit by the COVID-19 pandemic [14]. We retrospectively investigated time trends in COVID-19-related mortality, as well as that of pulmonary embolism and other cardiovascular causes in this region as a proxy for other regions in high-income countries.
2. Material and methods
Veneto is a region in Northern Italy, which in 2020 counted 4,879,133 inhabitants. Causes of death were classified according to the International Classification of Diseases, 10th edition (ICD-10), from the death certificates routinely filled by physicians and transferred to the regional epidemiology department. The standard mortality statistics are derived by applying international rules that identify the underlying cause of death (UCOD) among all conditions listed in the certificate. Usually the UCOD is chosen on the basis of what is indicated by the treating physician, but in some cases a different UCOD is chosen from those listed in the death certificate if considered more appropriate based on standardized algorithms. In order to correctly classify and standardize UCODs, the program IRIS was used, which is established in several European countries. The database also records the comorbidities listed in each death certificate, therefore providing information about multiple causes of death (MCODs).
All death certificates between 1st January 2018 and 31st December 2020 were examined. The causes of death of the year 2020 were compared with those of the two-year period 2018–2019. The analysis was conducted both on MCOD and the UCOD. The ratio of deaths observed in 2020 to those expected (2018–2019 average) was computed with 95% CIs based on the Poisson distribution both for the whole year, and separately for the two epidemic waves involving Italy in March–May and October–December.
The following diseases with their respective ICD-10 codes were used to identify the different conditions: hypertensive diseases (I10–I15), ischemic heart diseases (I20–I25), atrial fibrillation/flutter (I48), cerebrovascular diseases (I60–I69), and pulmonary embolism (I26). In the analysis of the UCOD, COVID-19 deaths were considered both separately and together with codes of respiratory diseases more likely to be used in cases of misrecognized COVID-19 infection (pneumonia and influenza, J09–J189; ARDS-acute respiratory distress syndrome, J80; interstitial pneumonia, J849; respiratory failure, J96.x).
Finally, data on the excess mortality by cause in the whole population and subdivided by sex and age groups are reported. Analyses were limited to deaths for COVID-19 and the main cardiovascular causes (I00–I99, excluding cardiac arrest-I46.9). The deviation in deaths observed in 2020 is expressed as the absolute number of deaths higher or lower than in 2018–2019.
3. Results
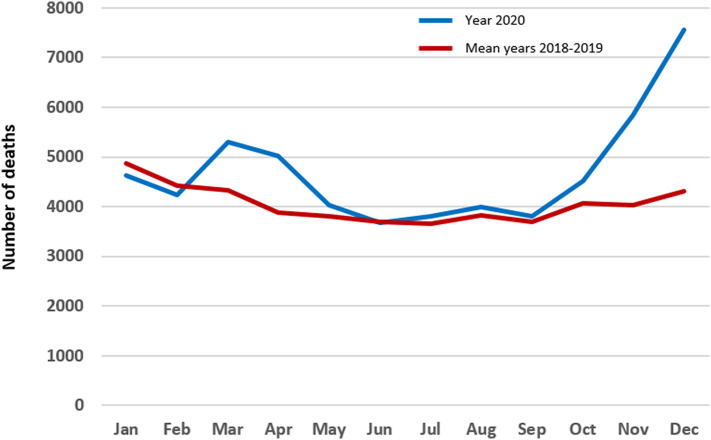
During the years 2018 and 2019, respectively, 48,618 and 48,594 deaths were recorded in Veneto, with an average of 48,606 deaths over the two years. In the year 2020 a total of 56,412 deaths were recorded. Compared with the previous two years, this corresponded to a 16% (n = 7806) increase in the number of deaths overall. In the period between March and May 2020, the relative increase was 19%, as compared to the same period in the two previous years. If one focuses only on the period comprised between October and December 2020, the so-called “second wave”, the relative increase was 44%. Fig. 1 provides information on the monthly number of deaths in the period 2018–2019 and in 2020: two peaks of excess deaths from all causes can be observed during the two coronavirus epidemic waves (March–May 2020 and October–December 2020). The largest increase in the number of all-cause deaths was recorded in nursing homes and long-term institutions (+31%), followed by patients´ homes (+26%), and hospitals (+12%).
