Abstract
Introduction
On March 13, 2020, the U.S. declared COVID-19 to be a national emergency. As communities adopted mitigation strategies, there were potential changes in the trends of injuries treated in emergency department. This study provides national estimates of injury-related emergency department visits in the U.S. before and during the pandemic.
Methods
A secondary retrospective cohort study was conducted using trained, on-site hospital coders collecting data for injury-related emergency department cases from medical records from a nationally representative sample of 66 U.S. hospital emergency departments. Injury emergency department visit estimates in the year before the pandemic (January 1, 2019–December 31, 2019) were compared with estimates of the year of pandemic declaration (January 1, 2020–December 31, 2020) for overall nonfatal injury-related emergency department visits, motor vehicle, falls-related, self-harm-, assault-related, and poisoning-related emergency department visits.
Results
There was an estimated 1.7 million (25%) decrease in nonfatal injury-related emergency department visits during April through June 2020 compared with those of the same timeframe in 2019. Similar decreases were observed for emergency department visits because of motor vehicle‒related injuries (199,329; 23.3%) and falls-related injuries (497,971; 25.1%). Monthly 2020 estimates remained relatively in line with 2019 estimates for self-harm‒, assault-, and poisoning-related emergency department visits.
Conclusions
These findings provide updates for clinical and public health practitioners on the changing profile of injury-related emergency department visits during the COVID-19 pandemic. Understanding the short- and long-term impacts of the pandemic is important to preventing future injuries.
INTRODUCTION
On March 13, 2020, the U.S. declared coronavirus disease 2019 (COVID-19) to be a national emergency. The COVID-19 pandemic resulted in major disruptions to the normal daily life of all individuals in the U.S. and the world. Many states in the U.S. issued stay-at-home orders because the U.S. population shifted to social distancing and transitioned away from in-person activities.1 The uncertainty around COVID-19 also changed health-seeking behaviors because individuals became hesitant to seek potentially necessary medical care.2 , 3 As such, there were potential changes in the pattern of injuries and presentations to emergency departments (EDs) for injuries.
Many studies have examined changes in ED utilization in the U.S. during COVID-19. Using data from the National Syndromic Surveillance Program, Adjemian et al.4 found that ED visits during December 2020–January 2021 were 25% lower than during the same months in the year before. Also using the National Syndromic Surveillance Program, Hartnett and colleagues5 found that ED visits decreased by 42% during March 2020–April 2020 compared with the estimates for the prepandemic period of 1 year earlier, and overall U.S. ED visits increased through July 2020 and then stabilized in August 2020 at levels 15% below those of the same prepandemic period. Holland et al.6 found that during March 15, 2020–October 10, 2020, the median ED visit counts related to mental and behavioral health–related concerns were higher than during the same time period in 2019. A report from the U.S. Consumer Product Safety Commission (CPSC) examined hospital ED data from March through September 2020 and found that visits for product-related injuries overall decreased by 24%, but only decreased by 1% for severe product-related injuries (e.g., thermal burns, amputations).7 Moreover, several national and local studies showed similar declines in ED utilization during March 2020–April 2020.1 , 2 , 8 , 9
Currently, no studies have provided nationally representative estimates of the impacts of the COVID-19 pandemic on injury ED visits in the U.S. since the declaration of the pandemic. The COVID-19 pandemic has affected the ways that many individuals interact and behave owing to public health prevention strategies implemented to slow the spread of COVID-19, such as stay-at-home orders, social distancing, school closures, and canceling of large gatherings. This study provides national estimates of injury ED visits for motor vehicles, falls, self-harm injuries, assault-related injuries, and poisonings before and during the pandemic period using data from the National Electronic Injury Surveillance System–All Injuries Program (NEISS-AIP).
