Abstract
Weight bias internalization (WBI), a process of weight-based self-devaluation, has been associated with adverse mental and physical health. However, there are limitations with the existing conceptualization and operationalization of WBI that raise questions about the implications of this evidence-base. To address these limitations, the present study investigated the construct validity of WBI by conducting a meta-analysis of associations between WBI (as currently operationalized) and conceptually-related correlates. Studies identified through October 2021 that provided zero-order correlations for associations between WBI and conceptually-related constructs were examined. Meta-regression determined whether these associations differed across WBI measures and demographic (age, sex/gender, race, BMI) and study-level (publication status, sample type, study quality) moderators. Data for 128 (sub)samples were identified (Msample size=477.83, SD=1,679.90; Mage=34.46, SD=12.17; range=10.21–56.60). Greater WBI exhibited large to very large associations with factors suggested to have considerable overlap with this construct (negative and positive body image, self-devaluation), general and weight-specific experiential avoidance, and individuals’ anticipation of future weight stigma. Associations varied for other constructs that have been differentially included in conceptualizations of WBI (endorsing weight bias, weight stigma stereotype awareness, weight stigma experiences), and via measurement-related, demographic, and study-level factors. These findings provide important information that can advance WBI conceptualization and measure-refinement.
Keywords: Weight Bias Internalization, Weight Stigma, Obesity, Psychological Methods
Weight stigma, or experiences of denigration and devaluation based on individuals’ body weights, has gained increased attention in recent decades as a prevalent correlate of multiple adverse mental health outcomes and physiological morbidity (Alimoradi et al., 2019; Emmer et al., 2020; Pearl & Puhl, 2018). Over time, individuals can internalize experiences of weight stigma via a process of weight-based self-devaluation, or weight bias internalization. Weight bias internalization presents at high levels among approximately 20% to 50% of adults with varied body weights (Puhl et al., 2018), and has consistently been identified as a mediator of associations between more frequent weight stigma experiences and poor health-related outcomes among youth and adults, including more disordered eating (Chen et al., 2020; O’Brien et al., 2016; Romano et al., 2021; Zuba & Warschburger, 2017), negative body image (Braun et al., 2020; Forbes & Donovan, 2019), and psychological distress (Magallares et al., 2017). Further, while weight bias internalization is associated with both mental and physical health outcomes, Pearl and colleagues (2018) found more robust relations with mental health compared to physical health outcomes. Although there has been considerable growth in research seeking to improve the understanding of weight bias internalization and its health-related implications in recent years, notable limitations have been identified with the existing conceptualization and operationalization of this construct that raise questions about the implications of these findings. This has incited calls for research that can improve the construct validity of weight bias internalization as this field of study continues to advance (Austen et al., 2020; Meadows & Higgs, 2020).
Limitations in Conceptualizing and Operationalizing Weight Bias Internalization
One notable limitation of the existing evidence-base that has considered weight bias internalization is that this construct has been inconsistently conceptualized over time. Although most definitions of this construct indicate that weight bias internalization involves individuals’ weight-related self-devaluation (Durso & Latner, 2008; Lillis et al., 2010; Pearl & Puhl, 2014), other definitions have suggested that additional factors are central to conceptualizing this construct. In particular, some conceptualizations of weight bias internalization have suggested that individuals need to endorse and apply weight-biased stereotypes to themselves in order to experience weight bias internalization, such as stereotyped beliefs that individuals possess larger body weights due to a lack of willpower (Durso & Latner, 2008; Pearl & Puhl, 2014, 2018). Other definitions have suggested that weight bias internalization involves individuals’ awareness of their identity as a stigmatized individual within society (Pearl & Puhl, 2018; Puhl et al., 2018) and the anticipation of future weight stigma experiences (Griffiths et al., 2018; Lillis et al., 2010). See Austen and colleagues (2020) for further discussion of these variations.
In addition to these conceptual variations, concerns have been raised about existing measures that have been used to operationalize weight bias internalization. In particular, a growing body of evidence has identified considerable overlap between this construct and measures assessing body image and self-worth or self-esteem (Austen et al., 2020; Meadows & Higgs, 2020; Pearl et al., 2021). Most notably, in a recent study of adults with elevated body mass indices (BMIs), bifactor analysis was used to examine the relative amounts of shared and unique variance that could be identified among measures of weight bias internalization (using the original Weight Bias Internalization Scale, WBIS; Durso & Latner, 2008), body image, and self-esteem (Meadows & Higgs, 2020). Results indicated that approximately 78% of the variance in individuals’ scores on the WBIS was explained by a general factor that reflected body-related self-judgment, whereas only 15% of the variance was accounted for by weight bias internalization factor-specific commonality. Such evidence of the jangle fallacy (wherein constructs with different names are measuring the same thing) raises questions about whether weight bias internalization (as currently operationalized) is truly distinct from aspects of self-esteem and body image and the utility of existing operationalizations.
Further, implicit within the process of weight bias internalization, and internalized stigma more generally, is that individuals generally first need to have weight stigma experiences and/or fear experiencing stigma. Yet, evidence has shown that a sizable proportion of individuals who do not report directly experiencing weight stigma nonetheless exhibit elevated weight bias internalization. For example, in a large-scale national study of adults in the U.S., between 21.8% and 41.7% of individuals with above average levels of weight bias internalization did not report three different types of prior weight stigma experiences, including weight-based discrimination, weight-based teasing, and unfair treatment due to their body weights (Puhl et al., 2018). From a construct validity perspective, the implications of this distinction are noteworthy. Although theoretical models of internalized stigma (or self-stigma) more generally do not specify that individuals must invariably experience stigma in order to exhibit self-stigma (Corrigan et al., 2009; Link et al., 1989), the notably high levels of these values may suggest that existing measures of weight bias internalization are not adequately assessing unique aspects of this construct that are distinct from negative body image and self-esteem alone (e.g., Meadows & Higgs, 2020); in other words, individuals who exhibit elevated weight bias internalization via these measures but do not report weight stigma experiences may actually be experiencing heightened negative body image and poor self-esteem (i.e., the jangle fallacy). Alternatively, it is possible that there are non-body image and non-esteem related factors involved in the process of weight-based self-devaluation that may stem, for example, by repeated exposure to societal messages promoting difficult to maintain weight loss goals that may result in individuals internalizing weight bias without also experiencing weight-based discrimination, and these construct-specific factors may not be adequately captured by existing measures of weight bias internalization. These possibilities warrant further assessment to determine potential courses of action for the field to take moving forward.
Central Components of Weight Bias Internalization
A viable first step in addressing this conceptual overlap and identifying ways to improve the construct validity of weight bias internalization is to provide a comprehensive quantitative synthesis of the nature and magnitude of associations between existing measures of weight bias internalization and conceptually-related constructs. As noted above and within a prior overview of this topic (Austen et al., 2020), there appears to be a consensus that weight bias internalization centrally involves a process of self-devaluation due to one’s body weight (Durso & Latner, 2008; Lillis et al., 2010; Pearl & Puhl, 2014), and may also involve individuals’ endorsement and application of weight biased stereotypes to themselves (Durso & Latner, 2008; Pearl & Puhl, 2014, 2018), a sense of awareness of one’s identity as a stigmatized individual within society (Pearl & Puhl, 2018; Puhl et al., 2018), and the anticipation of future weight stigma experiences (Griffiths et al., 2018; Lillis et al., 2010). Many of these elements align with existing theoretical models of internalized stigma in the literature more generally. For example, mental illness self-stigma is believed to involve four sequential steps. The first step involves individuals’ awareness of adverse stereotypes about individuals with mental illness that are held by people within society. The second step is individuals’ agreement with these stereotypes. The third step is individuals’ application of these stereotypes to themselves. The final step is experiences of self-devaluation and poor self-esteem (Corrigan et al., 2009; see also Austen et al., 2020).
Notably, none of the existing measures that have been used to operationalize weight bias internalization to date capture all four of these steps that have been identified as central components of self-stigma more generally (Corrigan et al., 2009) or conceptually-related aspects of this construct that have been included in weight bias internalization conceptualizations (e.g., Durso & Latner, 2008; Lillis et al., 2010; Pearl & Puhl, 2014, 2018). There may also be other construct-specific aspects of weight bias internalization that warrant consideration. For example, weight bias internalization is, in its most general sense, a psychological process that involves navigating difficult self-directed weight-related thoughts. A growing evidence-base has shown that individuals commonly try to avoid or distance themselves from these thoughts via a process of weight-related experiential avoidance. Weight-related experiential avoidance has been robustly associated with greater weight bias internalization at levels that suggest that the jangle fallacy may be evident for these two constructs (Lillis et al., 2010; Palmeira et al., 2018, 2019). In fact, a recent revision (Palmeira et al., 2016) and assessments (Dochat et al., 2020; Weineland et al., 2013) of the Acceptance and Action Questionnaire for Weight-Related Difficulties (AAQW), which has been used to assess weight-related experiential avoidance, have recently identified a weight self-stigma subscale within this measure. Examining the magnitude of the association between weight bias internalization and weight-related experiential avoidance within the literature at large may consequently prove useful in determining whether weight-related experiential avoidance warrants consideration in subsequent efforts to improve the construct validity of weight bias internalization.