Fig. 1.
Total deaths by month in Veneto, Italy (year 2020 vs. mean of the years 2018–2019).
Exponential increase of the number of deaths during the two epidemic waves of coronavirus disease in the year 2020 (blue line) compared to the mean number of deaths in the years 2018–2019. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
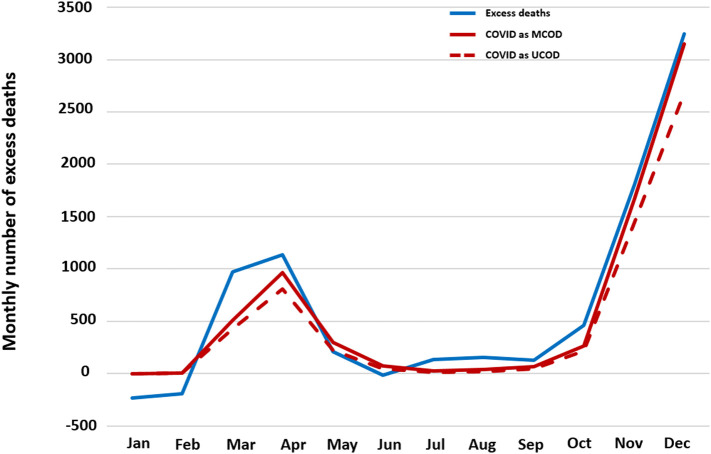
Of 7.806 excess deaths, COVID-19 was listed as the underlying cause of death (UCOD) in 5925 (76%), whereas COVID-19 was reported in any position (MCOD) of 7056 (90%) death certificates. Fig. 2 shows the monthly excess deaths expressed as absolute counts (year 2020 vs average two-year period 2018–2019) for patients with and without COVID-19-specific codes. The total number of COVID-19-related deaths and the proportional mortality rate increased with age, in men more rapidly than in women. In the 50–69 age group, 9% of all deaths recorded in men were due to COVID-19 (COVID-19 as the UCOD), compared to 5% in women. The proportional mortality rate peaked among patients aged 70 or older: in this group, COVID-19 explained at least 11% of all deaths among men and at least 8% among women, as depicted in Table 1 .
Fig. 2.
Monthly excess deaths. Overall and by mention of COVID-19 as underlying or concomitant cause in Veneto, Italy (year 2020 vs mean of years 2018–2019).
Exponential increase during the two epidemic waves of COVID-19 in the total monthly excess deaths in the year 2020 vs mean of the years 2018–2019 (blue line) and monthly excess deaths caused by (red dotted line) and with mention of (red continuous line) COVID-19. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 1.
Age- and sex-specific COVID-19 and non-COVID-19 mortality rates (per 100,000 population) and proportionate mortality (%) in Veneto, Italy (2020).
| Age group | COVID-19 as the underlying cause of death (UCOD) |
Other underlying causes of death |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
Men |
Women |
|||||||
| N | MR | PM | N | MR | PM | N | MR | N | MR | |
| <50 | 16 | 1.2 | 2.2 | 15 | 1.2 | 3.5 | 707 | 52.9 | 409 | 31.8 |
| 50–54 | 35 | 16.8 | 6.6 | 6 | 2.9 | 1.8 | 494 | 236.5 | 333 | 160.8 |
| 55–59 | 67 | 35.2 | 8.5 | 20 | 10.3 | 4.2 | 723 | 380.3 | 458 | 237.0 |
| 60–64 | 102 | 65.1 | 8.4 | 36 | 22.0 | 5.7 | 1106 | 706.2 | 591 | 360.6 |
| 65–69 | 182 | 133.2 | 10.6 | 43 | 29.4 | 4.8 | 1540 | 1127.2 | 846 | 579.2 |
| 70–74 | 317 | 250.6 | 11.7 | 129 | 91.1 | 8.2 | 2393 | 1891.7 | 1438 | 1015.9 |
| 75–79 | 484 | 473.7 | 12.9 | 212 | 170.6 | 8.6 | 3269 | 3199.6 | 2254 | 1814.4 |
| 80–84 | 709 | 931.7 | 13.1 | 435 | 411.8 | 9.5 | 4704 | 6181.8 | 4144 | 3922.9 |
| 85–89 | 641 | 1629.2 | 11.9 | 774 | 1075.7 | 11.6 | 4741 | 12,049.8 | 5904 | 8205.0 |
| 90+ | 491 | 2988.4 | 10.6 | 1211 | 2467.4 | 10.5 | 4129 | 25,130.9 | 10,304 | 20,994.3 |
Abbreviations: N, count; MR, mortality rate; PM, proportionate mortality (%).