METHODS
Study Sample
The NEISS is operated by CPSC to monitor consumer product-related injuries. NEISS collects information on first-time ED visits from a nationally representative sample of about 100 U.S. hospital EDs. Hospitals in the sample must have a 24-hour ED and have ≥6 beds.10
The Centers for Disease Control and Prevention (CDC)’s National Center for Injury Prevention and Control collaborates with CPSC on an expanded system, NEISS-AIP, which collects data from 66 of the 100 NEISS hospitals and includes about 500,000 unweighted cases nationwide annually.10 NEISS-AIP collects data on all nonfatal injury-related ED visits, whether or not they are associated with consumer products. Trained, on-site hospital coders collect data for injury-related ED cases from medical records at NEISS-AIP hospitals. Coded data and narratives are entered into a computer and electronically transmitted to CPSC. NEISS-AIP quality assurance coders at CPSC receive the data electronically and review all data elements and narratives for each case. Quality assurance coders then use the narrative and other data to assign codes for causes of injury for each case.
Measures
All injuries were classified for intent of injury (i.e., unintentional, assault, self-harm, and legal intervention) and mechanism of injury (e.g., fall, struck by/against, motor vehicle–related, cut/pierce, fire/burn). For intent, self-harm included nonfatal injury or poisoning resulting from a deliberate violent act inflicted on oneself with the intent to take one's own life or with the intent to harm oneself. Assault included nonfatal injuries where physical force by ≥1 people is used with the intent of causing harm, injury, or death to another person, including intentional poisoning by another person and sexual assault. For mechanism, falls included nonfatal injuries received when a person descends abruptly because of the force of gravity and strikes a surface at the same or lower level. Motor vehicle included nonfatal injury to a driver or passenger of a motor vehicle caused by a collision, rollover, crash, or some other event involving another vehicle, an object, or a pedestrian. Poisoning included nonfatal ingestion, inhalation, absorption through the skin, or injection of so much of a drug, toxin, or other chemicals that a harmful effect results (e.g., alcohol intoxication, drug overdose, carbon-monoxide exposure). Injury-related ED visits where the disposition was death were also excluded from this study.
Mechanisms of injury were classified by trained coders into recommended major external cause-of-injury groupings using definitions consistent with International Classification of Diseases, Clinical Modification external cause coding guidelines. Data are weighted to produce national estimates of nonfatal injury‒related ED visits.
Statistical Analysis
The NEISS-AIP data are publicly available for query 12–24 months after initial data collection. This study used an expedited process of cleaning the data and applying the weights to increase the timeliness of national estimates. Monthly weights were provided by CPSC and applied to derive national estimates. Data were analyzed by month of injury treatment, reported sex, and age. Age was grouped into 4 categories: 0–19, 20–35, 36–59, and ≥60 years. Two years before the pandemic (January 1, 2018–December 31, 2018) and the year before the pandemic (January 1, 2019–December 31, 2019) were compared with the year in which the pandemic occurred (January 1, 2020–December 31, 2020) to assess nominal monthly, quarterly, and annual increases and decreases in the number of nonfatal injuries, including motor vehicle‒related injuries, falls, self-harm injuries, assault-related injuries, and poisonings. The 95% CIs were calculated to show the stability of point estimates using the SURVEYMEANS procedure in SAS, version 9.4, that accounted for the sample weights and complex sample design (i.e., 4 strata defined by hospital size on the basis of the number of ED visits annually and 1 stratum of children's hospitals). Point estimate differences where the 95% CI does not overlap 0 were considered statistically significant at the 0.05 level.11 NEISS-AIP data collection, management, and analyses are determined to be public health surveillance activities by CDC human subjects oversight bodies and therefore do not require human subject review or IRB approval.