Effect Moderators
In addition to determining the nature and magnitude of associations between weight bias internalization and conceptually-related correlates, there is also utility in expanding our understanding of under which circumstances, and for whom, these interrelations may differ. Most notably, it is important to determine whether these associations vary based on the specific measure that is used to operationalize weight bias internalization. This information can determine whether different measures capture different aspects of this construct to greater or lesser extents and serve as a basis for measure refinement moving forward. Likewise, this information can determine whether particular measures exhibit especially large amounts of overlap with constructs like negative body image and self-devaluation/poor self-esteem (Meadows & Higgs, 2020) and may be contributing to the jangle fallacy, wherein constructs with different names are actually measuring the same thing. For example, the original WBIS (Durso & Latner, 2008) that was developed for use with individuals with obesity and the modified weight-neutral adaptation of this measure (WBIS-M; Pearl & Puhl, 2014) are unidimensional. These authors conceptualized weight bias internalization as a process of self-devaluation due to individuals’ body weights that stems from individuals’ beliefs that adverse weight biased stereotypes apply to themselves and included items targeting elements of this conceptualization in their measures. Associations between weight bias internalization and measures of self-devaluation and explicit weight bias (e.g., anti-fat attitudes, weight controllability beliefs) may consequently be stronger for the WBIS and the WBIS-M than other measures. Further, the Weight Self-Stigma Questionnaire (WSSQ; Lillis et al., 2010) is a multidimensional measure that includes both a global score and two subscales that capture individuals’ self-devaluation and fear of enacted stigma. Inclusion of items assessing individuals’ fear of enacted stigma may result in stronger associations between weight bias internalization and both anticipated and prior weight stigma experiences for studies that use this measure versus others.
Further, examining whether associations between weight bias internalization and conceptually-related correlates are moderated by various demographic and anthropometric factors, including age, sex/gender, race, and BMI, can determine whether certain aspects of this construct are more or less applicable to different groups of people. For example, although there are no existing studies that have provided a comparison of associations between weight bias internalization and conceptually-related correlates between youth and adults, it is plausible that certain aspects of weight bias internalization, such as self-devaluation, may have a stronger association with weight bias internalization among adults, particularly if they have had repeated weight stigma experiences over the course of their lives. Different study-level characteristics like sample type may also moderate these associations. For example, individuals who seek weight loss treatment may do so, in part, to try to discard their perceived status as an “overweight or obese person” within society. Associations between weight bias internalization and factors such as negative body image, weight-related experiential avoidance, and self-devaluation may consequently be stronger for individuals who seek weight loss treatment than individuals from the general population. These potential differences warrant exploration.
Study Purpose
Weight bias internalization is prevalent (Puhl et al., 2018), and the field of study seeking to examine the health-related implications of this construct has exhibited considerable growth in recent decades. However, there are notable limitations in the existing conceptualization and operationalization of this construct. In response to recent calls for research to improve the construct validity of weight bias internalization (Austen et al., 2020; Meadows & Higgs, 2020), the present meta-analysis has two primary aims. First, the present meta-analysis aimed to serve as an initial step in clarifying the extent to which weight bias internalization, as currently operationalized within the literature, overlaps with conceptually-related constructs and may be contributing to the jangle fallacy. These constructs include self-devaluation, endorsing weight biased stereotypes, awareness of weight biased stereotypes, anticipating weight stigma experiences, weight-related experiential avoidance, body image, and weight stigma experiences. Second, the present meta-analysis aimed to determine whether these associations differ across weight bias internalization measures and participant and sample characteristics (e.g., demographic factors, sample type). Such evidence can serve as a starting point for measure refinement moving forward.
Method
Search Strategy and Study Selection
The following five databases were deemed relevant to address the present aims and were searched to identify studies for potential inclusion in the present meta-analysis: PubMed, PsycINFO, CINAHL, Web of Science, and ProQuest Dissertations and Theses Global. All searches were conducted from database inception through October 2021. As an example search strategy, the following terms were used for the PsycINFO database: weight bias internalization OR weight bias internalisation OR internalized weight bias OR internalised weight bias OR internalized weight stigma OR internalised weight stigma OR self-directed weight stigma OR self-directed weight bias OR weight self-stigma. Eligible studies were also identified via listservs and contact with study authors. The study selection process is summarized via the preferred reporting items for systematic reviews and meta-analyses (PRISMA) diagram in Figure 1.
Figure 1.
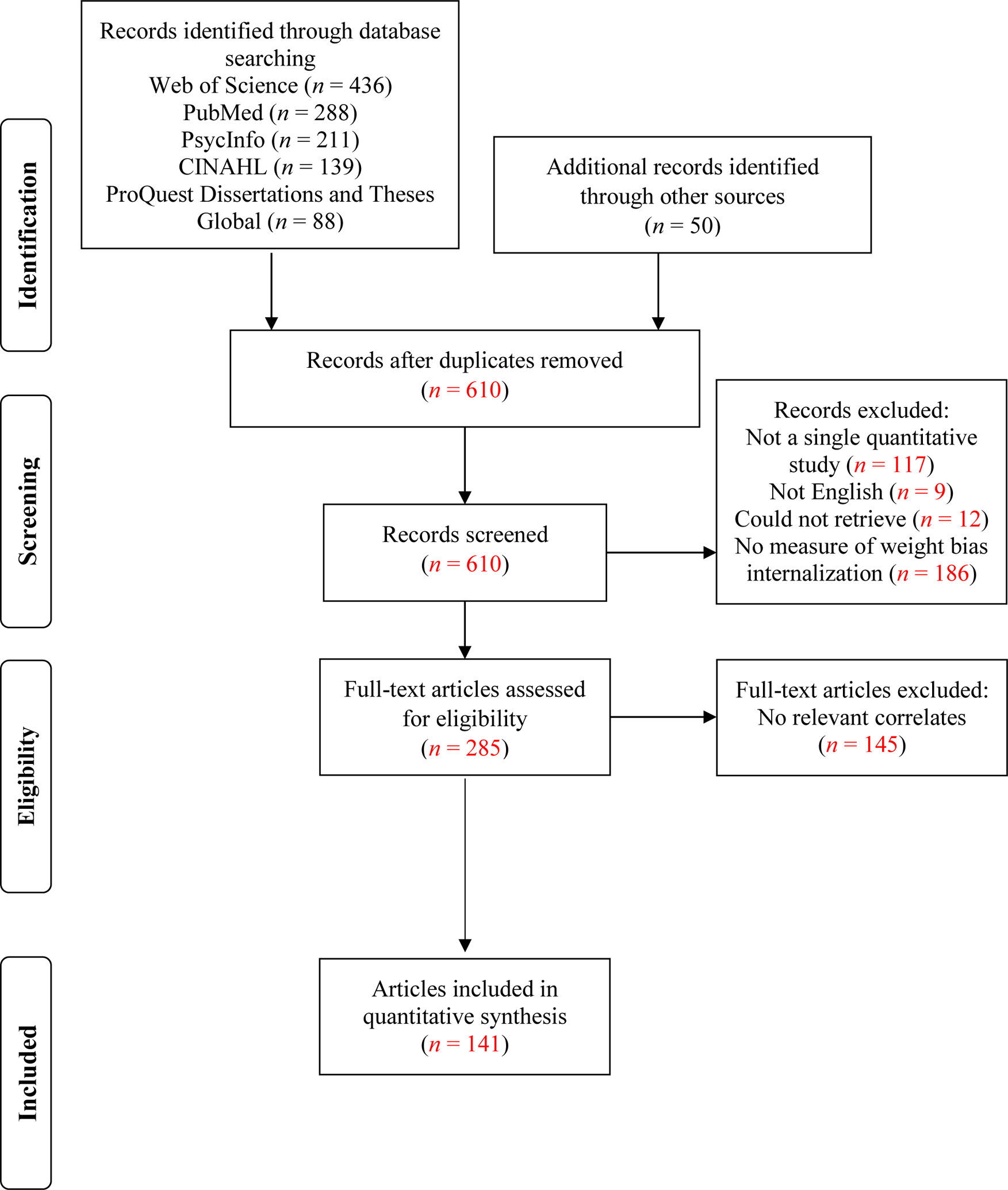
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram for study selection.
Studies were included if they provided a quantitative examination of associations between weight bias internalization and at least one of the following conceptual correlates: negative body image, positive body image, self-devaluation, experienced weight stigma, anti-fat attitudes, weight controllability beliefs (i.e., overweight blame attributions, wherein individuals are believed to have higher weights strictly due to personal factors such as a lack of willpower), general experiential avoidance, weight-related experiential avoidance, anticipated weight stigma, and weight stigma stereotype awareness. Both peer-reviewed and unpublished (e.g., theses, dissertations, conference presentations) studies were included. Studies were excluded if they were not in English, did not include a measure of weight bias internalization, or did not provide relevant data either in text or via correspondence with study authors. Review articles and commentaries were also excluded. However, the reference lists of review articles and commentaries that were collected during the search process were title searched, reviewed, and individually referenced studies were included if they met the present inclusion criteria. To increase the scope and generalizability of the present study’s findings to diverse populations, no study design, publication date, or demographic exclusionary criteria were applied. Further, although studies were not excluded based on whether concurrent (e.g., cross-sectional) or prospective associations were provided, only concurrent associations were identified for use in the present meta-analysis.
Data Collection
Key descriptive and quantitative information were extracted uniformly from each article by coders. These data included: (1) sample characteristics, including participants’ genders/sexes (percentage of females), ages (M, SD), races/ethnicities (percentage of White respondents), and BMIs (M, SD); (2) study-level characteristics, including publication status (peer-reviewed, unpublished), study design (cross-sectional, prospective, experimental, other), countries that participants resided in, and sample type (community, college/university, non-surgical weight loss treatment seeking, bariatric surgery, other); (3) information needed to compute overall effect sizes, including zero-order correlations, analytic sample sizes, and psychometric information for the measures used to assesses weight bias internalization and the assessed correlates (e.g., information relevant to measure interpretation, continuous versus categorical, measure reliability and validity); (4) information needed to assess the risk of study bias (see Risk of Bias and Study Quality below).