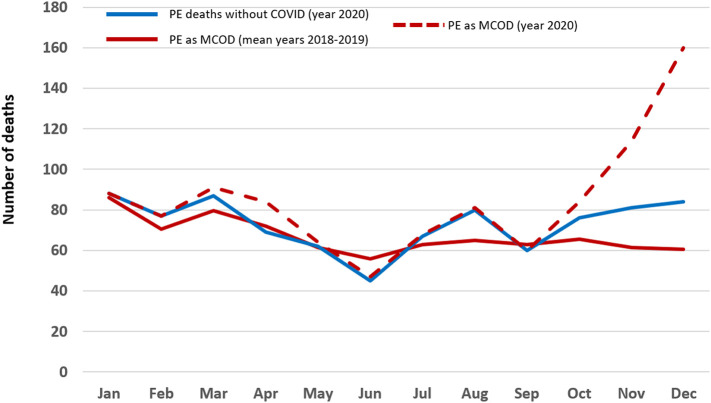
We analyzed the number of deaths related to pulmonary embolism during the year 2020 and compared the absolute count with the average of the years 2018–2019. Table 2, Table 3 provide information on the total number of deaths due to COVID-19, pulmonary embolism, and other cardiovascular diseases in 2020 and during the period 2018–2019. In 2020, there were 1.018 pulmonary embolism-related deaths (MCOD), 476 among males and 542 among females (1.8% of total deaths in 2020). This reflected a 27% (95%CI 19–35%) increase compared to the period 2018–2019. Deaths from pulmonary embolism without mention to COVID-19 codes increased in 2020 only by 9%. The increase in pulmonary embolism-related mortality was more evident in men (+45%, CI 32–58%) than in women (+14%, CI 5–24%). A 14.7% increase was observed also for pulmonary embolism listed as the UCOD.
Table 2.
Underlying cause of death: number of deaths observed in 2020 and % difference from the mean of the years 2018–2019. Patients in the Veneto region, Italy.
| Total |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| 2020 | Δ % vs 2018–2019 | 2020 | Δ % vs 2018–2019 | 2020 | Δ % vs 2018–2019 | |
| Any cause | 56,412 | 16.1 | 26,850 | 17.4 | 29,562 | 14.9 |
| COVID-19 | 5925 | – | 3044 | – | 2881 | – |
| COVID-19 or influenza/pneumonia | 7779 | 369.7 | 3962 | 410.6 | 3817 | 333.3 |
| Pulmonary embolism | 121 | 14.7 | 52 | 25.3 | 69 | 7.8 |
| Ischemic heart diseases | 4721 | 3.4 | 2452 | 2.8 | 2269 | 4.0 |
| Cerebrovascular diseases | 3708 | 1.9 | 1532 | 4.7 | 2176 | −0.0 |
| Atrial fibrillation | 849 | 15.0 | 290 | 7.4 | 559 | 19.4 |
| Hypertensive diseases | 3026 | 13.9 | 1050 | 18.1 | 1976 | 11.8 |
Abbreviations: COVID, Coronavirus Disease.
Table 3.
Underlying or contributing cause of death: number of deaths observed in 2020 and % difference from the mean of the years 2018–2019. Patients in the Veneto region, Italy.
| Total |
Men |
Women |
||||
|---|---|---|---|---|---|---|
| 2020 | Δ % vs. 2018–19 | 2020 | Δ % vs. 2018–19 | 2020 | Δ % vs. 2018–19 | |
| COVID-19 | 7056 | – | 3518 | 3538 | ||
| Pulmonary embolism | 1018 | 26.6 | 476 | 44.7 | 542 | 14.1 |
| Ischemic heart diseases | 8874 | 11.5 | 4987 | 12.6 | 3887 | 10.0 |
| Cerebrovascular diseases | 7355 | 11.4 | 3156 | 14.0 | 4199 | 9.5 |
| Atrial fibrillation | 7170 | 20.7 | 3233 | 24.7 | 3937 | 17.6 |
| Hypertensive diseases | 11,351 | 26.0 | 4765 | 31.3 | 6586 | 22.4 |
Abbreviations: COVID. Coronavirus Disease.