RESULTS
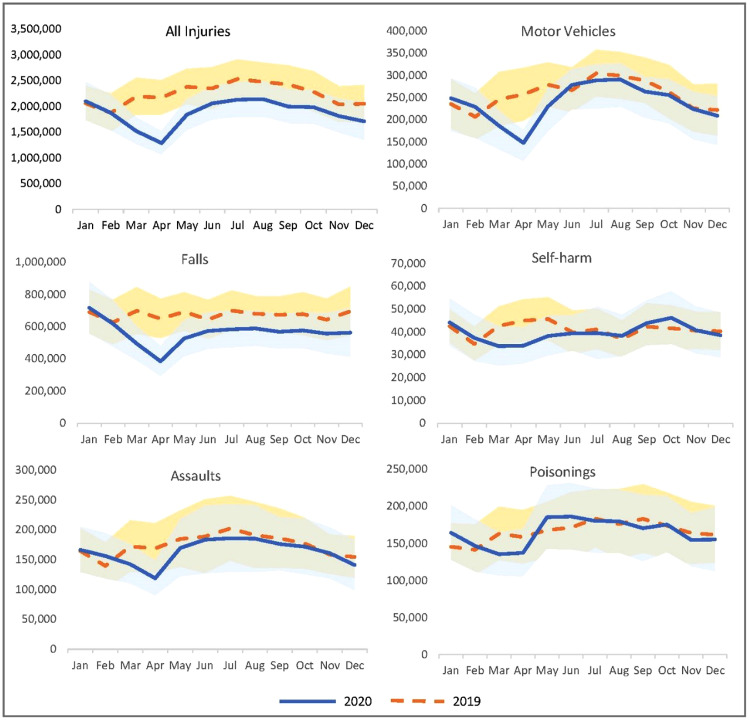
Overall, there was an estimated 4.6 million (17.1%) decrease in nonfatal injury-related ED visits in the U.S. between 2019 and 2020 and an estimated 5.7 (20.5%) decrease between 2018 and 2020. There was a statistically significant decrease during the April through June quarter, with an estimated 1,735,154 (25%) decrease in 2020 compared with that in 2019 (Table 1). The month with the largest decrease (40.7%) was April, where the estimated number of nonfatal injury ED visits in 2020 was 1,288,101 compared with 2,171,386 in 2019 (Figure 1 ). Children and young adults (aged 0–19 years) had the largest and most significant relative decrease in injury ED visits between 2019 and 2020, with a 27.6% decrease in injury-related ED visits (Appendix Table 2, available online).
Table 1.
Quarterly Estimated Differences in Injury-Related Emergency Department Visits by Injury Cause, U.S.—January 1, 2019–December 31, 2020
| Variables | January‒March |
April‒June |
July‒September |
October‒December |
||||
|---|---|---|---|---|---|---|---|---|
| n (%) | (95% CI) | n (%) | (95% CI) | n (%) | (95% CI) | n (%) | (95% CI) | |
| All injuries | −783,316 (−12.8) |
(−2,193,771, −627,139) |
−1,735,154 (−25)** |
(−3,025,471, −44,837)* | −1,180,790 (−15.8) |
(−2,696,007, 334,427) | −888,303 (−13.8) |
(−2,388,671, 612,065) |
| Self-harma | −6,705 (−5.6) |
(−39,968, 26,558) | −18,744 (−14.4) |
(−52,023, 14,535) | 1,076 (0.9) |
(−38,146, 40,298) | 2,641 (2.2) |
(−36,096, 41,378) |
| Assaulta | −26,623 (−7.5) |
(−167,686, 114,440) | −52,418 (−12.7) |
(−233,252, 128,416) | −33,605 (−7.3) |
(−238,515, 171,305) | −19,934 (−5.4) |
(−174,735, 134,867) |
| Fallsa | −245,337 (−12.2) |
(−821,820, 331,146) |
−497,971 (−25.1) |
(−960,447, −35,495) | −314,844 (−15.3) |
(−791,675, 161,987) | −330,057 (−16.3%) |
(−896,570, 236,456) |
| Motor vehiclea | −106,867 (−14.5) |
(−336,736, 123,002) |
−199,329 (−23.3) |
(−390,519, −8,139) | −102,009 (−10.8) |
(−326,188, 122,170) | −75,443 (−9.9) |
(−316,635, 165,749) |
| Poisoninga | −5,337 (−1.2) |
(−144,287, 133,613) | 11,529 (2.3) |
(−152,829, 175,887) | −12,504 (−2.3) |
(−196,893, 171,885) | −15,996 (−3.2) |
(−185,552, 153,560) |
Source: National Electronic Injury Surveillance System—All Injuries program.