The first author screened all potentially eligible studies to determine whether they met the present inclusion criteria. This process was confirmed by two additional research assistants who independently evaluated one-half of the potentially eligible articles. Next, the first author coded all articles that were eligible for inclusion. Four additional coders, first, independently coded the same three articles to ensure that all coders extracted data uniformly. After ensuring coding uniformity for these three articles, each coder then independently coded one-fourth of the eligible articles. The average percent agreement was then computed, given that both qualitative and quantitative data from the articles that met the present inclusion criteria were extracted. The average percent agreement between coders across the coded variables was high (97.37%). Coding discrepancies were resolved through discussions. Further, authors were contacted in cases in which insufficient data were presented to calculate some or all effect sizes and when authors’ reported results implied that they had relevant data (e.g., reported administering a measure of weight bias internalization and at least one other relevant correlate).
Risk of Bias and Study Quality
Criteria were modified from the National Heart, Lung, and Blood Institutes’ Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) and the Newcastle-Ottawa Quality Assessment Scale (Wells et al., 2000) to derive a risk of bias and study quality index. The selected criteria are reported in Supplement F. Each of the assessed criteria were rated as present (1) or absent (0). As above, any score disagreements between coders were resolved by discussion to derive a final rating for each study. A total (summed) score was computed for each study, with a possible range of 0 to 9. Higher scores reflect greater study quality and lower risk of bias. There was a high average percent agreement between coders in deriving this index (85.88%).
Publication bias was assessed and addressed as follows. First, visual examination of funnel plots was used to assess associations between precision (the inverse of the standard error, a function of sample size) and effect sizes. The identified studies will exhibit an asymmetric distribution around the aggregate effect size in cases in which publication bias is evident (Schmidt & Hunter, 2015). Second, Egger’s test of the intercept was used to further assess publication bias. This test suggests that publication bias is evident when it produces a statistically significant intercept value (p<.05). Third, in cases in which Egger’s test was significant (i.e., provides evidence of publication bias), Duval and Tweedie’s Trim and Fill method was used. This method uses an iterative process to trim and impute studies that are potentially missing and then recompute the overall effect. In doing so, it produces an estimate of what the overall effect would be if there was no publication bias (Schmidt & Hunter, 2015).
Data Analyses
Random effects meta-analysis models were run using the Comprehensive Meta-Analysis Version 3.0 software (Borenstein et al., 2014). These models examined associations between weight bias internalization and the identified conceptually-related covariates. Zero-order Pearson’s correlation coefficients (r) served as the effect type and can be interpreted as small (.10), medium (.30), or large (.50; Cohen, 1992). Each study or subsample (for instances in which data were presented separately for different groups of participants, such as females and males) could only provide one effect for use in computing each overall effect size, to ensure that the assumption of independence was met. Thus, data were averaged for use in overall effect size calculations when studies provided data for more than one measure of a construct (e.g., two measures of negative body image), per recommendations (Schmidt & Hunter, 2015). In instances in which multiple papers provided data for the same sample of participants, papers that provided larger analytic samples were used in the present analyses.
Overall effect size distribution heterogeneity was examined using the Cochran Q and I2 statistics. Cochran’s Q examines whether the heterogeneity of a given model is statistically significant. The I2 statistic is used to determine the amount of total variability in a set of effect sizes that can be ascribed to between-study differences (Huedo-Medina et al., 2006). Via the I2 statistic, the degree of between-study variability is considered low when this value is 25% or less, medium when it is approximately 50%, and high at 75% or higher.
Meta-analysis models that included at least 10 effects (Borenstein et al., 2009), were statistically significant, and exhibited significant and large effect size distribution heterogeneity (via significant Q values and/or I2 statistic ≥75%) were further assessed using random-effects meta-regression models with maximum likelihood estimation. Specifically, separate univariate meta-regression models were run with the following moderators: publication status (peer-reviewed=0, unpublished=1), sex/gender (percentage of female participants), mean age, race (percentage of participants who identified as White), mean BMI, sample type (dummy coded variable: community, non-surgical weight loss treatment-seeking [referent], bariatric surgery, college/university, multiple), study quality, and weight bias internalization measure (dummy coded variable: original WBIS [referent], WBIS-M, WSSQ, translated versions of the WBIS, translated versions of the WSSQ, AAQW weight self-stigma subscale, other measure). For sample type, non-surgical weight loss treatment-seeking and bariatric surgery categories were combined in models wherein there were non-significant differences between these groups for parsimony.
Results
Study characteristics are presented in Supplement A. The 141 articles included between 14 and 18,766 participants (M = 477.83, SD = 1,679.90) and provided data for 128 unique (sub)samples of participants. Data from 107 (83.59%) (sub)samples were reported in peer-reviewed publications and 21 (16.41%) in theses, dissertations, or conference presentations. Further, there were 26 (20.31%) non-surgical weight loss treatment-seeking (sub)samples, 9 (7.03%) bariatric (sub)samples, 59 (46.09%) (sub)samples recruited from the community, 29 (22.66%) from colleges or universities, and 5 (3.91%) that combined data from more than one of these sample types. Participants’ mean age was 34.46 (SD = 12.17; range = 10.21–56.60) and mean BMI was 31.43 (SD = 6.93; range = 18.46–49.62). Studies primarily included female respondents (M% female = 72.94, SD = 25.42; range = 0–100.00) and individuals who identified as White (M% White = 68.43, SD = 21.87; range = 0–100.00). There were 66 (51.97%) (sub)samples that included participants with a variety of body weights and 61 (48.03%) (sub)samples that included participants with overweight or obesity only. Participants in most (k = 78, 63.93%) (sub)samples resided in the U.S. only. The average study quality/risk of bias rating score was 6.06 (SD = 1.11; range = 3–9). The most commonly reported measures of weight bias internalization were the modified (Pearl & Puhl, 2014) and the original (Durso & Latner, 2008) Weight Bias Internalization Scale and the Weight Self-Stigma Questionnaire (Lillis et al., 2010).
Overall Effects
Overall effect sizes and heterogeneity for associations between weight bias internalization and the assessed conceptually-related correlates are presented in Table 1 and forest plots are presented in Supplement B. First, strong associations were identified for constructs that have been suggested to exhibit considerable overlap with weight bias internalization measures. Specifically, large effects that were approximately equal in magnitude were found for associations between greater weight bias internalization relative to less positive body image and more negative body image and self-devaluation (rs=−0.580 to 0.581).
Table 1.
Overall Effect Sizes for Associations between Weight Bias Internalization and Health-Related Correlates, Heterogeneity, and Publication Bias
| Effect Size and 95% Confidence Interval | Heterogeneity | Egger’s Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlate | Effects (k) | r | Lower Limit | Upper Limit | Z | p | Q | df | p | I 2 | B0 (SE) | p (1 tailed) |
| Concurrent | ||||||||||||
| Negative Body Image | 67 | 0.581 | 0.530 | 0.628 | 17.438 | <.001 | 2030.207 | 66 | <.001 | 96.749 | −0.928 (1.642) | .287 |
| Positive Body Image | 25 | −0.580 | −0.647 | −0.505 | −12.140 | <.001 | 460.422 | 24 | <.001 | 94.788 | 2.430 (2.298) | .151 |
| Self-Devaluation | 32 | 0.532 | 0.455 | 0.601 | 11.436 | <.001 | 789.336 | 31 | <.001 | 96.073 | 3.396 (2.473) | .090 |
| Experienced Weight Stigma | 55 | 0.430 | 0.389 | 0.469 | 18.440 | <.001 | 983.183 | 54 | <.001 | 94.508 | 1.644 (0.825) | .026 |
| Anti-Fat Attitudes | 26 | 0.202 | 0.138 | 0.264 | 6.093 | <.OO1 | 205.983 | 25 | <.001 | 87.863 | 0.670 (1.233) | .296 |
| Weight Controllability Beliefs | 18 | 0.071 | −0.003 | 0.144 | 1.880 | 0.060 | 144.278 | 17 | <.001 | 88.217 | 0.896 (1.365) | .260 |
| General Experiential Avoidance | 7 | 0.529 | 0.428 | 0.618 | 8.752 | <.001 | 26.361 | 6 | <.001 | 77.239 | 0.775 (2.263) | .373 |
| Weight-Related Experiential Avoidance | 8 | 0.759 | 0.707 | 0.803 | 17.407 | <.001 | 19.300 | 7 | .007 | 63.730 | 1.296 (1.484) | .208 |
| Anticipated Weight Stigma | 3 | 0.657 | 0.490 | 0.778 | 6.129 | <.001 | 12.027 | 2 | .002 | 83.371 | −2.421 (4.684) | .348 |
| Awareness | 2 | 0.260 | 0.208 | 0.310 | 9.458 | <.001 | 0.226 | 1 | .634 | 0.000 | - | - |
Note. Random effects meta-analysis models were run; - = tests of publication bias cannot be run when k < 3.
Patterns of association exhibited more variability for associations between weight bias internalization and other conceptually-related correlates. For example, whereas greater weight bias internalization exhibited a small to moderate association with more anti-fat attitudes (r=0.202), weight bias internalization was not associated with weight controllability beliefs. Further, a moderate to large effect was found for an association between greater weight bias internalization and more experienced weight stigma (r=0.430). Large to very large associations were also identified between greater weight bias internalization and more general and weight-related experiential avoidance (rs=0.529 and 0.759, respectively). In addition, although there were few effects, preliminary evidence suggests that greater weight bias internalization is robustly associated with more anticipated weight stigma (r=0.657) and moderately associated with greater weight stigma stereotype awareness (r=0.260). Finally, apart from the effect for weight stigma stereotype awareness, which was comprised of a small number of individual effects, notable between-study heterogeneity was found across the assessed models.