The majority of excess deaths related to pulmonary embolism were recorded during the second wave (October–December 2020), Fig. 3 . If one focuses only on this three-month period, deaths with a diagnosis of pulmonary embolism in any position (MCOD) increased by 91% and deaths with pulmonary embolism as the main cause of death (UCOD) by 46%. This increase was larger in the male population than in the female population, with 140% more deaths versus 58% in cases with pulmonary embolism as concomitant (MCOD) cause, respectively. Two-third of confirmed pulmonary embolism-related deaths were recorded in hospital: the relative increase of deaths occurring in nursing homes and long-term institutions was 44%, followed by patients´ homes (+33%), and hospitals (+28%).
Fig. 3.
Deaths from pulmonary embolism. Overall and by concomitant mention of COVID-19 in Veneto, Italy (year 2020 vs mean of years 2018–2019).
Exponential increase of the number of deaths for pulmonary embolism during the year 2020 (red dotted line) vs the mean numbers of deaths for pulmonary embolism in the years 2018–2019 (continuous red line). Number of deaths for pulmonary embolism without mention of COVID-19 during the year 2020 (blue line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
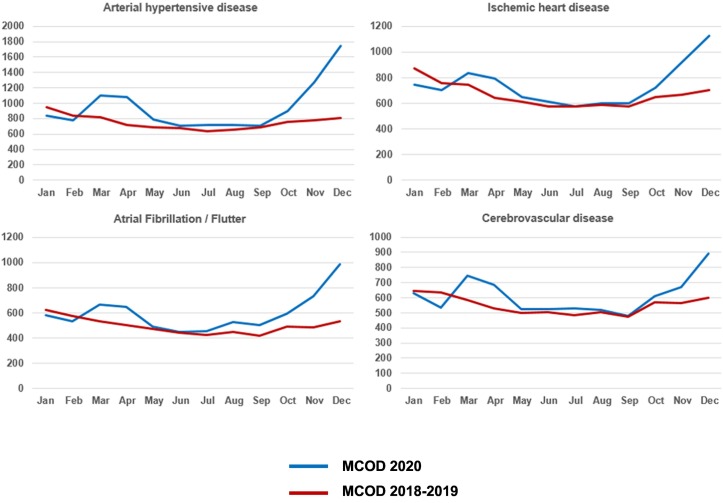
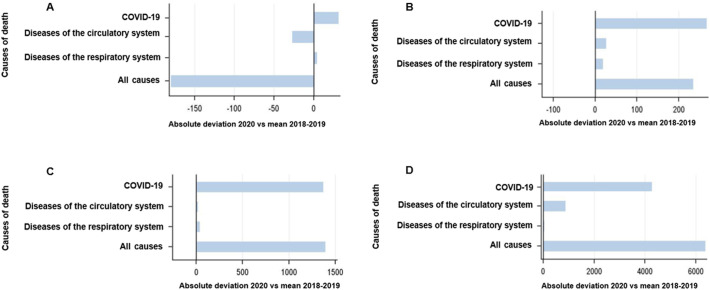
An excess of deaths was also observed for other cardiovascular diseases (Table 2, Table 3), notably atrial fibrillation and hypertensive disease as UCOD, and hypertensive disease, atrial fibrillation, cerebrovascular disease and ischemic heart disease as MCOD. The relative increase in cardiovascular deaths was more prominent in men than in women, and during the second wave than in the first wave (Fig. 4 ). The increase in the number of deaths (COVID-19, cardiovascular diseases, respiratory diseases) across age groups is depicted in Fig. 5 , showing a substantial burden of cardiovascular diseases especially for the elderly.
Fig. 4.
Trends in monthly cause-specific mortality in Veneto, Italy (year 2020 vs mean of years 2018–2019).
Fig. 5.
Excess mortality by cause: absolute deviation in 2020 compared to the mean in 2018–2019 in Veneto, Italy.