Note: Boldface indicates statistical significance (p<0.05).
95% CIs were calculated using the SAS SURVEYMEANS procedure that accounted for sample weights and complex sample design.
Self-harm included nonfatal injury or poisoning resulting from a deliberate violent act inflicted on oneself with the intent to take one's own life or with the intent to harm oneself; assault included nonfatal injuries where physical force by ≥1 persons is used with the intent of causing harm, injury, or death to another person, including intentional poisoning by another person and sexual assault; falls included nonfatal injuries received when a person descends abruptly owing to the force of gravity and strikes a surface at the same or lower level; motor vehicle injuries included nonfatal injury to a driver or passenger of a motor vehicle caused by a collision, rollover, crash or some other event involving another vehicle, an object, or a pedestrian; and poisoning included nonfatal ingestion, inhalation, absorption through the skin, or injection of so much of a drug, toxin, or other chemicals that a harmful effect results (e.g., alcohol intoxication, drug overdose, carbon-monoxide exposure).
Figure 1.
Monthly estimated injury-related emergency department visits by type of injury, U.S.—January 1, 2019–December 31, 2020.
Note: 95% CIs were calculated using the SAS SURVEYMEANS procedure that accounted for the sample weights and complex sample design. Self-harm included nonfatal injury or poisoning resulting from a deliberate violent act inflicted on oneself with the intent to take one's own life or with the intent to harm oneself; assault included nonfatal injuries where physical force by ≥1 persons is used with the intent of causing harm, injury, or death to another person, including intentional poisoning by another person and sexual assault; falls included nonfatal injuries received when a person descends abruptly owing to the force of gravity and strikes a surface at the same or lower level; motor vehicle injuries included nonfatal injury to a driver or passenger of a motor vehicle caused by a collision, rollover, crash, or some other events involving another vehicle, an object, or a pedestrian; and poisoning included nonfatal ingestion, inhalation, absorption through the skin, or injection of so much of a drug, toxin, or other chemicals that a harmful effect results (e.g., alcohol intoxication, drug overdose, carbon-monoxide exposure).
Apr, April; Aug, August; Dec, December; Feb, February; Jan, January; Jul, July; Jun, June; Mar, March; Nov, November; Oct, October; Sep, September.
Source: National Electronic Injury Surveillance System—All Injuries program.
The ED visits owing to motor vehicle-related injuries decreased by 483,649 (14.7%) between 2019 and 2020. There was a statistically significant decrease during the April through June quarter, with an estimated 199,329 (−23.3%) fewer motor vehicle–related ED visits in 2020 than in 2019. The largest decrease (46.1%) was during April when the estimated number of motor vehicle–related ED visits in 2020 was 147,522 compared with 256,621 in 2019 (Figure 1). There was a larger decrease in visits among female individuals than among male individuals (20.7% decrease vs 9.3% decrease) (Appendix Table 2, available online).
The ED visits for falls-related injuries decreased by 1,388,207 (17.2%) between 2019 and 2020. There was a statistically significant decrease during the April through June quarter, with an estimated 497,971 (25.1%) fewer falls-related ED visits in 2020 than in 2019. The largest decrease was in April 2020 (384,077) when visits were almost half (59%) of the estimated number of visits in April 2019 (648,347) (Figure 1). The children and young adult age category (0–19 years) decreased by 27.7% between 2019 and 2020, the largest decrease among all age groups (Appendix Table 2, available online).