Publication Bias
Visual examination of funnel plots (see Supplement C) and Egger’s regression test (Table 1) suggested that publication bias may be evident for the model that examined an association between weight bias internalization and experienced weight stigma. To assess this potential impact, Duval and Tweedie’s Trim and Fill procedure was used. There was a slight increase in the magnitude of the adjusted correlation (r=0.478, 95%CI = 0.437 to 0.516) following the imputation of studies identified as missing via this procedure when compared to the original model estimate (r=0.430, 95%CI = 0.389 to 0.469).
Effect Moderation
Results of univariate meta-regressions examining moderators of overall effect magnitude for models with sufficient data (k≥10) are presented in Table 2. Figures depicting models with significant moderators are presented in Supplement D. Associations between weight bias internalization and measures of body image were shown to vary based on the measure that was used to assess weight bias internalization. Specifically, the positive association between greater weight bias internalization and more negative body image was larger in studies that used the WBIS-M and smaller in studies that used the English language and translated versions of the WSSQ, when compared to the original WBIS (R2analogue=0.39). In contrast, the negative association between greater weight bias internalization and less positive body image was larger in studies that used the original WBIS when compared to translated versions of the WBIS and an “other” measure of weight bias internalization (R2analogue=0.52).
Table 2.
Univariate Random Effects Meta-Regressions
| Outcome | Covariate | k | Coefficient | SE | 95% CI Lower | 95% CI Upper | Z | p | Q | df | p | R2 Analog |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Negative Body Image | Publication Status | 67 | −0.065 | 0.101 | −0.262 | 0.132 | −0.65 | .519 | 0.42 | 1 | .519 | 0.01 |
| Sex/Gender | 67 | 0.0003 | 0.001 | −0.002 | 0.003 | 0.26 | .797 | 0.07 | 1 | .797 | 0.00 | |
| Age | 65 | −0.002 | 0.003 | −0.008 | 0.005 | −0.48 | .631 | 0.23 | 1 | .631 | 0.00 | |
| Race | 50 | −0.002 | 0.002 | −0.006 | 0.002 | −1.11 | .267 | 1.23 | 1 | .267 | 0.02 | |
| BMI | 61 | −0.003 | 0.005 | −0.013 | 0.008 | −0.50 | .617 | 0.25 | 1 | .617 | 0.00 | |
| Population: Community | 67 | 0.118 | 0.086 | −0.051 | 0.286 | 1.37 | .171 | 1.88 | .598 | 0.02 | ||
| Population: College / University | 67 | 0.074 | 0.092 | −0.107 | 0.254 | 0.80 | .424 | 1.88 | 3 | .598 | 0.02 | |
| Population: Multiple | 67 | 0.063 | 0.285 | −0.495 | 0.621 | 0.22 | .825 | 1.88 | 3 | .598 | 0.02 | |
| Study Quality | 67 | 0.065 | 0.034 | −0.001 | 0.131 | 1.94 | .053 | 3.75 | 1 | .053 | 0.06 | |
| Measure a : WBIS-M | 67 | 0.140 | 0.064 | 0.015 | 0.266 | 2.19 | .029 | 37.79 | 5 | <.001 | 0.39 | |
| Measure a : WSSQ | 67 | −0.452 | 0.118 | −0.683 | −0.222 | −3.84 | <.001 | 37.79 | 5 | <.001 | 0.39 | |
| Measure a : Translated WBIS | 67 | −0.079 | 0.111 | −0.296 | 0.138 | −0.71 | .475 | 37.79 | 5 | <.001 | 0.39 | |
| Measure a : Translated WSSQ | 67 | −0.328 | 0.113 | −0.550 | −0.106 | −2.89 | .004 | 37.79 | 5 | <.001 | 0.39 | |
| Measure a : AAQW-WS | 67 | −0.081 | 0.140 | −0.356 | 0.195 | −0.57 | .566 | 37.79 | 5 | <.001 | 0.39 | |
| Positive Body Image | Publication Status | 25 | −0.012 | 0.140 | −0.287 | 0.263 | −0.09 | .932 | 0.01 | 1 | .932 | 0.00 |
| Sex/Gender | 25 | −0.001 | 0.003 | −0.007 | 0.005 | −0.17 | .861 | 0.03 | 1 | .861 | 0.00 | |
| Age | 24 | 0.001 | 0.005 | −0.009 | 0.010 | 0.11 | .911 | 0.01 | 1 | .911 | 0.00 | |
| Race | 19 | 0.002 | 0.004 | −0.005 | 0.010 | 0.59 | .554 | 0.35 | 1 | .554 | 0.02 | |
| BMI | 22 | 0.003 | 0.007 | −0.011 | 0.018 | 0.42 | .672 | 0.18 | 1 | .672 | 0.00 | |
| Population: Community | 25 | 0.011 | 0.156 | −0.294 | 0.316 | 0.07 | .945 | 1.62 | 3 | .654 | 0.06 | |
| Population: College / University | 25 | −0.074 | 0.143 | −0.354 | 0.206 | −0.52 | .604 | 1.62 | 3 | .654 | 0.06 | |
| Population: Multiple | 25 | −0.321 | 0.293 | −0.895 | 0.253 | −1.10 | .273 | 1.62 | 3 | .654 | 0.06 | |
| Study Quality | 25 | −0.069 | 0.044 | −0.156 | 0.018 | −1.56 | .118 | 2.44 | 1 | .118 | 0.08 | |
| Measure b : WBIS-M | 25 | −0.131 | 0.103 | −0.334 | 0.072 | −1.27 | .205 | 24.55 | 5 | <.001 | 0.52 | |
| Measure b : WSSQ | 25 | −0.054 | 0.150 | −0.348 | 0.241 | −0.36 | .722 | 24.55 | 5 | <.001 | 0.52 | |
| Measure b : Translated WBIS | 25 | 0.277 | 0.136 | 0.011 | 0.543 | 2.04 | .041 | 24.55 | 5 | <.001 | 0.52 | |
| Measure b : Translated WSSQ | 25 | 0.299 | 0.158 | −0.011 | 0.609 | 1.89 | .059 | 24.55 | 5 | <.001 | 0.52 | |
| Measure b : Other | 25 | 0.578 | 0.168 | 0.249 | 0.906 | 3.44 | <.001 | 24.55 | 5 | <.001 | 0.52 | |
| Self-Devaluation | Publication Status | 32 | 0.017 | 0.142 | −0.261 | 0.295 | 0.12 | .906 | 0.01 | 1 | .906 | 0.00 |
| Sex/Gender | 32 | 0.003 | 0.002 | −0.001 | 0.006 | 1.67 | .095 | 2.78 | 1 | .095 | 0.09 | |
| Age | 32 | 0.010 | 0.003 | 0.004 | 0.016 | 3.31 | <.001 | 10.98 | 1 | <.001 | 0.27 | |
| Race | 19 | 0.001 | 0.001 | −0.001 | 0.004 | 0.85 | .395 | 0.72 | 1 | .395 | 0.07 | |
| BMI | 24 | 0.006 | 0.004 | −0.002 | 0.013 | 1.49 | .136 | 2.23 | 1 | .136 | 0.16 | |
| Population: Community | 32 | −0.172 | 0.107 | −0.382 | 0.039 | −1.60 | .110 | 3.28 | 3 | .351 | 0.10 | |
| Population: College / University | 32 | −0.068 | 0.131 | −0.325 | 0.189 | −0.52 | .605 | 3.28 | 3 | .351 | 0.10 | |
| Population: Multiple | 32 | 0.029 | 0.167 | −0.298 | 0.357 | 0.17 | .861 | 3.28 | 3 | .351 | 0.10 | |
| Study Quality | 32 | 0.084 | 0.040 | 0.005 | 0.163 | 2.09 | .036 | 4.39 | 1 | .036 | 0.13 | |
| Measure b c : WBIS-M | 32 | −0.078 | 0.108 | −0.290 | 0.133 | −0.72 | .469 | 13.17 | 4 | .011 | 0.32 | |
| Measure b c : Translated WBIS | 32 | −0.362 | 0.108 | −0.572 | −0.151 | −3.36 | .001 | 13.17 | 4 | .011 | 0.32 | |
| Measure b c : Translated WSSQ | 32 | −0.267 | 0.138 | −0.537 | 0.003 | −1.94 | .053 | 13.17 | 4 | .011 | 0.32 | |
| Measure b c : Other | 32 | −0.153 | 0.177 | −0.499 | 0.194 | −0.86 | .388 | 13.17 | 4 | .011 | 0.32 | |
| Experienced Weight Stigma | Publication Status | 55 | 0.066 | 0.084 | −0.098 | 0.230 | 0.79 | .429 | 0.63 | 1 | .429 | 0.01 |
| 53 | −0.003 | 0.001 | −0.005 | −0.001 | −2.81 | .005 | 7.88 | 1 | .005 | 0.15 | ||
| Sex/Gender | ||||||||||||
| Age | 55 | −0.004 | 0.002 | −0.009 | 0.0004 | −1.78 | .076 | 3.15 | 1 | .076 | 0.05 | |
| Race | 41 | −0.0002 | 0.002 | −0.003 | 0.003 | −0.16 | .875 | 0.02 | 1 | .875 | 0.00 | |
| BMI | 51 | −0.013 | 0.005 | −0.022 | −0.003 | −2.64 | .008 | 6.97 | 1 | .008 | 0.13 | |
| Population: Community | 55 | −0.021 | 0.081 | −0.180 | 0.138 | −0.26 | .795 | 0.21 | 3 | .975 | 0.00 | |
| Population: College / University | 55 | 0.007 | 0.094 | −0.178 | 0.191 | 0.07 | .944 | 0.21 | 3 | .975 | 0.00 | |
| Population: Multiple | 55 | 0.017 | 0.143 | −0.264 | 0.297 | 0.12 | .907 | 0.21 | 3 | .975 | 0.00 | |
| Study Quality | 55 | −0.015 | 0.030 | −0.074 | 0.045 | −0.48 | .631 | 0.23 | 1 | .631 | 0.00 | |
| Measure b : WBIS-M | 55 | 0.124 | 0.059 | 0.010 | 0.239 | 2.12 | .034 | 13.45 | 5 | .020 | 0.24 | |
| Measure b : WSSQ | 55 | −0.072 | 0.209 | −0.482 | 0.339 | −0.34 | .733 | 13.45 | 5 | .020 | 0.24 | |
| Measure b : Translated WBIS | 55 | 0.117 | 0.103 | −0.085 | 0.320 | 1.14 | .256 | 13.45 | 5 | .020 | 0.24 | |