Panel A. Age group <50 years; Panel B. Age group 50–64 years; Panel C. Age group 65–79 years; Panel D. Age group >80 year.
4. Discussion
In this retrospective analysis of death certificates in a large Italian region, we observed a dramatic increase in the number of all-cause deaths during the COVID-19 pandemic. COVID-19 itself was the main cause of death or a concomitant cause in 9 out of 10 excess deaths. Death from pulmonary embolism, a frequent and harmful complication of COVID-19, also increased during the period considered. Its presence as MCOD almost doubled at the peak of the pandemic, with a substantial increase in pulmonary embolism-related deaths during the second COVID-19 wave of October–December. At the same time, an excess of mortality was also observed for other cardiovascular causes. The increase in the number of deaths from cardiovascular diseases was larger in men.
An excess of mortality associated with the COVID-19 pandemic has been reported in several countries [15], [16], [17]. A time series analysis of mortality data confirmed a mortality excess in 2020 in 29 high-income countries. Specifically, Italy had among these countries the highest number of excess deaths. In the first wave of the pandemic, when Italy suffered a major surge of COVID-19 cases, an estimated excess of 47,490 deaths was reported, corresponding to nearly 30% increase in expected mortality. This phenomenon was particularly marked in Northern Italian regions, such as Veneto [18]. In our study, we have also observed a larger excess of COVID-19 deaths and cardiovascular deaths in the male population. Previous studies have also highlighted the importance of age- and sex-specific patterns in excess mortality. Mortality rates in the younger population did not deviate from the expected levels, but excess death numbers rose linearly with advancing age [19]. Age-standardization for the analysis of sex differences showed that men were affected more markedly than women [15]. During the peak of the first pandemic wave in Italy age-standardized mortality rates were 37.5 and 23.7 per 100,000 population-year among men and women, respectively [20]. As expected, women represented the majority of the population aged 80 or older and the total number of deaths, as well as the crude mortality, was higher in women.
Our study provides insights in the different causes of excess death rates observed during the pandemic. Pulmonary embolism was one of the death causes that showed substantially increased rates in 2020 compared to the period 2018–2019. A previous study on the time trends in the pulmonary embolism-related mortality rates in Veneto showed a decreasing trend consistent with the overall decreasing trend in the European population until 2018 [21], [22]. In contrast, the current study demonstrated an upward trend of pulmonary embolism-related mortality in 2020 and showed a marked relationship with COVID-19. Notably, pulmonary embolism as cause of death increased also in patients without any mention of COVID-19 in the death certificate. These findings are similar to what reported by French authors concerning national emergency hospitalisations due to pulmonary embolism and in-hospital fatality in 2020 [13]. The recognition (or not) of COVID-19 as the cause of pulmonary embolism may have therapeutic consequences also concerning the length of anticoagulation. Although small, this change in trend compared with the previous years can be attributed to the fact that some patients affected by COVID-19 may have been undiagnosed, and that risk factors for pulmonary embolism, such as sedentary lifestyle, may have been exaggerated during the pandemic. A study of 272,423 hospital admissions in England showed an increased incidence and mortality from thromboembolic events (both arterial and venous) during 2020 compared to 2018 and 2019. Similarly to our findings, the higher risk was observed particularly in pulmonary embolism, with an adjusted relative risk of 1.49 over the pre-COVID-19 period [23]. Furthermore, in accordance with our results, the frequency of deaths from venous thromboembolism among those not diagnosed with COVID-19 also increased [23].
We postulate that the difference observed between the two waves may indicate underdiagnosis of pulmonary embolism, particularly during the first wave and especially considering the discrepancy with reference data from the literature, which estimates a prevalence of pulmonary embolism of at least 15% among hospitalized patients and a 6-week cumulative incidence of 1–2% after hospital discharge [8], [24]. Indeed, one cannot exclude that the increased number of in situ pulmonary thrombosis detected during the course of the pandemic could partly explain this rise [25]. However, the published information concerning the period February–March 2020 from the so-called “red areas” in Italy, including Veneto, suggests a much lower prevalence of pulmonary embolism compared to other European regions a few weeks later, but a similar overall fatality [26], [27], [28]. This is consistent with the challenging logistic situation caused by a novel disease [10] and with the fact that several centers, in line with available guidances, opted for a routine increase in the dosage of anticoagulation for COVID-19 patients with progressive respiratory worsening even in the absence of a confirmed pulmonary embolism diagnosis.