There was not a pronounced decrease in self-harm‒related nonfatal ED visits between 2019 and 2020. The largest decrease was in the April to June quarter, with an estimated decrease of 18,744 (14.4%), with the largest monthly decrease during April, but none of these findings were statistically significant. Monthly 2020 self-harm estimates remained relatively in line with 2019 estimates (Figure 1). Female individuals were the largest proportion of self-harm ED visits for both 2019 (59.5%) and 2020 (59.4%). Male and female individuals had similar relative decreases in self-harm ED visits throughout the year (4.0% decrease for male vs 4.7% decrease for female individuals) (Appendix Table 2, available online).
Similar to self-harm, there was not a pronounced decrease in assault-related nonfatal ED visits between 2019 and 2020. The largest decrease was during April when the estimated number of assault-related ED visits in 2020 (118,665) was 29.7% (50,084) lower than in 2019 (168,749), but these findings were not significant (Figure 1). Male individuals had the largest proportion of assault-related ED visits for both 2019 (61.5%) and 2020 (62.8%). Children and young adults (aged 0–19 years) had the largest relative decrease (26.4%) between 2019 and 2020 (Appendix Table 2, available online).
There were no pronounced changes to poisoning-related nonfatal ED visits between 2019 and 2020 for all quarters and months. Male individuals constituted the largest proportion of poisoning-related ED visits for both 2019 (62.8%) and 2020 (63.7%); the group aged 20–35 years was the largest proportion for 2019 (32.4%) and 2020 (33.4%).
DISCUSSION
Overall, injury-related nonfatal ED visits decreased shortly after declaration of the pandemic and mitigation measures such as stay-at-home orders were instituted by states. Although this study did not investigate the reasons for the decline, one contributing factor may be that patients delayed emergency care during the pandemic. Shortly after the implementation of state and local stay-at-home orders, CDC issued health messaging that reinforced the importance of immediately seeking care for serious conditions for which ED visits cannot be avoided, such as myocardial infarction.12 However, Hartnett and colleagues5 hypothesized that people avoided seeking care because of concerns about the COVID-19 infection risk in the ED. Other potential contributing factors could be increased use of telemedicine or virtual visits for care, loss of health insurance because of job loss, or less use of the ED as a safety net for those who lack access to primary care. CPSC suggests that the nationwide surge in COVID-19 cases, consumers’ abundance of caution, and accompanying stay-at-home restrictions likely led to fewer hospital visits.13 It is not known whether injuries decreased during the pandemic or whether the decrease was attributable to ≥1 of these contributing factors. The NEISS-AIP system does not capture injuries that were self-treated or treated in physician offices or urgent care centers, and it is not currently known whether those sites experienced increases or decreases in treatment of injuries while EDs saw decreases.13 Furthermore, overall injury ED visits were likely reduced as explained for specific types of injuries in this section.
The findings from this study on motor vehicle–related injuries are consistent with those of other studies examining motor vehicle‒related injuries before and during the pandemic.14, 15, 16, 17 Sutherland et al16 found that there was a general downward trend of vehicle collisions and vehicle-related injuries in Florida, New York, and Massachusetts during October 1, 2019–March 31, 2020. The authors hypothesized that one of the most important factors likely contributing to these trends is the nationwide practice of social distancing in combination with state-mandated stay-at-home orders. As people stayed at home and reduced their amount of driving, the number of crashes declined, thus reducing the number of traffic-related injuries.14 , 15 Another potential contributing factor was a reduction in alcohol-impaired driving. The consumption of alcohol before driving is a well-known risk factor for traffic collisions.14 As states ordered the closure of nonessential businesses, the prevalence of drinking alcohol at bars, nightclubs, and restaurants decreased and may have led to fewer alcohol-related vehicle collisions and subsequent injuries. It should be noted that this study only assessed ED visits because of motor vehicle–related injuries and that this study did not include fatalities from motor vehicle–related injuries.