| Measure b : Translated WSSQ | 55 | 0.445 | 0.146 | 0.159 | 0.732 | 3.05 | .002 | 13.45 | 5 | .020 | 0.24 | |
| Measure b : Other | 55 | 0.315 | 0.186 | −0.049 | 0.678 | 1.70 | .090 | 13.45 | 5 | .020 | 0.24 | |
| Anti-Fat Attitudes | Publication Status | 26 | −0.065 | 0.077 | −0.216 | 0.086 | −0.84 | .400 | 0.71 | 1 | .400 | 0.02 |
| Sex/Gender | 26 | 0.001 | 0.001 | −0.001 | 0.003 | 0.72 | .475 | 0.51 | 1 | .475 | 0.03 | |
| Age | 26 | 0.0002 | 0.003 | −0.006 | 0.007 | 0.06 | .949 | 0.00 | 1 | .949 | 0.00 | |
| Race | 24 | 0.003 | 0.002 | −0.002 | 0.008 | 1.26 | .208 | 1.59 | 1 | .208 | 0.07 | |
| BMI | 23 | 0.012 | 0.006 | 0.001 | 0.023 | 2.17 | .030 | 4.73 | 1 | .030 | 0.27 | |
| Population: Community | 26 | 0.005 | 0.097 | −0.185 | 0.195 | 0.05 | .960 | 2.82 | 3 | .420 | 0.11 | |
| Population: College / University | 26 | −0.129 | 0.113 | −0.350 | 0.092 | −1.14 | .253 | 2.82 | .420 | 0.11 | ||
| Population: Multiple | 26 | −0.097 | 0.183 | −0.455 | 0.262 | −0.53 | .596 | 2.82 | 3 | .420 | 0.11 | |
| Study Quality | 26 | −0.107 | 0.030 | −0.166 | −0.047 | −3.52 | <.001 | 12.37 | 1 | <.001 | 0.40 | |
| Measureabd: WBIS-M | 26 | −0.051 | 0.071 | −0.190 | 0.089 | −0.72 | .475 | 4.75 | 3 | .191 | 0.23 | |
| Measureabd: WSSQ | 26 | −0.031 | 0.093 | −0.213 | 0.152 | −0.33 | .744 | 4.75 | 3 | .191 | 0.23 | |
| Measureabd: Translated WBIS | 26 | 0.284 | 0.156 | −0.022 | 0.589 | 1.82 | .069 | 4.75 | 3 | .191 | 0.23 | |
| Weight Controllability Beliefs | Publication Status | 18 | −0.023 | 0.071 | −0.161 | 0.116 | −0.32 | .748 | 0.10 | 1 | .748 | 0.03 |
| Sex/Gender | 18 | 0.002 | 0.001 | −0.001 | 0.004 | 1.41 | .158 | 2.00 | 1 | .158 | 0.12 | |
| Age | 18 | −0.003 | 0.003 | −0.010 | 0.004 | −0.85 | .396 | 0.72 | 1 | .396 | 0.05 | |
| Race | 17 | −0.0002 | 0.002 | −0.003 | 0.003 | −0.15 | .882 | 0.02 | 1 | .882 | 0.00 | |
| BMI | 17 | 0.005 | 0.009 | −0.012 | 0.022 | 0.55 | .583 | 0.30 | 1 | .583 | 0.02 | |
| Population: Community | 18 | −0.016 | 0.129 | −0.268 | 0.236 | −0.12 | .901 | 0.49 | 3 | .922 | 0.04 | |
| Population: College / University | 18 | 0.036 | 0.139 | −0.236 | 0.308 | 0.26 | .796 | 0.49 | 3 | .922 | 0.04 | |
| Population: Multiple | 18 | 0.040 | 0.184 | −0.321 | 0.401 | 0.22 | .829 | 0.49 | 3 | .922 | 0.04 | |
| Study Quality | 18 | −0.014 | 0.047 | −0.107 | 0.078 | −0.30 | .763 | 0.09 | 1 | .763 | 0.00 | |
| Measureabde: WBIS-M | 18 | −0.024 | 0.077 | −0.176 | 0.128 | −0.31 | .755 | 0.40 | 2 | .817 | 0.01 | |
| Measureabde: WSSQ | 18 | −0.068 | 0.106 | −0.276 | 0.141 | −0.63 | .526 | 0.40 | 2 | .817 | 0.01 |
Note. All presented models reflect associations between weight bias internalization and the respective correlates for analyses with sufficient data (k≥10); all models used maximum likelihood estimation; publication status = peer-reviewed (0), unpublished (1); sex/gender = percentage of female participants per sample; race = percentage of participants who identified as White per sample; population = a dummy coded variable set with the following categories: community, non-surgical weight loss treatment-seeking (referent category), bariatric, college/university, multiple; for population, non-surgical weight loss treatment-seeking and bariatric categories were combined in models wherein there were non-significant differences between these groups; measure = a dummy coded variable set with the following categories: modified weight bias internalization scale (WBIS-M), WBIS (referent category), Weight Self-Stigma Questionnaire (WSSQ), non-English translations of the WBIS, non-English translations of the WSSQ, Acceptance and Action Questionnaire for Weight-Related Difficulties Weight Self-Stigma Subscale (AAQW-WS), Other measure.
No studies in this model included an Other measure
No studies in the model included the AAQW-WS as a measure
No studies in the model included the English language WSSQ as a measure
No studies in the model included translated versions of the WSSQ as a measure
No studies in the model included translated versions of the WBIS as a measure
Associations between weight bias internalization and other conceptually-related correlates exhibited additional variation as a function of demographic, study-level, and measurement-related factors. In particular, the positive association between greater weight bias internalization and greater self-devaluation was larger in studies with older participants (R2analogue=0.27) and better study quality (R2analogue=0.13), and smaller in studies that used translated versions of the WBIS (versus the original WBIS; R2analogue=0.32). Further, the positive association between greater weight bias internalization and more experienced weight stigma was larger in studies with fewer females (R2analogue=0.15), lower BMIs (R2analogue=0.13), and those that used the WBIS-M and translated versions of WSSQ (versus the original WBIS, note that no studies provided data for this association using the English language WSSQ; R2analogue=0.24). Finally, the positive association between greater weight bias internalization and greater anti-fat attitudes was larger in samples with higher BMIs (R2analogue=0.27) and studies with lower quality (R2analogue=0.40). None of the assessed correlates moderated the association between weight bias internalization and weight controllability beliefs.
Discussion
Weight bias internalization is prevalent and has consistently been associated with adverse mental health outcomes and physiological morbidity (Alimoradi et al., 2019; Emmer et al., 2020; Pearl & Puhl, 2018). However, evidence increasingly suggests that there are notable limitations in the existing conceptualization and operationalization of weight bias internalization. These limitations lower confidence in the state of the literature that has considered this construct and its implications as a correlate of mental and physical health outcomes. The present study aimed to answer recent calls for research to improve the construct validity of weight bias internalization (Austen et al., 2020; Meadows & Higgs, 2020). This was done by conducting a comprehensive quantitative synthesis of associations between weight bias internalization, as currently operationalized, and both aspects of this construct that have been posited to be central to its conceptualization and factors that may be contributing to the jangle fallacy (wherein constructs with different names are measuring the same thing). Results indicated that greater weight bias internalization exhibited large to very large concurrent associations with factors that have been suggested to have considerable overlap with this construct (i.e., negative and positive body image, self-devaluation) as well as general and weight-specific experiential avoidance and individuals’ anticipation of future weight stigma experiences. In contrast, associations were shown to vary in magnitude for other conceptually-related constructs, including prior weight stigma experiences, endorsement of weight biased stereotypes, and weight stigma stereotype awareness. There were also notable moderation effects suggesting that associations between weight bias internalization and related constructs varied as a function of various measurement-related, demographic, and study-level factors. Collectively, these findings provide important information that can help advance weight bias internalization conceptualization and measure refinement moving forward.