Mortality from other diseases than COVID-19 also increased in 2020 compared to 2018–2019, especially as concomitant causes (MCOD). This finding is probably related to the fact that older individuals with mostly cardiovascular comorbidities such as arterial hypertension, atrial fibrillation/flutter and diabetes mellitus were particularly vulnerable to COVID-19. Moreover, excess deaths from cardiovascular disease and diabetes present with a similar temporal trajectory to deaths from COVID-19 [29]. There is also evidence that the pandemic also affected the outcomes of patients with chronic diseases through the disruption of usual care. Patients with cardiovascular disease presented with increased diagnostic delay and disease severity, especially in the early phases of the pandemic. This effect was particularly evident in patients with ischemic heart disease [30], [31], [32], [33]. In the United States, in the first semester of 2020 deaths by ischemic and hypertensive heart disease increased [7]. However, in Brazil, no changes in cardiovascular disease mortality rates were found during the pandemic, although at-home cardiovascular mortality, especially among older and more socially vulnerable individuals, increased [34]. Whether or not the disruption of care for chronic diseases, such as cardiovascular diseases, will affect mortality rates in the future remains to be investigated [35].
A major strength of this study is the use of causes of death data coded by a standardized method in an administratively homogeneous population to investigate mortality during the years 2020 and 2018–2019, which minimizes the risk of selection bias. This study has several limitations. It refers to the Veneto region of Italy and extrapolation to other European regions must be cautious, given the differences in the baseline characteristics among populations (particularly age), but, most importantly, given the disparate mitigation measures taken by the healthcare authorities to control the surge of the pandemic and the differences across the capacity of healthcare resources and lock-down measures. What these results could, however, suggest is that several countries may have faced a huge discrepancy in the way venous thromboembolic complications were assessed, prevented, and treated between the two waves: to some extent, this data indicates that pulmonary embolism-related mortality paralleled all-cause mortality. Indeed, due to the limited testing capacity at the beginning of the pandemics as well as the increased prevalence of COVID-19 during pandemic peaks (with subsequent reduction of the negative predictive value of testing), COVID-19 deaths were prone to being underestimated. This may have especially been the case in patients who died with pulmonary embolism. In addition, especially in the early phases of the pandemic, misclassification of non-COVID-19 deaths in the elderly and those with comorbidities (cardiovascular disease, diabetes) could have occurred [36]. Access to patient level data for the in-hospital stay as well as long term follow-up (such as demographics and comorbidities) to explore the mechanisms of death was not available in our analysis. Conclusions on the causality between comorbidities and death should be drawn with care: COVID-19 may have simply accelerated the natural process of death in certain vulnerable individuals, who would have soon died anyway from pre-existing diseases (the so-called “mortality displacement”). However, the study design is not appropriate to reject or confirm this hypothesis.