For falls-related injuries, many studies have reported syncope or nonmechanical falls as a presenting feature in patients with COVID-19, particularly among older adult patients.18, 19, 20 This may result in an increase in falls-related visits to the ED among the older adult population throughout the pandemic. However, this study found that falls-related ED visits overall dropped at the beginning of the pandemic and did not see any significant increase in falls among older populations aged ≥60 years. Reasons for this decrease may be related to a decrease in falls outside of the home, where 21% of older adult falls occur.21 Falls constituted the largest proportion of injury-related ED visits and are likely a driving factor for the overall decreasing trends in injury-related ED visits.
Past research has indicated that negative consequences related to large-scale disasters include short- and long-term increases in mental health challenges, which can manifest as suicide ideation and attempts.22, 23, 24 Reports have highlighted increases in suicide attempt–related ED visits in the early stages of the pandemic. Notably, reports have shown a 31% increase in mental health‒related ED visits among adolescents aged 12–17 years and a 26% increase in recent suicidal ideation among people aged 18–24 years.25 This study did not find any statistically significant increases in self-harm ED visits during any month in 2020. These results differed from those of Holland and colleagues,6 who found that the median ED visit counts for suicide attempts during March 15, 2020–October 10, 2020 increased compared with those of the same period in 2019. However, notable differences between the data used by Holland et al6 and those in this study include a difference in case definitions (suicide attempt ED visits versus self-harm ED visits) and the inclusion of deaths. This study used a more restrictive definition that bodily harm results from acute exposure to an external force or substance and includes nonsuicidal and suicidal self-harm-related causes.
Although children and young adults represented a small proportion of nonfatal assault‒related ED visits, they had the largest relative decrease between 2019 and 2020. A contributing factor to this decrease may be the national closure of in-person schooling during March and April, which is often a setting for younger adult assault incidents.26 Swedo and colleagues27 assessed trends in U.S. ED visits related to child abuse and neglect using National Syndromic Surveillance Program data from January 6, 2019 to September 6, 2020. Despite decreases in the weekly number of ED visits related to child abuse and neglect, the weekly number of these visits resulting in hospitalizations remained stable in 2020. Similarly, Holland et al6 found decreases in suspected child abuse and neglect when comparing median ED visit counts between March 15 and October 10, 2020 with those in the same time period in 2019. Holland et al. also found decreases in median ED visit counts for intimate partner violence.
Poisoning-related ED visits continue to be predominant among male individuals and among people aged 20–35 years, with the sex and age category proportions remaining relatively unchanged between 2019 and 2020. Several studies have observed increases in specific types of poisonings during the pandemic period.6 , 28 , 29 Holland and colleagues6 found that when median ED visit counts between March 15 and October 10, 2020 were compared with those of the same timeframe in 2019, the 2020 counts were significantly higher for all drug overdoses and opioid overdoses. Although drug and opioid overdoses are included in overall poisonings, this study did not see similar increases. Further research into specific types of poisonings in nonfatal ED visits may better ascertain the nuances of changing poisoning trends during the pandemic.
Although this study provides national estimates of changing injury ED visit trends during the pandemic, further research is needed to ascertain why these changing trends occurred and why trends differed by injury type. For example, motor vehicle ED visits declined in April 2020 but reverted very quickly to levels similar to those in 2019, whereas falls ED visits declined in April 2020 but had estimates below 2019 levels for the rest of the year. Moreover, trends likely differed by city and state because each jurisdiction had different stay-at-home orders and ED utilization behaviors, which are obscured in this national-level analysis.
Limitations
This study has several limitations. Because this analysis is limited to ED visit data, the proportion of people who did not visit EDs but received treatment elsewhere or who did not seek treatment were not captured. Decreases observed in injury ED visits may not be fully attributable to the COVID-19 pandemic because slight decreases (4.0%) were observed comparing 2018 with 2019, suggesting a potentially small decreasing trend even before the pandemic (Appendix Table 1 , available online). In addition, NEISS-AIP did not include information on risk or protective factors, limiting the understanding of the changes observed between 2019 and 2020. NEISS-AIP does not include all information about circumstance and only includes what is in the medical record; therefore, investigators are limited in understanding all the contributing factors behind changing trends. NEISS-AIP is designed to provide national estimates but not state or local estimates.