Conceptual Overlap
Findings of large effects, which were approximately equal in magnitude, for associations between greater weight bias internalization relative to less positive body image and more negative body image and self-devaluation aligns with a growing body of evidence that has identified considerable overlap between weight bias internalization and measures of body image and self-esteem/self-worth (Austen et al., 2020; Meadows & Higgs, 2020; Pearl et al., 2021). Such evidence raises questions about whether weight bias internalization, as currently operationalized, is truly distinct from aspects of body image and self-esteem. Although the exact implications of this overlap from a conceptual standpoint are not yet fully understood, these findings appear to suggest that the current operationalization of weight bias internalization may be contributing to the jangle fallacy (i.e., when different terms are used to refer to constructs that are posited to differ from one another yet are capturing the same construct). Likewise, in line with recent research that used bifactor analysis to examine the shared and unique amounts of variance that are accounted for in measures of weight bias internalization, body image, and self-devaluation/self-esteem (Meadows & Higgs, 2020), it is plausible that these three constructs tap into a higher-order latent construct reflecting body-related self-judgment. However, it should also be noted that the magnitude of associations between weight bias internalization relative to positive and negative body image and self-devaluation in the present study were large in magnitude (~|.5–.6|) yet nonetheless provide evidence of some degree of construct-specific uniqueness. In future studies that examine the implications of weight bias internalization, it will be important for researchers to control for aspects of body image and/or self-devaluation/self-esteem to determine what independent contribution weight bias internalization makes to the explained variance of the associations of interest.
Further, it is noteworthy that this overlap between weight bias internalization and measures of body image and self-devaluation was shown to vary based on the measures used to operationalize weight bias internalization. First, when compared to the original WBIS, the association between greater weight bias internalization and greater negative body image was larger in studies that used the WBIS-M and smaller in studies that used both the English language and translated versions of the WSSQ. These findings have two particularly important implications. First, the larger magnitude of the association between greater weight bias internalization and greater negative body image for the WBIS-M versus the original WBIS is interesting to consider, given that the primary difference between these measures is that the former replaced references to the term “overweight” with weight-neutral terminology that is applicable to individuals with a variety of body weights (e.g., “As an overweight person…” was changed to “Because of my weight…”). It is possible that such weight-neutral language, which is important from a weight stigma reduction and inclusivity perspective, may also draw out aspects of individuals’ negatively valenced body image to a greater extent than is evident when the term “overweight” is used. Such an explanation would be consistent with evidence that individuals consider terms such as “overweight” and “obesity” to be stigmatizing (Puhl, 2020). Consequently, individuals may be less forthcoming with their responses to items that use these terms if language of this nature makes them feel stigmatized. It will prove useful to consider this possibility further in future research and measure refinement. Second, that the positive association between weight bias internalization and negative body image was smaller in studies that used the English language and translated versions of the WSSQ, when compared to the original WBIS, suggests that the high degree of overlap between weight bias internalization and aspects of negative body image is less apparent when the WSSQ is used, both in its original form and across the cultures that this measure has been translated for. This notion warrants consideration in future measure refinement efforts.
In addition to these measurement differences that were identified for associations between weight bias internalization and aspects of negative body image, results indicated that the association between greater weight bias internalization and more self-devaluation was smaller in studies that used translated versions of the WBIS when compared to the original (and English language) WBIS. Likewise, the association between greater weight bias internalization and less positive body image was smaller in studies that used translated versions of the WBIS versus the original WBIS. This suggests that there may be cultural variations in conceptualizations of weight bias internalization, self-devaluation, positive body image, or perhaps all three constructs, that are evident when the WBIS is used. Notably, few effects were identified for different translated versions of this measure, such that all non-English language versions of the WBIS were categorized within one category in our meta-regression models due to power considerations. Consequently, it is difficult to determine whether this measurement-related difference in associations between weight bias internalization relative to self-devaluation and positive body image can be attributed to a particular language and cultural translation of the WBIS, given that a variety of translations were accounted for in these effects, including Chinese (e.g., Chen et al., 2020; Pakpour et al., 2019), German (e.g., Ciupitu-Plath et al., 2018; Hilbert, Braehler et al., 2014), and Italian (e.g., Innamorati et al., 2017). Future cross-cultural examinations in this area will prove useful in adding clarity in this regard.
Variability across Conceptually-Related Constructs
In the present meta-analysis, associations were shown to vary in magnitude across constructs that have been differentially included in conceptualizations of weight bias internalization and theoretical models of self-stigma (e.g., Corrigan et al., 2009) to date. Consistent with the present finding noted above that greater weight bias internalization was robustly associated with greater self-devaluation, most conceptualizations of weight bias internalization posit that this construct centrally involves a process of self-devaluation due to one’s body weight (Durso & Latner, 2008; Lillis et al., 2010; Pearl & Puhl, 2014). In contrast, some researchers have posited that weight bias internalization involves individuals’ endorsement and application of weight biased stereotypes to themselves (Durso & Latner, 2008; Pearl & Puhl, 2014, 2018). However, the present results indicated that greater weight bias internalization exhibited only a small to moderate sized effect with individuals’ endorsement of weight biased attitudes and stereotypes captured via measures of anti-fat attitudes and that weight bias internalization was not associated with individuals’ weight controllability beliefs (i.e., overweight blame attributions, in which individuals are believed to have higher weights strictly due to personal factors such as a lack of willpower). The small to moderate and trivial magnitude of these effects are important to contextualize with existing theoretical models of internalized stigma (or self-stigma) in the literature more generally, wherein self-stigma is posited to centrally involve individuals’ agreement with adverse beliefs and stereotypes that are associated with a stigmatized identity (e.g., obesity, mental illness; Corrigan et al., 2009). This suggests that the current operationalization of weight bias internalization within the literature may not adequately capture a component of this aspect of self-stigma that appears to warrant representation, namely beliefs and stereotypes related to weight controllability. It may consequently prove useful for future refinements of weight bias internalization measures to ensure that this element is duly represented in pools of candidate items used in the measure refinement or development process.
Implicit within the process of self-stigma more generally is that most individuals previously have experienced weight stigma and/or otherwise view themselves as belonging to a stigmatized group and fear facing stigma (Corrigan et al., 2009; Corrigan & Rao, 2012; Link et al., 1989; Link & Phelan, 2001). The anticipation or fear of future weight stigma experiences, in particular, has specifically been accounted for in two conceptualizations of weight bias internalization (Griffiths et al., 2018; Lillis et al., 2010) and one measure of this construct (i.e., WSSQ; Lillis et al., 2010). In line with this notion, in the present study moderate to large effects were found for associations between greater weight bias internalization and more experienced and anticipated weight stigma. The finding for anticipated weight stigma can only be considered preliminary, given that very few effects (k = 3) were identified for use in this model, and consequently this association was not subjected to additional moderation analyses. In contrast, results indicated that the association between greater weight bias internalization and more experienced weight stigma was larger in studies that used translated versions of the WSSQ (no data using the English language WSSQ were identified for use in this model) and the WBIS-M, when compared to the original (and English language) WBIS. The former finding is consistent with the notion that the WSSQ is the only existing measure of weight bias internalization that includes multiple items that make up a subscale assessing individuals’ experiences and fears of weight stigma. The latter finding may stem from the use of weight-neutral terminology in items comprising the WBIS-M, which may capture or otherwise draw out individuals’ prior experiences of weight stigma to a greater degree than use of the term “overweight” in the original WBIS, possibly due to the stigmatizing nature of terms such as “overweight” and “obese” (Puhl, 2020).
It remains unclear whether and to what extent experienced or anticipated weight stigma warrant consideration in future refinements of the conceptualization and, in turn, operationalization (i.e., via measures) of weight bias internalization. For example, in line with perspectives used to understand self-stigma more generally (e.g., Corrigan et al., 2009; Link et al., 1989), experiences of weight stigma may confirm and strengthen individuals’ self-devaluing beliefs about themselves as individuals who embody negative stereotypes associated with obesity. In turn, individuals may fear future weight stigma experiences that can further confirm and strengthen their negative thoughts and beliefs. Alternatively, experienced or (fears of) anticipated weight stigma may not inherently reflect “core elements” of weight bias internalization but rather factors involved in the development and maintenance of such. These possibilities warrant particular consideration in future research.
It is noteworthy that a very large association was identified between greater weight bias internalization and more weight-related experiential avoidance. Weight-related experiential avoidance, or the process of avoiding negative thoughts and feelings related to one’s weight, has not previously been considered in existing weight bias internalization conceptualizations. However, the magnitude of this effect (>.7) raises the question of whether current measures of weight bias internalization substantively differ from the AAQW, which was used to assess weight-related experiential avoidance in all studies included in this model. Notably, although a recent revision (Palmeira et al., 2016) and additional assessments (Dochat et al., 2020; Weineland et al., 2013) of the AAQW have identified a weight self-stigma subscale within it, the present findings suggest that the full measure may be capturing aspects of weight bias internalization. Alternatively, it is possible that weight-related experiential avoidance is an important aspect of weight bias internalization that has not explicitly been considered as a core element of such to date. This assertion is consistent with the notion that greater weight bias internalization also exhibited a large association with general (not weight-specific) experiential avoidance in the present meta-analysis. These two possibilities warrant assessment moving forward.
Effect Moderation
In addition to the variations identified in effects noted above based on the specific measures of weight bias internalization that were used across studies, various demographic and study-level factors were shown to influence overall effect magnitude. For example, studies in this meta-analysis included participants ranging in age from approximately 10 to 57 years old and the association between greater weight bias internalization and greater self-devaluation was larger in studies with older participants. Although no existing research has provided a longitudinal assessment of changes in this association or weight bias internalization on its own from childhood through adulthood, these findings could help inform future research that takes a developmental approach to understanding changes in this construct that occur over time. For example, over time heightened weight bias internalization may translate to continued increases in negative views of oneself more generally and perhaps in a bidirectional manner. This notion would be consistent with initial short-term (12–24 months post-baseline) longitudinal research that has shown that poorer self-esteem was subsequently associated with higher weight bias internalization among children (Gmeiner & Warschburger, 2020) and that decreases in weight bias internalization were associated with improvements in more general health-related outcomes among adults (Lillis et al., 2019; Olson et al., 2018).