5. Conclusions
In summary, our study highlights a considerable increase of mortality in Veneto, Italy, during the year 2020, which was driven principally by the presence of COVID-19, and which mainly affected older individuals with cardiovascular comorbidities. Deaths from pulmonary embolism increased particularly during the second wave and even in non-COVID-19 patients, suggesting possible underdiagnosis of both pulmonary embolism and COVID-19 during the first wave. Future studies should confirm these findings in diverse populations and explore whether the mass vaccination programs deployed in 2021 will result in a “normalization” of mortality rates in subsequent years.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Vandoros S. Excess mortality during the COVID-19 pandemic: early evidence from England and Wales. Soc. Sci. Med. 2020;258 doi: 10.1016/j.socscimed.2020.113101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solomon M.D., McNulty E.J., Rana J.S., Leong T.K., Lee C., Sung S.H., et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N. Engl. J. Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 3.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of COVID-19 on stroke evaluation in the United States. N. Engl. J. Med. 2020;383(4):400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu J., Mamas M., Rashid M., Weston C., Hains J., Luescher T., et al. Patient response, treatments, and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur. Heart J. Qual. Care Clin. Outcomes. 2021;7(3):238–246. doi: 10.1093/ehjqcco/qcaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banerjee A., Pasea L., Harris S., Gonzalez-Izquierdo A., Torralbo A., Shallcross L., et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395(10238):1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wadhera R.K., Shen C., Gondi S., Chen S., Kazi D.S., Yeh R.W. Cardiovascular deaths during the COVID-19 pandemic in the United States. J. Am. Coll. Cardiol. 2021;77(2):159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roncon L., Zuin M., Barco S., Valerio L., Zuliani G., Zonzin P., et al. Incidence of acute pulmonary embolism in COVID-19 patients: systematic review and meta-analysis. Eur. J. Intern. Med. 2020;82:29–37. doi: 10.1016/j.ejim.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roncon L., Zuin M., Barco S., Zuliani G., Konstantinides S.V. Increased interest in acute pulmonary embolism in Italy during the COVID-19 pandemic: a google trends-based analysis. J. Thromb. Thrombolysis. 2021;52(1):92–94. doi: 10.1007/s11239-020-02336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nopp S., Janata-Schwatczek K., Prosch H., Shulym I., Konigsbrugge O., Pabinger I., et al. Pulmonary embolism during the COVID-19 pandemic: decline in diagnostic procedures and incidence at a university hospital. Res. Pract. Thromb. Haemost. 2020;4(5):835–841. doi: 10.1002/rth2.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sholzberg M., da Costa B.R., Tang G.H., Rahhal H., AlHamzah M., Baumann Kreuziger L., et al. Randomized trials of therapeutic heparin for COVID-19: a meta-analysis. Res. Pract. Thromb. Haemost. 2021;5(8) doi: 10.1002/rth2.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramacciotti E., Barile Agati L., Calderaro D., Aguiar V.C.R., Spyropoulos A.C., de Oliveira C.C.C., et al. Rivaroxaban versus no anticoagulation for post-discharge thromboprophylaxis after hospitalisation for COVID-19 (MICHELLE): an open-label, multicentre, randomised, controlled trial. Lancet. 2022;399(10319):50–59. doi: 10.1016/S0140-6736(21)02392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tankere P., Cottenet J., Tubert-Bitter P., Mariet A.S., Beltramo G., Cadranel J., et al. Impact of COVID-19 and lockdowns on pulmonary embolism in hospitalized patients in France: a nationwide study. Respir. Res. 2021;22(1):298. doi: 10.1186/s12931-021-01887-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Russo F., Pitter G., Da Re F., Tonon M., Avossa F., Bellio S. Epidemiology and public health response in early phase of COVID-19 pandemic, Veneto Region, Italy, 21 February to 2 April 2020. Euro Surveill. 2020;25(47) doi: 10.2807/1560-7917.ES.2020.25.47.2000548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Islam N., Shkolnikov V.M., Acosta R.J., Klimkin I., Kawachi I., Irizarry R.A., et al. Excess deaths associated with COVID-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373 doi: 10.1136/bmj.n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bilinski A., Emanuel E.J. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020;324(20):2100–2102. doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hobohm L., Sagoschen I., Barco S., Schmidtmann I., Espinola-Klein C., Konstantinides S., et al. Trends and risk factors of in-hospital mortality of patients with COVID-19 in Germany: results of a large nationwide inpatient sample. Viruses. 2022;14:275. doi: 10.3390/v14020275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scortichini M., Schneider Dos Santos R., De' Donato F., De Sario M., Michelozzi P., Davoli M., et al. Excess mortality during the COVID-19 outbreak in Italy: a two-stage interrupted time-series analysis. Int. J. Epidemiol. 2021;49(6):1909–1917. doi: 10.1093/ije/dyaa169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention NCHS Excess Deaths Associated with COVID-19 US. 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm#references Available from.