CONCLUSIONS
These findings provide updates for clinical and public health practitioners on the changing profile of injury-related ED visits during the COVID-19 pandemic. Understanding the short- and long-term impacts of the public health response to the pandemic is important to preventing future injuries. It remains to be determined whether avoided or deferred care after an injury may have impacted health and well-being. Understanding the changes in healthcare-seeking behavior and messaging the importance to the public to seek guidance and emergency care for acute healthcare needs are needed as the U.S. continues to respond to the ongoing pandemic.
Acknowledgments
ACKNOWLEDGMENTS
The coauthors would like to acknowledge the Consumer Product Safety Commission for providing the raw data for this study.
The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
No financial disclosures have been reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Royal Law: Conceptualization, Project administration, Writing - original draft. Amy Wolkin: Supervision, Writing - original draft, Writing - Review and editing. Nimesh Patel: Conceptualization, Data curation, Formal analysis, Writing - review and editing. Alen Alic: Data curation, Formal analysis, Visualizations, Writing - review and editing. Keming Yuan: Formal analysis, Writing - review and editing. Kamran Ahmen: Methodology, Software, Writing - review and editing. Nimi Idaikkadar: Writing - review and editing. Tadesse Haileyesus: Methodology, Writing reivew and editing.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.01.018.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Fuchs VR. Health care policy after the COVID-19 pandemic. JAMA. 2020;324(3):233–234. doi: 10.1001/jama.2020.10777. [DOI] [PubMed] [Google Scholar]
- 2.Jeffery MM, D'Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the U.S. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong L, Hawkins J, Murrell K. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. Waltham, MA: NEJM Catalyst Innovation in Care Delivery. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193. Published May 14, 2020. Accessed April 24, 2021.
- 4.Adjemian J, Hartnett KP, Kite-Powell A, et al. Update: COVID-19 pandemic-associated changes in emergency department visits - United States, December 2020 ‒ January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(15):552–556. doi: 10.15585/mmwr.mm7015a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019‒May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in U.S. Emergency Department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Consumer Product Safety Commission . Consumer Product Safety Commission; Bethesda, MD: March 4, 2021. Hospital emergency room treatment for some product-related injuries rose during the pandemic, even as overall ER visits.https://www.cpsc.gov/content/hospital-emergency-room-treatment-for-some-product-related-injuries-rose-during-the-pandemic PublishedAccessed April 24, 2021. [Google Scholar]
- 8.Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020;76(5):595–601. doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smulowitz PB, O'Malley AJ, Khidir H, Zaborski L, McWilliams JM, Landon BE. National trends in ED visits, hospital admissions, and mortality for Medicare patients during the COVID-19 pandemic. Health Aff (Millwood) 2021;40(9):1457–1464. doi: 10.1377/hlthaff.2021.00561. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) National estimates of nonfatal injuries treated in hospital emergency departments – United States, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(17):340–346. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5017a4.htm [PubMed] [Google Scholar]
- 11.Schenker N, Gentleman JF. On judging the significance of differences by examining the overlap between confidence intervals. Am Stat. 2001;55(3):182–186. doi: 10.1198/000313001317097960. [DOI] [Google Scholar]
- 12.Centers for Disease Control and Prevention. COVID-19: framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. Atlanta, GA: HHS, CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Published April 24, 2020. Accessed June 30, 2020.