In addition to age moderation effects, the association between greater weight bias internalization and more experienced weight stigma was larger in studies with fewer females and among individuals with lower BMIs. These findings suggest that the implications of having negative weight-related experiences on individuals’ internalization of weight-based self-devaluing beliefs may be especially harmful among males and those with lower body weights. Given that these groups are understudied in the weight bias internalization literature, additional research that examines not only the interconnectivity of weight biased experiences and internalization but also how these factors relate to health-related outcomes over time among these groups is warranted.
The association between greater weight bias internalization and greater explicit anti-fat attitudes was also larger in samples with higher BMIs. Although the implications of this finding are unclear at present, this result is consistent with research that was conducted with individuals with overweight and obesity prior to the development of measures of weight bias internalization. Such research used measures of explicit anti-fat attitudes with individuals with overweight and obesity based on the assumption that examining such beliefs about individuals with higher weights in general among this population was equivalent to measuring weight bias internalization (Durso & Latner, 2008). However, explicit anti-fat attitude measures strictly examine individuals’ beliefs about other individuals with overweight and obesity and do not assess whether individuals consider themselves to be overweight or obese, or apply these beliefs to themselves. It is plausible that the larger magnitude of the positive association that was identified between weight bias internalization and anti-fat attitudes for samples with higher BMIs in this meta-analysis may be tapping into an aspect of weight bias internalization that may be particularly relevant for individuals with higher weights, or perhaps may suggest that individuals with higher weights are more aware of these stereotypes and negative attitudes than their lower weight counterparts. These possibilities could be interesting to explore in future research.
Strengths, Limitations, and Future Directions
The present meta-analysis has various strengths, including the large number of identified effects, the importance of the implications of the present result for this field of study moving forward, and the assessment of a broad range of conceptually-relevant outcomes and moderators. Also, no studies were excluded based on sample or participant demographic characteristic, which improves the potential generalizability of these results. The evidence-base on associations between weight bias internalization and the assessed conceptually-related correlates also has multiple strengths. For example, existing studies in this area have generally included large samples of participants across a wide span of ages and body weights. There is also a good representation of studies that have included clinical samples (e.g., individuals seeking weight loss treatment) and individuals from the communities of many countries. Despite these strengths, various limitations of the literature in this area warrant attention.
A vital limitation of the existing evidence-base on the conceptually-related correlates of weight bias internalization is the predominate focus on females and individuals who identify as White. Likewise, very few of the identified studies provided data on participants’ sexual orientations. Consequently, little is known about whether the observed associations generalize to individuals with a variety of diverse racial, ethnic, gender, and sexual identities. Given that the central aim of this study was to serve as a basis for weight bias internalization conceptualization and measure refinement moving forward, this serves as a vital research gap that warrants attention as this research area continues to advance, in order to ensure that subsequent work exploring weight bias internalization adequately accounts for the experiences of individuals with varied cultural identities.
Although concurrent data permitted the examination of our primary research questions, the lack of prospective effects that were identified for use in the present meta-analysis served as a limitation for investigating other important psychometric questions. Consequently, how the nature and directionality of associations between weight bias internalization and the assessed correlates manifest over time remains unknown. This is important, as such evidence could provide insight into whether certain aspects of weight bias internalization (e.g., self-devaluation, endorsing weight biased stereotypes) are more or less central elements of this construct at different points in individuals’ development of weight bias internalization.
Third, the overlap between weight bias internalization and individuals’ endorsement of weight biased stereotypes was able to be assessed via measures of anti-fat attitudes and weight controllability beliefs. However, no existing studies provided data that independently (i.e., apart from measures of weight bias internalization) accounts for individuals’ application of these stereotypes and beliefs to themselves. Consequently, we were unable to assess whether this aspect of weight bias internalization is adequately captured via existing weight bias internalization measures.
Fourth, there were very few effects identified for associations between weight bias internalization and both weight stigma stereotype awareness and anticipated weight stigma. Consequently, these results can only be considered preliminary at present. Additional research is needed before conclusions regarding whether existing measures of weight bias internalization exhibit adequate amounts of overlap with these constructs.
The central question that warrants assessment in future research is to determine which of the assessed correlates should be considered “core elements” of weight bias internalization and, consequently, should be accounted for in the development of an improved measure of this construct. From a conceptual standpoint, there appears to be a consensus that body image and self-devaluation are both centrally involved in the process of weight bias internalization (Durso & Latner, 2008; Lillis et al., 2010; Pearl & Puhl, 2014), and the present results suggest that weight bias internalization (as currently operationalized) exhibits robust associations with these constructs. However, whether this identified overlap should be considered “too much” and as evidence of the jangle fallacy is unclear and warrants further consideration and empirical scrutiny. In particular, given that body image is a multifaceted construct comprised of cognitive, affective, perceptual, and behavioral elements (Cash, 2004), it will be important for future research to determine if certain aspects of body image exhibit greater degrees of overlap with weight bias internalization than others. Given that associations between weight bias internalization and both negative and positive body image were similarly large in magnitude, these evaluations should involve assessments of types of body image that are both negatively and positively valenced. Future studies that examine the implications of weight bias internalization would also benefit from controlling for measures of body image and/or self-devaluation/self-esteem, to determine weight bias internalization’s independent contribution to the explained variance of the associations of interest (see Gmeiner & Warschburger, 2020 as an example of this nature).
Qualitative research (e.g., interviews, focus groups) that examines what individuals with lived experiences view as central aspects of weight bias internalization will prove essential in future construct refinement and scale development efforts. In addition, in line with the suggestion made by Austen and colleagues (2020), we agree that a Delphi study (in which experts in a given area work together to come to a consensus about a topic; Sumsion, 1998) will prove useful to employ in an effort to determine which factors should be considered the core elements of weight bias internalization and, in turn, accounted for in a subsequent measure development study. Based on the results of the present meta-analysis, such a study would benefit from addressing the following aims. First, it will prove useful to determine which aspects of weight bias internalization that appear to be underrepresented in existing measures of this construct should be better accounted for in a refined weight bias internalization measure. Based on the trivial magnitude of the effect identified in the present meta-analysis for the association between weight bias internalization and weight controllability beliefs (as a measure of individuals’ endorsement of a weight biased stereotype), this factor and perhaps other biased attitudes and stereotypes appear to warrant particular consideration. Second, the field would greatly benefit from identifying ways to ensure that a new measure captures construct-specific aspects of weight bias internalization, rather than those that were shown to exhibit considerable overlap with this construct. In addition to self-devaluation and negative and positive body image as noted above, this effort should have a particular focus on weight-related experiential avoidance, given the very large association identified between weight bias internalization and this construct. Third, there is a need to determine whether having prior weight stigma experiences and anticipating future weight stigma should be considered core elements of weight bias internalization that warrant representation in a measure of this construct. In contrast, it is plausible that these are important factors to consider conceptually (e.g., as constructs that may be involved in the development and maintenance of weight bias internalization), yet that may be best represented in other construct-specific measures. A summary of the directions for future research that were informed by the present meta-analysis can be found in Table 3.
Table 3.
Directions for Future Research Aiming to Improve the Conceptualization and Operationalization of Weight Bias Internalization
| The central question that warrants assessment in future research is to determine which aspects of weight bias internalization that have been included in different conceptualizations of this construct should be considered the “core elements” of weight bias internalization and, consequently, accounted for in the development of an improved measure of this construct. | |
|---|---|
| Findings | Interpretations and Recommendations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Conclusions
Greater weight bias internalization was shown to exhibit large to very large associations with conceptually similar, yet theoretically distinct, constructs (i.e., negative and positive body image, self-devaluation), as well general and weight-specific experiential avoidance and individuals’ anticipation of future weight stigma experiences. In contrast, associations were shown to vary in magnitude for other constructs that have been differentially included in conceptualizations of weight bias internalization to date (i.e., prior weight stigma experiences, endorsement of weight biased stereotypes, and weight stigma stereotype awareness), and as a function of various measurement-related, demographic, and study-level factors. Collectively, these findings provide important information that can advance weight bias internalization conceptualization and measure refinement moving forward.
Supplementary Material
Highlights.
The conceptualization of weight bias internalization (WBI) exhibits limitations
Meta-analysis examined associations between WBI and conceptually-related correlates
Relations varied for constructs that have been included in WBI conceptualizations
The jangle fallacy may be evident with measures of body image and self-devaluation
The jangle fallacy may be evident with measures of experiential avoidance
Funding acknowledgement:
This work was completed in part with support from the National Institute of Mental Health of the National Institutes of Health under award number F31MH120982 to Kelly A. Romano. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None.
Data Availability:
Data used in the present meta-analysis will be made available by the first author upon the receipt of reasonable requests.