- 20.Gianicolo E.A.L., Russo A., Buchler B., Taylor K., Stang A., Blettner M. Gender specific excess mortality in Italy during the COVID-19 pandemic accounting for age. Eur. J. Epidemiol. 2021;36(2):213–218. doi: 10.1007/s10654-021-00717-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barco S., Mahmoudpour S.H., Valerio L., Klok F.A., Munzel T., Middeldorp S., et al. Trends in mortality related to pulmonary embolism in the European Region, 2000–15: analysis of vital registration data from the WHO mortality database. Lancet Respir. Med. 2020;8(3):277–287. doi: 10.1016/S2213-2600(19)30354-6. [DOI] [PubMed] [Google Scholar]
- 22.Valerio L., Fedeli U., Schievano E., Avossa F., Barco S. Decline in overall pulmonary embolism-related mortality and increasing prevalence of cancer-associated events in the Veneto region (Italy), 2008–2019. Thromb. Haemost. 2021 doi: 10.1055/a-1548-4948. In press. [DOI] [PubMed] [Google Scholar]
- 23.Aktaa S., Wu J., Nadarajah R., Rashid M., de Belder M., Deanfield J., et al. Incidence and mortality due to thromboembolic events during the COVID-19 pandemic: multi-sourced population-based health records cohort study. Thromb. Res. 2021;202:17–23. doi: 10.1016/j.thromres.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zuin M., Engelen M.M., Barco S., Spyropoulos A.C., Vanassche T., Hunt B.J., et al. Incidence of venous thromboembolic events in COVID-19 patients after hospital discharge: a systematic review and meta-analysis. Thromb. Res. 2022;209:94–98. doi: 10.1016/j.thromres.2021.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Dam L.F., Kroft L.J.M., van der Wal L.I., Cannegieter S.C., Eikenboom J., de Jonge E., et al. Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: a different phenotype of thrombotic disease? Thromb. Res. 2020;193:86–89. doi: 10.1016/j.thromres.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mumoli N., Conte G., Cei M., Vitale J., Capra R., Rotiroti G., et al. In-hospital fatality and venous thromboembolism during the first and second COVID-19 waves at a center opting for standard-dose thromboprophylaxis. Thromb. Res. 2021;203:82–84. doi: 10.1016/j.thromres.2021.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dutch C., Thrombosis C., Kaptein F.H.J., Stals M.A.M., Grootenboers M., Braken S.J.E., et al. Incidence of thrombotic complications and overall survival in hospitalized patients with COVID-19 in the second and first wave. Thromb. Res. 2021;199:143–148. doi: 10.1016/j.thromres.2020.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastian T., et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan,Italy. Thromb. Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu D., Ozaki A., Virani S.S. Disease-specific excess mortality during the COVID-19 pandemic: an analysis of weekly US death data for 2020. Am. J. Public Health. 2021;111(8):1518–1522. doi: 10.2105/AJPH.2021.306315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seidu S., Kunutsor S.K., Cos X., Khunti K. Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: a systematic review. Prim. Care Diabetes. 2021;15(4):653–681. doi: 10.1016/j.pcd.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lechner I., Reindl M., Tiller C., Holzknecht M., Troger F., Fink P., et al. Impact of COVID-19 pandemic restrictions on ST-elevation myocardial infarction: a cardiac magnetic resonance imaging study. Eur. Heart J. 2021;00:1–13. doi: 10.1093/eurheartj/ehab621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Porter A., Brown C.C., Tilford J.M., Cima M., Zohoori N., McCormick D., et al. Association of the COVID-19 pandemic and dying at home due to ischemic heart disease. Prev. Med. 2021;153 doi: 10.1016/j.ypmed.2021.106818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Solomon M.D., Nguyen-Huynh M., Leong T.K., Alexander J., Rana J.S., Klingman J., et al. Changes in patterns of hospital visits for acute myocardial infarction or ischemic stroke during COVID-19 surges. JAMA. 2021;326(1):82–84. doi: 10.1001/jama.2021.8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LCC Brant, Pinheiro P.C., ALP Ribeiro, Machado I.E., PRL Correa, Santos M.R. 2021. Cardiovascular mortality during the COVID-19 pandemics in a large Brazilian city: a comprehensive analysis. medRxiv. 2021.10.08.21264699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Banerjee A., Chen S., Pasea L., Lai A.G., Katsoulis M., Denaxas S., et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur. J. Prev. Cardiol. 2021;28:1599–1609. doi: 10.1093/eurjpc/zwaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michelozzi P., de'Donato F., Scortichini M., Pezzotti P., Stafoggia M., De Sario M. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health. 2020;20(1):1238. doi: 10.1186/s12889-020-09335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]