- 13.Schroeder T. Consumer Product Safety Commission; Bethesda, MD: January 11, 2021. Effect of novel coronavirus pandemic on 2020 preliminary NEISS estimates.https://www.cpsc.gov/s3fs-public/Effect%20of%20Novel%20Coronavirus%20Pandemic%20on%202020%20Preliminary%20NEISS%20Estimates%20%28March%20%E2%80%93%20September%202020%29.pdf?eBqDdRMGIEQOtp.VG_9IdBCjlFk262hu PublishedAccessed April 24, 2021. [Google Scholar]
- 14.Vandoros S. Covid-19, lockdowns and motor vehicle collisions: empirical evidence from Greece. Inj Prev. 2022;28(1):81–85. doi: 10.1136/injuryprev-2020-044139. [DOI] [PubMed] [Google Scholar]
- 15.Calderon-Anyosa RJC, Kaufman JS. Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med. 2021;143 doi: 10.1016/j.ypmed.2020.106331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutherland M, McKenney M, Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 2020;38(9):1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Doucette ML, Tucker A, Auguste ME, et al. Initial impact of COVID-19’s stay-at-home order on motor vehicle traffic and crash patterns in Connecticut: an interrupted time series analysis. Inj Prev. 2021;27(1):3–9. doi: 10.1136/injuryprev-2020-043945. [DOI] [PubMed] [Google Scholar]
- 18.Chen T, Hanna J, Walsh EE, Falsey AR, Laguio-Vila M, Syncope Lesho E. near syncope, or nonmechanical falls as a presenting feature of COVID-19. Ann Emerg Med. 2020;76(1):115–117. doi: 10.1016/j.annemergmed.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gawronska K, Lorkowski J. Falls as one of the atypical presentations of COViD-19 in older population. Geriatr Orthop Surg Rehabil. 2021;12 doi: 10.1177/2151459321996619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Freitas RF, Torres SC, Martín-Sánchez FJ, Carbó AV, Lauria G, Nunes JPL. Syncope and COVID-19 disease-a systematic review. Auton Neurosci. 2021;235 doi: 10.1016/j.autneu.2021.102872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreland BL, Kakara R, Haddad YK, Shakya I, Bergen G. A descriptive analysis of location of older adult falls that resulted in emergency department visits in the United States, 2015. Am J Lifestyle Med. 2021;15(6):590–597. doi: 10.1177/1559827620942187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grattan LM, Roberts S, Mahan WT Jr., McLaughlin PK, Otwell WS, Morris JG Jr. The early psychological impacts of the Deepwater Horizon oil spill on Florida and Alabama communities. Environ Health Perspect. 2011;119(6):838‒843. https://doi.org/10.1289/ehp.1002915. [DOI] [PMC free article] [PubMed]
- 23.Lee AM, Wong JG, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- 24.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic - United States, January 1‒October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Young AM, Grey M, Boyd CJ. Adolescents’ experiences of sexual assault by peers: prevalence and nature of victimization occurring within and outside of school. J Youth Adolesc. 2009;38(8):1072–1083. doi: 10.1007/s10964-008-9363-y. [DOI] [PubMed] [Google Scholar]
- 27.Swedo E, Idaikkadar N, Leemis R, et al. Trends in U.S. Emergency Department visits related to suspected or confirmed child abuse and neglect among children and adolescents aged < 18 years before and during the COVID-19 pandemic-United States, January 2019‒September 2020 [published correction appears in MMWR Morb Mortal Wkly Rep. 2021;70(2):63] MMWR Morb Mortal Wkly Rep. 2020;69(49):1841–1847. doi: 10.15585/mmwr.mm6949a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chary MA, Overbeek DL, Papadimoulis A, Sheroff A, Burns MM. Geospatial correlation between COVID-19 health misinformation and poisoning with household cleaners in the Greater Boston area. Clin Toxicol (Phila) 2021;59(4):320–325. doi: 10.1080/15563650.2020.1811297. [DOI] [PubMed] [Google Scholar]
- 29.Le Roux G, Sinno-Tellier S, Puskarczyk E, et al. Poisoning during the COVID-19 outbreak and lockdown: retrospective analysis of exposures reported to French poison control centres. Clin Toxicol (Phila) 2021;59(9):832–839. doi: 10.1080/15563650.2021.1874402. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.