References
- Alimoradi Z, Golboni F, Griffiths MD, Broström A, Lin CY, & Pakpour AH (2019). Weight-related stigma and psychological distress: A systematic review and meta-analysis. Clinical Nutrition, 39, 2001–2013. 10.1016/j.clnu.2019.10.016 [DOI] [PubMed] [Google Scholar]
- Austen E, Pearl RL, & Griffiths S (2020). Inconsistencies in the conceptualisation and operationalisation of internalized weight stigma: A potential way forward. Body Image, 36. 10.1016/j.bodyim.2020.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, & Rothstein HR (2009). Introduction to meta-analysis. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Borenstein M, Hedges L, Higgins J, & Rothstein H (2014). Comprehensive meta-analysis: Version 3.0
- Braun TD, Quinn DM, Stone A, Gorin AA, Ferrand J, Puhl RM, … & Papasavas P (2020). Weight bias, shame, and self-compassion: Risk/protective mechanisms of depression and anxiety in prebariatic surgery patients. Obesity, 28(10), 1974–1983. 10.1002/oby.22920 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Cash TF (2004). Body image: Past, present, and future. Body Image. 10.1016/S1740-1445(03)00011-1 [DOI] [PubMed] [Google Scholar]
- Chen H, Ye Y, & Guo J (2020). Impact of weight stigma on preadolescents’ and adolescents’ disordered eating behaviors: Testing two mediation models. Social Behavior and Personality: An International Journal, 48(10), e9392. 10.2224/sbp.9392 [DOI] [Google Scholar]
- Ciupitu-Plath C, Wiegand S, & Babitsch B (2018). The Weight Bias Internalization Scale for Youth: Validation of a specific tool for assessing internalized weight bias among treatment-seeking German adolescents with overweight. Journal of Pediatric Psychology, 43(1), 40–51. 10.1093/jpepsy/jsx079 [DOI] [PubMed] [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112(1), 155–159. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, & Rao D (2012). On the self-stigma of mental illness: Stages, disclosure, and strategies for change. The Canadian Journal of Psychiatry, 57(8), 464–469. 10.1177/070674371205700804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Larson JE, & Ruesch N (2009). Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry, 8(2), 75–81. 10.1002/j.2051-5545.2009.tb00218.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dochat C, Afari N, Wooldridge JS, Herbert MS, Gasperi M, & Lillis J (2020). Confirmatory factor analysis of the Acceptance and Action Questionnaire for Weight-Related Difficulties-Revised (AAQW-R) in a United States sample of adults with overweight and obesity. Journal of Contextual Behavioral Science, 15, 189–196. 10.1016/j.jcbs.2020.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durso LE, & Latner JD (2008). Understanding Self-directed Stigma: Development of the Weight Bias Internalization Scale. Obesity, 16, S80–S86. 10.1038/oby.2008.448 [DOI] [PubMed] [Google Scholar]
- Emmer C, Bosnjak M, & Mata J (2020). The association between weight stigma and mental health: A meta-analysis. Obesity Reviews, 21(1), e12935. 10.1111/obr.12935 [DOI] [PubMed] [Google Scholar]
- Forbes Y, & Donovan C (2019). The role of internalised weight stigma and self-compassion in the psychological well-being of overweight and obese women. Australian Psychologist, 54, 471–482. 10.1111/ap.12407 [DOI] [Google Scholar]
- Gmeiner MS, & Warschburger P (2020). Intrapersonal predictors of weight bias internalization among elementary school children: A prospective analysis. BMC pediatrics, 20(1), 1–9. 10.1186/s12887-020-02264-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths C, Williamson H, Zucchelli F, Paraskeva N, & Moss T (2018). A systematic review of the effectiveness of Acceptance and Commitment Therapy (ACT) for body image dissatisfaction and weight self-stigma in adults. Journal of Contemporary Psychotherapy, 48(4), 189–204. 10.1007/s10879-018-9384-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Braehler E, Haeuser W, & Zenger M (2014). Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity, 22(1), 79–85. 10.1002/oby.20561 [DOI] [PubMed] [Google Scholar]
- Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, & Botella J (2006). Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods, 11, 193–206. 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- Innamorati M, Imperatori C, Lamis DA, Contardi A, Castelnuovo G, Tamburello S, … Fabbricatore M (2017). Weight Bias Internalization Scale discriminates obese and overweight patients with different severity levels of depression: the Italian version of the WBIS. Current Psychology, 36(2), 242–251. 10.1007/s12144-016-9406-6 [DOI] [Google Scholar]
- Lillis J, Luoma JB, Levin ME, & Hayes SC (2010). Measuring Weight Self-stigma: The Weight Self-Stigma Questionnaire. Obesity, 18(5), 971–976. 10.1038/oby.2009.353 [DOI] [PubMed] [Google Scholar]
- Lillis J, Thomas JG, Olson K, & Wing RR (2019). Weight self-stigma and weight loss during behavioural weight loss intervention. Obesity Science & Practice, 5(1), 21–27. 10.1002/osp4.314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, & Dohrenwend BP (1989). A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review, 400–423. [Google Scholar]
- Magallares A, Bolanos-Rios P, Ruiz-Prieto I, de Valle PB, Irles JA, & Jauregui-Lobera I (2017). The mediational effect of weight self-stigma in the relationship between blatant and subtle discrimination and depression and anxiety. Spanish Journal of Psychology, 20. 10.1017/sjp.2017.1 [DOI] [PubMed] [Google Scholar]
- Meadows A, & Higgs S (2020). A bifactor analysis of the Weight Bias Internalization Scale: What are we really measuring?. Body Image, 33, 137–151. 10.1016/j.bodyim.2020.02.013 [DOI] [PubMed] [Google Scholar]
- O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, … O’Brien KS (2016). The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite, 102, 70–76. https://doi-org.proxy.lib.odu.edu/10.1016/j.appet.2016.02.032 [DOI] [PubMed] [Google Scholar]
- Olson KL, Lillis J, Graham Thomas J, & Wing RR (2018). Prospective evaluation of internalized weight bias and weight change among successful weight-loss maintainers. Obesity (19307381), 26(12), 1888–1892. 10.1002/oby.22283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakpour AH, Tsai MC, Lin YC, Strong C, Latner JD, Fungg XCC, Lin CY … Tsang HWH (2019). Psychometric properties and measurement invariance of the Weight Self-Stigma Questionnaire and Weight Bias Internalization Scale in children and adolescents. International Journal of Clinical and Health Psychology, 19(2), 150–159. 10.1016/j.ijchp.2019.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmeira L, Cunha M, & Pinto-Gouveia J (2018). The weight of weight self-stigma in unhealthy eating behaviours: The mediator role of weight-related experiential avoidance. Eating & Weight Disorders, 23(6), 785–796. 10.1007/s40519-018-0540-z [DOI] [PubMed] [Google Scholar]
- Palmeira L, Cunha M, & Pinto-Gouveia J (2019). Processes of change in quality of life, weight self-stigma, body mass index and emotional eating after an acceptance-, mindfulness- and compassion-based group intervention (Kg-Free) for women with overweight and obesity. Journal of Health Psychology, 24(8), 1056–1069. https://doi-org.proxy.lib.odu.edu/10.1177/1359105316686668 [DOI] [PubMed] [Google Scholar]
- Palmeira L, Cunha M, Pinto-Gouveia J, Carvalho S, & Lillis J (2016). New developments in the assessment of weight-related experiential avoidance (AAQW-Revised). Journal of Contextual Behavioral Science, 5(3), 193–200. 10.1016/j.jcbs.2016.06.001 [DOI] [Google Scholar]
- Pearl RL, & Puhl RM (2014). Measuring internalized weight attitudes across body weight categories: Validation of the modified weight bias internalization scale. Body Image, 11(1), 89–92. 10.1016/j.bodyim.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Pearl RL, & Puhl RM (2018). Weight bias internalization and health: A systematic review. Obesity Reviews, 19(8), 1141–1163. 10.1111/obr.12701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, Puhl RM, Lessard LM, Himmelstein MS, & Foster GD (2021). Prevalence and correlates of weight bias internalization in weight management: A multinational study. SSM-Population Health, 13, 100755. 10.1016/j.ssmph.2021.100755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM (2020). What words should we use to talk about weight? A systematic review of quantitative and qualitative studies examining preferences for weight-related terminology. Obesity Reviews, 21(6), e13008. 10.1111/obr.13008 [DOI] [PubMed] [Google Scholar]
- Puhl RM, Himmelstein MS, & Quinn DM (2018). Internalizing weight stigma: prevalence and sociodemographic considerations in US adults. Obesity, 26(1), 167–175. 10.1002/oby.22029 [DOI] [PubMed] [Google Scholar]
- Puhl RM, Himmelstein MS, & Quinn DM (2018). Internalizing weight stigma: Prevalence and sociodemographic considerations in US adults. Obesity, 26(1), 167–175. 10.1002/oby.22029 [DOI] [PubMed] [Google Scholar]
- Romano KA, Heron KE, & Henson JM (2021). Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: Does weight status matter?. Body Image, 37, 38–49. 10.1016/j.bodyim.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt FL, & Hunter JE (2015). Methods of meta-analysis: Correcting error and bias in research findings (3rd ed.). New York, NY: Sage. [Google Scholar]
- Sumsion T (1998). The Delphi technique: An adaptive research tool. British Journal of Occupational Therapy, 61(4), 153–156. 10.1177/030802269806100403 [DOI] [Google Scholar]
- Weineland S, Lillis J, & Dahl J (2013). Measuring experiential avoidance in a bariatric surgery population—Psychometric properties of AAQ-W. Obesity Research & Clinical Practice, 7(6), e464–e475. 10.1016/j.orcp.2012.06.002 [DOI] [PubMed] [Google Scholar]
- Wells GA, Shea B, O’Connell DA, Peterson J, Welch V, Losos M, & Tugwell P (2000). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. [Google Scholar]
- Zuba A, & Warschburger P (2017). The role of weight teasing and weight bias internalization in psychological functioning: a prospective study among school-aged children. European Child & Adolescent Psychiatry, 26(10), 1245–1255. https://doi-org.proxy.lib.odu.edu/10.1007/s00787-017-0982-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in the present meta-analysis will be made available by the first author upon the receipt of reasonable requests.


